Abstract
The main purpose of this paper is to propose solutions for overcoming the obstacles that healthcare organizations might face when implementing lean. An in-depth review of existing barriers for lean implementation in healthcare supply chain is presented and validated by experts. Although there is a widespread use of lean concepts in developed countries, little attention has been paid to implementing a lean approach by healthcare providers in developing countries. The present study’s key novelty and contribution is related to this research gap. The study is thus focused in proposing solutions for healthcare organisations in developing countries, especially in Saudi Arabia. The efficacy of these solutions is assessed through experts’ opinion. The paper enhances the body of knowledge for the successful implementation of lean in a hospital setting.
1. Introduction
Several organisations attempt to adopt the lean management philosophy without necessarily understanding the lean principles and the possible barriers that they will have to face during the implementation. Most of these entities struggle to attain the desired outcomes and give up their attempts eventually [1,2,3]. Identification of potential barriers and obstacles prior to the implementation of lean (or any other continuous improvement tool) within the organisation is significant, as trying to overcoming these barriers after the implementation has started can be a hard task for the practitioners [4]. The healthcare organisations, as of any other organisations, should address barriers before beginning their lean journey [5].
Glasgow et al. [6] reviewed 47 lean related studies in healthcare and mentioned that 62% of the reported lean projects failed. These failures in most of the cases are attributed to organisations failing to pay attention to the barriers and the Critical Success Factors (CSFs) before and during lean implementation. After reviewing literature, as can be seen in Section 3 of the present paper, it was found that barriers for implementing lean principles in healthcare in general and in the hospital supply chain in particular, have not been investigated. Most of the existing studies have extracted their set of barriers from relevant publications in manufacturing setting while the healthcare perspective was neglected.
Literature review also revealed gaps that need to be addressed, especially in healthcare context, such as lean barriers, and motivation factors [7,8,9]. Moreover, there is a clear shortage in the literature with regards the ranking or prioritization of the barriers and enablers for lean implementation even though they are crucial and impact on healthcare organisation’s performance [4].
Understanding of organisations’ context is key for the suitable lean implementation in the supply chain [10]. Healthcare organisations’ have their own context and barriers in healthcare supply chain management (HSCM), which has not been covered yet. In real-life, it becomes indeed challenging for decision makers to overcome all barriers and apply all the solutions because of several unavoidable limitations such as the associated cost [2]. Considering different healthcare systems and different organisational cultures make this study the first of its kind. The purpose of this study is thus identifying barriers for implementing lean in a hospital supply chain from the Saudi perspective, prioritize them and indicate how to overcome these barriers.
2. Research Methodology
Because the barriers of lean implementation in healthcare supply chain management have not been investigated in depth and there is not enough information about how lean barriers can be avoided in such setting, the exploratory approach is adopted in this study. This study aims to help decision makers in healthcare institutions explore and determine how to avoid lean barriers in the supply chain context. To achieve the aim of the paper, the research methodology adopted includes a thorough literature review aiming at the lean barriers, a field study for verifying these barriers in the context of Saudi healthcare sector, subsequent analysis of the findings and finally employing experts for validating the results. Figure 1 illustrates graphically this process.
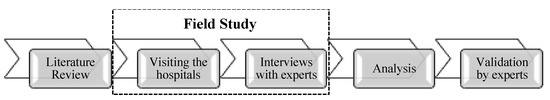
Figure 1.
Research methodology.
The thorough literature review (that will be presented in Section 3 of the present paper) was based on several material sources. Google Scholar, Emerald, Business Source Complete, Elsevier, Science-Direct, Scopus, and ProQuest, etc., were used. The barriers of implementing lean activities in HSCM were the cornerstone when literature was intensively checked with focus on the Saudi context. The gaps were identified, and the research areas were the key factors determining the context of this research.
The next step to this research was visiting three hospital in the Kingdom of Saudi Arabia (KSA) and conducting interviews with experienced staff who is working at these organisations to identify and assess lean implementation barriers in hospital supply chain and make sure that these factors are related to hospitals. The staff has been selected based on their experience, knowledge, and understanding of lean concepts, and their track record in participating continuous improvement initiatives. Their profile will be discussed in Section 4 of the present paper.
The interviews transcripts were coded in Nvivo software and thematic analysis was undertaken for identifying specific lean barriers that health sector in KSA is facing when attempting implementing lean. The thematic analysis also revealed potential solutions that are discussed and compared to what the literature is suggesting. Finally, the results were validated through experts’ judgement. As part of the validation exercise, the importance of the lean barriers as well as the effectiveness of the proposed solutions was assessed. Such a ranking can lead to prioritisation of these solutions that can assist health sector organizations to introduce and implement lean.
3. Literature Review: Implementation Barriers
As highlighted in the research methodology section, the research started with an extensive and thorough literature review. A number of find strings were used for collecting the relevant papers in a number of successive “passes”. Starting with searching with keywords such as “lean” AND “implementation”, and then filtering the results with further key strings such as “supply chain management” OR “supplier”, “healthcare” OR “hospital”. A huge number of articles were listed at the first round. The articles irrelevant to the aim of this research were excluded. The filtration process was conducted to remove redundancy by checking abstract and to what extent paper is related to the aim of research. Eventually, 60 papers were considered relevant and were analysed for identifying the implementation barriers.
The critical reviewing of the papers resulted into identifying a large number of barriers when implementing lean. Table 1 lists these barriers along with relevant references. In the following paragraphs these will be presented and discussed in more detail. During the critical review, specific themes were revealed. Salonitis and Tsinopoulos [3] categorized the barriers to lean implementation into four key themes: financial barriers, senior management related barriers, workforce related barriers, and other ones. In the present study, however, they are classified into the themes of: Culture, People, Business operations, and Strategy as can be seen in Figure 2.
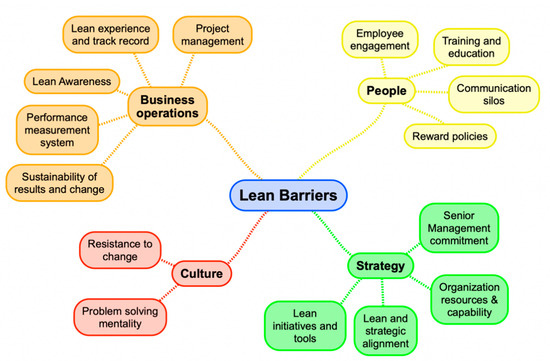
Figure 2.
Lean barriers classification.
Culture related barriers are always listed in any lean implementation related research. With regards the health sector and its supply chain this is still the case. Bhasin [11] mentioned that resistance to changing culture is one of the most serious issues that health-care organisations are facing, and the organisational culture determines which approach and methodology is most suitable for an organisation. The organization’s culture can also be a barrier when it is not characterized by a problem-solving and “can-do” mentality [12].
People related barriers repeatedly appeared in the literature review. Lack of employee involvement and engagement is key in this category. Willingness of the medical staff to implement lean transformation and a commitment to apply revised process improvement is crucial to the success of the lean initiative [13]. Lack of training and education of hospital staff was also raised in a number of publications, as can be seen in Table 1. Antony et al. [14] highlighted the lack of communication between employees (but at the healthcare institution level as well) is a main challenge for the lean implementation. Finally, applying an effective rewarding and recognition system (incentive) in healthcare organization can be considering a motivational approach for implementing lean concept and facilitate change transformation [15].
Key strategic decisions can be considered as barriers in implementing lean. Nwabueze [16] mentioned that there are many issues related to executives; for example, a poor investment in staff training and believing that training is just extra cost and waste of money and employees’ time. Al-Balushi et al. [15] highlighted the need for senior management and leadership commitment to lean implementation. In addition, poor organisation capabilities and lack of necessary resources can be considered barrier for implementing lean. In a number of publications, it was reported that due to lack of resources, hospitals focus on other initiatives considered more important and lean initiatives are postponed until the challenges are resolved [17,18].
The way healthcare organizations handle their operations is critical and can be a barrier. For example, the lack of a structured and fit-for-purpose performance measurement system results in organizations not being able to assess clearly the benefits of lean and thus losing momentum and focus [19]. Moreover, shortage of experience in lean and misunderstanding of lean tools can be a considerable barrier [20]. Finally, lack of awareness of lean, as mentioned by Psychogios et al. [21], is a considerable challenge for lean project, e.g., a lack of awareness of the benefits of lean as well as a poor of top management support.
Lean barriers differ according to different contexts and industries. Organisation’s capabilities, technology-based barriers and cultural barriers (employees’ culture) play a vital role in shaping in how an organisation intends to implement lean concept and to what extent the organisation has the abilities and capabilities to successfully carry it out. Based on that, the organisation decides to continue, postpone to a certain time or refuse to implement lean initiative permanently [2,22,23].

Table 1.
Lean Implementation barriers.
Table 1.
Lean Implementation barriers.
| Theme | Identified Barrier | References |
|---|---|---|
| Culture | Resistance to change | [2,9,24,25,26] |
| Problem solving mentality | [12] | |
| Strategy | Lean initiatives and tools | [2,16,19,23,25,27] |
| Lean and strategic alignment | [14,23,25,26] | |
| Organization resources and capability | [2,25,26,28] | |
| Senior Management commitment | [2,12,16,23,25,27,29,30] | |
| People | Employee engagement | [2,23,31] |
| Training and education | [2,21,23,26,29,30,32,33] | |
| Communication silos | [2,12,23,25,26,29,30] | |
| Reward policies | [2,23,26,30] | |
| Business | Project management | [23,26,29,30] |
| operations | Lean experience and track record | [2,23,27,33] |
| Lean awareness | [2,21,23,26,33] | |
| Performance measurement system | [2] | |
| Sustainability of results and change | [12,30] |
4. Field Study: Implementation Barriers from Saudi’s Perspective and Possible Solutions
Although lean has been implemented in several western organisations for decades, its implementation in the Middle Eastern countries in general [34], and in Saudi Arabia, in particular, remains in early phases. Identifying lean implementation’s barriers in the hospital supply chain has become a must to implement lean principles successfully in the Saudi context [28]. For capturing the lean implementation barriers in health sector organizations in KSA, with a focus on the supply chain management, a field study was undertaken. A number of healthcare organisations were visited, and 15 interviews were conducted on three different healthcare providers (named as X, Y, and Z for anonymity reasons) in KSA to identify the practical lean implementation barriers.
Table 2 presents the profiles of the interviewees. Semi-structured interviews have been conducted with experienced employees who had qualifications such as lean six sigma green, black, or master black belt (LSSGB, LSSBB, and LSSMBB, respectively) or who participated in continuous improvement projects. Moreover, the issues and problems identified in the literature review have been compared with the first-hand accounts of those qualified practitioners. From the interviews, nine themes were revealed along with probable solutions. These are discussed in detail in the following paragraphs.

Table 2.
Interviewees profiles.
4.1. Existence of Physicians’ Preferences (B1)
Participants indicated that physicians’ preferences constitute a real challenge for implementing lean thinking. A couple of indicative statements supporting this conclusion include, for example, the associate executive director for supply from hospital (X) stating that “clinical decision making: medical staff’s preferences should be avoided to implement any continuous improvement initiatives such as lean thinking.” Additionally, the medical purchasing manager from hospital (Y) stated that “disagree between doctors about certain medication play role in obstructing the implementation of lean.”
One of the ultimate goals of lean implementation is reducing the cost. Disagreement between medical staff plays a significant role in increasing medical supplies’ cost. One of the major barriers that healthcare supply chain face is physicians’ preferences. Due to physician’s preferences and patient characteristics, process variability is becoming higher in the healthcare supply chain [35]. According to Toba et al. [36], Physician Preference Items (PPIs) constitute 40% of total medical supply spending for a hospital. Montgomery and Schneller [37] defined PPIs as, “those for which physicians have strong preferences and make the choice in hospital purchasing—typically not based on cost but rather on personal experience with the device and relationships with the vendor’s sales representative.”
It is believed that physicians exhibit change resistance. However, in most of the cases medical doctors’ opinion is valid [38]. Certain preferences by clinicians for medical supplies and variation in processes are adopted to ensure the safety of patients. However, these preferences increase HSCM cost. Recently, healthcare providers have become aware of the financial cost of allowing clinicians the independence to order whatever medical items they select [36].
“Physicians preferences” barrier can be overcome by physician buy-in, especially those clinical items that have high-cost medical product evaluation, and review committees or value-analysis committees have been recommended to overcome the issue [38]. This approach was successful in one of the largest healthcare organisations in the United States, which is Kaiser Permanente (KP). KP encourages physicians for buy-in and agreement. For instance, their purchase decision takes place based on team consensus. The compliance of this approach was more than 90% [36]. Creating “standards and sourcing committee” can assist in overcoming this problem. This committee consists of physicians, pharmacists, medical equipment experts and purchasing/sourcing representatives.
4.2. Unpredictable Patient Demand (B2)
The interviews also revealed that it is difficult for hospitals to predict patients demand accurately and it constitutes real barrier for implementing lean thinking. For example, the demand planning and forecasting manager from hospital (Y) stated that, “in healthcare context, it is difficult to predict customers’ demand precisely.” Furthermore, the material management manager from hospital (Z) stated that, “It would be impossible at a certain point to predict the demand of patients it is too difficult.”
It is challenging for hospital supply chain decision makers to make sure that there are enough medicines and medical supplies for every patient’s needs. Lean is less applicable due to unstable demand [39]. The medical supply will be either overstocked or in shortage; in both of these cases, hospital supply chain cost will be increased. Medicines shortages pose risks for patient health as a result of non-treatment, under-treatment and possible medication errors from attempts to substitute missing medicines. Medicine shortages have been increasing in recent years [40]. For example, in the USA, new medications shortages increased from 70 in 2006 to more than 267 in 2011. The total number of new and ongoing shortages crossed the 450 mark in 2012. International Pharmaceutical Federation (FIP) mentioned that shortages cost American hospitals US $416 million, i.e., US $216 million in labor costs and US $200 million to purchase more expensive alternatives [40].
Bhakoo et al. [41] mentioned the unanticipated lead-times of medical supplies and unexpected patient demand, especially in the case of emergencies. In a large survey conducted by European Association of Hospital Pharmacists (EAHP), 21% of hospital pharmacists mentioned experiencing a shortage of medicines on a daily basis and 45% of them mentioned experiencing it on a weekly basis. Pharmacists who participated in the interview mentioned that they could not manage the shortage most of the time; they reported that the shortages causes patients to suffer disruption to their treatment [42].
Boutsioli [43] reported that healthcare organisations’ demand is unpredictable and can differ from hospital to hospital. Forecasting cannot be accurate, and it is difficult to predict precisely. Hospitals policies, procedures, and practices can play a role in increasing demand variation. Lack of policies of hospital admissions (sometimes called preadmission policies and referral policies) can create a high variation of demand. As a result, the number of patients cannot be predicted accurately. Clear policies, procedures and practices should be implemented by hospitals to manage the demand of patients, especially the cases that can wait for some time without any serious harm. Moreover, using different mathematical models can contribute significantly to control patients’ demands [22,43].
The use of information technology can minimize the uncertainty and the unpredictable demand in healthcare organisations. For example, using radio-frequency-identification (RFID) that can allow the monitoring of the patients and provide information that can be used to identify their number and status amongst others. These data can be easily accessible by computers and then simulation models can be developed and run. By using such methods, healthcare providers can optimise the use of their resources and reduce variation in patients’ numbers and therefore improve the forecasting process and reduce uncertainty [22].
4.3. Inadequate Knowledge and Lack of Understanding of Lean Concepts (B3)
The interviewees also indicated that inadequate knowledge and lack of understanding of lean thinking constitute a major challenge for implementing lean thinking. For example, medical purchasing manager from hospital (Y) stated that, “it is not clear what the aim of lean thinking in the hospitals nor is it clear what the supply chain wants to achieve.” Medical equipment manager from hospital (Z) stated that, “absence of the knowledge of lean approach is considered a real challenge for implementing lean initiative […]. Unfortunately, this problem is found in the healthcare sector in Saudi Arabia”.
Lack of understanding impacts organisations in different sectors, e.g., the lack of understanding of managers on how to apply continuous improvement initiatives and their poor grasp on the implementation of lean techniques and tools in a particular environment. In addition, many organisations have failed to earn any advantages from lean application due to the unclear understanding of leaders of lean performance and how to assess its impact on the performance [19,44]. Moreover, the lack understanding of how to begin and what should be conducted first [16] as well as a lack of realizing the benefit or change that will occur after applying lean [45] is another challenge.
Misunderstanding lean practices may create bad impression on managers. Many directors believe that lean implementation is costly, and its benefits are not worthy to invest in lean initiatives. A poor knowledge and misunderstanding by hospital supply chain decision makers are considered to be one of the biggest barriers [45,46].
By presenting a real-life scenario, such as lean success in another hospital and indicating how much healthcare organisations benefit from implementing lean in their processes may convince healthcare executives to adopt the lean approach. Well-trained and coached people are vital for implementing lean successfully [28,44]. If healthcare SCM managers are trained and made to understand the knowledge for implementing lean, then they will be more likely to accept lean initiatives.
Jeyaraman and Kee Teo [47] mentioned that using benchmark approach and narrating lean success stories can motivate managers to adopt the lean approach and attain what others have attained. This makes people in HSCM better understand lean approach benefits and become aware of lean’s advantages. Psychogios et al. [21] mentioned that insufficiency of awareness is a considerable challenge for any lean project, e.g., a lack of awareness of the benefits of lean and poor top management support.
4.4. Waste Identification in Hospital Supply Chain Processes (Delivering Value to the Patient) (B4)
Identifying waste in hospital supply chain management process is another barrier to lean implementation. The interviewees indicated that physicians’ preferences constitute real challenge for implementing lean thinking. For example, medical warehouse manager from hospital (Y) stated that, “So far, the main problem which is facing hospitals and supply chain departments have not been accurately identified wastes in supply chain practices”.
One of the key barriers in the healthcare context is to manage and deal with the intangibility of waste emerging because of the difficulty to identify it [20,48]. One of the main aims of lean implementation is to eliminate waste from the processes. Process analysis should be used to identify waste in each process, and then waste can be eliminated during improvement steps [49]. Healthcare staff is struggling to identify key processes that do not add value to patients [20].
Interviewees suggested value stream mapping (VSM) to identify waste in healthcare supply chain processes. VSM or process mapping is highlighting many types of problems in day-to-day operations and processes. They support lean initiative transformation by identifying waste (non-value-added) and value-added activities. VSM visualises wastes for elimination and areas for further improvement [20,50,51]. Moreover, the 5S approach (sort, straighten, shine, standardise, and sustain) plays a vital role in identifying and removing waste (non-added processes) from HSCM activities [20]. Applying VSM and 5S need well-trained staff. Shortage of people who can implement lean tools successfully is another barrier.
4.5. Lack of Hospital Support, Commitment, and Disbelief in Lean (B5)
The field study highlighted that poor commitment and support from top management can delay lean implementation significantly. Interviewees indicated that lack of support and commitment and disbelief is considered challenge for implementing lean thinking. For example, the purchasing and tendering manager from hospital (X) stated that, “without top management support, it is impossible to deploy lean approach.” Similarly, the procurement and contract manager from hospital (Y) stated that, “if the decision makers in hospitals do not strongly support continuous improvement projects, the projects definitely fail”.
One of the main reasons behind the failure of lean or any continuous improvement initiative is the poor commitment of top leadership [44]. All directors in each level of the hospital should be persuaded that adopting lean is the right initiative. Decision makers at the hospital supply chain need to demonstrate strong commitment and full support in providing all lean implementation requirements such resources, employees training, budget, and other needs that help, facilitate, and accelerate lean implementation.
To overcome this challenge, building a lean dashboard at workplace facilitates both operators and managers to track the ongoing processes, reduce nonvalue adding activities (NVA) and pay attention toward bottlenecks [52,53]. In addition, the senior management must be committed to improve the quality, include it within its objectives and strategic plan and regularly review the extent of its achievement. Moreover, leveraging previous lean implementation experience can also enhance hospital’s commitment toward lean initiatives.
4.6. Hospital Culture and Resistance to Change (B6)
Visiting hospitals also revealed that hospital culture and resistance to change constitute barrier for implementing lean thinking in supply chain. For example, the associate executive director for supply from hospital (X) stated that, “resistance culture is the biggest issue in changing journey.” The associate executive director for logistic from hospital (Z) also stated that, “the absence of advocate/supportive culture for change is considered a big issue in lean roadmap.”
Organisational culture is a key element in the successful adoption of lean practices [53]. Bhasin [54] claim that 80% of successful lean implementation is related to cultural issues. The culture of an organisation has the probability of creating resistance or restricting change efforts and may not be supportive to initiative [24]. Bhasin [55] mentioned that culture change resistance is one of the serious issues healthcare organisations are facing. Healthcare organisations need to alter their culture totally to guarantee successful lean adoption. Albliwi et al. [23] claimed that resistance to change is the most frequent cause leading to failure of lean implementation in the healthcare organisations. SCM in healthcare is suffering from the absence of process improvement culture [35]. Such practices create a type of resistance to implementing lean initiatives in HSCM.
Organisational Culture is considered one of the most important factors in implementing lean in the Saudi context [28,56]. Sharing information about lean, effective communication and lean project success initiative stories can enhance lean culture and reduce resistance to change. Even though Saudi organisations lack the priority regarding training on lean six sigma yellow belt (LSSYB), many authors suggest all employees should be LSSYB certified. Attending awareness sessions such as LSSYB can play a vital role in changing organisational culture and lowering the level of change resistance [28].
Applying effective rewarding and recognition system (incentive) in healthcare organisation can be considered a motivational approach for implementing lean concept and facilitate change transformation. For example, bonus or monetary prize can facilitate implementation of lean [57].
4.7. Scarcity of Qualified Human Resources and Lack of Training (B7)
Interviewees also mentioned that lack and shortage of qualified and well-trained staff constitute real barrier for implementing lean thinking. For example, the associate executive director for supply from hospital (Y) stated that, “Although there is training and qualified staff but hospital still suffers from shortage of high skilled employees and needs the intensive training which is required for implementing lean thinking.” The associate executive director for logistic from hospital (Z) also stated that, “there is no training specifically about lean and its applications […] hospital’s staff need to know how to implement lean practically.”
Training is vital for the success of lean implementation in HSCM. No healthcare organisation can deliver high-quality patient satisfaction and safety and work process without well-trained employees. Lean implementation most likely requires different training than what is currently offered. During training sessions, many questions will be answered, and these answers will motivate employees to adopt and accept lean initiatives. These questions include why the lean project is necessary or needed, what the benefits of applying lean are, to what extent lean add value to patients. Taring is may be the first step toward lean implementation.
Large investments in training represent another problem for quality improvement programmes in healthcare [14]. A healthcare organisation should invest in their employees’ competencies to build and sustain lean implementation. The dependency on external lean consultant will be costly and not support lean sustainability. This is contrary and inconsistent with the objective of the lean concept.
Nwabueze [16] mentioned that there are many issues related to executives, for example, poor investment in staff training and believing that training is just extra cost and waste of money and employees’ time. Trained people drive change in the healthcare organisation so the staff should have the skills, knowledge, and capabilities to lead the lean initiative and implement it properly. The presence of non-specialized staff in leadership positions who they do not believe in change and the concept of lean is a major obstacle to its successful application. This can be attributed to poor training and lack of understanding of the concepts of continuous improvement such as lean.
4.8. Absence of the Required Level of Leanness (B8)
Interviewees indicated that absence of required level of lean constitute challenge for implementing lean thinking. For example, the associate executive director for supply from hospital (X) stated that, “measuring the maturity of level in terms of lean is a serious problem in supply chain practices.” The associate executive director for supply from hospital (Y) stated that, “measuring the degree of leanness in supply chain operations is a real challenge facing decision makers in hospital.”
Numerous and diverse organizations have implemented lean principles and practices, which concentrate on improving the efficiency of business processes by reducing cost, waste, consumptions and effort. Almutairi et al. [58] suggested a model as to enable decision makers in hospital supply chain to take suitable actions for improving lean implementation level. Healthcare institutions, as any other investigation, need to be able to assess their current level of leanness as at lease a starting point for implementing lean [11,55]. The absence of accurate criteria and precise attributes for determining the level of leanness required for the implementation of lean concept in the hospital supply chain result in a lack of clarity in the application of the lean concept. This challenge can be avoided by implementing leanness level assessment model [47,59].
4.9. Lack of Effective Communication and Information Sharing (B9)
Field study also revealed that lack of effective communication and information sharing. The interviewees indicated that lack of support and commitment and disbelief is considered challenge for implementing lean thinking. For example, the material management manager from hospital (X) stated that, “Unfortunately, there is no effective communication between departments and staff […] this means there is sharing information in suitable time.” The medical warehouse manager from hospital (Y) stated that, “without effective communication and information sharing between supply chain departments, lean implementation would be impossible.”
In addition, poor communication between healthcare professional departments is another challenge in hospital setting. In the healthcare supply chain, the breakdown of effective/visual communication between the different departments/parties within the procurement process leads to dysfunctional supply chain [60]. The lack of communication within the healthcare is a main challenge for the lean implementation [14,20]. Poor communication may lead to increase in the time of delivery, raising the cost of medical items distribution, not meeting physicians’ needs and reducing purchase of the right medical equipment [60].
To overcome this barrier, there is need to share information, work closely, and go against “silo working” (not sharing information) by documenting all information and making it available on intranet (internal network). Communication can affect organisational culture in terms of lean implantation [57]. Poor communication was observed in United Kingdom’s healthcare system. Silo working (no sharing information) is usually expected in any organisation. This practice can hinder effective communication between parties while implementing continuous improvement initiatives [20].
Establishing effective and clear channels for communication at all healthcare SCM levels ensures the engagement of all the employees in the lean initiative, for example, using electronic channels rather than paperwork. These communication channels will help supply chain in healthcare organisations to solve issues related to the lack of communication.
5. Suggested Framework for Overcoming Barriers
As it was discussed in the previous chapter, during visiting the hospitals, the interviews that were held with participants also focused in identifying the suitable solutions to overcome lean implementation barriers. The suggested solutions presented in the previous sections are summarized in Table 3. Specific solutions have been proposed for each barrier, that directly help in overcoming specific barriers. However, lean philosophy intends to introduce a more systemic and holistic approach, and as such it is obvious that the solutions proposed indirectly have positive impact in overcoming the other barriers as well. A force field analysis (a graphical way for assessing the driving and hindering factors for a planned change) can be used for summarizing these findings as shown in Figure 3. Such a force field analysis as well as the suggested solutions for overcoming the barriers can serve a framework for the easier implementation of lean in lean in the health sector.

Table 3.
Suggested Solutions to overcome Barrier.
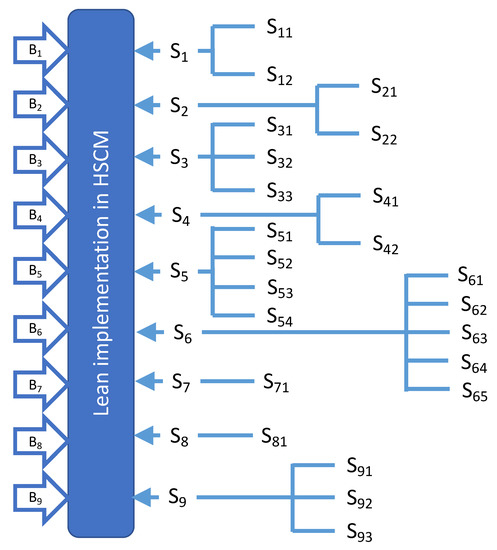
Figure 3.
Force field analysis.
6. Validation and Prioritization of Solutions Based on Experts’ Judgment
The barriers and their proposed solutions were validated with experts from three hospitals. For example, associate executive director for supply from hospital (X) stated that, “If the hospital implements proposed solutions correctly the SCM departments is ready to start lean journey without obstacles.”
One of the key objectives of this phase was also the prioritization of the solutions. Such prioritization extremely important and useful for them to plan their improvement initiatives. The main reason of the focusing on some barriers and neglect others are that individual barriers possess different levels of significance that change with organisation, its priorities, its nature, and its type [2]. In addition, it is extremely difficult for healthcare organisations to overcome all of these barriers simultaneously [4]. The 15 participants were presented the barriers and associated solutions and were asked to rank each solution and barrier in a scale from 1 to 5 with 1 being the least important barrier or least effective solution and 5 being the most important barrier or important solution. Table 4 presents the results of this ranking.

Table 4.
Prioritization exercise and results.
It is clear from Table 4 that the most important barrier faced by healthcare organisations when they attempt to deploy lean initiative in their supply chain is scarcity of qualified human resources and lack of training (B7) with importance of 4.80. Most participants agreed that absence of well-trained employees constitutes the most challenge to start a lean journey. Some respondents mentioned that without qualified people, it is impossible to start a lean project. This was followed by hospital culture and resistance to change (B6), lack of effective communication and information sharing (B9), absence of the required level of leanness (B8), and the identifying type of waste through hospital supply chain processes (delivering value to the patient) (B4) with relative importance of 4.67, 4.47, 4.40, and 4.13, respectively. In order to assess if there is any significant difference between the experts’ opinions on the various barriers, the standard deviation is shown for each barrier in Table 4. As it can be seen, this is well controlled within 10 to 15%. It should be noted that analysis of variance was not conducted to compare the means, as the set of response for each barrier cannot be considered as a sample from the population of answers.
Figure 4 represents relative importance of lean barriers in HSCM. Based on interviewees, the proposed solutions can contribute effectively to overcome the barriers. For example, the suggested solutions can overcome the barrier to overcome Scarcity of qualified human resources and lack of training challenge with 96% effectiveness. Table 4 and Figure 5 illustrate the extent to which proposed solutions can effectively overcome barriers when implementing lean in SCM. The results presented are in agreement with similar studies presented in the past, for example with the ones presented by Albliwi et al. [28]. In a similar way as with the barriers, the standard deviation was calculated for each solution, and follows similar behaviour as with the barriers.
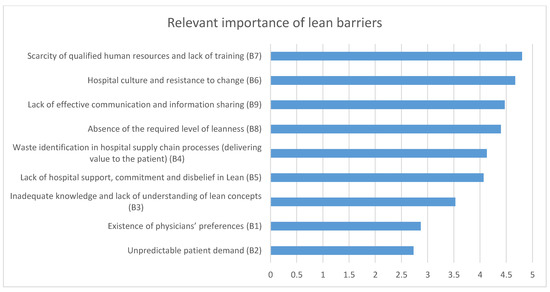
Figure 4.
Relevant importance of lean barriers.
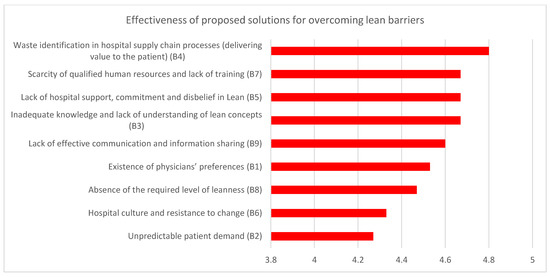
Figure 5.
Effectiveness of proposed solutions for overcoming lean barriers.
7. Managerial Implications
The research presented in this paper resulted in a number of actions that can help overcome the barriers that health sector organizations face when they try to implement lean within their organization and their supply chain. The actions, characterised as solutions, were listed in Table 3.
The first key implication is that the potential barriers are coded, and thus can more easily identified by the supply chain managers. This research assists the supply chain manager in developing plans for overcoming specific lean implementation barriers. The senior management in a health sector, after identifying the key barriers, can prioritize and rank them as to decide on actions that can have the highest possible impact. Finally, the list of barriers and their associated solutions can be used as a check list when recruiting new employees for a number of non-medical departments in a health sector organization such as the purchasing departments.
8. Conclusions
There is no easy and quick method to become a lean healthcare organisation. Toyota has taken over 50 years to implement continuous improvement approach throughout the whole company [20]. In the present study, nine key barriers were identified. These barriers are as follows: existence of physicians’ preferences; unpredictable patient demand; inadequate knowledge and lack of understanding lean concept; identifying the type of waste through hospital supply chain processes (delivering value to the patient); lack of hospital support, commitment, and disbelief in lean; organisational culture and resistance to change; scarcity of qualified human resources and lack of training; and absence of the required level of leanness and lack of effective communication and information sharing.
These barriers to successful lean implementation can be overcome with adopting many practices. Factors such as physicians’ buy-in, using technology, hospital leadership support, improving organisational culture to reduce resistance to change, setting up a rewarding system to motivate people to accept the change, excellent communication, effective sharing of information, and train employees will enable the healthcare organisation to build its own lean philosophy based on patient value satisfaction and not simply implementing techniques and tools adopted from other industries. In general, lack trained of SCM employees in Saudi healthcare organisations was clearly observed and is consider the main issue by the decision makers in HSCM.
Author Contributions
Conceptualization, A.M.A. and K.S.; methodology, A.M.A.; validation, A.M.A., A.A.-A. and K.S.; formal analysis, A.M.A.; investigation, A.M.A.; resources, K.S.; writing—original draft preparation, A.M.A.; writing—review and editing, M.A. and K.S.; supervision, A.A.-A. and K.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are available in the paper.
Conflicts of Interest
The authors declare no conflict of interest.
References
- AlManei, M.; Salonitis, K.; Xu, Y. Lean implementation frameworks: The challenges for SMEs. Procedia CIRP 2017, 63, 750–755. [Google Scholar] [CrossRef]
- Yadav, G.; Seth, D.; Desai, T.N. Prioritising solutions for Lean Six Sigma adoption barriers through fuzzy AHP-modified TOPSIS framework. Int. J. Lean Six Sigma 2018, 9, 270–300. [Google Scholar] [CrossRef]
- Salonitis, K.; Tsinopoulos, C. Drivers and Barriers of Lean Implementation in the Greek Manufacturing Sector. Procedia CIRP 2016, 57, 189–194. [Google Scholar] [CrossRef]
- Yadav, G.; Desai, T.N. Lean Six Sigma: A categorized review of the literature. Int. J. Lean Six Sigma 2016, 7, 2–24. [Google Scholar] [CrossRef]
- Matteo, M.; Terrence, P.; Darmanata, J. Sustaining Lean and Six Sigma Improvements in healthcare: Results from a pilot Survey Sustaining Lean and Six Sigma Improvements in healthcare. In Proceedings of the Third European Research Conference on Continuous Improvement and Lean Six Sigma, Glasgow, Scotland, 28 March 2011. [Google Scholar]
- Glasgow, J.M.; Scott-Caziewell, J.R.; Kaboli, P.J. Guiding inpatient quality improvement: A systematic review of Lean and Six Sigma. Jt. Comm. J. Qual. Patient Saf. 2010, 36, 533–540. [Google Scholar] [CrossRef]
- Vashishth, A.; Chakraborty, A.; Antony, J. Lean Six Sigma in financial services industry: A systematic review and agenda for future research. Total Qual. Manag. Bus. Excel. 2017, 30, 447–465. [Google Scholar] [CrossRef]
- Laureani, A.; Antony, J. Leadership characteristics for Lean Six Sigma. Int. J. Product. Perform. Manag. 2011, 61, 110–120. [Google Scholar] [CrossRef]
- Pepper, M.; Spedding, T. The evolution of lean Six Sigma. Int. J. Qual. Reliab. Manag. 2010, 27, 138–155. [Google Scholar] [CrossRef]
- Tortorella, G.L.; Miorando, R.; Marodin, G. Lean supply chain management: Empirical research on practices, contexts and performance. Int. J. Prod. Econ. 2017, 193, 98–112. [Google Scholar] [CrossRef]
- Bhasin, S. An appropriate change strategy for lean success. Manag. Decis. 2012, 50, 439–458. [Google Scholar] [CrossRef]
- Gijo, E.V.; Antony, J. Reducing Patient Waiting Time in Outpatient Department Using Lean Six Sigma Methodology. Qual. Reliab. Eng. Int. 2014, 30, 1481–1491. [Google Scholar] [CrossRef]
- Laureani, A.; Brady, M.; Antony, J. Applications of Lean Six Sigma in an Irish hospital. Leadersh. Health Serv. 2013, 26, 322–337. [Google Scholar] [CrossRef]
- Antony, J.; Downey-Ennis, K.; Antony, F.; Seow, C. Can Six Sigma be the ‘cure’ for our ‘ailing’ NHS? Leadersh. Health Serv. 2007, 20, 242–253. [Google Scholar] [CrossRef]
- Al-Balushi, S.; Sohal, A.; Singh, P.; Al Hajri, A.; Al Farsi, Y.; Al Abri, R. Readiness factors for lean implementation in healthcare settings—A literature review. J. Health Organ. Manag. 2014, 28, 135–153. [Google Scholar] [CrossRef]
- Nwabueze, U. Process improvement: The case of a drugs manufacturing company. Bus. Process. Manag. J. 2012, 18, 576–584. [Google Scholar] [CrossRef]
- D’Andreamatteo, A.; Ianni, L.; Lega, F.; Sargiacomo, M. Lean in healthcare: A comprehensive review. Health Policy 2015, 119, 1197–1209. [Google Scholar] [CrossRef]
- Kim, C.S.; Spahlinger, D.A.; Kin, J.M.; Billi, J.E. Lean health care: What can hospitals learn from a world-class automaker? J. Hosp. Med. 2006, 1, 191–199. [Google Scholar] [CrossRef]
- Karim, A.; Arif-Uz-Zaman, K. A methodology for effective implementation of lean strategies and its performance evaluation in manufacturing organizations. Bus. Process Manag. J. 2013, 19, 169–196. [Google Scholar] [CrossRef]
- Grove, A.L.; Meredith, J.O.; MacIntyre, M.; Angelis, J.; Neailey, K. UK health visiting: Challenges faced during lean implementation. Leadersh. Health Serv. 2010, 23, 204–218. [Google Scholar] [CrossRef]
- Psychogios, A.G.; Atanasovski, J.; Tsironis, L.K. Lean Six Sigma in a service context: A multi-factor application approach in the telecommunications industry. Int. J. Qual. Reliab. Manag. 2012, 29, 122–139. [Google Scholar] [CrossRef]
- Gupta, D.; Potthoff, S.J. Matching Supply and Demand for Hospital Services. Found. Trends Technol. Inf. Oper. Manag. 2016, 8, 131–274. [Google Scholar] [CrossRef]
- Albliwi, S.; Antony, J.; Abdul Halim Lim, S.; van der Wiele, T. Critical failure factors of Lean Six Sigma: A systematic literature review. Int. J. Qual. Reliab. Manag. 2014, 31, 1012–1030. [Google Scholar] [CrossRef]
- McLean, R.; Antony, J. Why continuous improvement initiatives fail in manufacturing environments? A systematic review of the evidence. Int. J. Prod. Perform. Manag. 2014, 63, 370–376. [Google Scholar] [CrossRef]
- Antony, J.; Krishan, N.; Cullen, D.; Kumar, M. Lean Six Sigma for higher education institutions (HEIs): Challenges, barriers, success factors, tools/techniques. Int. J. Product. Perform. Manag. 2012, 61, 940–948. [Google Scholar] [CrossRef]
- Pedersen, E.R.G.; Huniche, M. Determinants of lean success and failure in the Danish public sector. Int. J. Public Sect. Manag. 2011, 24, 403–420. [Google Scholar] [CrossRef]
- Reijula, J.; Tommelein, I.D. Lean hospitals: A new challenge for facility designers. Intell. Build. Int. 2012, 4, 126–143. [Google Scholar] [CrossRef]
- Albliwi, S.A.; Antony, J.; Arshed, N.; Ghadge, A. Implementation of Lean Six Sigma in Saudi Arabian organisations. Int. J. Qual. Reliab. Manag. 2017, 34, 508–529. [Google Scholar] [CrossRef]
- Chakravorty, S.S.; Shah, A.D. Lean Six Sigma (LSS): An implementation experience. Eur. J. Ind. Eng. 2012, 6, 118. [Google Scholar] [CrossRef]
- Snee, R.D. Lean Six Sigma—Getting better all the time. Int. J. Lean Six Sigma 2010, 1, 9–29. [Google Scholar] [CrossRef]
- Arumugam, V.; Antony, J.; Douglas, A. Observation: A Lean tool for improving the effectiveness of Lean Six Sigma. TQM J. 2012, 24, 275–287. [Google Scholar] [CrossRef]
- Hilton, R.J.; Sohal, A. A conceptual model for the successful deployment of Lean Six Sigma. Int. J. Qual. Reliab. Manag. 2012, 29, 54–70. [Google Scholar] [CrossRef]
- Panizzolo, R.; Garengo, P.; Sharma, M.K.; Gore, A. Lean manufacturing in developing countries: Evidence from Indian SMEs. Prod. Plan. Control. 2012, 23, 769–788. [Google Scholar] [CrossRef]
- Alefari, M.; AlManei, M.; Salonitis, K. Lean manufacturing, leadership and employees: The case of UAE SME manufacturing companies. Prod. Manuf. Res. 2020, 8, 222–243. [Google Scholar] [CrossRef]
- Moons, K.; Waeyenbergh, G.; Pintelon, L. Measuring the logistics performance of internal hospital supply chains—A literature study. Omega 2019, 82, 205–217. [Google Scholar] [CrossRef]
- Toba, S.; Tomasini, M.; Yang, Y. Supply Chain Management in hospital: A case study. Calif. J. Oper. Manag. 2018, 6, 55. [Google Scholar]
- Montgomery, K.; Schneller, E.S. Hospitals’ Strategies for Orchestrating Selection of Physician Preference Items. Milbank Q. 2007, 85, 307–335. [Google Scholar] [CrossRef]
- Neumann, L. Streamlining the Supply Chain. Healthc. Financ. Manag. 2003, 57, 56–62. [Google Scholar]
- Wilson, L. How to Implement Lean Manufacturing; McGraw-Hill: New York, NY, USA, 2010. [Google Scholar]
- Hedman, L. Global approaches to addressing shortages of essential medicines in health systems. WHO Drug Inf. 2016, 30, 180–185. [Google Scholar]
- Bhakoo, V.; Singh, P.J.; Sohal, A. Collaborative management of inventory in Australian hospital supply chains: Practices and issues. Supply Chain Manag. Int. J. 2012, 17, 217–230. [Google Scholar] [CrossRef]
- European Association of Hospital Pharmacists (EAHP) 2014. Medicines Shortages in European Hospitals—EAHP Survey Reports. Available online: https://www.eahp.eu/news/eahps-2014-medicines-shortages-report-now-published (accessed on 15 December 2020).
- Boutsioli, Z. Estimation of unpredictable hospital demand variations in two Piraeus public hospitals, Greece. J. Hosp. Adm. 2013, 2, 126–137. [Google Scholar] [CrossRef]
- Alefari, M.; Salonitis, K.; Xu, Y. The Role of Leadership in Implementing Lean Manufacturing. Procedia CIRP 2017, 63, 756–761. [Google Scholar] [CrossRef]
- Gurumurthy, A.; Kodali, R. Design of lean manufacturing systems using value stream mapping with simulation. J. Manuf. Technol. Manag. 2011, 22, 444–473. [Google Scholar] [CrossRef]
- De Souza, L.B.; Pidd, M. Exploring the barriers to lean health care implementation. Public Money Manag. 2011, 31, 59–66. [Google Scholar] [CrossRef]
- Jeyaraman, K.; Teo, L.K. A conceptual framework for critical success factors of lean Six Sigma. Int. J. Lean Six Sigma 2010, 1, 191–215. [Google Scholar] [CrossRef]
- Gupta, S.; Sharma, M.; Sunder, M.V. Lean services: A systematic review. Int. J. Product. Perform. Manag. 2016, 65, 1025–1056. [Google Scholar] [CrossRef]
- Walley, P.; Radnor, Z.; Stephens, A.; Bucci, G. Evaluation of the lean approach to business management and its use in the public sector. Scott. Exec. Soc. Res. 2006, 20, 1–6. [Google Scholar]
- Cottyn, J.; Van Landeghem, H.; Stockman, K.; Derammelaere, S. A method to align a manufacturing execution system with Lean objectives. Int. J. Prod. Res. 2011, 49, 4397–4413. [Google Scholar] [CrossRef]
- Mostafa, S.; Dumrak, J.; Soltan, H. A framework for lean manufacturing implementation. Prod. Manuf. Res. 2013, 1, 44–64. [Google Scholar] [CrossRef]
- Gremyr, I.; Fouquet, J. Design for Six Sigma and lean product development. Int. J. Lean Six Sigma 2012, 3, 45–58. [Google Scholar] [CrossRef]
- Pakdil, F.; Leonard, K.M. The effect of organizational culture on implementing and sustaining lean processes. J. Manuf. Technol. Manag. 2015, 26, 725–743. [Google Scholar] [CrossRef]
- Bhasin, S. Measuring the Leanness of an organisation. Int. J. Lean Six Sigma 2011, 2, 55–74. [Google Scholar] [CrossRef]
- Bhasin, S. Prominent obstacles to lean. Int. J. Prod. Perform. Manag. 2012, 61, 403–425. [Google Scholar] [CrossRef]
- Alkhoraif, A.; McLaughlin, P. Lean implementation within manufacturing SMEs in Saudi Arabia: Organizational culture aspects. J. King Saud Univ. Eng. Sci. 2018, 30, 232–242. [Google Scholar] [CrossRef]
- Brkic, V.S.; Tomic, B. Employees factors importance in Lean Six Sigma concept. TQM J. 2016, 28, 774–785. [Google Scholar] [CrossRef]
- Almutairi, A.M.; Salonitis, K.; Al-Ashaab, A. Assessing the leanness of a supply chain using multi-grade fuzzy logic: A health-care case study. Int. J. Lean Six Sigma 2019, 10, 81–105. [Google Scholar] [CrossRef]
- Oleghe, O.; Salonitis, K. Leanness Assessment Tools and Frameworks. In Progress in Lean Manufacturing; Management and Industrial Engineering; Springer: Cham, Switzerland, 2018. [Google Scholar] [CrossRef]
- Al-Karaghouli, W.; Ghoneim, A.; Sharif, A.; Dwivedi, Y.K. The Effect of Knowledge Management in Enhancing the Procurement Process in the UK Healthcare Supply Chain. Inf. Syst. Manag. 2013, 30, 35–49. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).