3D Technology Development and Dental Education: What Topics Are Best Suited for 3D Learning Resources?
Abstract
1. Introduction
2. Materials and Method
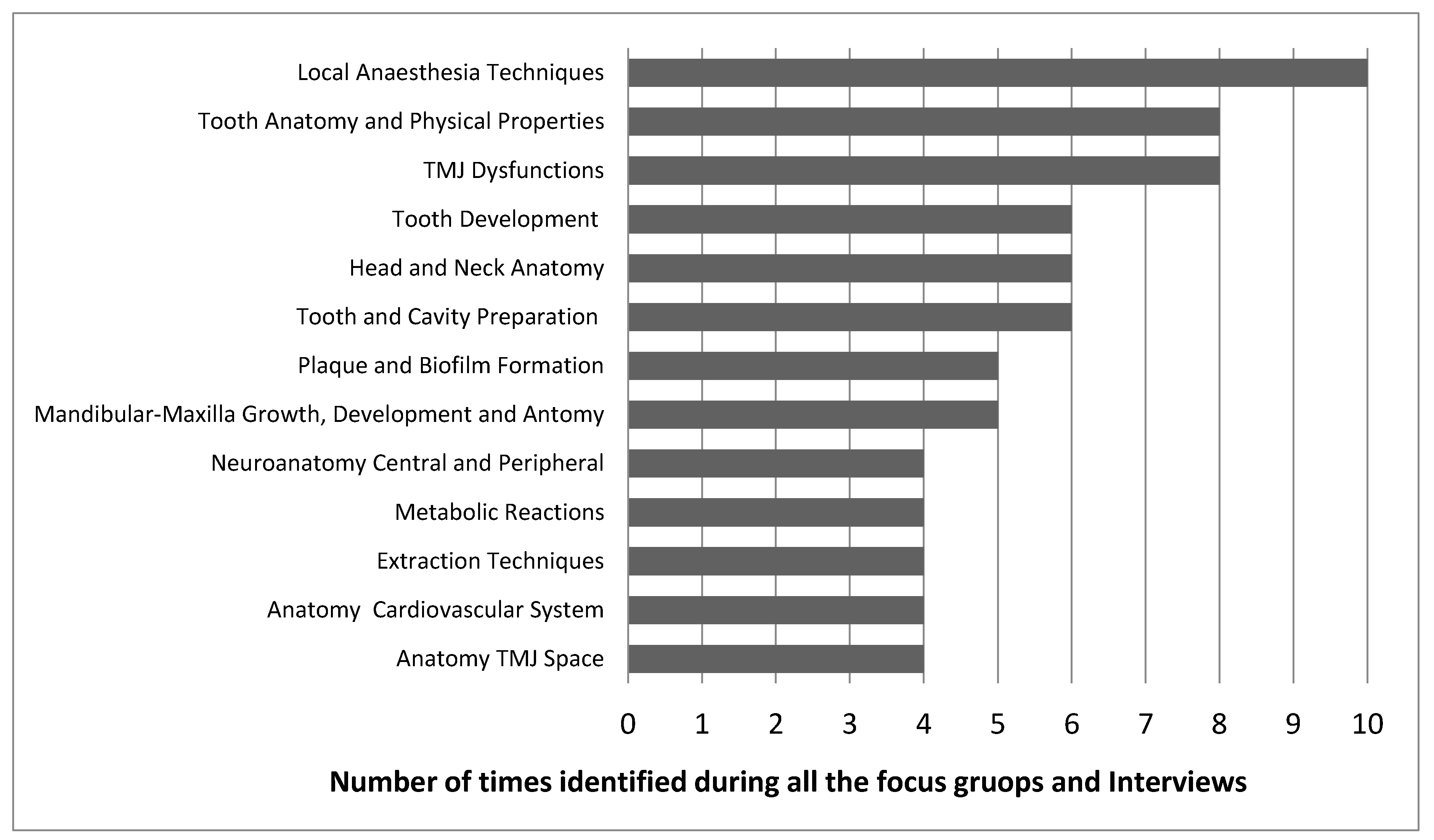
2.1. Phase 1: Focus Groups and Interviews
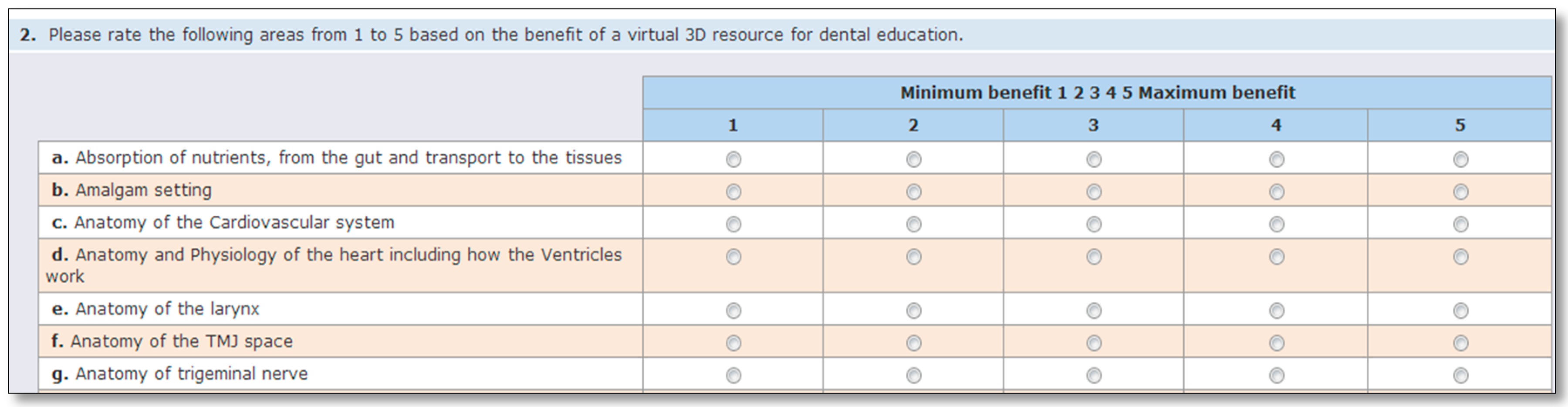
2.2. Phase 2: Survey
3. Results
4. Discussion
5. Conclusions
- There are key topics that would benefit from 3D digital learning resources: anatomy of temporomandibular joints, detail anatomy of head and neck, dental anaesthesiology, dental clinical skills techniques, dental occlusion and mandibular functioning.
- Perception of need and benefit of 3D learning resource does not vary by level of formation (undergraduate/graduate). Gender analysis only revealed difference around one topic: ‘Extraction techniques: movements and force’.
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Ethical Considerations
References
- Kirkwood, A.; Price, L. Learners and learning in the twenty-first century: What do we know about students’ attitudes towards and experiences of information and communication technologies that will help us design courses? Stud. High. Educ. 2005, 30, 257–274. [Google Scholar] [CrossRef]
- Vernon, T.; Peckham, D. The benefits of 3D modelling and animation in medical teaching. J. Vis. Commun. Med. 2002, 25, 142–148. [Google Scholar] [CrossRef]
- Bransford, J.D.; Brown, A.L.; Cocking, R.R. How People Learn: Brain, Mind, Experience, and School, Expanded ed.; Committee on Developments in the Science of Learning and Committee on Learning Research and Educational Practice, Commission on Behavioral and Social Sciences and Education; National Research Council, Ed.; National Academy Press: Washington, DC, USA, 2000. [Google Scholar]
- Kolcu, M.I.B.; Öztürkçü, Ö.S.K.; Kaki, G.D. Evaluation of a Distance Education Course Using the 4C-ID Model for Continuing Endodontics Education. J. Dent. Educ. 2020, 84, 62–71. [Google Scholar] [CrossRef]
- Tse, B.; Harwin, W.; Barrow, A.; Quinn, B.; San Diego, J.; Cox, M. Design and Development of a Haptic Dental Training System - hapTEL. In Haptics: Generating and Perceiving Tangible Sensations. EuroHaptics 2010; Lecture Notes in Computer Science; Kappers, A.M.L., van Erp, J.B.F., Bergmann Tiest, W.M., van der Helm, F.C.T., Eds.; Springer: Berlin/Heidelberg, Germany, 2010; Volume 6192. [Google Scholar] [CrossRef]
- Vincent, M.; Joseph, D.; Amory, C.; Paoli, N.; Ambrosini, P.; Mortier, É.; Tran, N. Contribution of haptic simulation to analogic training environment in restorative dentistry. J. Dent. Educ. 2020, 84, 367–376. [Google Scholar] [CrossRef] [PubMed]
- Nassar, H.M.; Tekian, A. Computer-simulation and virtual reality in undergraduate operative and restorative dental education: A critical review. J. Dent. Educ. 2020, 84, 1–18. [Google Scholar] [CrossRef]
- Brenton, H.; Hernandez, J.; Bello, F.; Strutton, P.; Purkayastha, S.; Firth, T.; Darzi, A. Using multimedia and Web3D to enhance anatomy teaching. Comput. Educ. 2007, 49, 32–53. [Google Scholar] [CrossRef]
- Brenton, H.; Hernandez, J.; Bello, F.; Strutton, P.; Firth, T.; Darzi, A. Web Based Delivery of 3D Developmental Anatomy. In Proceedings of the LET-WEB3D 2004 Workshop on Web3D Technologies, Udine, Italy, 30 September–1 October 2004; pp. 53–57. [Google Scholar]
- De Ribaupierre, S.; Wilson, T.D. Construction of a 3-D anatomical model for teaching temporal lobectomy. Comput. Biol. Med. 2012, 42, 692–696. [Google Scholar] [CrossRef] [PubMed]
- Wolfgang, K.; Friedl, R.; Preisack, M.B.; Rose, T.; Stracke, S.; Quast, K.J.; Hannekum, A.; Gödje, O. Virtual Reality and 3D Visualizations in Heart Surgery Education. In The Heart Surgery Forum; Forum Multimedia Publishing: Charlottesville, VA, USA, 2002; p. E17. [Google Scholar]
- Grimstead, I.J.; Walker, D.W.; Avis, N.J.; Kleinermann, F.; McClure, J. 3D Anatomical Model Visualization within a Grid-Enabled Environment. Comput. Sci. Eng. 2007, 9, 32–38. [Google Scholar] [CrossRef]
- Henn, J.S.; Lemole, G.M., Jr.; Ferreira, M.A.; Gonzalez, L.F.; Schornak, M.; Preul, M.C.; Spetzler, R.F. Interactive stereoscopic virtual reality: A new tool for neurosurgical education. J. Neurosurg. 2002, 96, 144–149. [Google Scholar] [CrossRef]
- Nguyen, N.; Wilson, T.D. A head in virtual reality: Development of a dynamic head and neck model. Anat. Sci. Educ. 2009, 2, 294–301. [Google Scholar] [CrossRef]
- Nowinski, W.L.; Thirunavuukarasuu, A.; Volkau, I.; Marchenko, Y.; Aminah, B.; Gelas, A.; Huang, S.; Lee, L.C.; Liu, J.; Ng, T.T.; et al. A new presentation and exploration of human cerebral vasculature correlated with surface and sectional neuroanatomy. Anat. Sci. Educ. 2009, 2, 24–33. [Google Scholar] [CrossRef] [PubMed]
- Rubin, J.S.; Summers, P.; Harris, T. Visualization of the human larynx: A three-dimensional computer modeling tool. Auris Nasus Larynx 1998, 25, 303–308. [Google Scholar] [CrossRef]
- Warrick, P.A.; Funnell, W.R.J. A VRML-based anatomical visualization tool for medical education. IEEE Trans. Inform. Technol. Biomed. 1998, 2, 55–61. [Google Scholar] [CrossRef] [PubMed]
- Field, J.; Walmsley, A.; Paganelli, C.; McLoughlin, J.; Szep, S.; Kavadella, A.; Cespedes, M.C.M.; Davies, J.R.; DeLap, E.; Levy, G.; et al. The graduating european dentist: Contemporaneous methods of teaching, learning and assessment in dental undergraduate education. Eur. J. Dent. Educ. 2017, 21, 28–35. [Google Scholar] [CrossRef] [PubMed]
- Mitov, G.; Dillschneider, T.; Abed, M.R.; Hohenberg, G.; Pospiech, P. Introducing and evaluating morphodent, a web-based learning program in dental morphology. J. Dent. Educ. 2010, 74, 1133–1139. [Google Scholar] [CrossRef] [PubMed]
- Nagasawa, S.; Yoshida, T.; Tamura, K.; Yamazoe, M.; Hayano, K.; Arai, Y.; Yamada, H.; Kasahara, E.; Ito, M. Construction of database for three-dimensional human tooth models and its ability for education and research-Carious tooth models. Dent. Mater. J. 2010, 29, 132–137. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.-S.; Yoon, T.-H.; Lee, J.-W.; Kim, D.-J. Interactive toothbrushing education by a smart toothbrush system via 3D visualization. Comput. Methods Progr. Biomed. 2009, 96, 125–132. [Google Scholar] [CrossRef]
- Gao, Y.; Peters, O.A.; Wu, H.; Zhou, X. An application framework of three-dimensional reconstruction and measurement for endodontic research. J. Endod. 2009, 35, 269–274. [Google Scholar] [CrossRef]
- Cantin, M.; Muñoz, M.; Olate, S. Generation of 3D tooth models based on three-dimensional scanning to study the morphology of permanent teeth. Int. J. Morphol. 2015, 33, 782–787. [Google Scholar] [CrossRef]
- Steinberg, A.D.; Bashook, P.G.; Drummond, J.; Ashrafi, S.; Zefran, M. Assessment of faculty perception of content validity of Periosim\copyright, a haptic-3D virtual reality dental training simulator. J. Dent. Educ. 2007, 71, 1574–1582. [Google Scholar] [CrossRef]
- De Boer, I.R.; Wesselink, P.R.; Vervoorn, J.M. The creation of virtual teeth with and without tooth pathology for a virtual learning environment in dental education. Eur. J. Dent. Educ. 2013, 17, 191–197. [Google Scholar] [CrossRef] [PubMed]
- Marras, I.; Nikolaidis, N.; Mikrogeorgis, G.; Lyroudia, K.; Pitas, I. A virtual system for cavity preparation in endodontics. J. Dent. Educ. 2008, 72, 494–502. [Google Scholar] [CrossRef] [PubMed]
- Suman, S.; Amini, A.; Elson, B.; Reynolds, P. Design and Development of Virtual leaning environment using open source virtual world technology. In Proceedings of the IFIP TC 3 International Conference on Key Competencies in the Knowledge Society (KCKS)/Held as Part of World Computer Congress (WCC), Brisbane, Australia, 20–23 September 2010; pp. 379–388, ff. ffhal-01058316f. [Google Scholar] [CrossRef]
- Dias, D.R.C.; Brega, J.R.F.; De Paiva Guimarães, M.; Modesto, F.; Gnecco, B.B.; Lauris, J.R.P. 3d semantic models for dental education. In Proceedings of the International Conference on ENTERprise Information Systems, Beijing, China, 8–11 June 2011; Springer: Berlin/Heidelberg, Germany, 2011; pp. 89–96. [Google Scholar]
- Mowery, D.; Clayton, M.; Hu, J.; Schleyer, T.K. Tooth Atlas 3.D. version 63. J. Dent. Educ. Am. Dent. Educ. Assoc. 2010, 74, 1261–1264. [Google Scholar]
- Salajan, F.D.; Mount, G.J.; Prakki, A. An Assessment of Students’ Perceptions of Learning Benefits Stemming from the Design and Instructional Use of a Web3D Atlas. Electron. J. E-Learn. 2015, 13, 120–137. [Google Scholar]
- Yamaguchi, S.; Yamada, Y.; Yoshida, Y.; Noborio, H.; Imazato, S. Development of three-dimensional patient face model that enables real-time collision detection and cutting operation for a dental simulator. Dent. Mater. J. 2012, 31, 1047–1053. [Google Scholar] [CrossRef]
- Anderson, P.; Chapman, P.; Ma, M.; Rea, P. Real-time medical visualization of human head and neck anatomy and its applications for dental training and simulation. Curr. Med. Imaging Rev. 2013, 9, 298–308. [Google Scholar] [CrossRef]
- Anderson, P.; Ma, M.; Poyade, M.; Anderson, P.; Ma, M.; Poyade, M. A Haptic-Based Virtual Reality Head and Neck Model for Dental Education. In Virtual, Augmented Reality and Serious Games for Healthcare 1; Springer: Berlin/Heidelberg, Germany, 2014; pp. 29–50. [Google Scholar]
- Ammann, A.; Klebba, A.; Krueckeberg, J.; Matthies, H. The next generation of patient education: Multilingual Dental Explorer 3D. Int. J. Comput. Dent. 2010, 13, 43–55. [Google Scholar]
- Maggio, M.P.; Hariton-Gross, K.; Gluch, J. The use of independent, interactive media for education in dental morphology. J. Dent. Educ. 2012, 76, 1497–1511. [Google Scholar] [CrossRef]
- Hamil, L.M.; Mennito, A.S.; Renné, W.G.; Vuthiganon, J. Dental Students’ Opinions of Preparation Assessment with E4D Compare Software Versus Traditional Methods. J. Dent. Educ. 2014, 78, 1424–1431. [Google Scholar] [CrossRef]
- Soares, P.V.; De Almeida, M.G.; Pereira, F.A.; Reis, B.R.; Soares, C.J.; De Sousa Meneses, M.; De Freitas Santos-Filho, P.C. Rapid prototyping and 3D-virtual models for operative dentistry education in Brazil. J. Dent. Educ. 2013, 77, 358–363. [Google Scholar] [CrossRef]
- Vuchkova, J.; Maybury, T.S.; Farah, C.S. Testing the educational potential of 3D visualization software in oral radiographic interpretation. J. Dent. Educ. 2011, 75, 1417–1425. [Google Scholar] [CrossRef] [PubMed]
- Wright, E.F.; Hendricson, W.D. Evaluation of a 3-D interactive tooth atlas by dental students in dental anatomy and endodontics courses. J. Dent. Educ. 2010, 74, 110–122. [Google Scholar] [CrossRef] [PubMed]
- Papadopoulos, L.; Pentzou, A.-E.; Louloudiadis, K.; Tsiatsos, T.-K. Design and evaluation of a simulation for pediatric dentistry in virtual worlds. J. Med. Internet Res. 2013, 15, e240. [Google Scholar] [CrossRef] [PubMed]
- Hu, J.; Yu, H.; Shao, J.; Li, Z.; Wang, J.; Wang, Y. Effects of dental 3D multimedia system on the performance of junior dental students in preclinical practice: A report from China. Adv. Health Sci. Educ. 2009, 14, 123–133. [Google Scholar] [CrossRef]
- Qi, S.; Yan, Y.; Li, R.; Hu, J. The Impact of Active Versus Passive Use of 3D Technology: A Study of Dental Students at Wuhan University, China. J. Dent. Educ. 2013, 77, 1536–1542. [Google Scholar] [CrossRef]
- Kikuchi, H.; Ikeda, M.; Araki, K. Evaluation of a virtual reality simulation system for porcelain fused to metal crown preparation at Tokyo Medical and Dental University. J. Dent. Educ. 2013, 77, 782–792. [Google Scholar] [CrossRef]
- Höhne, C.; Schwarzbauer, R.; Schmitter, M. 3D Printed Teeth with Enamel and Dentin Layer for Educating Dental Students in Crown Preparation. J. Dent. Educ. 2019, 83, 1457–1463. [Google Scholar] [CrossRef]
- Kröger, E.; Dekiff, M.; Dirksen, D. 3D printed simulation models based on real patient situations for hands-on practice. Eur. J. Dent. Educ. 2017, 21, e119–e125. [Google Scholar] [CrossRef]
- Jenson, C.E.; Forsyth, D.M. Virtual Reality Simulation: Using Three-dimensional Technology to Teach Nursing Students. Comput. Inf. Nurs. 2012, 30, 312–318. [Google Scholar] [CrossRef]
- Dickey, M.D. 3D Virtual Worlds: An Emerging Technology for Traditional and Distance Learning. Distance Educ. 2003, 24, 105–121. [Google Scholar] [CrossRef]
- Towers, A.; Field, J.; Stokes, C.; Maddock, S.; Martin, N. A scoping review of the use and application of virtual reality in pre-clinical dental education. Br. Dent. J. 2019, 226, 358–366. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, M.; Nakajima, T.; Mori, A.; Tanaka, D.; Fujino, T.; Chiyokura, H. Three-dimensional computer graphics for surgical procedure learning: Web three-dimensional application for cleft lip repair. Cleft Palate Craniofac. J. 2006, 43, 266–271. [Google Scholar] [CrossRef] [PubMed]
- Spallek, H.; Kaiser, R.; Boberick, K.; Boston, D.; Schleyer, T. Web-Based 3D Online Crown Preparation Course for Dental Students. In Proceedings of the AMIA Symposium, Los Angeles, CA, USA, 4–8 November 2000; p. 1138. [Google Scholar]
- Marsh, K.R.; Giffin, B.F.; Lowrie, D.J. Medical Student Retention of Embryonic Development: Impact of the Dimensions Added by Multimedia Tutorials. Anat. Sci. Educ. 2008, 1, 252–257. [Google Scholar] [CrossRef] [PubMed]
- Hisley, K.C.; Anderson, L.D.; Smith, S.E.; Kavic, S.M.; Tracy, J.K. Coupled physical and digital cadaver dissection followed by a visual test protocol provides insights into the nature of anatomical knowledge and its evaluation. Anat. Sci. Educ. 2008, 1, 27–40. [Google Scholar] [CrossRef]
- Jones, D.G. Reassessing the importance of dissection: A critique and elaboration. Clin. Anat. 1997, 10, 123–127. [Google Scholar] [CrossRef]
- Petersson, H.; Sinkvist, D.; Wang, C.; Smedby, Ö. Web-based interactive 3D visualization as a tool for improved anatomy learning. Anat. Sci. Educ. 2009, 2, 61–68. [Google Scholar] [CrossRef]
- Nguyen, N.; Nelson, A.J.; Wilson, T.D. Computer visualizations: Factors that influence spatial anatomy comprehension. Anat. Sci. Educ. 2012, 5, 98–108. [Google Scholar] [CrossRef]
- Creswell, J.W. Educational Research: Planning, Conducting, and Evaluating Quantitative; Prentice Hall: Upper Saddle River, NJ, USA, 2002. [Google Scholar]
- Nassar-McMillan, S.C.; Borders, L.D. Use of Focus Groups in Survey Item Development. Qual. Rep. 2002, 7, 1–12. Available online: https://nsuworks.nova.edu/tqr/vol7/iss1/3 (accessed on 24 June 2020).
- Nichter, M.; Nichter, M.; Thompson, P.J.; Shiffman, S.; Moscicki, A.-B. Using qualitative research to inform survey development on nicotine dependence among adolescents. Drug Alcohol Depend. 2002, 68, 41–56. [Google Scholar] [CrossRef]
- Wolff, B.; Knodel, J.; Sittitrai, W. Focus groups and surveys as complementary research methods. Complement. Res. Methods 1993, 118–136. [Google Scholar]
- Riquelme, A.; Padilla, O.; Herrera, C.; Olivos, T.; Román, J.A.; Sarfatis, A.; Solis, N.; Pizarro, M.; Torres, P.; Roff, S. Development of ACLEEM questionnaire, an instrument measuring residents’ educational environment in postgraduate ambulatory setting. Med. Teach. 2013, 35, e861–e866. [Google Scholar] [CrossRef] [PubMed]
- Fern, E.F. Advanced Focus Group Research; Sage Publication Inc.: Newbury Park, CA, USA, 2001. [Google Scholar]
- Krueger, R.A. Focus Groups. A Practical Guide for Applied Research; SAGE: Thousand Oaks, CA, USA, 2009. [Google Scholar]
- Deutskens, E.; De Ruyter, K.; Wetzels, M.; Oosterveld, P. Response rate and response quality of internet-based surveys: An experimental study. Mark. Lett. 2004, 15, 21–36. [Google Scholar] [CrossRef]
- Salajan, F.D.; Mount, G.J. University of Toronto’s dental school shows “new teeth”: Moving towards online instruction. J. Dent. Educ. 2008, 72, 532–542. [Google Scholar] [CrossRef] [PubMed]
- Hu, A.; Wilson, T.; Ladak, H.; Haase, P.; Doyle, P.; Fung, K. Evaluation of a Three-Dimensional Educational Computer Model of the Larynx: Voicing a New Direction. J. Otolaryngol. Head Neck Surg. 2010, 39, 315–322. [Google Scholar] [PubMed]
- Lewis, T.; Burnett, B.; Tunstall, R.; Abrahams, P. Complementing anatomy education using three-dimensional anatomy mobile software applications on tablet computers. Clin. Anat. 2013, 27, 313–320. [Google Scholar] [CrossRef] [PubMed]
- Murray, F.J.; Blinkhorn, A.S.; Bulman, J. An assessment of the views held by recent graduates on their undergraduate course. Eur. J. Dent. Educ. 1999, 3, 3–9. [Google Scholar] [CrossRef]
- Brand, H.; Kuin, D.; Baart, J. A survey of local anaesthesia education in European dental schools. Eur. J. Dent. Educ. 2008, 12, 85–88. [Google Scholar] [CrossRef]
- Jenkins, D.B.; Spackman, G.K. A method for teaching the classical inferior alveolar nerve block. Clin. Anat. 1995, 8, 231–234. [Google Scholar] [CrossRef]
- Vandenberg, S.G.; Kuse, A.R. Mental rotations, a group test of three-dimensional spatial visualization. Percept. Mot. Skills. 1978, 47, 599–604. [Google Scholar] [CrossRef]
- Newcombe, N.S.; Stieff, M. Six myths about spatial thinking. Int. J. Sci. Educ. 2012, 34, 955–971. [Google Scholar] [CrossRef]
- Gonzales, R.A.; Ferns, G.; Vorstenbosch, M.A.T.M.; Smith, C.F. Does spatial awareness training affect anatomy learning in medical students? Anat. Sci. Educ. 2020. [Google Scholar] [CrossRef] [PubMed]
- Macluskey, M.; Durham, J.; Bell, A.; Cowpe, J.; Crean, S.J.; Dargue, A.; Dawson, L.; Freeman, C.; Jones, J.; McDouagh, A.; et al. A national survey of UK final year students’ opinion of undergraduate oral surgery teaching. Eur. J. Dent. Educ. 2012, 16, e205–e212. [Google Scholar] [CrossRef] [PubMed]
- Cottrell, D.A.; Reebye, U.N.; Blyer, S.M.; Hunter, M.J.; Mehta, N. Referral patterns of general dental practitioners for oral surgical procedures. J. Oral Maxillofac. Surg. 2007, 65, 686–690. [Google Scholar] [CrossRef] [PubMed]
- Okeson, J.P. Management of Temporomandibular Disorders and Occlusion, 7th ed.; Elsevier: Amsterdam, The Netherlands, 2013. [Google Scholar]
- Ash, M.M. Occlusion, TMDs, and dental education. Head Face Med. 2007, 3, 1–4. [Google Scholar] [CrossRef]
- Stockstill, J.; Greene, C.S.; Kandasamy, S.; Campbell, D.; Rinchuse, D. Survey of orthodontic residency programs: Teaching about occlusion, temporomandibular joints, and temporomandibular disorders in postgraduate curricula. Am. J. Orthod. Dentofac. Orthop. 2011, 139, 17–23. [Google Scholar] [CrossRef]
- Türp, J.; Greene, C.; Strub, J. Dental occlusion: A critical reflection on past, present and future concepts. J. Oral Rehabil. 2008, 35, 446–453. [Google Scholar] [CrossRef]
- Jasinevicius, T.; Yellowitz, J.A.; Vaughan, G.G.; Brooks, E.S.; Baughan, L.W.; Cline, N.; Theiss, L.B. Centric relation definitions taught in 7 dental schools: Results of faculty and student surveys. J. Prosthodont. 2000, 9, 87–94. [Google Scholar] [CrossRef]
- Gross, D.; Schäfer, G. “Feminization” in German dentistry. Career paths and opportunities—A gender comparison. Women Stud. Int. Forum 2011, 34, 130–139. [Google Scholar] [CrossRef]
- McKay, J.C.; Quiñonez, C.R. The feminization of dentistry: Implications for the profession. J. Can. Dent. Assoc. 2012, 78, c1. [Google Scholar]
- Neumann, L.M. Trends in dental and allied dental education. J. Am. Dent. Assoc. 2004, 135, 1253–1259. [Google Scholar] [CrossRef]
- Nulty, D.D. The adequacy of response rates to online and paper surveys: What can be done? Assess. Eval. High. Educ. 2008, 33, 301–314. [Google Scholar] [CrossRef]
- Gal, G.B.; Weiss, E.I.; Gafni, N.; Ziv, A. Preliminary assessment of faculty and student perception of a haptic virtual reality simulator for training dental manual dexterity. J. Dent. Educ. 2011, 75, 496–504. [Google Scholar] [CrossRef] [PubMed]
- Hanson, L.M. The Utilization of Mixed-Reality Technologies to Teach Techniques for Administering Local Anesthesia. All Graduate Theses and Dissertations. 2011, p. 850. Available online: https://digitalcommons.usu.edu/etd/850 (accessed on 24 June 2020).
- GDC Preparing for Practice-Dental Team Learning Outcomes for Registration [Internet]. London: General Dental Council. 2015. Available online: https://www.gdc-uk.org/docs/default-source/quality-assurance/preparing-for-practice-(revised-2015).pdf (accessed on 20 May 2019).
| Focus Group Template |
|---|
|
| Ranking | Item | Percentage of Participant that Ranked the Item as Beneficial |
|---|---|---|
| Anatomy of the TMJ space | 98% |
| Root canal treatment model representing what happens inside the canal and how to determine the working length | 92% |
| Local anaesthesia techniques including the needle position, the tissues and how the needle passes through or close to. | 90% |
| Anatomy of trigeminal nerve | 91% |
| Concepts in occlusion such as Bennett angle, Bennett movement, condylar guidance, anterior guide, excursive movements | 89% |
| Tooth and cavity preparation for crowns, onlays, inlays, ¾ crowns, endodontic access | 88% |
| Head and neck anatomy | 86% |
| Suturing techniques | 86% |
| TMJ dysfunction; including for example clicking temporomandibular joints | 86% |
| Impacted tooth identification and extraction techniques | 85% |
| Extraction techniques: movements and force to extract the tooth | 84% |
| Third molar extractions | 84% |
| Surgical procedures for implants | 84% |
| Course of cranial nerves until the innervated tissues | 83% |
| Occlusion functioning and types | 83% |
| Masticatory muscles anatomy and physiology | 82% |
| Caries removal including tactile feedback | 80% |
| Flap design | 79% |
| Mandibular and maxillary development, growth and anatomy | 77% |
| Use of elevators | 77% |
| Mandibular fracture | 76% |
| Tooth anatomy and tooth physical properties | 77% |
| Denture design—3D model to design cobalt-chrome dentures | 76% |
| Normal movements of the jaw and pathological movement | 76% |
| Removal of large lesions such as cysts | 76% |
| Space infections of the head and neck | 76% |
| Model showing most common errors and bad decision making for restorative dentistry (e.g., errors in prosthesis design, errors in crown preparation) | 74% |
| Development of the dental arch | 73% |
| Le Fort fractures | 73% |
| Periradicular surgery | 73% |
| Mastication process | 70% |
| Biomechanics in orthodontics (tooth movement) | 70% |
| Indirect vision practice model | 70% |
| Model in 3D of oral cancer development and progress | 70% |
| Pathogenesis of diseases | 30% |
| Pharmacology—models of how drugs work in the tissues | 29% |
| Ear anatomy model | 28% |
| Respiratory system model, including process of ventilation, perfusion | 24% |
| Kidney anatomy | 23% |
| Cell mitosis and meiosis | 22% |
| Drugs clearance methods | 21% |
| Physiology of the GI tract | 21% |
| Exchange of oxygen in the alveolus | 20% |
| DNA double helix | 20% |
| Hormonal cycles. From hormone production to their action | 20% |
| Metabolic reactions—Pathways of chemical reactions represented as interactive models | 19% |
| Absorption of nutrients, from the gut and transport to the tissues | 19% |
| Renal physiology | 19% |
| Protein synthesis | 15% |
| Functions of mitochondria and Golgi complexes | 14% |
| Molecular interaction of amino acids synthesis | 10% |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Poblete, P.; McAleer, S.; Mason, A.G. 3D Technology Development and Dental Education: What Topics Are Best Suited for 3D Learning Resources? Dent. J. 2020, 8, 95. https://doi.org/10.3390/dj8030095
Poblete P, McAleer S, Mason AG. 3D Technology Development and Dental Education: What Topics Are Best Suited for 3D Learning Resources? Dentistry Journal. 2020; 8(3):95. https://doi.org/10.3390/dj8030095
Chicago/Turabian StylePoblete, Paulina, Sean McAleer, and Andrew G Mason. 2020. "3D Technology Development and Dental Education: What Topics Are Best Suited for 3D Learning Resources?" Dentistry Journal 8, no. 3: 95. https://doi.org/10.3390/dj8030095
APA StylePoblete, P., McAleer, S., & Mason, A. G. (2020). 3D Technology Development and Dental Education: What Topics Are Best Suited for 3D Learning Resources? Dentistry Journal, 8(3), 95. https://doi.org/10.3390/dj8030095




