Conservative Non-Surgical Management of Horizontal Root-Fractured Maxillary Incisors in a Young Male with Angle Class II, Division 2, Malocclusion
Abstract
1. Introduction
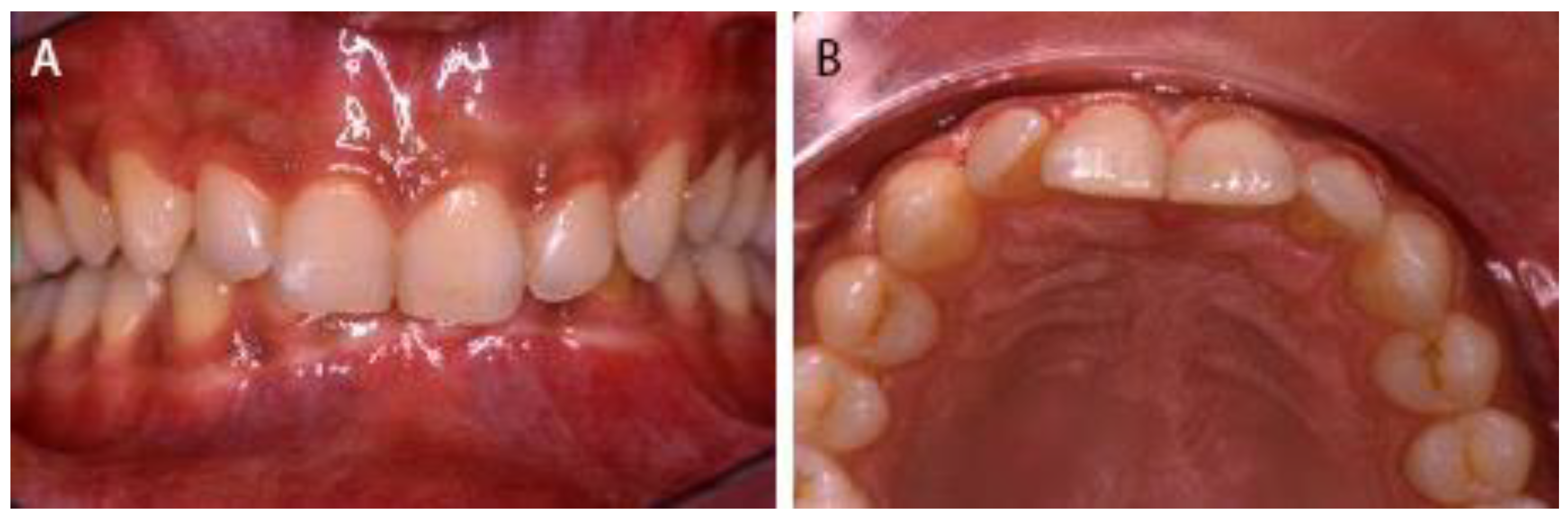
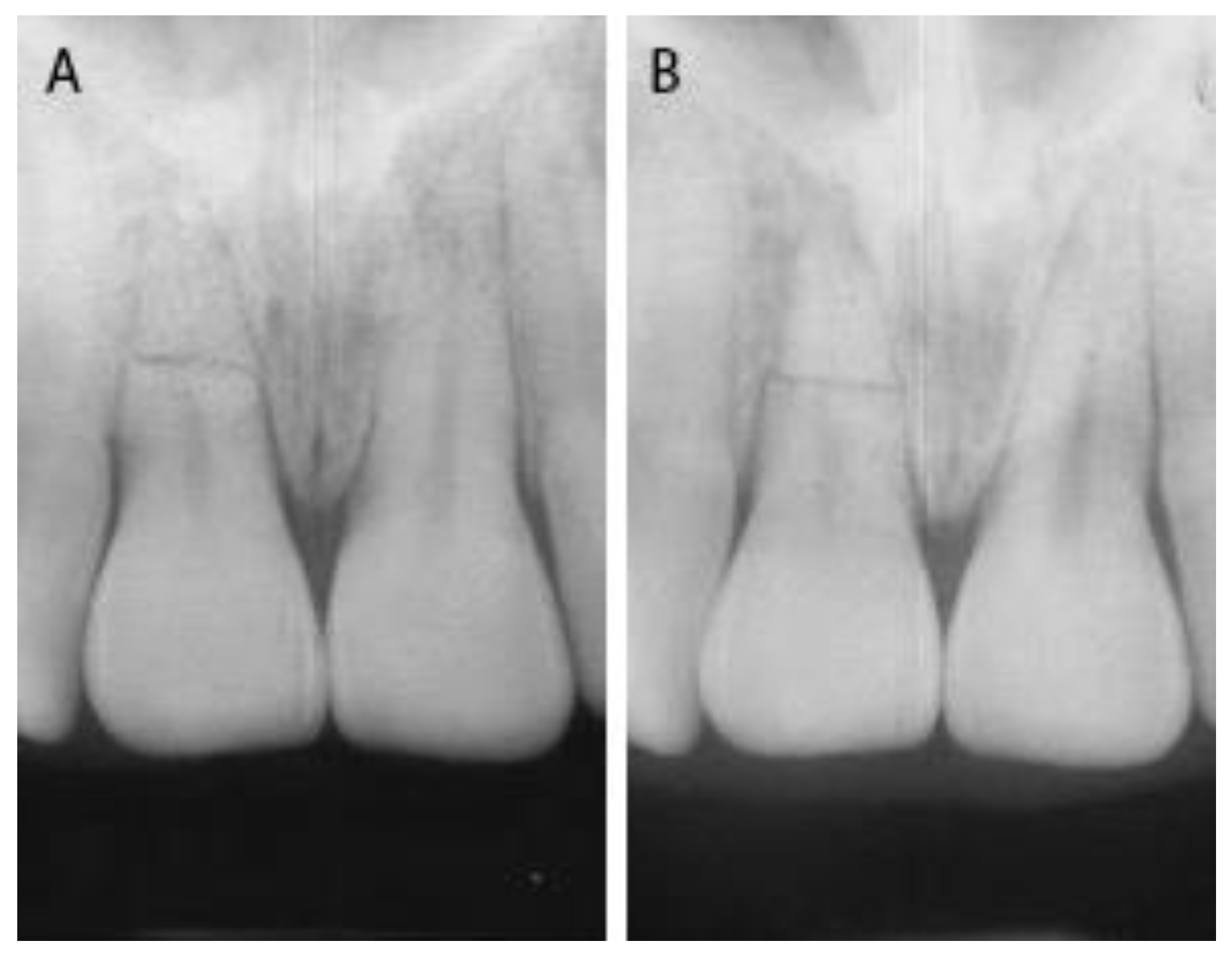
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Andreasen, F.M.; Andreasen, J.O.; Cveck, M. Root Fractures. In Textbook and Color Atlas of Traumatic Injuries to the Teeth, 4th ed.; Andreasen, J.O., Andreasen, F.M., Andersson, L., Eds.; Blackwell Publishing Ltd.: Oxford, UK, 2007; pp. 337–371. [Google Scholar]
- Caliscan, M.K.; Pehlivan, Y. Prognosis of root-fractured permanent incisors. Endod. Dent. Traumatol. 1996, 12, 129–136. [Google Scholar] [CrossRef] [PubMed]
- Andreasen, J.O.; Hjorting-Hansen, E. Intra-alveolar root fractures: Radiographic and histologic study of 50 cases. J. Oral. Surg. 1967, 25, 414–426. [Google Scholar]
- Andreasen, J.O.; Ahrensburg, S.S.; Tsilingaridis, G. Tooth mobility changes subsequent to root fractures: A longitudinal clinical study of 44 permanent teeth. Dent. Traumatol. 2012, 28, 410–414. [Google Scholar] [CrossRef] [PubMed]
- Glendor, U. Aetiology and risk factors related to traumatic dental injuries—A review of the literature. Dent. Traumatol. 2009, 25, 19–31. [Google Scholar] [CrossRef] [PubMed]
- Zaleckiene, V.; Peciuliene, V.; Brukiene, V.; Drukteinis, S. Traumatic dental injuries: Etiology, prevalence and possible outcomes. Stomatologija 2014, 16, 7–14. [Google Scholar] [PubMed]
- Andreasen, J.O.; Andreasen, F.M.; Mejare, I.; Cvek, M. Healing of 400 intra-alveolar root fractures. 1. Effect pre-injury and injury factors such as sex, age, stage of root development, fracture type, location of fracture and severity of dislocation. Dent. Traumatol. 2004, 20, 192–202. [Google Scholar] [CrossRef]
- Andreasen, F.M. Pulpal healing after luxation injuries and root fracture in the permanent dentition. Endod. Dent. Traumatol. 1989, 5, 111–131. [Google Scholar] [CrossRef] [PubMed]
- Tsukiboshi, M. Root Fracture. Treatment Planning for Traumatized Teeth; Quintessence Publishing Co., Inc.: Carol Stream, IL, USA, 2000; pp. 47–57. [Google Scholar]
- Andreasen, J.O.; Andreasen, F.M.; Skeie, A.; Hiorting-Hansen, E. Effect of treatment delay upon pulp and periodontal healing of traumatic dental injuries—A review article. Dent. Traumatol. 2002, 18, 116–128. [Google Scholar] [CrossRef] [PubMed]
- Kahler, B.; Hu, J.Y.; Marriot-Smith, C.S.; Heithersay, G.S. Splinting of teeth following trauma: A review and a new splinting recommendation. Aust. Dent. J. 2016, 61, 59–73. [Google Scholar] [CrossRef] [PubMed]
- Thaler, C.B.A.; Petschelt, A. Rigidity of commonly used dental trauma splints. Dent. Traumatol. 2009, 25, 248–255. [Google Scholar]
- Bourguignon, C.; Cohenca, N.; Lauridsen, E.; Flores, M.T.; O‘Connell, A.C.; Day, P.F.; Tsilingaridis, G.; Abbott, P.V.; Fouad, A.F.; Hicks, L.; et al. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries.1. Fractures and luxations. Dent. Traumatol. 2020, 36, 314–330. [Google Scholar] [CrossRef] [PubMed]
- Bardini, G.; Musu, D.; Mezzena, S.; Dettori, C.; Cotti, E. Combined management of apical root fracture and avulsion of two maxillary permanent central incisors: A case report. Dent. J. 2021, 9, 39. [Google Scholar] [CrossRef] [PubMed]
- Kahler, B.; Heithersay, G.S. An evidence_based appraisal of splinting luxated, avulsed and root-fracture teeth. Dent. Traumatol. 2008, 24, 2–10. [Google Scholar] [CrossRef] [PubMed]
- Spinas, E.; Pipi, L.; Mezzena, S.; Giannetti, L. Use of orthodontic methods in the treatment of dental luxations: A scoping review. Dent. J. 2021, 9, 182. [Google Scholar] [CrossRef] [PubMed]
- Arikan, V.; Celikten, Z.K.; Sari, S. Treatment of horizontal root fractured central incisors and 30 months follow up: 2 case reports. Eur. J. Paediatr. Dent. 2014, 15, 199–202. [Google Scholar] [PubMed]
- Andreasen, J.O.; Andreasen, F.M.; Mejare, I.; Cveck, M. Healing of 400 intra-alveolar root fractures. 2. Effect of treatment factors such as treatment delay, repositioning, splinting type and period and antibiotics. Dent. Traumatol. 2004, 20, 203–211. [Google Scholar] [CrossRef] [PubMed]
- Abbott, P.V. Diagnosis and management of transverse root fractures. Dent. Traumatol. 2019, 3, 333–347. [Google Scholar] [CrossRef] [PubMed]
- Andreasen, F.M.; Andreasen, J.O. Prognosis of root-fractured permanent incisors prediction of healing modalities. Endod. Dent. Traumatol. 1989, 5, 11–22. [Google Scholar] [CrossRef] [PubMed]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Biagi, R.; Bardini, G.; Guidazzi, G.; Spinas, E. Conservative Non-Surgical Management of Horizontal Root-Fractured Maxillary Incisors in a Young Male with Angle Class II, Division 2, Malocclusion. Dent. J. 2021, 9, 55. https://doi.org/10.3390/dj9050055
Biagi R, Bardini G, Guidazzi G, Spinas E. Conservative Non-Surgical Management of Horizontal Root-Fractured Maxillary Incisors in a Young Male with Angle Class II, Division 2, Malocclusion. Dentistry Journal. 2021; 9(5):55. https://doi.org/10.3390/dj9050055
Chicago/Turabian StyleBiagi, Roberto, Giulia Bardini, Giuseppe Guidazzi, and Enrico Spinas. 2021. "Conservative Non-Surgical Management of Horizontal Root-Fractured Maxillary Incisors in a Young Male with Angle Class II, Division 2, Malocclusion" Dentistry Journal 9, no. 5: 55. https://doi.org/10.3390/dj9050055
APA StyleBiagi, R., Bardini, G., Guidazzi, G., & Spinas, E. (2021). Conservative Non-Surgical Management of Horizontal Root-Fractured Maxillary Incisors in a Young Male with Angle Class II, Division 2, Malocclusion. Dentistry Journal, 9(5), 55. https://doi.org/10.3390/dj9050055







