e-Cigarette Vapour Condensate Reduces Viability and Impairs Function of Human Osteoblasts, in Part, via a Nicotine Dependent Mechanism
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethical Approval and Subject Recruitment
2.2. Primary Human Osteoblast Cell Culture
2.3. e-Cigarette Devices
2.4. e-Cigarette Vapour Condensate Collection
2.5. Osteoblast Challenge and Intervention
2.6. Primary Human Osteoblast Viability and Cellular Morphology
2.7. Quantification of OPG and RANK-L Secretion from Primary Human Osteoblasts
2.8. Statistical Analysis
3. Results
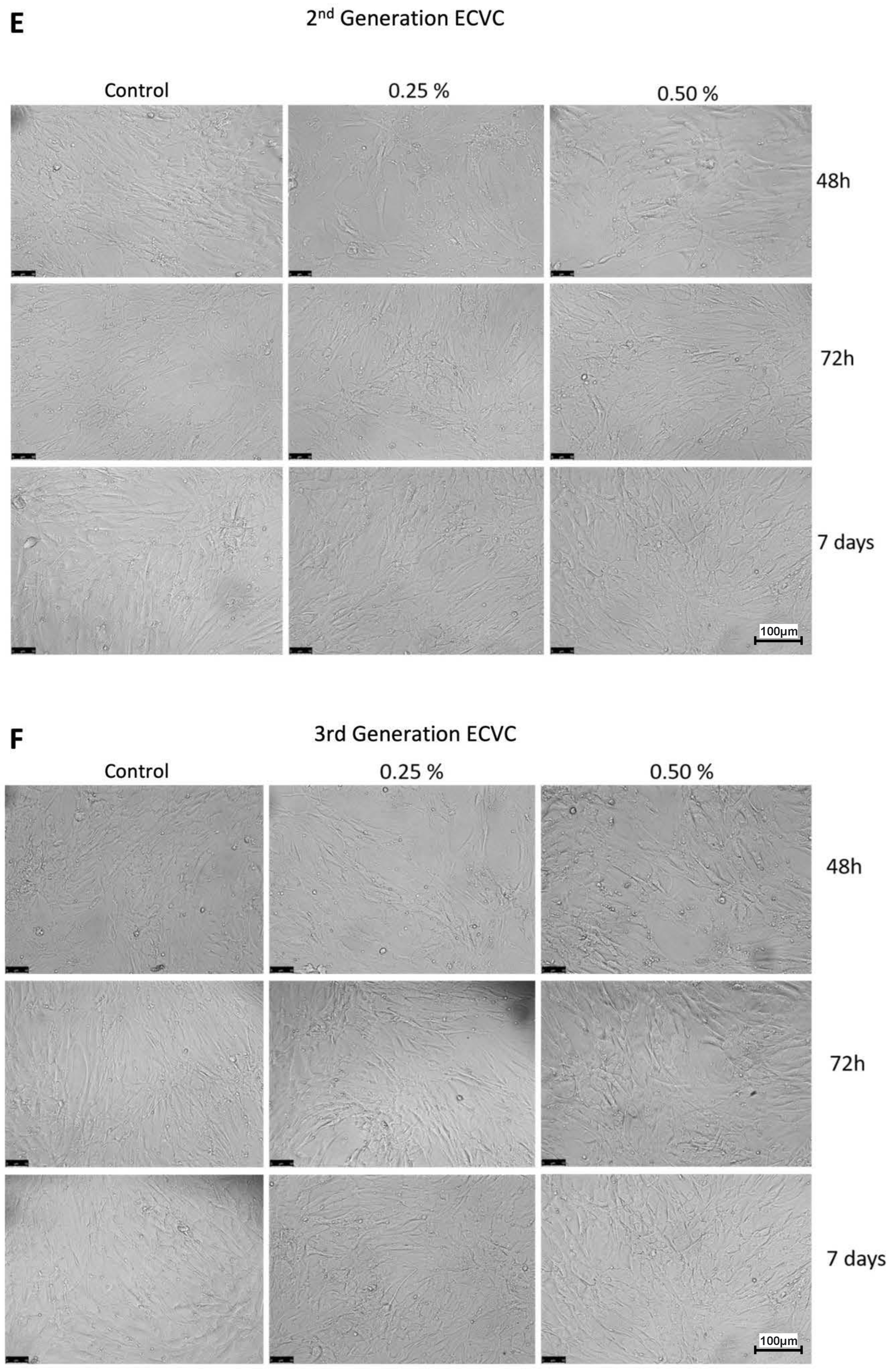
3.1. ECVC from either 2nd or 3rd Generation e-Cigarette Devices Reduces Human Osteoblast Viability and Alters Cellular Morphology
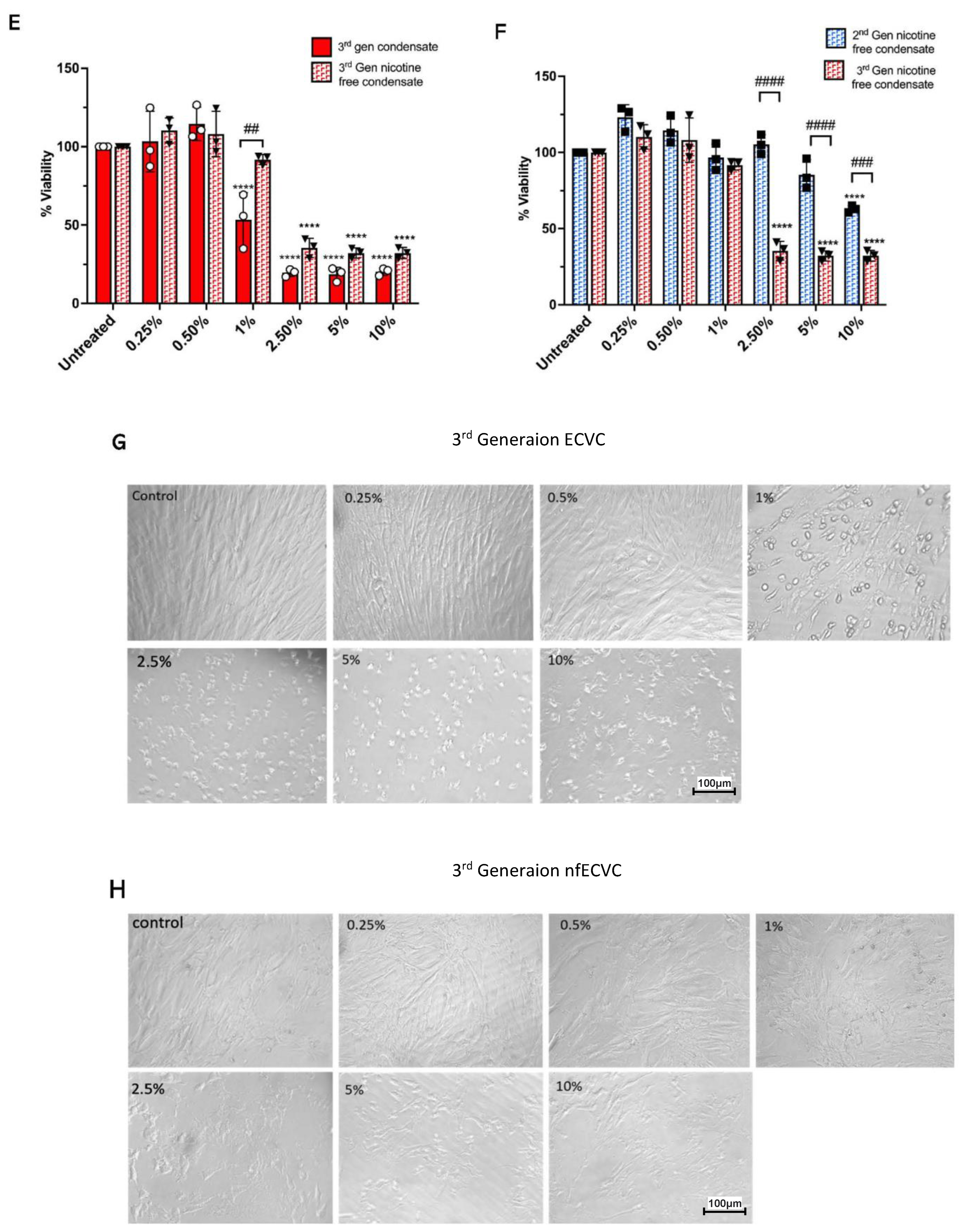
3.2. ECVC from Nicotine-Free 3rd Generation Devices Has a Greater Effect on Reducing Osteoblast Viability than Nicotine-Free 2nd Generation e-Cigarette Devices
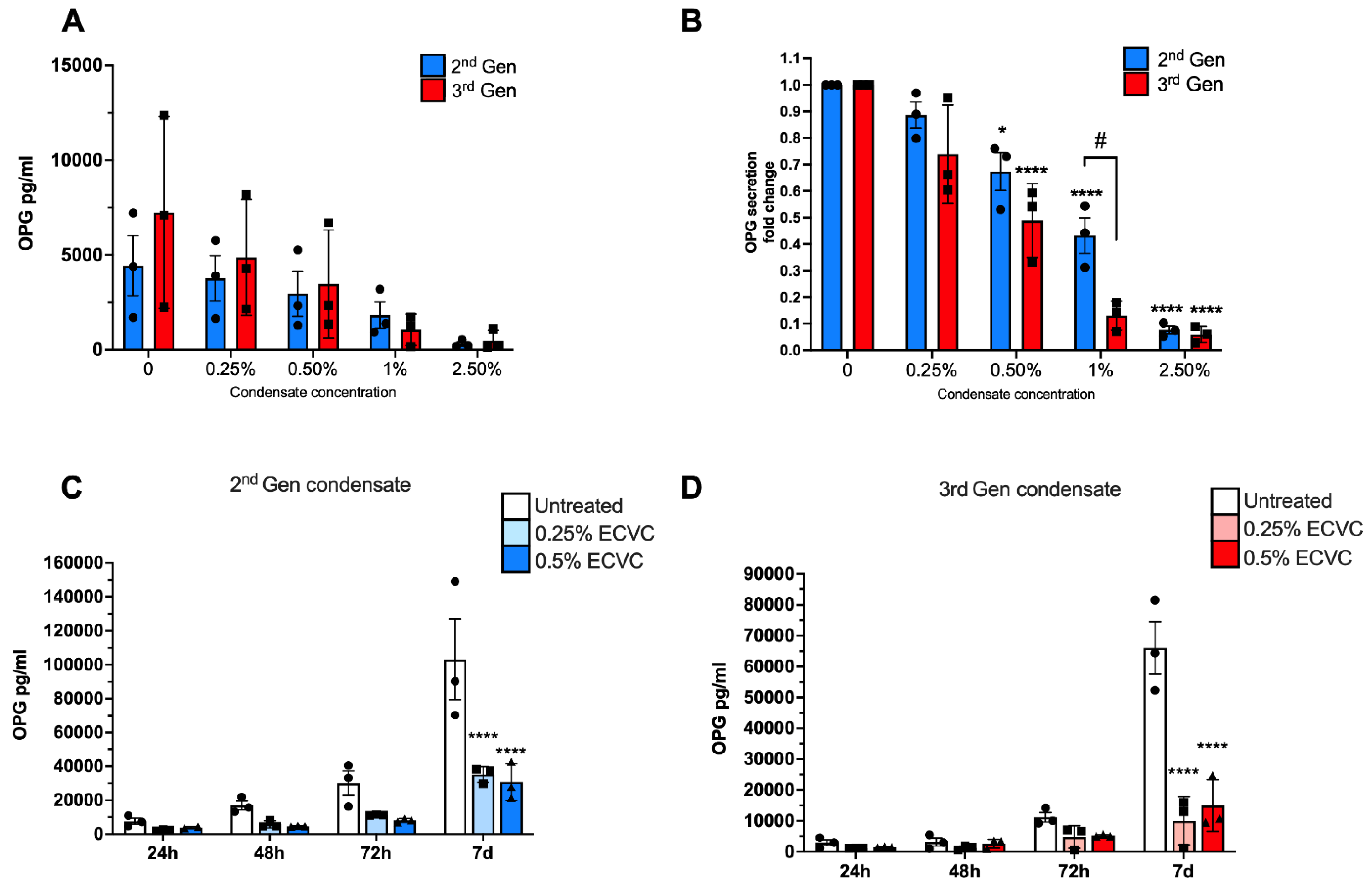
3.3. Sub-Cytotoxic Doses of e-Cigarette Condensate Alters Human Osteoblast Function
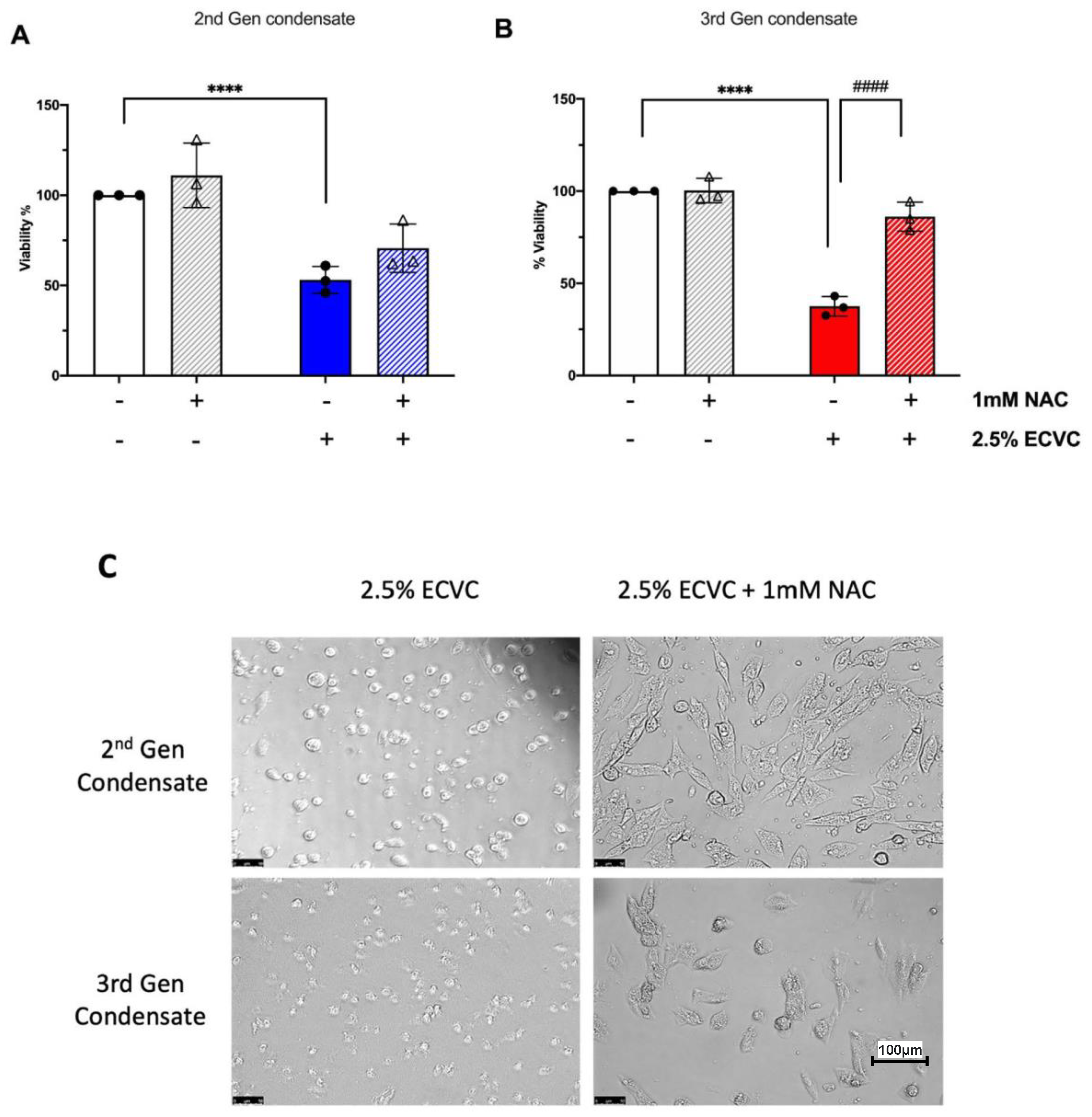
3.4. The Antioxidant N-Acetyl Cysteine Rescues the ECVC-Induced Reduction in Osteoblast Viability
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A

References
- Patel, R.A.; Wilson, R.F.; Patel, P.A.; Palmer, R.M. The effect of smoking on bone healing: A systematic review. Bone Jt. Res. 2013, 2, 102–111. [Google Scholar] [CrossRef] [PubMed]
- Law, M.R.; Hackshaw, A.K. A meta-analysis of cigarette smoking, bone mineral density and risk of hip fracture: Recognition of a major effect. BMJ 1997, 315, 841–846. [Google Scholar] [CrossRef] [PubMed]
- Tamaki, J.; Iki, M.; Sato, Y.; Kajita, E.; Kagamimori, S.; Kagawa, Y.; Yoneshima, H. Smoking among premenopausal women is associated with increased risk of low bone status: The JPOS Study. J. Bone Min. Metab. 2010, 28, 320–327. [Google Scholar] [CrossRef]
- Ward, K.D.; Klesges, R.C. A meta-analysis of the effects of cigarette smoking on bone mineral density. Calcif. Tissue Int. 2001, 68, 259–270. [Google Scholar] [CrossRef] [PubMed]
- Szulc, P.; Debiesse, E.; Boutroy, S.; Vilauphiou, N.; Chapurlat, R. Poor trabecular microarchitecture in male current smokers: The cross-sectional STRAMBO study. Calcif. Tissue Int. 2011, 89, 303–311. [Google Scholar] [CrossRef] [PubMed]
- Rudang, R.; Darelid, A.; Nilsson, M.; Nilsson, S.; Mellstrom, D.; Ohlsson, C.; Lorentzon, M. Smoking is associated with impaired bone mass development in young adult men: A 5-year longitudinal study. J. Bone Min. Res. 2012, 27, 2189–2197. [Google Scholar] [CrossRef] [PubMed]
- Singh, J.A.; Schleck, C.; Harmsen, W.S.; Jacob, A.K.; Warner, D.O.; Lewallen, D.G. Current tobacco use is associated with higher rates of implant revision and deep infection after total hip or knee arthroplasty: A prospective cohort study. BMC Med. 2015, 13, 283. [Google Scholar] [CrossRef] [PubMed]
- Matharu, G.S.; Mouchti, S.; Twigg, S.; Delmestri, A.; Murray, D.W.; Judge, A.; Pandit, H.G. The effect of smoking on outcomes following primary total hip and knee arthroplasty: A population-based cohort study of 117,024 patients. Acta Orthop. 2019, 90, 559–567. [Google Scholar] [CrossRef]
- Teng, S.; Yi, C.; Krettek, C.; Jagodzinski, M. Smoking and risk of prosthesis-related complications after total hip arthroplasty: A meta-analysis of cohort studies. PLoS ONE 2015, 10, e0125294. [Google Scholar] [CrossRef]
- Abrahamsen, B.; Brask-Lindemann, D.; Rubin, K.H.; Schwarz, P. A review of lifestyle, smoking and other modifiable risk factors for osteoporotic fractures. BoneKey Rep. 2014, 3, 574. [Google Scholar] [CrossRef]
- Rom, O.; Pecorelli, A.; Valacchi, G.; Reznick, A.Z. Are E-cigarettes a safe and good alternative to cigarette smoking? Ann. N.Y. Acad. Sci. 2015, 1340, 65–74. [Google Scholar] [CrossRef] [PubMed]
- McNeill, A.; Brose, L.S.; Calder, R.; Bauld, L.; Robson, D. Evidence Review of E-Cigarettes and Heated Tobacco Products 2018; Public Health England: London, UK, 2018. [Google Scholar]
- Cornish, D.; Brookman, A.; Horton, M.; Scanlon, S. Adult Smoking Habits in the UK: 2018; Office for National Statistics, Ed.; Office for National Statistics: Newport, UK, 2019. [Google Scholar]
- Agoons, D.D.; Agoons, B.B.; Emmanuel, K.E.; Matawalle, F.A.; Cunningham, J.M. Association between electronic cigarette use and fragility fractures among US adults. Am. J. Med. Open 2021, 1, 100002. [Google Scholar] [CrossRef]
- Davis, L.C.; Sapey, E.; Thickett, D.R.; Scott, A. Predicting the pulmonary effects of long-term e-cigarette use: Are the clouds clearing? Eur. Respir. Rev. 2022, 31, 210121. [Google Scholar] [CrossRef]
- Jasper, A.E.; McIver, W.J.; Sapey, E.; Walton, G.M. Understanding the role of neutrophils in chronic inflammatory airway disease. F1000Research 2019, 8, F1000 Faculty Rev-55. [Google Scholar] [CrossRef]
- Son, Y.; Wackowski, O.; Weisel, C.; Schwander, S.; Mainelis, G.; Delnevo, C.; Meng, Q. Evaluation of E-Vapor Nicotine and Nicotyrine Concentrations under Various E-Liquid Compositions, Device Settings, and Vaping Topographies. Chem. Res. Toxicol. 2018, 31, 861–868. [Google Scholar] [CrossRef]
- Hiler, M.; Karaoghlanian, N.; Talih, S.; Maloney, S.; Breland, A.; Shihadeh, A.; Eissenberg, T. Effects of electronic cigarette heating coil resistance and liquid nicotine concentration on user nicotine delivery, heart rate, subjective effects, puff topography, and liquid consumption. Exp. Clin. Psychopharmacol. 2020, 28, 527–539. [Google Scholar] [CrossRef]
- Kosmider, L.; Spindle, T.R.; Gawron, M.; Sobczak, A.; Goniewicz, M.L. Nicotine emissions from electronic cigarettes: Individual and interactive effects of propylene glycol to vegetable glycerin composition and device power output. Food Chem. Toxicol. 2018, 115, 302–305. [Google Scholar] [CrossRef]
- Geiss, O.; Bianchi, I.; Barrero-Moreno, J. Correlation of volatile carbonyl yields emitted by e-cigarettes with the temperature of the heating coil and the perceived sensorial quality of the generated vapours. Int. J. Hyg. Envrion. Health 2016, 219, 268–277. [Google Scholar] [CrossRef]
- Uchiyama, S.; Noguchi, M.; Sato, A.; Ishitsuka, M.; Inaba, Y.; Kunugita, N. Determination of Thermal Decomposition Products Generated from E-Cigarettes. Chem. Res. Toxicol. 2020, 33, 576–583. [Google Scholar] [CrossRef]
- Gillman, I.G.; Kistler, K.A.; Stewart, E.W.; Paolantonio, A.R. Effect of variable power levels on the yield of total aerosol mass and formation of aldehydes in e-cigarette aerosols. Regul. Toxicol. Pharm. 2016, 75, 58–65. [Google Scholar] [CrossRef] [PubMed]
- Scott, A.; Lugg, S.T.; Aldridge, K.; Lewis, K.E.; Bowden, A.; Mahida, R.Y.; Grudzinska, F.S.; Dosanjh, D.; Parekh, D.; Foronjy, R.; et al. Pro-inflammatory effects of e-cigarette vapour condensate on human alveolar macrophages. Thorax 2018, 73, 1161–1169. [Google Scholar] [CrossRef] [PubMed]
- Corriden, R.; Moshensky, A.; Bojanowski, C.M.; Meier, A.; Chien, J.; Nelson, R.K.; Crotty Alexander, L.E. E-cigarette use increases susceptibility to bacterial infection by impairment of human neutrophil chemotaxis, phagocytosis, and NET formation. Am. J. Physiol. Cell Physiol. 2020, 318, C205–C214. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Arcos, I.; Geraghty, P.; Baumlin, N.; Campos, M.; Dabo, A.J.; Jundi, B.; Cummins, N.; Eden, E.; Grosche, A.; Salathe, M.; et al. Chronic electronic cigarette exposure in mice induces features of COPD in a nicotine-dependent manner. Thorax 2016, 71, 1119–1129. [Google Scholar] [CrossRef] [PubMed]
- Carson, J.L.; Zhou, L.; Brighton, L.; Mills, K.H.; Zhou, H.; Jaspers, I.; Hazucha, M. Temporal structure/function variation in cultured differentiated human nasal epithelium associated with acute single exposure to tobacco smoke or E-cigarette vapor. Inhal. Toxicol. 2017, 29, 137–144. [Google Scholar] [CrossRef]
- Higham, A.; Bostock, D.; Booth, G.; Dungwa, J.V.; Singh, D. The effect of electronic cigarette and tobacco smoke exposure on COPD bronchial epithelial cell inflammatory responses. Int. J. Chronic Obstr. Pulm. Dis. 2018, 13, 989–1000. [Google Scholar] [CrossRef]
- Shen, Y.; Wolkowicz, M.J.; Kotova, T.; Fan, L.; Timko, M.P. Transcriptome sequencing reveals e-cigarette vapor and mainstream-smoke from tobacco cigarettes activate different gene expression profiles in human bronchial epithelial cells. Sci. Rep. 2016, 6, 23984. [Google Scholar] [CrossRef]
- Nicholson, T.; Scott, A.; Newton Ede, M.; Jones, S.W. The impact of E-cigarette vaping and vapour constituents on bone health. J. Inflamm. 2021, 18, 16. [Google Scholar] [CrossRef]
- Nicholson, T.; Scott, A.; Newton Ede, M.; Jones, S.W. Do E-cigarettes and vaping have a lower risk of osteoporosis, nonunion, and infection than tobacco smoking? Bone Jt. Res. 2021, 10, 188–191. [Google Scholar] [CrossRef]
- ASH. Use of E-Cigarettes (Vapes) among Adults in Great Britain; Action on Smoking and Health: London, UK, 2021. [Google Scholar]
- Ghosh, A.; Coakley, R.D.; Ghio, A.J.; Muhlebach, M.S.; Esther, C.R., Jr.; Alexis, N.E.; Tarran, R. Chronic E-Cigarette Use Increases Neutrophil Elastase and Matrix Metalloprotease Levels in the Lung. Am. J. Respir. Crit. Care Med. 2019, 200, 1392–1401. [Google Scholar] [CrossRef]
- Braun, K.F.; Ehnert, S.; Freude, T.; Egaña, J.T.; Schenck, T.L.; Buchholz, A.; Schmitt, A.; Siebenlist, S.; Schyschka, L.; Neumaier, M.; et al. Quercetin protects primary human osteoblasts exposed to cigarette smoke through activation of the antioxidative enzymes HO-1 and SOD-1. Sci. World J. 2011, 11, 2348–2357. [Google Scholar] [CrossRef] [PubMed]
- Shaito, A.; Saliba, J.; Husari, A.; El-Harakeh, M.; Chhouri, H.; Hashem, Y.; Shihadeh, A.; El-Sabban, M. Electronic Cigarette Smoke Impairs Normal Mesenchymal Stem Cell Differentiation. Sci. Rep. 2017, 7, 14281. [Google Scholar] [CrossRef] [PubMed]
- Philp, A.M.; Collier, R.L.; Grover, L.M.; Davis, E.T.; Jones, S.W. Resistin promotes the abnormal Type I collagen phenotype of subchondral bone in obese patients with end stage hip osteoarthritis. Sci. Rep. 2017, 7, 4042. [Google Scholar] [CrossRef] [PubMed]
- Tonge, D.P.; Pearson, M.J.; Jones, S.W. The hallmarks of osteoarthritis and the potential to develop personalised disease-modifying pharmacological therapeutics. Osteoarthr. Cartil. 2014, 22, 609–621. [Google Scholar] [CrossRef] [PubMed]
- Newton Ede, M.M.; Jones, S.W. Adolescent idiopathic scoliosis: Evidence for intrinsic factors driving aetiology and progression. Int. Orthop. 2016, 40, 2075–2080. [Google Scholar] [CrossRef]
- Kallala, R.; Barrow, J.; Graham, S.M.; Kanakaris, N.; Giannoudis, P.V. The in vitro and in vivo effects of nicotine on bone, bone cells and fracture repair. Expert Opin. Drug Saf. 2013, 12, 209–233. [Google Scholar] [CrossRef]
- Samburova, V.; Bhattarai, C.; Strickland, M.; Darrow, L.; Angermann, J.; Son, Y.; Khlystov, A. Aldehydes in Exhaled Breath during E-Cigarette Vaping: Pilot Study Results. Toxics 2018, 6, 46. [Google Scholar] [CrossRef]
- Pereira, M.L.; Carvalho, J.C.; Peres, F.; Fernandes, M.H. Simultaneous effects of nicotine, acrolein, and acetaldehyde on osteogenic-induced bone marrow cells cultured on plasma-sprayed titanium implants. Int. J. Oral Maxillofac. Implant. 2010, 25, 112–122. [Google Scholar]
- Hoshi, H.; Hao, W.; Fujita, Y.; Funayama, A.; Miyauchi, Y.; Hashimoto, K.; Miyamoto, K.; Iwasaki, R.; Sato, Y.; Kobayashi, T.; et al. Aldehyde-stress resulting from Aldh2 mutation promotes osteoporosis due to impaired osteoblastogenesis. J. Bone Min. Res. 2012, 27, 2015–2023. [Google Scholar] [CrossRef]
- Mittal, M.; Pal, S.; China, S.P.; Porwal, K.; Dev, K.; Shrivastava, R.; Raju, K.S.; Rashid, M.; Trivedi, A.K.; Sanyal, S.; et al. Pharmacological activation of aldehyde dehydrogenase 2 promotes osteoblast differentiation via bone morphogenetic protein-2 and induces bone anabolic effect. Toxicol. Appl. Pharm. 2017, 316, 63–73. [Google Scholar] [CrossRef]
- Uchiyama, S.; Ohta, K.; Inaba, Y.; Kunugita, N. Determination of carbonyl compounds generated from the E-cigarette using coupled silica cartridges impregnated with hydroquinone and 2,4-dinitrophenylhydrazine, followed by high-performance liquid chromatography. Anal. Sci. 2013, 29, 1219–1222. [Google Scholar] [CrossRef] [PubMed]
- Goel, R.; Durand, E.; Trushin, N.; Prokopczyk, B.; Foulds, J.; Elias, R.J.; Richie, J.P., Jr. Highly reactive free radicals in electronic cigarette aerosols. Chem. Res. Toxicol. 2015, 28, 1675–1677. [Google Scholar] [CrossRef] [PubMed]
- Domazetovic, V.; Marcucci, G.; Iantomasi, T.; Brandi, M.L.; Vincenzini, M.T. Oxidative stress in bone remodeling: Role of antioxidants. Clin. Cases Min. Bone Metab. 2017, 14, 209–216. [Google Scholar] [CrossRef] [PubMed]
- Mody, N.; Parhami, F.; Sarafian, T.A.; Demer, L.L. Oxidative stress modulates osteoblastic differentiation of vascular and bone cells. Free Radic. Biol. Med. 2001, 31, 509–519. [Google Scholar] [CrossRef]
- Bai, X.C.; Lu, D.; Bai, J.; Zheng, H.; Ke, Z.Y.; Li, X.M.; Luo, S.Q. Oxidative stress inhibits osteoblastic differentiation of bone cells by ERK and NF-kappaB. Biochem. Biophys. Res. Commun. 2004, 314, 197–207. [Google Scholar] [CrossRef]
- Bai, X.C.; Lu, D.; Liu, A.L.; Zhang, Z.M.; Li, X.M.; Zou, Z.P.; Zeng, W.S.; Cheng, B.L.; Luo, S.Q. Reactive oxygen species stimulates receptor activator of NF-kappaB ligand expression in osteoblast. J. Biol. Chem. 2005, 280, 17497–17506. [Google Scholar] [CrossRef]
- Ezeriņa, D.; Takano, Y.; Hanaoka, K.; Urano, Y.; Dick, T.P. N-Acetyl Cysteine Functions as a Fast-Acting Antioxidant by Triggering Intracellular H(2)S and Sulfane Sulfur Production. Cell Chem. Biol. 2018, 25, 447–459.e444. [Google Scholar] [CrossRef]
- Beklen, A.; Uckan, D. Electronic cigarette liquid substances propylene glycol and vegetable glycerin induce an inflammatory response in gingival epithelial cells. Hum. Exp. Toxicol. 2021, 40, 25–34. [Google Scholar] [CrossRef]
- Woodall, M.; Jacob, J.; Kalsi, K.K.; Schroeder, V.; Davis, E.; Kenyon, B.; Khan, I.; Garnett, J.P.; Tarran, R.; Baines, D.L. E-cigarette constituents propylene glycol and vegetable glycerin decrease glucose uptake and its metabolism in airway epithelial cells in vitro. Am. J. Physiol. Cell Mol. Physiol. 2020, 319, L957–L967. [Google Scholar] [CrossRef]
- Reumann, M.K.; Schaefer, J.; Titz, B.; Aspera-Werz, R.H.; Wong, E.T.; Szostak, J.; Häussling, V.; Ehnert, S.; Leroy, P.; Tan, W.T.; et al. E-vapor aerosols do not compromise bone integrity relative to cigarette smoke after 6-month inhalation in an ApoE(-/-) mouse model. Arch. Toxicol. 2020, 94, 2163–2177. [Google Scholar] [CrossRef]
- Lin, V.Y.; Fain, M.D.; Jackson, P.L.; Berryhill, T.F.; Wilson, L.S.; Mazur, M.; Barnes, S.J.; Blalock, J.E.; Raju, S.V.; Rowe, S.M. Vaporized E-Cigarette Liquids Induce Ion Transport Dysfunction in Airway Epithelia. Am. J. Respir. Cell Mol. Biol. 2019, 61, 162–173. [Google Scholar] [CrossRef] [PubMed]
- Lappin, D.F.; Sherrabeh, S.; Jenkins, W.M.; Macpherson, L.M. Effect of smoking on serum RANKL and OPG in sex, age and clinically matched supportive-therapy periodontitis patients. J. Clin. Periodontol. 2007, 34, 271–277. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.W.; Park, S.H.; Weng, M.W.; Wang, H.T.; Huang, W.C.; Lepor, H.; Wu, X.R.; Chen, L.C.; Tang, M.S. E-cigarette smoke damages DNA and reduces repair activity in mouse lung, heart, and bladder as well as in human lung and bladder cells. Proc. Natl. Acad. Sci. USA 2018, 115, E1560–E1569. [Google Scholar] [CrossRef] [PubMed]
- Tang, M.S.; Wang, H.T.; Hu, Y.; Chen, W.S.; Akao, M.; Feng, Z.; Hu, W. Acrolein induced DNA damage, mutagenicity and effect on DNA repair. Mol. Nutr. Food Res. 2011, 55, 1291–1300. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Balbo, S.; Villalta, P.W.; Hecht, S.S. Analysis of Acrolein-Derived 1, N(2)-Propanodeoxyguanosine Adducts in Human Lung DNA from Smokers and Nonsmokers. Chem. Res. Toxicol. 2019, 32, 318–325. [Google Scholar] [CrossRef]
- Cheng, G.; Guo, J.; Carmella, S.G.; Lindgren, B.; Ikuemonisan, J.; Niesen, B.; Jensen, J.; Hatsukami, D.K.; Balbo, S.; Hecht, S.S. Increased acrolein-DNA adducts in buccal brushings of e-cigarette users. Carcinogenesis 2022, 43, 437–444. [Google Scholar] [CrossRef]
- Chen, Q.; Liu, K.; Robinson, A.R.; Clauson, C.L.; Blair, H.C.; Robbins, P.D.; Niedernhofer, L.J.; Ouyang, H. DNA damage drives accelerated bone aging via an NF-κB-dependent mechanism. J. Bone Min. Res. 2013, 28, 1214–1228. [Google Scholar] [CrossRef]
- Russell, M.A.; Wilson, C.; Patel, U.A.; Feyerabend, C.; Cole, P.V. Plasma nicotine levels after smoking cigarettes with high, medium, and low nicotine yields. Br. Med. J. 1975, 2, 414–416. [Google Scholar] [CrossRef][Green Version]


| 2nd Generation Device | 3rd Generation Device | Humectants | ||||
|---|---|---|---|---|---|---|
| ECVC | nfECVC | ECVC | nfECVC | PG | VG | |
| Dose to significantly reduce osteoblast viability (24 h) | 2.5% | 10% | 1% | 2.5% | Significant treatment effect 0.5–10% | No significant effect |
| Dose to significantly reduce osteoblast OPG secretion (24 h) | 0.5% | - | 0.5% | - | - | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nicholson, T.; Davis, L.; Davis, E.T.; Newton Ede, M.; Scott, A.; Jones, S.W. e-Cigarette Vapour Condensate Reduces Viability and Impairs Function of Human Osteoblasts, in Part, via a Nicotine Dependent Mechanism. Toxics 2022, 10, 506. https://doi.org/10.3390/toxics10090506
Nicholson T, Davis L, Davis ET, Newton Ede M, Scott A, Jones SW. e-Cigarette Vapour Condensate Reduces Viability and Impairs Function of Human Osteoblasts, in Part, via a Nicotine Dependent Mechanism. Toxics. 2022; 10(9):506. https://doi.org/10.3390/toxics10090506
Chicago/Turabian StyleNicholson, Thomas, Lauren Davis, Edward T. Davis, Matthew Newton Ede, Aaron Scott, and Simon W. Jones. 2022. "e-Cigarette Vapour Condensate Reduces Viability and Impairs Function of Human Osteoblasts, in Part, via a Nicotine Dependent Mechanism" Toxics 10, no. 9: 506. https://doi.org/10.3390/toxics10090506
APA StyleNicholson, T., Davis, L., Davis, E. T., Newton Ede, M., Scott, A., & Jones, S. W. (2022). e-Cigarette Vapour Condensate Reduces Viability and Impairs Function of Human Osteoblasts, in Part, via a Nicotine Dependent Mechanism. Toxics, 10(9), 506. https://doi.org/10.3390/toxics10090506








