PS-MPs Induced Inflammation and Phosphorylation of Inflammatory Signalling Pathways in Liver
Abstract
:1. Introduction
2. Materials and Methods
2.1. Polystyrene Microspheres
2.2. Animal Experiments
2.3. Serum Liver Function Indicators and Hepatic Pathology
2.4. Cell Material and Growth Conditions
2.5. Cell Morphology Analysis
2.6. Cytotoxicity Assay
2.7. Enzyme-Linked Immunosorbent Assay
2.8. Flow Cytometry Bead-Based Assay
2.9. Proteome Profiling Arrays
2.10. RNA Extraction and RT-qPCR Array
2.11. Western Blot Analysis
2.12. Statistical Analysis
3. Results
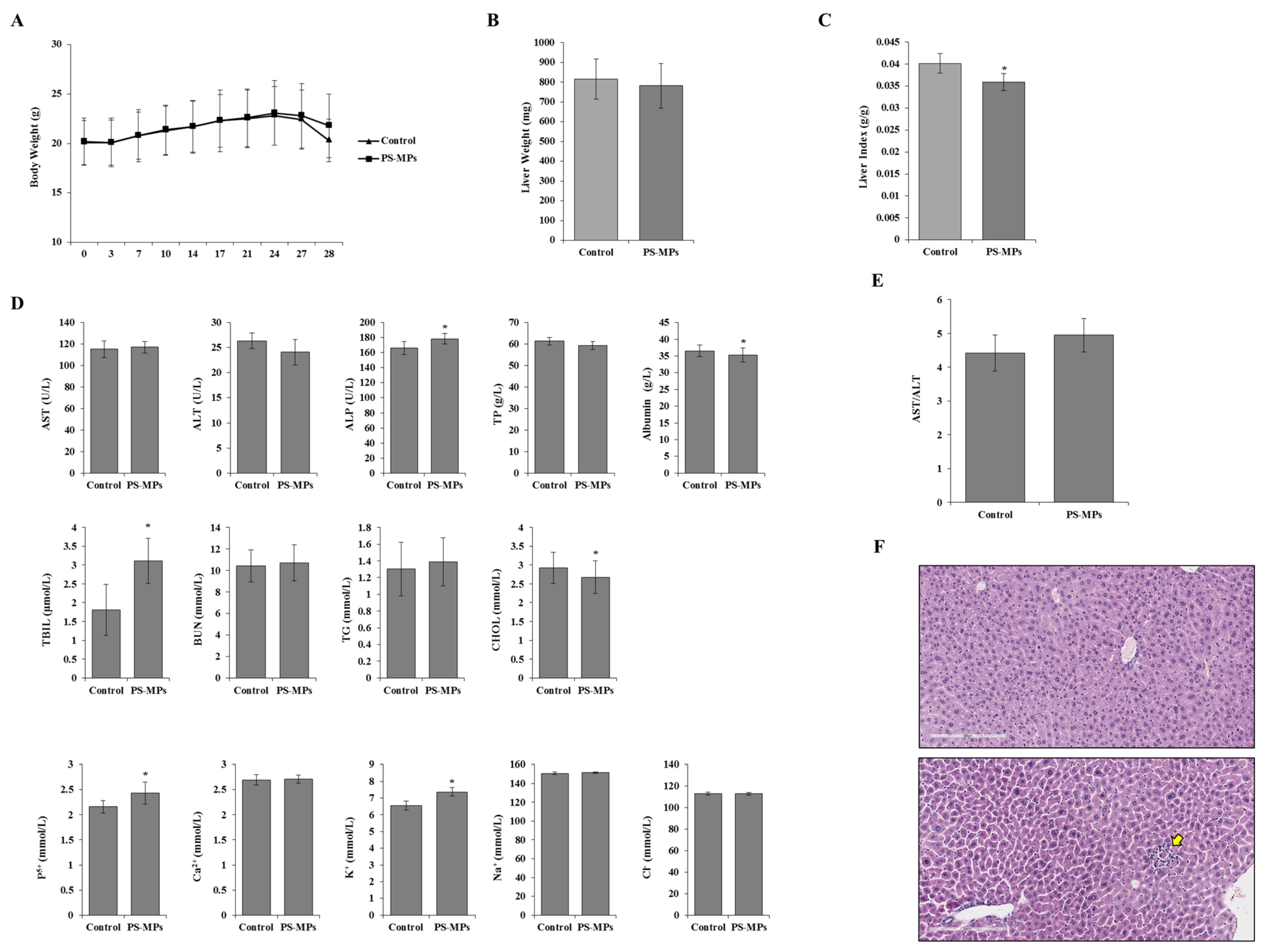
3.1. In Vivo Assay
Effects of PS-MPs on the Mouse
3.2. In Vitro Assay
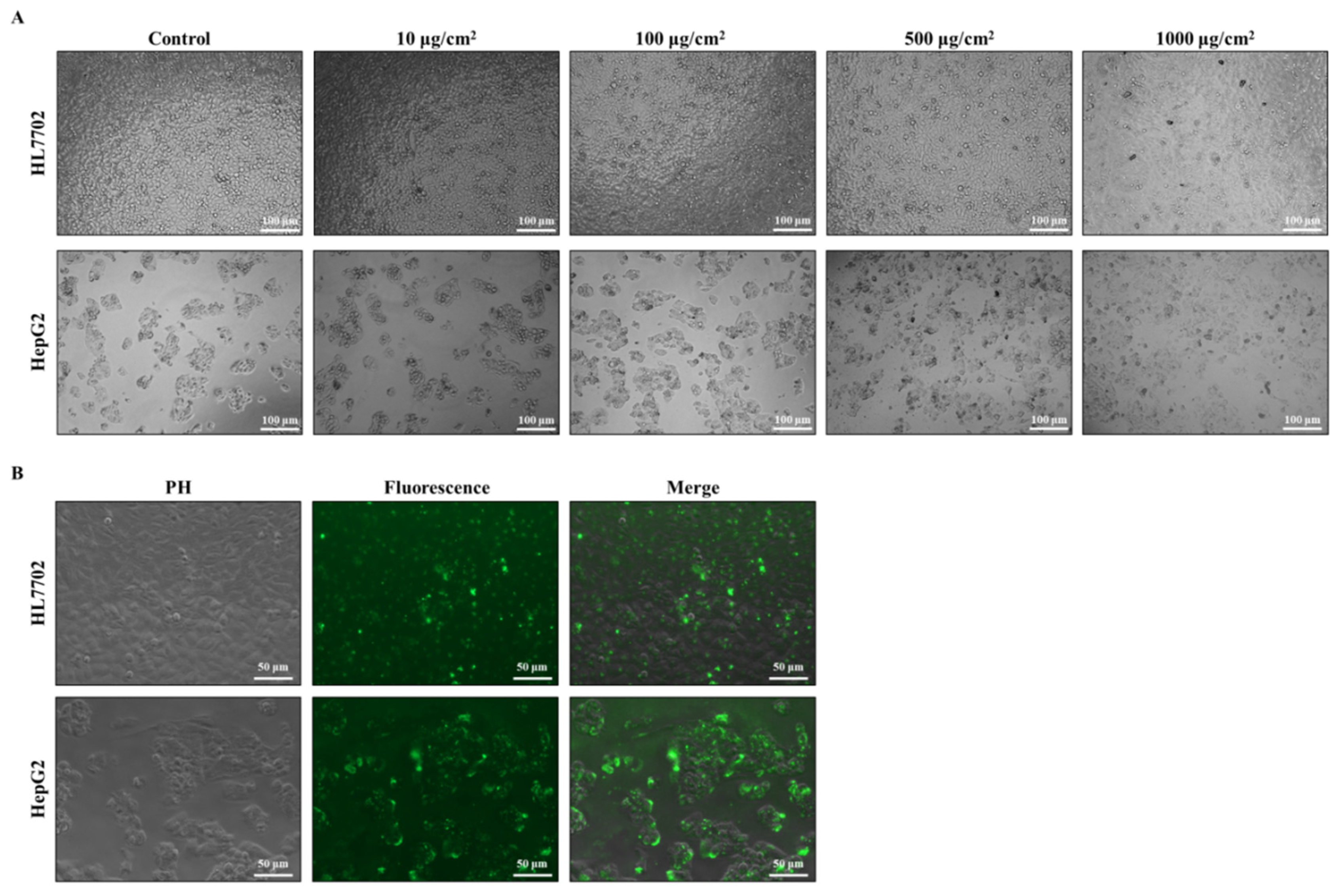
3.2.1. Effects of PS-MPs on Cell Morphology
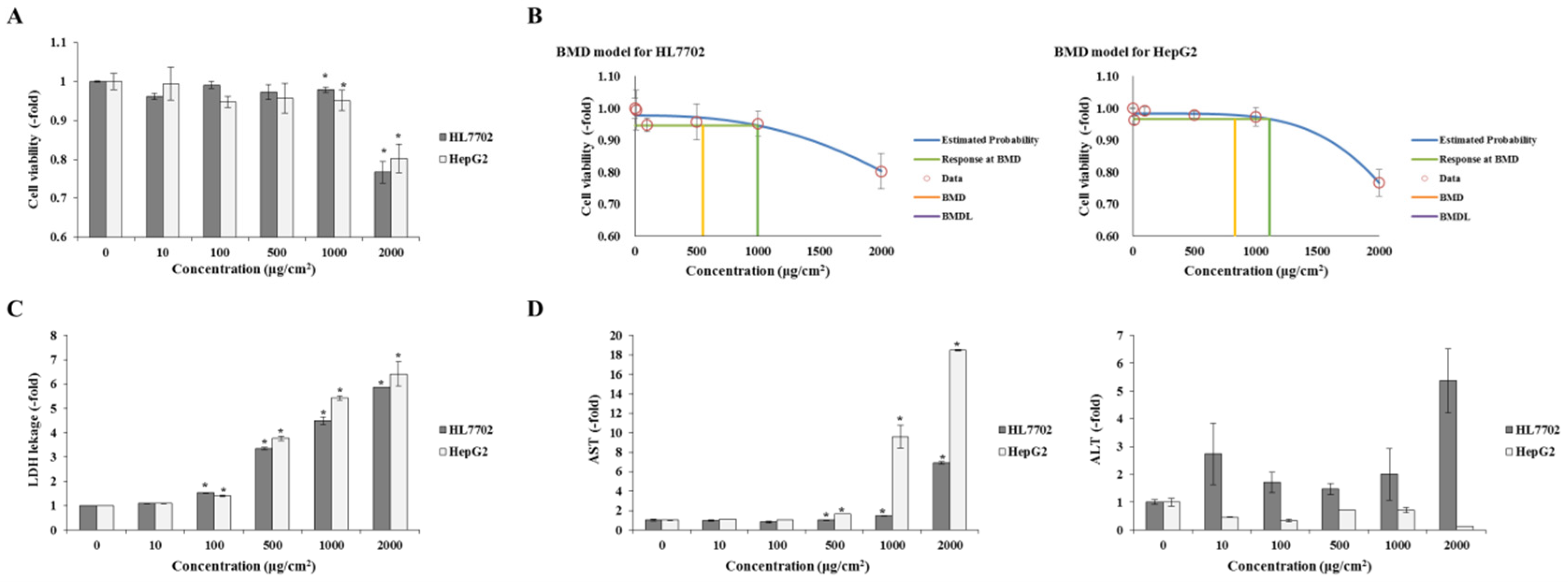
3.2.2. Cytotoxic Effects
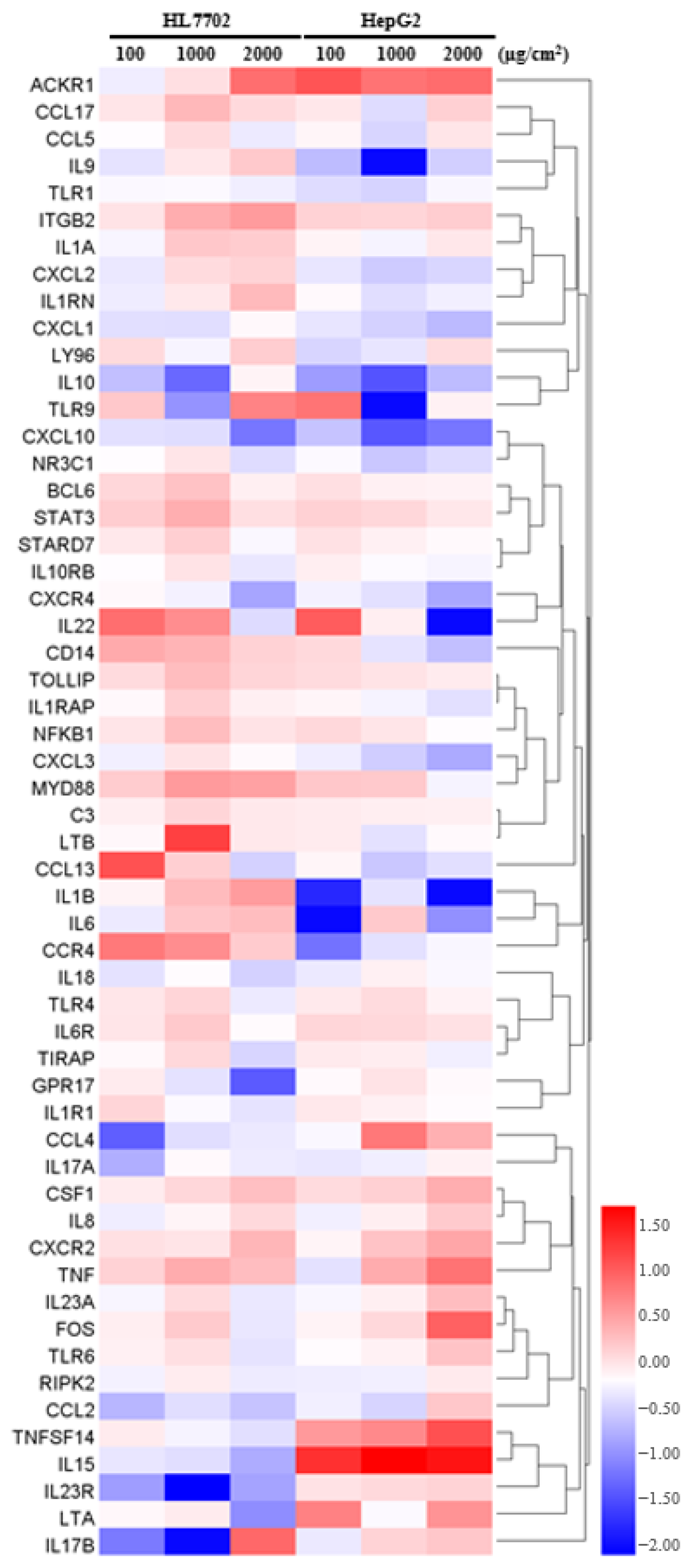
3.2.3. Effect of PS-MPs on Chemokines
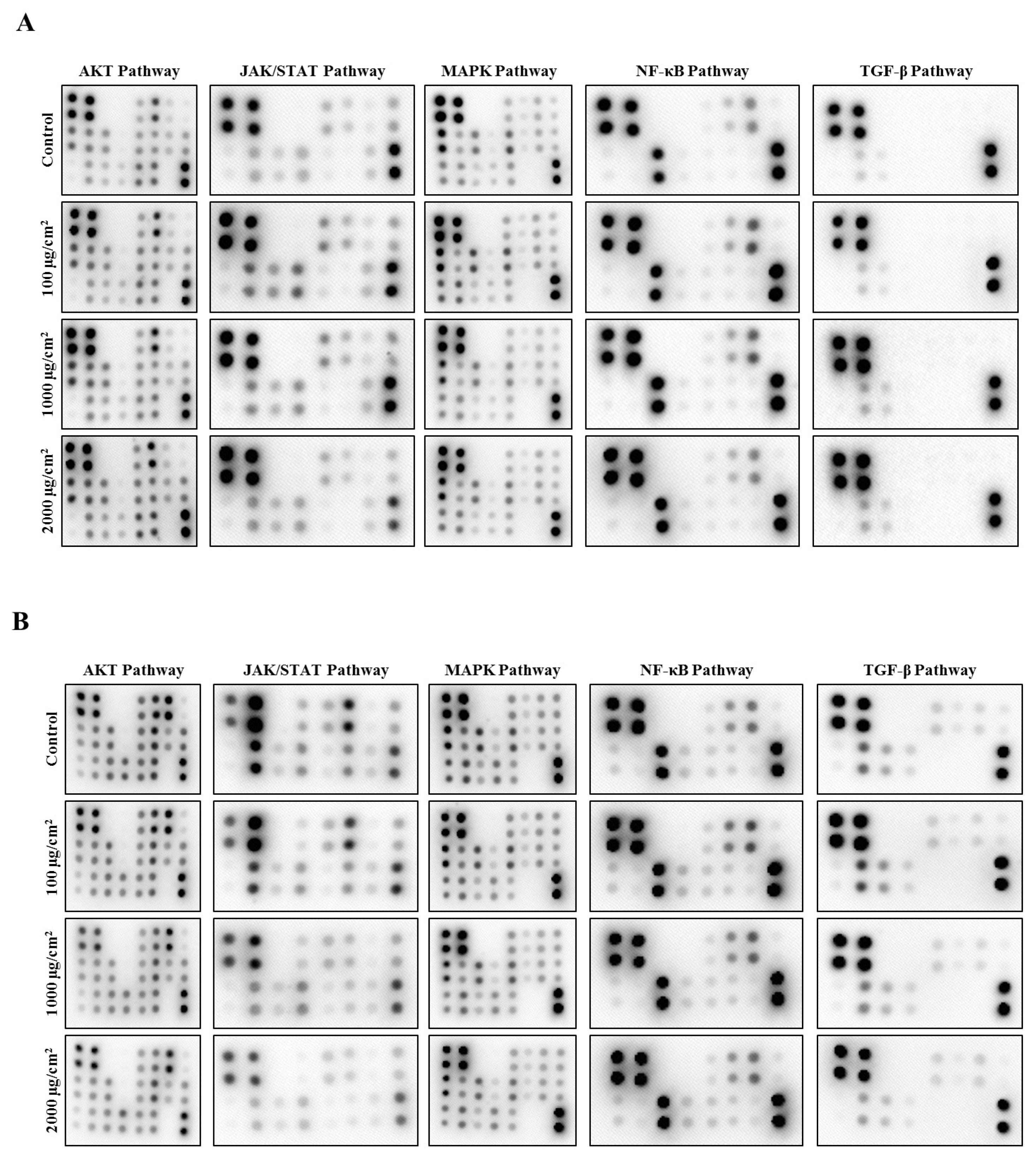
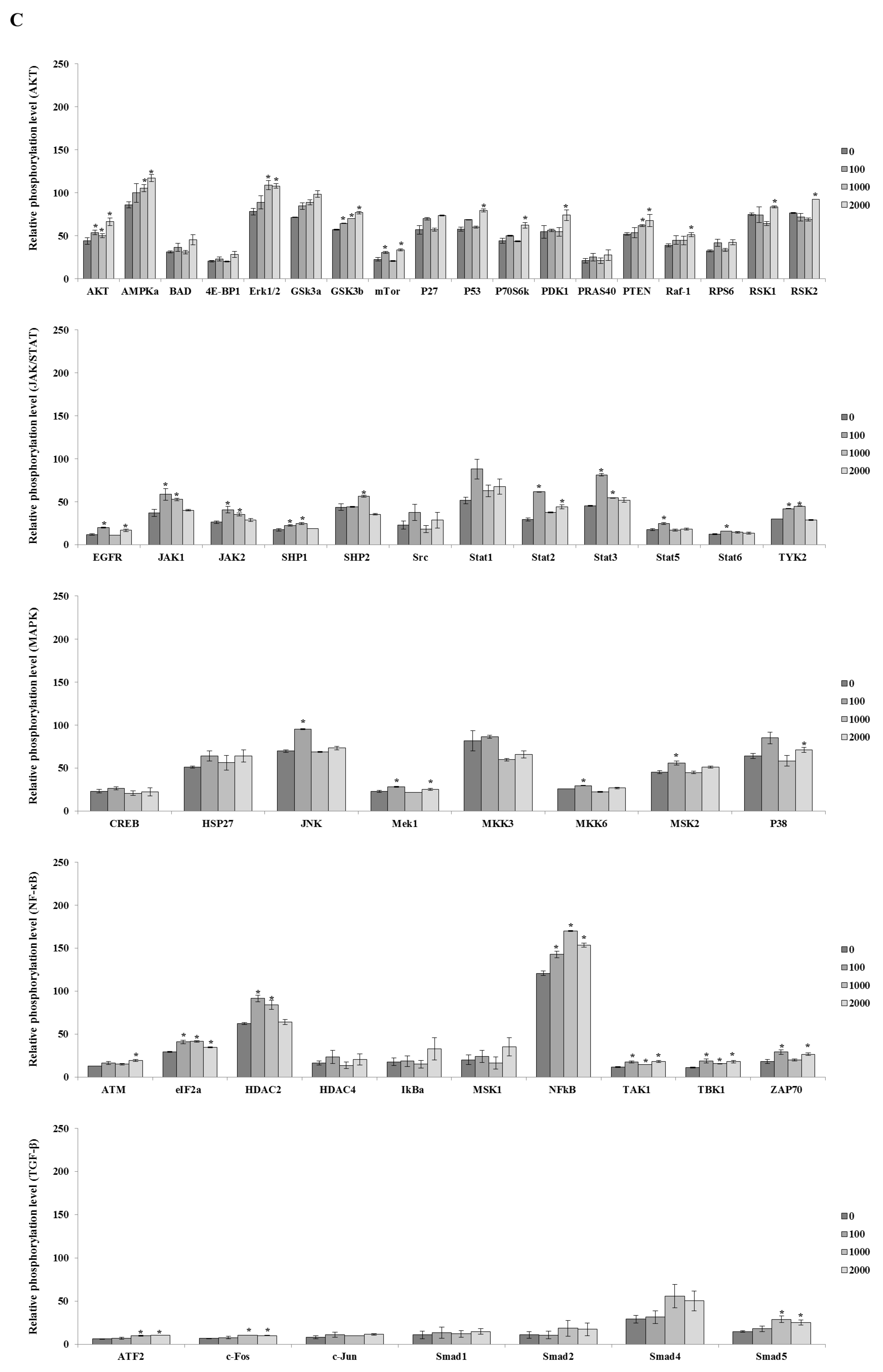
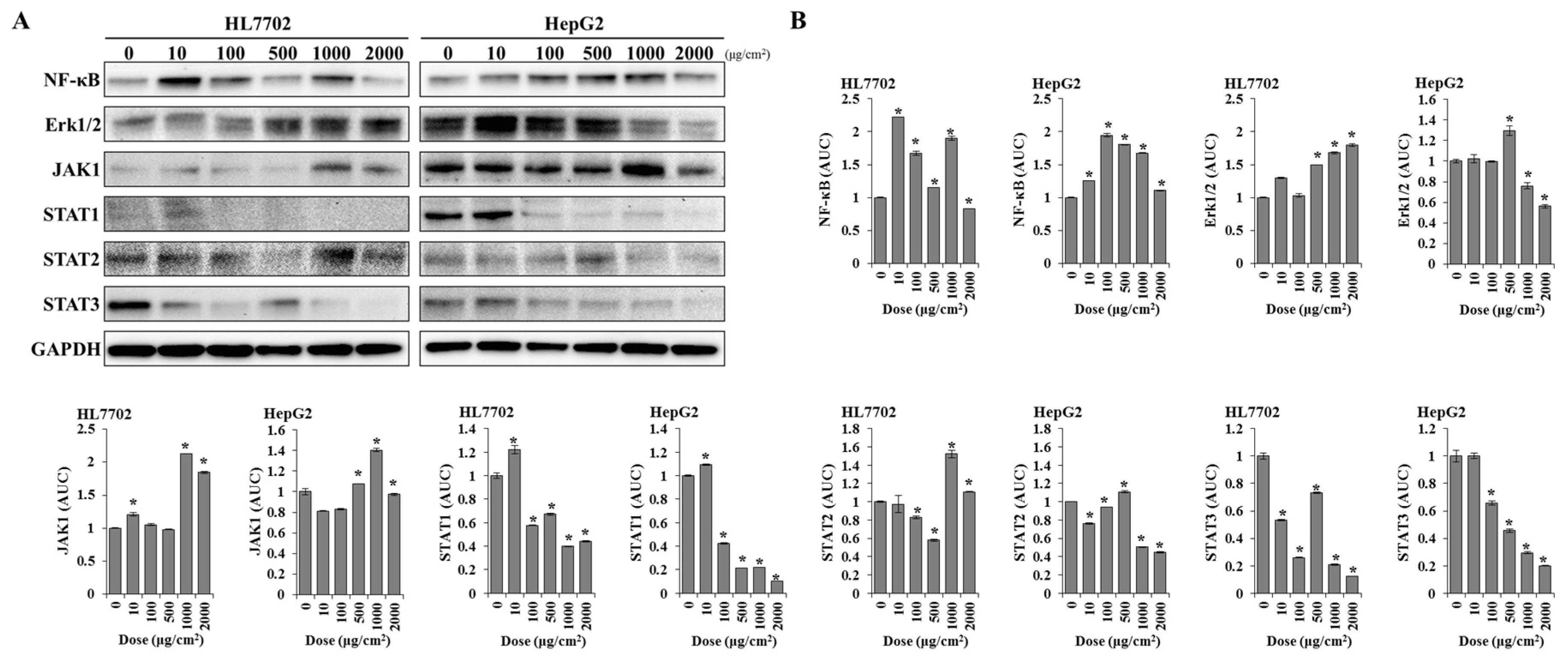
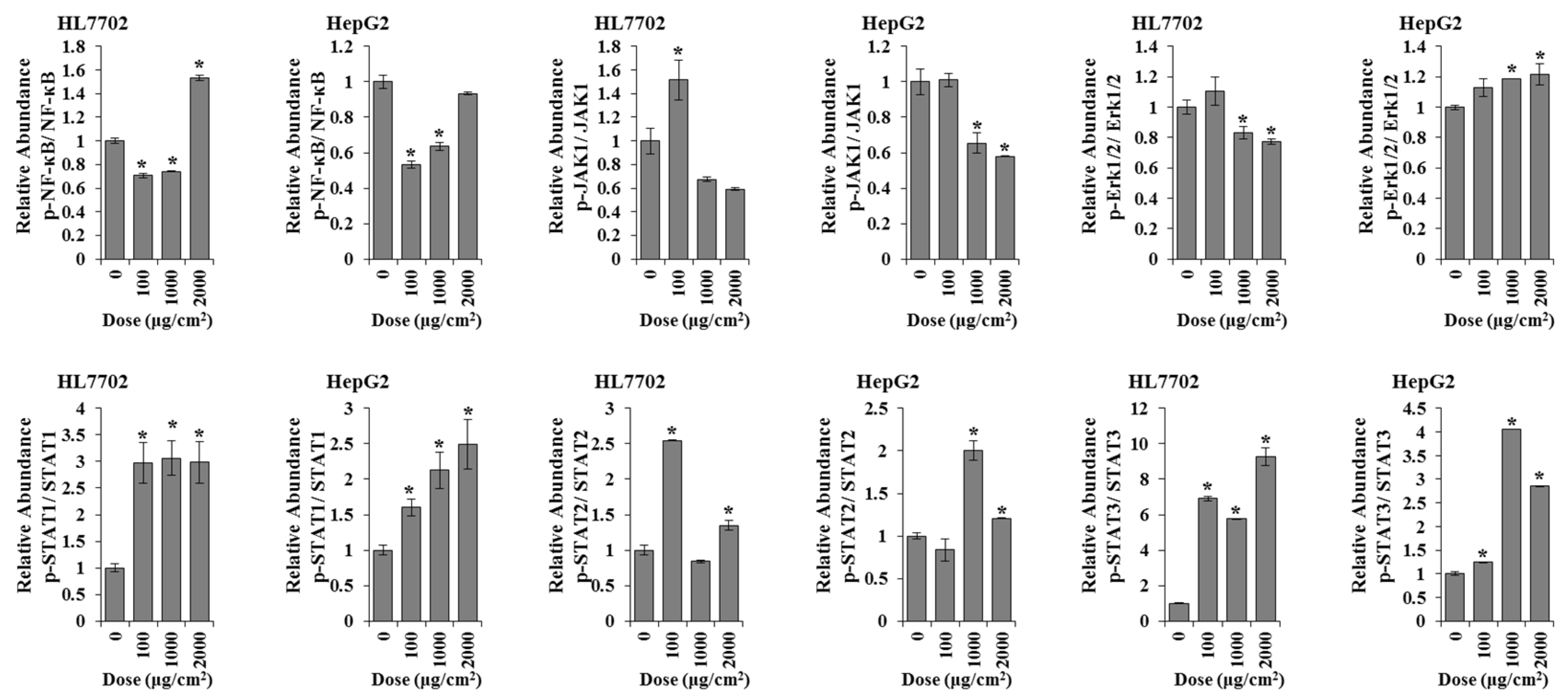
3.2.4. Detection of the Protein and Phosphorylation Levels of the Inflammation-Related Signalling Pathway
4. Discussion
5. Study Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Azzarello, M.; Van Vleet, E. Marine birds and plastic pollution. Mar. Ecol. Prog. Ser. 1987, 37, 295–303. [Google Scholar] [CrossRef]
- European Commission. Plastic Waste: Ecological and Human Health Impacts. Science for Environment Policy; European Commission: Brussels, Belgium, November 2011; Available online: https://anthropolis.hu/eathink-tankonyv/wp-content/uploads/2017/12/12_Plastic-Waste-Ecological-nad-Human-Health-Impacts.pdf (accessed on 19 December 2024).
- Thompson, R.C.; Olson, Y.; Mitchell, R.P.; Davis, A.; Rowland, S.J.; John, A.W.G.; McGonigle, D.; Russell, A.E. Lost at Sea: Where Is All the Plastic? Science 2004, 304, 838. [Google Scholar] [CrossRef] [PubMed]
- Gao, X.; Hou, L.; Sheng, J. Research progress on health hazards of microplastics. Prev. Med. 2020, 32, 800–804. [Google Scholar]
- Arthur, C.; Baker, J.; Bamford, H. (Eds.) Proceedings of the International Research Workshop on the Occurrence, Effects, and Fate of Microplastic Marine Debris, September 9–11, 2008, University of Washington Tacoma, Tacoma, WA, USA; NOAA Marine Debris Division: Silver Spring, MD, USA, 2008. Available online: https://repository.library.noaa.gov/view/noaa/2509/noaa_2509_DS1.pdf (accessed on 19 December 2024).
- Allen, S.; Allen, D.; Baladima, F.; Phoenix, V.R.; Thomas, J.L.; Le Roux, G.; Sonke, J.E. Evidence of free tropospheric and long-range transport of microplastic at Pic du Midi Observatory. Nat. Commun. 2021, 12, 7242. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.; Anshita, D.; Ravichandiran, V. MCP-1: Function, regulation, and involvement in disease. Int. Immunopharmacol. 2021, 101, 107598. [Google Scholar] [CrossRef]
- Li, L.; Luo, Y.; Li, R.; Zhou, Q.; Peijnenburg, W.J.G.M.; Yin, N.; Yang, J.; Tu, C.; Zhang, Y. Effective uptake of submicrometre plastics by crop plants via a crack-entry mode. Nat. Sustain. 2020, 3, 929–937. [Google Scholar] [CrossRef]
- Li, D.; Shi, Y.; Yang, L.; Xiao, L.; Kehoe, D.K.; Gun’ko, Y.K.; Boland, J.J.; Wang, J.J. Microplastic release from the degradation of polypropylene feeding bottles during infant formula preparation. Nat. Food 2020, 1, 746–754. [Google Scholar] [CrossRef]
- Zhang, J.; Wang, L.; Trasande, L.; Kannan, K. Occurrence of Polyethylene Terephthalate and Polycarbonate Microplastics in Infant and Adult Feces. Environ. Sci. Technol. Lett. 2021, 8, 989–994. [Google Scholar] [CrossRef]
- Ragusa, A.; Svelato, A.; Santacroce, C.; Catalano, P.; Notarstefano, V.; Carnevali, O.; Papa, F.; Rongioletti, M.C.A.; Baiocco, F.; Draghi, S.; et al. Plasticenta: First evidence of microplastics in human placenta. Environ. Int. 2021, 146, 106274. [Google Scholar] [CrossRef]
- Leslie, H.A.; van Velzen, M.J.M.; Brandsma, S.H.; Vethaak, A.D.; Garcia-Vallejo, J.J.; Lamoree, M.H. Discovery and quantification of plastic particle pollution in human blood. Environ. Int. 2022, 163, 107199. [Google Scholar] [CrossRef]
- Zhao, L.; Shi, W.; Hu, F.; Song, X.; Cheng, Z.; Zhou, J. Prolonged oral ingestion of microplastics induced inflammation in the liver tissues of C57BL/6J mice through polarization of macrophages and increased infiltration of natural killer cells. Ecotoxicol. Environ. Saf. 2021, 227, 112882. [Google Scholar] [CrossRef] [PubMed]
- Cheng, W.; Li, X.; Zhou, Y.; Yu, H.; Xie, Y.; Guo, H.; Wang, H.; Li, Y.; Feng, Y.; Wang, Y. Polystyrene microplastics induce hepatotoxicity and disrupt lipid metabolism in the liver organoids. Sci. Total Environ. 2022, 806, 150328. [Google Scholar] [CrossRef] [PubMed]
- OECD. Test No. 407: Repeated Dose 28-day Oral Toxicity Study in Rodents, OECD Guidelines for the Testing of Chemicals, Section 4; OECD Publishing: Paris, France, 2008. [Google Scholar] [CrossRef]
- Livak, K.J.; Schmittgen, T.D. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods 2001, 25, 402–408. [Google Scholar] [CrossRef] [PubMed]
- Deng, W.; Wang, Y.; Liu, Z.; Cheng, H.; Xue, Y. HemI: A toolkit for illustrating heatmaps. PLoS ONE 2014, 9, e111988. [Google Scholar] [CrossRef]
- United States Environmental Protection Agency. Benchmark Dose Software (BMDS) (Build 3.3.2; Model Library Version 2023.03.1) [Computer Software]. 2023. Available online: https://www.epa.gov/bmds/download-bmds (accessed on 19 December 2024).
- Souza Machado, A.A.; Kloas, W.; Zarfl, C.; Hempel, S.; Rillig, M.C. Microplastics as an emerging threat to terrestrial ecosystems. Glob. Chang. Biol. 2018, 24, 1405–1416. [Google Scholar] [CrossRef]
- Alimba, C.G.; Faggio, C. Microplastics in the marine environment: Current trends in environmental pollution and mechanisms of toxicological profile. Environ. Toxicol. Pharmacol. 2019, 68, 61–74. [Google Scholar] [CrossRef]
- Ma, H.Y.; Dong, L.; Quan, S.Z.; Li, R.Y.; Wang, X.R. Comparison of four markers of hepatic fibrosis and hepatic function indices in patients with liver cirrhosis and hepatoma. Ann. Palliat. Med. 2021, 10, 4108–4121. [Google Scholar] [CrossRef]
- Baggiolini, M.; Clark-Lewis, I. Interleukin-8, a chemotactic and inflammatory cytokine. FEBS Lett. 1992, 307, 97–101. [Google Scholar] [CrossRef]
- Sánchez-Gutiérrez, R.; Araujo-Pérez, J.; Alvarado-Hernández, D.L.; González-Amaro, A.M.; Méndez-González, V.; Rivas-Santiago, B.; González-Amaro, R.; Pozos-Guillén, A.; Vitales-Noyola, M. Increased IL-12p70 and IL-8 Produced by Monocytes in Response to Streptococcus spp. and Actinomyces spp. Causals of Endodontic Primary Infections. Int. J. Mol. Sci. 2023, 24, 16853. [Google Scholar] [CrossRef]
- Tanaka, T.; Narazaki, M.; Kishimoto, T. Il-6 in inflammation, Immunity, and disease. Cold Spring Harb. Perspect. Biol. 2014, 6, a016295. [Google Scholar] [CrossRef]
- Lupancu, T.J.; Eivazitork, M.; Hamilton, J.A.; Achuthan, A.A.; Lee, K.M. CCL17/TARC in autoimmunity and inflammation-not just a T-cell chemokine. Immunol. Cell Biol. 2023, 101, 600–609. [Google Scholar] [CrossRef] [PubMed]
- Crawford, K.S.; Volkman, B.F. Prospects for targeting ACKR1 in cancer and other diseases. Front. Immunol. 2023, 14, 1111960. [Google Scholar] [CrossRef] [PubMed]
- Amatya, N.; Garg, A.V.; Gaffen, S.L. IL-17 Signaling: The Yin and the Yang. Trends Immunol. 2017, 38, 310–322. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Zhao, C.; Meng, J.; Li, N.; Xu, Z.; Liu, X.; Hou, S. Galectin-3 regulates microglial activation and promotes inflammation through TLR4/MyD88/NF-kB in experimental autoimmune uveitis. Clin. Immunol. 2022, 236, 108939. [Google Scholar] [CrossRef]
- Zusso, M.; Lunardi, V.; Franceschini, D.; Pagetta, A.; Lo, R.; Stifani, S.; Frigo, A.C.; Giusti, P.; Moro, S. Ciprofloxacin and levofloxacin attenuate the microglial inflammatory response via the TLR4/NF-kB pathway. J. Neuroinflammation 2019, 16, 148. [Google Scholar] [CrossRef]
- Liu, G.; Lu, Y.; Shi, L.; Ren, Y.; Kong, J.; Zhang, M.; Chen, M.; Liu, W. TLR4-MyD88 signaling pathway is responsible for acute lung inflammation induced by reclaimed water. J. Hazard. Mater. 2020, 396, 122586. [Google Scholar] [CrossRef]
- Zhang, R.Y.; Zhang, X.S.; Lu, C.; Wang, Z.R.; Shi, Y.; Wang, Y.G.; Zhang, P.; Chen, Y. TLR4-MyD88-NF-κB signaling imbalances Th17 and Treg cells in thymoma with myasthenia gravis. Eur. Rev. Med. Pharmacol. Sci. 2023, 27, 10342–10364. [Google Scholar] [CrossRef]
- Yang, H.C.; Cheng, M.L.; Hua, Y.S.; Wu, Y.H.; Lin, H.R.; Liu, H.Y.; Ho, H.Y.; Chiu, D.T. Glucose 6-phosphate dehydrogenase knockdown enhances IL-8 expression in HepG2 cells via oxidative stress and NF-κB signaling pathway. J. Inflamm. 2015, 12, 34. [Google Scholar] [CrossRef]
- Xin, P.; Xu, X.; Deng, C.; Liu, S.; Wang, Y.; Zhou, X.; Ma, H.; Wei, D.; Sun, S. The role of JAK/STAT signaling pathway and its inhibitors in diseases. Int. Immunopharmacol. 2020, 80, 106210. [Google Scholar] [CrossRef]
- Philips, R.L.; Wang, Y.; Cheon, H.; Kanno, Y.; Gadina, M.; Sartorelli, V.; Horvath, C.M.; Darnell, J.E., Jr.; Stark, G.R.; O’Shea, J.J. The JAK-STAT pathway at 30: Much learned, much more to do. Cell 2022, 185, 3857–3876. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ying, M.; Shao, N.; Dong, C.; Sha, Y.; Li, C.; Hong, X.; Ding, Y.; Xu, J.; Qian, K.; Tao, G.; et al. PS-MPs Induced Inflammation and Phosphorylation of Inflammatory Signalling Pathways in Liver. Toxics 2024, 12, 932. https://doi.org/10.3390/toxics12120932
Ying M, Shao N, Dong C, Sha Y, Li C, Hong X, Ding Y, Xu J, Qian K, Tao G, et al. PS-MPs Induced Inflammation and Phosphorylation of Inflammatory Signalling Pathways in Liver. Toxics. 2024; 12(12):932. https://doi.org/10.3390/toxics12120932
Chicago/Turabian StyleYing, Mengchao, Naimin Shao, Cheng Dong, Yijie Sha, Chen Li, Xinyu Hong, Yu Ding, Jing Xu, Kelei Qian, Gonghua Tao, and et al. 2024. "PS-MPs Induced Inflammation and Phosphorylation of Inflammatory Signalling Pathways in Liver" Toxics 12, no. 12: 932. https://doi.org/10.3390/toxics12120932
APA StyleYing, M., Shao, N., Dong, C., Sha, Y., Li, C., Hong, X., Ding, Y., Xu, J., Qian, K., Tao, G., & Xiao, P. (2024). PS-MPs Induced Inflammation and Phosphorylation of Inflammatory Signalling Pathways in Liver. Toxics, 12(12), 932. https://doi.org/10.3390/toxics12120932




