Impact of COVID-19 Vaccination Status and Confidence on Dietary Practices among Chinese Residents
Abstract
:1. Introduction
2. Materials and Methods
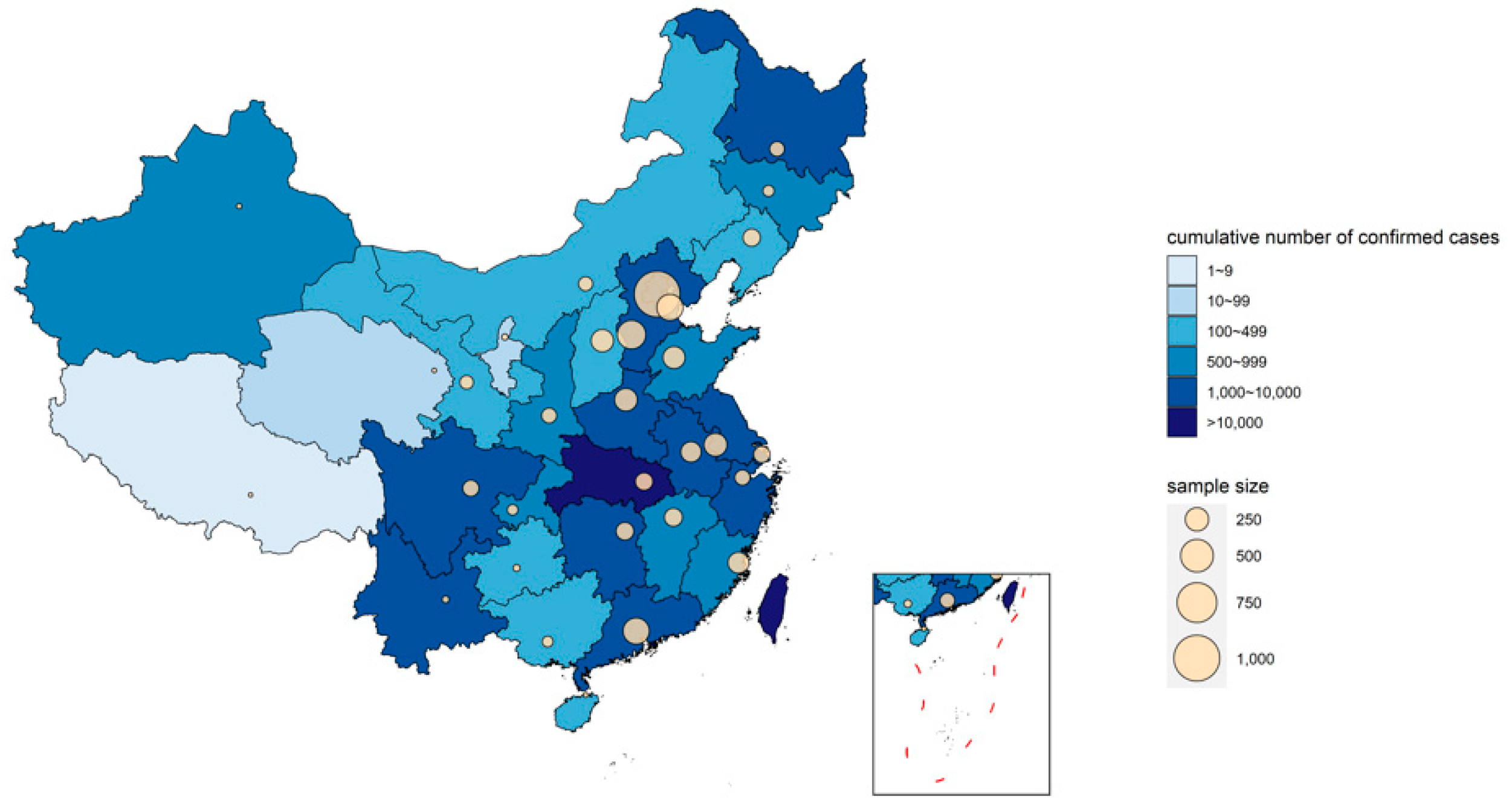
2.1. Study Design and Participants
2.2. Data Collection
2.3. Ethics
2.4. Statistical Analysis
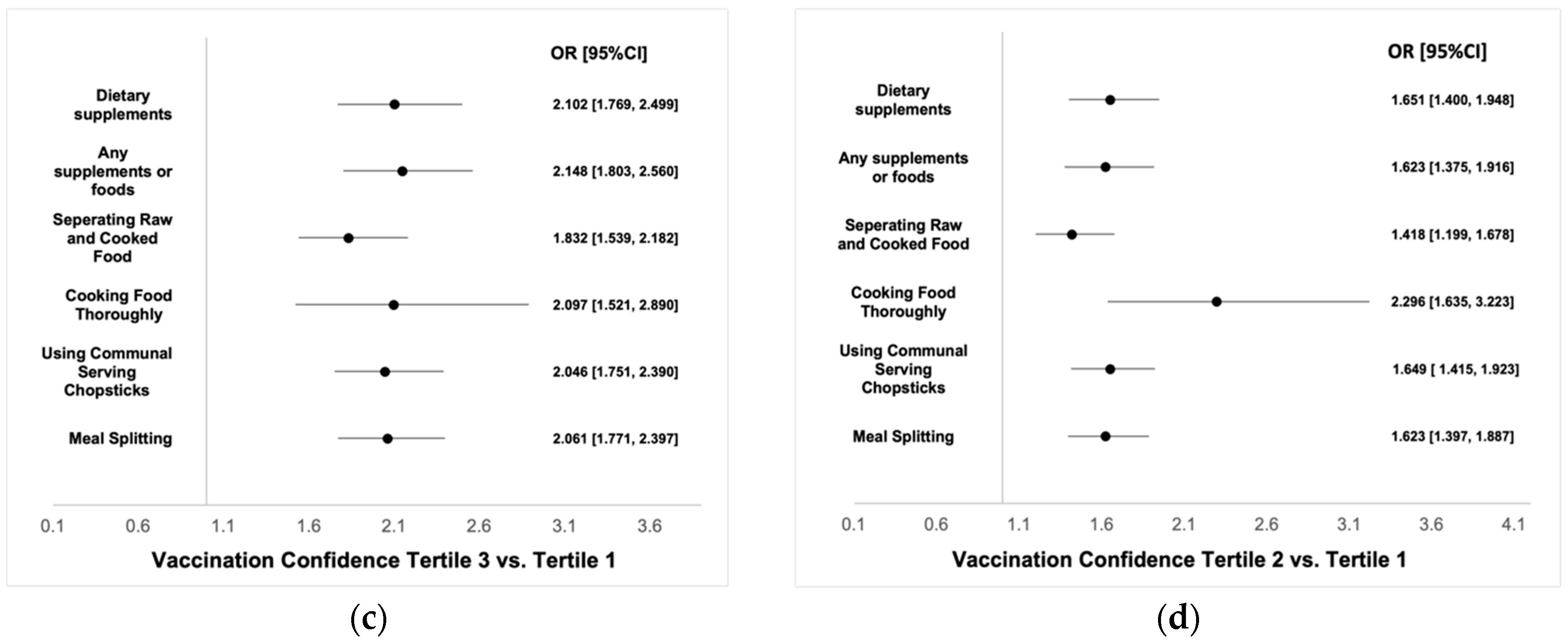
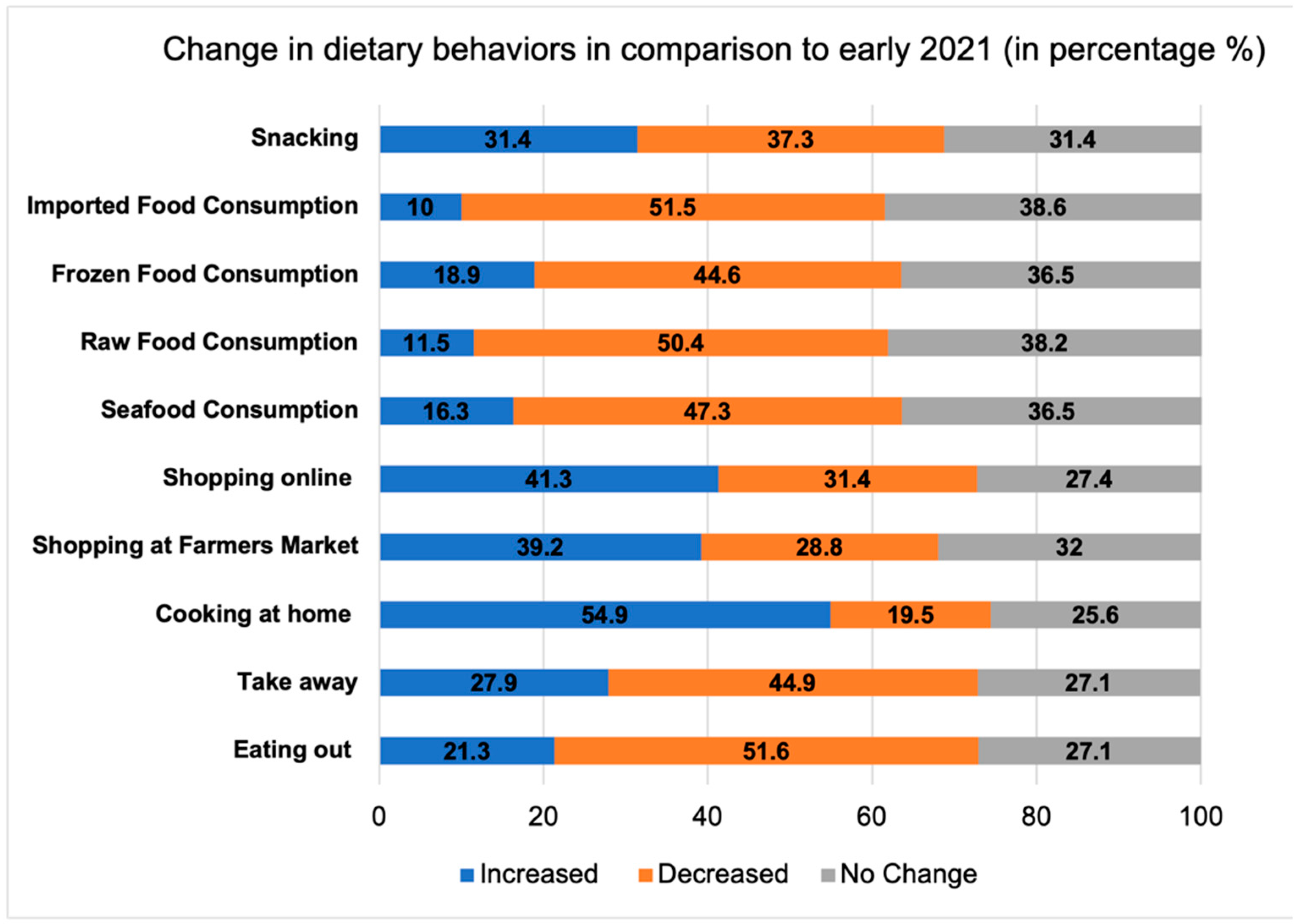
3. Results
4. Discussion
4.1. Dietary Diversity
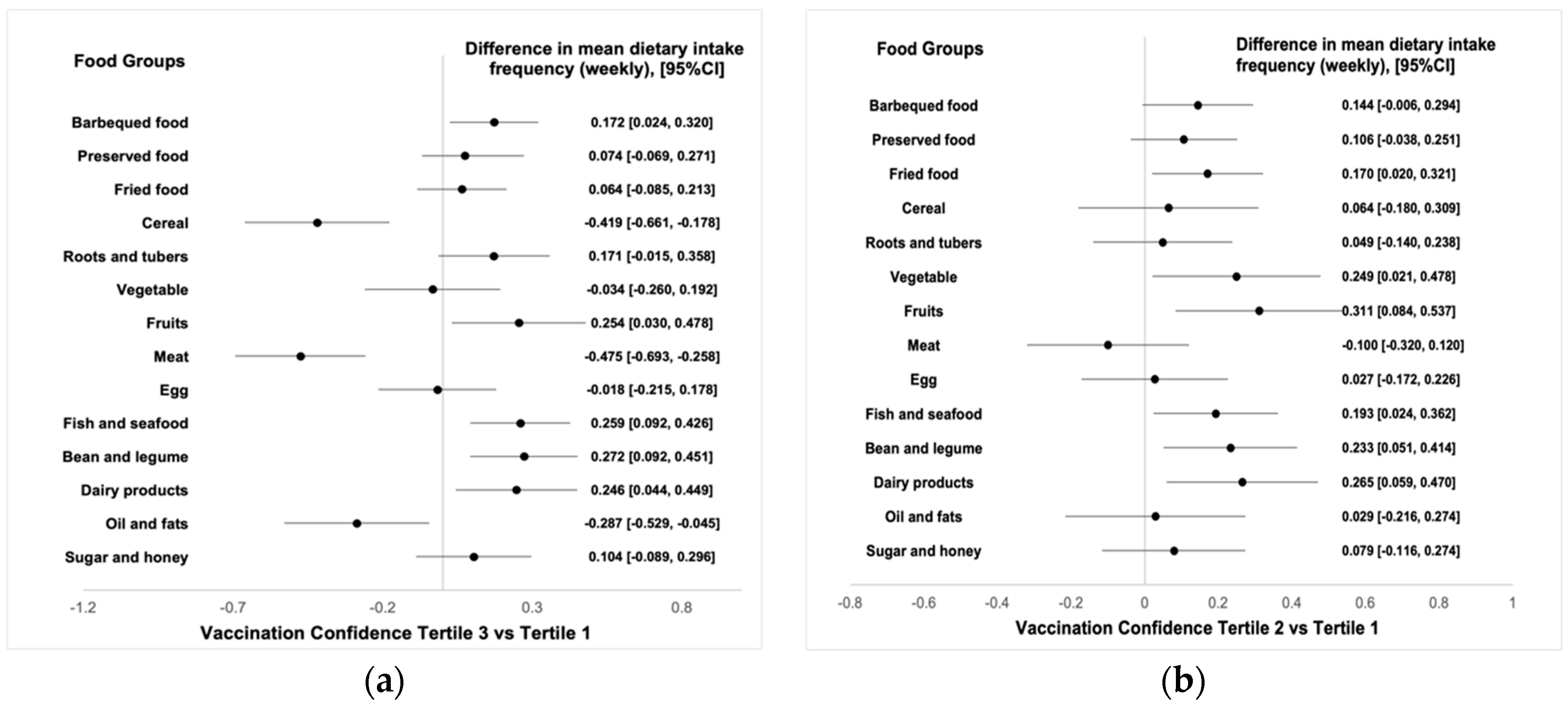
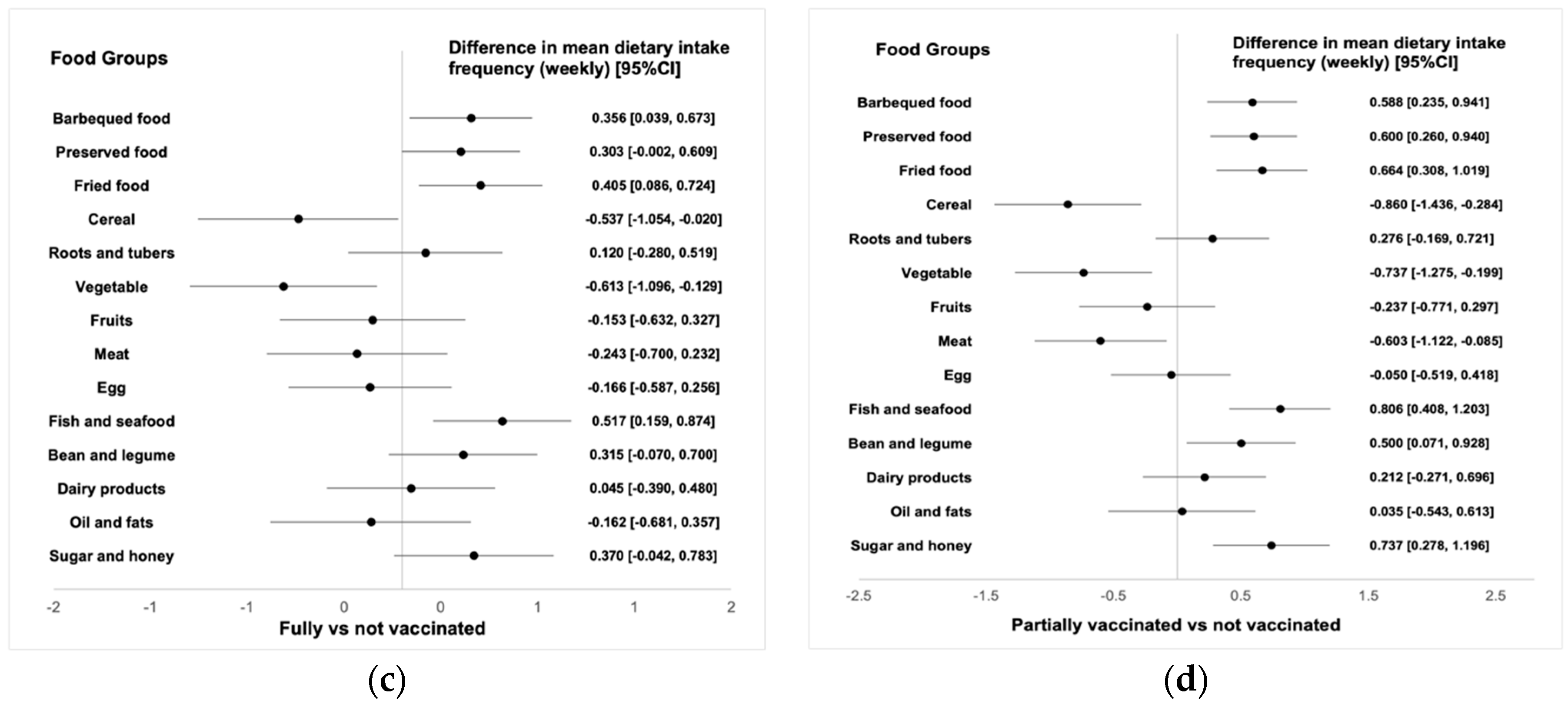
4.2. Dietary Intake Frequency
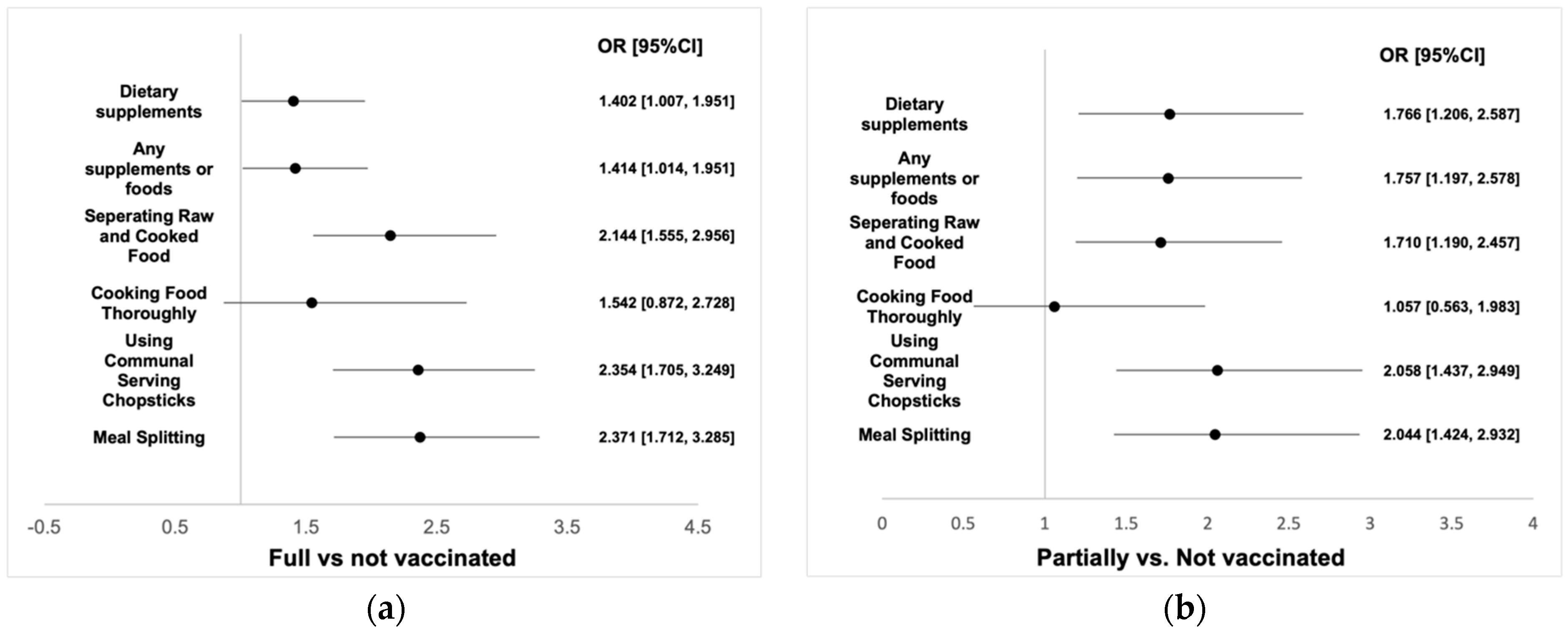
4.3. Other Dietary Behaviors and Changes in Comparison to Early 2021
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Boni, M.F.; Lemey, P.; Jiang, X.; Lam, T.T.; Perry, B.W.; Castoe, T.A.; Rambaut, A.; Robertson, D.L. Evolutionary origins of the SARS-CoV-2 sarbecovirus lineage responsible for the COVID-19 pandemic. Nat. Microbiol. 2020, 5, 1408–1417. [Google Scholar] [CrossRef] [PubMed]
- Johns Hopkins University. COVID-19 Dashboard. Available online: https://coronavirus.jhu.edu/map.html (accessed on 3 March 2022).
- Shivalkar, S.; Pingali, M.S.; Verma, A.; Singh, A.; Singh, V.; Paital, B.; Das, D.; Varadwaj, P.K.; Samanta, S.K. Outbreak of COVID-19: A Detailed Overview and Its Consequences. Adv. Exp. Med. Biol. 2021, 1353, 23–45. [Google Scholar] [CrossRef] [PubMed]
- Chakraborty, I.; Maity, P. COVID-19 outbreak: Migration, effects on society, global environment and prevention. Sci. Total Environ. 2020, 728, 138882. [Google Scholar] [CrossRef] [PubMed]
- Moore, J.P.; Klasse, P.J. COVID-19 Vaccines: “Warp Speed” Needs Mind Melds, Not Warped Minds. J. Virol. 2020, 94, e01083-20. [Google Scholar] [CrossRef] [PubMed]
- Amanat, F.; Krammer, F. SARS-CoV-2 Vaccines: Status Report. Immunity 2020, 52, 583–589. [Google Scholar] [CrossRef]
- Ritchie, H.; Ortiz-Ospina, E.; Beltekian, D.; Mathieu, E.; Hasell, J.; Macdonald, B.; Giattino, C.; Appel, C.; Rodés-Guirao, L.; Roser, M. Coronavirus (COVID-19) Vaccinations. Available online: https://ourworldindata.org/coronavirus (accessed on 12 March 2022).
- Maragakis, L. Coronavirus Second Wave, Third Wave and Beyond: What Causes a COVID Surge. Available online: https://www.hopkinsmedicine.org/health/conditions-and-diseases/coronavirus/first-and-second-waves-of-coronavirus (accessed on 12 March 2022).
- Dennis, P. International Update: Covid Infections Surge World Wide. Available online: https://www.pharmaceutical-technology.com/special-focus/covid-19/international-update-covid-infections-surge-world-wide/ (accessed on 12 March 2022).
- Bennett, G.; Young, E.; Butler, I.; Coe, S. The Impact of Lockdown During the COVID-19 Outbreak on Dietary Habits in Various Population Groups: A Scoping Review. Front. Nutr. 2021, 8, 626432. [Google Scholar] [CrossRef]
- Di Renzo, L.; Gualtieri, P.; Pivari, F.; Soldati, L.; Attina, A.; Cinelli, G.; Leggeri, C.; Caparello, G.; Barrea, L.; Scerbo, F.; et al. Eating habits and lifestyle changes during COVID-19 lockdown: An Italian survey. J. Transl. Med. 2020, 18, 229. [Google Scholar] [CrossRef]
- Filip, R.; Anchidin-Norocel, L.; Gheorghita, R.; Savage, W.K.; Dimian, M. Changes in Dietary Patterns and Clinical Health Outcomes in Different Countries during the SARS-CoV-2 Pandemic. Nutrients 2021, 13, 3612. [Google Scholar] [CrossRef]
- Grashuis, J.; Skevas, T.; Segovia, M.S. Grocery Shopping Preferences during the COVID-19 Pandemic. Sustainability 2020, 12, 5369. [Google Scholar] [CrossRef]
- Rummo, P.E.; Naik, R.; Thorpe, L.E.; Yi, S.S. Changes in diet and food shopping behaviors among Asian-American adults due to COVID-19. Obes. Sci. Pr. 2021, 7, 307–320. [Google Scholar] [CrossRef]
- Ruiz-Roso, M.B.; Knott-Torcal, C.; Matilla-Escalante, D.C.; Garcimartin, A.; Sampedro-Nunez, M.A.; Davalos, A.; Marazuela, M. COVID-19 Lockdown and Changes of the Dietary Pattern and Physical Activity Habits in a Cohort of Patients with Type 2 Diabetes Mellitus. Nutrients 2020, 12, 2327. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Zhao, A.; Li, J.; Ke, Y.; Huo, S.; Ma, Y. Food and Nutrition Related Concerns Post Lockdown during COVID-19 Pandemic and Their Association with Dietary Behaviors. Foods 2021, 10, 2858. [Google Scholar] [CrossRef] [PubMed]
- Dicken, S.J.; Mitchell, J.J.; Le Vay, J.N.; Beard, E.; Kale, D.; Herbec, A.; Shahab, L. Impact of COVID-19 pandemic on diet behaviour among UK adults: A longitudinal analysis of the HEBECO study. Front. Nutr. 2021, 8, 1102. [Google Scholar] [CrossRef] [PubMed]
- Kumar, P.; Kumar, M.; Bedi, O.; Gupta, M.; Kumar, S.; Jaiswal, G.; Rahi, V.; Yedke, N.G.; Bijalwan, A.; Sharma, S.; et al. Role of vitamins and minerals as immunity boosters in COVID-19. Inflammopharmacology 2021, 29, 1001–1016. [Google Scholar] [CrossRef]
- Alexander, J.; Tinkov, A.; Strand, T.A.; Alehagen, U.; Skalny, A.; Aaseth, J. Early Nutritional Interventions with Zinc, Selenium and Vitamin D for Raising Anti-Viral Resistance Against Progressive COVID-19. Nutrients 2020, 12, 2358. [Google Scholar] [CrossRef]
- Childs, C.E.; Calder, P.C.; Miles, E.A. Diet and Immune Function. Nutrients 2019, 11, 1933. [Google Scholar] [CrossRef] [Green Version]
- Mortaz, E.; Bezemer, G.; Alipoor, S.D.; Varahram, M.; Mumby, S.; Folkerts, G.; Garssen, J.; Adcock, I.M. Nutritional Impact and Its Potential Consequences on COVID-19 Severity. Front. Nutr. 2021, 8, 698617. [Google Scholar] [CrossRef]
- Shakoor, H.; Feehan, J.; Al Dhaheri, A.S.; Ali, H.I.; Platat, C.; Ismail, L.C.; Apostolopoulos, V.; Stojanovska, L. Immune-boosting role of vitamins D, C, E, zinc, selenium and omega-3 fatty acids: Could they help against COVID-19? Maturitas 2021, 143, 1–9. [Google Scholar] [CrossRef]
- Kim, H.; Rebholz, C.M.; Hegde, S.; LaFiura, C.; Raghavan, M.; Lloyd, J.F.; Cheng, S.; Seidelmann, S.B. Plant-based diets, pescatarian diets and COVID-19 severity: A population-based case-control study in six countries. BMJ Nutr. Prev. Health 2021, 4, 257–266. [Google Scholar] [CrossRef]
- Crooke, S.N.; Ovsyannikova, I.G.; Poland, G.A.; Kennedy, R.B. Immunosenescence: A systems-level overview of immune cell biology and strategies for improving vaccine responses. Exp. Gerontol. 2019, 124, 110632. [Google Scholar] [CrossRef]
- Zimmermann, P.; Curtis, N. Factors That Influence the Immune Response to Vaccination. Clin. Microbiol. Rev. 2019, 32, e00084-18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhao, A.; Li, Z.; Ke, Y.; Huo, S.; Ma, Y.; Zhang, Y.; Zhang, J.; Ren, Z. Dietary Diversity among Chinese Residents during the COVID-19 Outbreak and Its Associated Factors. Nutrients 2020, 12, 1699. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Zhao, A.; Ke, Y.; Huo, S.; Ma, Y.; Zhang, Y.; Ren, Z.; Li, Z.; Liu, K. Dietary Behaviors in the Post-Lockdown Period and Its Effects on Dietary Diversity: The Second Stage of a Nutrition Survey in a Longitudinal Chinese Study in the COVID-19 Era. Nutrients 2020, 12, 3269. [Google Scholar] [CrossRef] [PubMed]
- The Distribution of COVID-19. Available online: https://2019ncov.chinacdc.cn/2019-nCoV/. (accessed on 24 March 2022).
- Swindale, A.; Bilinsky, P. Household Dietary Diversity Score (HDDS) for Measurement of Household Food Access: Indicator Guide; Food and Nutrition Technical Assistance Project; Academy for Educational Development: Washington, DC, USA, 2006. [Google Scholar]
- Zhou, B.F. Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults--study on optimal cut-off points of body mass index and waist circumference in Chinese adults. Biomed. Environ. Sci. 2002, 15, 83–96. [Google Scholar]
- Mirmiran, P.; Azadbakht, L.; Azizi, F. Dietary diversity within food groups: An indicator of specific nutrient adequacy in Tehranian women. J. Am. Coll. Nutr. 2006, 25, 354–361. [Google Scholar] [CrossRef]
- Rathnayake, K.M.; Madushani, P.; Silva, K. Use of dietary diversity score as a proxy indicator of nutrient adequacy of rural elderly people in Sri Lanka. BMC Res. Notes 2012, 5, 469. [Google Scholar] [CrossRef] [Green Version]
- Muscogiuri, G.; Barrea, L.; Savastano, S.; Colao, A. Nutritional recommendations for CoVID-19 quarantine. Eur. J. Clin. Nutr. 2020, 74, 850–851. [Google Scholar] [CrossRef]
- Naja, F.; Hamadeh, R. Nutrition amid the COVID-19 pandemic: A multi-level framework for action. Eur. J. Clin. Nutr. 2020, 74, 1117–1121. [Google Scholar] [CrossRef] [Green Version]
- Cecchetto, C.; Aiello, M.; Gentili, C.; Ionta, S.; Osimo, S.A. Increased emotional eating during COVID-19 associated with lockdown, psychological and social distress. Appetite 2021, 160, 105122. [Google Scholar] [CrossRef]
- Boukrim, M.; Obtel, M.; Kasouati, J.; Achbani, A.; Razine, R. Covid-19 and Confinement: Effect on Weight Load, Physical Activity and Eating Behavior of Higher Education Students in Southern Morocco. Ann. Glob. Health 2021, 87, 7. [Google Scholar] [CrossRef]
- Alenko, A.; Agenagnew, L.; Beressa, G.; Tesfaye, Y.; Woldesenbet, Y.M.; Girma, S. COVID-19-Related Anxiety and Its Association with Dietary Diversity Score Among Health Care Professionals in Ethiopia: A Web-Based Survey. J. Multidiscip Healthc. 2021, 14, 987–996. [Google Scholar] [CrossRef] [PubMed]
- Albashir, A.A.D. The potential impacts of obesity on COVID-19. Clin. Med. 2020, 20, e109–e113. [Google Scholar] [CrossRef] [PubMed]
- Andersen, C.J.; Murphy, K.E.; Fernandez, M.L. Impact of Obesity and Metabolic Syndrome on Immunity. Adv. Nutr. 2016, 7, 66–75. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, C.; Han, B.; Zhao, T.; Liu, H.; Liu, B.; Chen, L.; Xie, M.; Liu, J.; Zheng, H.; Zhang, S.; et al. Vaccination willingness, vaccine hesitancy, and estimated coverage at the first round of COVID-19 vaccination in China: A national cross-sectional study. Vaccine 2021, 39, 2833–2842. [Google Scholar] [CrossRef]
- Husain, W.; Ashkanani, F. Does COVID-19 change dietary habits and lifestyle behaviours in Kuwait: A community-based cross-sectional study. Environ. Health Prev. Med. 2020, 25, 61. [Google Scholar] [CrossRef]
- Mendivil, C.O. Dietary Fish, Fish Nutrients, and Immune Function: A Review. Front. Nutr. 2020, 7, 617652. [Google Scholar] [CrossRef]
- Liu, C.; Ralston, N.V.C. Seafood and health: What you need to know? Adv. Food Nutr. Res. 2021, 97, 275–318. [Google Scholar] [CrossRef]
- Redondo-Useros, N.; Nova, E.; Gonzalez-Zancada, N.; Diaz, L.E.; Gomez-Martinez, S.; Marcos, A. Microbiota and Lifestyle: A Special Focus on Diet. Nutrients 2020, 12, 1776. [Google Scholar] [CrossRef]
- Qin, P.; Zhang, M.; Han, M.; Liu, D.; Luo, X.; Xu, L.; Zeng, Y.; Chen, Q.; Wang, T.; Chen, X.; et al. Fried-food consumption and risk of cardiovascular disease and all-cause mortality: A meta-analysis of observational studies. Heart 2021, 107, 1567–1575. [Google Scholar] [CrossRef]
- Parada, H., Jr.; Steck, S.E.; Bradshaw, P.T.; Engel, L.S.; Conway, K.; Teitelbaum, S.L.; Neugut, A.I.; Santella, R.M.; Gammon, M.D. Grilled, Barbecued, and Smoked Meat Intake and Survival Following Breast Cancer. J. Natl. Cancer Inst. 2017, 109, djw299. [Google Scholar] [CrossRef]
- Butler, M.J.; Barrientos, R.M. The impact of nutrition on COVID-19 susceptibility and long-term consequences. Brain Behav. Immun. 2020, 87, 53–54. [Google Scholar] [CrossRef] [PubMed]
- Merino, J.; Joshi, A.D.; Nguyen, L.H.; Leeming, E.R.; Mazidi, M.; Drew, D.A.; Gibson, R.; Graham, M.S.; Lo, C.H.; Capdevila, J.; et al. Diet quality and risk and severity of COVID-19: A prospective cohort study. Gut 2021, 70, 2096–2104. [Google Scholar] [CrossRef] [PubMed]
- Rosenstock, I.M. The Health Belief Model and Preventive Health Behavior. Health Educ. Monogr. 1974, 2, 354–386. [Google Scholar] [CrossRef]
- Rosenstock, I.M. Why people use health services. Milbank Mem. Fund Q. 1966, 44, 94–127. [Google Scholar] [CrossRef] [Green Version]
- National Vaccination Updates. Available online: https://covid19.who.int/table?tableDay (accessed on 29 March 2022).
- Ellison, B.; Ocepek, M.; Lee, L.; Kalaitzandonakes, M.; Schilling, N. How Will the COVID-19 Vaccine Change Food Acquisition Behaviors; Department of Agricultural and Consumer Economics, University of Illinois at Urbana-Champaign: Champaign, IL, USA, 2021; p. 123. [Google Scholar]
- Shmueli, L. Predicting intention to receive COVID-19 vaccine among the general population using the health belief model and the theory of planned behavior model. BMC Public Health 2021, 21, 804. [Google Scholar] [CrossRef]
- Mercadante, A.R.; Law, A.V. Will they, or Won’t they? Examining patients’ vaccine intention for flu and COVID-19 using the Health Belief Model. Res. Social Adm. Pharm 2021, 17, 1596–1605. [Google Scholar] [CrossRef]
- Keshani, P.; Hossein Kaveh, M.; Faghih, S.; Salehi, M.I. Improving diet quality among adolescents, using health belief model in a collaborative learning context: A randomized field trial study. Health Educ. Res. 2019, 34, 279–288. [Google Scholar] [CrossRef] [Green Version]
| Total | Fully Vaccinated | Partially Vaccinated | Not Vaccinated | p Value * | |
|---|---|---|---|---|---|
| N = 4873 | N = 4001 | N = 680 | N = 192 | ||
| Age | <0.001 | ||||
| 18–30 | 55.1% | 53.7% | 62.9% | 56.2% | |
| 31–45 | 36.3% | 37.7% | 28.1% | 35.9% | |
| 46–60 | 7.6% | 7.7% | 7.9% | 5.2% | |
| >60 | 1.0% | 0.9% | 1.0% | 2.6% | |
| Sex | <0.001 | ||||
| Male | 38.7% | 38.3% | 46.5% | 21.4% | |
| Female | 61.3% | 61.7% | 53.5% | 78.6% | |
| BMI (N = 4716) | <0.001 | ||||
| Underweight | 12.7% | 12.4% | 15.3% | 10.9% | |
| Normal | 53.1% | 54.7% | 46.3% | 44.3% | |
| Overweight | 25.2% | 24.8% | 24.4% | 35.4% | |
| Obese | 5.4% | 5.3% | 6.3% | 5.7% | |
| Missing | 3.5% | 2.8% | 7.6% | 3.6% | |
| Education level | <0.001 | ||||
| High school or less | 15.0% | 13.6% | 24.1% | 11.5% | |
| Bachelor’s degree | 68.7% | 70.2% | 63.2% | 55.7% | |
| Master’s degree or above | 16.3% | 16.2% | 12.6% | 32.8% | |
| Total annual household income | 0.001 | ||||
| <30K | 6.2% | 5.5% | 9.9% | 5.7% | |
| 30–100K | 27.5% | 27.5% | 28.1% | 26.6% | |
| 100–30K | 48.5% | 49.6% | 42.6% | 47.4% | |
| 300–500K | 13.1% | 13.0% | 14.1% | 13.0% | |
| 500k–1M | 3.6% | 3.3% | 4.4% | 5.7% | |
| >1M | 1.1% | 1.1% | 0.9% | 1.6% | |
| Diagnosed with chronic disease pre-COVID-19 | <0.001 | ||||
| No | 86.5% | 87.1% | 81.6% | 90.1% | |
| Yes | 13.5% | 12.9% | 18.4% | 9.9% | |
| Living with a child ≤ 5 y-o | 0.42 | ||||
| No | 65.3% | 65.6% | 65.0% | 60.9% | |
| Yes | 34.7% | 34.4% | 35.0% | 39.1% | |
| Living with elders ≥ 60 y-o | 0.011 | ||||
| No | 49.9% | 50.1% | 46.3% | 58.3% | |
| Yes | 50.1% | 49.9% | 53.7% | 41.7% | |
| Living with a pregnant woman | <0.001 | ||||
| No | 94.4% | 95.6% | 91.6% | 79.7% | |
| Yes | 5.6% | 4.4% | 8.4% | 20.3% | |
| Type of residence | <0.001 | ||||
| Rural | 16.4% | 15.2% | 25.3% | 8.9% | |
| Urban | 83.6% | 84.8% | 74.7% | 91.1% | |
| Total | Tertile 1 67.3 (14.1) | Tertile 2 86.3 (3.56) | Tertile 3 98.8 (2.20) | p Value * | |
|---|---|---|---|---|---|
| N = 4873 | N = 1845 | N = 1424 | N = 1604 | ||
| Age (%) | 0.001 | ||||
| 18–30 | 55.1% | 58.8% | 54.6% | 51.1% | |
| 31–45 | 36.3% | 32.8% | 36.8% | 40.0% | |
| 46–60 | 7.6% | 7.4% | 7.6% | 7.9% | |
| >60 | 1.0% | 1.0% | 1.0% | 1.1% | |
| Gender (%) | <0.001 | ||||
| Male | 38.7% | 35.2% | 39.8% | 41.9% | |
| Female | 61.3% | 64.8% | 60.2% | 58.1% | |
| BMI (N = 4716) | 0.16 | ||||
| Underweight | 12.7% | 13.6% | 12.3% | 12.2% | |
| Normal | 53.1% | 53.8% | 54.8% | 50.9% | |
| Overweight | 25.2% | 24.3% | 24.6% | 26.7% | |
| Obese | 5.4% | 4.9% | 5.3% | 6.2% | |
| Missing | 3.5% | 3.5% | 3.0% | 3.9% | |
| Education level (%) | <0.001 | ||||
| High school or less | 15.0% | 12.8% | 12.5% | 19.7% | |
| Bachelor’s degree | 68.7% | 63.3% | 71.8% | 72.1% | |
| Master’s degree and above | 16.3% | 23.8% | 15.7% | 8.2% | |
| Total annual household income (%) | <0.001 | ||||
| <30K | 6.2% | 6.3% | 4.3% | 7.7% | |
| 30–100K | 27.5% | 26.0% | 27.9% | 29.0% | |
| 100–30K | 48.5% | 46.6% | 51.8% | 47.8% | |
| 300–500K | 13.1% | 13.8% | 12.6% | 12.8% | |
| 500k–1M | 3.6% | 5.7% | 2.6% | 2.0% | |
| >1M | 1.1% | 1.6% | 0.8% | 0.7% | |
| Diagnosed with chronic disease pre-COVID-19 (%) | 0.018 | ||||
| No | 86.5% | 85.2% | 88.6% | 86.0% | |
| Yes | 13.5% | 14.8% | 11.4% | 14.0% | |
| Living with a child ≤ 5 y-o (%) | <0.001 | ||||
| No | 65.3% | 69.8% | 66.9% | 58.7% | |
| Yes | 34.7% | 30.2% | 33.1% | 41.3% | |
| Living with elders ≥ 60 y-o (%) | <0.001 | ||||
| No | 49.9% | 54.1% | 50.2% | 44.8% | |
| Yes | 50.1% | 45.9% | 49.8% | 55.2% | |
| Living with a pregnant woman (%) | 0.004 | ||||
| No | 94.4% | 93.1% | 95.8% | 94.6% | |
| Yes | 5.6% | 6.9% | 4.2% | 5.4% | |
| Type of residence (%) | <0.001 | ||||
| Rural | 16.4% | 14.1% | 15.9% | 19.4% | |
| Urban | 83.6% | 85.9% | 84.1% | 80.6% | |
| Vaccination status | |||
| Mean HDDS (SE) * | β (95% CI) # | p values | |
| Not vaccinated (n = 192) | 9.21 (0.148) | Reference | |
| Partially vaccinated (n = 680) | 9.38 (0.080) | 0.170 (−0.161, 0.500) | 0.315 |
| Fully vaccinated (n = 4001) | 9.54 (0.032) | 0.321 (0.024, 0.618) | 0.034 |
| Confidence in the protectiveness of vaccination against COVID-19 | |||
| Mean HDDS (SE) * | β (95% CI) # | p values | |
| Tertile 1 (n = 1845) | 9.22 (0.047) | Reference | |
| Tertile 2 (n = 1424) | 9.57 (0.053) | 0.350 (0.210, 0.490) | <0.001 |
| Tertile 3 (n = 1604) | 9.77 (0.050) | 0.544 (0.407, 0.682) | <0.001 |
| Relative Risk Ratio (RRR) (95% CI) # (Reference = No Change) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Vaccination Status (Reference= Not Vaccinated) | Belief in the Protectiveness of the Vaccination against COVID-19 (Reference = Tertile 1) | |||||||
| Partially Vaccinated (n = 680) | Fully Vaccinated (n = 4001) | Tertile 2 (n = 1424) | Tertile 3 (n = 1604) | |||||
| Increased | Decreased | Increased | Decreased | Increased | Decreased | Increased | Decreased | |
| Eating out | 1.251 (0.769, 2.033) | 1.447 * (0.982, 2.133) | 1.378 (0.896, 2.119) | 1.425 ** (1.010, 2.012) | 1.184 (0.962, 1.458) | 1.335 *** (1.127, 1.582) | 1.323 *** (1.074, 1.630) | 1.531 *** (1.290, 1.816) |
| Takeaway | 1.218 (0.765, 1.939) | 1.060 (0.710, 1.582) | 1.370 (0.904, 2.076) | 1.144 (0.801, 1.635) | 1.309 *** (1.079, 1.588) | 1.437 *** (1.205, 1.713) | 1.280 ** (1.052, 1.557) | 1.607 *** (1.349, 1.915) |
| Cooking at home | 1.150 (0.777, 1.704) | 1.884 ** (1.112, 3.191) | 1.157 (0.819, 1.634) | 1.481 (0.916, 2.393) | 1.530 *** (1.289, 1.814) | 1.185 (0.955, 1.470) | 1.902 *** (1.597, 2.266) | 1.374 *** (1.104, 1.709) |
| Shopping at a farmer’s market | 1.445 * (0.963, 2.169) | 1.639 ** (1.066, 2.520) | 1.249 (0.872, 1.790) | 1.237 (0.842, 1.816) | 1.549 *** (1.304, 1.839) | 1.179 * (0.981, 1.416) | 1.975 *** (1.661, 2.348) | 1.413 *** (1.174, 1.700) |
| Shopping online | 1.858 *** (1.239, 2.786) | 1.825 *** (1.175, 2.835) | 1.565 ** (1.097, 2.232) | 1.408 * (0.951, 2.087) | 1.417 *** (1.190, 1.687) | 1.258 ** (1.040, 1.521) | 1.494 *** (1.252, 1.782) | 1.451 *** (1.204, 1.750) |
| Seafood consumption | 1.321 (0.790, 2.211) | 1.367 (0.938, 1.991) | 1.390 (0.876, 2.204) | 1.299 (0.927, 1.821) | 1.261 ** (1.019, 1.561) | 1.405 *** (1.196, 1.650) | 1.366 *** (1.102, 1.693) | 1.669 *** (1.422, 1.960) |
| Raw food consumption | 1.777 * (0.919, 3.437) | 1.225 (0.853, 1.761) | 1.716 * (0.932, 3.162) | 1.160 (0.840, 1.602) | 1.183 (0.924, 1.514) | 1.409 *** (1.205, 1.648) | 1.246 * (0.978, 1.588) | 1.567 *** (1.341, 1.832) |
| Frozen food consumption | 1.521 * (0.945, 2.447) | 1.360 (0.923, 2.003) | 1.227 (0.798, 1.886) | 1.324 (0.937, 1.872) | 1.324 *** (1.083, 1.618) | 1.475 *** (1.251, 1.738) | 1.411 *** (1.150, 1.732) | 1.892 *** (1.606, 2.229) |
| Imported produce consumption | 1.923 * (0.928, 3.986) | 1.379 * (0.962, 1.975) | 1.855 * (0.938, 3.668) | 1.362 * (0.988, 1.877) | 1.340 ** (1.029, 1.744) | 1.479 *** (1.266, 1.727) | 1.432 *** (1.107, 1.853) | 1.708 *** (1.462, 1.995) |
| Snack and beverage consumption | 1.366 (0.876, 2.130) | 0.816 (0.545, 1.222) | 1.275 (0.853, 1.905) | 0.866 (0.605, 1.240) | 1.278 *** (1.066, 1.532) | 1.188 * (0.997, 1.416) | 1.353 *** (1.127, 1.623) | 1.331 *** (1.118, 1.583) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, Z.; Ma, Y.; Huo, S.; Ke, Y.; Zhao, A. Impact of COVID-19 Vaccination Status and Confidence on Dietary Practices among Chinese Residents. Foods 2022, 11, 1365. https://doi.org/10.3390/foods11091365
Li Z, Ma Y, Huo S, Ke Y, Zhao A. Impact of COVID-19 Vaccination Status and Confidence on Dietary Practices among Chinese Residents. Foods. 2022; 11(9):1365. https://doi.org/10.3390/foods11091365
Chicago/Turabian StyleLi, Zhongyu, Yidi Ma, Shanshan Huo, Yalei Ke, and Ai Zhao. 2022. "Impact of COVID-19 Vaccination Status and Confidence on Dietary Practices among Chinese Residents" Foods 11, no. 9: 1365. https://doi.org/10.3390/foods11091365
APA StyleLi, Z., Ma, Y., Huo, S., Ke, Y., & Zhao, A. (2022). Impact of COVID-19 Vaccination Status and Confidence on Dietary Practices among Chinese Residents. Foods, 11(9), 1365. https://doi.org/10.3390/foods11091365





