Minimally Invasive Diastema Restoration with Prefabricated Sectional Veneers
Abstract
1. Introduction
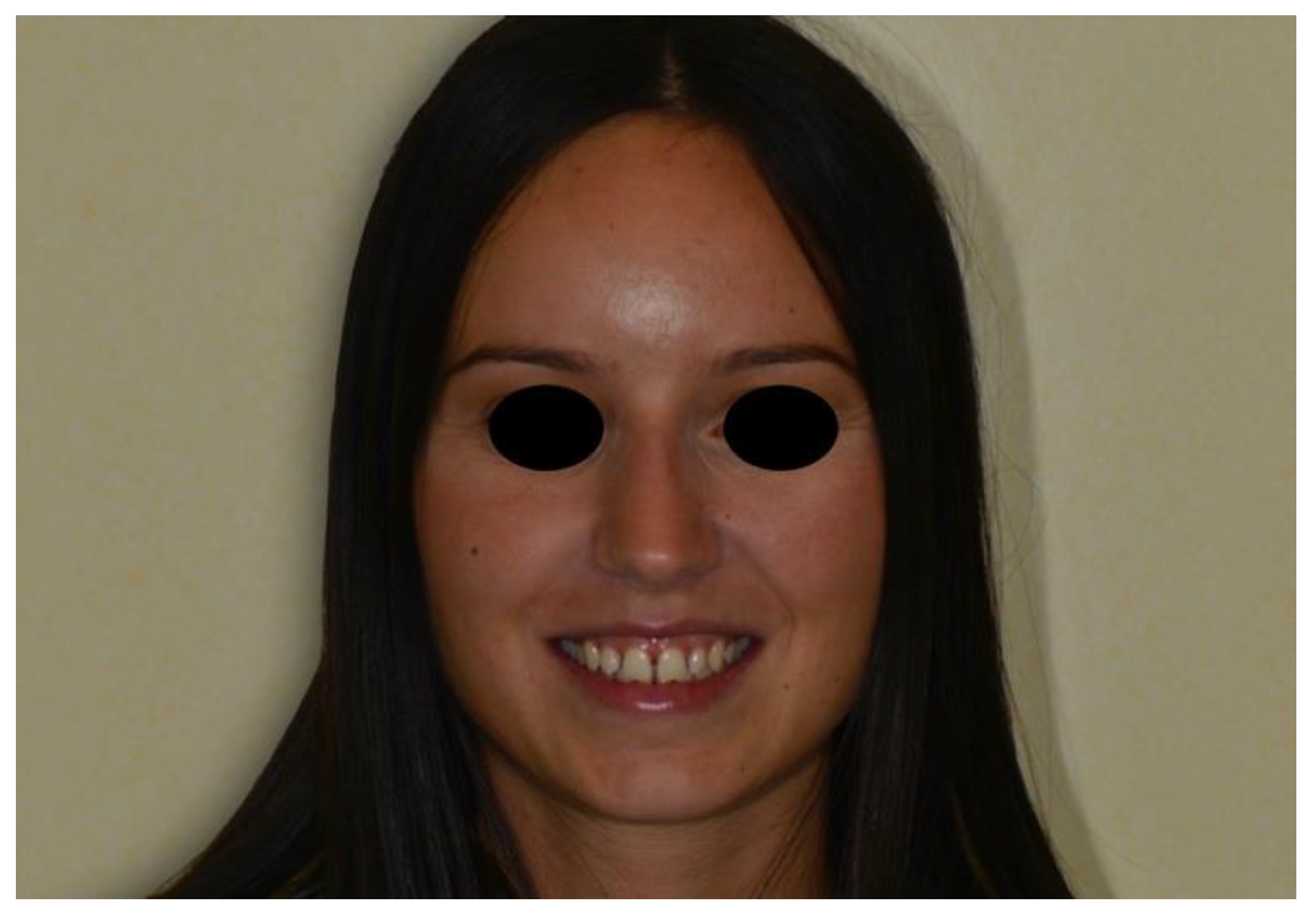
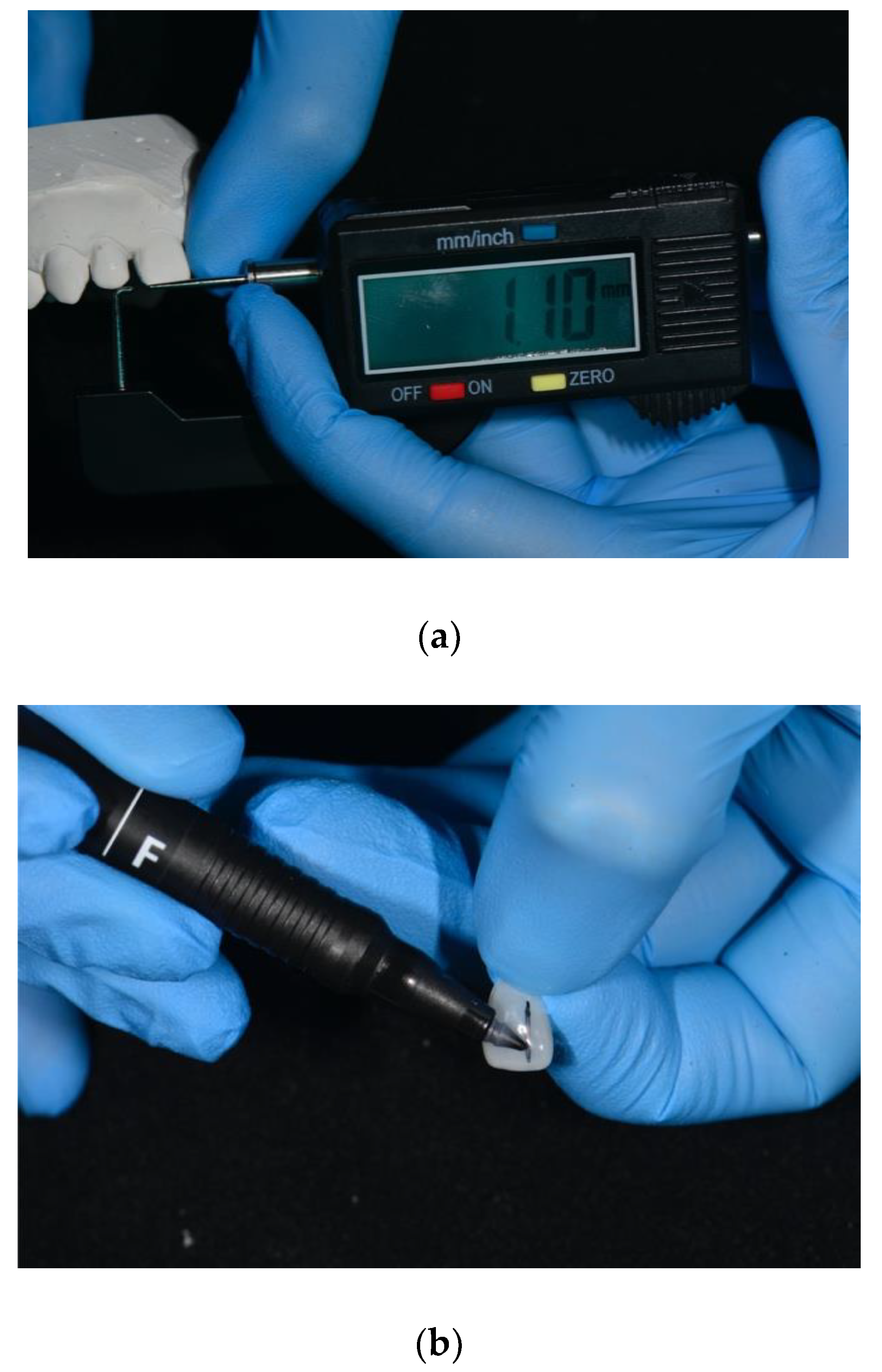
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Consent
References
- Kaya, D.; Taner, T. Management of an Adult with Spaced Dentition, Class III Malocclusion and Open-bite Tendency. Eur. J. Dent. 2011, 5, 121–129. [Google Scholar] [CrossRef]
- Gkantidis, N.; Psomiadis, S.; Topouzelis, N. Teeth spacing: Etiology and treatment. Hell. Orthod. Rev. 2007, 10, 75–92. [Google Scholar]
- Fuhrer, N.; Vardimon, A.D. Clinical analysis and treatment of spaced dentition. Pract. Periodontics Aesthetic Dent. 1997, 9, 493–501. [Google Scholar]
- Foruse, A.; Franco, E.J.; Mondelli, J. Esthetic and functional restoration for an anterior open occlusal relationship with multiple diastemata: A multidisciplinary approach. J. Prosthet. Dent. 2017, 99, 91–94. [Google Scholar] [CrossRef]
- Oquendo, A.; Brea, L.; David, S. Diastema: Correction of Excessive Spaces in the Esthetic Zone. Dent. Clin. N. Am. 2011, 55, 265–281. [Google Scholar] [CrossRef]
- Chu, F.C.; Siu, A.S.; Newsone, P.R.; Wei, S.H. Management of median diastema. Gen. Dent. 2001, 49, 282–287. [Google Scholar]
- Gestakovski, D. The injectable composite resin technique: Minimally invasive reconstruction of esthetics and function. Clinical case report with 2-year follow-up. Quintess Int. 2019, 50, 712–719. [Google Scholar]
- Lowe, R. Simplifying Direct Composite Veneer Placement. Dent. Today 2015, 5, 100–103. [Google Scholar]
- Terry, D.A.; Powers, J.M. A predictable resin composite injectable technique. Dent. Today 2014, 4, 98–101. [Google Scholar]
- Gomes, G.; Perdigão, J. Prefabricated composite vener: A clinical review. J. Esthet. Restor. Dent. 2014, 5, 302–313. [Google Scholar] [CrossRef]
- De Araujo, E.M., Jr.; Fortkamp, S.; Baratieri, L.N. Closure of diastema and gingival recontouring using direct adhesive restorations: A case report. J. Esthet. Restor. Dent. 2009, 21, 229–234. [Google Scholar] [CrossRef] [PubMed]
- Yeon-Hwa, K.; Yong-Bum, C. Diastema closure with direct composite: Architectural gingival contouring. JKA Cons. Dent. 2011, 36, 515–520. [Google Scholar]
- Barbosa, S.H.; Zanata, R.L.; Navarro, M.F.; Nunes, O. Effect of different finishing and polishing techniques on the surface roughness of microfilled, hybrid and composite resins. Braz. Dent. J. 2005, 16, 39–44. [Google Scholar] [CrossRef] [PubMed]
- Maj, G.; Maj, C. Conservative and esthetic management of diastema closure using porcelain laminate veneers. Med. J. Armed Forces India 2015, 71, 581–585. [Google Scholar]
- Magne, P.; Belser, U. Bonded Porcelain Restorations, 1st ed.; Quintessence Books: Chicago, IL, USA, 1999; pp. 3043–3107. [Google Scholar]
- Tasin, S.; Celilk, G.; Ismatullaev, A.; Usumez, A. The effect of artificial accelerated aging on the color stability, microhardness, and surface roughness of different dental laminate veneer materials. J. Esthet. Rest. Dent. 2020, 1, 1–7. [Google Scholar]
- Lewis, M.W. Prefabricated Composite Veneers. A Conservative Solution for the Aesthetic Zone. Dent. Today 2015, 34, 1001–1010. [Google Scholar]
- Singh, I.; Shetty, R.; Mehta, D.; Lampe, S.; Chida, N. Prefabricated Laser Sintered Composite Veneers and Occlusal Vertical Dimensions: Case Reports. J. Contemp. Dent. Pract. 2018, 19, 1418–1424. [Google Scholar]
- Levin, E.I. Dental esthetics and the golden proportion. J. Prosthet. Dent. 1978, 40, 244–252. [Google Scholar] [CrossRef]
- Snow, S.R. Esthetic smile analysis of maxillary anterior tooth width: The golden percentage. J. Esthet. Dent. 1999, 11, 177–184. [Google Scholar] [CrossRef]
- Ward, D.H. Proportional smile design using the recurring esthetic dental (RED) proportion. Dent. Clin. N. Am. 2001, 45, 143–154. [Google Scholar]
- Magne, P.; Gallucci, G.O.; Belser, U.C. Anatomic crown width/length ratios of unworn and worn maxillary teeth in white subjects. J. Prosthet. Dent. 2003, 89, 453–461. [Google Scholar] [CrossRef]
- Preston, J.D. The golden proportion revisited. J. Esthet. Restor. Dent. 1993, 5, 247–251. [Google Scholar] [CrossRef] [PubMed]
- Rosenstiel, S.F. Dentists’ preferences of anterior tooth proportion: A web-based study. J. Prosthet. Dent. 2000, 3, 123–136. [Google Scholar]
- Melo, M.; Ata-ali, F.; Huertas, J.; Teresa, C. Revisiting the maxillary teeth in 384 subjects reveals a deviation from the classical aesthetic dimensions. Sci. Rep. 2019, 9, 730. [Google Scholar] [CrossRef] [PubMed]
- Chu, J.S. Range and mean distribution frequency of individual tooth width of the maxillary anterior dentition. Pract. Proced. Aesthetic Dent. 2007, 19, 209–215. [Google Scholar]
- Gillen, R.J.; Schwartz, R.S.; Hilton, T.J.; Evans, D.B. An analysis of selected normative tooth proportions. Int. J. Prosthodont. 1994, 7, 410–417. [Google Scholar]
- Sterrett, J.D.; Oliver, T.; Robinson, F.; Fortson, W.; Knaak, B.; Russell, C.M. Width/length ratios of normal clinical crowns of the maxillary anterior dentition in man. J. Clin. Periodontol. 1999, 26, 153–157. [Google Scholar] [CrossRef]
- Duarte, S., Jr.; Schniner, P.; Lorenzo, A.P. The importance of width/length ratios of maxillary anterior permanent teeth in estethic rehabilitation. Eur. J. Esthet. Dent. 2008, 3, 224–234. [Google Scholar]
- Miyazaki, C.; Medeiros, I.S.; Lima, Santana, I.; Rosário, Matos, J.; Filho, L. Heat treatment of a direct composite resin: Influence on flexural strength. Braz. Oral Res. 2009, 23, 241–247. [Google Scholar] [CrossRef]
- Santana, I.L.; Lodovici, E.; Matos, J.R.; Medeiros, I.S.; Miyazaki, C.L.; Rodrigues-Filho, L.E. Effetc of experimental heat treatment on mechanical properties of resin composite. Braz. Dent. J. 2009, 20, 205–210. [Google Scholar] [CrossRef]
- Dietschi, D. Current status and future perspectives for the use of composite resins in the smile frame. J. Cosm. Dent 2011, 27, 112–127. [Google Scholar]
- Dietschi, D. Optimising aesthetics and facilitating clinical application of free-hand bonding using the ‘natural layering concept. Br. Dent. J. 2008, 204, 181–185. [Google Scholar] [CrossRef] [PubMed]
- Farias-Neto, A.; Gomes, E.M.D.C.F.; Sánchez-Ayala, A.; Sánchez-Ayala, A.; Vilanova, L.S.R. Esthetic Rehabilitation of the Smile with no-Prep Porcelain Laminates and Partial Veneers. Case Rep. Dent. 2015, 4, 206–211. [Google Scholar] [CrossRef]
- Gresnigt, M.; Ozcan, M. Esthetic rehabilitation of anterior teeth with porcelain laminates and anterior veneers. J. Can. Dent. Assoc. 2011, 77, 143. [Google Scholar]
- Magne, P.; Kwon, K.R.; Belser, C.; Hodges, J.S.; Douglas., W.H. Crack propensity of porcelain laminate veneers: A simulated operatory evaluation. J. Prosthet.Dent. 1999, 81, 327–334. [Google Scholar] [CrossRef]
- Magne, P.; Versluis, H.; Douglas, W.H. Effect of luting composite shrinkage and thermal loads on the stress distribution in porcelain laminate veneers. J. Prosthet.Dent. 1999, 81, 335–344. [Google Scholar] [CrossRef]
- Tsitrou, E.A.; van Noort, R. Brittleness index of machinable dental materials and its relation to the marginal chipping factor. J. Dent. 2007, 35, 897–902. [Google Scholar] [CrossRef] [PubMed]
- Haas, B.R. Mastique veneers: A cosmetic and financial alternative in post-periodontal care. J. N. J. Dent. Assoc. 1982, 53, 25–27. [Google Scholar] [PubMed]
- Jensen, O.E.; Soltys, J.L. Six months clinical evaluation of prefabricated veneer restorations after partial enamel removal. J. Oral Rehab. 1986, 13, 49–55. [Google Scholar] [CrossRef]
- Hoffding, J. Mastique laminate veneers: Results after 4 and 10 years of service. Acta Odontol. Scand. 1995, 53, 283–286. [Google Scholar] [CrossRef]
- Dietschi, D. Prefabricated veneers. Inside Dent. 2012, 8, 9–10. [Google Scholar]
- Dietschi, D.; Devigus, A. Prefabricated Composite Veneers: Historical Perspectives, Indications and Clinical Application. Eur. J. Esthet. Dent. 2011, 6, 2–11. [Google Scholar]
- Gresnigt, M.M.; Kalk, W.; Ozcan, M. Randomized controlled split-mouth clinical trial of direct laminate veneers with two micro-hybrid resin composites. J. Dent. 2012, 4, 766–775. [Google Scholar] [CrossRef]
- Davidson, C.L.; Feilzer, A.J. Polymwerization shrinkage and polymwerization shrinkage stress in polymer-based restoratives. J. Dent. 1997, 25, 435–440. [Google Scholar] [CrossRef]
- Benetti, A.; Peutzfeldt, A.; Lussi, A.; Flury, S. Resin composites: Modulus of elasticity and marginal quality. J. Dent. 2014, 42, 1185–1192. [Google Scholar] [CrossRef] [PubMed]
- Sarac, D.; Sarac, Y.S.; Yusbasioglu, E.; Bali, S. The effects of porcelain polishing systems on the colour and surface texture of feldspathic porcelain. J. Prosthet. Dent. 2007, 96, 122–128. [Google Scholar] [CrossRef] [PubMed]
- Da Silva, T.M.; Salvia, A.C.R.D.; de Carvalho, R.F.; Pagani, C.; da Rocha, D.M.; da Silva, E.G. Polishing for glass ceramics: Which protocol? J. Prosthodont. Res. 2014, 58, 160–170. [Google Scholar] [CrossRef] [PubMed]
- Da Costa, J.; Ferracane, J.; Paravina, R.D.; Mazur, R.F.; Roeder, L. The effect of different polishing systems on surface roughness and gloss of various resin composites. J. Esthet. Restor. Dent. 2007, 19, 214–224. [Google Scholar] [CrossRef] [PubMed]
- Endo, T.; Finger, W.J.; Kanehira, M.; Utterodt, A.; Komatsu, M. Surface texture and roughness of polished nanofill and nanohybrid resin composites. Dent. Mater. J. 2010, 29, 213–223. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kreulen, C.M.; Creugers, N.H.; Meijering, A.C. Meta-analysis of anterior veneer restorations in clinical studies. J. Dent. 1998, 26, 345–353. [Google Scholar] [CrossRef]
- Layton, D.M.; Clarke, M.; Walton, T.R. A systematic review and meta-analysis of the survival of feldspathic porcelain veneers over 5 and 10 years. Int. J. Prosthodont. 2012, 25, 590–603. [Google Scholar]
- Peumans, M.; De Munck, J.; Fieuws, S.; Lambrechts, P.; Vanherle, G.; Van Meerbeek, B. A prospective ten-year clinical trial of porce- lain veneers. J. Adhes. Dent. 2004, 6, 65–76. [Google Scholar] [PubMed]
- Marimoto, S.; Borges Albanesi, R.; Sesma, N.; Martinis Agra, C.; Braga Minatel, M. Main clinical outcomes of feldspathic porcelain and glass-ceramic laminate veneers: A systematic review and meta-analysis of survival and complication rates. Int. J. Prosthodont. 2016, 1, 38–49. [Google Scholar] [CrossRef] [PubMed]
- Mozayek, R.S.; Allaf, M.; Dayoub, S. Porcelain Sectional Veneers, an Ultra-Conservative Technique for Diastema Closure (Three-Dimensional Finite Element Stress Analysis). Dent. Med. Probl. 2019, 2, 179–183. [Google Scholar] [CrossRef] [PubMed]
- Hong, J.; Tak, S.M.; Baek, S.H.; Cho, B.H. The effect of the amount of interdental spacing on the stress distribution in maxillary central incisors restored with porcelain laminate veneer and composite resin: A 3D-finite element analysis. J. Korean Acad. Conserv. Dent. 2010, 1, 30–39. [Google Scholar] [CrossRef]
- Magne, P.; Douglas, W.H. Interdental design of porcelain veneers in the presence of composite fillings: Finite element analysis of composite shrinkage and thermal stresses. Int. J. Prosthodont. 2000, 2, 117–124. [Google Scholar]
- Nicotra, C.; Polizzi, A.; Zappalà, G.; Leonida, A.; Indelicato, F.; Caccianiga, G. A Comparative Assessment of Pain Caused by the Placement of Banded Orthodontic Appliances with and without Low-Level Laser Therapy: A Randomized Controlled Prospective Study. Dent. J. 2020, 8, 24. [Google Scholar] [CrossRef] [PubMed]
- Sfondrini, M.F.; Gandini, P.; Alcozer, R.; Vallittu, P.K.; Scribante, A. Failure load and stress analysis of orthodontic miniscrews with different transmucosal collar diameter. J. Mech. Behav. Biomed. Mater. 2018, 87, 132–137. [Google Scholar] [CrossRef]
- Madariaga, A.C.P.; Bucci, R.; Rongo, R.; Simeon, V.; D’Antò, V.; Valletta, R. Impact of Fixed Orthodontic Appliance and Clear Aligners on the Periodontal Health: A Prospective Clinical Study. Dent. J. 2020, 8, 4. [Google Scholar] [CrossRef]
- Sfondrini, M.F.; Debiaggi, M.; Zara, F.; Brerra, R.; Comelli, M.; Bianchi, M.; Pollone, S.R.; Scribante, A. Influence of lingual bracket position on microbial and periodontal parameters in vivo. J. Appl. Oral Sci. 2012, 20, 357–361. [Google Scholar] [CrossRef]
- Frese, C.; Schiller, P.; Staehle, H.J.; Wolff, D. Recontouring teeth and closing diastemas with direct composite buildups: A 5-year follow-up. J. Dent. 2013, 41, 979–985. [Google Scholar] [CrossRef]
- Peumans, M.; Van Meerbeek, B.; Lambrechts, P.; Vanherle, G. The 5-year clinical performance of direct composite additions to correct tooth form and position. II. Marginal qualities. Clin. Oral Investig. 1997, 1, 19–26. [Google Scholar] [CrossRef] [PubMed]
- Postiglione, A.; Pereira, S.; Delgado, L.C.; Phillipini, B.C. Color stability evaluation of aesthetic restorative materials. Braz. Oral Res. 2008, 22, 3–9. [Google Scholar]
- Kakaboura, A.; Rahiotis, C.; Zinelis, S.; Al-Dhamadi, Y.A.; Silikas, N.; Watts, D.C. In vitro characterization of two laboratory-processed resin composites. Dent. Mater. 2003, 19, 393–398. [Google Scholar] [CrossRef]
- Drummond, J.L. Degradation, fatigue and failure of resin dental composite materials. J. Dent. Res. 2008, 87, 710–719. [Google Scholar] [CrossRef]












© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Novelli, C.; Scribante, A. Minimally Invasive Diastema Restoration with Prefabricated Sectional Veneers. Dent. J. 2020, 8, 60. https://doi.org/10.3390/dj8020060
Novelli C, Scribante A. Minimally Invasive Diastema Restoration with Prefabricated Sectional Veneers. Dentistry Journal. 2020; 8(2):60. https://doi.org/10.3390/dj8020060
Chicago/Turabian StyleNovelli, Claudio, and Andrea Scribante. 2020. "Minimally Invasive Diastema Restoration with Prefabricated Sectional Veneers" Dentistry Journal 8, no. 2: 60. https://doi.org/10.3390/dj8020060
APA StyleNovelli, C., & Scribante, A. (2020). Minimally Invasive Diastema Restoration with Prefabricated Sectional Veneers. Dentistry Journal, 8(2), 60. https://doi.org/10.3390/dj8020060





