Laser Analgesia Associated with Restorative Dental Care: A Systematic Review of the Rationale, Techniques, and Energy Dose Considerations
Abstract
1. Introduction
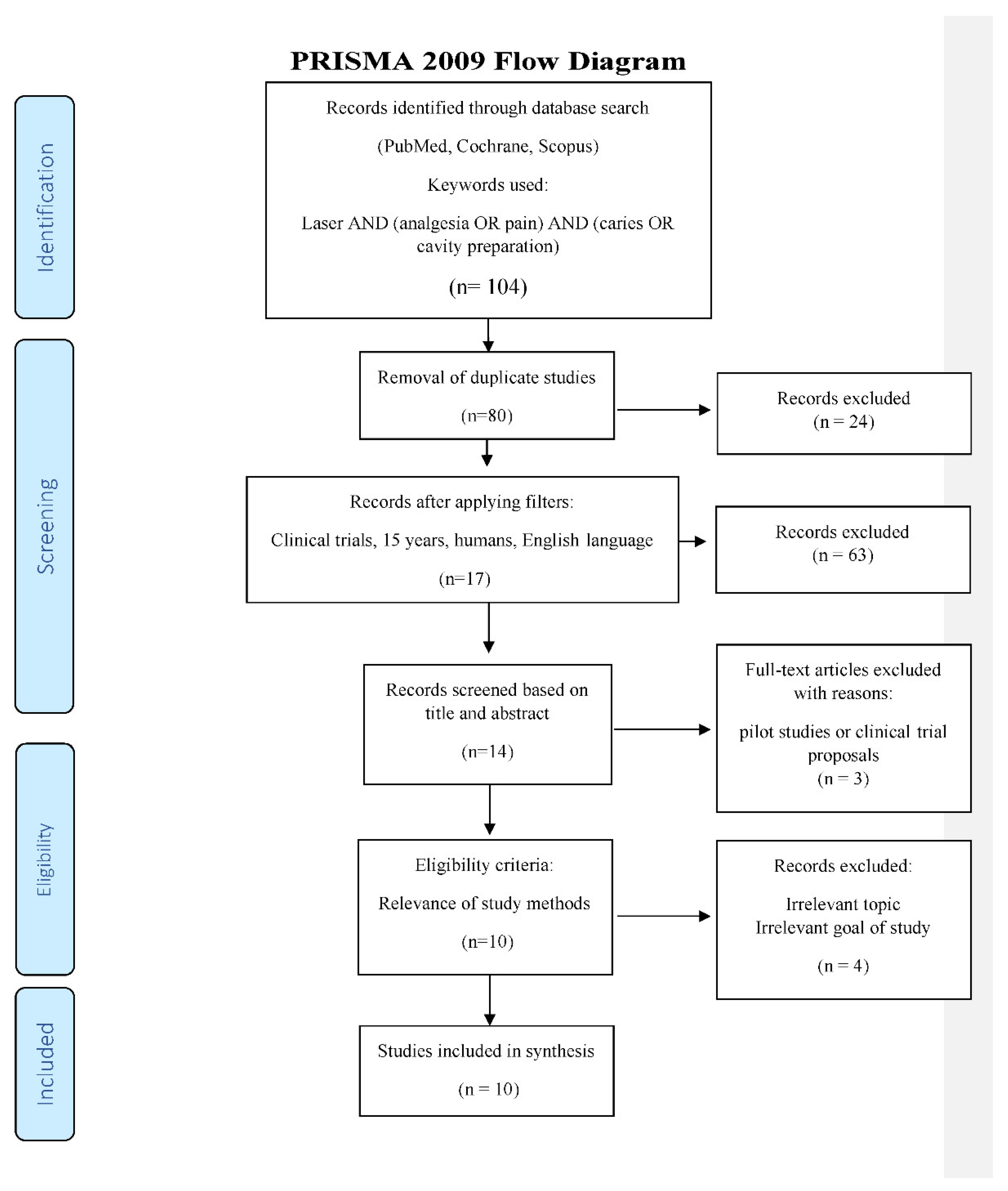
2. Materials and Methods
2.1. Search Strategy
- Laser used;
- At least 10 patients per group;
- Only clinical trials; and
- Laser use applicable to dental procedure to be carried out.
- Duplicates or studies with the same ethical approval number;
- Pain control studies where non-laser analgesia was employed;
- Less than 10 patients per group; and
- No clinical trials or study protocols or pilot studies.
2.2. Data Extraction
- Citation (first author and publication year);
- Type of study/number of patients;
- Test/control group;
- Aim/approach;
- Laser parameters applied; and
- Outcome.
2.3. Quality Assessment
- Randomization;
- Sample size calculation and required number included;
- Baseline situation similar;
- Blinding;
- Parameters of laser use described appropriately and calculations correct;
- Power meter used;
- Numerical results available (statistics);
- Outcome data complete; and
- Correct interpretation of data.
- High risk: 0–3;
- Moderate risk: 4–6; and
- Low risk: 7–9.
3. Results
3.1. Primary Outcome
3.2. Data Presentation
3.3. Quality Assessment Presentation
3.4. Analysis of Data
- In the parallel RCT study [35], results showed a significant difference in pain perception regarding the laser group.
4. Discussion
- Photo-acoustic effect of pulsed lasers [46];
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Tavares de Oliveira, M.; Galvão Arrais, C.A.; Aranha, A.C.; de Paula Eduardo, C.; Miyake, K.; Allen Rueggeberg, F.; Giannini, M. Micromorphology of resin-dentin interfaces using one-bottle etch & rinse and self-etching adhesive systems on laser-treated dentin surfaces: A confocal laser scanning microscope analysis. Lasers Surg. Med. 2010, 42, 662–670. [Google Scholar] [CrossRef]
- Frentzen, M.; Koort, H.J. Lasers in dentistry: New possibilities with advancing laser technology? Int. Dent. J. 1990, 40, 323–332. [Google Scholar] [PubMed]
- Wigdor, H.; Abt, E.; Asrafi, S.; Walsh, J.T. The effect of lasers on dental hard tissues. J. Am. Dent. Assoc. 1993, 124, 65–70. [Google Scholar] [CrossRef] [PubMed]
- Israel, M.; Cobb, C.M.; Rossmann, J.A.; Spencer, P. The effects of CO2, Nd:YAG and Er:YAG lasers with and without surface coolant on tooth root surfaces. An in vitro study. J. Clin. Periodontal. 1997, 24, 595–602. [Google Scholar] [CrossRef] [PubMed]
- Ceballos, L.; Osorio, R.; Toledo, M.; Marshall, G.W. Microleakage of composite restorations after acid or Er-YAG laser cavity treatments. Dent. Mater. 2001, 17, 340–346. [Google Scholar] [CrossRef]
- Keller, U.; Hibst, R.; Geurtsen, W.; Schilke, R.; Heidemann, D.; Klaiber, B.; Raab, W.H.M. Erbium:YAG laser application in caries therapy. Evaluation of patient perception and acceptance. J. Dent. 1998, 26, 649–656. [Google Scholar] [CrossRef]
- Pelagalli, J.; Gimbel, C.B.; Hansen, R.T.; Swett, A.; Winn, D.W. Investigational study of the use of Er:YAG laser versus dental drill for caries removal and cavity preparation—Phase I. J. Clin. Laser Med. Surg. 1997, 15, 109–115. [Google Scholar] [CrossRef]
- Matsumoto, K.; Nakamura, Y.; Mazeki, K.; Kimura, Y. Clinical dental application of Er:YAG laser for class V cavity preparation. J. Clin. Laser Med. Surg. 1996, 14, 123–127. [Google Scholar] [CrossRef]
- Cozean, C.; Arcoria, C.J.; Pelagalli, J.; Powell, G.L. Dentistry for the 21st century? Erbium:YAG laser for teeth. J. Am. Dent. Assoc. 1997, 128, 1080–1087. [Google Scholar] [CrossRef]
- Chan, A.; Armati, P.; Moorthy, A.P. Pulsed Nd:YAG laser induces pulpal analgesia: A randomized clinical trial. J. Dent. Res. 2012, 91, 79S–84S. [Google Scholar] [CrossRef]
- Holroyd, I. Conscious sedation in pediatric dentistry. A short review of the current UK guidelines and the technique of inhalation sedation with nitrous oxide. Pediatr. Anaesth. 2008, 18, 13–17. [Google Scholar] [CrossRef] [PubMed]
- Houpt, M.I.; Limb, R.; Livingstone, R.L. Clinical effects of nitrous oxide conscious sedation in children. Pediatr. Dent. 2004, 26, 29–36. [Google Scholar] [PubMed]
- Ryding, H.A.; Murphy, H.J. Use of Nitrous Oxide and Oxigen for Conscious Sedation to Manage Pain and Anxiety. J. Can. Dent. Assoc. 2007, 73, 7–11. [Google Scholar] [PubMed]
- Zacny, J.P.; Hurst, R.J.; Graham, L.; Janiszewski, D.J. Preoperative dental anxiety and mood changes during nitrous oxide inhalation. J. Am. Dent. Assoc. 2002, 133, 82–88. [Google Scholar] [CrossRef] [PubMed]
- Chow, R.T.; David, M.A.; Armati, P.J. 830 nm laser irradiation induces varicosity formation, reduces mitochondrial membrane potential and blocks fast axonal flow in small and medium diameter rat dorsal root ganglion neurons: Implications for the analgesic effects of 830 nm laser. J. Periph. Nerv. Syst. 2007, 12, 28–39. [Google Scholar] [CrossRef]
- Chow, R.T.; Armati, P.J. Photobiomodulation: Implications for anesthesia and pain relief. Photomed. Laser Surg. 2016, 34, 599–609. [Google Scholar] [CrossRef]
- Cronshaw, M.; Parker, S.; Arany, P. Feeling the Heat: Evolutionary and microbial basis for the analgesic mechanisms of photobiomodulation therapy. Photobiomodul. Photomed. Laser Surg. 2019, 37, 517–526. [Google Scholar] [CrossRef]
- Colucci, V.; Lucisano Botelho do Amaral, F.; Pécora, J.D.; Palma-Dibb, R.; Corona, S. Water flow on erbium:yttrium–aluminum–garnet laser irradiation: Effects on dental tissues. Lasers Med. Sci. 2009, 24, 811–818. [Google Scholar] [CrossRef]
- Bello-Silva, M.S.; Wehner, M.; de Paula Eduardo, C.; Lampert, F.; Poprawe, R.; Hermans, M.; Esteves-Oliveiraet, M. Precise ablation of dental hard tissues with ultra-short pulsed lasers. Preliminary exploratory investigation on adequate laser parameters. Lasers Med. Sci. 2013, 28, 171–184. [Google Scholar] [CrossRef]
- Bedi, R.; Sutcliff, P.; Donnan, P.T.; McConnachie, J. The prevalence of dental anxiety in a group of 13- and 14-year-old Scottish children. Int. J. Paediatr. Dent. 1992, 2, 17–24. [Google Scholar] [CrossRef]
- Ayer, W.A.; Domoto, P.K.; Gale, E.N.; Joy, E.D., Jr.; Melamed, B.G. Overcoming dental fear: Strategies for its prevention and management. J. Am. Dent. Assoc. 1983, 107, 18–27. [Google Scholar] [CrossRef] [PubMed]
- Caprioglio, A.; Mariani, L.; Tettamanti, L. A pilot study about emotional experiences by using CFSS-DS in young patients. Eur. J. Paediatr. Dent. 2009, 10, 121–124. [Google Scholar] [PubMed]
- Lundgren, J.; Berggren, U.; Carlsson, S.G. Psychophysiological reactions in dental phobic patients with direct vs. indirect fear acquisition. J. Behav. Ther. Exp. Psychiatry 2004, 35, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Myers, T.D.; McDaniel, J.D. The pulsed Nd:YAG dental laser: Review of clinical applications. J. Calif. Dent. Assoc. 1991, 19, 25–30. [Google Scholar]
- White, J.M.; Goodis, H.E.; Daniels, T.E. Effects of Nd:YAG laser on pulps of extracted teeth. Lasers Life Sci. 1991, 4, 191–200. [Google Scholar]
- The Institute for Laser Dentistry. Clinical Procedures Performed with the American Dental Laser; The Institute for Laser Dentistry: Hawaii, HI, USA, 1991. [Google Scholar]
- Parkins, F.; Miller, R. Nd:YAG laser analgesia of dentin. J. Dent. Res. 1992, 71, 162. [Google Scholar]
- Goodis, H.E.; White, J.M.; Harlan, L. Absence of pulpal response from Nd:YAG laser exposure on enamel. J. Dent. Res. 1992, 71, 162. [Google Scholar]
- Whitters, C.J.; Hall, A.; Creanor, S.L.; Moseley, H.; Gilmour, W.H.; Strang, R.; Saunders, W.P.; Orchardson, R. A clinical study of pulsed Nd: YAG laser-induced pulpal analgesia. J. Dent. 1995, 23, 145–150. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The Prizma Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement (Reprinted from Annals of Internal Medicine). PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Higgins, J.; Savović, J.; Page, M.; Elbers, R.; Sterne, J. Assessing risk of bias in a randomized trial. In Cochrane Handbook for Systematic Reviews of Interventions, 2nd ed.; Higgins, J., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M., Welch, V., Eds.; John Wiley & Sons: Chichester, UK, 2019; pp. 205–228. [Google Scholar] [CrossRef]
- Sarmadi, R.; Andersson, E.V.; Lingström, P.; Gabre, P. A Randomized Controlled Trial Comparing Er:YAG Laser and Rotary Bur in the Excavation of Caries—Patients’ Experiences and the Quality of Composite Restoration. Open Dent. J. 2018, 12, 443–454. [Google Scholar] [CrossRef]
- Liang, R.; George, R.; Walsh, L.J. Pulpal response following photo-biomodulation with a 904-nm diode laser: A double-blind clinical study. Lasers Med. Sci. 2016, 31, 1811–1817. [Google Scholar] [CrossRef] [PubMed]
- Poli, R.; Parker, S. Achieving dental analgesia with the Erbium Chromium Yttrium Scandium Gallium Garnet Laser (2780 nm): A protocol for painless conservative treatment. Photomed. Laser Surg. 2015, 33, 364–371. [Google Scholar] [CrossRef] [PubMed]
- Belcheva, A.; Shindova, M. Subjective Acceptance of Pediatric Patients during Cavity Preparation with Er:YAG Laser and Conventional Rotary Instruments. J. IMAB 2014, 20, 634–637. [Google Scholar] [CrossRef][Green Version]
- Tanboga, I.; Eren, F.; Altinok, B.; Peker, S.; Ertugral, F. The effect of low level laser therapy on pain during dental tooth-cavity preparation in children. Eur. Arch. Paediatr. Dent. 2011, 12, 93–95. [Google Scholar] [CrossRef]
- Genovese, M.D.; Olivi, G. Laser in paediatric dentistry: Patient acceptance of hard and soft tissue therapy. Eur. J. Paediatr. Dent. 2008, 9, 13–17. [Google Scholar] [PubMed]
- Matsumoto, K.; Wang, X.; Zhang, C.; Kinoshita, J.I. Effect of a Novel Er:YAG Laser in Caries Removal and Cavity Preparation: A Clinical Observation. Photomed. Laser Surg. 2007, 25, 8–13. [Google Scholar] [CrossRef]
- Liu, J.F.; Lai, Y.L.; Shu, W.Y.; Lee, S.Y. Acceptance and efficiency of Er:YAG laser for cavity preparation in children. Photomed. Laser Surg. 2006, 24, 489–493. [Google Scholar] [CrossRef]
- Boj, J.; Galofre, N.; Espana, A.; Espasa, E. Pain Perception in pediatric patients undergoing laser treatments. J. Oral Laser Appl. 2005, 5, 85–89. [Google Scholar]
- Chen, W. The Clinical applications for the Er,Cr:YSGG laser system. Chen Laser Inst. 2011, 12, 42–86. [Google Scholar]
- Bjordal, J.M.; Johnson, M.I.; Iversen, V.; Aimbire, F.; Lopes-Martins, R. Photoradiation in acute pain: A systematic review of possible mechanisms of action and clinical effects in randomized placebo-controlled trials. Photomed. Laser Surg. 2006, 24, 158–168. [Google Scholar] [CrossRef]
- Angelieri, F.; Sousa, M.V.D.S.; Kanashiro, L.K.; Siquera, D.F.; Maltagliati, L.A. Effects of low intensity laser on pain sensitivity during orthodontic movement. Dent. Press J. Orthod. 2011, 16, 95–102. [Google Scholar] [CrossRef][Green Version]
- Figueiredo Deiana, N.; Zaror, C.; Sandoval, P.; Alves, N. Effectiveness of Low-Level Laser Therapy in reducing orthodontic pain: A systematic review and meta-analysis. Pain Res. Manag. 2017, 2017, 1–18. [Google Scholar] [CrossRef]
- Moseley, G.L.; Butler, D.S. Fifteen years of explaining pain: The past, present, and future. J. Pain 2015, 16, 807–813. [Google Scholar] [CrossRef] [PubMed]
- Walsh, L.J. Laser analgesia with pulsed infrared lasers: Theory and practice. J. Oral Laser Appl. 2008, 8, 7–16. [Google Scholar]
- Hoke, J.A.; Burkes, E.J., Jr.; Gomnes, E.D.; Wolbarsht, M.L. Erbium:YAG (2.94 μm) Laser Effects on Dental Tissues. J. Laser Appl. 1990, 2, 61–65. [Google Scholar] [CrossRef]
- Cavalcanti, B.N.; Lage-Marques, J.L.; Rode, S.M. Pulpal temperature increases with Er:YAG laser and high-speed handpieces. J. Prosthet. Dent. 2003, 90, 447–451. [Google Scholar] [CrossRef]
- Attrill, D.C.; Davies, R.M.; King, T.A.; Dickinson, M.R.; Blinkhorn, A.S. Thermal effects of the Er:YAG laser on a simulated dental pulp: A quantitative evaluation of the effects of a water spray. J. Dent. 2004, 32, 35–40. [Google Scholar] [CrossRef]
- Yan, W.; Chow, R.; Armati, P.J. Inhibitory effects of visible 650-nm and infrared 808-nm laser irradiation on somatosensory and compound muscle action potentials in rat sciatic nerve: Implications for laser-induced analgesia. J. Peripher. Nerv. Syst. 2011, 16, 130–135. [Google Scholar] [CrossRef]
- Melzack, R.; Wall, P. Pain mechanisms: A new theory. Science 1965, 150, 171–179. [Google Scholar] [CrossRef]
- Testani, E.; Le Pera, D.; Del Percio, C.; Miliucci, R.; Brancucci, A.; Costanza, P.; De Armas, L.; Babiloni, C.; Rossini, P.M.; Valeriani, M. Cortical inhibition of laser pain and laser-evoked potentials by non-nociceptive somatosensory input. Eur. J. Neurosci. 2015, 42, 2407–2414. [Google Scholar] [CrossRef]
- Orchardson, R.; Peacock, J.M.; Whitters, C.J. Effect of pulsed Nd:YAG laser radiation on action potential conduction in isolated mammalian spinal nerves. Lasers Surg. Med. 1997, 21, 142–148. [Google Scholar] [CrossRef]
- Orchardson, R.; Peacock, J.M.; Whitters, C.J. Effects of pulsed Nd:YAG laser radiation on action potential conduction in nerve fibres inside teeth in vitro. J. Dent. 1998, 26, 421–426. [Google Scholar] [CrossRef]
- Orchardson, R.; Whitters, C.J. Effect of HeNe and pulsed Nd:YAG laser irradiation on intradental nerve responses to mechanical stimulation of dentine. Lasers Surg. Med. 2000, 26, 241–249. [Google Scholar] [CrossRef]
- Zeredo, J.L.; Sasaki, K.M.; Fujiyama, R.; Okada, Y.; Toda, K. Effects of low power Er:YAG laser on the tooth pulp-evoked jaw-opening reflex. Lasers Surg. Med. 2003, 33, 169–172. [Google Scholar] [CrossRef] [PubMed]
- Zeredo, J.L.; Sasaki, K.M.; Takeuchi, Y.; Toda, K. Antinociceptive effect of Er:YAG laser irradiation in the orofacial formalin test. Brain Res. 2005, 1032(1-2), 149–153. [Google Scholar] [CrossRef]
- Snyder-Mackler, L.; Bork, C.E. Effect of helium-neon laser irradiation on peripheral sensory nerve latency. Phys. Ther. 1988, 68, 223–225. [Google Scholar] [CrossRef]
- Sono, T.; Kasai, S.; Sakamoto, T.; Mito, M. Cord dorm potentials suppressed by low power laser irradiation on a peripheral nerve in the cat. J. Clin. Laser Med. Surg. 1993, 11, 115–118. [Google Scholar] [CrossRef]
- Elbay, Ü.Ś.; Tak, Ö.; Elbay, M.; Ugurluel, C.; Kaya, C. Efficacy of Low-level laser therapy in the management of postoperative pain in children after primary teeth extraction: A randomized clinical trial. Photomed. Laser Surg. 2016, 34, 171–177. [Google Scholar] [CrossRef]
- Hamblin, M.R. The role of nitric oxide in low level light therapy. Proc. SPIE 2008, 6846, 1–14. [Google Scholar] [CrossRef]
- Rochkind, S. Phototherapy in peripheral nerve regeneration: From basic science to clinical study. Neurosurg. Focus 2009, 26, E8. [Google Scholar] [CrossRef]
- Kneebone, W.J. Practical applications of low level laser therapy. Pract. Pain Manag. 2006, 6, 34–40. [Google Scholar]
- Martin, R. Laser-accelerated inflammation/pain reduction and healing. Pract. Pain. Manag. 2003, 3, 20–25. [Google Scholar]
- Farivar, S.; Malekshahabi, T.; Shiari, R. Biological effects of low level laser therapy. J. Lasers Med. Sci. 2014, 5, 58–62. [Google Scholar] [PubMed]
- Laasko, E.; Cabot, P.J. Nociceptive scores and endorphin-containing cells reduced by low-level laser therapy (LLLT) in inflamed paws of Wistar rat. Photomed. Laser Surg. 2005, 23, 32–35. [Google Scholar] [CrossRef]
- Bruehl, S.; Burns, J.W.; Chung, O.Y.; Chont, M. What do plasma beta-endorphin levels reveal about endogenous opioid analgesic function? Eur. J. Pain 2012, 16, 370–380. [Google Scholar] [CrossRef] [PubMed]
- Moriyama, Y.; Nguyen, J.; Akens, M.; Moriyama, E.H.; Lilge, L. In vivo effects of low-level laser therapy on inducible nitric oxide synthase. Lasers Surg. Med. 2009, 41, 227–231. [Google Scholar] [CrossRef] [PubMed]
- Cidral-Filho, F.J.; Mazzardo-Martins, L.; Martins, D.F.; Santos, A.R.S. Light-emitting diode therapy induces analgesia in a mouse model of postoperative pain through activation of peripheral opioid receptors and the L-arginine/nitric oxide pathway. Lasers Med. Sci. 2014, 29, 695–702. [Google Scholar] [CrossRef]
- Aimbire, F.; Albertini, R.; Pacheco, M.T.T.; Castro-Faria-Neto, H.C.; Bjordal, J.M. Low-level laser therapy indices dose-dependent reduction of TNFa levels in acute inflammation. Photomed. Laser Surg. 2006, 24, 33–37. [Google Scholar] [CrossRef]
- Fulop, M.A.; Dimmer, S.; Deluca, J.R.; Johanson, D.D.; Lenz, R.V.; Patel, K.B.; Douris, P.C.; Enwemeka, C.S. A meta-analysis of the efficacy of laser phototherapy on pain relief. Clin. J. Pain 2010, 26, 729–736. [Google Scholar] [CrossRef]
- Boschi, E.S.; Leite, C.E.; Saciura, V.C.; Caberlon, E.; Lunardelli, A.; Bitencourt, S.; Melo, D.A.S.; Oliveira, J.R. Anti-inflammatory effects of low-level laser therapy (660 nm) in the early phase in carrageenan-induced pleurisy in rat. Lasers Surg. Med. 2008, 40, 500–508. [Google Scholar] [CrossRef]
- Doukas, A.G.; Flotte, T.J. Physical characteristics and biological effects of laser-induced stress waves. Ultrasound Med. Biol. 1996, 22, 151–164. [Google Scholar] [CrossRef]


| Citation [Ref] | Type of Study/Number of Patients | Test/Control Group | Aim/Approach | Laser Parameters | Outcome |
|---|---|---|---|---|---|
| Sarmadi et al. (2018) [32] | Split-mouth RCT/25 patients with at least 2 primary caries of equal size and same location (occlusal or interproximal) | 2940 nm (28 cavities)/rotary bur (28 cavities) | Discomfort and Pain (VAS) | Enamel preparation: 250–300 mJ, VSP pulse, 30 Hz, water/air Dentin preparation: 200–300 mJ, VSP/SP pulse, 10–20 Hz, water/air Excavation dentin caries: 200–300 mJ, VSP/SP pulse, 20–30 Hz, water/air Excavation deep caries: 150–250 mJ, SP pulse, 5–15 Hz, water/air | Laser group: 10/28 patients required LA Bur group: 15/28 patients required LA No difference immediately after tx (p = 0.881) |
| Liang et al. (2016) [33] | Split-mouth RCT/30 patients, healthy maxillary first premolars examined (one tooth/group) | PBM with 904 nm (30 teeth)/placebo effect (30 teeth) | Pulpal response (EPT) 2 min prior and immediately after irradiation | PBM: Average Power 30 mW, 25 Hz, 50% duty cycle, buccal surface for 60 s, 3.6 J, 1 cm2 spot size | Significant difference p < 0.0001 |
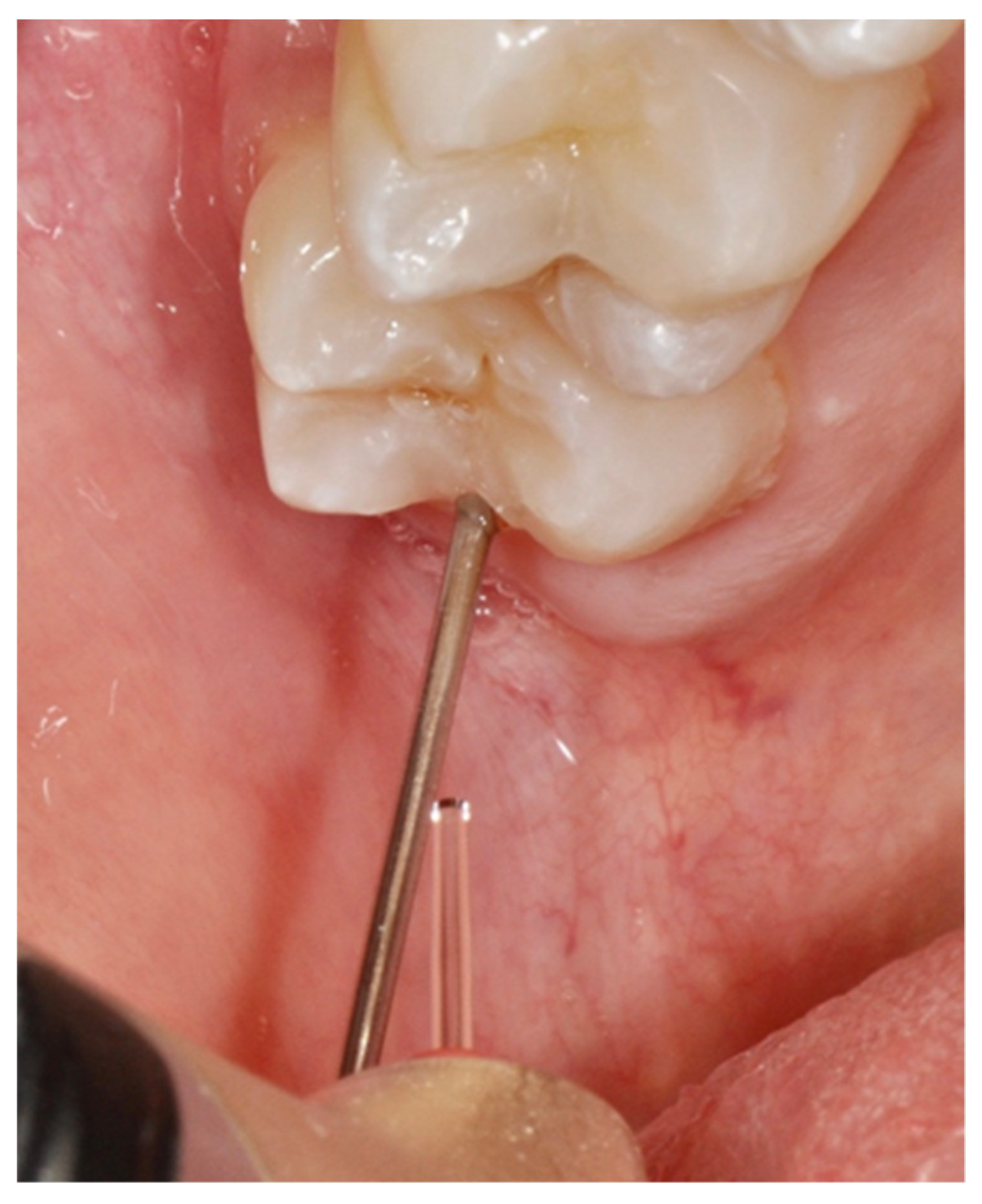
| Poli et al. (2015) [34] | Clinical trial/30 patients with a single cavity | 2780 nm | Pulpal response (EPT) for pre-, intra- and post-treatment evaluation Pain (VAS) | ANALGESIA: The delivery tip used was the MGG6 sapphire tip, diam- eter 0.600 mm, length, 6 mm (beam spot area = 0.283 mm2). Power of 0.1 W and then 0.2 W (energy per pulse 10 and 20 mJ), for 30 s each (without air/water spray), 10 Hz, tip at 10 mm from the tooth using a spacer. Subsequently, the power was increased to 0.5 and then to 1 W (33 and 67 mJ) for 60 s each, with a spray of 15% water (*10 mL/min) and 20% air, 15 Hz, keeping the same distance. Hard tissues were preconditioned with 2 W for 30 s, spray 50% water (*20 mL/min) and 80% air, 15 Hz, tip at 1 mm from the tooth. The laser was defocused if the patient felt discomfort | VAS: 0–1 values at 24/30 (80%) of patients EPT values variations: No difference (p > 0.05) |
| Chan et al. (2012) [10] | Split-mouth RCT/44 patients having a cavity by bur at bilateral premolars (one tooth/group) | Nd:YAG + sham EMLA (44 teeth)/EMLA + sham laser (44 teeth) | Pain (EPT and VAS) | ANALGESIA: 150 μsec, AP 1.1 W, 15 Hz; 60–87 mJ, 0.3–0.45 W/cm2, 73–107 J/cm2, total energy, 211- 312 J, 320 μm fiber, scanning motion (speed at 3 mm/s) approximately 1 mm (spot diameter = 6 mm) from the buccal and lingual/palatal cervical areas for 240 s | Both groups achieved analgesic effects No significant difference in EPT and VAS scores between groups |
| Belcheva et al. (2014) [35] | Parallel-group RCT/90 patients. 1 or more dentine carious lesions without pulp involvement or pain. Occlusal or proximal surface of a primary or a permanent molar | Er:YAG (45 patients)/Rotary bur (45 patients) | Pain (universal pain assessment tool) | 200–300 mJ/20 Hz, water 8 for the permanent teeth. 100–200 mJ/ 20 Hz, water 8 for the primary teeth. | Laser group significant lower pain (p = 0.005) Laser group significant difference in low degree of pain (p < 0.005) and in severe degree (p < 0.01) compared to control group, respectively |
| Tanboga et al. (2012) [36] | Split-mouth RCT/10 patients (6–9 y.o) with primary molars (one tooth/group) | LLLT (Er:YAG) + Er:YAG prep (10 teeth)/Er:YAG prep (10 teeth) | Pain (VAS) | ANALGESIA: at a distance of 2 mm from the tooth surface on the gingival margin and slowly moved for 2 min, 60 mJ, 20 Hz, 250 ms pulse, additional water spray | Test group significant better p = 0.004 |
| Genovese et al. (2008) [37] | Clinical trial/50 patients (6–12 y.o) required both hard and soft tissue therapy, without anaesthesia | Er:YAG and Er,Cr:YSGG Cavity prep: 20 permanent molars and 30 deciduous molars soft tissues: 23 frenectomies, 12 gingivectomies, 15 operculectomies | Patient’s experience (Wong-Baker modified facial image scale) | ANALGESIA: 0.5–2.5 W, 20 Hz, 75 mJ, Air 20%, Water 15%, at a distance of 3 mm from the tooth surface, in defocused mode on the gingival margin (1–3 mm), and slowly moved for 2 min | Pain values 1–2 at 44/50 (88%) of patients tested for cavity preparation |
| Matsumoto et al. (2007) [38] | Clinical trial/45 patients (95 teeth) with primary carious lesions in vital teeth | Cavity preparation in enamel and dentin with Er:YAG (95 teeth) | Pain (4-point scale) | CAVITY PREP: 100–700 mJ, 80–700 ms pulse, 8–20 Hz, water 12 mL/min | Pain values 1–2 at 85/95 (89.5%) of patients |
| Liu et al. (2006) [39] | Split-mouth RCT/40 patients (4–12 y.o) with two maxillary anterior carious teeth, same type of lesion and approximately equal-sized cavities | Er:YAG (40 teeth)/rotary bur (40 teeth) | Pain (simple modified face scale) | CAVITY PREP: 700 mJ, 10 Hz, non-contact 1 mm distance, 800 μm tip, water 24 mL/min | Laser group significantly better than control p < 0.001 |
| Boj et al. (2005) [40] | Clinical trial/33 patients (8–16 y.o.) required restorations in permanent teeth | Er,Cr:YSGG used for restorations in permanent teeth | Pain (Wong-Baker facial image scale) | Manufacturer’s recommendations | Pain values 1–2 at 22/33 (66.7%) of patients |
| Citation [Ref] | Randomization | Sample Size Calculation and Required Number Included | Baseline Situation Similar | Blinding | Parameters of Laser Use Described Appropriately and Calculations Correct | Power Meter Used | Numerical Results Available (Statistics) | No Missing Outcome Data | Correct Interpretation of Data | Total Score/ 9 |
|---|---|---|---|---|---|---|---|---|---|---|
| Sarmadi et al. (2018) [32] | yes | yes | yes | yes | no | no | yes | yes | yes | 7 |
| Liang et al. (2016) [33] | yes | no | yes | yes | yes | no | yes | yes | yes | 7 |
| Poli et al. (2015) [34] | no | no | no | no | yes | no | yes | yes | yes | 4 |
| Chan et al. (2012) [10] | yes | no | yes | yes | yes | yes | yes | yes | yes | 8 |
| Belcheva et al. (2014) [35] | yes | no | yes | no | no | no | yes | yes | yes | 5 |
| Tanboga et al. (2012) [36] | yes | no | yes | no | no | no | yes | yes | yes | 5 |
| Genovese et al. (2008) [37] | no | no | no | no | no | no | yes | yes | yes | 3 |
| Matsumoto et al. (2007) [38] | no | no | no | no | no | no | yes | yes | yes | 3 |
| Liu et al. (2006) [39] | yes | no | yes | no | no | no | yes | yes | yes | 5 |
| Boj et al. (2005) [40] | no | no | no | no | no | no | yes | yes | yes | 3 |
| Study | Pts Total/ | Cavities by Group | Treatment | Response | |
|---|---|---|---|---|---|
| Pain | No Pain | ||||
| Sarnadi [32] | 1 | 25/28 | Control | 13 | 12 |
| 25/28 | Laser | 9 | 16 | ||
| Chan [10] | 2 | 44/44 | Control | 18 | 26 |
| 44/44 | Laser | 14 | 30 | ||
| Liu [39] | 3 | 40/40 | Control | 29 | 11 |
| 40/40 | Laser | 7 | 33 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Poli, R.; Parker, S.; Anagnostaki, E.; Mylona, V.; Lynch, E.; Grootveld, M. Laser Analgesia Associated with Restorative Dental Care: A Systematic Review of the Rationale, Techniques, and Energy Dose Considerations. Dent. J. 2020, 8, 128. https://doi.org/10.3390/dj8040128
Poli R, Parker S, Anagnostaki E, Mylona V, Lynch E, Grootveld M. Laser Analgesia Associated with Restorative Dental Care: A Systematic Review of the Rationale, Techniques, and Energy Dose Considerations. Dentistry Journal. 2020; 8(4):128. https://doi.org/10.3390/dj8040128
Chicago/Turabian StylePoli, Riccardo, Steven Parker, Eugenia Anagnostaki, Valina Mylona, Edward Lynch, and Martin Grootveld. 2020. "Laser Analgesia Associated with Restorative Dental Care: A Systematic Review of the Rationale, Techniques, and Energy Dose Considerations" Dentistry Journal 8, no. 4: 128. https://doi.org/10.3390/dj8040128
APA StylePoli, R., Parker, S., Anagnostaki, E., Mylona, V., Lynch, E., & Grootveld, M. (2020). Laser Analgesia Associated with Restorative Dental Care: A Systematic Review of the Rationale, Techniques, and Energy Dose Considerations. Dentistry Journal, 8(4), 128. https://doi.org/10.3390/dj8040128








