Identification and Time Series Analysis of PM2.5 and O3 Associated Health Risk Prevention and Control Areas
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Data
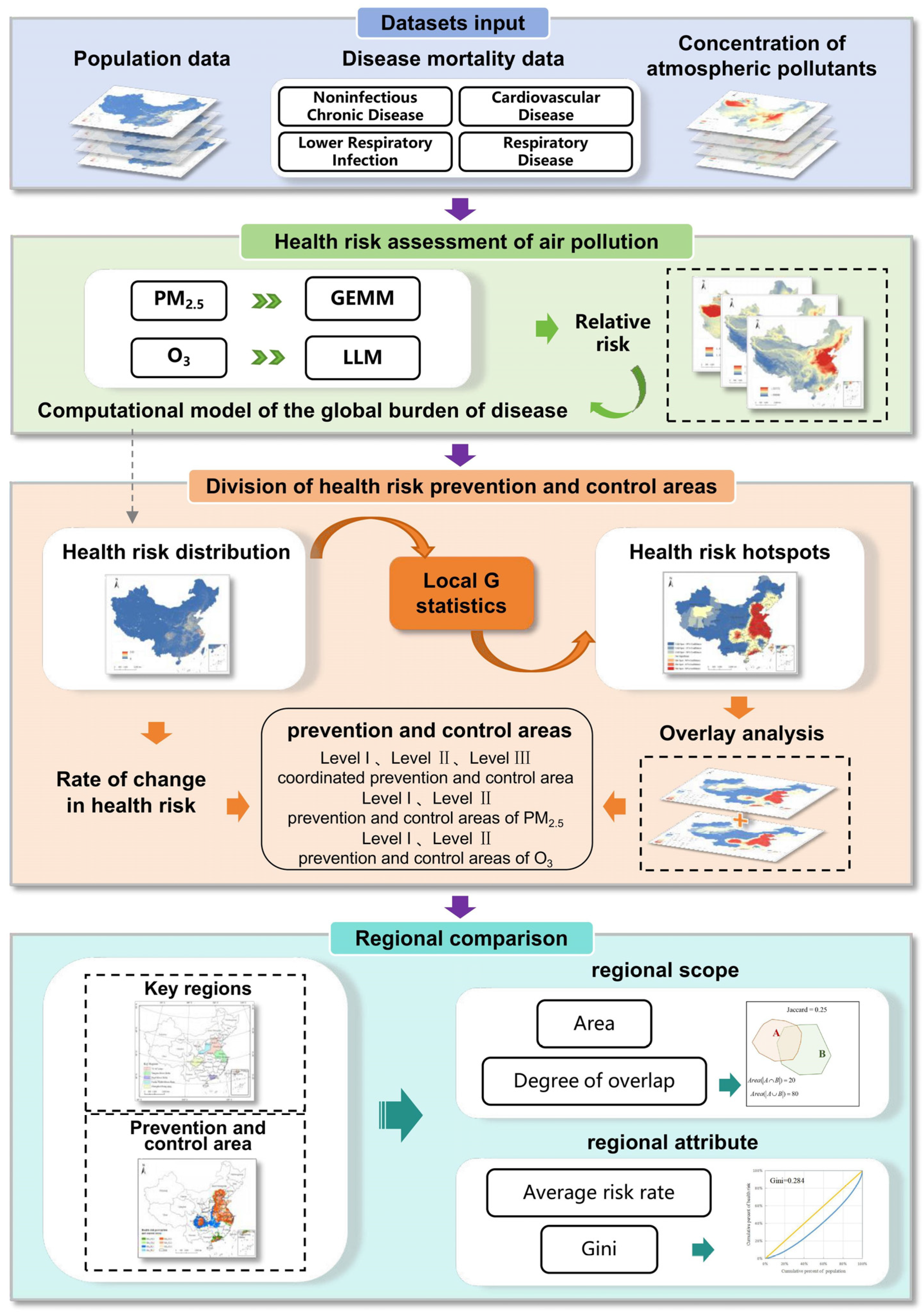
2.2. Methods
2.2.1. Data
2.2.2. Health Risk Assessment of Air Pollution
2.2.3. Division of Health Risk Prevention and Control Areas
Hotspot Area Identification
Rules of Dividing Health Risk Prevention and Control Areas
2.2.4. Regional Comparison
Quantitative Comparison of the Regional Scope
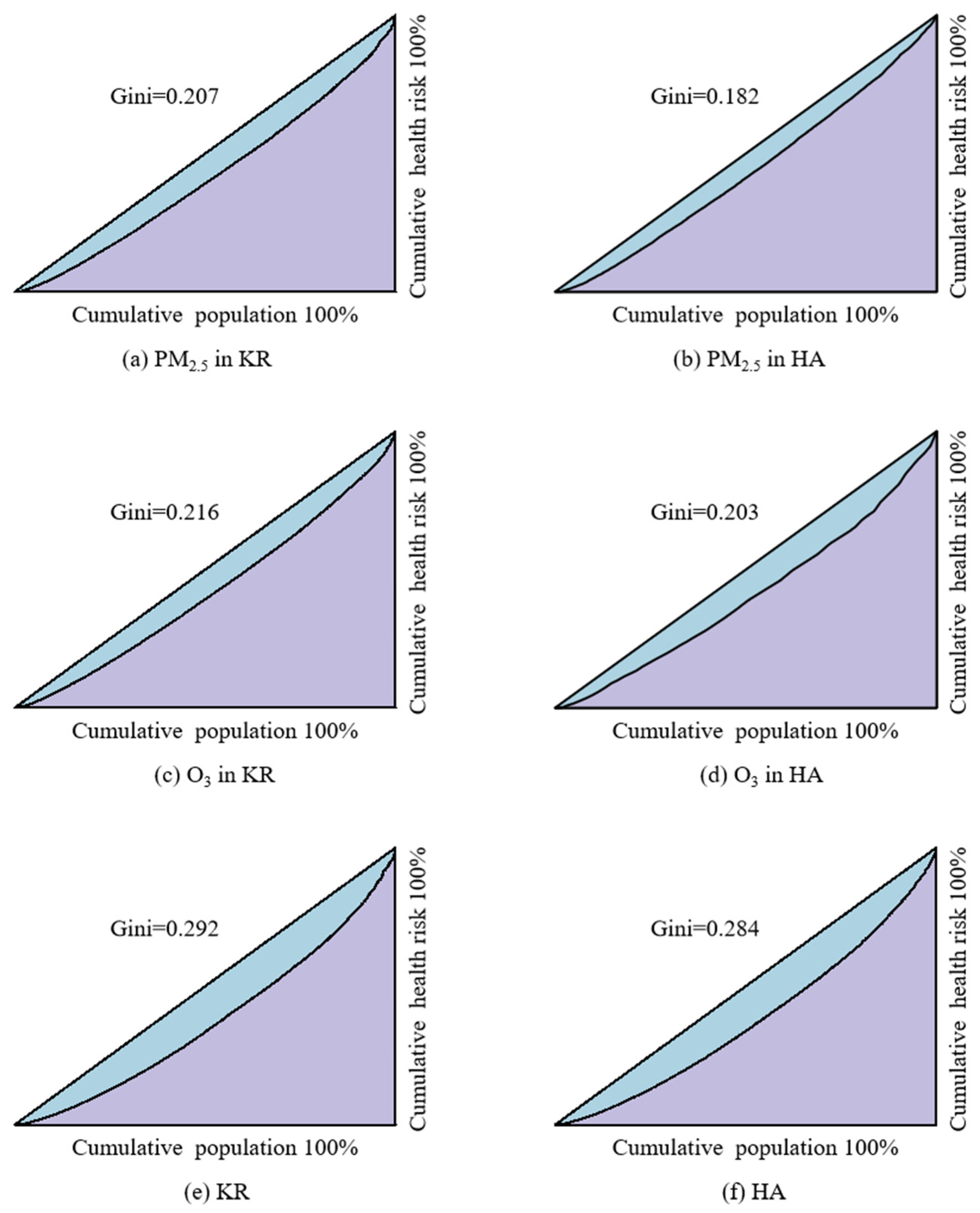
Quantitative Comparison of the Regional Attributes
3. Results
3.1. Health Risk Assessment of Air Pollution
3.1.1. Nationwide Health Risk Analysis
3.1.2. Health Risk Analysis of Key Regions
3.2. Division and Analysis of Health Risk Prevention and Control Areas
3.2.1. Division of Health Risk Prevention and Control Areas
3.2.2. Quantitative Comparison of Scope Between KRs and HAs
3.2.3. Quantitative Comparison of Attributes Between KRs and HAs
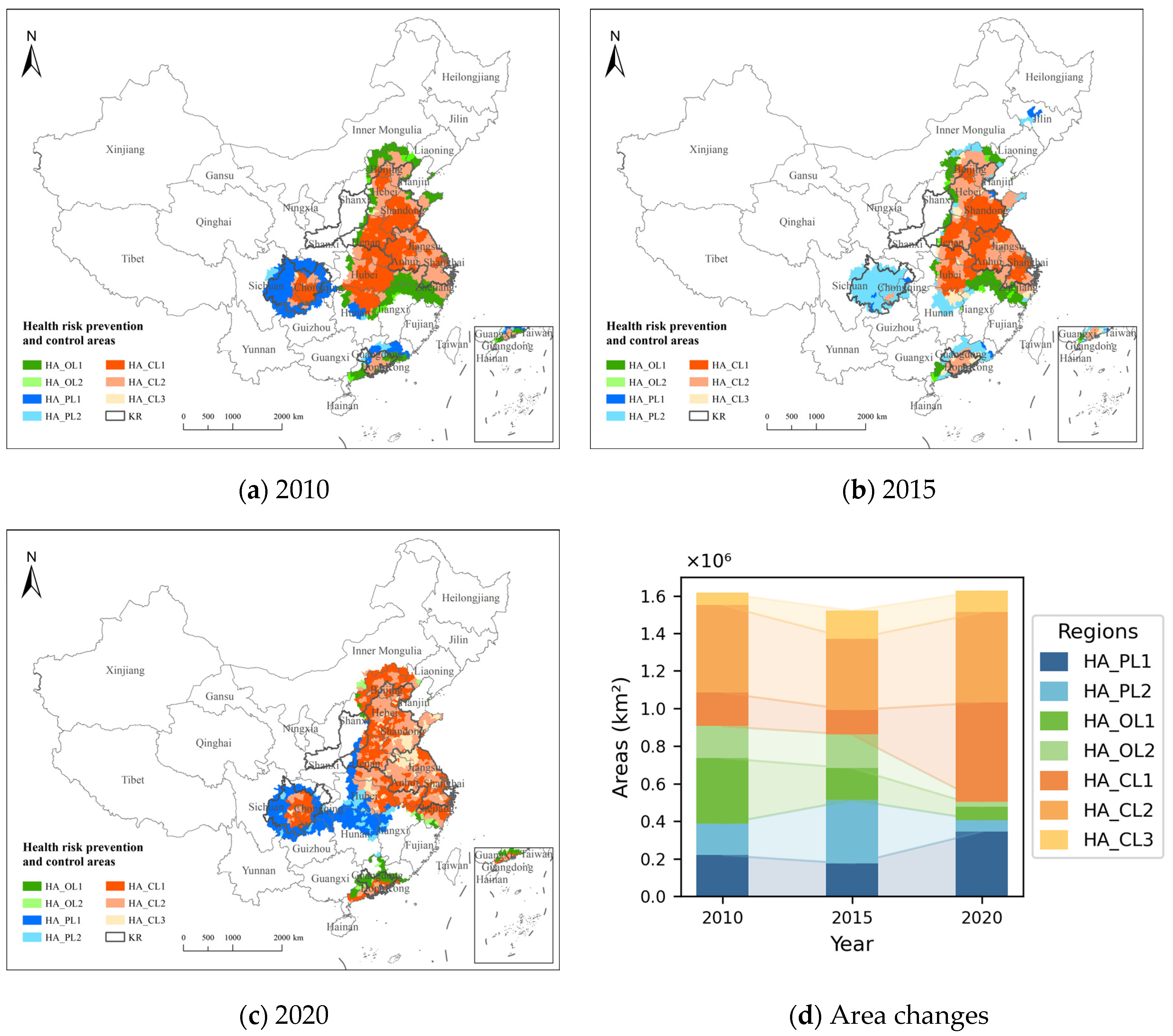
3.3. Spatiotemporal Variations in Health Risk Prevention and Control Areas
3.3.1. Health Risk Variations in Health Risk Prevention and Control Areas
3.3.2. Scope of Variation in Health Risk Prevention and Control Areas
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hao, Y.; Song, X.; Zhu, X.; Wang, J.; Cheng, P.; Bi, X. Health Benefit and Scenario Forecast of PM2.5 and O3 in Fenwei Plain. Res. Environ. Sci. 2024, 37, 696–707. [Google Scholar] [CrossRef]
- Li, T.; Qiu, J.; Fang, C. A brief analysis of the hazards of ozone in the environment and relevant prevention and treatment. World Environ. 2020, 5, 16–18. [Google Scholar]
- Xue, W.; Xu, Y.; Shi, X.; Lei, Y. Atmospheric Environment Management in China: Progress and Outlook. Chin. J. Environ. Manag. 2021, 13, 52–60. [Google Scholar] [CrossRef]
- Li, Y.; Henze, D.K.; Jack, D.; Kinney, P.L. The influence of air quality model resolution on health impact assessment for fine particulate matter and its components. Air Qual. Atmos. Health 2016, 9, 51–68. [Google Scholar] [CrossRef]
- Xue, T.; Liu, J.; Zhang, Q.; Geng, G.; Zhang, Y.; Tong, D.; Liu, Z.; Guan, D.; Bo, Y.; Zhu, T.; et al. Rapid improvement of PM2.5 pollution and associated health benefits in China during 2013–2017. Sci. China Earth Sci. 2020, 50, 441–452. [Google Scholar] [CrossRef]
- Xiao, Q.; Geng, G.; Xue, T.; Liu, S.; Cai, C.; He, K.; Zhang, Q. Tracking PM2.5 and O3 Pollution and the Related Health Burden in China 2013–2020. Environ. Sci. Technol. 2021, 56, 6922–6932. [Google Scholar] [CrossRef]
- Zou, B.; You, J.; Lin, Y.; Duan, X.; Zhao, X.; Fang, X.; Campen, M.J.; Li, S. Air pollution intervention and life-saving effect in China. Environ. Int. 2019, 125, 529–541. [Google Scholar] [CrossRef]
- Wei, J.; Li, Z.; Lyapustin, A.; Wang, J.; Dubovik, O.; Schwartz, J.; Sun, L.; Li, C.; Liu, S.; Zhu, T. First close insight into global daily gapless 1 km PM2.5 pollution, variability, and health impact. Nat. Commun. 2023, 14, 8349. [Google Scholar] [CrossRef]
- Wei, J.; Li, Z.; Chen, X.; Li, C.; Sun, Y.; Wang, J.; Lyapustin, A.; Brasseur, G.P.; Jiang, M.; Sun, L.; et al. Separating Daily 1 km PM2.5 Inorganic Chemical Composition in China since 2000 via Deep Learning Integrating Ground, Satellite, and Model Data. Environ. Sci. Technol. 2023, 57, 18282–18295. [Google Scholar] [CrossRef]
- Cheng, F.; Li, Z.; Yang, Z.; Li, R.; Wang, D.; Jia, A.; Li, K.; Zhao, B.; Wang, S.; Yin, D.; et al. First retrieval of 24-hourly 1-km-resolution gapless surface ozone (O3) from space in China using artificial intelligence: Diurnal variations and implications for air quality and phytotoxicity. Remote Sens. Environ. 2025, 316, 114482. [Google Scholar] [CrossRef]
- Burnett, R.T.; Arden, P.C.; Majid, E.; Casey, O.; Lim, S.S.; Sumi, M.; Shin, H.H.; Gitanjali, S.; Bryan, H.; Michael, B.; et al. An integrated risk function for estimating the global burden of disease attributable to ambient fine particulate matter exposure. Environ. Health Perspect. 2014, 122, 397–403. [Google Scholar] [CrossRef] [PubMed]
- Richard, B.; Hong, C.; Mieczysław, S.; Neal, F.; Bryan, H.; Arden, P.C.; Apte, J.S.; Michael, B.; Aaron, C.; Scott, W.; et al. Global estimates of mortality associated with long-term exposure to outdoor fine particulate matter. Proc. Natl. Acad. Sci. USA 2018, 115, 9592–9597. [Google Scholar]
- Maji, K.J.; Ye, W.-F.; Arora, M.; Nagendra, S.M.S. Ozone pollution in Chinese cities: Assessment of seasonal variation, health effects and economic burden. Environ. Pollut. 2019, 247, 792–801. [Google Scholar] [CrossRef]
- Dong, Z.; Xing, J.; Zhang, F.; Wang, S.; Ding, D.; Wang, H.; Huang, C.; Zheng, H.; Jiang, Y.; Hao, J. Synergetic PM2.5 and O3 control strategy for the Yangtze River Delta, China. J. Environ. Sci. 2023, 123, 281–291. [Google Scholar] [CrossRef]
- Zeng, X.; Ruan, F.; Jiang, Y. Spatial distribution and health effects of ozone pollution in China. China Environ. Sci. 2019, 39, 4025–4032. [Google Scholar] [CrossRef]
- Liu, J.; Niu, X.; Zhang, L.; Yang, X.; Zhao, P.; He, C. Exposure risk assessment and synergistic control pathway construction for O3–PM2.5 compound pollution in China. Atmos. Environ. X 2024, 21, 100240. [Google Scholar] [CrossRef]
- Lu, X.; Zhang, S.; Xing, J.; Wang, Y.; Chen, W.; Ding, D.; Wu, Y.; Wang, S.; Duan, L.; Hao, J. Progress of Air Pollution Control in China and Its Challenges and Opportunities in the Ecological Civilization Era. Engineering 2020, 6, 1423–1431. [Google Scholar] [CrossRef]
- Bai, L.; Liu, J.; Yu, Q.; Choi, J.; Zhang, W. A Collision Resolution Protocol for Random Access in Massive MIMO. IEEE J. Sel. Areas Commun. 2021, 39, 686–699. [Google Scholar] [CrossRef]
- Zhang, H.; Jiang, H.; Gao, J.; Li, H. Formation Mechanism and Management Strategy of Cooperative Control of PM2.5 and O3. Res. Environ. Sci. 2022, 35, 611–620. [Google Scholar] [CrossRef]
- Li, S.; Zou, B.; Zhang, F.; Liu, N.; Xue, C.; Liu, J. Regionalization and Analysis of PM2.5 and O3 Synergetic Prevention and Control Areas Based on Remote Sensing Data. Environ. Sci. 2022, 43, 4293–4304. [Google Scholar] [CrossRef]
- Xie, R.; Sabel, C.E.; Lu, X.; Zhu, W.; Kan, H.; Nielsen, C.P.; Wang, H. Long-Term trend and spatial pattern of PM2.5 induced premature mortality in China. Environ. Int. 2016, 97, 180–186. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Zhang, K. Contrast Study on the Local Indices of Spatial Autocorrelation. J. Geod. Geodyn. 2007, 7, 65–67. [Google Scholar] [CrossRef]
- Lelieveld, J.; Evans, J.S.; Fnais, M.; Giannadaki, D.; Pozzer, A. The contribution of outdoor air pollution sources to premature mortality on a global scale. Nature 2015, 525, 367–371. [Google Scholar] [CrossRef]
- Liu, N.; Yang, S.; Gao, X. Policy Implementation Effect of Coordinated Control for Air Pollutants and Greenhouse Gases. J. Nanjing Univ. Financ. Econ. 2024, 3, 12–22. [Google Scholar] [CrossRef]
- Chen, L.; Zhu, J.; Liao, H.; Yang, Y.; Yue, X. Meteorological influences on PM2.5 and O3 trends and associated health burden since China’s clean air actions. Sci. Total Environ. 2020, 744, 140837. [Google Scholar] [CrossRef]
- Han, J.; Li, Y.Z.; Li, F. Spatio-Temporal distribution characteristic of PM2.5 concentration and the difference of PM2.5 concentration between urban areas and rural areas in China from 2000 to 2015. Acta Ecol. Sin. 2019, 39, 2954–2962. [Google Scholar]
- Wang, X.; Chen, C.; He, J.; Zhu, S.; Guan, X. Learning-Based Online Transmission Path Selection for Secure Estimation in Edge Computing Systems. IEEE Trans. Ind. Inform. 2021, 17, 3577–3587. [Google Scholar] [CrossRef]
- Jiang, X.; Li, G.; Fu, W. Government environmental governance, structural adjustment and air quality: A quasi-natural experiment based on the Three-year Action Plan to Win the Blue Sky Defense War. J. Environ. Manag. 2021, 277, 111470. [Google Scholar] [CrossRef]
- Liu, H.; Lei, J.; Liu, Y.; Zhu, T.; Chan, K.; Chen, X.; Wei, J.; Deng, F.; Li, G.; Jiang, Y.; et al. Hospital admissions attributable to reduced air pollution due to clean-air policies in China. Nat. Med. 2025, 1–10. [Google Scholar] [CrossRef]
- Li, M.; Huang, X.; Yan, D.; Lai, S.; Zhang, Z.; Zhu, L.; Lu, Y.; Jiang, X.; Wang, N.; Wang, T.; et al. Coping with the concurrent heatwaves and ozone extremes in China under a warming climate. Sci. Bull. 2024, 69, 2938–2947. [Google Scholar] [CrossRef]
- Ban, J.; Lu, K.; Wang, Q.; Li, T. Climate change will amplify the inequitable exposure to compound heatwave and ozone pollution. One Earth 2022, 5, 677–686. [Google Scholar] [CrossRef]
- Liu, J.; Qi, J.; Yin, P.; Liu, W.; He, C.; Gao, Y.; Zhou, L.; Zhu, Y.; Kan, H.; Chen, R.; et al. Rising cause-specific mortality risk and burden of compound heatwaves amid climate change. Nat. Clim. Change 2024, 14, 1201–1209. [Google Scholar] [CrossRef]
- Xu, R.; Sun, H.; Zhong, Z.; Zheng, Y.; Liu, T.; Li, Y.; Liu, L.; Luo, L.; Wang, S.; Lv, Z.; et al. Ozone, Heat Wave, and Cardiovascular Disease Mortality: A Population-Based Case-Crossover Study. Environ. Sci. Technol. 2023, 58, 171–181. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Li, X.; Yang, X. Health in 15-minute Life Sphere: Community Response to Public Health Emergency. Planners 2020, 36, 102–106+120. [Google Scholar]
- Wang, L.; Zhou, K.; Wang, Z. Spatial Distribution of Community Pension Facilities From The Perspective of Health Equity: A Case Study of The Central City of Shanghai. Hum. Geogr. 2021, 36, 48–55. [Google Scholar] [CrossRef]
- Clark, L.P.; Millet, D.B.; Marshall, J.D. Air quality and urban form in U.S. urban areas: Evidence from regulatory monitors. Environ. Sci. Technol. 2011, 45, 7028–7035. [Google Scholar] [CrossRef]
- Xing, Q.; Zhang, L.; Liu, H.; Zhu, C.; Yao, M. Toxicological analysis and organ damages of rats injected with soluble ambient particulate matter from 31 cities in China. Atmos. Environ. 2025, 343, 121005. [Google Scholar] [CrossRef]
- Liu, T.; Meng, H.; Yu, M.; Xiao, Y.; Huang, B.; Lin, L.; Zhang, H.; Hu, R.; Hou, Z.; Xu, Y.; et al. Urban-Rural disparity of the short-term association of PM2.5 with mortality and its attributable burden. Innovation 2021, 2, 100171. [Google Scholar] [CrossRef]
- Zhou, H.; Hong, F.; Wang, L.; Tang, X.; Guo, B.; Luo, Y.; Yu, H.; Mao, D.; Liu, T.; Feng, Y. Air pollution and risk of 32 health conditions: Outcome-wide analyses in a population-based prospective cohort in Southwest China. BMC Med. 2024, 22, 370. [Google Scholar] [CrossRef]
- Wang, L.; Yang, J.; Wang, Z.; Wu, M.X. Rectifying the impairment of immune thrombocytopenia plasmas through photobiomodulation. Innov. Med. 2024, 2, 100046. [Google Scholar] [CrossRef]
- Xu, X.; Huang, L.; Yao, L.; Yoshida, Y.; Long, Y. Rising socio-economic costs of PM2.5 pollution and medical service mismatching. Nat. Sustain. 2025, 8, 265–275. [Google Scholar] [CrossRef]






| Area Type | Pollutants Objects | Prevention and Control Level | Constraint Condition |
|---|---|---|---|
| HA_CL1 | PM2.5 and O3 coordinated prevention and control | Level I | [R(PM2.5) ≥ 0] ∩ [R(O3) ≥ 0] |
| HA_CL2 | Level II | {[R(PM2.5) ≥ 0] ∩ [R(O3) < 0]} [23]∪{[R(PM2.5) < 0] ∩ [R(O3) ≥ 0]} | |
| HA_CL3 | Level III | [R(PM2.5) ≥ 0] ∩ [R(O3) ≥ 0] | |
| HA_PL1 | PM2.5 prevention and control | Level I | R(PM2.5) ≥ 0 |
| HA_PL2 | Level II | R(PM2.5) < 0 | |
| HA_OL1 | O3 prevention and control | Level I | R(O3) ≥ 0 |
| HA_OL2 | Level II | R(O3) < 0 |
| Type of Prevention and Control Area | Area (104 km2) | County-Level Administrative Districts | PM2.5 Health Risk (104 People) |
|---|---|---|---|
| HA_PL1 | 34.54 | 183 | 1.21 |
| HA_PL2 | 6.17 | 47 | 0.27 |
| HA_OL1 | 7.16 | 44 | 0.22 |
| HA_OL2 | 2.57 | 17 | 0.08 |
| HA_CL1 | 52.75 | 454 | 3.71 |
| HA_CL2 | 48.12 | 435 | 3.78 |
| Year | Area (104 km2) | Degree of Overlap | |||||
|---|---|---|---|---|---|---|---|
| KR | HA | HA_P | HA_O | HA | HA_P | HA_O | |
| 2010 | 104.33 | 161.64 | 109.72 | 122.98 | 0.47 | 0.51 | 0.44 |
| 2015 | 152.31 | 117.60 | 100.91 | 0.49 | 0.53 | 0.42 | |
| 2020 | 162.87 | 153.13 | 122.15 | 0.48 | 0.48 | 0.49 | |
| Year | Health Risk (104 People) | Average risk Rate (%) | ||||||
|---|---|---|---|---|---|---|---|---|
| PM2.5 | O3 | PM2.5 | O3 | |||||
| KR | HA | KR | HA | KR | HA_P | KR | HA_O | |
| 2010 | 77.81 | 99.26 | 7.57 | 9.61 | 0.12520 | 0.12861 | 0.01218 | 0.01228 |
| 2015 | 83.40 | 103.02 | 7.76 | 9.52 | 0.12788 | 0.12829 | 0.01189 | 0.01243 |
| 2020 | 82.45 | 102.30 | 8.95 | 10.97 | 0.12122 | 0.12020 | 0.01315 | 0.01316 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huang, X.; Zou, B.; Li, S. Identification and Time Series Analysis of PM2.5 and O3 Associated Health Risk Prevention and Control Areas. Toxics 2025, 13, 356. https://doi.org/10.3390/toxics13050356
Huang X, Zou B, Li S. Identification and Time Series Analysis of PM2.5 and O3 Associated Health Risk Prevention and Control Areas. Toxics. 2025; 13(5):356. https://doi.org/10.3390/toxics13050356
Chicago/Turabian StyleHuang, Xinyu, Bin Zou, and Shenxin Li. 2025. "Identification and Time Series Analysis of PM2.5 and O3 Associated Health Risk Prevention and Control Areas" Toxics 13, no. 5: 356. https://doi.org/10.3390/toxics13050356
APA StyleHuang, X., Zou, B., & Li, S. (2025). Identification and Time Series Analysis of PM2.5 and O3 Associated Health Risk Prevention and Control Areas. Toxics, 13(5), 356. https://doi.org/10.3390/toxics13050356






