Multi-Objective Technology-Based Approach to Home Healthcare Routing Problem Considering Sustainability Aspects
Abstract
1. Introduction
2. Literature Review
2.1. Home Healthcare Vehicle Routing
2.2. Quality of Service in Vehicle Routing
2.3. Smart Vehicle Routing
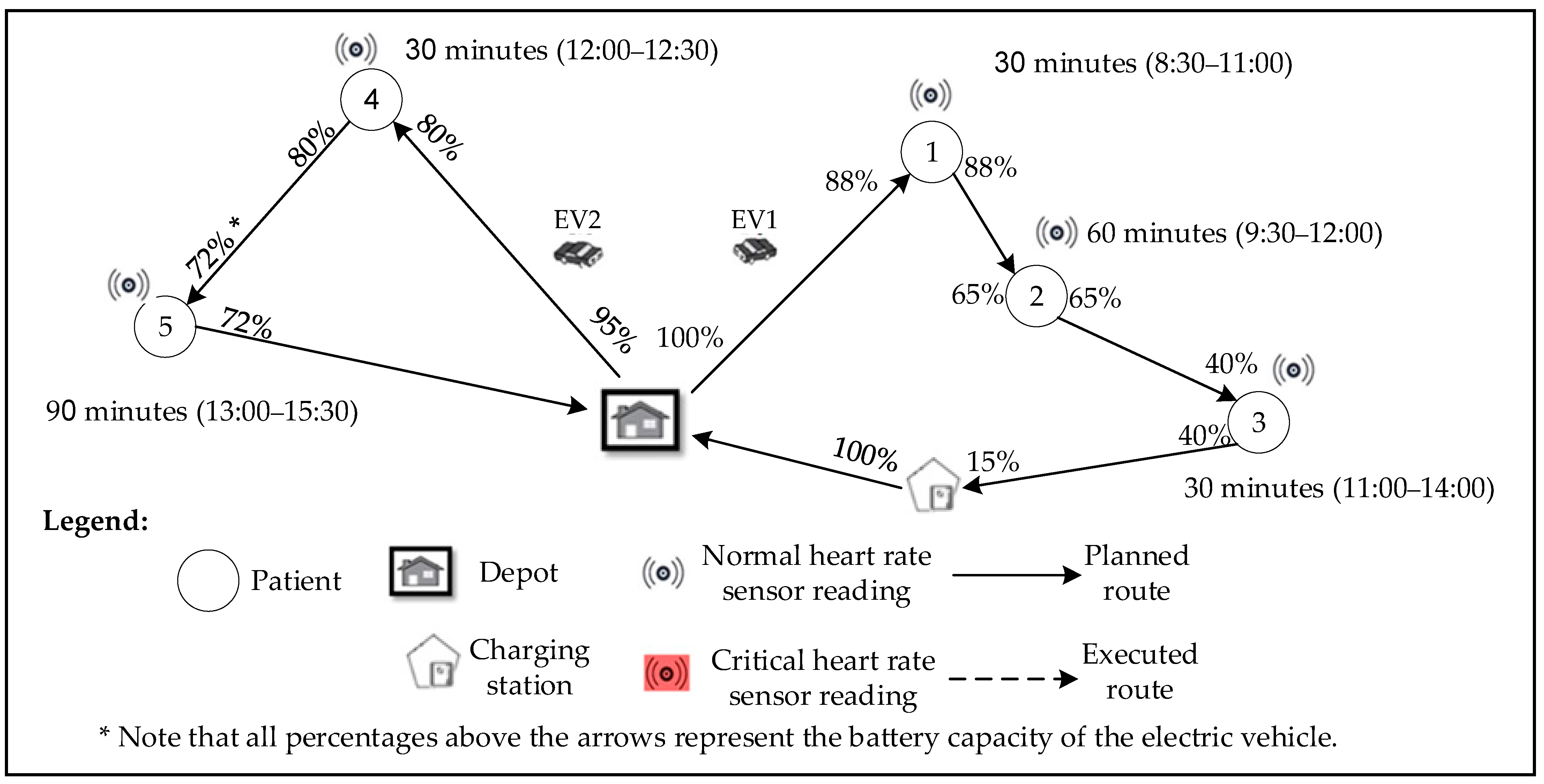
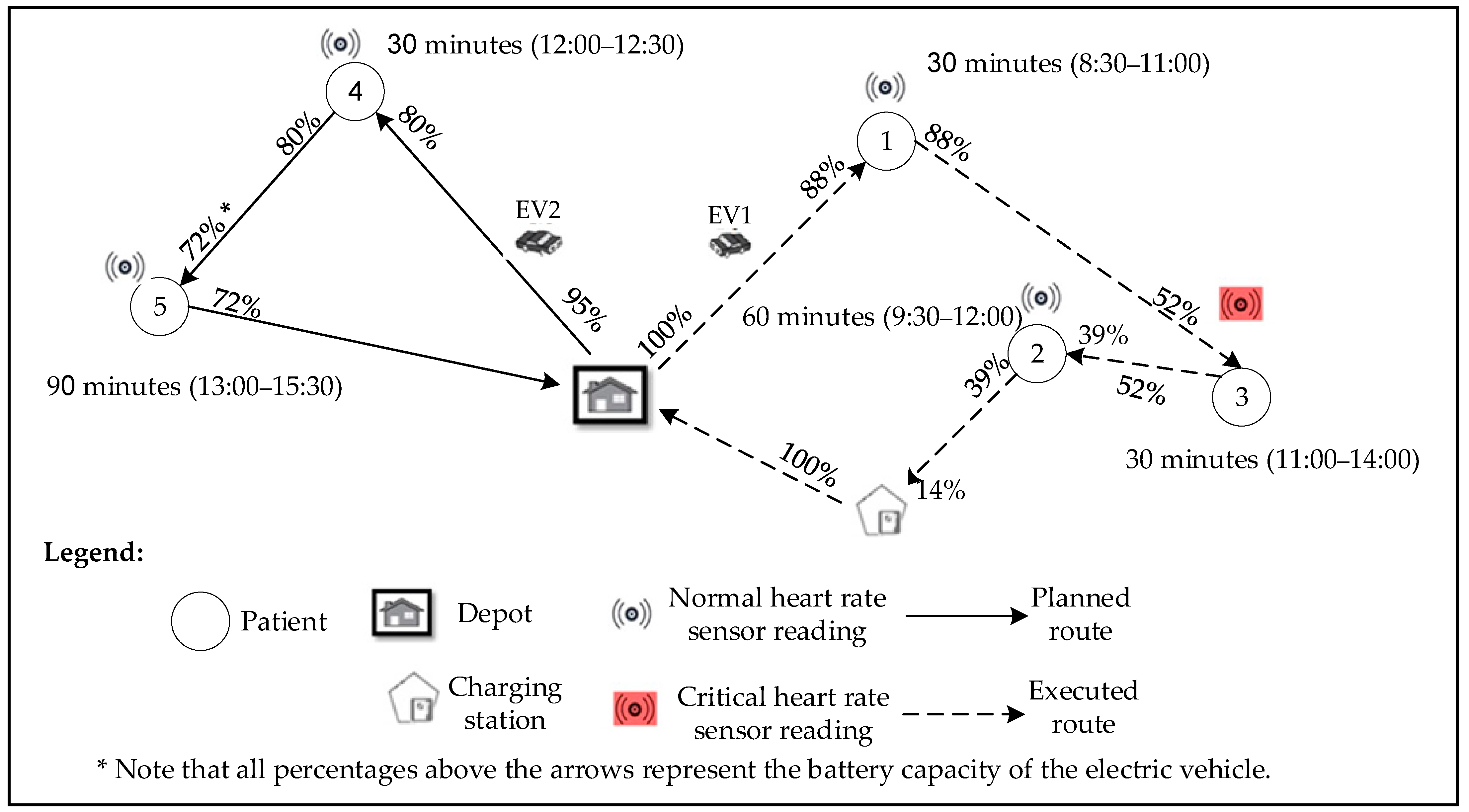
3. Problem Presentation
3.1. Mathematical Modeling
3.1.1. Model Assumptions
- Single depot (starting point) and multi-destination points (patients to be served);
- The patients to be served are assumed to have cardiovascular conditions, such as patients recovering from heart diseases or patients with chronic heart conditions;
- A caregiver must visit all patients;
- Normal patients are assumed to have a heart rate between 60 and 100 beats per minute (BPM), whereas heart beats below 60 BPM and above 100 BPM classify a patient as under critical conditions [45];
- There are variations in the distances between the same pair of nodes when driving on different kinds of routes;
- The limited battery capacity of the electric vehicle is assumed to illustrate real-world scenarios where different EVs have different batteries and can be used under various driving conditions. This assumption will ensure the generalizability and robustness of the mathematical model.
- The electric vehicle must visit a charging station if battery capacity falls below 50%;
- The location of charging stations is assumed to be fixed;
- Electric vehicle battery capacity should be 100% charged after visiting a charging station;
- Electric vehicle energy consumption differs from one route to another and was classified according to Hosseini-Nasab and Lotfalian (2017) [44] as follows:
- Route 1: 0.14 (kWh/km);
- Route 2: 0.12 (kWh/km);
- Route 3: 0.10 (kWh/km);
- Route 4: 0.13 (kWh/km).
- The degree of patient importance (priority) is based on the complexity of their medical condition, needed care, and how they are affected by time of service, i.e., time of medication and needed checkups.
3.1.2. Sets and Indices
| N | Set of a source or destination node; |
| S | Set of recharging stations; |
| S′ | Set of dummy recharging stations to allow multiple visits; |
| P | Set of a patient under normal conditions; |
| C | Set of a patient under critical conditions; |
| M | Set of measures of quality of service; |
| i | ); |
| j | ); |
| j′ | ); |
| r | Index of type of route (r = 1,2,3,4); |
| h | ); |
| d | ); |
| t | ); |
| k | ); |
| q | ); |
| , β | , β). |
3.1.3. Model Parameters
| Parameter | Description |
| normalized work time on day d; | |
| costs associated with the caregiver h’s workload deviation from the normalized value on day d; | |
| maximum working time in a single day for caregiver h on day d; | |
| E | heart rate sensor reading for patients; |
| velocity of travel between node i and node j along route r (Km/hr); | |
| the upper speed limit allowed on route r (Km/hr); | |
| earliest arrival time within a time window of service at patient node i; | |
| latest arrival time within a time window of service at patient node i; | |
| the duration of service time at patient node i; | |
| the desired time of service at patient node i; | |
| waiting time at patient node i; | |
| importance degree of a patient at node i based on medical status and needed service; | |
| total travel time of vehicle k; | |
| A | sufficiently large positive number; |
| constant for violating the hard time windows; | |
| travel time from node i to node j along route r (i, j); | |
| travel distance from node i to node j along route r (i, j); | |
| recharging rate of electric vehicle k; | |
| the battery capacity of electric vehicle k; | |
| the consumption rate of electric vehicles k; | |
| the normalized relationship between the qth service quality dimension and the αth internal measure of service; | |
| the dependencies and correlation between internal measures where α and β M; | |
| the relationship between the qth service quality dimension and the βth internal measure of service; | |
| the cost (USD) of poor quality of service for the qth dimension of service quality; | |
| predefined target weight for objective function Zi, set by decision makers; | |
| summation of all objective functions with their weights. |
3.1.4. Decision Variables
| =1, if a caregiver travels from i to j through route r serving patient p under normal conditions; =0, otherwise; | |
| =1, if a caregiver travels from i to j′ through route r serving patient c under critical conditions; =0, otherwise; | |
| HR | =1 if the heart rate of a patient is within critical range; =0, otherwise; |
| battery state of an electric vehicle k K, at node i; | |
| battery state of an electric vehicle k K after visiting a charging station; | |
| the total workload of caregiver h on day d; | |
| electric vehicle k charging duration; | |
| the expected level of patient satisfaction from the qth dimension of service quality; | |
| the perceived level of patients’ satisfaction from the qth dimension of service quality; | |
| the level of fulfillment of the αth internal measure; | |
| membership function of patient node i; | |
| control variable for each patient at node i; | |
| actual arrival time at patient node i; | |
| start time of service at patient node i. |
3.1.5. Defining Equations
3.1.6. Objective Functions
3.1.7. Constraints
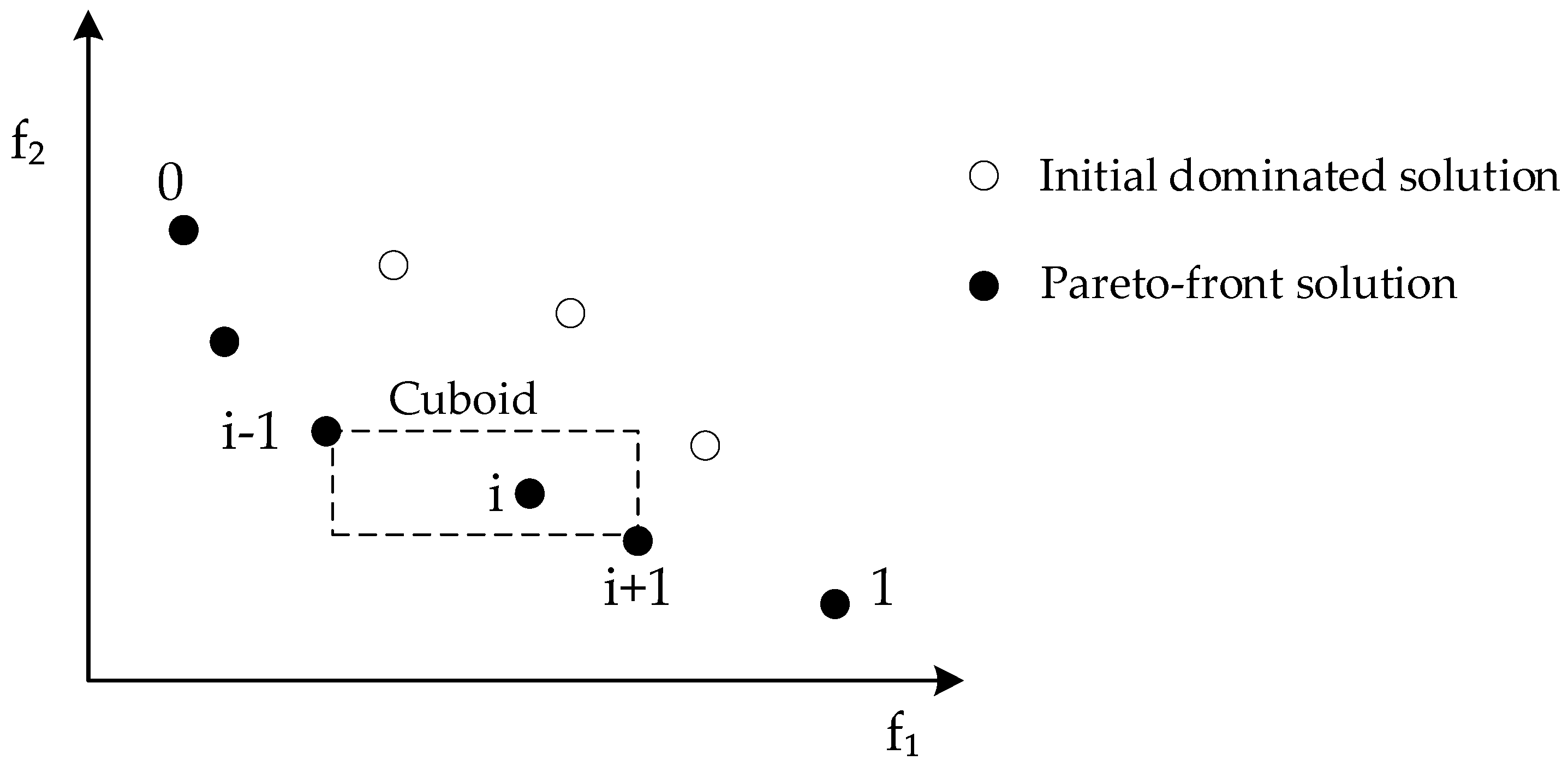
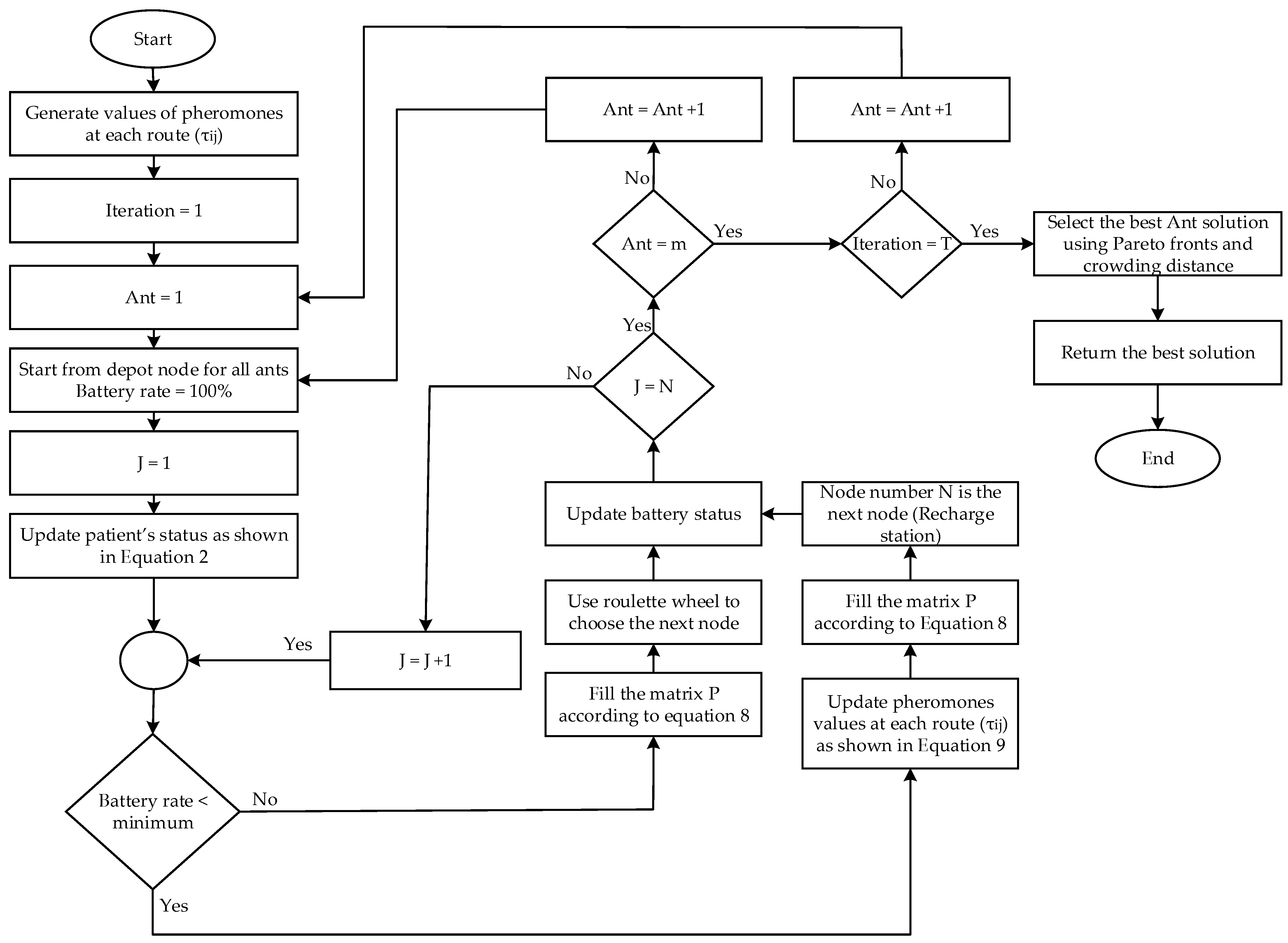
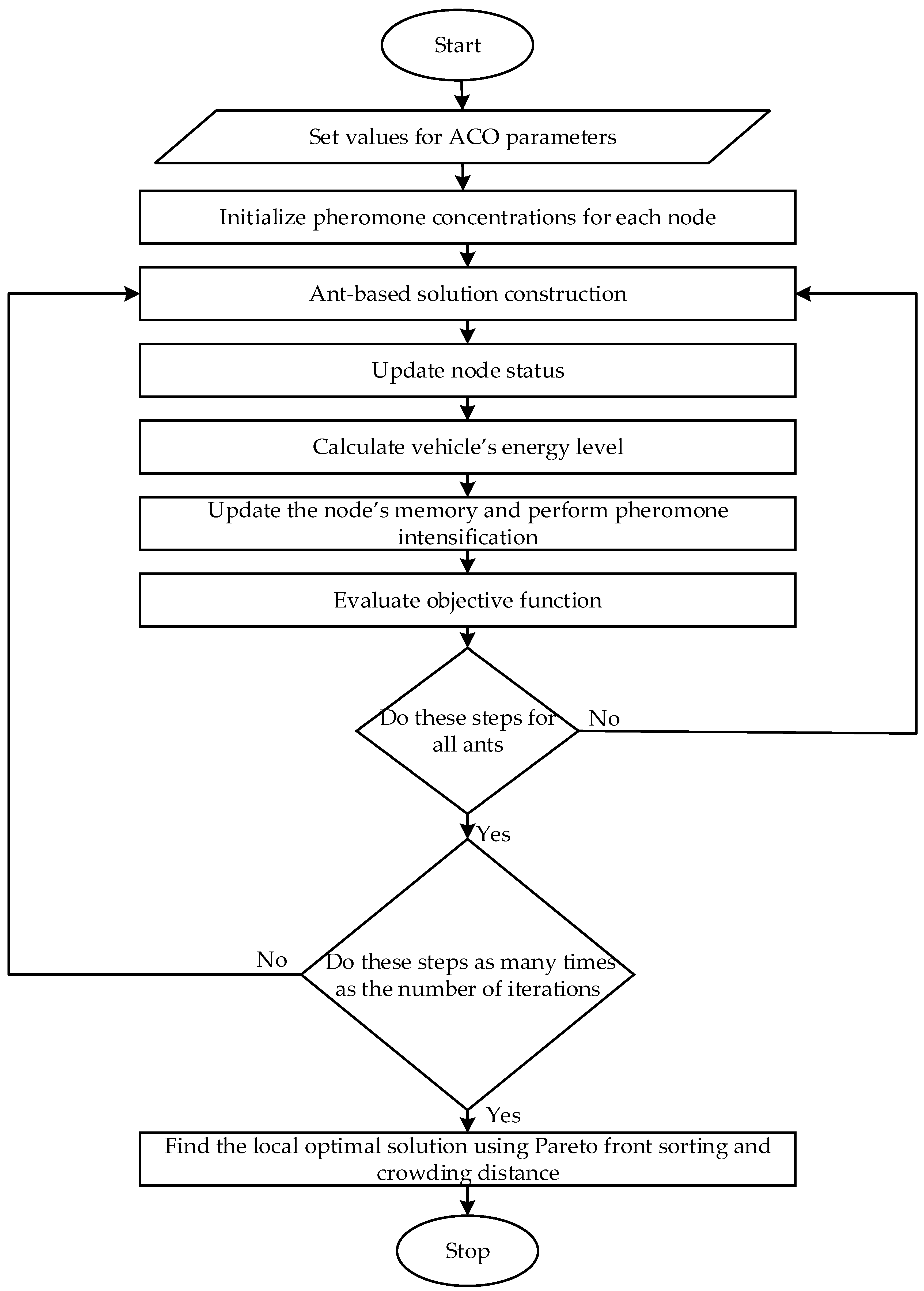
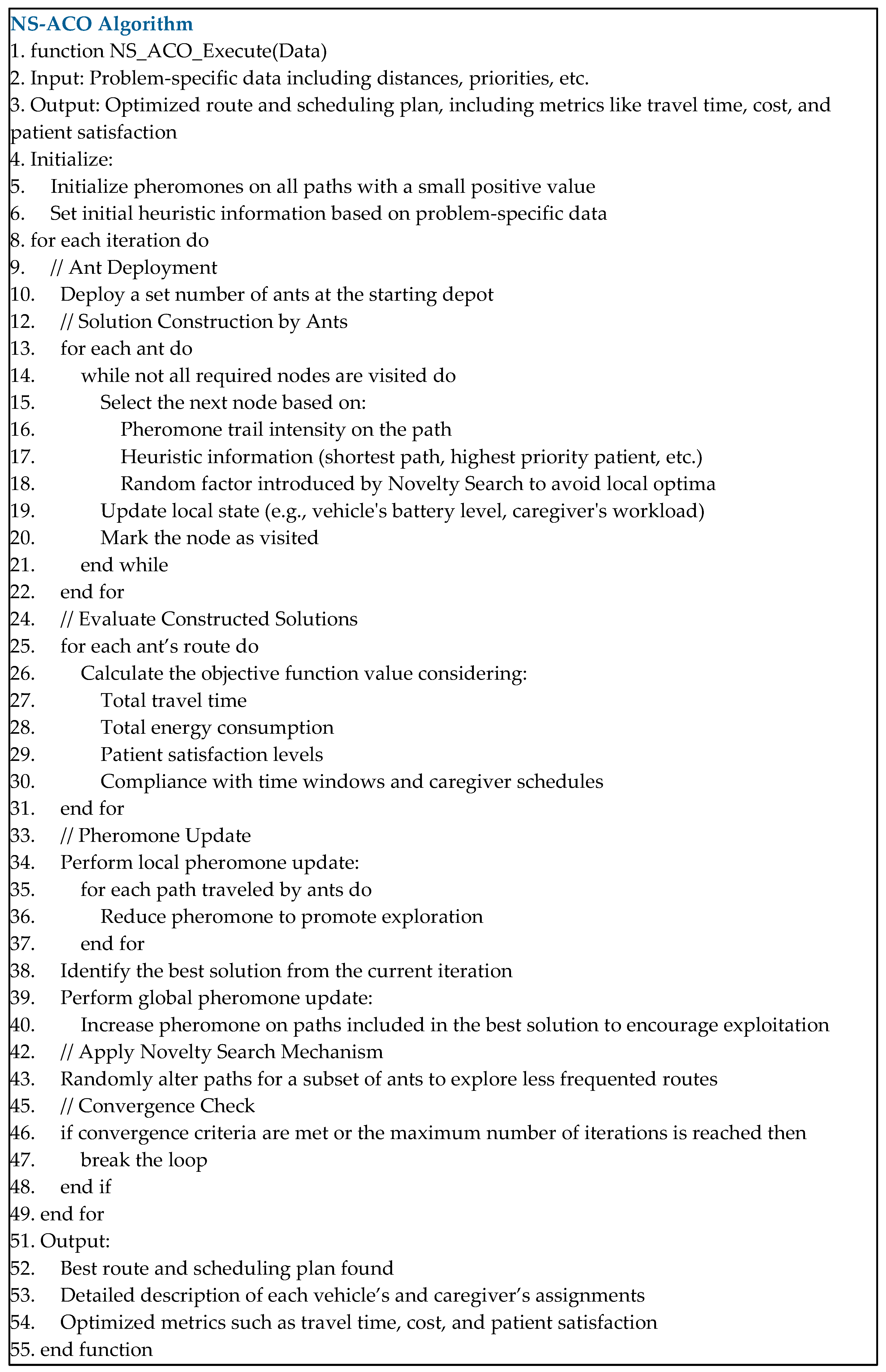
3.2. Solution Methodology
4. Model Results
4.1. Numerical Data
4.2. Numerical Results
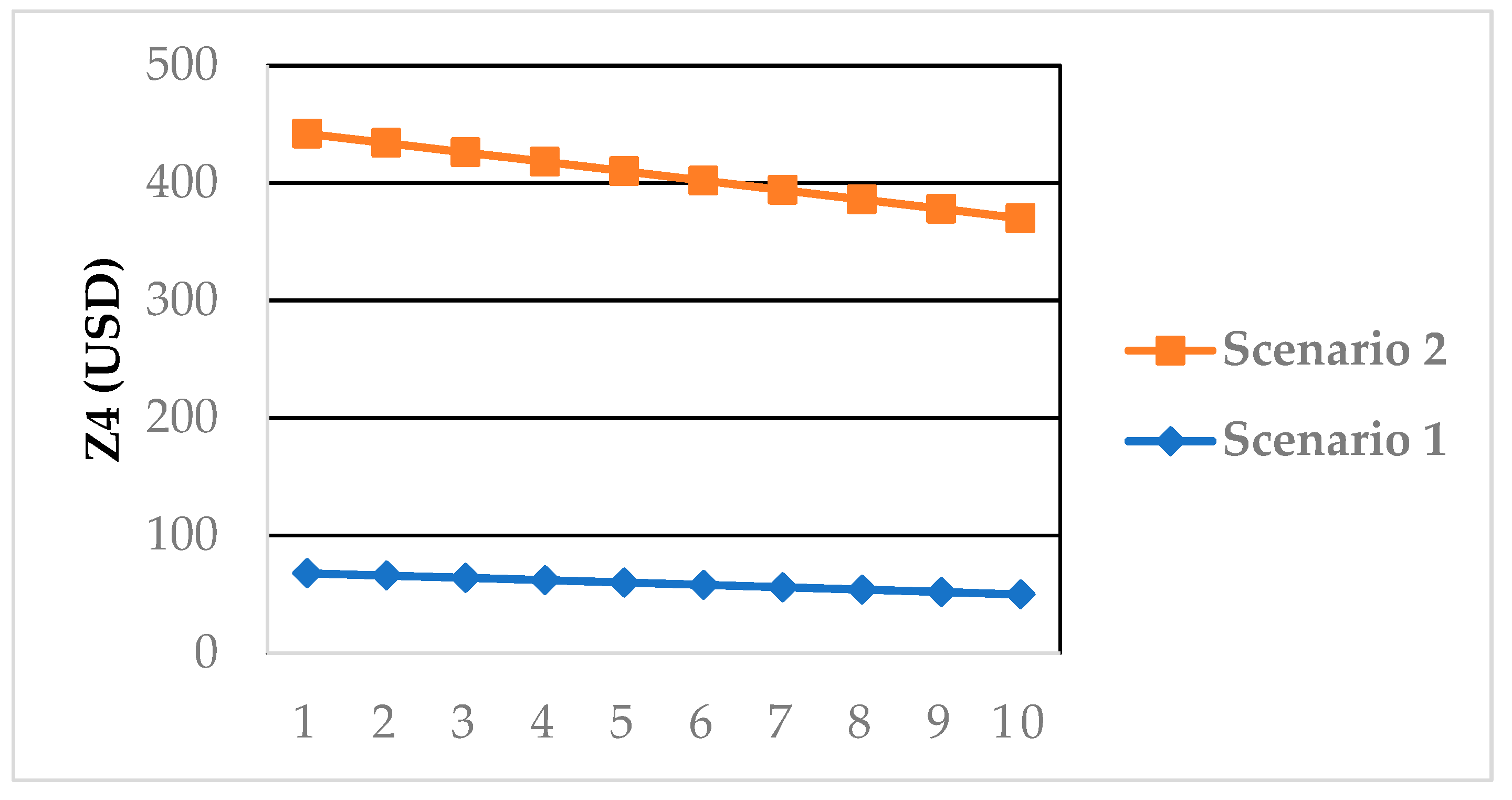
5. Sensitivity Analysis
5.1. The Effect of Using Heart Rate Sensor
5.2. The Effect of Different Patient’s Priority Levels on Quality Costs
6. Managerial Insights
7. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Alves, F.; Costa, L.A.; Rocha, A.M.A.C.; Pereira, A.I.; Leitão, P. The Sustainable Home Health Care Process Based on Multi-Criteria Decision-Support. Mathematics 2023, 11, 6. [Google Scholar] [CrossRef]
- Oliveira, C.; Pereira, J.; Santos, E.; Lima, T.M.; Gaspar, P.D. Optimization of the COVID-19 vaccine distribution route using the vehicle routing problem with time windows model and capacity constraint. Appl. Syst. Innov. 2023, 6, 17. [Google Scholar] [CrossRef]
- Erdem, M.; Koç, Ç. Analysis of electric vehicles in home health care routing problem. J. Clean. Prod. 2019, 234, 1471–1483. [Google Scholar] [CrossRef]
- Fathollahi-Fard, A.M.; Hajiaghaei-Keshteli, M.; Tavakkoli-Moghaddam, R. A bi-objective green home health care routing problem. J. Clean. Prod. 2018, 200, 423–443. [Google Scholar] [CrossRef]
- Shi, Y.; Boudouh, T.; Grunder, O. A hybrid genetic algorithm for a home health care routing problem with time window and fuzzy demand. Expert Syst. Appl. 2017, 72, 160–176. [Google Scholar] [CrossRef]
- Fathollahi-Fard, A.M.; Govindan, K.; Hajiaghaei-Keshteli, M.; Ahmadi, A. A green home health care supply chain: New modified simulated annealing algorithms. J. Clean. Prod. 2019, 240, 118200. [Google Scholar] [CrossRef]
- Zhang, S.; Lee, C.K.M.; Choy, K.L.; Ho, W.; Ip, W.H. Design and development of a hybrid artificial bee colony algorithm for the environmental vehicle routing problem. Transp. Res. Part D Transp. Environ. 2014, 31, 85–99. [Google Scholar] [CrossRef]
- Gandhi, V.; Singh, J. An automated review of body sensor networks research patterns and trends. J. Ind. Inf. Integr. 2020, 18, 100132. [Google Scholar] [CrossRef]
- Bouleft, Y.; Elhilali Alaoui, A. Dynamic Multi-Compartment Vehicle Routing Problem for Smart Waste Collection. Appl. Syst. Innov. 2023, 6, 30. [Google Scholar] [CrossRef]
- Rout, R.R.; Vemireddy, S.; Raul, S.K.; Somayajulu, D.V.L.N. Fuzzy logic-based emergency vehicle routing: An IoT system development for smart city applications. Comput. Electr. Eng. 2020, 88, 106839. [Google Scholar] [CrossRef]
- Elkington, J. Cannibals with Forks: The Triple Bottom Line of 21st-Century Business; New Society Publishers: Gabriola Island, BC, Canada, 1998. [Google Scholar]
- Moghdani, R.; Salimifad, K.; Demir, E.; Benyettou, A. The green vehicle routing problem: A systematic literature review. J. Clean. Prod. 2021, 279, 123691. [Google Scholar] [CrossRef]
- Secundo, G.; Shams, S.M.R.; Nucci, F. Digital technologies and collective intelligence for healthcare ecosystem: Optimizing Internet of Things adoption for pandemic management. J. Bus. Res. 2021, 131, 563–572. [Google Scholar] [CrossRef] [PubMed]
- WCED. Report of the World Commission on Environment and Development: Our Common Future; WCED: Cape Town, South Africa, 1987. [Google Scholar]
- Vega-Mejía, C.A.; Montoya-Torres, J.R.; Islam, S.M.N. Consideration of triple bottom line objectives for sustainability in the optimization of vehicle routing and loading operations: A systematic literature review. Ann. Oper. Res. 2019, 273, 311–375. [Google Scholar] [CrossRef]
- Lin, C.; Choy, K.L.; Ho, G.T.S.; Chung, S.H.; Lam, H.Y. Survey of green vehicle routing problem: Past and future trends. Expert Syst. Appl. 2014, 41, 1118–1138. [Google Scholar] [CrossRef]
- Eslamipoor, R. A fuzzy multi-objective model for supplier selection to mitigate the impact of vehicle transportation gases and delivery time. J. Data Inf. Manag. 2022, 4, 231–241. [Google Scholar] [CrossRef]
- Bhinge, R.; Moser, R.; Moser, E.; Lanza, G.; Dornfeld, D. Sustainability optimization for global supply chain decision-making. Procedia CIRP 2015, 26, 323–328. [Google Scholar] [CrossRef]
- Seuring, S. A review of modeling approaches for sustainable supply chain management. Decis. Support Syst. 2013, 54, 1513–1520. [Google Scholar] [CrossRef]
- Yang, B.; Hu, Z.H.; Wei, C.; Li, S.Q.; Zhao, L.; Jia, S. Routing with time-windows for multiple environmental vehicle types. Comput. Ind. Eng. 2015, 89, 150–161. [Google Scholar] [CrossRef]
- Yan, T.; Lu, F.; Wang, S.; Wang, L.; Bi, H. A hybrid metaheuristic algorithm for the multi-objective location-routing problem in the early post-disaster stage. J. Ind. Manag. Optim. 2023, 19, 4663–4691. [Google Scholar] [CrossRef]
- Wang, X.; Fan, T.; Chen, M.; Deng, B.; Wu, B.; Tremont, P. Safety modeling of urban arterials in Shanghai, China. Accid. Anal. Prev. 2015, 83, 57–66. [Google Scholar] [CrossRef]
- Matl, P.; Hartl, R.F.; Vidal, T. Workload equity in vehicle routing problems: A survey and analysis. Transport. Sci. 2018, 52, 239–260. [Google Scholar] [CrossRef]
- Habibnejad-Ledari, H.; Rabbani, M.; Ghorbani-Kutenaie, N. Solving a multi-objective model toward home care staff planning considering cross-training and staff preferences by NSGA-II and NRGA. Sci. Iran. 2019, 26, 2919–2935. [Google Scholar] [CrossRef]
- Fernandez, A.; Gregory, G.; Hindle, A.; Lee, A.C. A Model for community nursing in a rural country. Oper. Res. Quart. 1974, 25, 231–239. [Google Scholar] [CrossRef]
- Ait Haddadene, S.R.; Labadie, N.; Prodhon, C. Bicriteria vehicle routing problem with preferences and timing constraints in home health care services. Algorithms 2019, 12, 152. [Google Scholar] [CrossRef]
- Fikar, C.; Hirsch, P. Home health care routing and scheduling: A review. Comput. Oper. Res. 2017, 77, 86–95. [Google Scholar] [CrossRef]
- Rest, K.D.; Hirsch, P. Daily scheduling of home health care services using time-dependent public transport. Flex. Serv. Manuf. J. 2016, 28, 495–525. [Google Scholar] [CrossRef]
- Shi, Y.; Boudouh, T.; Grunder, O. A robust optimization for a home health care routing and scheduling problem with consideration of uncertain travel and service times. Trasnport. Res. E-Log. 2019, 128, 52–95. [Google Scholar] [CrossRef]
- Doulabi, H.H.; Pesant, G.; Rousseau, L.M. Vehicle routing problems with synchronized visits and stochastic travel and service times: Applications in healthcare. Transport. Sci. 2020, 54, 1053–1072. [Google Scholar] [CrossRef]
- Hiermann, G.; Prandtstetter, M.; Rendl, A.; Puchinger, J.; Raidl, G.R. Metaheuristics for solving a multimodal home-healthcare scheduling problem. Cent. Eur. J. Oper. Res. 2015, 23, 89–113. [Google Scholar] [CrossRef]
- Expósito, A.; Brito, J.; Moreno, J.A.; Expósito-Izquierdo, C. Quality of service objectives for vehicle routing problem with time windows. Appl. Soft. Comput. 2019, 84, 105707. [Google Scholar] [CrossRef]
- Yang, Z.; Emmerich, M.; Bäck, T. Ant based solver for dynamic vehicle routing problem with time windows and multiple priorities. In Proceedings of the 2015 IEEE Congress on Evolutionary Computation (CEC), Sendai, Japan, 25–28 May 2015; pp. 2813–2819. [Google Scholar]
- Orlis, C.; Laganá, D.; Dullaert, W.; Vigo, D. Distribution with quality-of-service considerations: The capacitated routing problem with profits and service level requirements. Omega 2020, 93, 102034. [Google Scholar] [CrossRef]
- Khorshidi, H.A.; Hejazi, S.R. Optimising service quality translating via quantitative quality function deployment. Int. J. Serv. Stand. 2011, 7, 169–180. [Google Scholar] [CrossRef]
- Ghannadpour, S.F.; Zarrabi, A. Multi-objective heterogeneous vehicle routing and scheduling problem with energy minimizing. Swarm. Evol. Comput. 2019, 44, 728–747. [Google Scholar] [CrossRef]
- Albino, V.; Berardi, U.; Dangelico, R.M. Smart cities: Definitions, dimensions, performance, and initiatives. J. Urban Technol. 2015, 22, 3–21. [Google Scholar] [CrossRef]
- Mamun, M.A.A.; Hannan, M.A.; Hussain, A.; Basri, H. Theoretical model and implementation of a real time intelligent bin status monitoring system using rule-based decision algorithms. Expert Syst. Appl. 2016, 48, 76–88. [Google Scholar] [CrossRef]
- Hannan, M.A.; Akhtar, M.; Begum, R.A.; Basri, H.; Hussain, A.; Scavino, E. Capacitated vehicle-routing problem model for scheduled solid waste collection and route optimization using PSO algorithm. Waste Manag. 2018, 71, 31–41. [Google Scholar] [CrossRef] [PubMed]
- Ramos, T.R.P.; de Morais, C.S.; Barbosa-Póvoa, A.P. The smart waste collection routing problem: Alternative operational management approaches. Expert Syst. Appl. 2018, 103, 146–158. [Google Scholar] [CrossRef]
- Ding, Y.; Jin, M.; Li, S.; Feng, D. Smart logistics based on the internet of things technology: An overview. Int. J. Logist-Res. App. 2020, 24, 323–345. [Google Scholar] [CrossRef]
- Lai, X.; Liu, Q.; Wei, X.; Wang, W.; Zhou, G.; Han, G. A survey of body sensor networks. Sensors 2013, 13, 5406–5447. [Google Scholar] [CrossRef]
- Gope, P.; Hwang, T. BSN-Care: A secure IoT-based modern healthcare system using body sensor network. IEEE Sens. J. 2015, 16, 1368–1376. [Google Scholar] [CrossRef]
- Hosseini-Nasab, H.; Lotfalian, P. Green routing for trucking systems with classification of path types. J. Clean. Prod. 2017, 146, 228–233. [Google Scholar] [CrossRef]
- Avram, R.; Tison, G.H.; Aschbacher, K.; Kuhar, P.; Vittinghoff, E.; Butzner, M.; Runge, R.; Wu, N.; Pletcher, M.J.; Marcus, G.M.; et al. Real-world heart rate norms in the Health eHeart study. NPJ Digit. Med. 2019, 2, 58. [Google Scholar] [CrossRef]
- Lu, F.; Chen, W.; Feng, W.; Bi, H. 4PL Routing Problem Using Hybrid Beetle Swarm Optimization. Soft Comput. 2023, 27, 17011–17024. [Google Scholar] [CrossRef]
- Lu, F.; Feng, W.; Gao, M.; Bi, H.; Wang, S. The Fourth-Party Logistics Routing Problem Using Ant Colony System-Improved Grey Wolf Optimization. J. Adv. Transp. 2020, 2020, e8831746. [Google Scholar] [CrossRef]
- Dorigo, M.; Di Caro, G. The Ant Colony Optimization meta-heuristic, In New Ideas in Optimization; Corne, D., Dorigo, M., Glover, F., Dasgupta, D., Moscato, P., Poli, R., Price, K.V., Eds.; McGraw Hill: London, UK, 1999; pp. 11–32. [Google Scholar]
- Rader, D.J. Deterministic Operations Research: Models and Methods in Linear Optimization; John Wiley & Sons: Hoboken, NJ, USA, 2010. [Google Scholar]
- Deb, K.; Agrawal, S.; Pratap, A.; Meyarivan, T. A fast elitist non-dominated sorting genetic algorithm for multi-objective optimization: NSGA-II. In Parallel Problem Solving from Nature PPSN VI; Schoenauer, M., Deb, K., Rudolph, G., Yao, X., Lutton, E., Merelo, J.J., Schwefel, H.-P., Eds.; Springer: Berlin/Heidelberg, Germany, 2000; pp. 849–858. [Google Scholar] [CrossRef]
- Statista Research Department. Predicted Average Battery Capacities in EVs Worldwide 2017–2025. 2018. Available online: https://www.statista.com/statistics/309584/battery-capacity-estimates-for-electric-vehicles-worldwide/. (accessed on 10 December 2022).
- Younes, Z.; Boudet, L.; Suard, F.; Gérard, M.; Rioux, R. Analysis of the Main Factors Influencing the Energy Consumption of Electric Vehicles. In Proceedings of the 2013 International Electric Machines & Drives Conference, Chicago, IL, USA, 12–15 May 2013; pp. 247–253. [Google Scholar] [CrossRef]
- Kostopoulos, E.D.; Spyropoulos, G.C.; Kaldellis, J.K. Real-world study for the optimal charging of electric vehicles. Energy Rep. 2020, 6, 418–426. [Google Scholar] [CrossRef]
- Izu, L.; Scholtz, B.; Fashoro, I. Wearables and Their Potential to Transform Health Management: A Step towards Sustainable Development Goal 3. Sustainability 2024, 16, 1850. [Google Scholar] [CrossRef]
- Canali, S.; Schiaffonati, V.; Aliverti, A. Challenges and recommendations for wearable devices in digital health: Data quality, interoperability, health equity, fairness. PLOS Digit. Health 2022, 1, e0000104. [Google Scholar] [CrossRef]
- Nizetic, S.; Solic, P.; Gonzalez-de-Artaza, D.L.; Patrono, L. Internet of Things (IoT): Opportunities, issues and challenges towards a smart and sustainable future. J. Clean. Prod. 2020, 274, 122877. [Google Scholar] [CrossRef]
- Li, C.; Wang, J.; Wang, S.; Zhang, Y. A review of IoT applications in healthcare. Neurocomputing 2024, 565, 127017. [Google Scholar] [CrossRef]
- Segura Anaya, L.H.; Alsadoon, A.; Costadopoulos, N.; Prasad, P.W.C. Ethical Implications of User Perceptions of Wearable Devices. Sci. Eng. Ethics 2018, 24, 1–28. [Google Scholar] [CrossRef]
- Rahat, N.; Sahni, S.; Nasim, S. Mapping sustainability practices in the healthcare sector: A systematic literature review and future research agenda. Int. J. Consum. Stud. 2024, 48, e12997. [Google Scholar] [CrossRef]
- Hao, Y.; Foster, R. Wireless body sensor networks for health-monitoring applications. Physiol. Meas. 2008, 29, R27. [Google Scholar] [CrossRef]
- Abu Al Hla, Y.; Othman, M.; Saleh, Y. Optimizing an eco-friendly vehicle routing problem model using regular and occasional drivers integrated with driver behavior control. J. Clean. Prod. 2019, 234, 984–1001. [Google Scholar] [CrossRef]
- Di Mascolo, M.; Martinez, C.; Espinouse, M.L. Routing and scheduling in home health care: A literature survey and bibliometric analysis. Comput. Ind. Eng. 2021, 158, 107255. [Google Scholar] [CrossRef]

| Parameter | Value |
|---|---|
| U [10,50] km | |
| U [1120] km/h | |
| ≥0.1 | |
| 43 kWh | |
| Threshold | 50% |
| $30 per hour. | |
| $100 | |
| 8 h | |
| ≤10 h |
| Route Type | ||||
|---|---|---|---|---|
| (km/h) [44] | 30 | 55 | 80 | 120 |
| Maximum (km) [44] | 10 | 20 | 30 | 50 |
| (kWh/km) [52] | 0.14 | 0.12 | 0.10 | 0.13 |
| Source Node | Destination Node | (h) | (h) | (kWh) | |
|---|---|---|---|---|---|
| 1 | 2 | 1 | 8:51 | 9:03 | 34.30 |
| 2 | 4 | - | 9:13 | 9:53 | 32.62 |
| 4 | 6 | - | 10:22 | 10:52 | 30.22 |
| 6 | 14 | - | 11:40 | 12:12 | 24.76 |
| 14 | 9 | 1 | 12:34 | 12:46 | 23.64 |
| 9 | 13 | 1 | 13:20 | 14:30 | 21.24 |
| 13 | 15 | - | 15:04 | 15:34 | 43.00 |
| 15 | 1 | - | 16:08 | - | 38.45 |
| 1 | 5 | - | 8:40 | 8:52 | 38.32 |
| 5 | 10 | - | 9:14 | 9:26 | 37.62 |
| 10 | 8 | - | 10:19 | 10:31 | 31.77 |
| 8 | 12 | 1 | 11:09 | 11:33 | 29.07 |
| 12 | 3 | 1 | 12:05 | 12:17 | 26.91 |
| 3 | 11 | - | 13:01 | 13:19 | 21.06 |
| 11 | 16 | - | 13:53 | 14:25 | 43.00 |
| 16 | 7 | - | 15:02 | 15:17 | 38.71 |
| 7 | 1 | - | 15:48 | - | 33.51 |
| Source Node | Destination Node | Energy Consumption (kWh) | (Km/h) | (h) | |
|---|---|---|---|---|---|
| 1 | 2 | 2.70 | 3 | 73 | 0:20 |
| 2 | 4 | 1.68 | 2 | 67 | 0:29 |
| 4 | 6 | 2.40 | 2 | 56 | 0:56 |
| 6 | 14 | 5.46 | 4 | 103 | 0:22 |
| 14 | 9 | 1.12 | 1 | 22 | 0:34 |
| 9 | 13 | 2.40 | 3 | 72 | 0:30 |
| 13 | 15 | 2.60 | 3 | 90 | 0:32 |
| 15 | 1 | 4.55 | 4 | 102 | 0:39 |
| 1 | 5 | 1.68 | 1 | 27 | 0:22 |
| 5 | 10 | 0.70 | 2 | 59 | 0:54 |
| 10 | 8 | 5.85 | 4 | 95 | 0:38 |
| 8 | 12 | 2.70 | 3 | 78 | 0:32 |
| 12 | 3 | 2.16 | 3 | 81 | 0:44 |
| 3 | 11 | 5.85 | 4 | 96 | 0:34 |
| 11 | 16 | 5.2 | 4 | 100 | 0:36 |
| 16 | 7 | 4.29 | 4 | 108 | 0:34 |
| 7 | 1 | 5.2 | 4 | 90 | 0:28 |
| Driver 1 | Route | 1 | 2 | 4 | 6 | 14 | 9 | 13 | 15 | 1 | - | Deviation from avg. workload (h) | 0:08 |
| Arrival time | - | 8:51 | 9:13 | 10:22 | 11:40 | 12:34 | 13:20 | 15:04 | 16:08 | - | Total cost (USD) | 4 | |
| Departure time | 8:12 | 9:03 | 9:53 | 10:52 | 12:12 | 12:46 | 14:30 | 15:34 | - | - | Total working hours (h) | 8:08 | |
| Driver 2 | Route | 1 | 5 | 10 | 8 | 12 | 3 | 11 | 16 | 7 | 1 | Deviation from avg. workload (h) | 0:12 |
| Arrival time | - | 8:40 | 9:14 | 10:19 | 11:09 | 12:05 | 13:01 | 13:53 | 15:02 | 15:48 | Total cost (USD) | 6 | |
| Departure time | 8:12 | 8:52 | 9:26 | 10:31 | 11:33 | 12:17 | 13:19 | 14:25 | 15:17 | - | Total working hours (h) | 7:48 | |
| Driver 1 | Route | 1 | 8 | 7 | 9 | 4 | 11 | 15 | 3 | 5 | 1 | Deviation from avg. workload (h) | 1:05 |
| Arrival time | - | 8:39 | 9:01 | 10:47 | 11:14 | 12:37 | 13:40 | 15:20 | 16:05 | 17:05 | Total cost (USD) | 33 | |
| Departure time | 8:12 | 8:51 | 10:27 | 10:59 | 12:05 | 13:02 | 14:15 | 15:45 | 16:33 | - | Total working hours (h) | 9:05 | |
| Driver 2 | Route | 1 | 10 | 12 | 2 | 14 | 6 | 13 | 16 | 1 | - | Deviation from avg. workload (h) | 0:22 |
| Arrival time | - | 8:30 | 9:10 | 10:02 | 10:47 | 12:08 | 13:40 | 14:40 | 15:38 | - | Total cost (USD) | 11 | |
| Departure time | 8:12 | 8:49 | 9:37 | 10:27 | 11:40 | 13:10 | 14:10 | 15:10 | - | - | Total working hours (h) | 7:38 |
| Patient’s Node | Urgent/Non-Urgent | Quality Costs | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 2 | Urgent | 1 | 4 | 8:51 | 0:06 | 8:45 | 8:30 | 9:00 | 100% | 80% | 0 |
| 4 | Urgent | 0 | 4 | 9:13 | 0:01 | 9:15 | 9:00 | 9:30 | 93% | 86% | 0 |
| 6 | Non-urgent | 0 | 3 | 10:22 | 0.09 | 10:30 | 10:00 | 10:45 | 73% | 85% | 36 |
| 14 | Urgent | 0 | 4 | 11:40 | 0.02 | 11:45 | 11:30 | 12:00 | 80% | 75% | 0 |
| 9 | Non-urgent | 1 | 2 | 12:34 | 0:03 | 12:30 | 12:15 | 13:00 | 100% | 86% | 0 |
| 13 | Non-urgent | 1 | 3 | 13:20 | 0:06 | 13:30 | 13:00 | 13:45 | 100% | 84% | 0 |
| 5 | Non-urgent | 0 | 2 | 8:40 | 0:03 | 8:45 | 8:30 | 9:15 | 86% | 80% | 0 |
| 10 | Non-urgent | 0 | 2 | 9:14 | 0:08 | 9:15 | 9:00 | 9:45 | 77% | 86% | 18 |
| 8 | Urgent | 0 | 5 | 10:19 | 0:06 | 10:30 | 10:15 | 10:30 | 67% | 75% | 40 |
| 12 | Non-urgent | 1 | 2 | 11:09 | 0:05 | 11:15 | 10:45 | 11:30 | 100% | 84% | 0 |
| 3 | Urgent | 1 | 4 | 12:05 | 0:04 | 12:00 | 11:45 | 12:15 | 100% | 70% | 0 |
| 11 | Non-urgent | 0 | 3 | 13:01 | 0:03 | 13:00 | 12:30 | 13:15 | 73% | 90% | 51 |
| 7 | Non-urgent | 0 | 1 | 15:02 | 0:01 | 15:00 | 14:45 | 15:30 | 90% | 75% | 0 |
| Threshold | Senser | Z1 (h) | Z2 (km/h) | Z3 (USD) | Z4 (USD) | Energy Consumption (kWh/km) |
|---|---|---|---|---|---|---|
| Scenario 1 (20–80%) [53] | Yes | 8:39 | 82.3 | 16.8 | 69.2 | 48.6 |
| Scenario 2 (20–80%) [53] | No | 8:08 | 95.6 | 15.9 | 350.2 | 48.9 |
| Scenario 3 (50%) | Yes | 9:13 | 78.3 | 19.9 | 69.2 | 48.2 |
| Scenario 4 (50%) | No | 8:51 | 93.7 | 16.9 | 375.2 | 49.8 |
| Patient | E (BPM) (20–80%) | HR |
|---|---|---|
| 1 | 70 | 0 |
| 2 | 115 | 1 |
| 3 | 83 | 0 |
| 4 | 62 | 0 |
| 5 | 99 | 0 |
| 6 | 105 | 1 |
| 7 | 68 | 0 |
| 8 | 40 | 1 |
| 9 | 76 | 0 |
| 10 | 118 | 1 |
| Experiment Number | Patient’s Importance Level | Route | Z4 (USD) | Percentage of Change in Z4 (%) | |
|---|---|---|---|---|---|
| Scenario 1 | 1 | EV1: 2→5→4→9→7→6→15 EV2: 3→13→10→8→12→16→14→11 | 127.8 | 86% | - |
| Scenario 2 | 1,2,3 | EV1: 5→3→12→4→10→15 EV2: 14→7→9→13→6→8→16→11 | 372.9 | 83% | 192% |
| Scenario 3 | 1,2,3,4,5 | EV1: 2→5→3→12→4→10→15 EV2: 14→7→9→13→6→8→16→11 | 548.6 | 81% | 47% |
| Scenario 4 | 4,5 | EV1: 2→12→5→3→9→15→13 EV2: 10→4→11→7→8→15→6→14 | 677.2 | 80% | 23% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zaid, A.A.; Asaad, A.R.; Othman, M.; Haj Mohammad, A. Multi-Objective Technology-Based Approach to Home Healthcare Routing Problem Considering Sustainability Aspects. Logistics 2024, 8, 75. https://doi.org/10.3390/logistics8030075
Zaid AA, Asaad AR, Othman M, Haj Mohammad A. Multi-Objective Technology-Based Approach to Home Healthcare Routing Problem Considering Sustainability Aspects. Logistics. 2024; 8(3):75. https://doi.org/10.3390/logistics8030075
Chicago/Turabian StyleZaid, Ahmed Adnan, Ahmed R. Asaad, Mohammed Othman, and Ahmad Haj Mohammad. 2024. "Multi-Objective Technology-Based Approach to Home Healthcare Routing Problem Considering Sustainability Aspects" Logistics 8, no. 3: 75. https://doi.org/10.3390/logistics8030075
APA StyleZaid, A. A., Asaad, A. R., Othman, M., & Haj Mohammad, A. (2024). Multi-Objective Technology-Based Approach to Home Healthcare Routing Problem Considering Sustainability Aspects. Logistics, 8(3), 75. https://doi.org/10.3390/logistics8030075






