Dietary Supplements on Controlling Multiple Sclerosis Symptoms and Relapses: Current Clinical Evidence and Future Perspectives
Abstract
1. Introduction
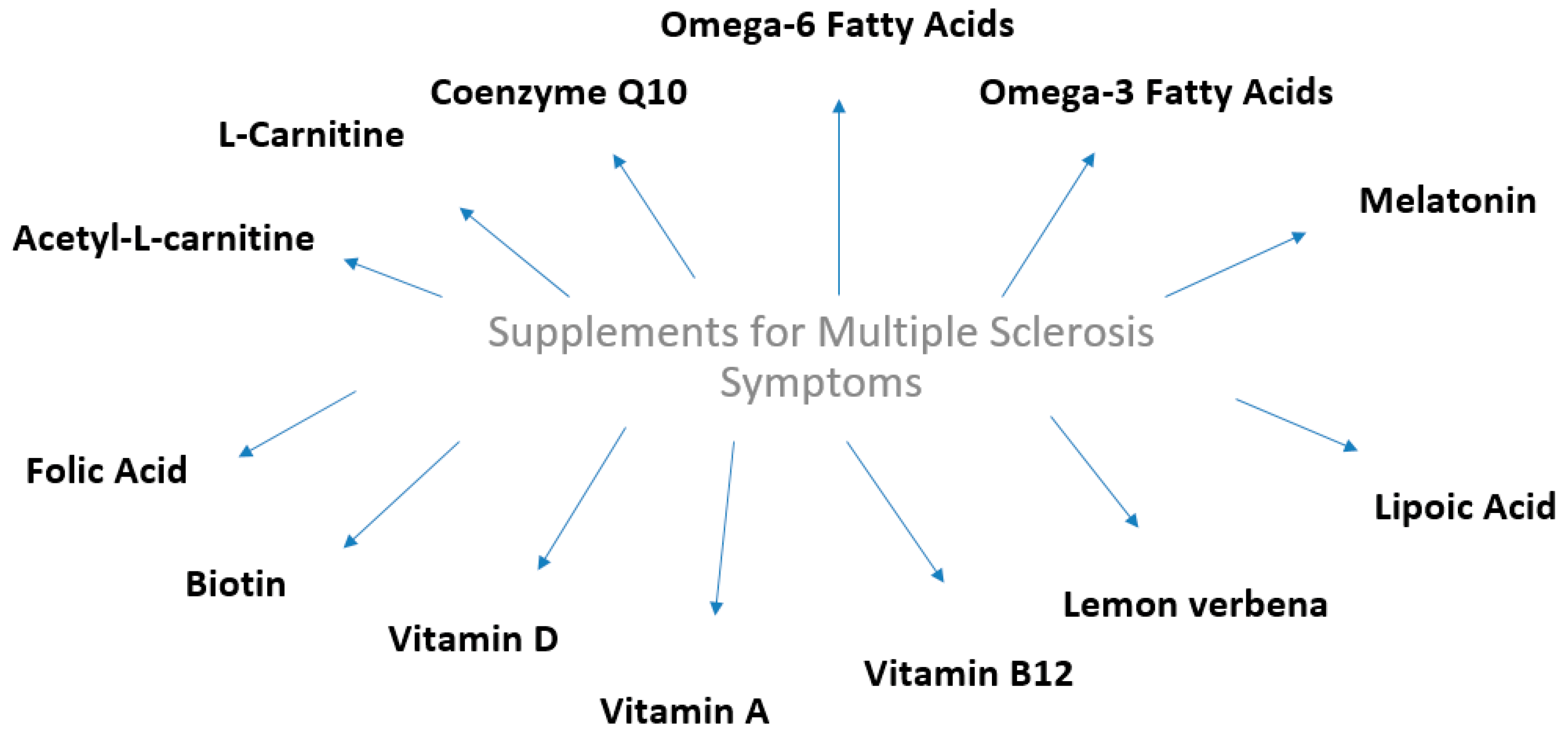
2. Dietary Supplements and Multiple Sclerosis
2.1. Fatty Acids
2.1.1. Omega-6 Fatty Acids
2.1.2. Omega-3 Fatty Acids
2.2. Coenzyme Q10
2.3. Vitamin B7 (Biotin)
2.4. Vitamin A
2.5. Vitamin B12
2.6. Lemon Verbena
2.7. Melatonin
2.8. L-Carnitine and Acetyl-L-Carnitine
2.9. Vitamin D
2.10. Lipoic Acid
2.11. Folic Acid
3. Conclusions
- The evaluation of the composition of the gut microbial load;
- The assessment of the defects of the intestinal immune system;
- The clarification of the role of metabolism of polyphenols and Vitamin D;
- The study the effect of dietary agents, extracts and drugs on the signaling pathways involved in AMPK/SIRT/PPAR cascade or to study the NF-kB transcription factor in the light of the disease;
- The identification of possible interactions between complementary dietary interventions and medication agents taken by the patient with MS.;
- The establishment of a committee to organize a campaign to inform and educate patients about the importance of maintaining a healthy dietary pattern during treatment.
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Gaby, A. Multiple Sclerosis. Glob. Adv. Health Med. 2013, 1, 50–56. [Google Scholar] [CrossRef] [PubMed]
- Warren, S.A.; Janzen, W.; Warren, K.G.; Svenson, L.W.; Schopflocher, D.P. Multiple Sclerosis Mortality Rates in Canada, 1975–2009. Can. J. Neurol. Sci. 2016, 43, 134–141. [Google Scholar] [CrossRef] [PubMed]
- Poppe, A.Y.; Wolfson, C.; Zhu, B. Prevalence of multiple sclerosis in Canada: A systematic review. Can. J. Neurol. Sci. 2008, 5, 593–601. [Google Scholar] [CrossRef] [PubMed]
- Files, D.K.; Jausurawong, T.; Katrajian, R.; Danoff, R. Multiple sclerosis. Prim. Care 2015, 2, 159–175. [Google Scholar] [CrossRef] [PubMed]
- Kurtzke, J.F. Rating neurologic impairment in multiple sclerosis: An expanded disability status scale (EDSS). Neurology 1983, 11, 1444–1452. [Google Scholar] [CrossRef] [PubMed]
- Orton, S.M.; Wald, L.; Confavreux, C.; Vukusic, S.; Krohn, J.P.; Ramagopalan, S.V.; Herrera, B.M.; Sadovnick, A.D.; Ebers, G.C. Association of UV radiation with multiple sclerosis prevalence and sex ratio in France. Neurology 2011, 76, 425–431. [Google Scholar] [CrossRef] [PubMed]
- Dorman, E.; Kansal, A.R.; Sarda, S. The budget impact of introducing delayed-release dimethyl fumarate for treatment of relapse-remitting multiple sclerosis in Canada. J. Med. Econ. 2015, 12, 1085–1091. [Google Scholar] [CrossRef]
- Bates, D.; Fawcett, P.R.W.; Shaw, D.A.; Weightman, D. Polyunsaturated fatty acids in treatment of acute remitting multiple sclerosis. Br. Med. J. 1978, 2, 1390–1391. [Google Scholar] [CrossRef]
- Bates, D.; Cartlidge, N.E.; French, J.M.; Jackson, M.J.; Nightingale, S.; Shaw, D.A.; Smith, S.; Woo, E.; Hawkins, S.A.; Millar, J.H. A double-blind controlled trial of long chain n-3 polyunsaturated fatty acids in the treatment of multiple sclerosis. J. Neurol. Neurosurg. Psychiatry 1989, 52, 18–22. [Google Scholar] [CrossRef]
- Weinstock-Guttman, B.; Baier, M.; Park, Y.; Feichter, J.; Lee-Kwen, P.; Gallagher, E.; Venkatraman, J.; Meksawan, K.; Deinehert, S.; Pendergast, D.; et al. Low fat dietary intervention with ω-3 fatty acid supplementation in multiple sclerosis patients. Prostaglandins Leukot. Essent. Fatty Acids 2005, 73, 397–404. [Google Scholar] [CrossRef]
- Shinto, L.; Marracci, G.; Baldauf-Wagnera, S.; Strehlow, A.; Yadav, V.; Stubera, L.; Bourdettea, D. Omega-3 fatty acid supplementation decreases matrix metalloproteinase-9 production in relapsing-remitting multiple sclerosis. Prostaglandins Leukot. Essent. Fatty Acids 2009, 80, 131–136. [Google Scholar] [CrossRef] [PubMed]
- Sanoobar, M.; Dehghan, P.; Khalili, M.; Azimi, A.; Seifar, F. Coenzyme Q10 as a treatment for fatigue and depression in multiple sclerosis patients: A double blind randomized clinical trial. Nutr. Neurosci. 2015, 3, 138–143. [Google Scholar] [CrossRef] [PubMed]
- Sanoobar, M.; Eghtesadi, S.; Azimi, A.; Khalil, M.; Khodadadi, B. Coenzyme Q10 supplementation ameliorates inflammatory markers in patients with multiple sclerosis a double blind, placebo, controlled randomized clinical trial. Nutr. Neurosci. 2015, 18, 169–176. [Google Scholar] [CrossRef] [PubMed]
- Sanoobar, M.; Eghtesadi, S.; Azimi, A.; Khalili, M.; Jazayeri, S. Coenzyme Q10 supplementation reduces oxidative stress and increases antioxidant enzyme activity in patients with relapsing–remitting multiple sclerosis. Int. J. Neurosci. 2013, 123, 776–782. [Google Scholar] [CrossRef] [PubMed]
- Sedel, F.; Papeix, C.; Bellanger, A.; Touitou, V.; Lebrun-Frenay, C.; Galanaud, D.; Gout, O.; Lyon-Caen, O.; Tourbah, A. High doses of biotin in chronic progressive multiple sclerosis: A pilot study. Mult. Scler. Relat. Disord. 2015, 4, 159–169. [Google Scholar] [CrossRef] [PubMed]
- Tourbah, A.; Lebrun-Frenay, C.; Edan, G.; Clanet, M.; Papeix, C.; Vukusic, S.; De Sèze, J.; Debouverie, M.; Gout, O.; Clavelou, P.; et al. MD1003 (high-dose biotin) for the treatment of progressive multiple sclerosis: A randomised, double-blind, placebo-controlled study. Mult. Scler. J. 2016, 22, 1719–1731. [Google Scholar] [CrossRef]
- Sahraian, M.A.; Nafissi, S.; Togha, M.; BeladiMoghadam, N.; Roostaei, T.; Siassi, F.; Eshraghian, M.R.; Ghanaati, H.; Hanrchian, M.H. Impact of Vitamin A Supplementation on Disease Progression in Patients with Multiple Sclerosis. Arch. Iran. Med. 2015, 18, 435–440. [Google Scholar]
- Bitarafan, S.; Saboor-Yaraghi, A.; Sahraian, M.A.; Soltani, D.; Nafissi, S.; Togha, M.; Moghadam, N.B.; Roostaei, T.; Honarvar, N.M.; Harirchian, M.H. Effect of Vitamin A Supplementation on fatigue and depression in Multiple Sclerosis patients: A Double-Blind Placebo-Controlled Clinical Trial. Iran. J. Allergy Asthma Immunol. 2016, 15, 13–19. [Google Scholar]
- Mauriz, E.; Vallejo, D.; Tuñón, M.J.; Rodriguez-López, J.M.; Rodríguez-Pérez, R.; Sanz-Gómez, J.; del Camino García-Fernández, M. Effects of dietary supplementation with lemon verbena extracts on serum inflammatory markers of multiple sclerosis patients. Nutr. Hosp. 2015, 31, 764–771. [Google Scholar]
- Ledineka, A.; Sajkob, M.; Rotaa, U. Evaluating the effects of amantadin, modafinil and acetyl-l-carnitine on fatigue in multiple sclerosis—Result of a pilot randomized, blind study. Clin. Neurol. Neurosurg. 2013, 115, S86–S89. [Google Scholar] [CrossRef]
- Toghianifar, Ν.; Ashtari, F.; Zarkesh-Esfahani, S.H.; Mansourian, M. Effect of high dose vitamin D intake on interleukin-17 levels in multiple sclerosis: A randomized, double-blind, placebo-controlled clinical trial. J. Neuroimmunol. 2015, 285, 125–128. [Google Scholar] [CrossRef]
- Achiron, A.; Givon, U.; Magalashvili, D.; Dolev, M.; Liraz Zaltzman, S.; Kalron, A.; Stern, Y.; Mazor, Z.; Ladkani, D.; Barak, Y. Effect of Alfacalcidol on multiple sclerosisrelated sclerosisrelated placebo-controlled study. Mult. Scler. J. 2015, 21, 767–775. [Google Scholar] [CrossRef]
- Baker, R.W.R.; Thompson, R.H.S.; Zilkha, K.J. Serum fatty acids in multiple sclerosis. J. Neurol. Neurosurg. Psychiatry 1964, 5, 408–414. [Google Scholar] [CrossRef]
- Belin, J.; Pettet, N.; Smith, A.D.; Thompson, R.H.S.; Zilkha, K.J. Linoleate metabolism in multiple sclerosis. J. Neurol. Neurosurg. Psychiatry 1971, 34, 25–29. [Google Scholar] [CrossRef]
- Tsang, W.M.; Belin, J.; Monro, J.A.; Smith, A.D.; Thompson, R.H.; Zilkha, K.J. Relationship between plasma and lymphocyte linoleate in multiple sclerosis. J. Neurol. Neurosurg. Psychiatry 1976, 8, 767–771. [Google Scholar] [CrossRef][Green Version]
- Yoshida, M.; Takase, S.; Itahara, K.; Nakanishi, T. Linoleate and fatty acid compositions in the serum lipids of Japanese patients with multiple sclerosis. Acta Neurol. Scand. 1983, 68, 362–364. [Google Scholar] [CrossRef]
- Rammohan, K.W. Cerebrospinal fluid in multiple sclerosis. Ann. Indian Acad. Neurol. 2009, 12, 246–253. [Google Scholar] [CrossRef]
- Gupta, J.K.; Ingegno, A.P.; Cook, A.W.; Pertschuk, L.P. Multiple sclerosis and malabsorption. Am. J. Gastroenterol. 1977, 68, 560–566. [Google Scholar]
- Millar, J.H.; Zilkha, K.J.; Langman, M.J.S.; Wright, H.P.; Smith, A.D.; Belin, J.; Thompson, R.H.S. Double-blind trial of linoleate supplementation of the diet in multiple sclerosis. Br. Med. J. 1973, 1, 765–768. [Google Scholar] [CrossRef]
- Paty, D.W.; Cousin, H.K.; Read, S.; Adlakha, K. Linoleic acid in multiple sclerosis: Failure to show any therapeutic benefit. Acta Neurol. Scand. 1978, 58, 53–58. [Google Scholar] [CrossRef]
- Dworkin, R.H.; Bates, D.; Millar, J.H.; Paty, D.W. Linoleic acid and multiple sclerosis: A reanalysis of three double-blind trials. Neurology 1984, 11, 1441–1445. [Google Scholar] [CrossRef]
- Mirshafiey, A.; Asghari, B.; Ghalamfarsa, G.; Jadidi-Niaragh, F.; Azizi, G. The Significance of Matrix Metalloproteinases in the Immunopathogenesis and Treatment of Multiple Sclerosis. Sultan Qaboos Univ. Med. J. 2014, 14, e13. [Google Scholar] [CrossRef]
- Sedel, F.; Bernard, D.; Mock, D.M.; Tourbah, A. Targeting demyelination and virtual hypoxia with high-dose biotin as a treatment for progressive multiple sclerosis. Neuropharmacology 2016, 110, 644–653. [Google Scholar] [CrossRef]
- Birnbaum, G.; Stulc, J. High dose biotin as treatment for progressive multiple sclerosis. Mult. Scler. Relat. Disord. 2017, 18, 141–143. [Google Scholar] [CrossRef]
- Maillart, E.; Mochel, F.; Acquaviva, C.; Maisonobe, T.; Stankoff, B. Severe transient myopathy in a patient with progressive multiple sclerosis after high-dose biotin. Neurology 2019, 92, 1060–1062. [Google Scholar] [CrossRef]
- Abdolahi, M.; Yavari, P.; Honarvar, N.M.; Bitarafan, S.; Mahmoudi, M.; Saboor-Yaraghi, A.A. Molecular Mechanisms of the Action of Vitamin A in Th17/Treg Axis in Multiple Sclerosis. J. Mol. Neurosci. 2015, 57, 605–613. [Google Scholar] [CrossRef]
- Løken-Amsrud, K.I.; Myhr, K.M.; Bakke, S.J.; Beiske, A.G.; Bjerve, K.S.; Bjørnarå, B.T.; Hovdal, H.; Lilleås, F.; Midgard, R.; Pedersen, T.; et al. Retinol levels are associated with magnetic resonance imaging outcomes in multiple sclerosis. Mult. Scler. J. 2013, 19, 451–457. [Google Scholar] [CrossRef]
- Cassani, B.; Villablanca, E.J.; Calisto, J.; Wang, S.; Mora, R.J. Vitamin A and immune regulation: Role of retinoic acid in gut-associated dendritic cell education, immune protection and tolerance. Mol. Asp. Med. 2012, 33, 63–76. [Google Scholar] [CrossRef]
- Eriksen, A.B.; Berge, T.; Gustavsen, M.W.; Leikfoss, I.S.; Bos, S.D.; Spurkland, A.; Harbo, H.F.; Blomhoff, H.K. Retinoic acid enhances the levels of IL-10 in TLR-stimulated B cells from patients with relapsing-remitting multiple sclerosis. J. Neuroimmunol. 2015, 278, 11–18. [Google Scholar] [CrossRef]
- Jafarirad, S.; Siassi, F.; Harirchian, M.H.; Amani, R.; Bitarafan, S.; Saboor-Yaraghi, A. The effect of vitamin a supplementation on biochemical parameters in multiple sclerosis patients. Iran. Red Crescent Med. J. 2013, 15, 194–198. [Google Scholar] [CrossRef][Green Version]
- Wade, D.T.; Young, C.A.; Chaudhuri, K.R.; Davidson, D.W. A randomised placebo controlled exploratory study of vitamin B-12, lofepramine, and L-phenylalanine (the “Cari Loder regime”) in the treatment of multiple sclerosis. J. Neurol. Neurosurg. Psychiatry 2002, 73, 246–249. [Google Scholar] [CrossRef]
- Kira, J.; Tobimatsu, S.; Goto, I. Vitamin B12 metabolism and massive-dose methyl vitamin B12 therapy in Japanese patients with multiple sclerosis. Intern. Med. 1994, 33, 82–86. [Google Scholar] [CrossRef]
- Wurtman, R. Multiple Sclerosis, Melatonin, and Neurobehavioral Diseases. Front. Endocrinol. 2017, 8, 280. [Google Scholar] [CrossRef]
- Adamczyk-Sowa, M.; Pierzchala, K.; Sowa, P.; Polaniak, R.; Kukla, M.; Hartel, M. Influence of melatonin supplementation on serum antioxidative properties and impact of the quality of life in Multiple Sclerosis patients. J. Physiol. Pharmacol. 2014, 64, 543–550. [Google Scholar]
- Golan, D.; Ram, E.; Glass-Marmor Lavi, I.; Rozenberg, O.; Dishon, S. The influence of vitamin D supplementation on melatonin status in patients with multiple sclerosis. Brain Behav. Immun. 2013, 32, 180–185. [Google Scholar] [CrossRef]
- Lebrun, C.; Alchaar, H.; Candito, M.; Bourg, V.; Chatel, M. Levocarnitine administration in multiple sclerosis patients with immunosuppressive therapy-induced fatigue. Mult. Scler. J. 2006, 12, 321–324. [Google Scholar] [CrossRef]
- Tomassinia, V.; Pozzillia, C.; Onestia, E.; Pasqualetti, P.; Marinellia, F.; Pisania, A.; Fieschi, C. Comparison of the effects of acetyl L-carnitine and amantadine for the treatment of fatigue in multiple sclerosis: Results of a pilot, randomised, double-blind, crossover trial. J. Neurol. Sci. 2004, 218, 103–108. [Google Scholar] [CrossRef]
- Drezner, M.; Rosen, C.; Mulder, J. Patient Information: Vitamin d Deficiency: Beyond the Basics. Available online: http://www.lernergyn.com/DataDownloadFiles/bone%20health_Patient%20information%20Vitamin%20D%20deficiency%20(The%20Basics)(UpToDate)%20.pdf (accessed on 12 September 2019).
- Raghuwanshi, A.; Joshi, S.S.; Christakos, S. Vitamin D and multiple sclerosis. J. Cell Biochem. 2008, 2, 338–343. [Google Scholar] [CrossRef]
- Smolders, J.; Hupperts, R.; Barkhof, F.; Grimaldi, L.; Holmoy, T. Efficacy of vitamin D3 as add-on therapy in patients with relapsing–remitting multiple sclerosis receiving subcutaneous interferon beta-1a: A Phase II, multicenter, double-blind, randomized, placebo-controlled trial. J. Neurol. Sci. 2011, 311, 44–49. [Google Scholar] [CrossRef]
- Najafipoor, Α.; Roghanian, Ρ.; Zarkesh-Esfahani, S.H.; Bouzari, M.; Etemadifar, M. The beneficial effects of vitamin D3 on reducing antibody titers against Epstein–Barr virus in multiple sclerosis patients. Cell. Immunol. 2015, 294, 9–12. [Google Scholar] [CrossRef]
- Lossius, A.; Riise, T.; Pugliatti, M.; Bjørnevik, K.; Casetta, I.; Drulovic, J.; Granieri, E.; Kampman, M.T.; Landtblom, A.M.; Lauer, K.; et al. Season of infectious mononucleosis and risk of multiple sclerosis at different latitudes; the EnvIMS Study. Mult. Scler. J. 2014, 20, 669–674. [Google Scholar] [CrossRef]
- Kubicka, K.; Pierzcha, K. Concentration of 25(OH)D3 and calcium and phosphorus metabolism in patients suffering from relapsing-remitting multiple sclerosis. A pilot study. Neurologia i Neurochirurgia Polska 2013, 2, 126–130. [Google Scholar] [CrossRef][Green Version]
- Mahon, B.D.; Gordon, S.A.; Cruzb, J.; Cosman, F.; Cantorn, M.T. Cytokine profile in patients with multiple sclerosis following vitamin D supplementation. J. Neuroimmunol. 2003, 134, 128–132. [Google Scholar] [CrossRef]
- Burton, J.M.; Kimball, S.; Vieth, R.; Bar-Or, A.; Dosch, H.M.; Cheung, R.; Gagne, D.; D’souza, C.; Ursell, M.; O’connor, P. A phase I/II dose-escalation trial of vitamin D3 and calcium in multiple sclerosis. Neurology 2010, 74, 1852–1859. [Google Scholar] [CrossRef]
- Åivo, J.; Hänninenb, A.; Ilonen, J.; Soilu-Hänninen, M. Vitamin D3 administration to MS patients leads to increased serum levels of latency activated peptide (LAP) of TGF-beta. J. Neuroimmunol. 2015, 280, 12–15. [Google Scholar] [CrossRef]
- Muris, A.H.; Smolders, J.; Rolf, L.; Thewissen, M.; Hupperts, R.; Damoiseaux, J.; SOLARIUM Study Group. Immune regulatory effects of high dose vitamin D3 supplementation in a randomized controlled trial in relapsing remitting multiple sclerosis patients receiving IFNβ; the SOLARIUM study. J. Neuroimmunol. 2016, 300, 47–56. [Google Scholar] [CrossRef]
- Muris, A.H.; Smolders, J.; Rolf, L.; Klinkenberg, L.J.; van der Linden, N.; Meex, S.; Damoiseaux, J.; Hupperts, R. Vitamin D Status Does Not Affect Disability Progression of Patients with Multiple Sclerosis over Three Year Follow-Up. PLoS ONE 2016, 11, e0156122. [Google Scholar] [CrossRef]
- Holmøy, T.; Lindstrøm, J.C.; Eriksen, E.F.; Steffensen, L.H. High dose vitamin D supplementation does not affect biochemical bone markers in multiple sclerosis—A randomized controlled trial. BMC Neurol. 2017, 17, 67. [Google Scholar] [CrossRef]
- Steffensen, L.H.; Jørgensen, L.; Straume, B.; Mellgren, S.I.; Kampman, M.T. Can vitamin D3 supplementation prevent bone loss in persons with MS? A placebo-controlled trial. J. Neurol. 2011, 258, 1624–1631. [Google Scholar] [CrossRef]
- Golan, D.; Halhal, B.; Glass-Marmor, L.; Staun-Ram, E.; Rozenberg, O.; Lavi, I.; Dishon, S.; Barak, M.; Ish-Shalom, S.; Miller, A. Vitamin D supplementation for patients with multiple sclerosis treated with interferon-beta: A randomized controlled trial assessing the effect on flu-like symptoms and immunomodulatory properties. BMC Neurol. 2013, 13, 60. [Google Scholar] [CrossRef]
- Khalili, M.; Eghtesadi, S.; Mirshafiey, A.; Eskandari, G.; Sanoobar, M.; Sahraian, M.A.; Motevalian, A.; Norouzi, A.; Moftakhar, S.; Azimi, A. Effect of lipoic acid consumption on oxidative stress among multiple sclerosis patients: A randomized controlled clinical trial. Nutr. Neurosci. 2014, 17, 16–20. [Google Scholar] [CrossRef]
- Yadav, V.; Marracci, G.; Lovera, J.; Woodward, W.; Bogardus, K.; Marquardt, W.; Shinto, L.; Morris, C.; Bourdette, D. Lipoic acid in multiple sclerosis: A pilot study. Mult. Scler. J. 2005, 11, 159–165. [Google Scholar] [CrossRef]
- Isager, H. Serum folate in patients with multiple sclerosis. Acta Neurol. Scand. 1970, 46, 238–242. [Google Scholar] [CrossRef]
| Dietary Supplement | Study Type | Measured Parameters | Number of Patients and Type of MS | Supplement Administration | Effects | References |
|---|---|---|---|---|---|---|
| FA | Double-blind control clinical study | Relapse rates | 116 MS | 2 groups received linoleic acid, and 2 control groups received oleic acid | 20 g linoleic acid marginally affected the duration and severity of relapses of MS but had no effect on overall disability | [8] |
| Ω-3 FA | Double-blind control clinical study | Kurtzke Disability Status Scale Score | 112 RRMS | 10 g/day of FO and diet or placebo OO and diet | After 2 years, 51% of patients in the FO group and 41.4% of those OO group showed improved or unchanged scores, according to the Kurtzke Disability Status Scale | [9] |
| Ω-3 FA | Double-blind clinical study | Qol questionnaire: Neurological status and relapse rate | 31 RRMS | 1 group received a low fat diet (15% fat) with FO and 1 group received the AHA Step I diet (fat 30%) with OO | Decreased fatigue on the OO group at 6 months. Both groups had reduced relapse rates compared to the rates during the 1 year prior to the study | [10] |
| Ω-3 FA | Open-label designed clinical study | Immune cell secretion of MMP-9 | 10 RRMS | ω-3 FA for 3 months | ω-3 FA decreased MMP-9 levels, while their immune cell secretion of MMP-9 was considerably reduced by 58% after 3-months and a significant increase in ω-3 FA levels in red blood cell membranes was recorded | [11] |
| CoQ10 | Controlled randomized double-blinded clinical study | Inflammatory markers (TNF-α, IL-6, and MMP-9) | 48 RRMS | 500 mg CoQ10/day and or placebo for 12 weeks | CoQ10 supplementation at a dose of 500 mg/day may improve fatigue and depression in MS patients | [12] |
| CoQ10 | Controlled randomized double-blinded clinical study | TNF-α levels | 48 RRMS | 500 mg CoQ10/day and or placebo for 12 weeks | TNF-α levels decreased significantly in the CoQ10 group. CoQ10 supplementation also resulted in decreased serum levels of MMP-9 as compared to the placebo group | [13] |
| CoQ10 | Controlled randomized double-blinded clinical study | MDA, TAC and antioxidant markers (SOD, GPx) | 48 RRMS | 500 mg CoQ10/day and or placebo for 12 weeks | Decrease of oxidative stress and increase antioxidant enzyme activity in RRMS | [14] |
| Vitamin B7 (Biotin) | Uncontrolled, non-blinded proof of concept study | Quantitative and qualitative measures: Visual actuality, magnetic resonance spectroscopy (H-MRS) of the Choline/Creatine ratio, disability and progression in progressive MS. | 23 MS | 100–300 mg/day biotin for a period from 2 to 36 months | High biotin doses exerted a positive effect on disability and progression in this MS patient population | [15] |
| Vitamin B7 (Biotin) | Double-blind, placebo-controlled study | (EDSS) score: Reversal of MS-related disability. | 154 PRMS | MD1003 (biotin 100 mg) or placebo orally thrice daily | Reduction EDSS progression and improved clinical impression of change compared with placebo | [16] |
| Vitamin A | Controlled randomized clinical study | Relapse rate: (EDSS) and (MSFC) | 101 RRMS | 25,000 IU/dretinyl palmitate for 6 months followed by 10,000 IU/d retinylpalitate for another 6 months | Reduction of progression of disability, upper limb and cognitive functions | [17] |
| Vitamin A | Controlled randomized clinical study | Modified fatigue impact scale and Beck Depression Inventory-II (fatigue and depression) | 101 RRMS | 25,000 IU/dretinyl palmitate for 6 months followed by 10,000 IU/d retinyl palitate for another 6 months | Vitamin A improved the depression through the modulation of inflammatory conditions | [18] |
| Lemon verbena | Randomized double-blinded placebo-controlled study | Serum levels of C reactive protein and 8 cytokines/ inflammatory markers (IFN-γ, IL-12, IL-23, IL-6, TNF-α, TGF-β, IL-4 and IL-10) | 30 MS | Lemon verbena supplementation (10% w/w verbascoside) | After 28 days, CRP concentrations were considerably lower in SPMS patients compared to the placebo group, IFN-γ levels decreased for all MS-treated groups, whereas reduced IL-12 levels for RRMS patients were noted. Anti-inflammatory cytokine concentrations of IL-4 and IL-10 increased in SPMS patients | [19] |
| ALC | Pilot randomized, blind clinical study | Kurtzke Expanded Disability Status Scale (EDSS) and fatigue | 60 MS | A 1 month treatment with either 200 mg amantadine, 2 g ALC, 200 mg modafinil or placebo | The amantadine treatment for a period of 1 month improved fatigue in RRMS patients as assessed by MFIS | [20] |
| Vitamin D | Controlled randomized double-blinded clinical study | IL-17 levels | 94 RRMS | Received 50,000 IU vitamin D3/5 days for 12 weeks or placebo | IL-17 levels showed significant change in RRMS patients after receiving high dose vitamin D3 for 12 weeks | [21] |
| Alfacalcidol | Controlled randomized double-blinded clinical study | Fatigue Impact Scale (FIS) score | 600 MS | 80 patients received alfacalcidol (1 mcg/) and 78 patients placebo for 6 months | QoL improved in Alfacalcidol-treated patients as compared with placebo. The Alfacalcidol-treated group had reduced number of relapses and higher proportion of relapse-free patients | [22] |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tryfonos, C.; Mantzorou, M.; Fotiou, D.; Vrizas, M.; Vadikolias, K.; Pavlidou, E.; Giaginis, C. Dietary Supplements on Controlling Multiple Sclerosis Symptoms and Relapses: Current Clinical Evidence and Future Perspectives. Medicines 2019, 6, 95. https://doi.org/10.3390/medicines6030095
Tryfonos C, Mantzorou M, Fotiou D, Vrizas M, Vadikolias K, Pavlidou E, Giaginis C. Dietary Supplements on Controlling Multiple Sclerosis Symptoms and Relapses: Current Clinical Evidence and Future Perspectives. Medicines. 2019; 6(3):95. https://doi.org/10.3390/medicines6030095
Chicago/Turabian StyleTryfonos, Christina, Maria Mantzorou, Dimitris Fotiou, Michael Vrizas, Konstantinos Vadikolias, Eleni Pavlidou, and Constantinos Giaginis. 2019. "Dietary Supplements on Controlling Multiple Sclerosis Symptoms and Relapses: Current Clinical Evidence and Future Perspectives" Medicines 6, no. 3: 95. https://doi.org/10.3390/medicines6030095
APA StyleTryfonos, C., Mantzorou, M., Fotiou, D., Vrizas, M., Vadikolias, K., Pavlidou, E., & Giaginis, C. (2019). Dietary Supplements on Controlling Multiple Sclerosis Symptoms and Relapses: Current Clinical Evidence and Future Perspectives. Medicines, 6(3), 95. https://doi.org/10.3390/medicines6030095







