Surveillance of Chemical Foodborne Disease Outbreaks in Zhejiang Province, China, 2011–2023
Abstract
1. Introduction
2. Methods
2.1. Definitions
2.2. Diagnostic Criteria
2.3. Data Sources
2.4. Statistical Analysis
3. Results
3.1. General Characteristics
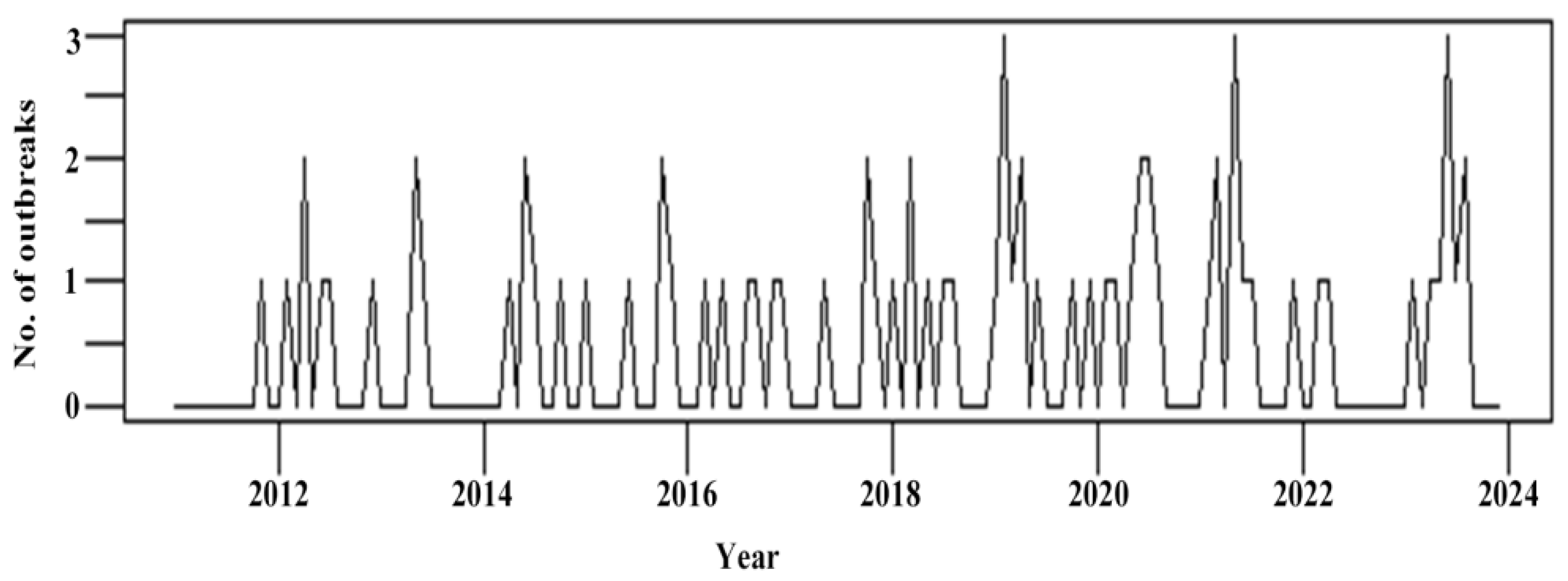
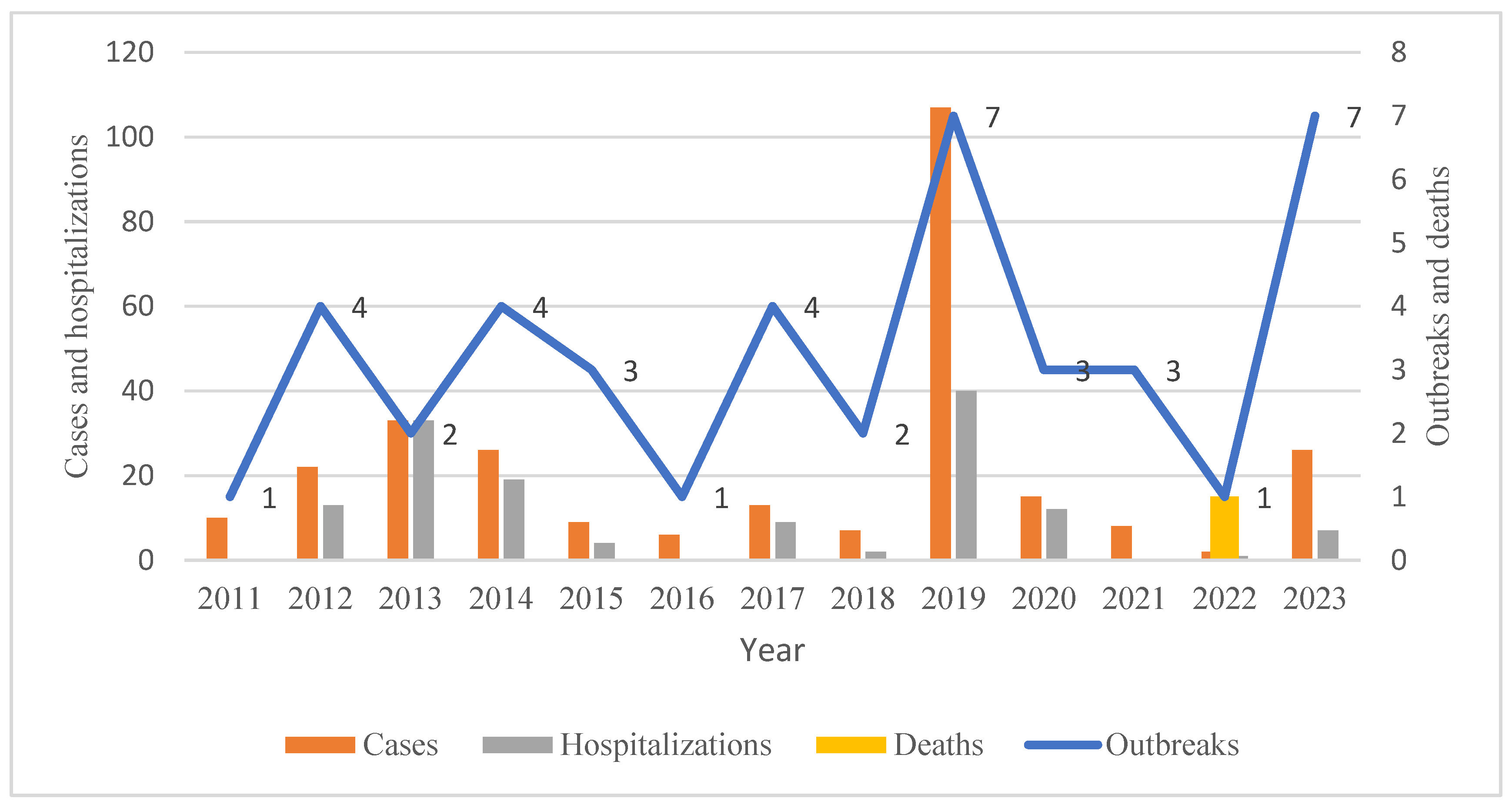
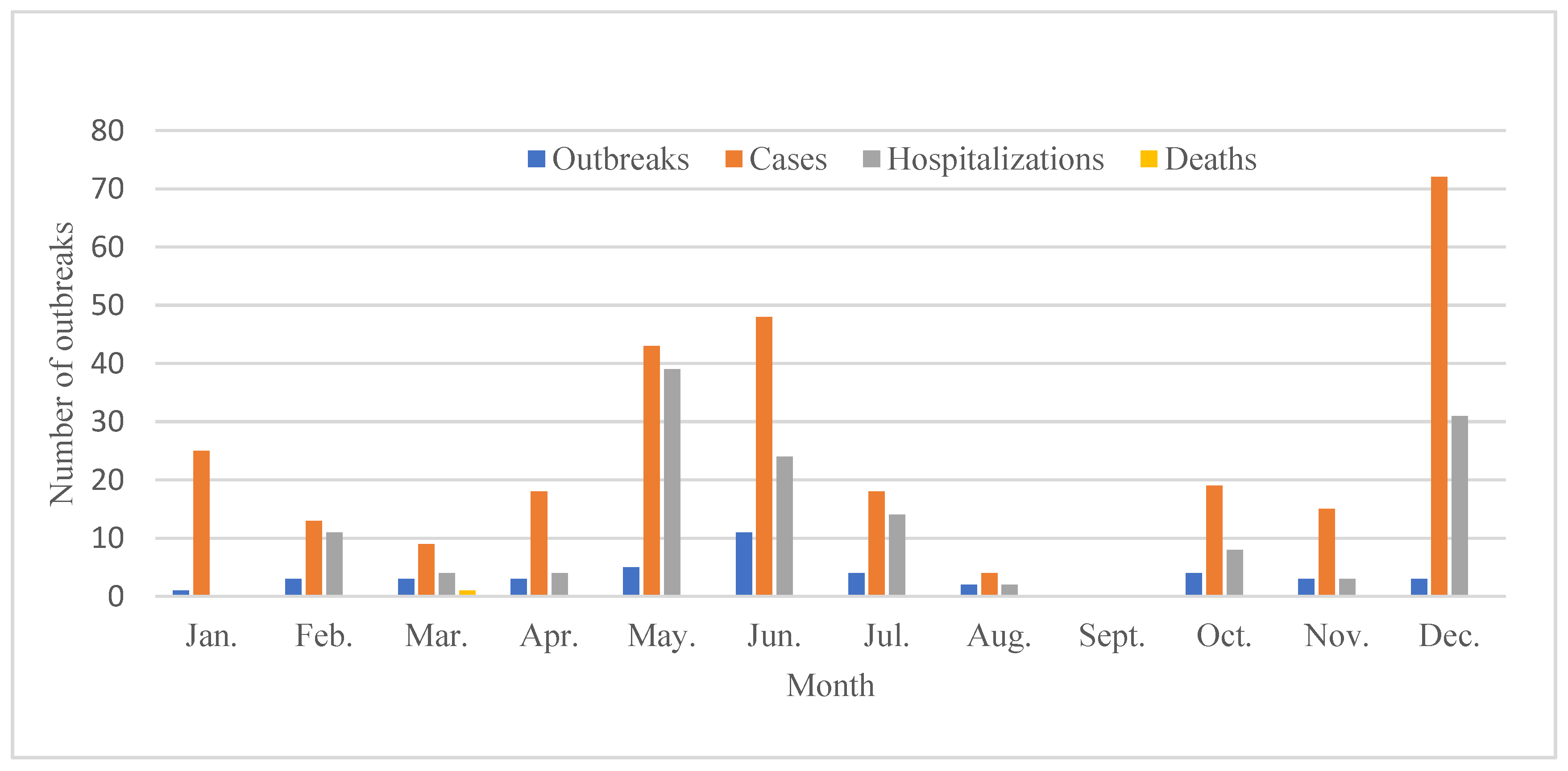
3.2. Temporal Distribution
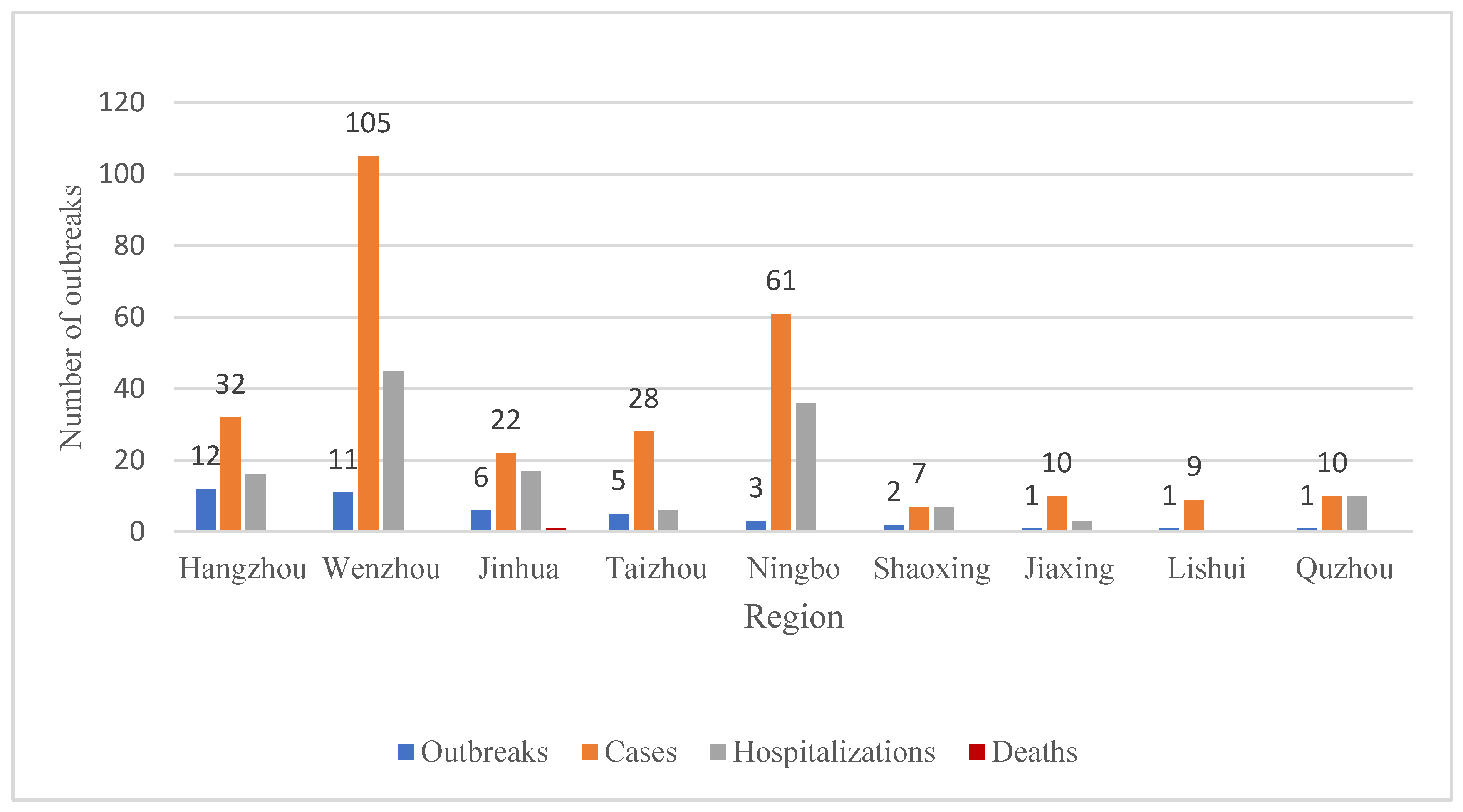
3.3. Regional Distribution
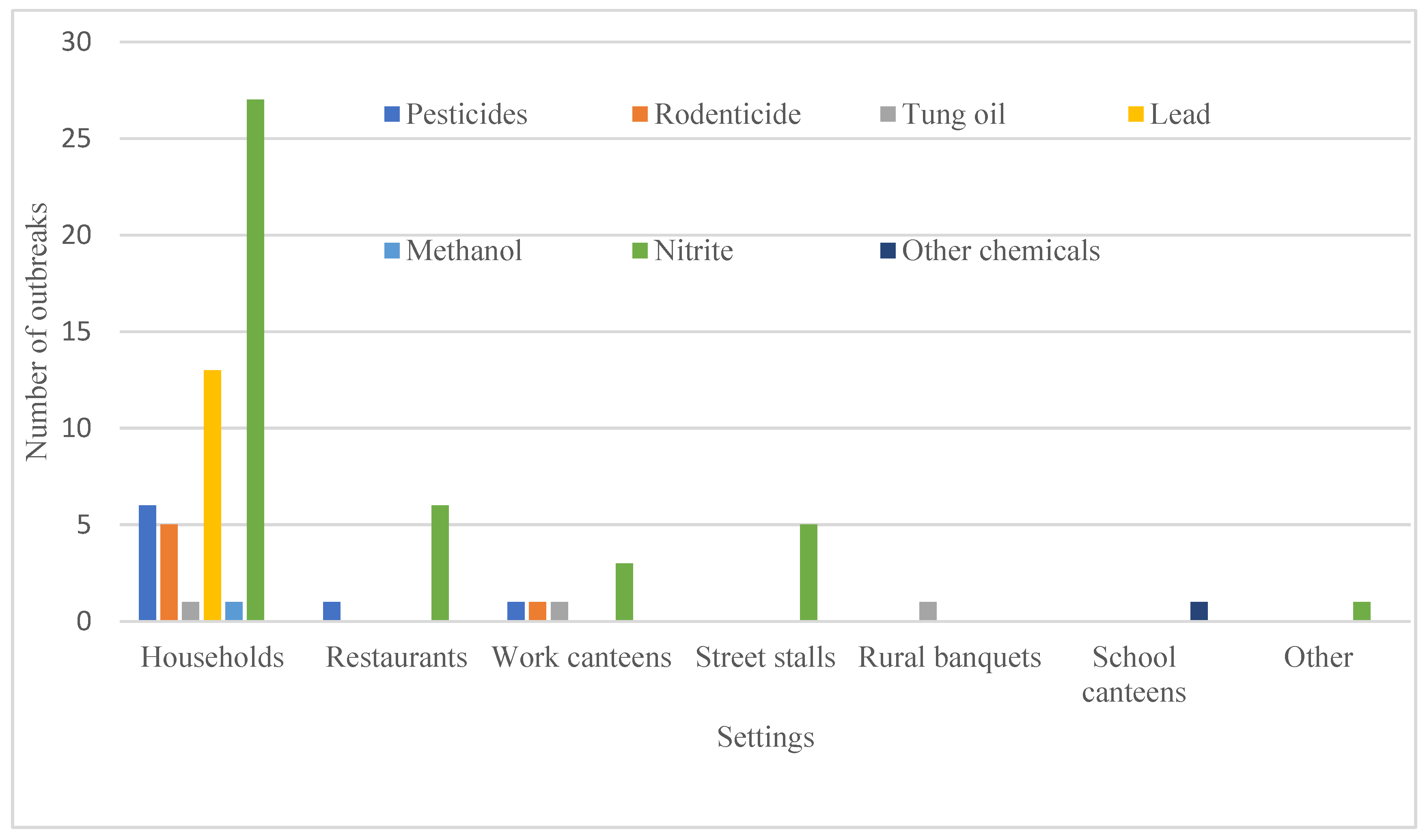
3.4. Setting
3.5. Food
3.6. Etiology
3.7. Chemical FBDOs Caused by Nitrite
3.8. Chemical FBDOs Caused by Lead
3.9. Chemical FBDOs Caused by Other Etiologies
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Food Safety. Available online: https://www.who.int/news-room/fact-sheets/detail/food-safety (accessed on 7 April 2021).
- World Health Organization. WHO Estimates of the Global Burden of Foodborne Diseases: Foodborne Disease Burden Epidemiology Reference Group 2007–2015. 2015. Available online: https://apps.who.int/iris/bitstream/handle/10665/199350/9789241565165_eng.pdf;jsessionid=697B7265BD372CBF07E0013D9FAAB585?sequence=1 (accessed on 7 April 2021).
- Jaffee, S.; Henson, S.; Unnevehr, L.; Grace, D.; Cassou, E. The Safe Food Imperative: Accelerating Progress in Low- and Middle-Income Countries; Agriculture and Food Series; World Bank. ©: Washington, DC, USA, 2019; Available online: https://openknowledge.worldbank.org/handle/10986/30568 (accessed on 2 March 2025).
- Rather, I.A.; Koh, W.Y.; Paek, W.K.; Lim, J. The Sources of Chemical Contaminants in Food and Their Health Implications. Front. Pharmacol. 2017, 8, 830. [Google Scholar] [CrossRef] [PubMed]
- Yorifuji, T.; Tsuda, T.; Harada, M. Minamata disease: A challenge for democracy and justice. In Late Lessons from Early Warnings: Science, Precaution, Innovation; European Environment Agency: Copenhagen, Denmark, 2013; pp. 124–152. [Google Scholar]
- Harada, M. Minamata disease: Methylmercury poisoning in Japan caused by environmental pollution. Crit. Rev. Toxicol. 1995, 25, 1–24. [Google Scholar] [CrossRef] [PubMed]
- Yorifuji, T.; Tsuda, T.; Takao, S.; Harada, M. Long-term exposure to methylmercury and neurologic signs in Minamata and neighboring communities. Epidemiology 2008, 19, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Harada, M. Congenital Minamata disease: Intrauterine methylmercury poisoning. Teratology 1978, 18, 285–288. [Google Scholar] [CrossRef]
- Eto, K. Minamata disease. Neuropathology 2000, 20, S14–S19. [Google Scholar] [CrossRef]
- Bakir, F.; Damluji, S.F.; Amin-Zaki, L.; Murtadha, M.; Khalidi, A.; Al-Rawi, N.Y.; Tikriti, S.; Dhahir, H.I.; Clarkson, T.W.; Smith, J.C.; et al. Methylmercury poisoning in Iraq. Science 1973, 181, 230–241. [Google Scholar] [CrossRef]
- Goldman, L.R.; Smith, D.F.; Neutra, R.R.; Saunders, L.D.; Pond, E.M.; Stratton, J.; Waller, K.; Jackson, R.J.; Kizer, K.W. Pesticide food poisoning from contaminated watermelons in California, 1985. Arch. Environ. Health 1990, 45, 229–236. [Google Scholar] [CrossRef] [PubMed]
- Gautami, S.; Rao, R.N.; Raghuram, T.C.; Rajagopalan, S.; Bhat, R.V. Accidental Acute Fatal Sodium Nitrite Poisoning. J. Toxicol. Clin. Toxicol. 1995, 33, 131–133. [Google Scholar] [CrossRef]
- Beligaswatte, A.M.; Kularatne, S.A.; Seneviratne, A.B.; Wijenayake, M.S.P.; Kularatne, W.K.; Pathirage, L.M. An outbreak of fatal pneumonitis caused by contamination of illicit alcohol with paraquat. Clin. Toxicol. 2008, 46, 768–770. [Google Scholar] [CrossRef]
- Idrovo, A.J. Food poisoned with pesticide in Bihar, India: New disaster, same story. Occup. Environ. Med. 2013, 71, 228. [Google Scholar] [CrossRef]
- Handley, M.A.; Hall, C.; Sanford, E.; Diaz, E.; Gonzalez-Mendez, E.; Drace, K.; Wilson, R.; Croughan, M. Globalization, Binational Communities, and Imported Food Risks: Results of an Outbreak Investigation of Lead Poisoning in Monterey County, California. Am. J. Public Health 2007, 97, 900–906. [Google Scholar] [CrossRef] [PubMed]
- Woolf, A.D. Childhood Lead Poisoning in 2 Families Associated with Spices Used in Food Preparation. Pediatrics 2005, 116, e314–e318. [Google Scholar] [CrossRef] [PubMed]
- Tabaku, A.; Panariti, E. Lead intoxication in rural Albania. Vet. Hum. Toxicol. 1996, 38, 434–435. [Google Scholar] [PubMed]
- Bai, L.; Liu, J.K.; Li, W.W.; Fu, P.; Li, N.; Liu, X.M.; Guo, Y. Comparison of foodborne disease surveillance systems in China and the U.S. Cap. J. Public Health 2018, 12, 62–66. [Google Scholar]
- World Health Organization. Foodborne Disease Outbreaks: Guidelines for Investigation and Control; World Health Organization: Geneva, Switzerland, 2008; Available online: https://www.who.int/publications/i/item/9789241547222 (accessed on 15 January 2025).
- World Health Organization. Strengthening Surveillance of and Response to Foodborne Diseases: A Practical Manual. Introductory Module; World Health Organization: Geneva, Switzerland, 2017; Available online: https://www.who.int/publications/i/item/9789241513234 (accessed on 11 July 2024).
- Ministry of Health of China. Diagnostic Criteria and Principles of Management for Food Poisoning. 1996. Available online: http://down.foodmate.net/ (accessed on 11 July 2024).
- Ministry of Health of China. Norms for Epidemiological Investigation of Food Safety Accidents. 2011. Available online: http://www.nhc.gov.cn/wjw/gfxwj/201304/2ff1616ba26140bd94616ff65f61fa4b.shtml (accessed on 27 May 2024).
- Ministry of Health of China. Technical Guidelines for Epidemiological Investigation of Food Safety Accidents. 2012. Available online: http://www.nhc.gov.cn/sps/s3594/201206/f6704ce99c66438b832771b12aa0a903.shtml (accessed on 27 May 2024).
- Zhejiang Provincial Bureau of Statistics. Available online: http://tjj.zj.gov.cn/ (accessed on 15 January 2025).
- Cui, Y.; Liang, X.C. Analysis of chemical foodborne disease outbreaks in Gansu Province from 2011 to 2015. Cap. Public Health 2017, 11, 165–166. [Google Scholar]
- Xu, L.Z.; Jin, S.H. Epidemiological analysis of chemical foodborne disease outbreaks in Anhui Province from 2010 to 2016. Anhui J. Prev. Med. 2017, 23, 268–270+274. [Google Scholar]
- Li, H.Q.; Guo, Y.C.; Song, Z.Z.; Ma, Y.; Lu, D.; Yuan, X.; Guo, W.; Zhou, J.; Liu, J.; Li, W.; et al. Analysis of foodborne disease outbreaks in China in 2019. Chin. J. Food Hyg. 2021, 33, 650–656. [Google Scholar]
- Harper, C.; Keith, S.; Todd, G.D.; Williams, M. Toxicological Profile for Nitrate and Nitrite; Agency for Toxic Substances and Disease Registry: Atlanta, GA, USA, 2017. Available online: https://www.ncbi.nlm.nih.gov/books/NBK592476/ (accessed on 2 March 2025).
- PubChem. Compound Summary for CID 23668193, Sodium Nitrite; National Library of Medicine (US), National Center for Biotechnology Information: Bethesda, MD, USA, 2004. Available online: https://pubchem.ncbi.nlm.nih.gov/compound/Sodium-nitrite (accessed on 2 March 2025).
- Hwang, C.; Yeon, S.-H.; Jung, J.; Na, J.-Y. An autopsy case of sodium nitrite-induced methemoglobinemia with various post-mortem analyses. Forensic Sci. Med. Pathol. 2021, 17, 475–480. [Google Scholar] [CrossRef]
- Gladwin, M.T. Evidence Mounts That Nitrite Contributes to Hypoxic Vasodilation in the Human Circulation. Circulation 2008, 117, 594–597. [Google Scholar] [CrossRef]
- McCann, S.D.; Tweet, M.S.; Wahl, M.S. Rising incidence and high mortality in intentional sodium nitrite exposures reported to US poison centers. Clin. Toxicol. 2021, 59, 1264–1269. [Google Scholar] [CrossRef]
- Bebarta, V.S.; Brittain, M.; Chan, A.; Garrett, N.; Yoon, D.; Burney, T.; Mukai, D.; Babin, M.; Pilz, R.B.; Mahon, S.B.; et al. Sodium Nitrite and Sodium Thiosulfate Are Effective Against Acute Cyanide Poisoning When Administered by Intramuscular Injection. Ann. Emerg. Med. 2017, 69, 718–725.e4. [Google Scholar] [CrossRef] [PubMed]
- Tusiewicz, K.; Kuropka, P.; Workiewicz, E.; Wachełko, O.; Szpot, P.; Zawadzki, M. Nitrites: An Old Poison or a Current Hazard? Epidemiology of Intoxications Covering the Last 100 Years and Evaluation of Analytical Methods. Toxics 2023, 11, 832. [Google Scholar] [CrossRef]
- Lee, C.; Jang, E.J.; Yum, H.; Choi, Y.S.; Hong, J. Unintentional mass sodium nitrite poisoning with a fatality. Clin. Toxicol. 2017, 55, 678–679. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.; Teng, C.G.; Zhang, N.; Zhang, J.; Conway, G. A family cluster of nitrite poisoning, Suzhou City, Jiangsu Province, China, 2013. West. Pac. Surveill. Response J. 2013, 4, 33–36. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Methemoglobinemia following unintentional ingestion of sodium nitrite–New York, 2002. MMWR Morb. Mortal Wkly. Rep. 2002, 51, 639–642. [Google Scholar]
- O’Neill, C.; Najjar, Z.; Ingleton, A.; Edwards, A.; Dawson, A.; Gupta, L. Methaemoglobinaemia associated with the atypical use of sodium nitrite as a food additive. Med. J. Aust. 2021, 215, 256–257.e1. [Google Scholar] [CrossRef]
- Tung, S.P.; How, C.K.; Chern, C.H. Methaemoglobinaemia Secondary to the Ingestion of Sodium Nitrite in Mistake for Common Salt. Resuscitation 2006, 70, 168–169. [Google Scholar] [CrossRef]
- Chen, W.; Zhang, Y. Epidemiological analysis of chemical foodborne disease outbreaks in Sichuan, 2010–2016. Mod. Prev. Med. 2018, 45, 2305–2308+2323. [Google Scholar]
- Honikel, K.-O. The use and control of nitrate and nitrite for the processing of meat products. Meat Sci. 2008, 78, 68–76. [Google Scholar] [CrossRef]
- Marco, A.; Navarro, J.L.; Flores, M. The influence of nitrite and nitrate on microbial, chemical and sensory parameters of slow dry fermented sausage. Meat Sci. 2006, 73, 660–673. [Google Scholar] [CrossRef]
- Vidal, V.A.S.; Lorenzo, J.M.; Munekata, P.E.S.; Pollonio, M.A.R. Challenges to reduce or replace NaCl by chloride salts in meat products made from whole pieces—A review. Crit. Rev. Food Sci. Nutr. 2020, 61, 2194–2206. [Google Scholar] [CrossRef]
- Pegg, R.B.; Honikel, K.O. Principles of curing. In Handbook of Fermented Meat and Poultry; Toldrá, F., Hui, Y.H., Astiasarán, I., Sebranek, J.G., Talon, R., Eds.; Wiley: Hoboken, NJ, USA, 2014; pp. 19–30. [Google Scholar] [CrossRef]
- Cvetković, D.; Živković, V.; Lukić, V.; Nikolić, S. Sodium nitrite food poisoning in one family. Forensic Sci. Med. Pathol. 2018, 15, 102–105. [Google Scholar] [CrossRef]
- Maric, P.; Ali, S.S.; Heron, L.G.; Rosenfeld, D.; Greenwood, M. Methaemoglobinaemia following ingestion of a commonly available food additive. Med. J. Aust. 2008, 188, 156–158. [Google Scholar] [CrossRef] [PubMed]
- State Administration for Market Regulation. The Announcement of Prohibition of Nitrite by Food Service Providers and the Strengthening of Alcohol-Based Fuel Management (No. 18, 2018). 2018. Available online: https://amr.ahsz.gov.cn/ztzl/gg/194271661.html (accessed on 7 April 2024).
- Yu, Y.; Yu, Y.; Xu, Z. Evaluation of Nitrite, Ethyl Carbamate, and Biogenic Amines in Four Types of Fermented Vegetables. Foods 2021, 10, 3150. [Google Scholar] [CrossRef] [PubMed]
- Tang, T.; Zhang, M.; Law, C.L.; Mujumdar, A.S. Novel strategies for controlling nitrite content in prepared dishes: Current status, potential benefits, limitations and future challenges. Food Res. Int. 2023, 170, 112984. [Google Scholar] [CrossRef] [PubMed]
- Gräf, M.; Stangl, R.; Hood-Nowotny, R.; Kodym, A. Urban farming in indoor settings: Nitrate limits compliance check of leafy green vegetables under LED lighting. Eur. J. Hortic. Sci. 2020, 85, 321–328. [Google Scholar] [CrossRef]
- Santamaria, P. Nitrate in vegetables: Toxicity, content, intake and EC regulation. J. Sci. Food Agric. 2005, 86, 10–17. [Google Scholar] [CrossRef]
- Chan, T.Y. Vegetable-borne nitrate and nitrite and the risk of methaemoglobinaemia. Toxicol. Lett. 2011, 200, 107–108. [Google Scholar] [CrossRef]
- Cintya, H.; Silalahi, J.; De Lux Putra, E.; Siburian, R. The influence of storage condition on nitrite, nitrate and vitamin C levels in vegetables. F1000Research 2018, 7, 1899. [Google Scholar] [CrossRef]
- Han, L.Y.; Chen, H.Y.; Hang, S.P. Study on the growth rule of nitrite in pickled vegetable. J. Shangrao Norm. Coll. 2007, 27, 56–59. [Google Scholar]
- Hou, J.C.; Jiang, C.G.; Long, Z.C. Nitrite level of pickled vegetables in Northeast China. Food Control 2013, 29, 7–10. [Google Scholar] [CrossRef]
- Sun, D.; Zhu, B.; Zhang, Y.; Cai, G.; Xia, J. Study on discovering and eliminating lead poisoning of tin pot in mass crowds in Rudong county. Chin. J. Public Health Manag. 2017, 33, 465–468. [Google Scholar]
- Cai, J.; Yang, X. Investigation on lead poisoning caused by drinking yellow rice wine in tin pot. Mod. Prev. Med. 2005, 32, 169. [Google Scholar]
- Wang, J.; El-Fahmawi, A.; Yan, C.; Liu, J. Childhood lead poisoning from domestic products in China: A case study with implications for practice, education, and policy. Public Health Nurs. 2019, 36, 806–812. [Google Scholar] [CrossRef]
- GB/T 13662-2018; Yellow Rice Wine. State Administration for Market Regulation, Standardization Administration: Beijing, China, 2019. Available online: http://down.foodmate.net/standard/sort/3/53650.html (accessed on 7 April 2024).
- Han, X.P. Analysis of lead dissolution in the process of wine—Heating in tin pot. Chin. J. Health Lab. Technol. 2017, 27, 2470–2471. [Google Scholar]
- Decree of The State Council of the People’s Republic of China. Pesticide Management Regulations (2022 revision). 2022. Available online: https://baike.baidu.com/item/%E5%86%9C%E8%8D%AF%E7%AE%A1%E7%90%86%E6%9D%A1%E4%BE%8B?fromModule=lemma_search-box (accessed on 15 January 2025).
- Li, X.Y. Investigation on a suspected group food poisoning caused by tung oil ingestion at a family dinner. China Rural Health 2024, 16, 64–65. [Google Scholar]
- Di, M.; Zhang, C.L.; Yin, J.N.; Wang, Z. Analysis of food poisoning caused by accidental consumption of tung oil. Chin. J. Health Lab. 2014, 24, 3636–3637. [Google Scholar]
- Zhao, B.; Ma, G.J. Analysis of causes and prevention strategies of food poisoning in breakfast contaminated by tung oil. World Latest Med. Inf. 2018, 18, 165. [Google Scholar]
- Zheng, L. Cause analysis and preventive measures of food poisoning in a middle school in Taoyuan County. Pract. Prev. Med. 2010, 17, 510–512. [Google Scholar]
| Etiology | Outbreaks | Cases | Hospitalizations | Deaths | Mean Number of Cases per Outbreak | Hospitalizations /Cases × 100% †† | p-Value † | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Number | % | Number | % | Number | % | Number | % | ||||
| Fungi and their toxins | 408 | 21.73 | 1408 | 8.67 | 403 | 20.70 | 20 | 68.97 | 3.5 | 28.62 a | <0.001 |
| Plant toxins | 106 | 5.64 | 631 | 3.88 | 116 | 5.96 | 4 | 13.79 | 6.0 | 18.38 b | |
| Animal toxins | 34 | 1.81 | 241 | 1.48 | 27 | 1.39 | 1 | 3.45 | 7.1 | 11.20 c | |
| Biological * | 784 | 41.75 | 10,277 | 63.27 | 1009 | 51.82 | 3 | 10.34 | 13.1 | 9.82 c | |
| Chemicals ** | 74 | 3.94 | 461 | 2.84 | 209 | 10.73 | 1 | 3.45 | 6.2 | 45.34 d | |
| Unknown etiology | 469 | 24.97 | 3214 | 19.79 | 183 | 9.40 | 0 | 0.00 | 6.9 | 5.69 e | |
| Multiple etiologies | 3 | 0.16 | 11 | 0.07 | 0 | 0.00 | 0 | 0.00 | 3.7 | 0.00 | |
| Total | 1878 | 100.00 | 16,243 | 100.00 | 1947 | 100.00 | 29 | 100.00 | 8.6 | 11.99 | |
| Year | Outbreaks | Cases | Hospitalizations | Hospitalizations/Cases | Deaths | |||
|---|---|---|---|---|---|---|---|---|
| Number | % | Number | % | Number | % | ×100% | ||
| 2011 | 1 | 1.35 | 10 | 2.17 | 0 | 0.00 | 0.00 | 0 |
| 2012 | 6 | 8.11 | 59 | 12.80 | 13 | 6.22 | 22.03 | 0 |
| 2013 | 3 | 4.05 | 38 | 8.24 | 33 | 15.79 | 86.84 | 0 |
| 2014 | 5 | 6.76 | 28 | 6.07 | 19 | 9.09 | 67.86 | 0 |
| 2015 | 5 | 6.76 | 14 | 3.04 | 8 | 3.83 | 57.14 | 0 |
| 2016 | 6 | 8.11 | 26 | 5.64 | 7 | 3.35 | 26.92 | 0 |
| 2017 | 4 | 5.41 | 13 | 2.82 | 9 | 4.31 | 69.23 | 0 |
| 2018 | 6 | 8.11 | 20 | 4.34 | 5 | 2.39 | 25.00 | 0 |
| 2019 | 10 | 13.51 | 129 | 27.98 | 42 | 20.10 | 32.56 | 0 |
| 2020 | 8 | 10.81 | 37 | 8.03 | 20 | 9.57 | 54.05 | 0 |
| 2021 | 9 | 12.16 | 48 | 10.41 | 37 | 17.70 | 77.08 | 0 |
| 2022 | 2 | 2.70 | 5 | 1.08 | 4 | 1.91 | 80.00 | 1 |
| 2023 | 9 | 12.16 | 34 | 7.38 | 12 | 5.74 | 35.29 | 0 |
| Total | 74 | 100.00 | 461 | 100.00 | 209 | 100.00 | 45.34 | 1 |
| Region | Outbreaks | Cases | Hospitalizations | Deaths | Incidence Rates of Cases per Million | p-Value * | |||
|---|---|---|---|---|---|---|---|---|---|
| Number | % | Number | % | Number | % | Number | |||
| Hangzhou | 18 | 24.32 | 68 | 14.72 | 25 | 11.96 | 0 | 9.02 | <0.001 |
| Jinhua | 17 | 22.97 | 60 | 12.99 | 29 | 13.88 | 1 | 12.36 | |
| Wenzhou | 14 | 18.92 | 130 | 28.14 | 48 | 22.97 | 0 | 15.77 | |
| Taizhou | 9 | 12.16 | 41 | 8.87 | 19 | 9.09 | 0 | 6.79 | |
| Ningbo | 6 | 8.11 | 73 | 15.80 | 36 | 17.22 | 0 | 12.23 | |
| Quzhou | 3 | 4.05 | 27 | 5.84 | 17 | 8.13 | 0 | 10.47 | |
| Shaoxing | 3 | 4.05 | 14 | 3.03 | 7 | 3.35 | 0 | 3.14 | |
| Jiaxing | 2 | 2.70 | 14 | 3.03 | 3 | 1.44 | 0 | 3.93 | |
| Huzhou | 1 | 1.35 | 25 | 5.41 | 25 | 11.96 | 0 | 9.39 | |
| Lishui | 1 | 1.35 | 9 | 1.95 | 0 | 0.00 | 0 | 3.34 | |
| Total | 74 | 100.00 | 461 | 99.78 | 209 | 100.00 | 1 | 9.48 | |
| Setting | Outbreaks | Cases | Hospitalizations | Deaths | Hospitalizations/Cases ×100% | Mean Number of Cases per Outbreak | |||
|---|---|---|---|---|---|---|---|---|---|
| Number | % | Number | % | Number | % | Number | |||
| Households | 53 | 71.62 | 202 | 43.82 | 86 | 41.15 | 1 | 42.57 | 4 |
| Restaurants | 7 | 9.46 | 66 | 14.32 | 44 | 21.05 | 0 | 66.67 | 9 |
| Work canteens | 6 | 8.11 | 125 | 27.11 | 61 | 29.19 | 0 | 48.80 | 21 |
| Street stalls | 5 | 6.76 | 28 | 6.07 | 16 | 7.66 | 0 | 57.14 | 6 |
| Rural banquets | 1 | 1.35 | 12 | 2.60 | 2 | 0.96 | 0 | 16.67 | 12 |
| School canteens | 1 | 1.35 | 18 | 3.90 | 0 | 0.00 | 0 | 0.00 | 18 |
| Other | 1 | 1.35 | 10 | 2.17 | 0 | 0.00 | 0 | 0.00 | 10 |
| Total | 74 | 100.00 | 461 | 100.00 | 209 | 100.00 | 1 | 45.34 | 6 |
| Food | Outbreaks | Cases | Hospitalizations | Deaths Number | 100 × Hospitalizations/Cases (%) | p-Value ** | |||
|---|---|---|---|---|---|---|---|---|---|
| Number | % | Number | % | Number | % | ||||
| Non-food (nitrite) | 25 | 33.78 | 187 | 40.56 | 95 | 45.45 | 1 | 50.80 a | <0.001 |
| Liquor | 13 | 17.57 | 43 | 9.33 | 19 | 9.09 | 0 | 44.19 a, d | |
| Vegetable (pickle) | 11 | 14.86 | 30 | 6.51 | 11 | 5.26 | 0 | 36.67 a, d | |
| Other cooking vegetables | 8 | 10.81 | 57 | 12.36 | 30 | 14.35 | 0 | 52.63 a | |
| Grain product | 4 | 5.41 | 42 | 9.11 | 33 | 15.79 | 0 | 78.57 b | |
| Cooked meat | 5 | 6.76 | 30 | 6.51 | 13 | 6.22 | 0 | 43.33 a, d | |
| Non-food (Tung oil) | 3 | 4.05 | 35 | 7.59 | 2 | 0.96 | 0 | 5.71 c | |
| Water | 2 | 2.70 | 12 | 2.60 | 2 | 0.96 | 0 | 16.67 d, e, c | |
| Fruit | 1 | 1.35 | 5 | 1.08 | 3 | 1.44 | 0 | 60.00 a, b, e | |
| Vegetable oil | 1 | 1.35 | 18 | 3.90 | 0 | 0.00 | 0 | 0.00 c | |
| Unidentified food | 1 | 1.35 | 2 | 0.43 | 1 | 0.48 | 0 | 50.00 | |
| Total | 74 | 100.00 | 461 | 100.00 | 209 | 100.00 | 1 | 45.34 | |
| Etiology | Outbreaks | Cases | Hospitalizations | Deaths Number | |||
|---|---|---|---|---|---|---|---|
| Number | % | Number | % | Number | % | ||
| Nitrite | 42 | 56.76 | 284 | 61.61 | 140 | 66.99 | 1 |
| Lead | 13 | 17.57 | 43 | 9.33 | 20 | 9.57 | 0 |
| Pesticides | 8 | 10.81 | 59 | 12.80 | 30 | 14.35 | 0 |
| Rodenticides | 6 | 8.11 | 20 | 4.34 | 16 | 7.66 | 0 |
| Tung oil | 3 | 4.05 | 35 | 7.59 | 2 | 0.96 | 0 |
| Methanol | 1 | 1.35 | 2 | 0.43 | 1 | 0.48 | 0 |
| Other chemicals | 1 | 1.35 | 18 | 3.90 | 0 | 0.00 | 0 |
| Total | 74 | 100.00 | 461 | 100.00 | 209 | 100.00 | 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, L.; Chen, J.; Wang, J.; Qi, X.; Zhang, H.; He, Y.; Zhang, R. Surveillance of Chemical Foodborne Disease Outbreaks in Zhejiang Province, China, 2011–2023. Foods 2025, 14, 936. https://doi.org/10.3390/foods14060936
Chen L, Chen J, Wang J, Qi X, Zhang H, He Y, Zhang R. Surveillance of Chemical Foodborne Disease Outbreaks in Zhejiang Province, China, 2011–2023. Foods. 2025; 14(6):936. https://doi.org/10.3390/foods14060936
Chicago/Turabian StyleChen, Lili, Jiang Chen, Jikai Wang, Xiaojuan Qi, Hexiang Zhang, Yue He, and Ronghua Zhang. 2025. "Surveillance of Chemical Foodborne Disease Outbreaks in Zhejiang Province, China, 2011–2023" Foods 14, no. 6: 936. https://doi.org/10.3390/foods14060936
APA StyleChen, L., Chen, J., Wang, J., Qi, X., Zhang, H., He, Y., & Zhang, R. (2025). Surveillance of Chemical Foodborne Disease Outbreaks in Zhejiang Province, China, 2011–2023. Foods, 14(6), 936. https://doi.org/10.3390/foods14060936







