Sinus Mucosa Thickness Changes and Ostium Involvement after Maxillary Sinus Floor Elevation in Sinus with Septa. A Cone Beam Computed Tomography Study
Abstract
:1. Introduction
2. Materials and Methods
Data Analyses
3. Results
3.1. Clinical Report
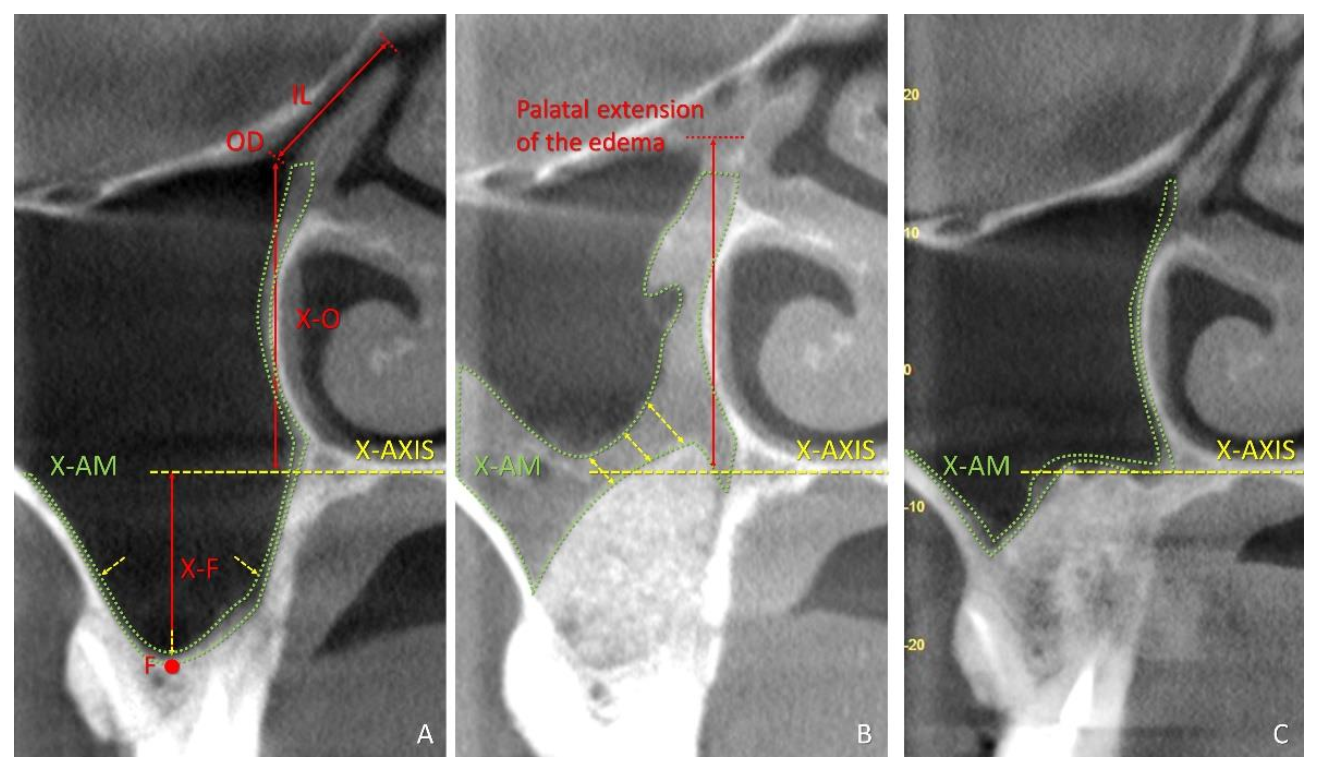
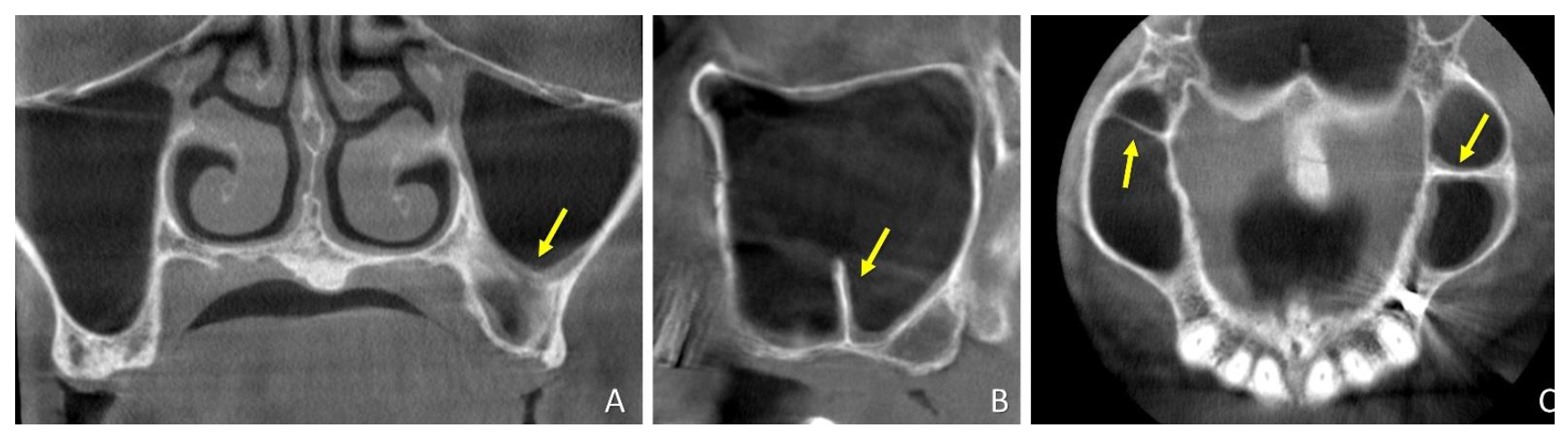
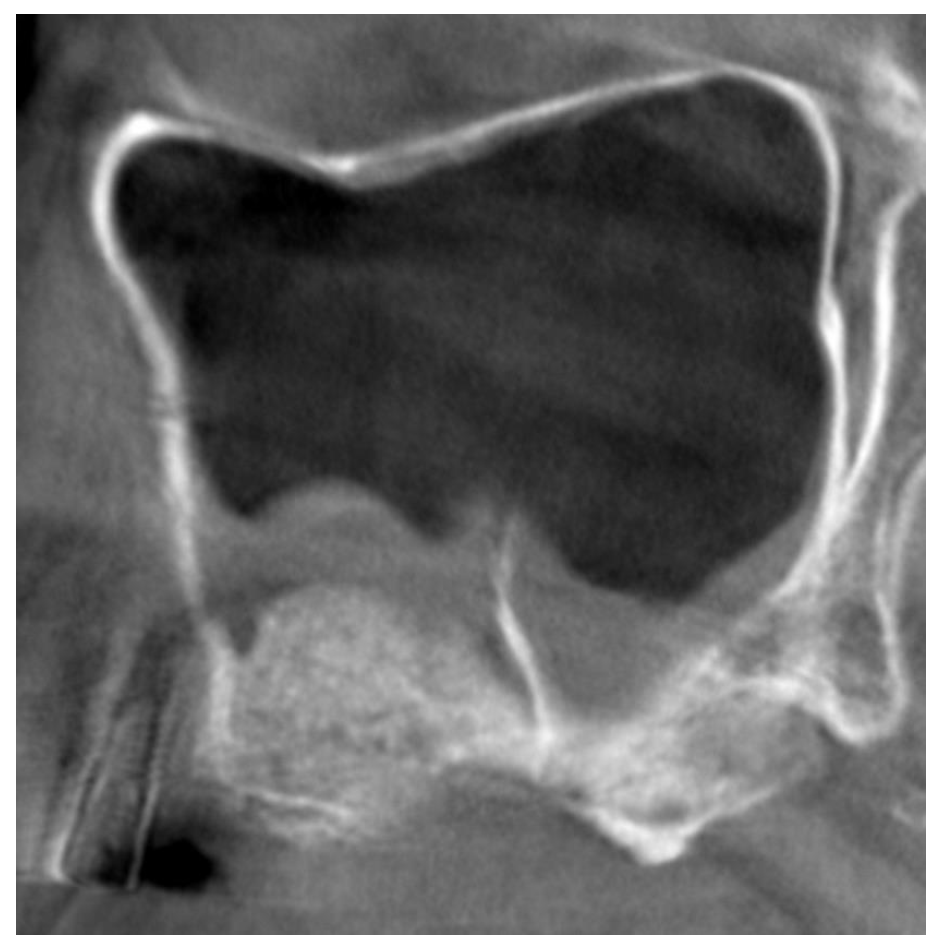
3.2. CBCTs Assessments
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Del Fabbro, M.; Wallace, S.S.; Testori, T. Long-term implant survival in the grafted maxillary sinus: A systematic review. Int. J. Periodontics Restor. Dent. 2013, 33, 773–783. [Google Scholar] [CrossRef] [PubMed]
- Kawakami, S.; Botticelli, D.; Nakajima, Y.; Sakuma, S.; Baba, S. Anatomical analyses for maxillary sinus floor augmentation with a lateral approach: A cone beam computed tomography study. Ann. Anat. 2019, 226, 29–34. [Google Scholar] [CrossRef] [PubMed]
- Chan, H.L.; Monje, A.; Suarez, F.; Benavides, E.; Wang, H.L. Palatonasal recess on medial wall of the maxillary sinus and clinical implications for sinus augmentation via lateral window approach. J. Periodontol. 2013, 84, 1087–1093. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kawakami, S.; Lang, N.P.; Iida, T.; Ferri, M.; Apaza Alccayhuaman, K.A.; Botticelli, D. Influence of the position of the antrostomy in sinus floor elevation assessed with cone-beam computed tomography: A randomized clinical trial. J. Investig. Clin. Dent. 2018, 9, e12362. [Google Scholar] [CrossRef]
- Kawakami, S.; Lang, N.P.; Ferri, M.; Apaza Alccayhuaman, K.A.; Botticelli, D. Influence of the height of the antrostomy in sinus floor elevation assessed by cone beam computed tomography—A randomized clinical trial. Int J. Oral Maxillofac. Implants. 2019, 34, 223–232. [Google Scholar] [CrossRef]
- Testori, T.; Rosano, G.; Taschieri, S.; Del Fabbro, M. Ligation of an unusually large vessel during maxillary sinus floor augmentation. A case report. Eur. J. Oral Implantol. 2010, 3, 255–258. [Google Scholar]
- Tükel, H.C.; Tatli, U. Risk factors and clinical outcomes of sinus membrane perforation during lateral window sinus lifting: Analysis of 120 patients. Int. J. Oral Maxillofac. Surg. 2018, 47, 1189–1194. [Google Scholar] [CrossRef]
- Irinakis, T.; Dabuleanu, V.; Aldahlawi, S. Complications During Maxillary Sinus Augmentation Associated with Interfering Septa: A New Classification of Septa. Open Dent. J. 2017, 11, 140–150. [Google Scholar] [CrossRef] [Green Version]
- Becker, S.T.; Terheyden, H.; Steinriede, A.; Behrens, E.; Springer, I.; Wiltfang, J. Prospective observation of 41 perforations of the Schneiderian membrane during sinus floor elevation. Clin. Oral Implant. Res. 2008, 19, 1285–1289. [Google Scholar] [CrossRef]
- Nolan, P.J.; Freeman, K.; Kraut, R.A. Correlation between Schneiderian membrane perforation and sinus lift graft outcome: A retrospective evaluation of 359 augmented sinus. J. Oral Maxillofac. Surg. 2014, 72, 47–52. [Google Scholar] [CrossRef]
- Shanbhag, S.; Karnik, P.; Shirke, P.; Shanbhag, V. Cone-beam computed tomographic analysis of sinus membrane thickness, ostium patency, and residual ridge heights in the posterior maxilla: Implications for sinus floor elevation. Clin. Oral Implant. Res. 2014, 25, 755–760. [Google Scholar] [CrossRef]
- Scala, A.; Botticelli, D.; Faeda, R.S.; Rangel, I.G., Jr. Américo de Oliveira, J.; Lang, N.P. Lack of influence of the Schneiderian membrane in forming new bone apical to implants simultaneously installed with sinus floor elevation: An experimental study in monkeys. Clin. Oral Implant. Res. 2012, 23, 175–181. [Google Scholar] [CrossRef]
- Scala, A.; Botticelli, D.; Rangel, I.G., Jr.; De Oliveira, J.A.; Okamoto, R.; Lang, N.P. Early healing after elevation of the maxillary sinus floor applying a lateral access: A histological study in monkeys. Clin. Oral Implant. Res. 2010, 21, 1320–1326. [Google Scholar] [CrossRef]
- Quirynen, M.; Lefever, D.; Hellings, P.; Jacobs, R. Transient swelling of the Schneiderian membrane after transversal sinus augmentation: A pilot study. Clin. Oral Implant. Res. 2014, 25, 36–41. [Google Scholar] [CrossRef]
- Temmerman, A.; Van Dessel, J.; Cortellini, S.; Jacobs, R.; Teughels, W.; Quirynen, M. Volumetric changes of grafted volumes and the Schneiderian membrane after transcrestal and lateral sinus floor elevation procedures: A clinical, pilot study. J. Clin. Periodontol. 2017, 44, 660–671. [Google Scholar] [CrossRef]
- Nosaka, Y.; Nosaka, H.; Arai, Y. Complications of postoperative swelling of the maxillary sinus membrane after sinus floor augmentation. J. Oral Sci. Rehabil. 2015, 1, 26–33. [Google Scholar]
- Guo, Z.Z.; Liu, Y.; Qin, L.; Song, Y.L.; Xie, C.; Li, D.H. Longitudinal response of membrane thickness and ostium patency following sinus floor elevation: A prospective cohort study. Clin. Oral Implants Res. 2016, 27, 724–729. [Google Scholar] [CrossRef]
- Makary, C.; Rebaudi, A.; Menhall, A.; Naaman, N. Changes in Sinus Membrane Thickness After Lateral Sinus Floor Elevation: A Radiographic Study. Int. J. Oral Maxillofac. Implants 2016, 31, 331–337. [Google Scholar] [CrossRef] [Green Version]
- Hirota, A.; Lang, N.P.; Ferri, M.; Fortich Mesa, N.; Apaza Alccayhuaman, K.A. Botticelli Tomographic evaluation of the influence of the placement of a collagen membrane subjacent to the sinus mucosa during maxillary sinus floor augmentation: A randomized clinical trial. Int. J. Implant. Dent. 2019, 5, 31. [Google Scholar] [CrossRef]
- Imai, H.; Lang, N.P.; Ferri, M.; Hirota, A.; Apaza Alccayhuaman, K.A.; Botticelli, D. Tomographic Assessment on the Influence of the Use of a Collagen Membrane on Dimensional Variations to Protect the Antrostomy After Maxillary Sinus Floor Augmentation: A Randomized Clinical Trial. Int. J. Oral Maxillofac. Implant. 2020, 35, 350–356. [Google Scholar] [CrossRef]
- Sakuma, S.; Ferri, M.; Imai, H.; Fortich Mesa, N.; Blanco Victorio, D.J.; Apaza Alccayhuaman, K.A.; Botticelli, D. Involvement of the maxillary sinus ostium (MSO) in the edematous processes after sinus floor augmentation: A cone-beam computed tomographic study. Int. J. Implant. Dent. 2020, 6, 35. [Google Scholar] [CrossRef]
- Maestre-Ferrín, L.; Galán-Gil, S.; Rubio-Serrano, M.; Peñarrocha-Diago, M.; Peñarrocha-Oltra, D. Maxillary sinus septa: A systematic review. Med. Oral Patol Oral Cir. Bucal. 2010, 15, e383–e386. [Google Scholar] [CrossRef] [Green Version]
- Bornstein, M.M.; Seiffert, C.; Maestre-Ferrín, L.; Fodich, I.; Jacobs, R.; Buser, D.; von Arx, T. An Analysis of Frequency, Morphology, and Locations of Maxillary Sinus Septa Using Cone Beam Computed Tomography. Int. J. Oral Maxillofac. Implants 2016, 31, 280–287. [Google Scholar] [CrossRef] [Green Version]
- Lozano-Carrascal, N.; Salomó-Coll, O.; Gehrke, S.A.; Calvo-Guirado, J.L.; Hernández-Alfaro, F.; Gargallo-Albiol, J. Radiological evaluation of maxillary Sinus anatomy: A cross-sectional study of 300 patients. Ann. Anat. 2017, 214, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Janner, S.F.; Caversaccio, M.D.; Dubach, P.; Sendi, P.; Buser, D.; Bornstein, M.M. Characteristics and dimensions of the Schneiderian membrane: A radiographic analysis using cone beam computed tomography in patients referred for dental implant surgery in the posterior maxilla. Clin. Oral Implants Res. 2011, 22, 1446–1453. [Google Scholar] [CrossRef] [PubMed]
- Kuligowski, P.; Jaroń, A.; Preuss, O.; Gabrysz-Trybek, E.; Bladowska, J.; Trybek, G. Association between Odontogenic and Maxillary Sinus Conditions: A Retrospective Cone-Beam Computed Tomographic Study. J. Clin. Med. 2021, 10, 2849. [Google Scholar] [CrossRef] [PubMed]
- Block, M.S.; Dastoury, K. Prevalence of sinus membrane thickening and association with unhealthy teeth: A retrospective review of 831 consecutive patients with 1662 cone-beam scans. J. Oral Maxillofac. Surg. 2014, 72, 2454–2460. [Google Scholar] [CrossRef]
| Gender | Age (Years) | Smokers | Sinus Side | Type of Edentulism | Ostium Position | Septa Position | |
|---|---|---|---|---|---|---|---|
| SEPTA | 9 females 3 males | 55.2 ± 9.4 | NONE | 7 right; 8 left | 10 partial, 5 total | 9 PM1, 4 PM2, 2 M1 | 1 PM2, 3 M1, 11 M2 |
| CONTROL | 8 females 7 males | 57.8 ± 8.1 | NONE | 3 right; 12 left | 13 partial, 2 total | 2 PM1, 7 PM2, 6 M1 | |
| PM1, PM2 = First or second premolar regions; M1, M2 = First or second molar regions. | |||||||
| MSO to X-Axis | MSO to Sinus Floor | Infundibulum Length | MSO Diameter | Number of Obstructions | Mucosa Thickness | Mucosa Area | Distance between Ostium and Edema | ||
|---|---|---|---|---|---|---|---|---|---|
| SEPTA Mean values ± SD Minimum; Maximum | T0 | 24.2 ± 3.4 18.5; 31.1 | 33.2 ± 3.9 25.2; 38.4 | 8.5 ± 1.3 6.3; 10.8 | 1.7 ± 0.4 b 1.3; 2.7 | 0 | 1.1 ± 0.7 b 0.3; 2.3 | 13.2 ± 8.3 b 5.6; 27.1 | - |
| T1w | - | - | 1.0 ± 0.6 b,c 0.0; 2.2 | 3 (20%) | 6.7 ± 7.8 b,c 0.5; 31.2 | 168.7 ± 161.0 b.c 7.9; 576.4 | 11.8 ± 10.7 c −1.4; 29.5 | ||
| T9m | - | - | 1.6 ± 0.4 c 1.3; 2.2 | 0 | 0.9 ± 0.6 a,c 0.5; 2.4 | 14.3 ± 7.3 a,c 10.0; 27.8 | 24.6 ± 6.0 c 9.8; 31.9 | ||
| CONTROL Mean values ± SD Minimum; Maximum | T0 | 24.9 ± 4.1 13.7; 30.0 | 32.6 ± 4.6 26.3; 41 | 9.2 ± 2.1 7.0; 13.6 | 2.1 ± 0.8 b 1.2; 4.6 | 0 | 1.0 ± 0.7 b 0.5; 2.4 | 14.7 ± 15.7 b 5.4; 66.3 | - |
| T1w | - | - | 1.0 ± 0.8 b,c 0.0; 2.5 | 5 (33.3%) | 8.2 ± 7.0 b,c 0.9; 24.1 | 199.9 ± 135.7 b,c 11.3; 449.5 | 7.5 ± 8.8 c 1.5; 24.7 | ||
| T9m | - | - | 1.6 ± 0.7 c 0.6; 2.9 | 0 | 2.3 ± 2.8 a,c 0.6; 11.4 | 44.0 ± 69.1 a,c 8.7; 283.0 | 21.5 ± 8.0 c 11.7; 34.7 |
| Mucosa Area | Mesial Vertical Extension above (+) or below (−) the Z-Axis | Distal Vertical Extension above (+) or below (−) the Z-Axis | ||
|---|---|---|---|---|
| SEPTA Mean values ± SD Minimum; Maximum | T0 | 29.8 ± 30.7 b 15.8; 122.9 | - | - |
| T1w | 297.7 ± 262.0 b,c 11.8; 875.7 | 10.8 ± 9.1 c −2.8; 25.9 | 14.2 ± 10.4 2.6; 30.4 | |
| T9m | 41.2 ± 41.6 c 9.7; 157.9 | 1.7 ± 4.0 c −2.7; 8.3 | 0.7 ± 4.0 −2.8; 12.4 | |
| CONTROL Mean values ± SD Minimum; Maximum | T0 | 26.7 ± 20.0 b 11.8; 83.3 | - | - |
| T1w | 311.5 ± 205.3 b,c 21.5; 585.9 | 14.1 ± 10.8 c −5.7; 30.0 | 12.8 ± 11.1 −7.0; 36.0 | |
| T9m | 82.4 ± 144.8 c 14.2; 575.9 | 2.8 ± 6.9 c −5.9; 18.4 | 2.2 ± 6.1 −7.5; 19.0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kato, S.; Omori, Y.; Kanayama, M.; Hirota, A.; Ferri, M.; Apaza Alccayhuaman, K.A.; Botticelli, D. Sinus Mucosa Thickness Changes and Ostium Involvement after Maxillary Sinus Floor Elevation in Sinus with Septa. A Cone Beam Computed Tomography Study. Dent. J. 2021, 9, 82. https://doi.org/10.3390/dj9080082
Kato S, Omori Y, Kanayama M, Hirota A, Ferri M, Apaza Alccayhuaman KA, Botticelli D. Sinus Mucosa Thickness Changes and Ostium Involvement after Maxillary Sinus Floor Elevation in Sinus with Septa. A Cone Beam Computed Tomography Study. Dentistry Journal. 2021; 9(8):82. https://doi.org/10.3390/dj9080082
Chicago/Turabian StyleKato, Shingo, Yuki Omori, Masatsugu Kanayama, Atsuya Hirota, Mauro Ferri, Karol Alí Apaza Alccayhuaman, and Daniele Botticelli. 2021. "Sinus Mucosa Thickness Changes and Ostium Involvement after Maxillary Sinus Floor Elevation in Sinus with Septa. A Cone Beam Computed Tomography Study" Dentistry Journal 9, no. 8: 82. https://doi.org/10.3390/dj9080082
APA StyleKato, S., Omori, Y., Kanayama, M., Hirota, A., Ferri, M., Apaza Alccayhuaman, K. A., & Botticelli, D. (2021). Sinus Mucosa Thickness Changes and Ostium Involvement after Maxillary Sinus Floor Elevation in Sinus with Septa. A Cone Beam Computed Tomography Study. Dentistry Journal, 9(8), 82. https://doi.org/10.3390/dj9080082







