Compound Odontoma Removed by Endoscopic Intraoral Approach: Case Report
Abstract
1. Introduction
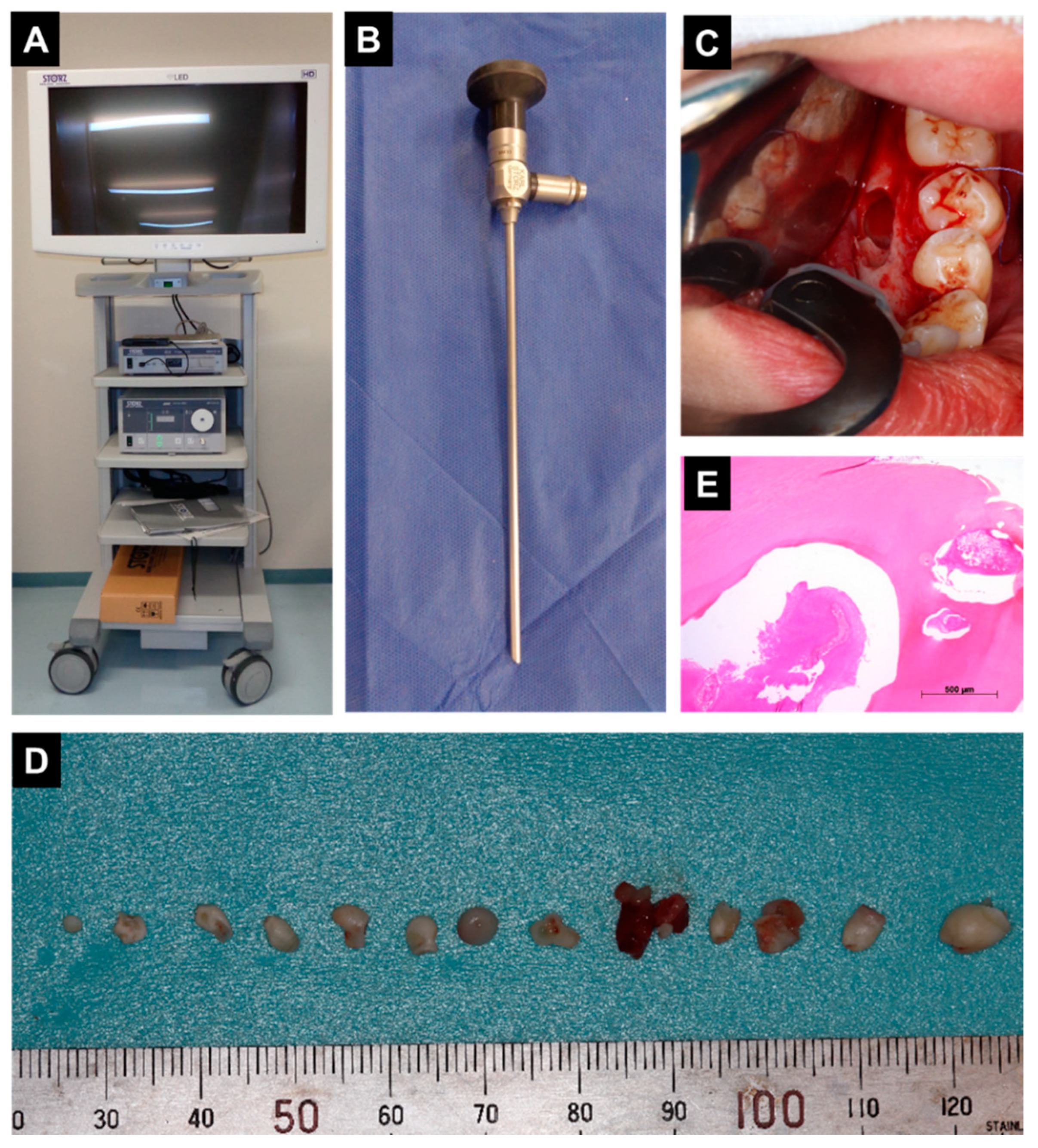
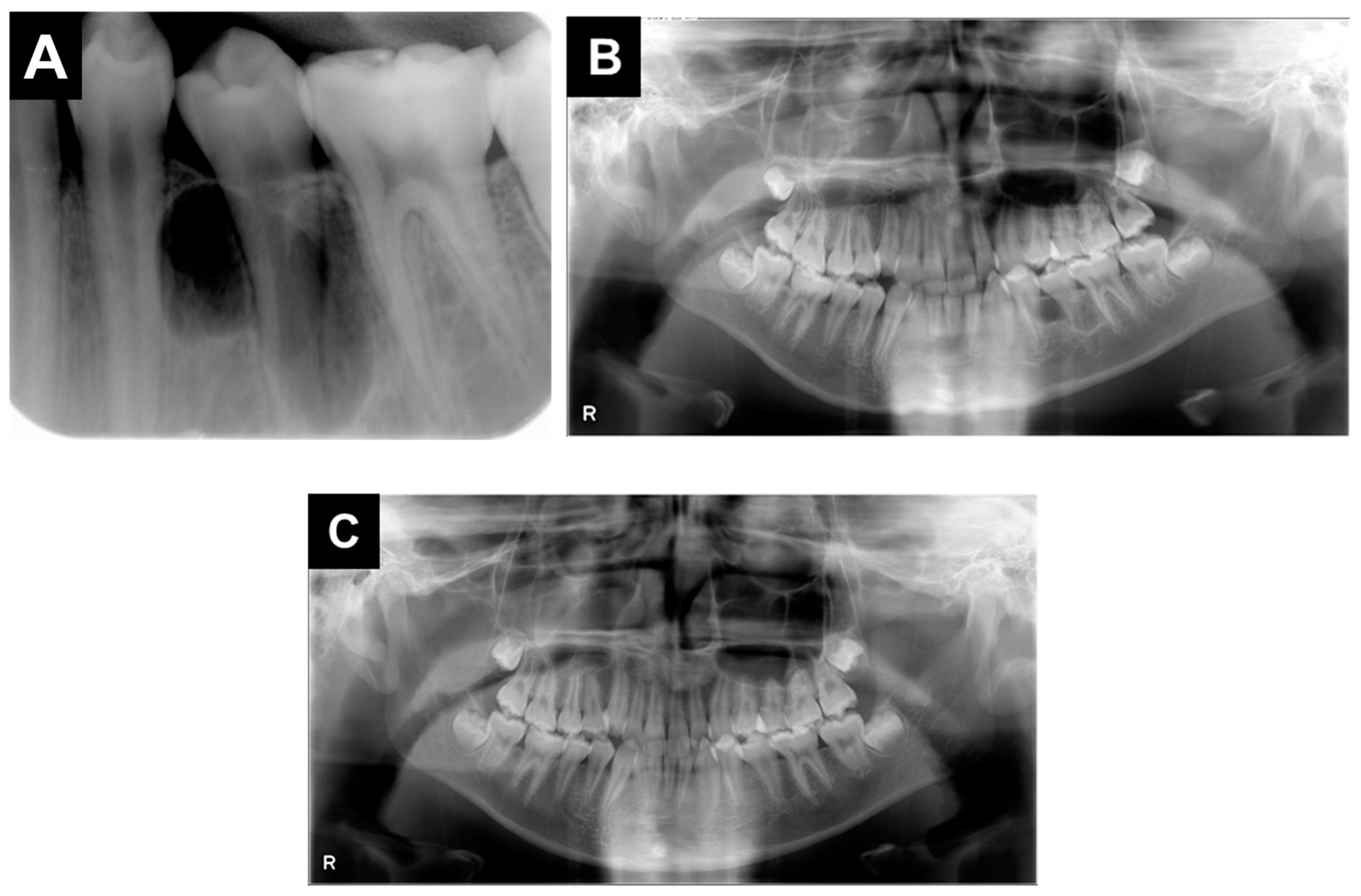
2. Case Report
3. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fernandes, A.M.; Duarte, E.C.B.; Pimenta, F.J.G.S.; Souza, L.N.; Santos, V.R.; Mesquita, R.A.; De Aguiar, M.C.F. Odontogenic tumors: A study of 340 cases in a Brazilian population. J. Oral Pathol. Med. 2005, 34, 583–587. [Google Scholar] [CrossRef] [PubMed]
- Nelson, B.L.; Thompson, L.D.R. Compound Odontoma. Head Neck Pathol. 2010, 4, 290–291. [Google Scholar] [CrossRef] [PubMed]
- Wright, J.M.; Vered, M. Update from the 4th Edition of the World Health Organization Classification of Head and Neck Tumours: Odontogenic and Maxillofacial Bone Tumors. Head Neck Pathol. 2017, 11, 68–77. [Google Scholar] [CrossRef] [PubMed]
- Bordini, J.; Contar, C.M.; Sarot, J.R.; Fernandes, Â.; Machado, M.A.N. Multiple Compound Odontomas in the Jaw: Case Report and Analysis of the Literature. J. Oral Maxillofac. Surg. 2008, 66, 2617–2620. [Google Scholar] [CrossRef] [PubMed]
- Hisatomi, M.; Asaumi, J.-I.; Konouchi, H.; Honda, Y.; Wakasa, T.; Kishi, K. A case of complex odontoma associated with an impacted lower deciduous second molar and analysis of the 107 odontomas. Oral Dis. 2002, 8, 100–105. [Google Scholar] [CrossRef] [PubMed]
- Kamakura, N.; Nakano, K.; Okawa, R.; Nomura, R.; Matsumoto, M.; Fukuda, Y.; Ooshima, T. Impacted primary second molar with odontoma identified in the adjacent tissue. Pediatr. Dent. J. 2009, 19, 117–122. [Google Scholar] [CrossRef][Green Version]
- Ye, Y.J.; Wang, S. Minimally invasive surgery for gastrointestinal stromal tumors--pursuing the trivial, or striving for perfection. Zhonghua Wei Chang Wai Ke Za Zhi 2019, 22, 820–825. [Google Scholar] [PubMed]
- Fukushima, T.; Miyazaki, S.; Takusagawa, Y.; Reichman, M. Unilateral Interhemispheric Keyhole Approach for Anterior Cerebral Artery Aneurysms. Neurosurg. Med. Ethics 1991, 53, 42–47. [Google Scholar]
- Leonhardt, H.; Franke, A.; Nowak, A.; McLeod, N.; Lauer, G. Clinical experience and results with a Rhombic Plate for transoral endoscopically-assisted osteosynthesis of fractures of the condylar neck. Br. J. Oral Maxillofac. Surg. 2019, 57, 1063–1067. [Google Scholar] [CrossRef] [PubMed]
- Liau, I.; Han, J.; Cheng, A.; Duke, P.; Sambrook, P.J.; Goss, A. Endoscopically Assisted Intraoral Removal of an Ectopic Third Molar in the Mandibular Subcondylar Region. J. Craniofacial Surg. 2017, 28, 970–972. [Google Scholar] [CrossRef] [PubMed]
- Gadre, K.; Waknis, P. Intra-oral removal of ectopic third molar in the mandibular condyle. Int. J. Oral Maxillofac. Surg. 2010, 39, 294–296. [Google Scholar] [CrossRef] [PubMed]
- Von Arx, T.; Steiner, R.G.; Tay, F.R. Apical surgery: Endoscopic findings at the resection level of 168 consecutively treated roots. Int. Endod. J. 2011, 44, 290–302. [Google Scholar] [CrossRef] [PubMed]
- Akiyama, K.; Nakai, Y.; Samukawa, Y.; Miyake, M.; Hoshikawa, H. Assessment of Simultaneous Surgery for Odontogenic Sinusitis: Endoscopic Sinus Surgery With Endoscopic Apicoectomy. J. Craniofacial Surg. 2019, 30, 239–243. [Google Scholar] [CrossRef] [PubMed]
- Preoteasa, C.T.; Preoteasa, E. Compound odontoma-morphology, clinical findings and treatment. Case report. Rom. J. Morphol. Embryol. 2018, 59, 997–1000. [Google Scholar] [PubMed]
- Kämmerer, P.W.; Schneider, D.; Schiegnitz, E.; Schneider, S.; Walter, C.; Frerich, B.; Kunkel, M. Clinical parameter of odontoma with special emphasis on treatment of impacted teeth-a retrospective multicentre study and literature review. Clin. Oral Investig. 2016, 20, 1827–1835. [Google Scholar] [CrossRef] [PubMed]

|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hamada, M.; Okawa, R.; Nishiyama, K.; Nomura, R.; Uzawa, N.; Nakano, K. Compound Odontoma Removed by Endoscopic Intraoral Approach: Case Report. Dent. J. 2021, 9, 81. https://doi.org/10.3390/dj9070081
Hamada M, Okawa R, Nishiyama K, Nomura R, Uzawa N, Nakano K. Compound Odontoma Removed by Endoscopic Intraoral Approach: Case Report. Dentistry Journal. 2021; 9(7):81. https://doi.org/10.3390/dj9070081
Chicago/Turabian StyleHamada, Masakazu, Rena Okawa, Kyoko Nishiyama, Ryota Nomura, Narikazu Uzawa, and Kazuhiko Nakano. 2021. "Compound Odontoma Removed by Endoscopic Intraoral Approach: Case Report" Dentistry Journal 9, no. 7: 81. https://doi.org/10.3390/dj9070081
APA StyleHamada, M., Okawa, R., Nishiyama, K., Nomura, R., Uzawa, N., & Nakano, K. (2021). Compound Odontoma Removed by Endoscopic Intraoral Approach: Case Report. Dentistry Journal, 9(7), 81. https://doi.org/10.3390/dj9070081






