Clinicians’ Publication Output: Self-Report Survey and Bibliometric Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Sample and Setting
2.2. Ethics Approval
2.3. Measures
2.3.1. Demographics
2.3.2. Primary Outcome Measure
2.3.3. Researching Habits
2.3.4. Journal Selection Metrics
2.3.5. Pilot Testing and Veracity
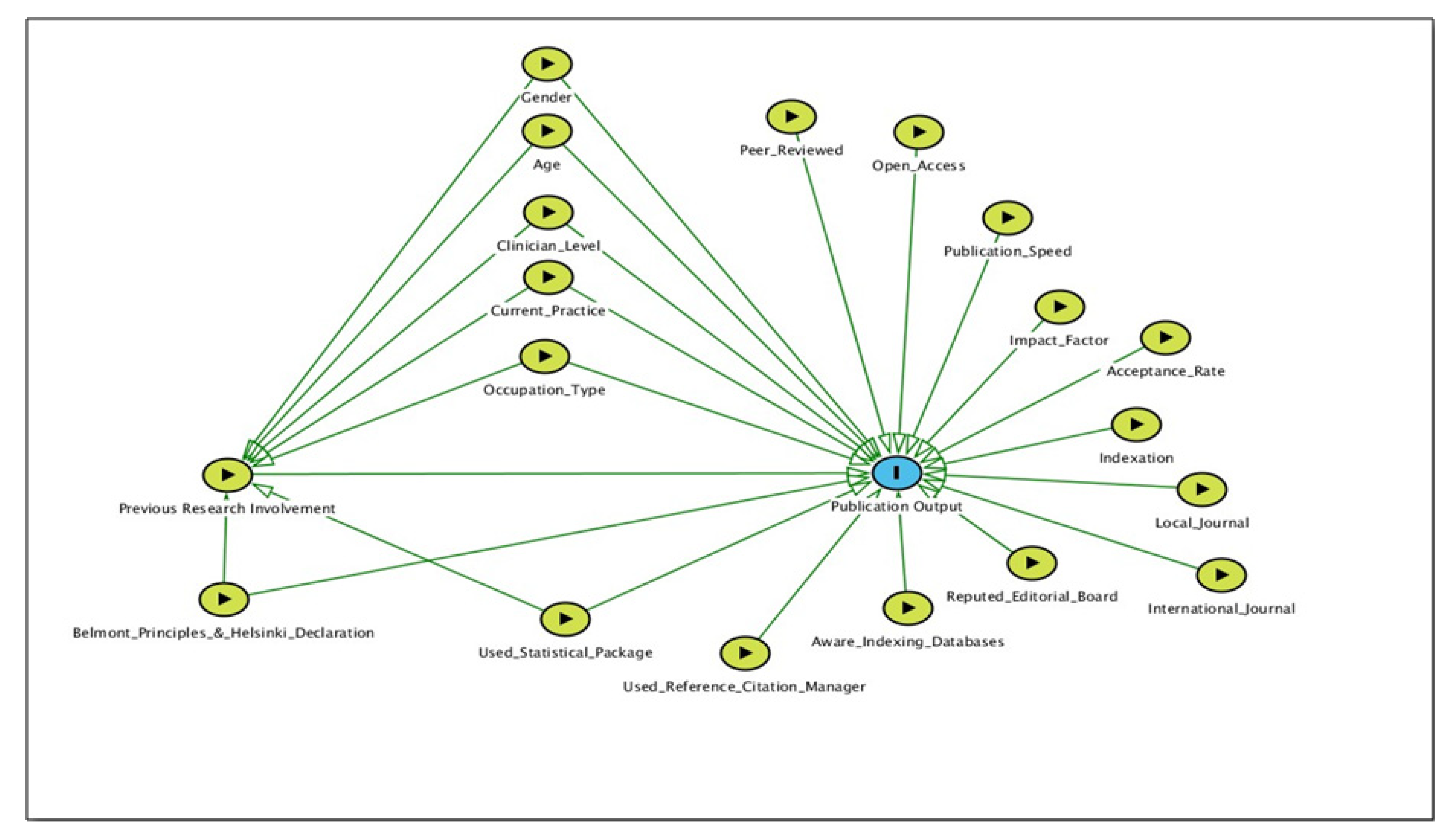
2.3.6. Visualizing Variable Associations
2.4. Data Analyses
2.4.1. Analyses of Self-Report Survey
2.4.2. Bibliometric Analyses
3. Results
3.1. Sample Characteristics
3.2. Clinicians’ Researching Habits
3.3. Clinicians’ Journal Selection Attributes
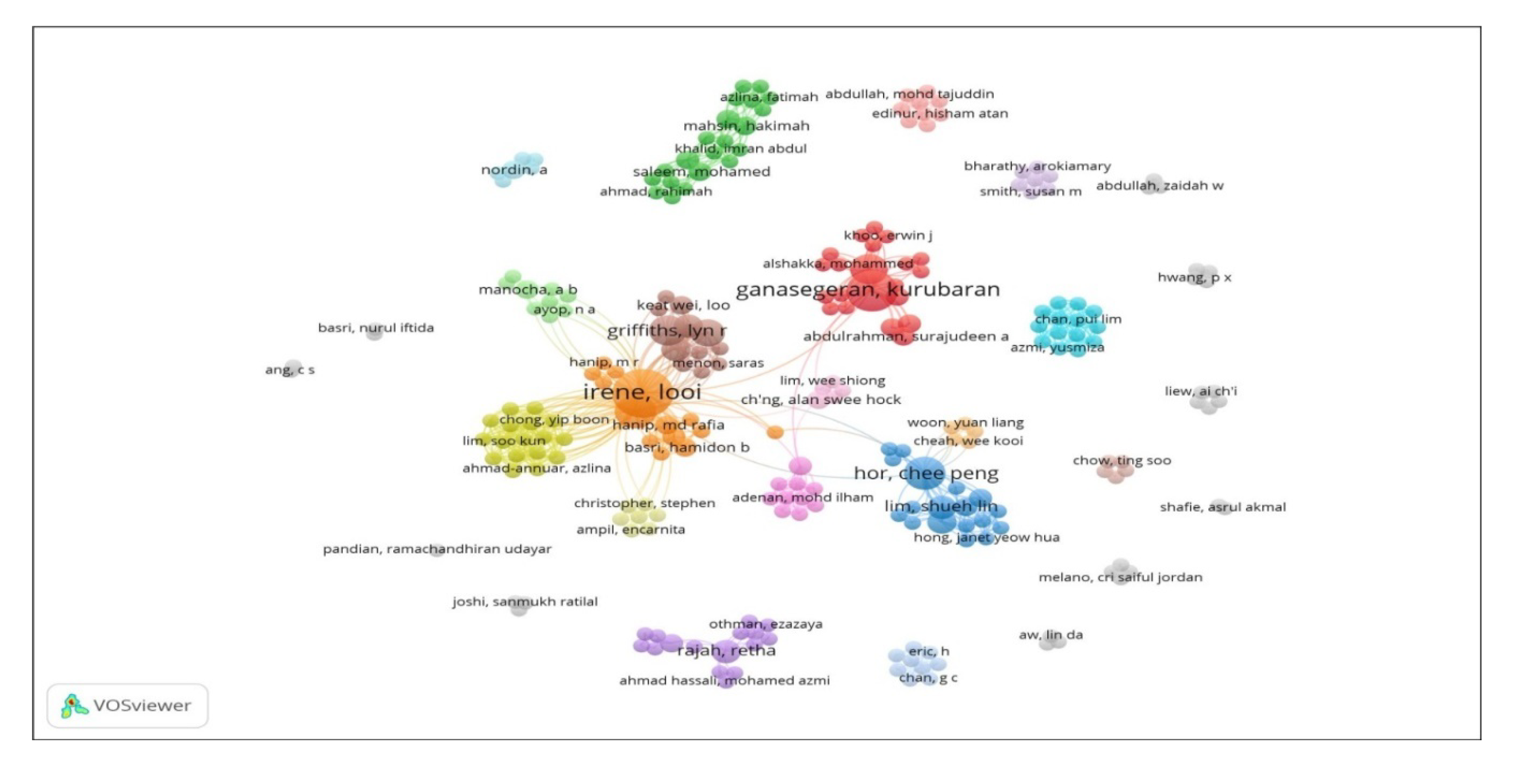
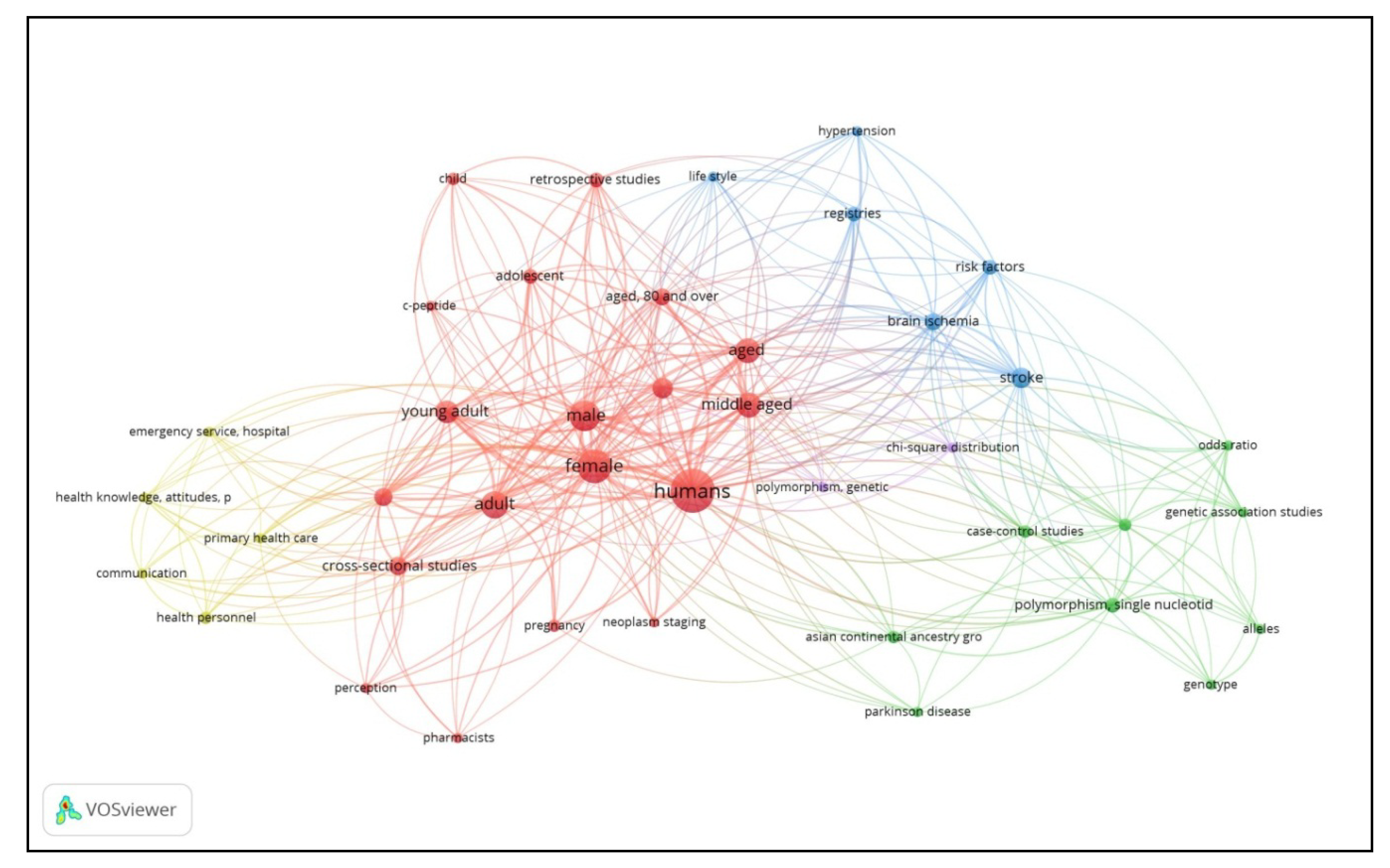
3.4. Bibliometric Analysis
3.5. Association between Sample Characteristics, Researching Habits and Publication Output
3.6. Association between Journal Selection Attributes and Publication Output
3.7. Factors Associated with Clinicians’ Publication Output by Multiple Logistic Regression Analysis
4. Discussion
4.1. Findings, Consistencies and Plausibilities from Self-Report Survey
4.2. Findings from Bibliometric Analysis
4.3. Study Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Baud, D.; Gubler, D.J.; Schaub, B.; Lanteri, M.C.; Musso, D. An update on Zika virus infection. Lancet 2017, 390, 2099–2109. [Google Scholar] [CrossRef]
- da Silva, I.R.F.; Frontera, J.A.; Bispo de Filippis, A.M.; Nascimento, O.J.M.D.; RIO-GBS-ZIKV Research Group. Neurologic complications associated with the Zika virus in Brazilian adults. JAMA Neurol. 2017, 74, 1190–1198. [Google Scholar] [CrossRef] [PubMed]
- Marusic, M. Why physicians should publish, how easy it is, and how important it is in clinical work. Arch. Oncol. 2003, 11, 59–64. [Google Scholar] [CrossRef]
- Noorden, R.V. Five in Asia. Nature 2018, 558, 500–501. [Google Scholar] [PubMed]
- National Institutes of Health, Ministry of Health Malaysia. Available online: http://nih.gov.my/web/ (accessed on 25 September 2019).
- Clinical Research Centre, Ministry of Health Malaysia. Available online: http://www.crc.gov.my/ (accessed on 25 September 2019).
- Seaburg, L.A.; Wang, A.T.; West, C.P.; Reed, D.A.; Halvorsen, A.J.; Engstler, G.; Oxentenko, A.S.; Beckman, T.J. Associations between resident physicians’ publications and clinical performance during residency training. BMC Med. Educ. 2016, 16, 22. [Google Scholar] [CrossRef] [PubMed]
- McGrail, M.R.; Rickard, C.M.; Jones, R. Publish or perish: A systematic review of interventions to increase academic publication rates. High. Educ. Res. Dev. 2006, 25, 19–35. [Google Scholar] [CrossRef]
- Khan, H.; Khan, S.; Iqbal, A. Knowledge, attitudes and practices around health research: The perspective of physicians-in-training in Pakistan. BMC Med Educ. 2009, 9, 46. [Google Scholar] [CrossRef]
- Olusegun, N.S.; Olayinka, A.M.; Modupe, S.; Ikenna, I.G. Determinants of journal choice among Nigerian medics. Pan Afr. Med. J. 2015, 21, 148. [Google Scholar] [CrossRef]
- Zou, Y.; Li, Q.; Xu, W. Scientific research output in orthopaedics from China and other top-ranking countries: A 10-year survey of the literature. BMJ Open 2016, 6, e011605. [Google Scholar] [CrossRef]
- Garfield, E. Citation indexes for science: A new dimension in documentation through association of ideas. Science 1955, 122, 108–111. [Google Scholar] [CrossRef]
- Choi, J.; You, J.S.; Joo, Y.S.; Kong, T.; Ko, D.R.; Chung, S.P. A bibliometric analysis of research productivity of emergency medicine researchers in South Korea. Clin. Exp. Emerg. Med. 2016, 3, 245–251. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Tess, B.H.; Furuie, S.S.; Castro, R.C.F.; Barreto, M.D.C.C.; Nobre, M.R.C. Assessing the scientific research productivity of a Brazilian healthcare institution: A case study at the Heart Institute of Sau Paulo, Brazil. Clinics 2009, 64, 571–576. [Google Scholar] [CrossRef] [PubMed]
- Matthiessen, C.W.; Schwarz, A.W. Scientific centres in Europe: An analysis of research strength and patterns of specialisation based on bibliometric indicators. Urban Stud. 1999, 36, 453–477. [Google Scholar] [CrossRef]
- Zhou, P.; Thijs, B.; Glanzel, W. Regional analysis on Chinese scientific output. Scientometrics 2009, 81, 839–857. [Google Scholar] [CrossRef]
- Penang State Health Department. Available online: http://jknpenang.moh.gov.my/jknpenang/index.php/my/ (accessed on 1 September 2018).
- Malaysia Public Service Department Service Scheme. Available online: http://www.jpa.gov.my/index.php?option=com_content&view=article&id=2609&Itemid=1052&lang=en (accessed on 1 September 2018).
- Malaysian Medical Register of Malaysian Medical Council. Available online: http://www.mmc.gov.my/index.php/medical-register (accessed on 1 September 2018).
- Bonilla-Escobar, F.J.; Bonilla-Velez, J.; Tobon-Garcia, D.; Ángel-Isaza, A.M. Medical student researchers in Colombia and associated factors with publication: A cross-sectional study. BMC Med. Educ. 2017, 17, 254. [Google Scholar] [CrossRef]
- Niwa, N.; Kikuchi, E.; Matsumoto, K.; Miyajima, A.; Oya, M. Influence of physician years on urological journal publication productivity among Japanese urologists. SpringerPlus 2016, 5, 2040. [Google Scholar] [CrossRef]
- Bovijn, J.; Kajee, N.; Esterhuizen, T.M.; Van Schalkwyk, S.C. Research involvement among undergraduate health sciences students: A cross-sectional study. BMC Med. Educ. 2017, 17, 186. [Google Scholar] [CrossRef]
- Textor, J.; van der Zander, B.; Gilthorpe, M.S.; Liskiewicz, M.; Ellison, G.T.H. Robust causal inference using directed acyclic graphs: The R package “dagitty”. Int. J. Epidemiol. 2016, 45, 1887–1894. [Google Scholar] [CrossRef]
- Merani, S.; Switzer, N.; Kayssi, A.; Blitz, M.; Ahmed, N.; Shapiro, A.M.J. Research productivity of residents and surgeons with formal research training. J. Surg. Educ. 2014, 71, 865–870. [Google Scholar] [CrossRef]
- Kanna, B.; Deng, C.; Erickson, S.N.; Valerio, J.A.; Dimitrov, V.; Soni, A. The research rotation: Competency-based structured and novel approach to research training of internal medicine residents. BMC Med. Educ. 2006, 6, 52–60. [Google Scholar] [CrossRef]
- Duclos, A.; Herquelot, E.; Polazzi, S.; Malbezin, M.; Claris, O. Performance curves of medical researchers during their career: Analysis of scientific production from a retrospective cohort. BMJ Open 2017, 7, e013572. [Google Scholar] [CrossRef]
- Buddeberg-Fischer, B.; Leemann, R.; Klaghofer, R. Socio-demographic and career aspects in female and male faculty members of Swiss medical schools. Swiss. Med. Wkly. 2003, 133, 318–322. [Google Scholar]
- Fridner, A.; Norell, A.; Akesson, G.; Senden, M.G.; Lovseth, L.T.; Schenck-Gustafsson, K. Possible reasons why female physicians publish fewer scientific articles than male physicians—A cross-sectional study. BMC Med. Educ. 2015, 15, 67. [Google Scholar] [CrossRef] [PubMed]
- Fox, M.F. Publication productivity among scientist: A critical review. Soc. Stud. Sci. 1983, 13, 285–305. [Google Scholar] [CrossRef]
- Verhaegen, P.; Salthouse, T.A. Meta-analyses of age-cognition relations in adulthood. Estimates of linear and non-linear age effects and structural models. Psychol. Bull. 1997, 122, 231–249. [Google Scholar] [CrossRef] [PubMed]
- Yang, G.; Zaid, U.B.; Erickson, B.A.; Blaschko, S.D.; Carroll, P.R.; Breyer, B.N. Urology resident publication output and its relationship to future academic achievement. J. Urol. 2011, 185, 642–646. [Google Scholar] [CrossRef] [PubMed]
- Merton, R.K. Social Theory and Social Structure; The Free Press: New York, NY, USA, 1968. [Google Scholar]
- Merton, R.K. The Sociology of Science: Theoretical and Empirical Investigations; University of Chicago Press: Chicago, IL, USA, 1973. [Google Scholar]
- Gingras, Y.; Lariviere, V.; Macaluso, B.; Robitaille, J.P. The effects of aging on researchers’ publication and citation patterns. PLoS ONE 2008, 3, e4048. [Google Scholar] [CrossRef] [PubMed]
- Choo, T.L.; Muninathan, P.; Pung, C.M.; Ramanathan, G.R.L. Attitudes, barriers and facilitators to the conduct of research in government hospitals: A cross-sectional study among specialists in government hospitals, northern states of Malaysia. Med. J. Malaysia. 2017, 72, 26–31. [Google Scholar]
- Omolase, C.O.; Egberongbe, A.A.; Komolafe, O.O.; Olasinde, A.A.; Omolase, B.O.; Adeosun, O.A. Practice of bio-medical research amongst doctors in Owo. J. S. Afr. Fam. Pract. 2015, 57, 112–115. [Google Scholar] [CrossRef]
- Carneiro, I.; Howard, N.; Bailey, L.; Vardulaki, K.; Langham, J.; Chandramohan, D. Introduction to Epidemiology—Interpreting Associations, 2nd ed.; London School of Hygiene, McGraw Hill—Open University Press: Berkshire, UK, 2011. [Google Scholar]
- Kali, A. Reference management: A critical element of scientific writing. J. Adv. Pharm. Technol. Res. 2016, 7, 27–29. [Google Scholar] [CrossRef]
- Schimmer, R. The transformation of scientific journal publishing: Open Access after the Berlin 12 Conference. Inf. Serv. Use 2017, 37, 7–11. [Google Scholar] [CrossRef]
- Wallach, J.D.; Egilman, A.C.; Gopal, A.D.; Swami, N.; Krumholz, H.M.; Ross, J.S. Biomedical journal speed and efficiency: A cross-sectional pilot survey of author experiences. Res. Integr. Peer. Rev. 2018, 3, 1. [Google Scholar] [CrossRef] [PubMed]
- Faxon, D.P. Changes in medical publishing—The challenges for an interventional journal. Circ. Cardiovasc. Interv. 2013, 6, 2–4. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Bean, R.B.; Bean, W.B. Sir William Osler: Aphorisms from His bedside Teachings and Writings; Hardcover Charles C. Thomas: Springfield, IL, USA, 1961. [Google Scholar]
- Koseoglu, M.A. Growth and structure of authorship and co-authorship network in the strategic management realm: Evidence from the Strategic Management Journal. BRQ Bus. Res. Q. 2016, 19, 153–170. [Google Scholar] [CrossRef]
- Zupic, I.; Cater, T. Bibliometric methods in management and organization. Organ. Res. Methods 2015, 18, 429–472. [Google Scholar] [CrossRef]
- Adigwe, I. Lotka’s Law and productivity patterns of authors in biomedical science in Nigeria on HIV/AIDS. Electron. Libr. 2016, 34, 789–807. [Google Scholar] [CrossRef]
- Nwagwu, W.E. Patterns of authorship in the biomedical literature of Nigeria. Libr. Inf. Sci. Res. Electron. J. 2007, 17, 1–28. [Google Scholar]
- Lotka, A.J. The frequency distribution of scientific productivity. J. Wash. Acad. Sci. 1926, 16, 317–323. [Google Scholar]
- Nwagwu, W.E. A bibliometric analysis of productivity patterns of biomedical authors of Nigeria during 1967–2002. Scientometrics 2006, 9, 259–269. [Google Scholar] [CrossRef]
| Characteristics | n (%) |
|---|---|
| Gender | |
| Men | 77 (38.3) |
| Women | 124 (61.7) |
| Age group (years) | |
| ≤30 | 90 (44.8) |
| >30 | 111 (55.2) |
| Clinician level | |
| Young clinician | 166 (82.6) |
| Senior clinician | 35 (17.4) |
| Current practice | |
| Medicine and allied | 82 (40.8) |
| Surgery and allied | 75 (37.3) |
| Others | 44 (21.9) |
| Occupation type | |
| Consultants/Clinical specialists | 38 (18.9) |
| Medical officers | 163 (81.1) |
| Previous involvement in research | |
| Yes | 106 (52.7) |
| No | 95 (47.3) |
| Ever used reference citation manager like ReadCube/Mendeley/EndNote/Zotero | |
| Yes | 38 (18.9) |
| No | 163 (81.1) |
| Ever used statistical package like SPSS/STATA | |
| Yes | 122 (60.7) |
| No | 79 (39.3) |
| Aware about major indexing databases like PubMed/Scopus/EBSCO, PsychInfo | |
| Yes | 137 (68.2) |
| No | 64 (31.8) |
| Awareness of Belmont Principles and Helsinki Declaration | |
| Yes | 41 (20.4) |
| No | 160 (79.6) |
| Published a scientific paper | |
| Yes | 34 (16.9) |
| No | 167 (83.1) |
| Characteristics | n (%) |
|---|---|
| Peer reviewed | |
| Lesser | 109 (54.2) |
| Greater | 92 (45.8) |
| Open access | |
| Lesser | 90 (44.8) |
| Greater | 111 (55.2) |
| Submission to publication speed | |
| Lesser | 91 (45.3) |
| Greater | 110 (54.7) |
| Impact factor | |
| Lesser | 69 (34.3) |
| Greater | 132 (65.7) |
| Manuscript acceptance rate | |
| Lesser | 87 (43.3) |
| Greater | 114 (56.7) |
| Journal indexations | |
| Lesser | 119 (59.2) |
| Greater | 82 (40.8) |
| Local journal (Malaysian) | |
| Lesser | 95 (47.3) |
| Greater | 106 (52.7) |
| International journal | |
| Lesser | 61 (30.3) |
| Greater | 140 (69.7) |
| Reputable editorial board | |
| Lesser | 68 (33.8) |
| Greater | 133 (66.2) |
| Cluster | Concepts Group | Keywords Occurrence |
|---|---|---|
| 1 (19 items) | Observational studies involving human subjects | Humans (33), female (19), male (16), adult (13), aged (11), middle aged (11), young adult (9), prospective studies (7), cross-sectional studies (6), surveys and questionnaire (6), aged 80 and above (5), retrospective studies (4), adolescent (4), child (3), pregnancy (3), neoplasm staging (2), c-peptide (2), perception (2), pharmacists (2) |
| 2 (9 items) | Genetic related studies | Polymorphism, single nucleotide (4), asian continental ancestry group (3), case-control studies (3), genetic predisposition to disease, alleles (2), genetic association study (2), genotype (2), odds ratio (2), parkinson disease (2). |
| 3 (6 items) | Stroke research | Stroke (7), brain ischemia (5), registries (4), risk factors (4), hypertension (2), lifestyle (2). |
| 4 (5 items) | Health services and systems research | Primary health care (4), health personnel (3), emergency service hospital (2), communication (2), health knowledge, attitude, practice (2) |
| 5 (2 items) | Overlap cluster | Chi-square distribution (2), polymorphism, genetic (2) |
| Characteristics | Published a Scientific Paper | OR | 95% CI | p-Value | |
|---|---|---|---|---|---|
| Yes n (%) | No n (%) | ||||
| Gender | |||||
| Men | 16 (20.8) | 61 (79.2) | 1.5 | 0.7–3.2 | 0.250 |
| Women | 18 (14.5) | 106 (85.5) | 1 | ||
| Age group (years) | |||||
| ≤30 | 16 (17.8) | 74 (82.2) | 1 | ||
| >30 | 18 (16.2) | 93 (83.8) | 0.9 | 0.4–2.0 | 0.769 |
| Clinician level | |||||
| Young clinician | 23 (13.9) | 143 (86.1) | 1 | ||
| Senior clinician | 11 (31.4) | 24 (68.6) | 2.8 | 1.2–6.6 | 0.012 |
| Current practice | |||||
| Medical based | 11 (13.4) | 71 (86.6) | 0.5 | 0.2–1.4 | 0.186 |
| Surgical based | 13 (17.3) | 62 (82.7) | 0.7 | 0.3–1.6 | 0.473 |
| Others | 10 (22.7) | 34 (77.3) | 1 | ||
| Occupation type | |||||
| Consultants/Clinician specialists | 14 (36.8) | 24 (63.2) | 4.2 | 1.9–9.4 | <0.001 |
| Medical officer | 20 (12.3) | 143 (87.7) | 1 | ||
| Previous involvement in research | |||||
| Yes | 28 (26.4) | 78 (73.6) | 5.3 | 2.1–13.5 | <0.001 |
| No | 6 (6.3) | 89 (93.7) | 1 | ||
| Ever used reference citation manager like ReadCube/Mendeley/EndNote/Zotero | |||||
| Yes | 14 (36.8) | 24 (63.2) | 4.2 | 1.9–9.4 | <0.001 |
| No | 20 (12.3) | 143 (87.7) | 1 | ||
| Ever used statistical package like SPSS/STATA | |||||
| Yes | 29 (23.8) | 93 (76.2) | 4.6 | 1.7–12.5 | 0.001 |
| No | 5 (6.3) | 74 (93.7) | 1 | ||
| Aware about major indexing databases like PubMed/Scopus/EBSCO, PsychInfo | |||||
| Yes | 29 (21.2) | 108 (78.8) | 3.2 | 1.2–8.6 | 0.019 |
| No | 5 (7.8) | 59 (92.2) | 1 | ||
| Awareness of Belmont Principles and Helsinki Declaration | |||||
| Yes | 12 (29.3) | 29 (70.7) | 2.6 | 1.2–5.8 | 0.018 |
| No | 22 (13.8) | 138 (86.3) | 1 | ||
| Characteristics | Published a Scientific Paper | OR | 95% CI | p-Value | |
|---|---|---|---|---|---|
| Yes n (%) | No n (%) | ||||
| Peer reviewed | |||||
| Lesser | 12 (11.0) | 97 (89.0) | 1 | ||
| Greater | 22 (23.9) | 70 (76.1) | 2.5 | 1.1–5.5 | 0.015 |
| Open access | |||||
| Lesser | 10 (11.1) | 80 (88.9) | 1 | ||
| Greater | 24 (21.6) | 87 (78.4) | 2.2 | 0.9–4.9 | 0.048 |
| Submission to publication speed | |||||
| Lesser | 10 (11.0) | 81 (89.0) | 1 | ||
| Greater | 24 (21.8) | 86 (78.2) | 2.2 | 1.1–5.0 | 0.041 |
| Impact factor | |||||
| Lesser | 5 (7.2) | 64 (92.8) | 1 | ||
| Greater | 29 (22.0) | 103 (78.0) | 3.6 | 1.3–9.8 | 0.008 |
| Manuscript acceptance rate | |||||
| Lesser | 9 (10.3) | 78 (89.7) | 1 | ||
| Greater | 25 (21.9) | 89 (78.1) | 2.4 | 1.1–5.5 | 0.030 |
| Journal indexations | |||||
| Lesser | 18 (15.1) | 101 (84.9) | 1 | ||
| Greater | 16 (19.5) | 66 (80.5) | 1.3 | 0.6–2.9 | 0.415 |
| Local journal | |||||
| Lesser | 14 (14.7) | 81 (85.3) | 1 | ||
| Greater | 20 (18.9) | 86 (81.1) | 1.3 | 0.6–2.8 | 0.435 |
| International journal | |||||
| Lesser | 5 (8.2) | 56 (91.8) | 1 | ||
| Greater | 29 (20.7) | 111 (79.3) | 2.9 | 1.1–8.0 | 0.030 |
| Reputable editorial board | |||||
| Lesser | 10 (14.7) | 58 (85.3) | 1 | ||
| Greater | 24 (18.2) | 108 (81.8) | 1.3 | 0.6–2.9 | 0.535 |
| Characteristics | B | SE | Wald | Exp (B) | 95% CI | p-Value |
|---|---|---|---|---|---|---|
| Occupation type | ||||||
| Consultants/Clinician specialists | 1.1 | 0.4 | 5.2 | 2.5 | 1.1–10.0 | 0.023 |
| Medical officer | Ref | Ref | Ref | Ref | Ref | Ref |
| Previous involvement in research | ||||||
| Yes | 1.4 | 0.5 | 8.3 | 4.2 | 1.5–11.4 | 0.004 |
| No | Ref | Ref | Ref | Ref | Ref | Ref |
| Ever used reference citation manager like ReadCube/Mendeley/EndNote/Zotero | ||||||
| Yes | 1.1 | 0.4 | 6.6 | 3.2 | 1.3–7.7 | 0.010 |
| No | Ref | Ref | Ref | Ref | Ref | Ref |
| Submission to publication speed | ||||||
| Lesser | Ref | Ref | Ref | Ref | Ref | Ref |
| Greater | 1.1 | 0.4 | 5.5 | 2.9 | 1.2–7.1 | 0.019 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ganasegeran, K.; Ch’ng, A.S.H.; Jamil, M.F.A.; Looi, I. Clinicians’ Publication Output: Self-Report Survey and Bibliometric Analysis. Publications 2020, 8, 15. https://doi.org/10.3390/publications8010015
Ganasegeran K, Ch’ng ASH, Jamil MFA, Looi I. Clinicians’ Publication Output: Self-Report Survey and Bibliometric Analysis. Publications. 2020; 8(1):15. https://doi.org/10.3390/publications8010015
Chicago/Turabian StyleGanasegeran, Kurubaran, Alan Swee Hock Ch’ng, Mohd Fadzly Amar Jamil, and Irene Looi. 2020. "Clinicians’ Publication Output: Self-Report Survey and Bibliometric Analysis" Publications 8, no. 1: 15. https://doi.org/10.3390/publications8010015
APA StyleGanasegeran, K., Ch’ng, A. S. H., Jamil, M. F. A., & Looi, I. (2020). Clinicians’ Publication Output: Self-Report Survey and Bibliometric Analysis. Publications, 8(1), 15. https://doi.org/10.3390/publications8010015





