Efficiency of In-Store Interventions to Impact Customers to Purchase Healthier Food and Beverage Products in Real-Life Grocery Stores: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Method
2.1. Eligibility Criteria
2.2. Information Source and Search Strategy
2.3. Data Collection
2.4. Data Extraction
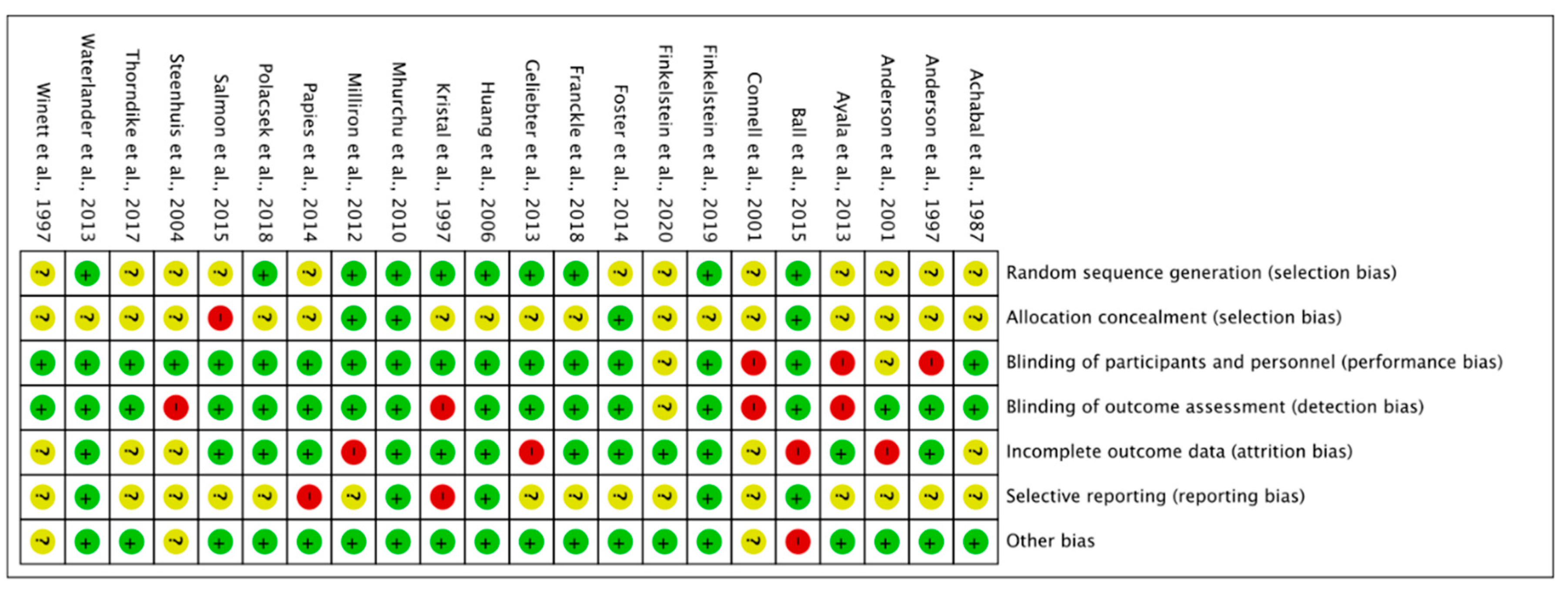
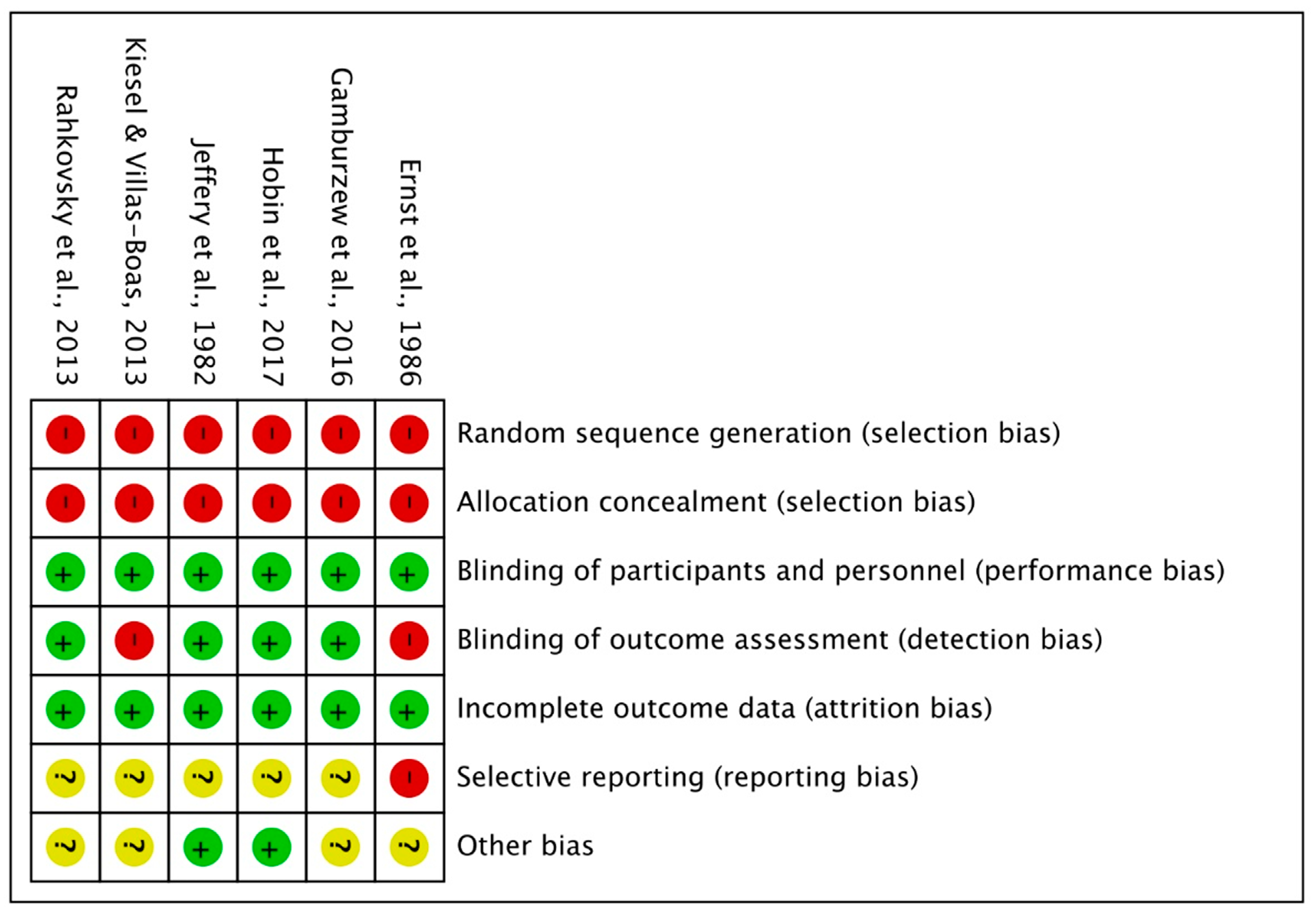
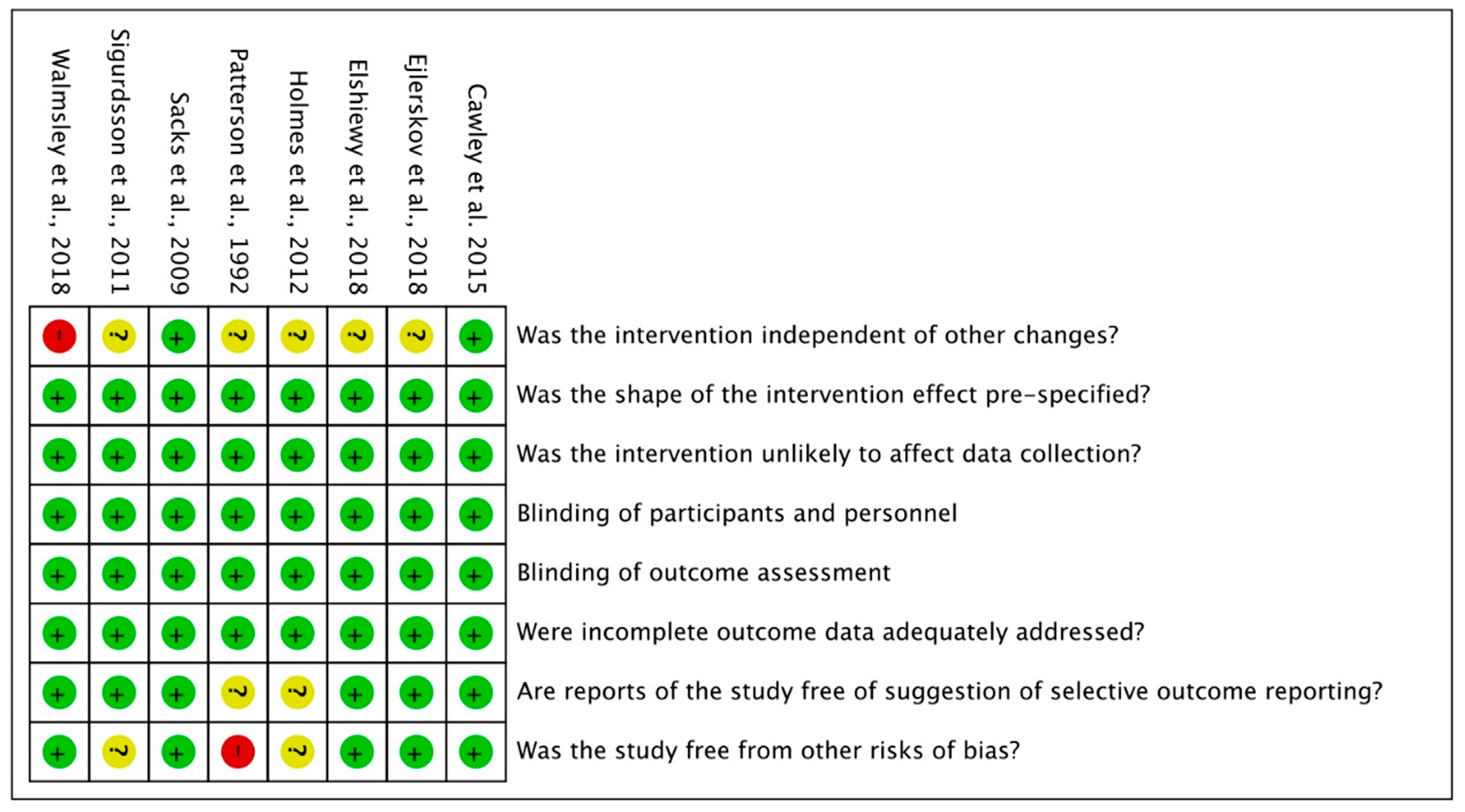
2.5. Risk of Bias within Individual Studies
2.6. Statistical Analysis
2.7. Quality of Evidence
3. Results
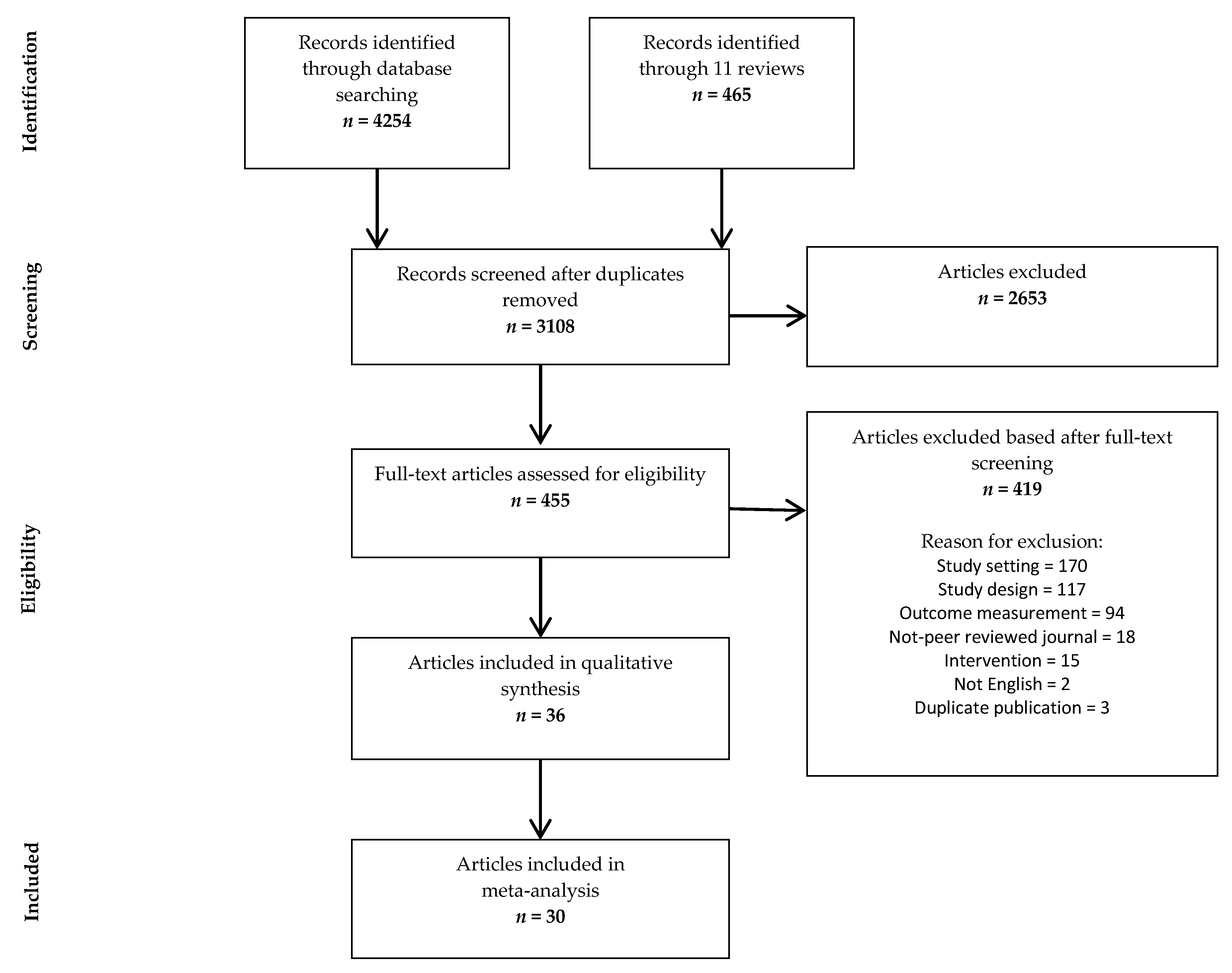
3.1. Study Selection
3.2. Study Characteristics
3.3. Risk of Bias
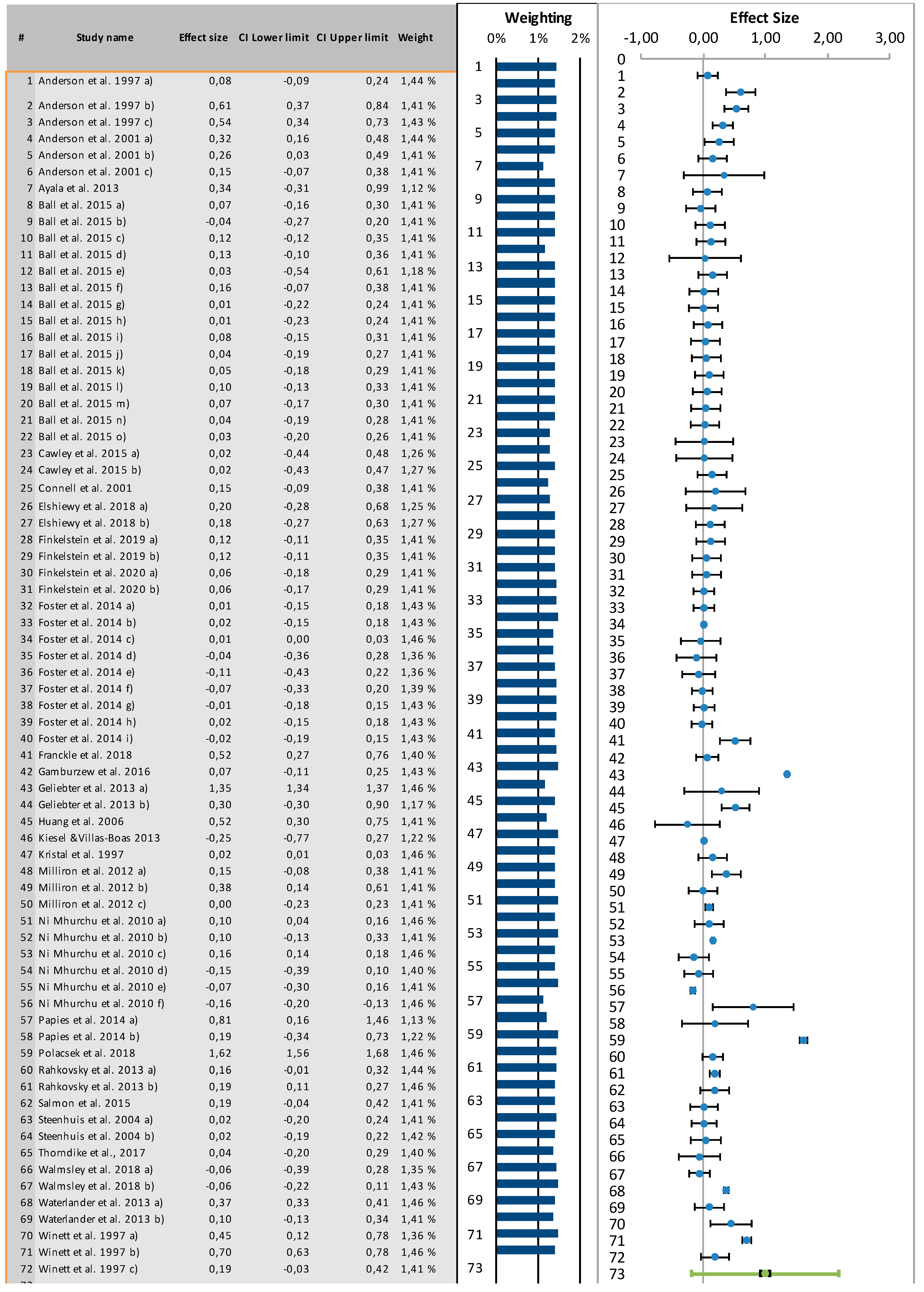
3.4. Results from Meta-Analysis
3.4.1. Analyses by Type of In-Store Intervention
3.4.2. Analysis by the Targeted Product Category
4. Discussion
4.1. Summary of the Main Findings
4.2. Quality of Evidence
4.3. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- GBD 2019 Risk Factors Collaborators. Global Burden of 87 Risk Factors in 204 Countries and Territories, 1990–2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1223–1249. [Google Scholar] [CrossRef]
- GBD 2017 Diet Collaborators. Health effects of dietary risks in 195 countries, 1990–2017: A systematic analysis for the Global Burden of Disease Study. Lancet 2019, 393, 1958–1972. [Google Scholar] [CrossRef]
- Forouzanfar, M.H.; Afshin, A.; Alexander, L.T.; Anderson, H.R.; Bhutta, Z.A.; Biryukov, S.; Brauer, M.; Burnett, R.; Cercy, K.; Charlson, F.J.; et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: A systematic analysis for the Global Burden of Disease Study. Lancet 2016, 388, 1659–1724. [Google Scholar] [CrossRef]
- European Commission. Health Inequalities: Dietary and Physical Activity-Related Determinants. Available online: https://ec.europa.eu/jrc/en/health-knowledge-gateway/societal-impacts/inequalities (accessed on 1 December 2020).
- Appelhans, B.M.; Milliron, B.-J.; Woolf, K.; Johnson, T.J.; Pagoto, S.L.; Schneider, K.L.; Whited, M.C.; Ventrelle, J.C. Socioeconomic Status, Energy Cost, and Nutrient Content of Supermarket Food Purchases. Am. J. Prev. Med. 2012, 42, 398–402. [Google Scholar] [CrossRef]
- Darmon, N.; Drewnowski, A. Does social class predict diet quality? Am. J. Clin. Nutr. 2008, 87, 1107–1117. [Google Scholar] [CrossRef] [PubMed]
- Giskes, K.; Avendaňo-Pabon, M.; Brug, J.; Kunst, A.E. A systematic review of studies on socioeconomic inequalities in dietary intakes associated with weight gain and overweight/obesity conducted among European adults. Obes. Rev. 2010, 11, 413–429. [Google Scholar] [CrossRef]
- Pechey, R.; Jebb, S.A.; Kelly, M.P.; Almiron-Roig, E.; Conde, S.; Nakamura, R.; Shemilt, I.; Suhrcke, M.; Marteau, T.M. Socioeconomic differences in purchases of more vs. less healthy foods and beverages: Analysis of over 25,000 British households in 2010. Soc. Sci. Med. 2013, 92, 22–26. [Google Scholar] [CrossRef]
- Hollands, G.J.; Shemilt, I.; Marteau, T.M.; A Jebb, S.; Kelly, M.P.; Nakamura, R.; Suhrcke, M.; Ogilvie, D. Altering micro-environments to change population health behaviour: Towards an evidence base for choice architecture interventions. BMC Public Health 2013, 13, 1218. [Google Scholar] [CrossRef]
- Loewenstein, G.; Brennan, T.; Volpp, K.G. Asymmetric Paternalism to Improve Health Behaviors. JAMA 2007, 298, 2415–2417. [Google Scholar] [CrossRef] [PubMed]
- Just, D.R.; Price, J. Using incentives to encourage healthy eating in children. J. Hum. Resour. 2013, 48, 855–872. [Google Scholar]
- Bauer, J.M.; Reisch, L.A. Behavioural Insights and (Un)healthy Dietary Choices: A Review of Current Evidence. J. Consum. Policy 2019, 42, 3–45. [Google Scholar] [CrossRef]
- European Commission. Policies and Interventions to Improve the Nutritional Intake and Physical Activity Levels of Europeans; I.C.S. Ltd., Ed.; European Commission: Brussels, Belgium, 2018. [Google Scholar]
- Van den Broucke, S. Theory-Informed Health Promotion: Seeing the Bigger Picture by Looking at the Details; Oxford University Press: Oxford, UK, 2012. [Google Scholar]
- Cadario, R.; Chandon, P. Which healthy eating nudges work best? A meta-analysis of field experiments. Market. Sci. 2020, 39, 465–486. [Google Scholar] [CrossRef]
- TimeTrade System. The State of Retail; TimeTrade System: Tewksbury, MA, USA, 2017. [Google Scholar]
- Askew, K. 2019 and Beyond: Six Trends Shaping the Supermarket of the Future. Available online: https://www.foodnavigator.com/Article/2018/12/21/2019-and-beyond-Six-trends-shaping-the-supermarket-of-the-future (accessed on 25 September 2019).
- Drewnowski, A.; Rehm, C.D. Energy intakes of US children and adults by food purchase location and by specific food source. Nutr. J. 2013, 12, 59. [Google Scholar] [CrossRef] [PubMed]
- Sunstein, C.R. The Council of Psychological Advisers. Annu. Rev. Psychol. 2016, 67, 713–737. [Google Scholar] [CrossRef]
- Mullainathan, S.; Shafir, E. Scarcity: Why Having Too Little Means So Much; Macmillan: Basingstoke, UK, 2013. [Google Scholar]
- Blakely, T.; Ni Mhurchu, C.; Jiang, Y.; Matoe, L.; Funaki-Tahifote, M.; Eyles, H.C.; Foster, R.H.; McKenzie, S.; Rodgers, A. Do effects of price discounts and nutrition education on food purchases vary by ethnicity, income and education? Results from a randomised, controlled trial. J. Epidemiol. Commun. Health 2011, 65, 902–908. [Google Scholar] [CrossRef]
- Marteau, T.M.; Ogilvie, D.; Roland, M.; Suhrcke, M.; Kelly, M. Judging nudging: Can nudging improve population health? Brit. Med. J. 2011, 342, 228. [Google Scholar] [CrossRef] [PubMed]
- Sunstein, C.R.; Thaler, R.H. Nudge: Improving Decisions about Health, Wealth and Happiness; Yale University Press: New Haven, CT, USA, 2008. [Google Scholar]
- Van´t Riet, J. Sales effects of product health information at points of purchase: A systematic review. Public Health Nutr. 2012, 16, 418–429. [Google Scholar] [CrossRef]
- Escaron, A.L.; Meinen, A.M.; Nitzke, S.A.; Martinez-Donate, A.P. Supermarket and Grocery Store–Based Interventions to Promote Healthful Food Choices and Eating Practices: A Systematic Review. Prev. Chronic Dis. 2013, 10, E50. [Google Scholar] [CrossRef] [PubMed]
- Glanz, K.; Bader, M.; Lyer, S. Retail Grocery Store Marketing Strategies and Obesity: An Integrative Review. Am. J. Prev. Med. 2012, 42, 503–512. [Google Scholar] [CrossRef]
- Hersey, J.C.; Wohlgenant, K.C.; E Arsenault, J.; Kosa, K.M.; Muth, M.K. Effects of front-of-package and shelf nutrition labeling systems on consumers. Nutr. Rev. 2013, 71, 1–14. [Google Scholar] [CrossRef]
- Adam, A.; Jensen, J.D. What is the effectiveness of obesity related interventions at retail grocery stores and supermarkets?—A systematic review. BMC Public Health 2016, 16, 1247. [Google Scholar] [CrossRef] [PubMed]
- Cameron, A.J.; Charlton, E.; Ngan, W.W.; Sacks, G. A Systematic Review of the Effectiveness of Supermarket-Based Interventions Involving Product, Promotion, or Place on the Healthiness of Consumer Purchases. Curr. Nutr. Rep. 2016, 5, 129–138. [Google Scholar] [CrossRef]
- Hartmann-Boyce, J.; Bianchi, F.; Piernas, C.; Riches, S.P.; Frie, K.; Nourse, R.; Jebb, S.A. Grocery store interventions to change food purchasing behaviors: A systematic review of randomized controlled trials. Am. J. Clin. Nutr. 2018, 107, 1004–1016. [Google Scholar] [CrossRef] [PubMed]
- Liberato, S.C.; Bailie, R.; Brimblecombe, J. Nutrition interventions at point-of-sale to encourage healthier food purchasing: A systematic review. BMC Public Health 2014, 14, 919. [Google Scholar] [CrossRef]
- Holden, S.S.; Zlatevska, N.; Dubelaar, C. Whether Smaller Plates Reduce Consumption Depends on Who’s Serving and Who’s Looking: A Meta-Analysis. J. Assoc. Consum. Res. 2016, 1, 134–146. [Google Scholar] [CrossRef]
- Hayes, A.; Lung, T.; Wen, L.M.; Baur, L.; Rissel, C.; Howard, K. Economic evaluation of “healthy beginnings” an early childhood intervention to prevent obesity. Obesity 2014, 22, 1709–1715. [Google Scholar] [CrossRef] [PubMed]
- Mishra, R.; Singh, R.K.; Koles, B. Consumer decision-making in omnichannel retailing: Literature review and future research agenda. Int. J. Consum. Stud. 2021, 45, 147–174. [Google Scholar] [CrossRef]
- Paul, J.; Mas, E. Toward a 7-P framework for international marketing. J. Strat. Mark. 2019, 28, 681–701. [Google Scholar] [CrossRef]
- Kumar, A.; Paul, J.; Unnithan, A.B. ‘Masstige’marketing: A review, synthesis and research agenda. J. Bus. Res. 2020, 113, 384–398. [Google Scholar] [CrossRef]
- Dhaliwal, A.; Singh, D.P.; Paul, J. The consumer behavior of luxury goods: A review and research agenda. J. Strat. Mark. 2020, 1–27. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e000097. [Google Scholar] [CrossRef] [PubMed]
- Ryan, R.; Hill, S.; Broclain, D.; Horey, D.; Oliver, S.; Prictor, M. Cochrane Consumers and Communication Review Group: Study Design Guide. 2013. Available online: https://cccrg.cochrane.org/author-resources (accessed on 12 April 2020).
- Hollands, G.J.; Bignardi, G.; Johnston, M.; Kelly, M.P.; Ogilvie, D.; Petticrew, M.; Prestwich, A.; Shemilt, I.; Sutton, S.; Marteau, T.M. The TIPPME intervention typology for changing environments to change behaviour. Nat. Hum. Behav. 2017, 1, 0140. [Google Scholar] [CrossRef]
- Kraak, V.I.; Englund, T.; Misyak, S.; Serrano, E.L. A novel marketing mix and choice architecture framework to nudge restaurant customers toward healthy food environments to reduce obesity in the United States. Obes. Rev. 2017, 18, 852–868. [Google Scholar] [CrossRef] [PubMed]
- Booth, A. Clear and present questions: Formulating questions for evidence based practice. Libr. Hi Tech 2006, 24, 355–368. [Google Scholar] [CrossRef]
- World Health Organization. Healthy Diet; Fact Sheet Number 394; World Health Organization: New York, NY, USA, 2018. [Google Scholar]
- Higgins, J.P.T.; Thomas, J. Cochrane Handbook for Systematic Reviews of Interventions; Version 6.2; Cochrane: London, UK, 2021. [Google Scholar]
- Ryan, R. Cochrane Consumers and Communication Review Group: Data synthesis and analysis. Cochrane Consumers and Communication Review Group. 2013. Available online: http://cccrg.cochrane.org (accessed on 11 November 2020).
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Erlbaum Association: New York, NY, USA, 1988. [Google Scholar]
- Higgins, J.P.T.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. Br. Med. J. 2003, 327, 557–560. [Google Scholar] [CrossRef]
- Suurmond, R.; Van Rhee, H.; Hak, T. Introduction, comparison, and validation ofMeta-Essentials: A free and simple tool for meta-analysis. Res. Synth. Methods 2017, 8, 537–553. [Google Scholar] [CrossRef]
- Lenhard, W.; Lenhard, A. Calculation of Effect Sizes. Psychometrica 2016. Available online: https://www.psychometrica.de/effect_size.html (accessed on 2 January 2021).
- Wilson, D.B. Pratical Meta-Analysis Effect Size Calculator. 2020. Available online: https://campbellcollaboration.org/escalc/html/EffectSizeCalculator-Home.php (accessed on 11 November 2020).
- Van Rhee, H.; Suurmond, R.; Hak, T. User Manual for Meta-Essentials: Workbooks for Meta-Analysis; Version 1.2; Erasmus Research Institute of Management: Rotterdam, The Netherlands, 2015. [Google Scholar]
- Ayala, G.X.; Baquero, B.; A Laraia, B.; Ji, M.; Linnan, L. Efficacy of a store-based environmental change intervention compared with a delayed treatment control condition on store customers’ intake of fruits and vegetables. Public Health Nutr. 2013, 16, 1953–1960. [Google Scholar] [CrossRef]
- Thorndike, A.N.; Bright, O.-J.M.; Dimond, M.A.; Fishman, R.; Levy, D.E. Choice architecture to promote fruit and vegetable purchases by families participating in the Special Supplemental Program for Women, Infants, and Children (WIC): Randomized corner store pilot study. Public Health Nutr. 2017, 20, 1297–1305. [Google Scholar] [CrossRef] [PubMed]
- Polacsek, M.; Moran, A.; Thorndike, A.N.; Boulos, R.; Franckle, R.L.; Greene, J.C.; Blue, D.J.; Block, J.P.; Rimm, E.B. A Supermarket Double-Dollar Incentive Program Increases Purchases of Fresh Fruits and Vegetables Among Low-Income Families with Children: The Healthy Double Study. J. Nutr. Educ. Behav. 2018, 50, 217–228.e1. [Google Scholar] [CrossRef]
- Franckle, R.L.; E Levy, D.; Macias-Navarro, L.; Rimm, E.B.; Thorndike, A.N. Traffic-light labels and financial incentives to reduce sugar-sweetened beverage purchases by low-income Latino families: A randomized controlled trial. Public Health Nutr. 2018, 21, 1426–1434. [Google Scholar] [CrossRef] [PubMed]
- Foster, G.D.; Karpyn, A.; Wojtanowski, A.C.; Davis, E.; Weiss, S.; Brensinger, C.; Tierney, A.; Guo, W.; Brown, J.; Spross, C.; et al. Placement and promotion strategies to increase sales of healthier products in supermarkets in low-income, ethnically diverse neighborhoods: A randomized controlled trial. Am. J. Clin. Nutr. 2014, 99, 1359–1368. [Google Scholar] [CrossRef]
- Gamburzew, A.; Darcel, N.; Gazan, R.; Dubois, C.; Maillot, M.; Tomé, D.; Raffin, S.; Darmon, N. In-store marketing of inexpensive foods with good nutritional quality in disadvantaged neighborhoods: Increased awareness, understanding, and purchasing. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 1–14. [Google Scholar] [CrossRef]
- Papies, E.K.; Potjes, I.; Keesman, M.; Schwinghammer, S.; Van Koningsbruggen, G.M. Using health primes to reduce unhealthy snack purchases among overweight consumers in a grocery store. Int. J. Obes. 2013, 38, 597–602. [Google Scholar] [CrossRef]
- Geliebter, A.; Ang, I.; Yi, H.; Bernales-Korins, M.; Hernandez, D.; Ochner, C.N.; Ungredda, T.; Miller, R.; Kolbe, L. Supermarket discounts of low-energy density foods: Effects on purchasing, food intake, and body weight. Obesity 2013, 21, E542–E548. [Google Scholar] [CrossRef]
- Achabal, D.D.; McIntyre, S.H.; Bell, C.H.; Tucker, N. The effect of nutrition POP signs on consumer attitudes and behavior. J. Retail. 1987, 63, 9–24. [Google Scholar]
- Anderson, E.S.; Winett, R.A.; Bickley, P.G.; Walberg-Rankin, J.; Moore, J.F.; Leahy, M.; Harris, C.E.; Gerkin, R.E. The Effects of a Multimedia System in Supermarkets to Alter Shoppers’ Food Purchases Nutritional Outcomes and Caveats. J. Health Psychol. 1997, 2, 209–223. [Google Scholar] [CrossRef] [PubMed]
- Anderson, E.S.; Winett, R.A.; Wojcik, J.R.; Winett, S.G.; Bowden, T. A computerized social cognitive intervention for nutrition behavior: Direct and mediated effects on fat, fiber, fruits, and vegetables, self-efficacy, and outcome expectations among food shoppers. Ann. Behav. Med. 2001, 23, 88–100. [Google Scholar] [CrossRef] [PubMed]
- Ball, K.; McNaughton, S.A.; Le, H.N.; Gold, L.; Ni Mhurchu, C.; Abbott, G.; Pollard, C.; Crawford, D. Influence of price discounts and skill-building strategies on purchase and consumption of healthy food and beverages: Outcomes of the Supermarket Healthy Eating for Life randomized controlled trial. Am. J. Clin. Nutr. 2015, 101, 1055–1064. [Google Scholar] [CrossRef] [PubMed]
- Connell, D.; Goldberg, J.P.; Folta, S.C. An intervention to increase fruit and vegetable consumption using audio communications: In-store public service announcements and audiotapes. J. Health Commun. 2001, 6, 31–43. [Google Scholar]
- Kristal, A.R.; Goldenhar, L.; Muldoon, J.; Morton, R.F. Evaluation of a supermarket intervention to increase consumption of fruits and vegetables. Am. J. Health Promot. 1997, 11, 422–425. [Google Scholar] [CrossRef] [PubMed]
- Milliron, B.-J.; Woolf, K.; Appelhans, B.M. A Point-of-Purchase Intervention Featuring In-Person Supermarket Education Affects Healthful Food Purchases. J. Nutr. Educ. Behav. 2012, 44, 225–232. [Google Scholar] [CrossRef] [PubMed]
- Sigurdsson, V.; Larsen, N.M.; Gunnarsson, D. An in-store experimental analysis of consumers’ selection of fruits and vegetables. Serv. Ind. J. 2011, 31, 2587–2602. [Google Scholar] [CrossRef]
- Walmsley, R.; Jenkinson, D.; Saunders, I.; Howard, T.; Oyebode, O. Choice architecture modifies fruit and vegetable purchasing in a university campus grocery store: Time series modelling of a natural experiment. BMC Public Health 2018, 18, 1149. [Google Scholar] [CrossRef] [PubMed]
- Waterlander, W.E.; De Boer, M.R.; Schuit, A.J.; Seidell, J.C.; Steenhuis, I.H. Price discounts significantly enhance fruit and vegetable purchases when combined with nutrition education: A randomized controlled supermarket trial. Am. J. Clin. Nutr. 2013, 97, 886–895. [Google Scholar] [CrossRef]
- Winett, R.A.; Anderson, E.S.; Bickley, P.G.; Walberg-Rankin, J.; Moore, J.F.; Leahy, M.; Harris, C.E.; Gerkin, R.E. Nutrition for a lifetime system: A multimedia system for altering food supermarket shoppers’ purchases to meet nutritional guidelines. Comput. Hum. Behav. 1997, 13, 371–392. [Google Scholar] [CrossRef]
- Finkelstein, E.A.; Ang, F.J.L.; Doble, B.; Wong, W.H.M.; Van Dam, R.M. A Randomized Controlled Trial Evaluating the Relative Effectiveness of the Multiple Traffic Light and Nutri-Score Front of Package Nutrition Labels. Nutrients 2019, 11, 2236. [Google Scholar] [CrossRef]
- Hobin, E.; Bollinger, B.; Sacco, J.; Liebman, E.; Vanderlee, L.; Zuo, F.; Rosella, L.; L’Abbe, M.; Manson, H.; Hammond, D. Consumers’ Response to an On-Shelf Nutrition Labelling System in Supermarkets: Evidence to Inform Policy and Practice. Milbank Q. 2017, 95, 494–534. [Google Scholar] [CrossRef]
- Rahkovsky, I.; Lin, B.-H.; Lin, C.-T.J.; Lee, J.-Y. Effects of the Guiding Stars Program on purchases of ready-to-eat cereals with different nutritional attributes. Food Policy 2013, 43, 100–107. [Google Scholar] [CrossRef]
- Cawley, J.; Sweeney, M.J.; Sobal, J.; Just, D.R.; Kaiser, H.M.; Schulze, W.D.; Wethington, E.; Wansink, B. The impact of a supermarket nutrition rating system on purchases of nutritious and less nutritious foods. Public Health Nutr. 2014, 18, 8–14. [Google Scholar] [CrossRef]
- Ernst, N.D.; Wu, M.; Frommer, P.; Katz, E.; Matthews, O.; Moskowitz, J.; Pinsky, J.L.; Pohl, S.; Schreiber, G.B.; Sondik, E.; et al. Nutrition education at the point of purchase: The foods for health project evaluated. Prev. Med. 1986, 15, 60–73. [Google Scholar] [CrossRef]
- Holmes, A.S.; Estabrooks, P.A.; Davis, G.C.; Serrano, E.L. Effect of a Grocery Store Intervention on Sales of Nutritious Foods to Youth and Their Families. J. Acad. Nutr. Diet. 2012, 112, 897–901. [Google Scholar] [CrossRef]
- Patterson, B.H.; Kessler, L.G.; Wax, Y.; Bernstein, A.; Light, L.; Midthune, D.N.; Portnoy, B.; Tenney, J.; Tuckermanty, E. Evaluation of a Supermarket Intervention The NCI-Giant Food Eat for Health Study. Eval. Rev. 1992, 16, 464–490. [Google Scholar] [CrossRef]
- Sacks, G.; Rayner, M.; Swinburn, B. Impact of front-of-pack ’traffic-light’ nutrition labelling on consumer food purchases in the UK. Health Promot. Int. 2009, 24, 344–352. [Google Scholar] [CrossRef] [PubMed]
- Salmon, S.J.; De Vet, E.; Adriaanse, M.A.; Fennis, B.M.; Veltkamp, M.; De Ridder, D.T. Social proof in the supermarket: Promoting healthy choices under low self-control conditions. Food Qual. Prefer. 2015, 45, 113–120. [Google Scholar] [CrossRef]
- Jeffery, R.W.; Pirie, P.L.; Rosenthal, B.S.; Gerber, W.M.; Murray, D.M. Nutrition education in supermarkets: An unsuccessful attempt to influence knowledge and product sales. J. Behav. Med. 1982, 5, 189–200. [Google Scholar] [CrossRef] [PubMed]
- Kiesel, K.; Villas-Boas, S.B. Can information costs affect consumer choice? Nutritional labels in a supermarket experiment. Int. J. Ind. Organ. 2013, 31, 153–163. [Google Scholar] [CrossRef]
- Steenhuis, I.; Van Assema, P.; Van Breukelen, G.; Glanz, K. The effectiveness of nutrition education and labeling in Dutch supermarkets. Am. J. Health Promot. 2004, 18, 221–224. [Google Scholar] [CrossRef] [PubMed]
- Huang, A.; Barzi, F.; Huxley, R.; Denyer, G.; Rohrlach, B.; Jayne, K.; Neal, B. The Effects on Saturated Fat Purchases of Providing Internet Shoppers with Purchase- Specific Dietary Advice: A Randomised Trial. PLoS Clin. Trials 2006, 1, e22. [Google Scholar] [CrossRef]
- Mhurchu, C.N.; Blakely, T.; Jiang, Y.; Eyles, H.C.; Rodgers, A. Effects of price discounts and tailored nutrition education on supermarket purchases: A randomized controlled trial. Am. J. Clin. Nutr. 2010, 91, 736–747. [Google Scholar] [CrossRef]
- Ejlerskov, K.T.; Sharp, S.J.; Stead, M.; Adamson, A.J.; White, M.; Adams, J. Supermarket policies on less-healthy food at checkouts: Natural experimental evaluation using interrupted time series analyses of purchases. PLoS Med. 2018, 15, e1002712. [Google Scholar] [CrossRef] [PubMed]
- Elshiewy, O.; Boztug, Y. When Back of Pack Meets Front of Pack: How Salient and Simplified Nutrition Labels Affect Food Sales in Supermarkets. J. Public Policy Mark. 2018, 37, 55–67. [Google Scholar] [CrossRef]
- Finkelstein, E.A.; Ang, F.J.L.; Doble, B. Randomized trial evaluating the effectiveness of within versus across-category front-of-package lower-calorie labelling on food demand. BMC Public Health 2020, 20, 312. [Google Scholar] [CrossRef]
- Afshin, A.; Peñalvo, J.L.; Del Gobbo, L.; Silva, J.; Michaelson, M.; O’Flaherty, M.; Capewell, S.; Spiegelman, D.; Danaei, G.; Mozaffarian, D. The prospective impact of food pricing on improving dietary consumption: A systematic review and meta-analysis. PLoS ONE 2017, 12, e0172277. [Google Scholar] [CrossRef]
- Epstein, L.H.; Jankowiak, N.; Nederkoorn, C.; Raynor, H.A.; French, S.A.; Finkelstein, E. Experimental research on the relation between food price changes and food-purchasing patterns: A targeted review. Am. J. Clin. Nutr. 2012, 95, 789–809. [Google Scholar] [CrossRef] [PubMed]
- Broers, V.J.V.; De Breucker, C.; Broucke, S.V.D.; Luminet, O. A systematic review and meta-analysis of the effectiveness of nudging to increase fruit and vegetable choice. Eur. J. Public Health 2017, 27, 912–920. [Google Scholar] [CrossRef] [PubMed]
- Arno, A.; Thomas, S. The efficacy of nudge theory strategies in influencing adult dietary behaviour: A systematic review and meta-analysis. BMC Public Health 2016, 16, 1–11. [Google Scholar] [CrossRef] [PubMed]
- De Pergola, G.; D’Alessandro, A. Influence of Mediterranean Diet on Blood Pressure. Nutrients 2018, 10, 1700. [Google Scholar] [CrossRef]
- Ge, L.; Sadeghirad, B.; Ball, G.D.C.; Da Costa, B.R.; Hitchcock, C.L.; Svendrovski, A.; Kiflen, R.; Quadri, K.; Kwon, H.Y.; Karamouzian, M.; et al. Comparison of dietary macronutrient patterns of 14 popular named dietary programmes for weight and cardiovascular risk factor reduction in adults: Systematic review and network meta-analysis of randomised trials. Br. Med. J. 2020, 369, m696. [Google Scholar] [CrossRef]
- Food and Agriculture Organization of the United Nations. New Food Balances. Available online: http://www.fao.org/faostat/en/#data/FBS (accessed on 20 November 2020).
- Thow, A.M.; Downs, S.; Jan, S. A systematic review of the effectiveness of food taxes and subsidies to improve diets: Understanding the recent evidence. Nutr. Rev. 2014, 72, 551–565. [Google Scholar] [CrossRef]
- Mhurchu, C.N.; Blakely, T.; Wall, J.; Rodgers, A.; Jiang, Y.; Wilton, J. Strategies to promote healthier food purchases: A pilot supermarket intervention study. Public Health Nutr. 2007, 10, 608–615. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lane, A.; Luminet, O.; Nave, G.; Mikolajczak, M. Is there a Publication Bias in Behavioural Intranasal Oxytocin Research on Humans? Opening the File Drawer of One Laboratory. J. Neuroendocr. 2016, 28. [Google Scholar] [CrossRef] [PubMed]
| Strategy | Description |
|---|---|
| Portioning | Reduce and/or standardize the portion size of food and beverage products that meet recommended nutrient targets to influence customers’ expectations about single servings and appropriate portions to support healthy dietary guidelines. |
| Place | Changing the internal setting (e.g., lighting, smell, music and branding of stores) that impact the ambience or atmospherics to highlight healthy food and beverage products. |
| Proximity | Placing healthier products at eye level or physically closer to customers at point-of-choice and point-of-purchase (e.g., placing healthier options at the entry or exit of store and giving healthy options better placement in the shelf). |
| Promotion | Use of marketing practices inside store that support healthier diets (i.e., products samples, taste-testing, in-store demonstrations, inside store audio public service announcements and education sessions inside store to promote healthy products). |
| Healthy Default Picks | Use of environmental cues that convenient, accepted and expected to socially normalize healthy defaults choices (e.g., introducing swaps that offer customers the opportunity to replace their usual food with healthier alternatives). |
| Pricing | Use of pricing strategies to increase sales of products that meet recommend nutrient targets to support healthy dietary guidelines (e.g., changes in price per unit, coupons and cash-back). |
| Prompting | Use of information on products to help customers make healthier choices at point-of choice and point-of-purchase (e.g., guiding star labeling system, nutrition labels and traffic-light labels). |
| Profile | Change in the product’s nutritional profile, quality, smell, taste, texture, flavor of food or beverage products that make meeting nutritional targets according to dietary guidelines. |
| Reference | Source | Country | Setting | Study Design | Intervention Type | Target Product | Study Duration | Store Number | Participant Number | Targeted Population Type | Outcome Measurement |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Achabal et al. [60] | Van ‘t Riet [24] + Hartman et al. [30] + Cadario and Chandon [15] + Cameron et al. [29] + Liberato et al. [31] | USA | Grocery store | RCT | Treatments assigned were:
| Increase volume sales of six targeted fruit and vegetable products (e.g., carrots, broccoli, cabbage, cauliflower, kiwi, tomatoes) | 4 weeks baseline, 4 weeks intervention and 4 weeks follow-up | 124 control stores and 248 intervention stores | 283, not specified how many in each group | Normal population | Sales data |
| Anderson et al. [61] * | Database search + Adam and Jensen [28] + Afshin et al. [87] + Liberato et al. [31] + Hartman et al. [30] | USA | Grocery store | RCT | Treatment part of the American Nutrition for a Lifetime System program administered via kiosks in supermarkets. Treatments assigned were:
| Reduce grams of fat, increase grams of fiber per 1000 kcal purchased and increase servings of fruits and vegetables sold | 10 weeks baseline and 14 weeks intervention | 2 intervention stores | Treatm. n = 54 Control n = 50 | Normal population | Self-reported |
| Anderson et al. [62] * | Database + Cameron et al. [29] | USA | Grocery store | RCT | Treatment part of the Nutrition for a Lifetime System program administered via kiosks in supermarkets. Treatments assigned were:
| Reduction percent of calories from total fat sold. Increase in percent calories from fiber and in servings of fruits and vegetables sold. | 4 weeks baseline and 15 weeks intervention | 5 intervention stores | Treatm. n = 145 Control n = 121 | Normal population | Sales data |
| Ayala et al. [52] * | Database search + Adam and Jensen [28] + Liberato et al. [31] | USA | Grocery store | RCT | Treatments assigned were:
| Increase servings of fruits and vegetables sold. | 3 weeks baseline, 8 weeks intervention and 2 weeks follow-up | 2 control stores and 2 intervention stores | Treatm. n = 61 Control n = 58 | Low-income neighborhood | Self-reported |
| Ball et al. [63] * | Database search + Adam and Jensen [28] + Hartman et al. [30] | Australia | Grocery store | RCT | Treatment part of the Australian Supermarket Healthy Eating for Life program. Treatments assigned were:
| Increase grams of fruits and vegetables sold separately (g/week) and increase in milliliters of water and diet beverage sold (mL/week). Reduction in sugar-sweetened beverage (mL/week) sold. | 12 weeks baseline, 12 weeks intervention and 24 weeks follow-up | 2 intervention stores | Treatm. n = 574 Control n = 147 | Normal population | Sales data |
| Cawley et al. [74] * | Database search + Cadario and Chandon [15] + Cameron et al. [29] | USA | Grocery store | ITS | Treatments assigned were:
| Increase in total volume sales of product categorized as healthy and reduction in products categorized as unhealthy according to the guiding star labeling system. Total of 102 products. | 40 weeks baseline, 12 weeks intervention and 104 weeks follow-up | 168 intervention stores | Treatm. n = 38,303 Control n = 335,120 | Normal population | Sales data |
| Connell et al. [64] * | Glanz et al. [26] + Liberato et al. [31] + Escaron et al. [25] + Cameron et al. [29] | USA | Grocery store | RCT | Treatments assigned were:
| Increase percentage average intake of fruits and vegetables | 4 weeks intervention | 3 control stores and 3 intervention stores | Treatm. n = 354 Control n = 328 | Normal population | Self-reported |
| Ejlerskov et al. [88] | Database search | UK | Grocery store | ITS | Treatments assigned were:
| Reduction in volume of common unhealthy checkout-foods (sugary confectionary, chocolate and potato crisps) sold | 52 weeks baseline and 52 weeks intervention | 3 control stores and 6 intervention stores | Treatm. n = 30,000 | Normal population | Sales data |
| Elshiewy et al. [85] * | Database search | UK | Grocery store | ITS | Treatments assigned were:
| Reduction in volume of unhealthy snacks (cookies), high sugar breakfast cereals and unhealthy beverage (soft drinks) | 52 weeks baseline and 52 weeks intervention | 2000 intervention stores | Treatm. n = 188,062 | Normal population | Sales data |
| Ernst et al. [75] | Cameron et al. [29] + Escaron et al. [25] + van ’t Riet [24] + Liberato et al. [31] | USA | Grocery store | CBA | Treatment part of the American Nutrition for a Lifetime System program called “Eat for Health” administered by the American National Cancer Institute. Treatments assigned were:
| Increase in total volume sales of product categorized as healthy and reduction in products categorized as unhealthy. Total of 246 products. | 52 weeks intervention | 10 control stores and 10 intervention stores | Treatm. n = 1202 Control n = 1197 | Normal population | Self-reported |
| Finkelstein et al. [71] * | Database search | Singapore | Online grocery store | RCT | Treatments assigned were:
| Increase in total volume sales of product categorized as healthy according to the healthy eating Index (AHEI-2010) | 3 weeks intervention | 1 intervention stores | Total sample = 147 | Normal population | Sales data |
| Finkelstein et al. [86] * | Database search | Singapore | Online grocery store | RCT | Treatments assigned were:
| Reduction in total sales of calories purchased across all products sold in store. | 3 weeks intervention | 1 intervention stores | Total sample = 146 | Normal population | Sales data |
| Foster et al. [56] * | Database search + Cadario and Chandon [15] + Adam and Jensen [28] + Liberato et al. [31] + Hartman et al. [30] + Cameron et al. [29] | USA | Grocery store | RCT | Treatments assigned were:
| Increase in overall sales of products categorizes as healthy (skim milk, water, cheerios cereal and honeycomb cereal, diet Pepsi) and reduction in sales of products categorizes as less healthy (1% fat milk, Pepsi, Aquafina and water) | 12 weeks baseline and 24 weeks intervention | 4 control stores and 4 intervention stores | Treatm. N = 562,247 Control n = 635,028 | Low-income neighborhood | Sales data |
| Franckle et al. [55] * | Database search | USA | Grocery store | RCT | Treatments assigned were:
| Reduction in volume sales of units of unhealthy beverage (sugar soda) | 8 weeks baseline and 16 weeks intervention | 1 intervention stores | Treatm. N = 71 Control n = 77 | Low-income neighborhood | Sales data |
| Gamburzew et al. [57] * | Database search + Cadario and Chandon [15] | France | Grocery store | CBA | Treatments assigned were:
| Increase in total volume sales of product categorized as healthy. | 24 weeks baseline and 24 weeks intervention | 2 control stores and 2 intervention stores | Treatm. N = 2651 Control n = 3974 | Low-income neighborhood | Sales data |
| Geliebter et al. [59] * | Database search + Adam and Jensen [28] + Hartman et al. [30] | USA | Grocery store | RCT | Treatments assigned were:
| Increase in total volume sales of fruits and vegetables | 4 weeks baseline, 8 weeks intervention and 4 weeks follow-up | 2 intervention stores | Treatm. N = 19 Control n = 28 | Targeting overweight or obesity customers | Sales data |
| Hobin et al. [72] | Database search | Canada | Grocery store | CBA | Treatments assigned were:
| Increase in total volume sales of product categorized as healthy (e.g., products with 3-stars, according to the Guiding Star labeling system) | 12 weeks baseline and 36 weeks intervention | 82 control stores and 44 intervention stores | n.a. | Normal population | Sales data |
| Holmes et al. [76] | Database search + Adam and Jensen [28] + Escaron et al. [25] + Cameron et al. [29] | USA | Grocery store | ITS | Treatments assigned were:
| Increase in proportion of total volume sales from 32 products categorized as healthy | 5 weeks baseline, 12 weeks intervention and 5 weeks follow-up | 1 intervention stores | Treatm. N = 112,072 Control (before) n = 46,960 | Normal population | Sales data |
| Huang et al. [83] * | Liberato et al. [31] + Hartman et al. [30] + Cameron et al. [29] | Australia | Online grocery store | RCT | Treatments assigned were:
| Reduction in grams of saturated-fat (g/100g) sold | 5 weeks intervention | 1 intervention stores | Treatm. N = 251 Control n = 246 | Normal population | Sales data |
| Jeffery et al. [80] | Database search + Escaron et al. [25] + van ’t Riet [24] + Liberato et al. [31] + Hartman et al. [30] + Cameron et al. [29] | USA | Grocery store | CBA | Treatments assigned were:
| Increase in volume sales of 25 low fat dairy products | 16 weeks baseline and 24 weeks intervention | 4 control stores and 4 intervention stores | n.a. | Normal population | Sales data |
| Kiesel & Villas-Boas [81] | Database search + Cadario and Chandon [15] | USA | Grocery store | CBA | Treatments assigned were:
| Increase in volume sales of 93 low-calorie microwave popcorn products | 3 weeks baseline and 3 weeks intervention | 27 control stores and 5 intervention stores | Treatm. N = 742 Control n = 1080 | Normal population | Sales data |
| Kristal et al. [65] * | Database search + Epstein et al. [89] + Escaron et al. [25] + Liberato et al. [31] + Hartman et al. [30] + Cameron et al. [29] | USA | Grocery store | RCT | Treatments assigned were:
| Increase in grams sold of fruits and vegetables by total weight (fresh, frozen and dried) or volume (canned) | 0 weeks baseline and 52 weeks intervention | 4 control stores and 4 intervention stores | Treatm. N = 356 Control n = 371 | Normal population | Self-reported |
| Mhurchu et al. [84] * | Database search + Adam and Jensen [28] + [26] Glanz et al. [26] + Liberato et al. [31] + Epstein et al. [89] + Hartman et al. [30] | New Zealand | Grocery store | RCT | Treatments assigned were:
| Reduction in percentage calories sold from saturated-fat | 24 weeks baseline, 24 weeks intervention and 24 week follow-up | 12 control stores and 12 intervention stores | Treatm. N = 826 Control n = 278 | Normal population | Sales data |
| Milliron et al. [66] * | Database search + Adam and Jensen [28] + Liberato et al. [31] + Hartman et al. [30] + Cameron et al. [29] | USA | Grocery store | RCT | Treatments assigned were:
| Increase in volume sales of saturated-fat (g/1000 kcals), and servings of fruits, vegetables (servings/1000 kcals) | 16 weeks baseline and 16 weeks intervention | 1 intervention stores | Treatm. N = 70 Control n = 83 | Normal population | Self-reported |
| Papies et al. [58] * | Cameron et al. [29] | Netherlands | Grocery store | RCT | Treatments assigned were:
| Reduction in volume sales of units of unhealthy snacks sold (e.g., sum of units of cake cookies, sweets chocolate, chips and other savory and nut snacks purchased) | n.a. | 1 intervention stores | Treatm. N = 49 Control n = 50 | Targeting overweight or obesity customers and normal population | Sales data |
| Patterson et al. [77] | Escaron et al. [25] + van ’t Riet [24] + Cameron et al. [29] | USA | Grocery store | ITS | Treatment part of the American Nutrition for a Lifetime System program called “Eat for Health” administered by the American National Cancer Institute. Treatments assigned were:
| Increase in total volume sales of product categorized as healthy and reduction in products categorized as unhealthy. Total of 8 food categories | 52 weeks baseline 24 and 104 weeks intervention | 20 control stores and 20 intervention stores | n = 1,920,000 | Normal population | Sales data |
| Polacsek et al. [54] * | Database search | USA | Grocery store | RCT | Treatments assigned were:
| Increase in overall dollars spent on fruits and vegetables | 12 weeks baseline and 16 weeks intervention | 1 intervention stores | Treatm. N = 183 Control n = 171 | Low-income neighborhood | Sales data |
| Rahkovsky et al. [73] * | Database search | USA | Grocery store | CBA | Treatments assigned were:
| Increase in total volume sales of product categorized as healthy (e.g., products with 3-stars). Reduction in total volume sales of product categorized as unhealthy (e.g., unstarred). | 52 weeks baseline and 88 weeks intervention | 134 intervention stores | After n = 11,658 Before n = 7102 | Normal population | Sales data |
| Sacks et al. [78] | Hersey et al. [27] | United Kingdom | Grocery store | ITS | Treatments assigned were:
| Increase in volume sales of product categorized as healthy (e.g., green-labeled). Reduction in volume sales of product categorized as unhealthy (red-labeled). Product categories were chilled prepackaged meals (ready meals) and fresh prepackaged sandwiches products. | 4 weeks baseline and 4 weeks intervention | 1 intervention stores | After n = 11,658 Before n = 7102 | Normal population | Sales data |
| Salmon et al. [79] * | Adam and Jensen [28] + Cameron et al. [29] | Netherlands | Grocery store | RCT | Treatments assigned were:
| Increase in volume sales in one healthier low fat cheese | 4 days baseline and 4 days intervention | 1 intervention stores | Treatm. N = 32 Control n = 41 | Normal population | Sales data |
| Sigurdsson et al. [67] | Cameron et al. [29] | Norway | Grocery store | ITS | Treatments assigned were:
| Increase sales volume of banana as proportion of total sales of fruits. | 4 weeks baseline and 4 weeks intervention | 1 intervention stores | n.a. | Normal population | Sales data |
| Steenhuis et al. [82] * | Database search | Netherlands | Grocery store | RCT | Treatments assigned were:
| Reduction in participants average fat intake | 4 weeks baseline and 24 weeks intervention | 4 control stores and 9 intervention stores | Treatm. N = 1464 Control n = 739 | Normal population | Self-reported |
| Thorndike et al. [53] * | Hartman et al. [30] | USA | Grocery store | RCT | Treatments assigned were:
| Increase in volume sales of fruits and vegetables | 44 weeks baseline 22, weeks intervention and 20 week follow-up | 3 control stores and 3 intervention stores | Treatm. N = 295 Control n = 280 | Low-income neighborhood | Self-reported |
| Walmsley et al. [68] * | Database search | United Kingdom | Grocery store | ITS | Treatments assigned were:
| Increase in volume sales of fruits and vegetables | 90 weeks baseline and 80 weeks intervention | 1 intervention stores | Treatm. N = 5464 Control n = 5790 | Normal population | Sales data |
| Waterlander et al. [69] * | Database search + Afshin et al. [87] + Adam and Jensen [28] + Liberato et al. [31] + Hartman et al. [30] | Netherlands | Grocery store | RCT | Treatments assigned were:
| Increase in volume sales of fruits and vegetables (kg per household for 2 week intervals) | 2 weeks baseline, 24 weeks intervention and 24 weeks follow-up | 1 control stores and 3 intervention stores | Treatm. n = 115 Control n = 36 | Normal population | Sales data |
| Winett et al. [70] * | van ’t Riet [24] + Hartman et al. [30] + Cameron et al. [29] + Cadario and Chandon [15] + Liberato et al. [31] | USA | Grocery store | RCT | Treatment part of a modified version of the Nutrition for a Lifetime System program administered via kiosks in supermarkets. Treatments assigned were:
| Reduction in % intake of calories from total fat, increase in gram fiber and increase in servings of fruits and vegetables | 10 weeks intervention and 4 weeks follow-up | 2 intervention stores | Treatm. n = 54 Control n = 51 | Normal population | Sales data |
| Intervention | Frequency (k) | ES (d) | CI Lower Limit | CI Higher Limit |
|---|---|---|---|---|
| Promotion and pricing | 17 | 0.21 * | 0.08 | 0.33 |
| Promotion | 15 | 0.10 * | 0.02 | 0.18 |
| Promotion and proximity | 12 | 0.01 * | 0.00 | 0.02 |
| Pricing | 11 | 0.40 * | 0.00 | 0.80 |
| Prompting | 12 | 0.14 * | 0.09 | 0.19 |
| Pricing and prompting | 1 | 0.52 * | 0.27 | 0.76 |
| Promotion and prompting | 1 | 0.02 | −0.20 | 0.24 |
| Healthy default picks | 1 | 0.52 * | 0.30 | 0.75 |
| Profile and Proximity | 1 | 0.04 | −0.20 | 0.29 |
| Proximity | 1 | −0.06 | −0.39 | 0.28 |
| Target Product Category | Frequency (k) | ES (d) | CI Lower Limit | CI Higher Limit |
|---|---|---|---|---|
| Increase healthy products | 46 | 0.19 * | 0.09 | 0.29 |
| Fruit and vegetables | 21 | 0.28 * | 0.08 | 0.48 |
| Healthy beverage | 10 | 0.01 * | 0.01 | 0.02 |
| Total volume healthy | 8 | 0.16 * | 0.14 | 0.17 |
| Fiber | 5 | 0.29 | −0.17 | 0.76 |
| Low-calorie snacks | 1 | −0.25 | −0.77 | 0.27 |
| Low-fat cheese | 1 | 0.19 * | −0.04 | 0.42 |
| Reduction less healthy products | 26 | 0.11 * | 0.03 | 0.19 |
| Fat | 7 | 0.19 | −0.01 | 0.39 |
| Unhealthy beverage | 7 | 0.09 | −0.07 | 0.25 |
| Total volume unhealthy | 6 | −0.03 | −0.19 | 0.12 |
| Calorie | 3 | 0.07 | −0.06 | 0.20 |
| Certainty Assessment | Summary of Findings | ||||||
|---|---|---|---|---|---|---|---|
| No of Studies | Risk of bias | Inconsistency | Indirectness | Imprecision | Publication Bias | Overall Certainty of Evidence | SMD Effect Size 95% CI |
| RCT studies | |||||||
| 22 | Very serious | Serious | Not serious | Serious | None | ⨁◯◯◯ Very low | 0.18 [0.10, 0.26] |
| CBA studies | |||||||
| 6 * | Serious | Not serious | Not serious | Serious | NA *** | Low | 0.14 [−0.01, 0.30] |
| ITS studies | |||||||
| 8 ** | Not serious | Not serious | Not serious | Not serious | NA *** | Low | −0.01 [−0.11, 0.09] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Slapø, H.; Schjøll, A.; Strømgren, B.; Sandaker, I.; Lekhal, S. Efficiency of In-Store Interventions to Impact Customers to Purchase Healthier Food and Beverage Products in Real-Life Grocery Stores: A Systematic Review and Meta-Analysis. Foods 2021, 10, 922. https://doi.org/10.3390/foods10050922
Slapø H, Schjøll A, Strømgren B, Sandaker I, Lekhal S. Efficiency of In-Store Interventions to Impact Customers to Purchase Healthier Food and Beverage Products in Real-Life Grocery Stores: A Systematic Review and Meta-Analysis. Foods. 2021; 10(5):922. https://doi.org/10.3390/foods10050922
Chicago/Turabian StyleSlapø, Helena, Alexander Schjøll, Børge Strømgren, Ingunn Sandaker, and Samira Lekhal. 2021. "Efficiency of In-Store Interventions to Impact Customers to Purchase Healthier Food and Beverage Products in Real-Life Grocery Stores: A Systematic Review and Meta-Analysis" Foods 10, no. 5: 922. https://doi.org/10.3390/foods10050922
APA StyleSlapø, H., Schjøll, A., Strømgren, B., Sandaker, I., & Lekhal, S. (2021). Efficiency of In-Store Interventions to Impact Customers to Purchase Healthier Food and Beverage Products in Real-Life Grocery Stores: A Systematic Review and Meta-Analysis. Foods, 10(5), 922. https://doi.org/10.3390/foods10050922






