Factors Influencing the Accuracy of Freehand Implant Placement: A Prospective Clinical Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Inclusion Criteria
- Submission of written informed consent;
- Restoration of a missing tooth using an implant;
- Restoration of single-tooth edentulous sites in the premolar or molar region;
- Sufficient existing bone. The implant had to be surrounded by 1.5 mm of bone on all sides after evaluation of the CBCT;
- Planned prosthetic restoration with occlusal screw-retained hybrid-abutment crowns;
- Healing of the extraction socket for at least 3 months.
- Patients under 18 years or without any legal capacity;
- Use of an implant placement template is not possible (restricted mouth opening);
- Heavy smoker (>10 cigarettes/day);
- known systematic conditions to alter bone metabolism or affect wound healing (e.g., bisphosphonates);
- Pregnant women;
- Alcohol and/or drug abuse;
- Patients with infectious diseases such as hepatitis, HIV, or AIDS;
- Patients with uncontrolled severe diabetes mellitus. The long-term glucose parameter HbA1c value was required to be below 6.7%.
2.3. Planning
2.4. Implant Placement
2.5. Registration of the Implant Position
2.6. Alignment of Datasets
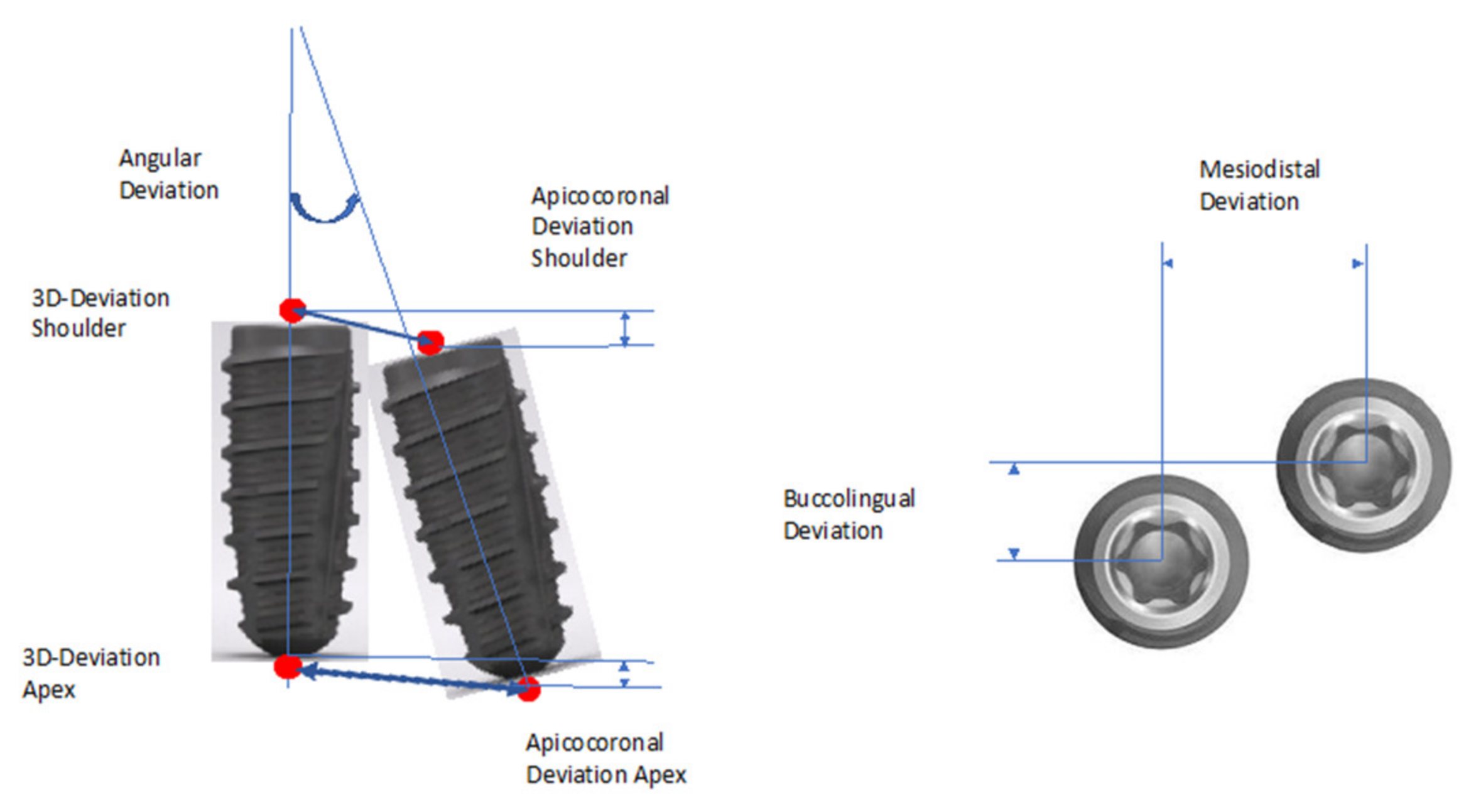
2.7. Analysis of the Implant Position
- Three-dimensional (3D) deviation.
- Two-dimensional deviations in apicocoronal direction (height deviation) and mesiodistal and buccolingual direction.
2.8. Statistical Analysis
3. Results
Description of the Study Population
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Vercruyssen, M.; Fortin, T.; Widmann, G.; Jacobs, R.; Quirynen, M. Different techniques of static/dynamic guided implant surgery: Modalities and indications. Periodontol 2000 2014, 66, 214–227. [Google Scholar] [CrossRef] [PubMed]
- D’Haese, J.; Ackhurst, J.; Wismeijer, D.; De Bruyn, H.; Tahmaseb, A. Current state of the art of computer-guided implant surgery. Periodontol 2000 2017, 73, 121–133. [Google Scholar] [CrossRef] [PubMed]
- Cattoni, F.; Chirico, L.; Merlone, A.; Manacorda, M.; Vinci, R.; Gherlone, E.F. Digital Smile Designed Computer-Aided Surgery versus Traditional Workflow in “All on Four” Rehabilitations: A Randomized Clinical Trial with 4-Years Follow-Up. Int. J. Environ. Res. Public Health 2021, 18, 3449. [Google Scholar] [CrossRef] [PubMed]
- Choi, W.; Nguyen, B.C.; Doan, A.; Girod, S.; Gaudilliere, B.; Gaudilliere, D. Freehand Versus Guided Surgery: Factors Influencing Accuracy of Dental Implant Placement. Implant Dent. 2017, 26, 500–509. [Google Scholar] [CrossRef]
- Behneke, A.; Burwinkel, M.; Behneke, N. Factors influencing transfer accuracy of cone beam CT-derived template-based implant placement. Clin. Oral Implant Res. 2012, 23, 416–423. [Google Scholar] [CrossRef]
- Nickenig, H.J.; Wichmann, M.; Hamel, J.; Schlegel, K.A.; Eitner, S. Evaluation of the difference in accuracy between implant placement by virtual planning data and surgical guide templates versus the conventional free-hand method-a combined in vivo-in vitro technique using cone-beam CT (Part II). J. Craniomaxillofac. Surg. 2010, 38, 488–493. [Google Scholar] [CrossRef]
- Vercruyssen, M.; Coucke, W.; Naert, I.; Jacobs, R.; Teughels, W.; Quirynen, M. Depth and lateral deviations in guided implant surgery: An RCT comparing guided surgery with mental navigation or the use of a pilot-drill template. Clin. Oral Implant Res. 2015, 26, 1315–1320. [Google Scholar] [CrossRef]
- Vercruyssen, M.; Cox, C.; Coucke, W.; Naert, I.; Jacobs, R.; Quirynen, M. A randomized clinical trial comparing guided implant surgery (bone- or mucosa-supported) with mental navigation or the use of a pilot-drill template. J. Clin. Periodontol. 2014, 41, 717–723. [Google Scholar] [CrossRef]
- Tahmaseb, A.; Wu, V.; Wismeijer, D.; Coucke, W.; Evans, C. The accuracy of static computer-aided implant surgery: A systematic review and meta-analysis. Clin. Oral Implant Res. 2018, 29 (Suppl. 16), 416–435. [Google Scholar] [CrossRef]
- Varga, E., Jr.; Antal, M.; Major, L.; Kiscsatari, R.; Braunitzer, G.; Piffko, J. Guidance means accuracy: A randomized clinical trial on freehand versus guided dental implantation. Clin. Oral Implant Res. 2020, 31, 417–430. [Google Scholar] [CrossRef]
- Gallucci, G.O.; Hamilton, A.; Zhou, W.; Buser, D.; Chen, S. Implant placement and loading protocols in partially edentulous patients: A systematic review. Clin. Oral Implant Res. 2018, 29 (Suppl. 16), 106–134. [Google Scholar] [CrossRef]
- Schnutenhaus, S.; Edelmann, C.; Rudolph, H.; Luthardt, R.G. Retrospective study to determine the accuracy of template-guided implant placement using a novel nonradiologic evaluation method. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2016, 121, e72–e79. [Google Scholar] [CrossRef]
- Tahmaseb, A.; Wismeijer, D.; Coucke, W.; Derksen, W. Computer technology applications in surgical implant dentistry: A systematic review. Int. J. Oral Maxillofac. Implant 2014, 29, 25–42. [Google Scholar] [CrossRef]
- Jorba-Garcia, A.; Figueiredo, R.; Gonzalez-Barnadas, A.; Camps-Font, O.; Valmaseda-Castellon, E. Accuracy and the role of experience in dynamic computer guided dental implant surgery: An in-vitro study. Med. Oral Patol. Oral Cir. Bucal 2019, 24, e76–e83. [Google Scholar] [CrossRef]
- Chen, C.K.; Yuh, D.Y.; Huang, R.Y.; Fu, E.; Tsai, C.F.; Chiang, C.Y. Accuracy of Implant Placement with a Navigation System, a Laboratory Guide, and Freehand Drilling. Int. J. Oral Maxillofac. Implant 2018, 33, 1213–1218. [Google Scholar] [CrossRef]
- Chen, Z.; Li, J.; Sinjab, K.; Mendonca, G.; Yu, H.; Wang, H.L. Accuracy of flapless immediate implant placement in anterior maxilla using computer-assisted versus freehand surgery: A cadaver study. Clin. Oral Implant Res. 2018, 29, 1186–1194. [Google Scholar] [CrossRef]
- Noharet, R.; Pettersson, A.; Bourgeois, D. Accuracy of implant placement in the posterior maxilla as related to 2 types of surgical guides: A pilot study in the human cadaver. J. Prosthet. Dent. 2014, 112, 526–532. [Google Scholar] [CrossRef]
- Schneider, D.; Sancho-Puchades, M.; Mir-Mari, J.; Muhlemann, S.; Jung, R.; Hammerle, C. A Randomized Controlled Clinical Trial Comparing Conventional and Computer-Assisted Implant Planning and Placement in Partially Edentulous Patients. Part 4: Accuracy of Implant Placement. Int. J. Periodont. Restor. Dent. 2019, 39, e111–e122. [Google Scholar] [CrossRef]
- Sun, T.M.; Lee, H.E.; Lan, T.H. Comparing Accuracy of Implant Installation with a Navigation System (NS), a Laboratory Guide (LG), NS with LG, and Freehand Drilling. Int. J. Environ. Res. Public Health 2020, 17, 2107. [Google Scholar] [CrossRef]
- Aydemir, C.A.; Arisan, V. Accuracy of dental implant placement via dynamic navigation or the freehand method: A split-mouth randomized controlled clinical trial. Clin. Oral Implant Res. 2020, 31, 255–263. [Google Scholar] [CrossRef]
- Smitkarn, P.; Subbalekha, K.; Mattheos, N.; Pimkhaokham, A. The accuracy of single-tooth implants placed using fully digital-guided surgery and freehand implant surgery. J. Clin. Periodontol. 2019, 46, 949–957. [Google Scholar] [CrossRef] [PubMed]
- Efstathiou, A.; Machtei, E.E.; Zigdon-Giladi, H.; Gutmacher, Z.; Horwitz, J. The effect of a surgeon’s position on the axial inclination of dental implants placed freehand: A single-blind study. Quintessence Int. 2021. [Google Scholar] [CrossRef]
- Marei, H.F.; Abdel-Hady, A.; Al-Khalifa, K.; Al-Mahalawy, H. Influence of surgeon experience on the accuracy of implant placement via a partially computer-guided surgical protocol. Int. J. Oral Maxillofac. Implant 2019, 34, 1177–1183. [Google Scholar] [CrossRef] [PubMed]
- Schnutenhaus, S.; Edelmann, C.; Rudolph, H.; Dreyhaupt, J.; Luthardt, R.G. 3D accuracy of implant positions in template-guided implant placement as a function of the remaining teeth and the surgical procedure: A retrospective study. Clin. Oral Investig. 2018, 22, 2363–2372. [Google Scholar] [CrossRef] [PubMed]
- Schnutenhaus, S.; von Koenigsmarck, V.; Blender, S.; Ambrosius, L.; Luthardt, R.G.; Rudolph, H. Precision of sleeveless 3D drill guides for insertion of one-piece ceramic implants: A prospective clinical trial. Int. J. Comput. Dent. 2018, 21, 97–105. [Google Scholar] [PubMed]
- Vercruyssen, M.; De Laat, A.; Coucke, W.; Quirynen, M. An RCT comparing patient-centred outcome variables of guided surgery (bone or mucosa supported) with conventional implant placement. J. Clin. Periodontol. 2014, 41, 724–732. [Google Scholar] [CrossRef] [PubMed]
- Pozzi, A.; Tallarico, M.; Marchetti, M.; Scarfo, B.; Esposito, M. Computer-guided versus free-hand placement of immediately loaded dental implants: 1-year post-loading results of a multicentre randomised controlled trial. Eur. J. Oral Implantol. 2014, 7, 229–242. [Google Scholar]
- Tang, T.; Huang, Z.; Liao, L.; Gu, X.; Zhang, J.; Zhang, X. Factors that Influence Direction Deviation in Freehand Implant Placement. J. Prosthodont. 2019, 28, 511–518. [Google Scholar] [CrossRef]
- Sicilia, A.; Botticelli, D.; Working, G. Computer-guided implant therapy and soft- and hard-tissue aspects. The Third EAO Consensus Conference 2012. Clin. Oral Implant Res. 2012, 23 (Suppl. 6), 157–161. [Google Scholar] [CrossRef]
- Abduo, J.; Lau, D. Accuracy of static computer-assisted implant placement in anterior and posterior sites by clinicians new to implant dentistry: In vitro comparison of fully guided, pilot-guided, and freehand protocols. Int. J. Implant Dent. 2020, 6, 10. [Google Scholar] [CrossRef]
- Arisan, V.; Karabuda, C.Z.; Mumcu, E.; Ozdemir, T. Implant positioning errors in freehand and computer-aided placement methods: A single-blind clinical comparative study. Int. J. Oral Maxillofac. Implant 2013, 28, 190–204. [Google Scholar] [CrossRef]
- Baldi, D.; Colombo, J.; Motta, F.; Motta, F.M.; Zillio, A.; Scotti, N. Digital vs. Freehand Anterior Single-Tooth Implant Restoration. BioMed Res. Int. 2020, 2020, 4012127. [Google Scholar] [CrossRef]
- Bernard, L.; Vercruyssen, M.; Duyck, J.; Jacobs, R.; Teughels, W.; Quirynen, M. A randomized controlled clinical trial comparing guided with nonguided implant placement: A 3-year follow-up of implant-centered outcomes. J. Prosthet. Dent. 2019, 121, 904–910. [Google Scholar] [CrossRef]
- Yogui, F.C.; Verri, F.R.; de Luna Gomes, J.M.; Lemos, C.A.A.; Cruz, R.S.; Pellizzer, E.P. Comparison between computer-guided and freehand dental implant placement surgery: A systematic review and meta-analysis. Int. J. Oral Maxillofac. Surg. 2021, 50, 242–250. [Google Scholar] [CrossRef]
- Ozden Yuce, M.; Gunbay, T.; Guniz Baksi, B.; Comlekoglu, M.; Mert, A. Clinical benefits and effectiveness of static computer-aided implant surgery compared with conventional freehand method for single-tooth implant placement. J. Stomatol. Oral Maxillofac. Surg. 2020, 121, 534–538. [Google Scholar] [CrossRef]
- Sancho-Puchades, M.; Alfaro, F.H.; Naenni, N.; Jung, R.; Hammerle, C.; Schneider, D. A Randomized Controlled Clinical Trial Comparing Conventional And Computer-Assisted Implant Planning and Placement in Partially Edentulous Patients. Part 2: Patient Related Outcome Measures. Int. J. Periodont. Restor. Dent. 2019, 39, e99–e110. [Google Scholar] [CrossRef]
| Right (N = 22) | Left (N = 30) | |
|---|---|---|
| Upper jaw (N = 20) | Premolars: 6 Molars: 1 | Premolars: 8 Molars: 5 |
| Lower jaw (N = 32) | Premolars: 3 Molars: 12 | Premolars: 7 Molars: 10 |
| Lengths/Diameters | 3.8 | 4.4 | 5.0 |
|---|---|---|---|
| 9 | 5 | 9 | 6 |
| 11 | 11 | 11 | 8 |
| 13 | 1 | 1 | 0 |
| Mean | Standard Deviation | Minimum | Maximum | ||
|---|---|---|---|---|---|
| Angle | Deviation | 8.70 | 4.8 | 1.8 | 22.3 |
| Shoulder | 3D deviation | 1.62 | 0.87 | 0.13 | 3.57 |
| Mesiodistal deviation | 0.87 | 0.75 | 0.00 | 3.13 | |
| Buccolingual deviation | 0.70 | 0.66 | 0.00 | 2.96 | |
| Apicocoronal deviation | 0.95 | 0.61 | 0.00 | 2.32 | |
| Apex | 3D deviation | 2.68 | 1.52 | 0.48 | 7.12 |
| Mesiodistal deviation | 1.93 | 1.51 | 0.09 | 6.51 | |
| Buccolingual deviation | 1.10 | 1.03 | 0.15 | 4.36 | |
| Apicocoronal deviation | 1.05 | 0.72 | 0.41 | 2.82 |
| Upper Jaw | Lower Jaw | |||||
|---|---|---|---|---|---|---|
| Mean | SE (95% CI) | Mean | SE (95% CI) | Sig. Level | ||
| Angle | Deviation | 6.98 | 0.89 (5.11–8.84) | 9.77 | 0.90 (7.94–11.60) | 0.050 |
| Shoulder | Mesiodistal deviation | 0.54 | 0.13 (0.27–0.82) | 1.07 | 0.14 (0.80–1.35) | 0.011 * |
| Buccolingual Deviation | 0.71 | 0.14 (0.41–1.01) | 0.69 | 0.12 (0.44–0.94) | 0.742 | |
| Apicocoronal Deviation | 0.97 | 0.14 (0.67–1.27) | 0.94 | 0.10 (0.72–1.15) | 0.903 | |
| Apex | Mesiodistal deviation | 1.36 | 0.27 (0.81–1.92) | 2.28 | 0.28 (1.70–2.85) | 0.038 * |
| Buccolingual deviation | 1.27 | 0.22 (0.80–1.74) | 0.99 | 0.19 (0.61–1.37) | 0.140 | |
| Apicocoronal deviation | 1.01 | 0.16 (0.67–1.34) | 1.08 | 0.13 (0.82–1.35) | 0.645 | |
| Premolar | Molar | |||||
|---|---|---|---|---|---|---|
| Mean | SE (95% CI) | Mean | SE (95% CI) | Sig. Level | ||
| Angle | Deviation | 7.43 | 0.76 (5.86–8.99) | 9.78 | 1.04 (7.66–11.91) | 0.163 |
| Shoulder | Mesiodistal deviation | 0.68 | 0.12 (0.44–0.92) | 1.03 | 0.16 (0.70–1.36) | 0.169 |
| Buccolingual deviation | 0.70 | 0.13 (0.43–0.96) | 0.70 | 0.13 (0.43–0.97) | 0.963 | |
| Apicocoronal deviation | 1.02 | 0.12 (0.77–1.28) | 0.89 | 0.12 (0.65–1.12) | 0.354 | |
| Apex | Mesiodistal deviation | 1.47 | 0.25 (0.97–1.98) | 2.31 | 0.31 (1.67–2.95) | 0.077 |
| Buccolingual deviation | 1.30 | 0.21 (0.87–1.73) | 0.93 | 0.19 (0.53–1.32) | 0.100 | |
| Apicocoronal deviation | 1.04 | 0.13 (0.76–1.31) | 1.07 | 0.15 (0.76–1.37) | 0.833 | |
| Right Side | Left Side | |||||
|---|---|---|---|---|---|---|
| Mean | SE (95% CI) | Mean | SE (95% CI) | Sig. Level | ||
| Angle | Deviation | 8.78 | 1.08 (6.54–11.02) | 8.62 | 0.85 (6.87–10.37) | 0.854 |
| Shoulder | Mesiodistal deviation | 0.77 | 0.15 (0.45–1.09) | 0.95 | 0.14 (0.37–1.24) | 0.364 |
| Buccolingual deviation | 0.68 | 0.12 (0.44–0.92) | 0.71 | 0.14 (0.43–1.00) | 0.755 | |
| Apicocoronal deviation | 1.04 | 0.10 (0.83–1.25) | 0.87 | 0.13 (0.61–1.14) | 0.088 | |
| Apex | Mesiodistal deviation | 1.79 | 0.32 (1.14–2.45) | 2.04 | 0.28 (1.46–2.62) | 0.474 |
| Buccolingual deviation | 1.19 | 0.25 (0.67–1.71) | 1.02 | 0.16 (0.69–1.34) | 0.941 | |
| Apicocoronal deviation | 1.12 | 0.12 (0.88–1.37) | 0.99 | 0.16 (0.67–1.31) | 0.169 | |
| Early Implant Placement | Late Implant Placement | |||||
|---|---|---|---|---|---|---|
| Mean | SE (95% CI) | Mean | SE (95% CI) | Sig. Level | ||
| Angle | Deviation | 11.03 | 1.05 (8.85–13.22) | 7.11 | 0.76 (5.55–8.67) | 0.005 * |
| Shoulder | Mesiodistal deviation | 1.06 | 0.15 (0.76–1.36) | 0.74 | 0.14 (0.45–1.03) | 0.050 |
| Buccolingual deviation | 0.86 | 0.18 (0.49–1.24) | 0.59 | 0.09 (0.40–1.24) | 0.275 | |
| Apicocoronal Deviation | 1.08 | 0.14 (0.79–1.37) | 0.86 | 1.04 (0.65–1.07) | 0.182 | |
| Apex | Mesiodistal deviation | 2.62 | 0.30 (1.99–3.24) | 1.46 | 0.26 (0.63–1.98) | 0.003 * |
| Buccolingual deviation | 1.41 | 0.29 (0.80–2.01) | 0.89 | 0.13 (0.62–1.16) | 0.309 | |
| Apicocoronal deviation | 1.27 | 0.18 (090–1.64) | 0.91 | 0.11 (0.68–1.14) | 0.081 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schnutenhaus, S.; Wagner, M.; Edelmann, C.; Luthardt, R.G.; Rudolph, H. Factors Influencing the Accuracy of Freehand Implant Placement: A Prospective Clinical Study. Dent. J. 2021, 9, 54. https://doi.org/10.3390/dj9050054
Schnutenhaus S, Wagner M, Edelmann C, Luthardt RG, Rudolph H. Factors Influencing the Accuracy of Freehand Implant Placement: A Prospective Clinical Study. Dentistry Journal. 2021; 9(5):54. https://doi.org/10.3390/dj9050054
Chicago/Turabian StyleSchnutenhaus, Sigmar, Marie Wagner, Cornelia Edelmann, Ralph G. Luthardt, and Heike Rudolph. 2021. "Factors Influencing the Accuracy of Freehand Implant Placement: A Prospective Clinical Study" Dentistry Journal 9, no. 5: 54. https://doi.org/10.3390/dj9050054
APA StyleSchnutenhaus, S., Wagner, M., Edelmann, C., Luthardt, R. G., & Rudolph, H. (2021). Factors Influencing the Accuracy of Freehand Implant Placement: A Prospective Clinical Study. Dentistry Journal, 9(5), 54. https://doi.org/10.3390/dj9050054









