Antimicrobial Prescribing Preparedness of Croatian Medical Students—Did It Change between 2015 and 2019?
Abstract
1. Introduction
Antibiotic Stewardship in Croatia
2. Materials and Methods
2.1. Study Design and Participants
2.2. Survey Development
2.3. Statistical Analyses
3. Results
3.1. Participants
3.2. Global Preparedness Scores
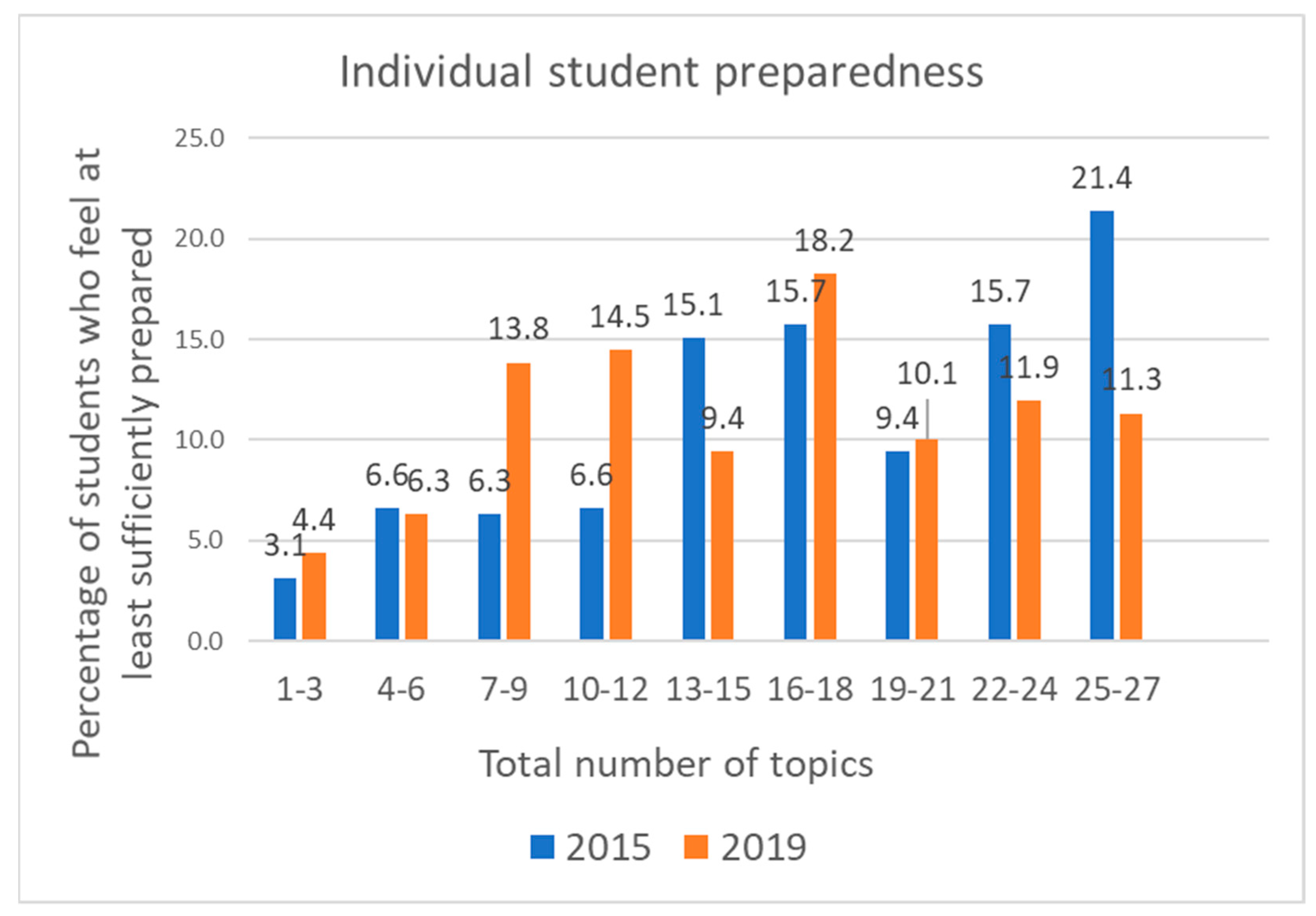
3.3. Preparedness for Individual Curriculum Topics
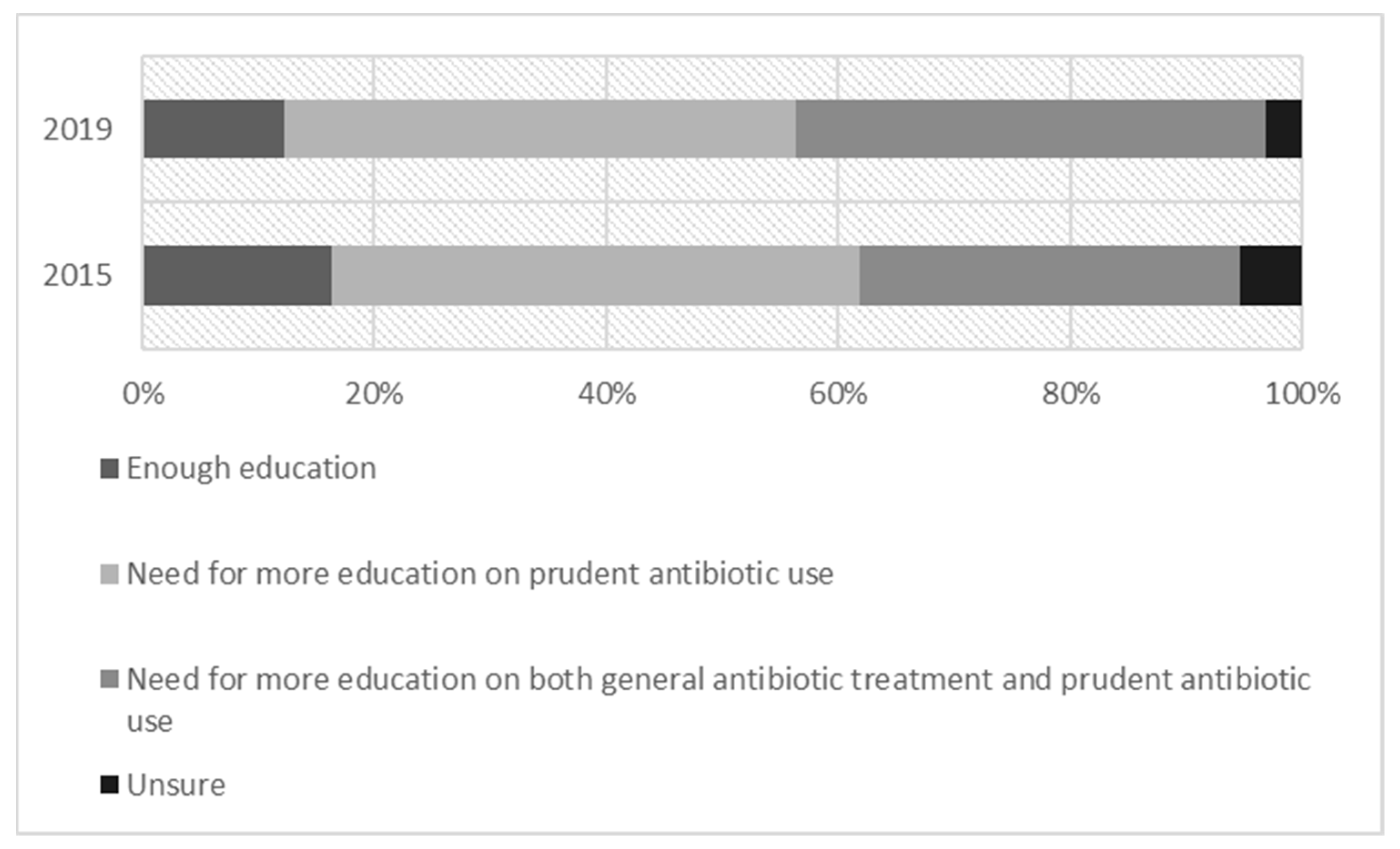
3.4. Perceptions of Antimicrobial Education
3.5. Teaching Methods
4. Discussion
4.1. Overall Preparedness
4.2. Preparedness for Individual Topics
4.3. Teaching Methods
4.4. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Maxwell, S.R.; Cascorbi, I.; Orme, M.; Webb, D.J. Educating European (junior) doctors for safe prescribing. Basic Clin. Pharmacol. Toxicol. 2007, 101, 395–400. [Google Scholar] [CrossRef] [PubMed]
- Tallentire, V.R.; Smith, S.E.; Skinner, J.; Cameron, H.S. The preparedness of UK graduates in acute care: A systematic literature review. Postgrad. Med. J. 2012, 88, 365–371. [Google Scholar] [CrossRef] [PubMed]
- Abbo, L.M.; Cosgrove, S.E.; Pottinger, P.S.; Pereyra, M.; Sinkowitz-Cochran, R.; Srinivasan, A.; Webb, D.J.; Hooton, T.M. Medical students’ perceptions and knowledge about antimicrobial stewardship: How are we educating our future prescribers. Clin. Infect. Dis. 2013, 57, 631–638. [Google Scholar] [CrossRef] [PubMed]
- Brinkman, D.J.; Tichelaar, J.; Schutte, T.; Benemei, S.; Böttiger, Y.; Chamontin, B.; Christiaens, T.; Likic, R.; Maˇiulaitis, R.; Marandi, T.; et al. Essential competencies in prescribing: A first european cross-sectional study among 895 final-year medical students. Clin. Pharmacol. Ther. 2017, 101, 281–289. [Google Scholar] [CrossRef] [PubMed]
- Brinkman, D.J.; Tichelaar, J.; Graaf, S.; Otten, R.H.J.; Richir, M.C.; van Agtmael, M.A. Do final-year medical students have sufficient prescribing competencies? A systematic literature review. Br. J. Clin. Pharmacol. 2018, 84, 615–635. [Google Scholar] [CrossRef] [PubMed]
- Dyar, O.J.; Nathwani, D.; Monnet, D.L.; Gyssens, I.C.; Stålsby Lundborg, C.; Pulcini, C.; Wechsler-Fördös, A.; Kostyanev, T.; Vlahović-Palčevski, V.; Kolar, M.; et al. Do medical students feel prepared to prescribe antibiotics responsibly? Results from a cross-sectional survey in 29 European countries. J. Antimicrob. Chemother. 2018, 73, 2236–2242. [Google Scholar] [CrossRef] [PubMed]
- Pulcini, C.; Wencker, F.; Frimodt-Møller, N.; Kern, W.V.; Nathwani, D.; Rodríguez-Baño, J.; Simonsen, G.S.; Vlahović-Palčevski, V.; Gyssens, I.C.; Gyssens, I.; et al. European survey on principles of prudent antibiotic prescribing teaching in undergraduate students. Clin. Microbiol. Infect. 2015, 21, 354–361. [Google Scholar] [CrossRef] [PubMed]
- WHO. Global Action Plan on Antimicrobial Resistance. 2015. Available online: http://apps.who.int/gb/ebwha/pdf_files/WHA68/A68_R7-en.pdf?ua=1 (accessed on 31 May 2023).
- Pulcini, C.; Gyssens, I.C. How to educate prescribers in antimicrobial stewardship practices. Virulence 2013, 4, 192–202. [Google Scholar] [CrossRef] [PubMed]
- ISKRA—Interdisciplinarna Sekcija za Kontrolu Rezistencije na Antibiotike. Available online: https://iskra.bfm.hr/ (accessed on 13 June 2023).
- Belančić, A.; Palčevski, D.; Likić, R.; Vlahović Palčevski, V. Samoprocjenjena spremnost za racionalno propisivanje antimikrobnih lijekova među diplomantima četiriju hrvatskih medicinskih fakulteta. Liječnički Vjesn. 2023, 145, 117–124. [Google Scholar] [CrossRef]
- Belančić, A.; Stanić Benić, M.; Skočibušić, N.; Palčevski, D.; Vlahović-Palčevski, V. Repeated point prevalence survey on antimicrobial use in a university hospital: What have we learned? Int. J. Pharm. Pract. 2021, 29, 362–368. [Google Scholar] [CrossRef] [PubMed]
- Radošević Quadranti, N.; Vlahović-Palčevski, V.; Popović, B.; Diminić-Lisica, I. Impact of guidelines on antibiotic prescribing approach in primary care-a 10-year study. Fam. Pract. 2021, 38, 259–264. [Google Scholar] [CrossRef] [PubMed]
- Rusic, D.; Bozic, J.; Bukic, J.; Vilovic, M.; Tomicic, M.; Seselja Perisin, A.; Leskur, D.; Modun, D.; Cohadzic, T.; Tomic, S. Antimicrobial Resistance: Physicians’ and Pharmacists’ Perspective. Microb. Drug Resist. 2021, 27, 670–677. [Google Scholar] [CrossRef] [PubMed]
- European Centre for Disease Prevention and Control. Antimicrobial Consumption in the EU/EEA (ESAC-Net)—Annual Epidemiological Report for 2021. Available online: https://www.ecdc.europa.eu/en/publications-data/surveillance-antimicrobial-consumption-europe-2021 (accessed on 13 June 2023).
- 2022 WHO Regional Office for Europe/European Centre for Disease Prevention and Control. Antimicrobial Resistance Surveillance in Europe 2022–2020 Data. Available online: https://www.ecdc.europa.eu/en/publications-data/antimicrobial-resistance-surveillance-europe-2022-2020-data (accessed on 13 June 2023).
- Alexander, C.; Millar, J.; Szmidt, N.; Hanlon, K.; Cleland, J. Can new doctors be prepared for practice? A review. Clin. Teach. 2014, 11, 188–192. [Google Scholar] [CrossRef] [PubMed]
- Deschepper, R.; Grigoryan, L.; Lundborg, C.S.; Hofstede, G.; Cohen, J.; Kelen, G.V.; Deliens, L.; Haaijer-Ruskamp, F.M. Are cultural dimensions relevant for explaining cross-national differences in antibiotic use in Europe. BMC Health Serv. Res. 2008, 8, 123. [Google Scholar] [CrossRef] [PubMed]
- Dyar, O.J.; Lund, M.; Lindsjö, C.; Stålsby Lundborg, C.; Pulcini, C. Preparedness to prescribe antibiotics responsibly: A comparison between final year medical students in France and Sweden. Eur. J. Clin. Microbiol. Infect. Dis. 2019, 38, 711–717. [Google Scholar] [CrossRef] [PubMed]
- van der Voort, T.; Brinkman, D.J.; Benemei, S.; Böttiger, Y.; Chamontin, B.; Christiaens, T.; Likic, R.; Mačiulaitis, R.; Marandi, T.; Monteiro, E.C.; et al. Appropriate antibiotic prescribing among final-year medical students in Europe. Int. J. Antimicrob. Agents 2019, 54, 375–379. [Google Scholar] [CrossRef] [PubMed]
- Brinkman, D.J.; Tichelaar, J.; van Agtmael, M.A.; Schotsman, R.; de Vries, T.P.; Richir, M.C. The prescribing performance and confidence of final-year medical students. Clin. Pharmacol. Ther. 2014, 96, 531–533. [Google Scholar] [CrossRef] [PubMed]
- Belančić, A.; Sans-Pola, C.; Jouanjus, E.; Alcubilla, P.; Arellano, A.L.; Žunić, M.; Nogueiras-Álvarez, R.; Roncato, R.; Sáez-Peñataro, J.; EACPT Young Clinical Pharmacologists Working Group. European association for clinical pharmacology and therapeutics young clinical pharmacologists working group: A cornerstone for the brighter future of clinical pharmacology. Eur. J. Clin. Pharmacol. 2022, 78, 691–694. [Google Scholar] [CrossRef] [PubMed]
- Minen, M.T.; Duquaine, D.; Marx, M.A.; Weiss, D. A survey of knowledge, attitudes, and beliefs of medical students concerning antimicrobial use and resistance. Microb. Drug Resist. 2010, 16, 285–289. [Google Scholar] [CrossRef] [PubMed]
| Topic | Sufficiently Prepared | p | Trend | ||
|---|---|---|---|---|---|
| 2015 (%), N = 318 | 2019 (%), N = 159 | ||||
| 1 | To recognize the clinical signs of infection | 93.7 | 88.7 | 0.056 | = |
| 2 | To differentiate between bacterial and viral upper respiratory tract infections | 89.6 | 85.5 | 0.191 | = |
| 3 | To interpret biochemical markers of inflammation (e.g., CRP) | 89.0 | 88.1 | 0.76 | = |
| 4 | To practise effective infection control and hygiene (to prevent spread of bacteria) | 83.7 | 84.9 | 0.723 | = |
| 5 | To interpret basic microbiological investigations (e.g., blood cultures, antibiotic susceptibility reporting) | 81.8 | 81.1 | 0.867 | = |
| 6 | To use knowledge of the negative consequences of antibiotic use (bacterial resistance, toxic/adverse effects, cost, Clostridium difficile infections) | 81.8 | 84.9 | 0.391 | = |
| 7 | To identify clinical situations when not to prescribe an antibiotic | 80.8 | 68.6 | 0.003 | ↘ |
| 8 | To discuss antibiotic use with patients who are asking for antibiotics, when I feel they are not necessary | 79.9 | 70.4 | 0.022 | ↘ |
| 9 | To differentiate between bacterial colonisation and infection (e.g., asymptomatic bacteriuria) | 78.6 | 64.8 | 0.001 | ↘ |
| 10 | To assess the clinical severity of infection (e.g., using criteria, such as the septic shock criteria) | 78.3 | 72.3 | 0.149 | = |
| 11 | To decide when it is important to take microbiological samples before starting antibiotic therapy | 73.9 | 64.8 | 0.039 | ↘ |
| 12 | To use knowledge of the common mechanisms of antibiotic resistance in pathogens | 68.6 | 61.6 | 0.133 | = |
| 13 | To assess antibiotic allergies (e.g., differentiating between anaphylaxis and hypersensitivity) | 61.3 | 50.9 | 0.031 | ↘ |
| 14 | To prescribe antibiotic therapy according to national/local guidelines | 59.1 | 48.4 | 0.027 | ↘ |
| 15 | To assess clinical outcomes and possible reasons for failure of antibiotic treatment | 57.6 | 44.0 | 0.005 | ↘ |
| 16 | To use point-of-care tests (e.g., urine dipstick, rapid diagnostic tests for streptococcal pharyngitis) | 57.2 | 43.4 | 0.004 | ↘ |
| 17 | To use knowledge of the epidemiology of bacterial resistance, including local/regional variations | 55.4 | 41.5 | 0.004 | ↘ |
| 18 | To decide the urgency of antibiotic administration in different situations (e.g., <1 h for severe sepsis, non-urgent for chronic bone infections) | 54.7 | 42.8 | 0.014 | ↘ |
| 19 | To review the need to continue or change antibiotic therapy after 48–72 h, based on clinical evolution and laboratory results | 54.4 | 49.7 | 0.332 | = |
| 20 | To select initial empirical therapy based on the most likely pathogen(s) and antibiotic resistance patterns, without using guidelines | 53.8 | 44.7 | 0.061 | = |
| 21 | To communicate with senior doctors in situations where I feel antibiotics are not necessary, but I feel I am being inappropriately pressured into prescribing antibiotics by senior doctors | 49.7 | 35.2 | 0.003 | ↘ |
| 22 | To identify indications for combination antibiotic therapy | 44.0 | 27.7 | 0.001 | ↘ |
| 23 | To work within the multi-disciplinary team in managing antibiotic use in hospitals | 44.0 | 28.9 | 0.002 | ↘ |
| 24 | To decide when to switch from intravenous (IV) to oral antibiotic therapy | 43.4 | 28.9 | 0.002 | ↘ |
| 25 | To prescribe using principles of surgical antibiotic prophylaxis | 42.5 | 32.7 | 0.04 | ↘ |
| 26 | To decide the shortest possible adequate duration of antibiotic therapy for a specific infection | 42.1 | 37.1 | 0.292 | = |
| 27 | To measure/audit antibiotic use in a clinical setting, and to interpret the results of such studies | 41.2 | 27.7 | 0.004 | ↘ |
| Teaching Method | 2015 (N = 318) | 2019 (N = 159) | ||||
|---|---|---|---|---|---|---|
| Useful or Very Useful (%) | Not Very Useful (%) | Not Available (%) | Useful or Very Useful (%) | Not Very Useful (%) | Not Available (%) | |
| Lectures (with > 15 people) | 53.5 | 10.7 | 0.3 | 49.7 | 12.6 | 1.5 |
| Small group teaching (with < 15 people) | 77.4 | 0.6 | 6.9 | 71.7 | 3.8 | 13.2 |
| Discussions of clinical cases and vignettes | 79.3 | 1.3 | 8.8 | 69.8 | 1.9 | 12.6 |
| Active learning assignments (e.g., article reading, group work, preparing an oral presentation) | 45.9 | 7.2 | 15.4 | 25.8 | 19.5 | 21.4 |
| E-learning | 19.2 | 11.0 | 41.5 | 23.9 | 8.2 | 44.0 |
| Role play or communication skills sessions dealing with patients demanding antibiotic therapy | 35.9 | 3.5 | 42.1 | 20.1 | 6.3 | 52.2 |
| Infectious diseases clinical placement (i.e., clinical rotation or training in infectious diseases, involving patients) | 66.3 | 2.8 | 11.6 | 66.0 | 4.4 | 7.6 |
| Microbiology clinical placement | 46.5 | 7.9 | 12.0 | 43.4 | 10.7 | 10.0 |
| Peer or near peer teaching (i.e., teaching led by other students, or recently qualified doctors) | 43.7 | 8.2 | 18.9 | 36.5 | 10.7 | 32.1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Palčevski, D.; Belančić, A.; Mikuličić, I.; Oštarijaš, E.; Likić, R.; Dyar, O.; Vlahović-Palčevski, V. Antimicrobial Prescribing Preparedness of Croatian Medical Students—Did It Change between 2015 and 2019? Medicines 2023, 10, 39. https://doi.org/10.3390/medicines10070039
Palčevski D, Belančić A, Mikuličić I, Oštarijaš E, Likić R, Dyar O, Vlahović-Palčevski V. Antimicrobial Prescribing Preparedness of Croatian Medical Students—Did It Change between 2015 and 2019? Medicines. 2023; 10(7):39. https://doi.org/10.3390/medicines10070039
Chicago/Turabian StylePalčevski, Dora, Andrej Belančić, Ivan Mikuličić, Eduard Oštarijaš, Robert Likić, Oliver Dyar, and Vera Vlahović-Palčevski. 2023. "Antimicrobial Prescribing Preparedness of Croatian Medical Students—Did It Change between 2015 and 2019?" Medicines 10, no. 7: 39. https://doi.org/10.3390/medicines10070039
APA StylePalčevski, D., Belančić, A., Mikuličić, I., Oštarijaš, E., Likić, R., Dyar, O., & Vlahović-Palčevski, V. (2023). Antimicrobial Prescribing Preparedness of Croatian Medical Students—Did It Change between 2015 and 2019? Medicines, 10(7), 39. https://doi.org/10.3390/medicines10070039







