Intermittent Proton Pump Inhibitor Therapy in Low-Risk Non-Variceal Upper Gastrointestinal Bleeding May Be Significantly Cost-Saving
Abstract
1. Introduction
2. Materials and Methods
2.1. Cohort Analysis
2.2. Costing
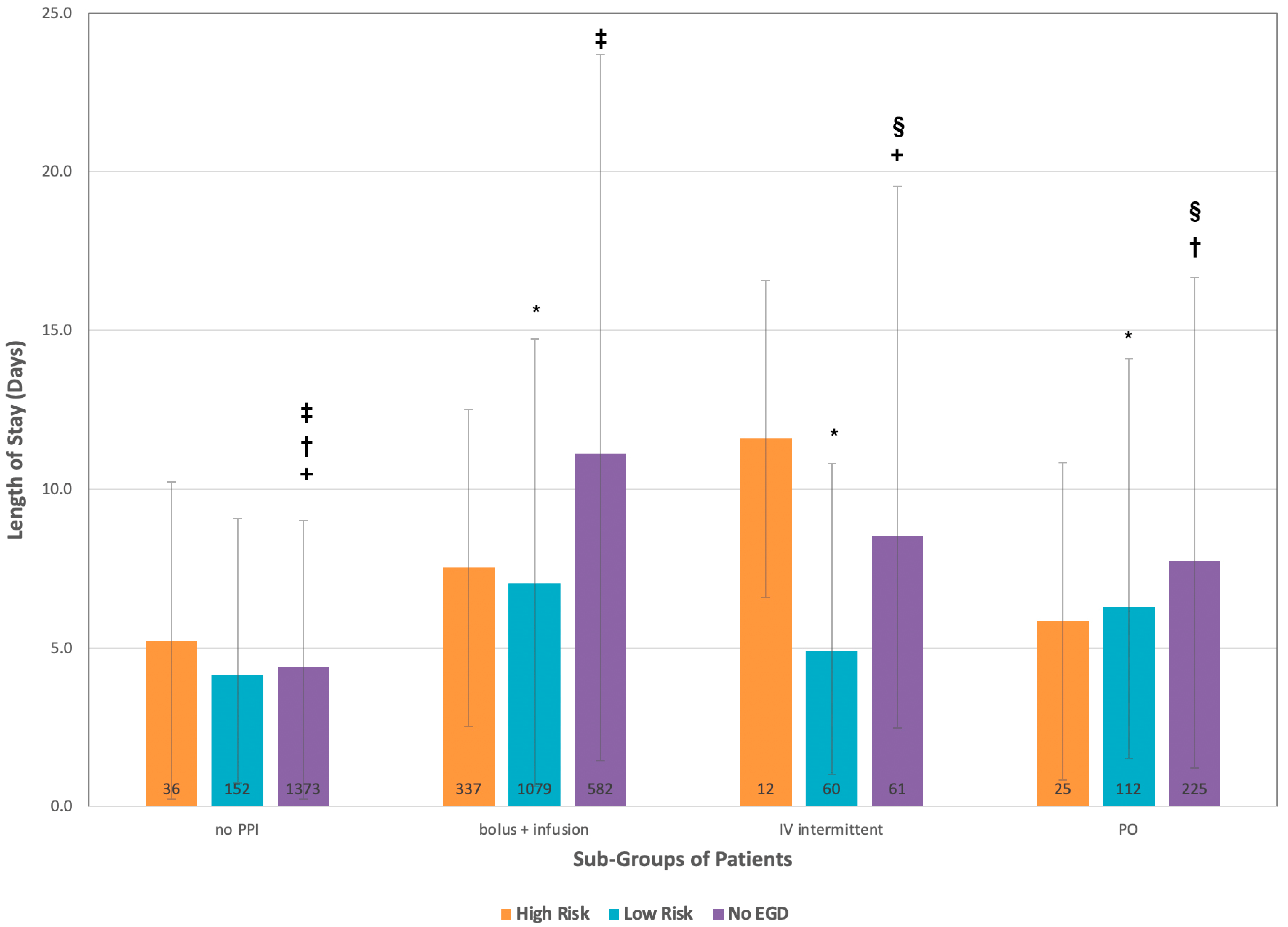
3. Results
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Barkun, A.N.; Bardou, M.; Kuipers, E.J.; Sung, J.; Hunt, R.H.; Martel, M.; Sinclair, P. International Consensus Recommendations on the Management of Patients with Nonvariceal Upper Gastrointestinal Bleeding. Ann. Intern. Med. 2010, 152, 101–113. [Google Scholar] [CrossRef] [PubMed]
- Barkun, A.; Fallone, C.A.; Chiba, N.; Fishman, M.; Flook, N.; Martin, J.; Rostom, A.; Taylor, A.; for the Nonvariceal Upper GI Bleeding Consensus Conference Group A. Canadian Clinical Practice Algorithm for the Management of Patients with Non-Variceal Upper Gastrointestinal Bleeding. Can. J. Gastroenterol. 2004, 18, 605–609. [Google Scholar] [CrossRef] [PubMed]
- Scally, B.; Emberson, J.R.; Spata, E.; Reith, C.; Davies, K.; Halls, H.; Holland, L.; Wilson, K.; Bhala, N.; Hawkey, C.; et al. Effects of Gastroprotectant Drugs for the Prevention and Treatment of Peptic Ulcer Disease and Its Complications: A Meta-Analysis of Randomised Trials. Lancet Gastroenterol. Hepatol. 2018, 3, 231–241. [Google Scholar] [CrossRef] [PubMed]
- Kanno, T.; Yuan, Y.; Tse, F.; Howden, C.W.; Moayyedi, P.; Leontiadis, G.I. Proton Pump Inhibitor Treatment Initiated Prior to Endoscopic Diagnosis in Upper Gastrointestinal Bleeding. Cochrane Database Syst. Rev. 2022, 1, CD005415. [Google Scholar] [CrossRef]
- Lau, J.Y.W.; Sung, J.J.Y.; Lee, K.K.C.; Yung, M.; Wong, S.K.H.; Wu, J.C.Y.; Chan, F.K.L.; Ng, E.K.W.; You, J.H.S.; Lee, C.W.; et al. Effect of Intravenous Omeprazole on Recurrent Bleeding after Endoscopic Treatment of Bleeding Peptic Ulcers. N. Engl. J. Med. 2000, 343, 310–316. [Google Scholar] [CrossRef]
- Sachar, H.; Haven, N.; Vaidya, K.; Haven, N.; Laine, L.; Haven, N.; Connecticut, A.; Haven, W. Intermittent vs Continuous Proton Pump Inhibitor Therapy for High-Risk Bleeding Ulcers: A Systematic Review and Meta-Analysis. JAMA Intern. Med. 2015, 174, 1755–1762. [Google Scholar] [CrossRef]
- Rodriguez, E.A.; Donath, E.; Waljee, A.K.; Sussman, D.A. Value of Oral Proton Pump Inhibitors in Acute, Nonvariceal Upper Gastrointestinal Bleeding: A Network Meta-Analysis. J. Clin. Gastroenterol. 2017, 51, 707–719. [Google Scholar] [CrossRef]
- Neumann, I.; Letelier, L.M.; Rada, G.; Claro, J.C.; Martin, J.; Howden, C.W.; Yuan, Y.; Leontiadis, G.I. Comparison of Different Regimens of Proton Pump Inhibitors for Acute Peptic Ulcer Bleeding. Cochrane Database Syst. Rev. 2013, 6, CD007999. [Google Scholar] [CrossRef]
- Zhu, W.; Chen, L.; Zhang, J.; Wang, P. Effects of High-Dose versus Low-Dose Proton Pump Inhibitors for Treatment of Gastrointestinal Ulcer Bleeding: A Meta-Analysis of Randomized Controlled Trials. J. Int. Med. Res. 2022, 50, 3000605211067396. [Google Scholar] [CrossRef]
- Barkun, A.N.; Almadi, M.; Kuipers, E.J.; Laine, L.; Sung, J.; Tse, F.; Leontiadis, G.I.; Abraham, N.S.; Calvet, X.; Chan, F.K.L.; et al. Management of Nonvariceal Upper Gastrointestinal Bleeding: Guideline Recommendations From the International Consensus Group. Ann. Intern. Med. 2019, 171, 805. [Google Scholar] [CrossRef]
- Laine, L.; Barkun, A.N.; Saltzman, J.R.; Martel, M.; Leontiadis, G.I. ACG Clinical Guideline: Upper Gastrointestinal and Ulcer Bleeding. Am. J. Gastroenterol. 2021, 116, 899–917. [Google Scholar] [CrossRef] [PubMed]
- Javid, G.; Zargar, S.A.; U-Saif, R.; Khan, B.A.; Yatoo, G.N.; Shah, A.H.; Gulzar, G.M.; Sodhi, J.S.; Khan, M.A. Comparison of p.o. or i.v. Proton Pump Inhibitors on 72-h Intragastric PH in Bleeding Peptic Ulcer. J. Gastroenterol. Hepatol. 2009, 24, 1236–1243. [Google Scholar] [CrossRef] [PubMed]
- Laine, L.; Shah, A.; Bemanian, S. Intragastric PH With Oral vs Intravenous Bolus Plus Infusion Proton-Pump Inhibitor Therapy in Patients With Bleeding Ulcers. Gastroenterology 2008, 134, 1836–1841. [Google Scholar] [CrossRef]
- Hartmann, M.; Ehrlich, A.; Fuder, H.; Lühmann, R.; Emeklibas, S.; Timmer, W.; Wurst, W.; Lücker, P.W. Equipotent Inhibition of Gastric Acid Secretion by Equal Doses of Oral or Intravenous Pantoprazole. Aliment. Pharmacol. Ther. 1998, 12, 1027–1032. [Google Scholar] [CrossRef] [PubMed]
- Al-Sabah, S.; Barkun, A.N.; Herba, K.; Adam, V.; Fallone, C.; Mayrand, S.; Pomier-Layrargues, G.; Kennedy, W.; Bardou, M. Cost-Effectiveness of Proton-Pump Inhibition Before Endoscopy in Upper Gastrointestinal Bleeding. Clin. Gastroenterol. Hepatol. 2008, 6, 418–425. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.; Adam, V.; Teich, V.; Barkun, A. Timing or Dosing of Intravenous Proton Pump Inhibitors in Acute Upper Gastrointestinal Bleeding Has Low Impact on Costs. Am. J. Gastroenterol. 2016, 111, 1389–1398. [Google Scholar] [CrossRef] [PubMed]
- Coronel, E.; Bassi, N.; Donahue-Rolfe, S.; Byrne, E.; Sokol, S.; Reddy, G.; Arora, V.M. Evaluation of a Trainee-Led Project to Reduce Inappropriate Proton Pump Inhibitor Infusion in Patients with Upper Gastrointestinal Bleeding: Skip the Drips. JAMA Intern. Med. 2017, 177, 1687–1689. [Google Scholar] [CrossRef]
- Quan, S.; Frolkis, A.; Milne, K.; Molodecky, N.; Yang, H.; Dixon, E.; Ball, C.G.; Myers, R.P.; Ghosh, S.; Hilsden, R.; et al. Upper-Gastrointestinal Bleeding Secondary to Peptic Ulcer Disease: Incidence and Outcomes. World J. Gastroenterol. 2014, 20, 17568–17577. [Google Scholar] [CrossRef]
- Ahmed, A.; Armstrong, M.; Robertson, I.; Morris, A.J.; Blatchford, O.; Stanley, A.J.; Ahmed, A.; Morris, A.J.; Stanley, A.J.; Unit, G.I.; et al. Upper Gastrointestinal Bleeding in Scotland 2000-2010: Improved Outcomes but a Significant Weekend Effect. World J. Gastroenterol. 2015, 21, 10890–10897. [Google Scholar] [CrossRef]
- Valkhoff, V.E.; Coloma, P.M.; Masclee, G.M.C.; Gini, R.; Innocenti, F.; Lapi, F.; Molokhia, M.; Mosseveld, M.; Schou, M.; Schuemie, M.; et al. Validation Study in Four Health-Care Databases: Upper Gastrointestinal Bleeding Misclassification Affects Precision but Not Magnitude of Drug-Related Upper Gastrointestinal Bleeding Risk. J. Clin. Epidemiol. 2014, 67, 921–931. [Google Scholar] [CrossRef]
- Canadian Institute for Health Information. CMG+ [Internet]. Available online: https://www.cihi.ca/en/cmg (accessed on 9 May 2023).
- Government of Alberta. Interactive Health Data Application [Internet]. Available online: http://www.ahw.gov.ab.ca/IHDA_Retrieval/ (accessed on 9 May 2023).
- Government of Alberta. ALBERTA HEALTH CARE INSURANCE PLAN Medical Price List As of 01 April 2017 [Internet]. Available online: https://open.alberta.ca/dataset/376dc12c-5bbb-494e-810b-ad3a6e13874a/resource/f4017e43-3407-4551-8ac7-8c60065617e4/download/somb-medical-prices-2017-04.pdf (accessed on 9 May 2023).
- Laine, L.; McQuaid, K.R. Endoscopic Therapy for Bleeding Ulcers: An Evidence-Based Approach Based on Meta-Analyses of Randomized Controlled Trials. Clin. Gastroenterol. Hepatol. 2009, 7, 33–47. [Google Scholar] [CrossRef] [PubMed]
- Sung, J.J.; Chiu, P.C.; Chan, F.K.L.; Lau, J.Y.; Goh, K.-L.; Ho, L.H.; Jung, H.-Y.; Sollano, J.D.; Gotoda, T.; Reddy, N.; et al. Asia-Pacific Working Group Consensus on Non-Variceal Upper Gastrointestinal Bleeding: An Update 2018. Gut 2018, 01136, 1757–1768. [Google Scholar] [CrossRef] [PubMed]
- Gralnek, I.; Dumonceau, J.-M.; Kuipers, E.; Lanas, A.; Sanders, D.; Kurien, M.; Rotondano, G.; Hucl, T.; Dinis-Ribeiro, M.; Marmo, R.; et al. Diagnosis and Management of Nonvariceal Upper Gastrointestinal Hemorrhage: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy 2015, 47, a1–a46. [Google Scholar] [CrossRef]
- Yamada, S.; Wongwanakul, P. Randomized Controlled Trial of High Dose Bolus versus Continuous Intravenous Infusion Pantoprazole as an Adjunct Therapy to Therapeutic Endoscopy in Massive Bleeding Peptic Ulcer. J. Med. Assoc. Thai. 2012, 95, 349–357. [Google Scholar]
- Mehmedovic-Redzepovic, A.; Mesihović, R.; Prnjavorac, B.; Kulo, A.; Merlina, K. Hematologic and Laboratory Parameters in Patientis with Peptic Ulcer Bleeding Treated by Two Modalities of Endoscopic Haemostasis and Proton Pompe Inhibitors. Med. Glas. 2011, 8, 151–157. [Google Scholar]
- Hsu, Y.C.; Perng, C.L.; Yang, T.H.; Wang, C.S.; Hsu, W.L.; Wu, H.T.; Cheng, Y.C.; Chiang, M.F.; Lin, H.J. A Randomized Controlled Trial Comparing Two Different Dosages of Infusional Pantoprazole in Peptic Ulcer Bleeding. Br. J. Clin. Pharmacol. 2010, 69, 245–251. [Google Scholar] [CrossRef] [PubMed]
- Sung, J.J.; Suen, B.-Y.; Wu, J.C.; Lau, J.Y.; Ching, J.Y.; Lee, V.W.; Chiu, P.W.; Tsoi, K.K.; Chan, F.K. Effects of Intravenous and Oral Esomeprazole in the Prevention of Recurrent Bleeding from Peptic Ulcers after Endoscopic Therapy. Am. J. Gastroenterol. 2014, 109, 1005–1010. [Google Scholar] [CrossRef]
- Kim, H.K.; Kim, J.S.; Kim, T.H.; Kim, C.W.; Cho, Y.S.; Kim, S.S.; Chae, H.S.; Han, S.W.; Park, Y.W.; Son, H.S.; et al. Effect of High-Dose Oral Rabeprazole on Recurrent Bleeding after Endoscopic Treatment of Bleeding Peptic Ulcers. Gastroenterol. Res. Pract. 2012, 2012, 317125. [Google Scholar] [CrossRef]
- Gralnek, I.M.; Stanley, A.J.; Morris, A.J.; Camus, M.; Lau, J.; Lanas, A.; Laursen, S.B.; Radaelli, F.; Papanikolaou, I.S.; Cúrdia Gonçalves, T.; et al. Endoscopic Diagnosis and Management of Nonvariceal Upper Gastrointestinal Hemorrhage (NVUGIH): European Society of Gastrointestinal Endoscopy (ESGE) Guideline—Update 2021. Endoscopy 2021, 53, 300–332. [Google Scholar] [CrossRef]
- Lu, Y.; Barkun, A.N.; Martel, M. Adherence to Guidelines: A National Audit of the Management of Acute Upper Gastrointestinal Bleeding. The REASON Registry. Can. J. Gastroenterol. Hepatol. 2014, 28, 495–501. [Google Scholar] [CrossRef]
- Craig, D.G.N.; Thimappa, R.; Anand, V.; Sebastian, S. Inappropriate Utilization of Intravenous Proton Pump Inhibitors in Hospital Practice-a Prospective Study of the Extent of the Problem and Predictive Factors. QJM 2010, 103, 327–335. [Google Scholar] [CrossRef] [PubMed]
- Enns, R.A.; Andrews, C.N.; Fishman, M.; Hahn, M.; Atkinson, K.; Kwan, P.; Levy, A. Description of Prescribing Practices in Patients with Upper Gastrointestinal Bleeding Receiving Intravenous Proton Pump Inhibitors: A Multicentre Evaluation. Can. J. Gastroenterol. 2004, 18, 567–571. [Google Scholar] [CrossRef] [PubMed]
- Kaplan, G.G.; Bates, D.; Mcdonald, D.; Panaccione, R.; Romagnuolo, J. Inappropriate Use of Intravenous Pantoprazole: Extent of the Problem and Successful Solutions. Clin. Gastroenterol. Hepatol. 2005, 3, 1207–1214. [Google Scholar] [CrossRef] [PubMed]
- Tsoi, K.K.F.; Lau, J.Y.W.; Sung, J.J.Y. Cost-Effectiveness Analysis of High-Dose Omeprazole Infusion before Endoscopy for Patients with Upper-GI Bleeding. Gastrointest. Endosc. 2008, 67, 1056–1063. [Google Scholar] [CrossRef]
- Spiegel, B.M.R.; Dulai, G.S.; Lim, B.S.; Mann, N.; Kanwal, F.; Gralnek, I.M. The Cost-Effectiveness and Budget Impact of Intravenous Versus Oral Proton Pump Inhibitors in Peptic Ulcer Hemorrhage. Clin. Gastroenterol. Hepatol. 2006, 4, 988–997.e2. [Google Scholar] [CrossRef]
- Garnock-Jones, K.P. Vonoprazan: First Global Approval. Drugs 2015, 75, 439–443. [Google Scholar] [CrossRef]
- Tsujita, K.; Deguchi, H.; Uda, A.; Sugano, K. Upper Gastrointestinal Bleeding in Japanese Patients with Ischemic Heart Disease Receiving Vonoprazan or a Proton Pump Inhibitor with Multiple Antithrombotic Agents: A Nationwide Database Study. J. Cardiol. 2020, 76, 51–57. [Google Scholar] [CrossRef]
- Abe, H.; Hatta, W.; Ogata, Y.; Koike, T.; Saito, M.; Jin, X.; Nakagawa, K.; Kanno, T.; Uno, K.; Asano, N.; et al. Prevention of Delayed Bleeding with Vonoprazan in Upper Gastrointestinal Endoscopic Treatment. J. Gastroenterol. 2021, 56, 640–650. [Google Scholar] [CrossRef]
- Jiang, X.; Li, J.; Xie, J.; Liang, Z.; Wan, N.; Jiang, J.; Zhang, T.; Wu, Y. Histamine2-Receptor Antagonists, Proton Pump Inhibitors, or Potassium-Competitive Acid Blockers Preventing Delayed Bleeding After Endoscopic Submucosal Dissection: A Meta-Analysis. Front. Pharmacol. 2019, 10, 1055. [Google Scholar] [CrossRef]
- Ishii, M.; Kawai, T.; Tsujita, K.; Igarashi, A.; Suzuki, M.; Deguchi, H.; Fernandez, J. Cost-Effectiveness of Vonoprazan Compared With Proton Pump Inhibitors in Patients Taking Low-Dose Aspirin for Secondary Prevention of Cardiovascular Events in Japan. Circ. J. 2023, 87, 348–359. [Google Scholar] [CrossRef]
| Variable | High-Risk Lesion | Low-Risk Lesion | No EGD | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All | No PPI | PPI B + I | PPI I–IV | PO | All | No PPI | PPI B + I | PPI I–IV | PO | All | No PPI | PPI B + I | PPI I–IV | PO | |
| Visits | 410 | 36 | 337 | 12 | 25 | 1403 | 152 | 1079 | 60 | 112 | 2241 | 1373 | 582 | 61 | 225 |
| No. (%) Female | 133 (32) | 10 (28) | 110 (33) | 4 (33) | 9 (36) | 553 (39) | 72 (47) | 406 (38) | 26 (43) | 49 (43) | 1051 (47) | 677 (49) | 247 (42) | 23 (38) | 104 (46) |
| Mean Age (95% CI) | 64 (62–66) | 64 (59–69) | 64 (62–66) | 66 (54–78) | 68 (62–73) | 63 (63–65) | 59 (56–62) | 64 (62–65) | 67 (63–72) | 67 (64–71) | 57 (56–58) | 54 (53–56) | 63 (61–65) | 57 (51–63) | 59 (56–62) |
| Age Range | 19–66 | 26–95 | 19–96 | 31–93 | 44–91 | 18–103 | 18–97 | 18–103 | 20–94 | 21–100 | 18–106 | 18–101 | 19–106 | 19–98 | 19–96 |
| Heart rate, mean, BPM (95% CI) | 92 (91–94) | 89 (83–95) | 93 (91–95) | 98 (88–108) | 87 (79–95) | 91 (90–92) | 86 (83–89) | 92 (91–93) | 89 (84–95) | 85 (82–88) | 88 (87–89) | 86 (85–87) | 93 (91–95) | 93 (87–98) | 87 (84–89) |
| Systolic Blood pressure, mean, mm Hg (95% CI) | 119 (116–121) | 126 (119–132) | 117 (115–119) | 131 (117–144) | 126 (117–134) | 126 (125–128) | 132 (129–135) | 125 (124–127) | 127 (121–133) | 128 (124–132) | 132 (131–133) | 134 (133–135) | 128 (126–130) | 131 (126–137) | 131 (128–134) |
| Diastolic Blood pressure, mean, mm Hg (95% CI) | 69 (67–71) | 75 (68–81) | 68 (67–70) | 76 (69–82) | 68 (63–74) | 73 (72–75) | 77 (74–79) | 73 (71–75) | 74 (70–78) | 70 (67–73) | 78 (77–79) | 80 (79–80) | 76 (73–78) | 75 (70–79) | 76 (74–78) |
| Hemoglobin, mean, g/L (95% CI) | 93 (90–95) | 108 (97–118) | 91 (88–94) | 103 (85–122) | 91 (80–102) | 103 (101–104) | 117 (112–122) | 101 (99–103) | 105 (96–113) | 100 (95–106) | 125 (124–127) | 132 (130–133) | 114 (111–116) | 119 (111–127) | 123 (119–127) |
| Number transfused (%) | 195 (48) | 5 (14) | 174 (52) | 4 (33) | 12 (48) | 476 (34) | 20 (13) | 411 (38) | 16 (27) | 29 (26) | 249 (11) | 71 (5) | 139 (24) | 7 (11) | 32 (14) |
| Number admitted (%) | 392 (96) | 29 (81) | 327 (97) | 12 (100) | 24 (96) | 1191 (85) | 98 (64) | 942 (87) | 52 (87) | 99 (88) | 746 (33) | 216 (16) | 383 (66) | 27 (44) | 120 (53) |
| Visits | Average LOS(95% CI) | Average Cost Per Admission | Overall Costs | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Total Cost | Lower 95% | Upper 95% | Hospital Cost | Physician Cost | Drug Cost | ||||
| High Risk | 410 | 7.4 (6.3–8.4) | N/A | ||||||
| no PPI | 36 | 5.2 (3.5–7) | CAD 7514 | CAD 5155 | CAD 10,011 | CAD 6673 | CAD 841 | CAD 0 | CAD 270,491 |
| bolus + infusion | 337 | 7.5 (6.3–8.8) | CAD 10,742 | CAD 9077 | CAD 12,545 | CAD 9624 | CAD 1860 | CAD 38 | CAD 3,620,086 |
| intermittent IV | 12 | 11.6 (5.8–17.3) | CAD 16,408 | CAD 8363 | CAD 24,316 | CAD 14,885 | CAD 2713 | CAD 17 | CAD 196,901 |
| PO | 25 | 5.8 (3.5–8.2) | CAD 8348 | CAD 5158 | CAD 11,678 | CAD 7443 | CAD 1507 | CAD 2 | CAD 208,707 |
| Subgroup Total | CAD 4,296,185 | ||||||||
| Low Risk | 1403 | 6.6 (6.1–7.2) | N/A | ||||||
| no PPI | 152 | 4.2 (3.4–4.9) | CAD 6126 | CAD 5017 | CAD 7097 | CAD 5389 | CAD 737 | CAD 0 | CAD 931,216 |
| bolus + infusion | 1231 | 6.8 (6.2–7.3) | CAD 9771 | CAD 8938 | CAD 10,464 | CAD 8726 | CAD 1007 | CAD 38 | CAD 10,542,659 |
| intermittent IV | 60 | 4.9 (3.9–5.9) | CAD 7111 | CAD 5724 | CAD 8499 | CAD 6288 | CAD 810 | CAD 14 | CAD 426,686 |
| PO | 112 | 6.3 (4.8–7.8) | CAD 9042 | CAD 6961 | CAD 11,123 | CAD 8084 | CAD 955 | CAD 3 | CAD 1,012,713 |
| Subgroup Total | CAD 12,913,274 | ||||||||
| No EGD | 2241 | 7.9 (7.5–8.4) | N/A | ||||||
| no PPI | 1373 | 4.4 (4.1–4.6) | CAD 6291 | CAD 5875 | CAD 6568 | CAD 5646 | CAD 645 | CAD 0 | CAD 8,637,095 |
| bolus + infusion | 582 | 11.1 (9.7–12.7) | CAD 15,624 | CAD 13,682 | CAD 17,705 | CAD 14,244 | CAD 1341 | CAD 39 | CAD 9,093,343 |
| intermittent IV | 61 | 8.5 (6–11) | CAD 11,994 | CAD 8526 | CAD 15,462 | CAD 10,907 | CAD 1071 | CAD 15 | CAD 731,612 |
| PO | 225 | 7.7 (6.5–8.9) | CAD 10,872 | CAD 9207 | CAD 12,536 | CAD 9881 | CAD 988 | CAD 3 | CAD 2,446,098 |
| Subgroup Total | CAD 20,908,148 | ||||||||
| Grand Total | CAD 38,117,607 | ||||||||
| American College of Gastroenterology (ACG) (2021) [11] | International Consensus Group (2019) [10] | Asia-Pacific Working Group (2018) [25] | European Society of Gastrointestinal Endoscopy (ESGE) (2021) [32] | |
|---|---|---|---|---|
| Post-endoscopy finding high-risk lesion | IV bolus + infusion | IV bolus + infusion | High-dose PO PPI as adjunct | IV bolus + infusion |
| High-dose intermittent, IV or PO | Neither for nor against intermittent IV | No comment on intermittent IV | Can consider intermittent IV or high-dose PO | |
| Pre-endoscopy | No recommendation. Previously recommended considering IV bolus + infusion | No comment Previously recommended IV bolus + infusion in 2010 version of guidelines | No agreement on recommending PPI | Consider IV bolus + infusion |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lei, Y.; Halasz, J.; Novak, K.L.; Congly, S.E. Intermittent Proton Pump Inhibitor Therapy in Low-Risk Non-Variceal Upper Gastrointestinal Bleeding May Be Significantly Cost-Saving. Medicines 2023, 10, 44. https://doi.org/10.3390/medicines10070044
Lei Y, Halasz J, Novak KL, Congly SE. Intermittent Proton Pump Inhibitor Therapy in Low-Risk Non-Variceal Upper Gastrointestinal Bleeding May Be Significantly Cost-Saving. Medicines. 2023; 10(7):44. https://doi.org/10.3390/medicines10070044
Chicago/Turabian StyleLei, Yang, Jennifer Halasz, Kerri L. Novak, and Stephen E. Congly. 2023. "Intermittent Proton Pump Inhibitor Therapy in Low-Risk Non-Variceal Upper Gastrointestinal Bleeding May Be Significantly Cost-Saving" Medicines 10, no. 7: 44. https://doi.org/10.3390/medicines10070044
APA StyleLei, Y., Halasz, J., Novak, K. L., & Congly, S. E. (2023). Intermittent Proton Pump Inhibitor Therapy in Low-Risk Non-Variceal Upper Gastrointestinal Bleeding May Be Significantly Cost-Saving. Medicines, 10(7), 44. https://doi.org/10.3390/medicines10070044






