Between Innovation and Standardization, Is There Still a Room for Scientific Reports? The Rise of a Formatting Tradition in Periodontal Research
Abstract
1. Introduction
2. The Rising Consensus
3. The Template
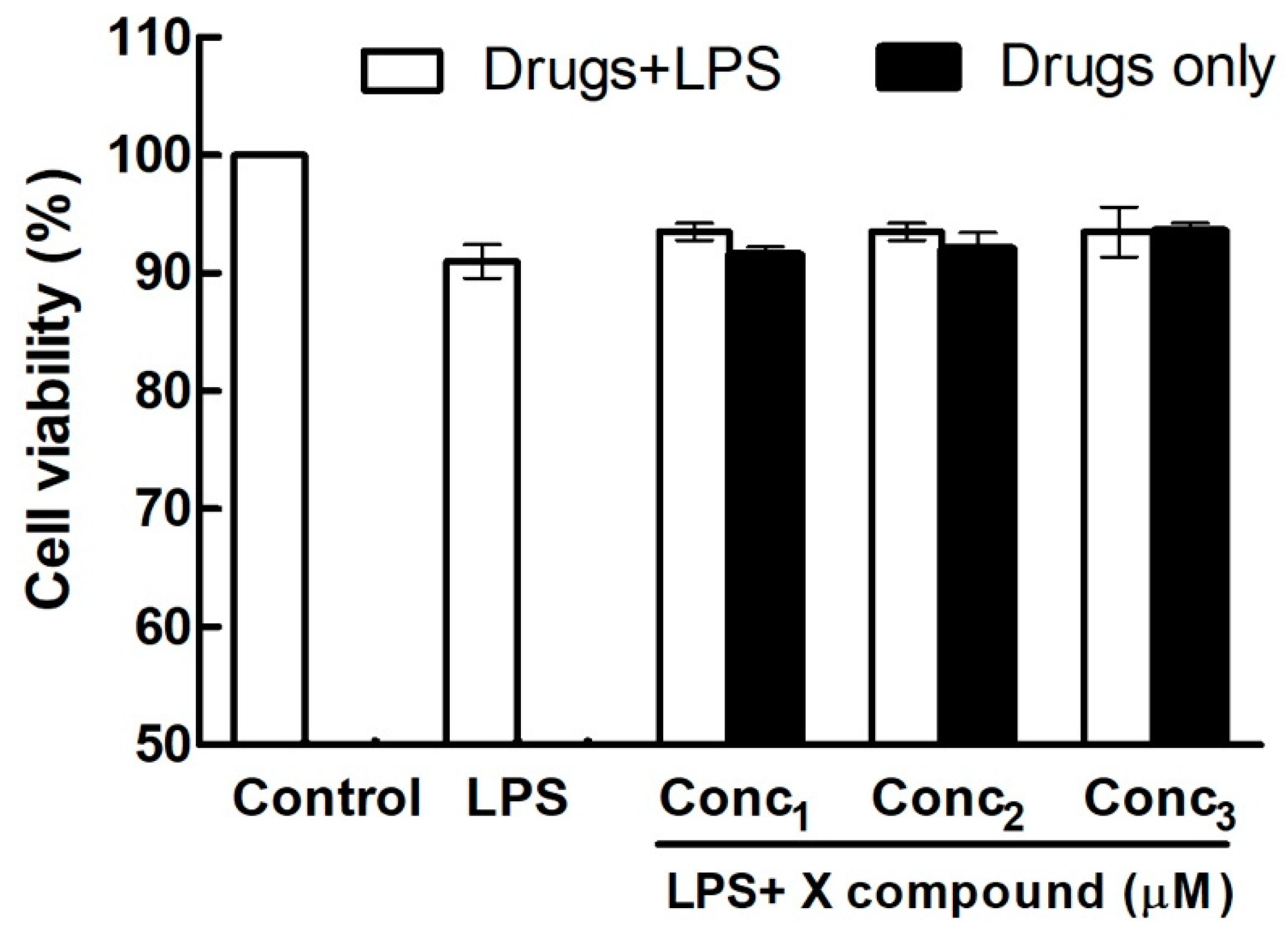
3.1. Figure 1
“Effects of X compound on the cell viability of HGFs. Cells were cultured with different concentrations of X compound in the absence or in the presence of 1 μg/mL LPS for 24 h. The cell viability was determined by MTT (or CCK-8, A/N) assay. The values presented are the means ± SEM of three independent experiments”.
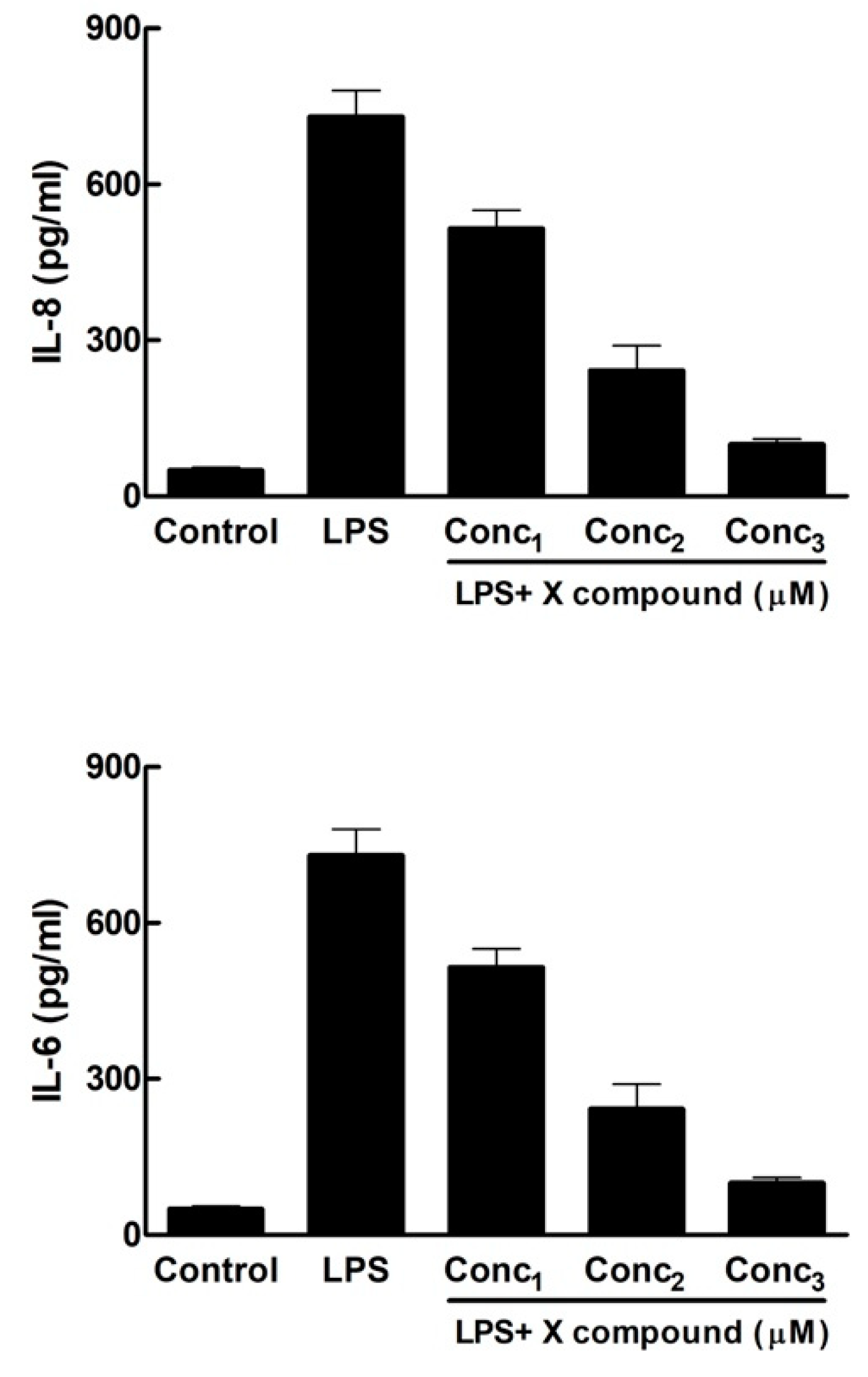
3.2. Figure 2
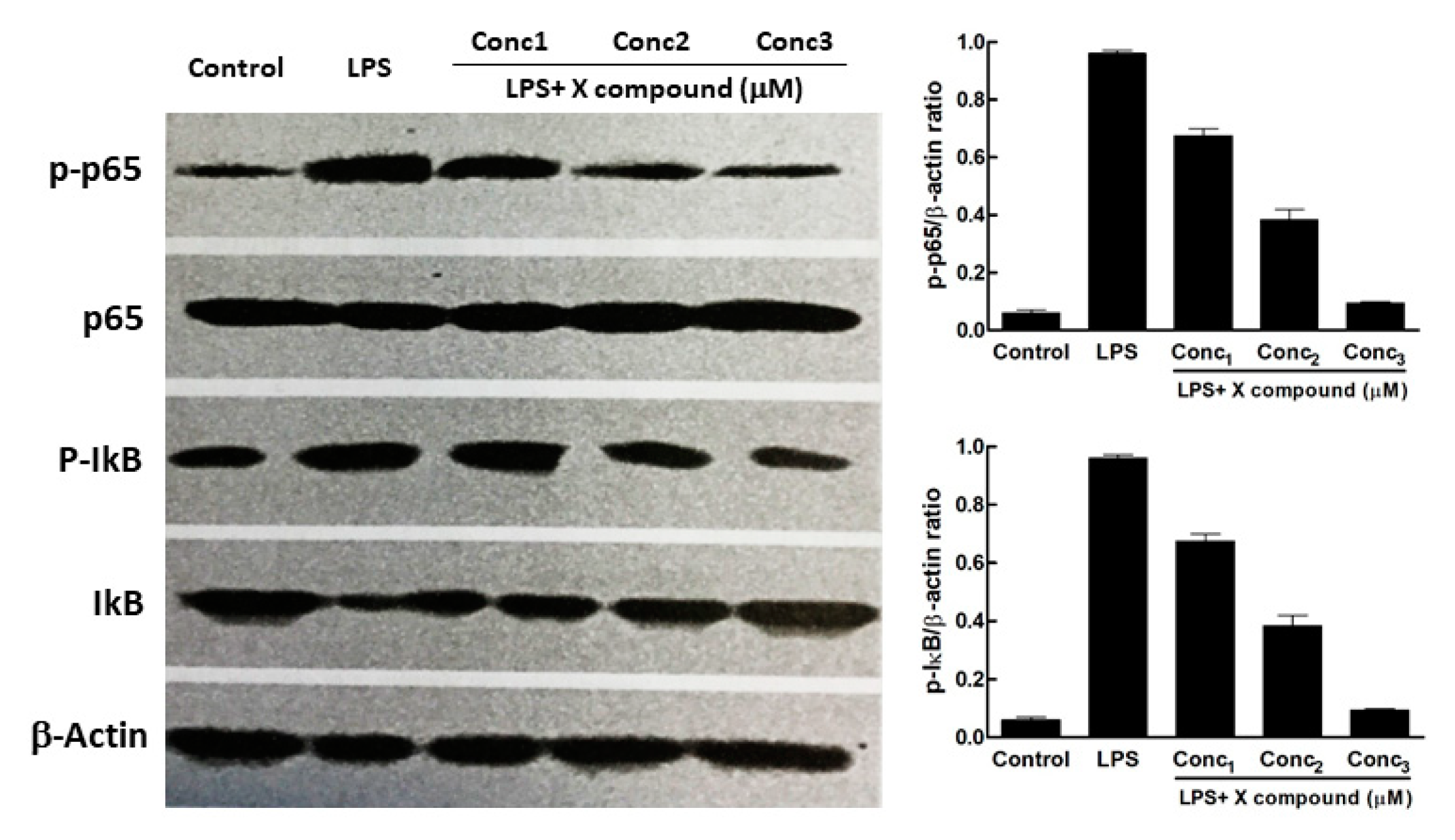
3.3. Figure 3
3.4. Figure 4
4. Establishing a Tradition
“Does X inhibit the inflammatory response triggered by LPS in human gingival fibroblasts?”
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Eke, P.I.; Dye, B.A.; Wei, L.; Slade, G.D.; Thornton-Evans, G.O.; Borgnakke, W.S.; Taylor, G.W.; Page, R.C.; Beck, J.D.; Genco, R.J. Update on Prevalence of Periodontitis in Adults in the United States: NHANES 2009 to 2012. J. Periodontol. 2015, 86, 611–622. [Google Scholar] [CrossRef] [PubMed]
- Kinane, D.F.; Stathopoulou, P.G.; Papapanou, P.N. Periodontal diseases. Nat. Rev. Dis. Prim. 2017, 3, 17038. [Google Scholar] [CrossRef] [PubMed]
- Germano, F.; Bramanti, E.; Arcuri, C.; Cecchetti, F.; Cicciù, M. Atomic force microscopy of bacteria from periodontal subgingival biofilm: Preliminary study results. Eur. J. Dent. 2013, 7, 152–158. [Google Scholar] [CrossRef] [PubMed]
- Fiorillo, L.; Cervino, G.; Herford, A.S.; Lauritano, F.; D’Amico, C.; Lo Giudice, R.; Laino, L.; Troiano, G.; Crimi, S.; Cicciù, M. Interferon crevicular fluid profile and correlation with periodontal disease and wound healing: A systemic review of recent data. Int. J. Mol. Sci. 2018, 19, 1908. [Google Scholar] [CrossRef]
- Klein, G.; Raina, S. Regulated Assembly of LPS, Its Structural Alterations and Cellular Response to LPS Defects. Int. J. Mol. Sci. 2019, 20, 356. [Google Scholar] [CrossRef]
- Mysak, J.; Podzimek, S.; Sommerova, P.; Lyuya-Mi, Y.; Bartova, J.; Janatova, T.; Prochazkova, J.; Duskova, J. Porphyromonas gingivalis: Major periodontopathic pathogen overview. J. Immunol. Res. 2014, 2014, 476068. [Google Scholar] [CrossRef]
- Ci, X.; Song, Y.; Zeng, F.; Zhang, X.; Li, H.; Wang, X.; Cui, J.; Deng, X. Ceftiofur impairs pro-inflammatory cytokine secretion through the inhibition of the activation of NF-jB and MAPK. Biochem. Biophys. Res. Commun. 2008, 372, 73–77. [Google Scholar] [CrossRef]
- Wang, Q.-B.; Sun, L.-Y.; Gong, Z.-D.; Du, Y. Veratric Acid Inhibits LPS-Induced IL-6 and IL-8 Production in Human Gingival Fibroblasts. Inflammation 2016, 39, 237–242. [Google Scholar] [CrossRef]
- Shin, S.; Jung, E.; Kim, S.; Lee, K.-E.; Youm, J.-K.; Park, D. Antagonist Effects of Veratric Acid against UVB-Induced Cell Damages. Molecules 2013, 18, 5405–5419. [Google Scholar] [CrossRef]
- Wei, C.; Tan, C.K.; Xiaoping, H.; Junqiang, J. Acanthoic Acid Inhibits LPS-Induced Inflammatory Response in Human Gingival Fibroblasts. Inflammation 2015, 38, 896–901. [Google Scholar] [CrossRef]
- Wu, Y.-L.; Jiang, Y.-Z.; Jin, X.-J.; Lian, L.-H.; Piao, J.-Y.; Wan, Y.; Jin, H.-R.; Joon Lee, J.; Nan, J.-X. Acanthoic acid, a diterpene in Acanthopanax koreanum, protects acetaminophen-induced hepatic toxicity in mice. Phytomedicine 2010, 17, 475–479. [Google Scholar] [CrossRef] [PubMed]
- Jian, C.-X.; Li, M.-Z.; Zheng, W.-Y.; He, Y.; Ren, Y.; Wu, Z.-M.; Fan, Q.-S.; Hu, Y.-H.; Li, C.-J. Tormentic acid inhibits LPS-induced inflammatory response in human gingival fibroblasts via inhibition of TLR4-mediated NF-κB and MAPK signalling pathway. Arch. Oral Biol. 2015, 60, 1327–1332. [Google Scholar] [CrossRef] [PubMed]
- Zhou, X.; Li, C.-G.; Chang, D.; Bensoussan, A. Current Status and Major Challenges to the Safety and Efficacy Presented by Chinese Herbal Medicine. Medicines 2019, 6, 14. [Google Scholar] [CrossRef] [PubMed]
- Sucher, N.J. The application of Chinese medicine to novel drug discovery. Expert Opin. Drug Discov. 2013, 8, 21–34. [Google Scholar] [CrossRef]
- Wang, Q.; Zhang, B.; Yu, J.-L. Farrerol inhibits IL-6 and IL-8 production in LPS-stimulated human gingival fibroblasts by suppressing PI3K/AKT/NF-κB signaling pathway. Arch. Oral Biol. 2016, 62, 28–32. [Google Scholar] [CrossRef]
- Zhang, N.; Lv, H.; Shi, B.-H.; Hou, X.; Xu, X. Inhibition of IL-6 and IL-8 production in LPS-stimulated human gingival fibroblasts by glycyrrhizin via activating LXRα. Microb. Pathog. 2017, 110, 135–139. [Google Scholar] [CrossRef]
- Hao, C.; Wu, B.; Hou, Z.; Xie, Q.; Liao, T.; Wang, T.; Ma, D. Asiatic acid inhibits LPS-induced inflammatory response in human gingival fibroblasts. Int. Immunopharmacol. 2017, 50, 313–318. [Google Scholar] [CrossRef]
- Liu, F.; Huang, X.; He, J.-J.; Song, C.; Peng, L.; Chen, T.; Wu, B.-L. Plantamajoside attenuates inflammatory response in LPS-stimulated human gingival fibroblasts by inhibiting PI3K/AKT signaling pathway. Microb. Pathog. 2019, 127, 208–211. [Google Scholar] [CrossRef]
- Wang, Y.; Zhou, J.; Fu, S.; Wang, C.; Zhou, B. Preventive Effects of Protocatechuic Acid on LPS-Induced Inflammatory Response in Human Gingival Fibroblasts via Activating PPAR-γ. Inflammation 2015, 38, 1080–1084. [Google Scholar] [CrossRef]
- Qi, F.; Sun, J.; Yan, J.; Li, C.; Lv, X. Anti-inflammatory effects of isorhamnetin on LPS-stimulated human gingival fibroblasts by activating Nrf2 signaling pathway. Microb. Pathog. 2018, 120, 37–41. [Google Scholar] [CrossRef]
- Kang, W.; Wang, T.; Hu, Z.; Liu, F.; Sun, Y.; Ge, S. Metformin Inhibits Porphyromonas gingivalis Lipopolysaccharide-Influenced Inflammatory Response in Human Gingival Fibroblasts via Regulating Activating Transcription Factor-3 Expression. J. Periodontol. 2017, 88, e169–e178. [Google Scholar] [CrossRef] [PubMed]
- Kang, W.; Shang, L.; Wang, T.; Liu, H.; Ge, S. Rho-kinase inhibitor Y-27632 downregulates LPS-induced IL-6 and IL-8 production via blocking p38 MAPK and NF-κB pathways in human gingival fibroblasts. J. Periodontol. 2018, 89, 883–893. [Google Scholar] [CrossRef] [PubMed]
- Yang, Z.; Zhou, E.; Wei, D.; Li, D.; Wei, Z.; Zhang, W.; Zhang, X. Emodin inhibits LPS-induced inflammatory response by activating PPAR-γ in mouse mammary epithelial cells. Int. Immunopharmacol. 2014, 21, 354–360. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Xiu, L.; Diao, J.; Wei, L.; Sun, J. Sparstolonin B inhibits lipopolysaccharide-induced inflammation in 3T3-L1 adipocytes. Eur. J. Pharmacol. 2015, 769, 79–85. [Google Scholar] [CrossRef] [PubMed]
- Han, Q.; Yuan, Q.; Meng, X.; Huo, J.; Bao, Y.; Xie, G. 6-Shogaol attenuates LPS-induced inflammation in BV2 microglia cells by activating PPAR-γ. Oncotarget 2017, 8, 42001–42006. [Google Scholar] [CrossRef]
- Li-hua, D.; Yan, L.; Shi-ji, W.; Guang, W.; Lu-lu, S.; Xue-feng, P.; Pengda, S. Esculentoside A inhibits LPS-induced BV2 microglia activation through activating PPAR-γ. Eur. J. Pharmacol. 2017, 813, 61–65. [Google Scholar] [CrossRef]
- Fu, Y.; Zhou, E.; Wei, Z.; Song, X.; Liu, Z.; Wang, T.; Wang, W.; Zhang, N.; Liu, G.; Yang, Z. Glycyrrhizin inhibits lipopolysaccharide-induced inflammatory response by reducing TLR4 recruitment into lipid rafts in RAW264.7 cells. Biochim. Biophys. Acta Gen. Subj. 2014, 1840, 1755–1764. [Google Scholar] [CrossRef]
- Li, Y.; Zhang, X.-S.; Yu, J.-L. Acanthoic acid inhibits LPS-induced inflammatory response by activating LXRα in human umbilical vein endothelial cells. Int. Immunopharmacol. 2016, 32, 111–115. [Google Scholar] [CrossRef]
- Liao, S.; Zhou, K.; Li, D.; Xie, X.; Wang, J. Schisantherin A suppresses interleukin-1β-induced inflammation in human chondrocytes via inhibition of NF-κB and MAPKs activation. Eur. J. Pharmacol. 2016, 780, 65–70. [Google Scholar] [CrossRef]
- Zhang, H.; Yan, J.; Zhuang, Y.; Han, G. Anti-inflammatory effects of farrerol on IL-1β-stimulated human osteoarthritis chondrocytes. Eur. J. Pharmacol. 2015, 764, 443–447. [Google Scholar] [CrossRef]
- Yu, T.; Xie, W.; Sun, Y. Oridonin inhibits LPS-induced inflammation in human gingival fibroblasts by activating PPARγ. Int. Immunopharmacol. 2019, 72, 301–307. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Sun, W.; Wu, T.; Lu, R.; Shi, B. Caffeic acid phenethyl ester attenuates lipopolysaccharide-stimulated proinflammatory responses in human gingival fibroblasts via NF-κB and PI3K/Akt signaling pathway. Eur. J. Pharmacol. 2017, 794, 61–68. [Google Scholar] [CrossRef] [PubMed]
- Stepanenko, A.A.; Dmitrenko, V.V. Pitfalls of the MTT assay: Direct and off-target effects of inhibitors can result in over/underestimation of cell viability. Gene 2015, 574, 193–203. [Google Scholar] [CrossRef] [PubMed]
- Okada, H.; Murakami, S. Cytokine expression in periodontal health and disease. Crit. Rev. Oral Biol. Med. 1998, 9, 248–266. [Google Scholar] [CrossRef] [PubMed]
- Nyman, S.; Schroeder, H.E.; Lindhe, J. Suppression of Inflammation and Bone Resorption by Indomethacin During Experimental Periodontitis in Dogs. J. Periodontol. 1979, 50, 450–461. [Google Scholar] [CrossRef] [PubMed]
- Williams, R.; Jeffcoat, M.; Kaplan, M.; Goldhaber, P.; Johnson, H.; Wechter, W. Flurbiprofen: A potent inhibitor of alveolar bone resorption in beagles. Science 1985, 227, 640–642. [Google Scholar] [CrossRef]
- Kim, S.; Kook, K.E.; Kim, C.; Hwang, J.K. Inhibitory effects of Curcuma xanthorrhiza supercritical extract and xanthorrhizol on LPS-induced inflammation in HGF-1 cells and RANKL-induced osteoclastogenesis in RAW264.7 cells. J. Microbiol. Biotechnol. 2018, 28, 1270–1281. [Google Scholar] [CrossRef]
- Li, K.; Lv, G.; Pan, L. Sirt1 alleviates LPS induced inflammation of periodontal ligament fibroblasts via downregulation of TLR4. Int. J. Biol. Macromol. 2018, 119, 249–254. [Google Scholar] [CrossRef]
- Shang, L.; Wang, T.; Tong, D.; Kang, W.; Liang, Q.; Ge, S. Prolyl hydroxylases positively regulated LPS-induced inflammation in human gingival fibroblasts via TLR4/MyD88-mediated AKT/NF-κB and MAPK pathways. Cell Prolif. 2018, 51, e12516. [Google Scholar] [CrossRef]
- Graves, D.T.; Cochran, D. The Contribution of Interleukin-1 and Tumor Necrosis Factor to Periodontal Tissue Destruction. J. Periodontol. 2003, 74, 391–401. [Google Scholar] [CrossRef]
- Noh, M.K.; Jung, M.; Kim, S.H.; Lee, S.R.; Park, K.H.; Kim, D.H.; Kim, H.H.; Park, Y.G. Assessment of IL-6, IL-8 and TNF-α levels in the gingival tissue of patients with periodontitis. Exp. Ther. Med. 2013, 6, 847–851. [Google Scholar] [CrossRef] [PubMed]
- Dongari-Bagtzoglou, A.I.; Ebersole, J.L. Increased Presence of Interleukin-6 (IL-6) and IL-8 Secreting Fibroblast Subpopulations in Adult Periodontitis. J. Periodontol. 1998, 69, 899–910. [Google Scholar] [CrossRef] [PubMed]
- Finoti, L.S.; Nepomuceno, R.; Pigossi, S.C.; Corbi, S.C.; Secolin, R.; Scarel-Caminaga, R.M. Association between interleukin-8 levels and chronic periodontal disease: A PRISMA-compliant systematic review and meta-analysis. Medicine (Baltimore) 2017, 96, e6932. [Google Scholar] [CrossRef] [PubMed]
- Ishimi, Y.; Miyaura, C.; Jin, C.H.; Akatsu, T.; Abe, E.; Nakamura, Y.; Yamaguchi, A.; Yoshiki, S.; Matsuda, T.; Hirano, T. IL-6 is produced by osteoblasts and induces bone resorption. J. Immunol. 1990, 145, 3297–3303. [Google Scholar] [PubMed]
- Tonetti, M.S.; Imboden, M.A.; Lang, N.P. Neutrophil Migration Into the Gingival Sulcus Is Associated With Transepithelial Gradients of Interleukin-8 and ICAM-1. J. Periodontol. 1998, 69, 1139–1147. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.J.; Viana, A.C.; Curtis, K.M.C.; Orrico, S.R.P.; Cirelli, J.A.; Mendes-Junior, C.T.; Scarel-Caminaga, R.M. Association of haplotypes in the IL8 gene with susceptibility to chronic periodontitis in a Brazilian population. Clin. Chim. Acta 2010, 411, 1264–1268. [Google Scholar] [CrossRef]
- Sajadi, M.; Shahmohammadi, A.; Mahmazi, S.; Bashiri, H.; Bavandpour, M.; Yari, K. Study of association between interleukin-8 − 845 T/C and + 781 C/T polymorphisms with periodontitis disease among population from Western Iran. Mol. Biol. Rep. 2018, 45, 1263–1268. [Google Scholar] [CrossRef]
- Chung, R.M.; Grbíc, J.T.; Lamster, I.B. Interleukin-8 and beta-glucuronidase in gingival crevicular fluid. J. Clin. Periodontol. 1997, 24, 146–152. [Google Scholar] [CrossRef]
- Jin, L.; Söder, B.; Corbet, E.F. Interleukin-8 and Granulocyte Elastase in Gingival Crevicular Fluid in Relation to Periodontopathogens in Untreated Adult Periodontitis. J. Periodontol. 2000, 71, 929–939. [Google Scholar] [CrossRef]
- Bing, X.; Sun, X.; Shen, G.; Xie, H.; Ma, M. Levels of IL-8,IL-10 in patients with chronic periodontitis and coronary heart disease. Shanghai Kou Qiang Yi Xue 2015, 24, 598–601. [Google Scholar]
- Gamonal, J.; Acevedo, A.; Bascones, A.; Jorge, O.; Silva, A. Levels of Interleukin-1β, -8, and -10 and RANTES in Gingival Crevicular Fluid and Cell Populations in Adult Periodontitis Patients and the Effect of Periodontal Treatment. J. Periodontol. 2000, 71, 1535–1545. [Google Scholar] [CrossRef] [PubMed]
- Hoesel, B.; Schmid, J.A. The complexity of NF-κB signaling in inflammation and cancer. Mol. Cancer 2013, 12, 86. [Google Scholar] [CrossRef] [PubMed]
- Ambili, R.; Janam, P.; Saneesh Babu, P.S.; Prasad, M.; Vinod, D.; Anil Kumar, P.R.; Kumary, T.V.; Asha Nair, S. Differential expression of transcription factors NF-κB and STAT3 in periodontal ligament fibroblasts and gingiva of healthy and diseased individuals. Arch. Oral Biol. 2017, 82, 19–26. [Google Scholar] [CrossRef] [PubMed]
- Ambili, R.; Santhi, W.S.; Janam, P.; Nandakumar, K.; Pillai, M.R. Expression of Activated Transcription Factor Nuclear Factor-κB in Periodontally Diseased Tissues. J. Periodontol. 2005, 76, 1148–1153. [Google Scholar] [CrossRef] [PubMed]
- Arabaci, T.; Cicek, Y.; Canakci, V.; Canakci, C.F.; Ozgoz, M.; Albayrak, M.; Keles, O.N. Immunohistochemical and Stereologic Analysis of NF-κB Activation in Chronic Periodontitis. Eur. J. Dent. 2010, 4, 454–461. [Google Scholar]
- Rhen, T.; Cidlowski, J.A. Antiinflammatory Action of Glucocorticoids-New Mechanisms for Old Drugs. N. Engl. J. Med. 2005, 353, 1711–1723. [Google Scholar] [CrossRef]
- Han, C.W.; Choi, J.H.; Kim, J.M.; Kim, W.Y.; Lee, K.Y.; Oh, G.T. Glucocorticoid-mediated repression of inflammatory cytokine production in fibroblast-like rheumatoid synoviocytes is independent of nuclear factor-κB activation induced by tumour necrosis factor α. Rheumatology 2001, 40, 267–273. [Google Scholar] [CrossRef][Green Version]
- Liu, J.; Zeng, J.; Wang, X.; Zheng, M.; Luan, Q. P53 mediates lipopolysaccharide-induced inflammation in human gingival fibroblasts. J. Periodontol. 2018, 89, 1142–1151. [Google Scholar] [CrossRef]
- Chambers, C. What’s next for Registered Reports? Nature 2019, 573, 187–189. [Google Scholar] [CrossRef]
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Galli, C.; Sala, R.; Colangelo, M.T.; Guizzardi, S. Between Innovation and Standardization, Is There Still a Room for Scientific Reports? The Rise of a Formatting Tradition in Periodontal Research. Publications 2019, 7, 67. https://doi.org/10.3390/publications7040067
Galli C, Sala R, Colangelo MT, Guizzardi S. Between Innovation and Standardization, Is There Still a Room for Scientific Reports? The Rise of a Formatting Tradition in Periodontal Research. Publications. 2019; 7(4):67. https://doi.org/10.3390/publications7040067
Chicago/Turabian StyleGalli, Carlo, Roberto Sala, Maria Teresa Colangelo, and Stefano Guizzardi. 2019. "Between Innovation and Standardization, Is There Still a Room for Scientific Reports? The Rise of a Formatting Tradition in Periodontal Research" Publications 7, no. 4: 67. https://doi.org/10.3390/publications7040067
APA StyleGalli, C., Sala, R., Colangelo, M. T., & Guizzardi, S. (2019). Between Innovation and Standardization, Is There Still a Room for Scientific Reports? The Rise of a Formatting Tradition in Periodontal Research. Publications, 7(4), 67. https://doi.org/10.3390/publications7040067





