Short-Term Impact of Non-Surgical and Surgical Periodontal Therapy on Oral Health-Related Quality of Life in a Greek Population—A Prospective Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Ethical Considerations
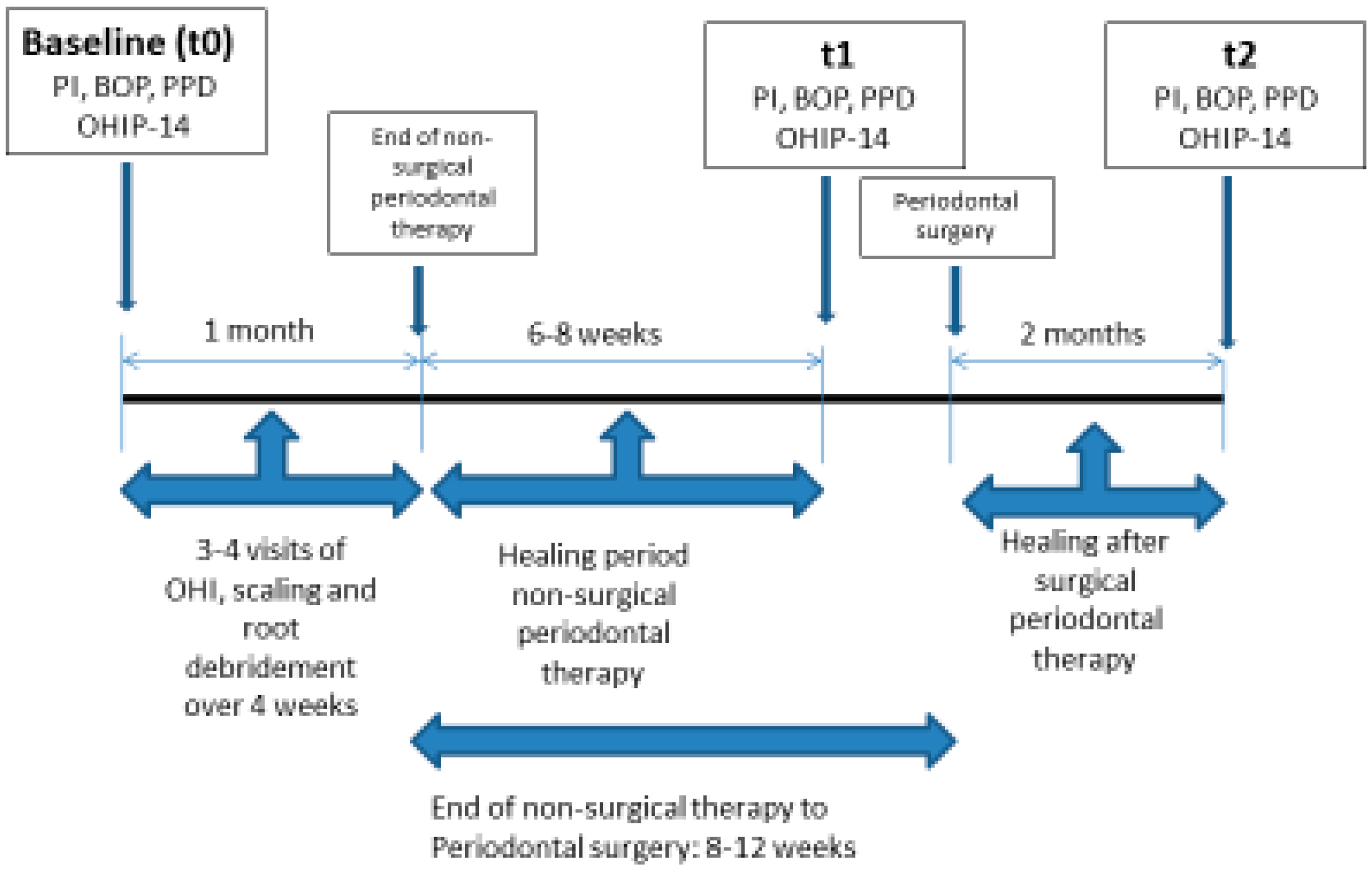
2.3. Study Design
- The medical and dental histories of the participants were obtained in order to meet the inclusion criteria. Socio-demographic data were also collected (age, gender, marital status, place of residence, years of education, family income per month, occupation, smoking habits, frequency of brushing, use of dental floss and frequency of previous dental visits).
- Assessment of oral health-related quality of life with the use of OHIP-14 questionnaire was performed:
- 1.
- At baseline (t0), before initial periodontal treatment
- 2.
- At phase I (t1), 6–8 weeks after non-surgical periodontal treatment
- 3.
- At phase II (t2), 8 weeks after surgical periodontal treatment
- Measurement of clinical parameters: The following periodontal clinical parameters were recorded at six sites per tooth, mesio-buccal, buccal, disto-buccal and mesio-lingual, lingual, disto-lingual; probing pocket depth (PD), Plaque Index (PI) and Bleeding On Probing (BOP). Clinical examination was performed using a periodontal probe (Hu-Friedy XP-23/QW, Hu-Friedy, Chicago, IL, USA), that was placed parallel to the long axis of each tooth; recordings were assessed to the nearest millimeter. The presence or absence of bleeding on probing was calculated as Full Mouth Bleeding scores (FMBS) [34] and the presence or absence of supragingival dental plaque was recorded using the O’Leary Plaque Control Record [35] expressed as percentages. Both the above indices were applied to evaluate patient compliance as well, with desired compliance being <20%. Probing pocket depth was measured and then expressed in the study as the proportion of the sites showing probing pocket depth ≥ 5 mm. The clinical examinations at each time point were performed by one trained examiner (A.V.). The assessment of intra-examiner reproducibility for the PPD, PI and BOP examinations was performed by double recordings in 20 participants. The intraclass correlation coefficients for intra-examiner reproducibility was 0.83 for PPD, 0.89 for PI and 0.91 for BOP.
2.4. Data Collection
2.5. Procedures
2.6. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
- Periodontal disease negatively affects the oral health-related quality of life and periodontal therapy has been beneficial from a patient-centered point of view in Greek adults.
- There is no correlation between the patients’ perception of quality of life expressed by OHIP-14 score and the surrogate clinical parameters assessed by the clinicians.
- The key message, according to the findings of the study, is that non-surgical periodontal treatment significantly improves function, aesthetics and psychological aspects of periodontal patients, while surgical therapy does not seem to offer any additional benefit in all the above aspects.
Author Contributions
Funding
Conflicts of Interest
References
- World Health Organization. Preamble to the Constitution of the World Health Organization as Adopted by the International Health Conference 1948, New York, 19–22 June 1946; signed on 22 July 1946 by the representatives of 61 States; World Health Organization: Geneva, Switzerland, 2003; p. 100. [Google Scholar]
- Slade, G.D.; Spencer, A.J. Development and evaluation of the Oral Health Impact Profile. Community Dent. Health 1994, 11, 2–11. [Google Scholar]
- McGrath, C.; Bedi, R. Can dental attendance improve quality of life? Br. Dent. J. 2001, 190, 262–265. [Google Scholar] [CrossRef]
- Allen, P.F. Assessment of oral health related quality of life. Health Qual. Life Outcomes 2003, 1, 40. [Google Scholar] [CrossRef]
- Engel, G.L. The need for a new medical model: A challenge for biomedicine science. Science 1977, 196, 129–136. [Google Scholar] [CrossRef] [PubMed]
- Wong, R.M.; Ng, S.K.; Corbet, E.F.; Keung, L.W. Non-surgical periodontal therapy improves oral health-related quality of life. J. Clin. Periodontol. 2012, 39, 53–61. [Google Scholar] [CrossRef] [PubMed]
- Needleman, I.; McGrath, C.; Floyd, P.; Biddle, A. Impact of oral health on the life quality of periodontal patients. J. Clin. Periodontol. 2004, 31, 454–457. [Google Scholar] [CrossRef] [PubMed]
- Ng, S.K.; Leung, W.K. Oral health-related quality of life and periodontal status. Community Dent. Oral Epidimiol. 2006, 34, 14–122. [Google Scholar] [CrossRef]
- Cunha-Cruz, J.; Hujoel, P.P.; Kressin, N.R. Oral health-related quality of life of periodontal patients. J. Periodontal Res. 2007, 42, 169–176. [Google Scholar] [CrossRef]
- Aslund, M.; Pjetursson, B.E.; Lang, N.P. Measuring oral health-related quality-of-life using OHQoL-GE in periodontal patients presenting at the University of Bern, Switzerland. Oral Health Prev. Dent. 2008, 6, 191–197. [Google Scholar]
- Patel, R.R.; Richards, P.S.; Inglehart, M.R. Periodontal health, quality of life, and smiling patterns-an exploration. J. Periodontol. 2008, 79, 224–231. [Google Scholar] [CrossRef]
- Shanbhag, S.; Dahiya, M.; Croucher, R. The impact of periodontal therapy on oral health-related quality of life in adults: A systematic review. J. Clin. Periodontol. 2012, 39, 725–735. [Google Scholar] [CrossRef] [PubMed]
- Lawrence, H.P.; Thomson, W.M.; Broadbent, J.M.; Poulton, R. Oral health-related quality of life in a birth cohort of 32-year olds. Community Dent Oral Epidemiol 2008, 36, 305–316. [Google Scholar] [CrossRef] [PubMed]
- Karlsson, E.; Lymer, U.B.; Hakeberg, M. Periodontitis from the patient’s perspective, a qualitative study. Int. J. Dent. Hyg. 2009, 7, 23–30. [Google Scholar] [CrossRef] [PubMed]
- Araujo, E.; Gusmao, E.S.; Batista, J.E.; Cimoes, R. Impact of Periodontal disease on quality of life. Quintessesnce Int. 2010, 41, 111–118. [Google Scholar]
- Borges, T.F.; Regalo, S.C.; Taba, M.; Siessere, S.; Mestriner, W., Jr.; Semprini, M. Changes in masticatory performance and quality of life in individuals with chronic periodontitis. J. Periodontol. 2013, 84, 325–331. [Google Scholar] [CrossRef]
- Jansson, H.; Wahlin, A.; Johansson, V. Impact of periodontal disease experience on oral health-related quality of life. J. Periodontol. 2014, 85, 438–445. [Google Scholar] [CrossRef]
- Tsakos, G.; Guarnizo-Herreno, C.C.; O’Connor, R.; Wildman, J.; Steele, J.G.; Allen, P.F. Explaining time changes in oral health-related quality of life in England: A decomposition analysis. J. Epidemiol. Community Health 2017, 71, 1203–1209. [Google Scholar] [CrossRef]
- Jowett, A.K.; Orr, M.T.; Rawlinson, A.; Robinson, P.G. Psychosocial impact of periodontal disease and its treatment with 24-h root surface debridement. J. Clin. Periodontol. 2009, 36, 413–418. [Google Scholar] [CrossRef]
- Saito, A.; Hosaka, Y.; Kikuchi, M.; Akamatsu, M.; Fukaya, C.; Matsumoto, S.; Ueshima, F.; Hayakawa, H.; Fujinami, K.; Nakagawa, T. Effect of initial periodontal therapy on oral health-related quality of life in patients with periodontitis in Japan. J. Periodontol. 2010, 81, 1001–1009. [Google Scholar] [CrossRef]
- Tsakos, G.; Bernabe, E.; D’Aiuto, F.; Pikhart, H.; Tonetti, M.; Sheiham, A.; Donos, N. Assessing the minimally important difference in the Oral Impact on Daily Performances Index in patients treated for periodontitis. J. Clin. Periodontol. 2010, 37, 903–909. [Google Scholar] [CrossRef]
- Nagarajan, S.; Chandra, R.V. Perception of oral health related quality of life (OHQoL-UK) among periodontal risk patients before and after periodontal therapy. Community Dent. Health 2012, 29, 90–94. [Google Scholar] [PubMed]
- Wong, M.C.; Liu, J.K.; Lo, E.C. Translation and validation of the Chinese version of GOHAI. J. Public Health Dent. 2002, 62, 78–83. [Google Scholar] [CrossRef] [PubMed]
- Brauchle, F.; Noack, M.; Reich, E. Impact of periodontal disease and periodontal therapy on the oral health -related quality of life. Int. Dent. J. 2013, 63, 306–311. [Google Scholar] [CrossRef] [PubMed]
- Jonsson, B.; Ohrn, K. Evaluation of the effect of non-surgical periodontal treatment on oral health related quality of life: Estimation of minimal important differences 1 year after treatment. J. Clin. Periodontol. 2014, 41, 275–282. [Google Scholar] [CrossRef] [PubMed]
- Santuchi, C.C.; Cortelli, J.R.; Cortelli, S.C.; Cota, L.O.; Fonseca, D.C.; Alencar, C.O.; Costa, F.O. Scaling and root planing per Quadrant versus one stage full mouth disinfection: Assessment of the impact of chronic periodontitis treatment on quality of life. A clinical Randomized controlled trial. J. Periodontol. 2016, 87, 114–123. [Google Scholar] [CrossRef]
- Ozcelik, O.; Haytac, M.C.; Seydaoglu, G. Immediate post-operative effects of different periodontal treatment modalities on oral health-related quality of life: A randomizes clinical trial. J. Clin. Periodontol. 2007, 34, 788–796. [Google Scholar] [CrossRef]
- Saito, A.; Ota, K.; Hosaka, Y.; Akamatsu, M.; Hayakawa, H.; Fukaya, C.; Ida, A.; Fujinami, K.; Sugito, H.; Nakagawa, T. Potential impact of surgical periodontal therapy on oral health related quality of life in patients with periodontitis: A pilot study. J. Clin. Periodontol. 2011, 38, 1115–1121. [Google Scholar] [CrossRef]
- Makino-Oi, A.; Ishii, Y.; Hoshino, T.; Okubo, N.; Sugito, H.; Hosaka, Y.; Fukaya, C.; Nakagawa, T.; Saito, A. Effect of periodontal surgery on oral health related quality of life in patients who have completed initial periodontal therapy. J. Periodontal Res. 2016, 51, 212–220. [Google Scholar] [CrossRef]
- Chou, Y.H.; Yang, Y.H.; Kuo, H.C. Periodontal surgery improves oral health-related quality of life in chronic periodontitis patients in Asian population. Kaohsiung J. Med. Sci. 2017, 33, 523–529. [Google Scholar] [CrossRef]
- Slade, G.D. Derivation and validation of a short-form oral heath impact profile. Community Dent. Oral Epidimiol. 1997, 25, 284–290. [Google Scholar] [CrossRef]
- Armitage, G.C. Development of a classification system for periodontal diseases and conditions. Ann. Periodontol. 1999, 4, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Armitage, G.C. Periodontal diagnoses and classification of periodontal diseases. Periodontol. 2000 2004, 34, 9–21. [Google Scholar] [CrossRef] [PubMed]
- Ainamo, J.; Bay, I. Problems and proposals for recording gingivitis and plaque. Int. Dent. J. 1975, 25, 229–235. [Google Scholar] [PubMed]
- O’Leary, T.; Drake, R.; Naylor, J.E. The plaque control record. J. Periodontol. 1972, 43, 38–39. [Google Scholar] [CrossRef] [PubMed]
- Slade, G.D.; Strauss, R.P.; Atchison, K.A.; Kressin, N.R.; Locker, D.; Reisine, S.T. Conference summary: Assessing oral health outcomes-measuring health status and quality of life. Community Dent. Health 1998, 15, 3–7. [Google Scholar]
- Mastrogeorgopoulou, C.; Anastassiadou, V. The contribution of the Greek version of OHIP-14 in cross-cultural adaptation. Stoma 2011, 39, 183–188. [Google Scholar]
- Papagiannopoulou, V.; Oulis, C.J.; Papaioannou, W.; Antonogeorgos, G.; Yfantopoulos, J. Validation of a Greek version of the oral health impact profile (OHIP-14) for use among adults. Health Qual. Life Outcomes 2012, 10, 7. [Google Scholar] [CrossRef]
- Locker, D. Issues in measuring change in self-perceived oral health status. Community Dent. Oral Epidimiol. 1998, 26, 41–47. [Google Scholar] [CrossRef]
- Ramfjord, S.P.; Nissle, R.R. The modified Widman flap. J. Periodontol. 1974, 45, 601–607. [Google Scholar] [CrossRef]
- Papaioannou, W.; Oulis, C.J.; Yfantopoulos, J. The oral health related quality of life in different groups of senior citizen as measured by the OHIP-14 questionnaire. Herbert Open Access J. 2015, 3, 4–6. [Google Scholar] [CrossRef]
- Mehta, C.; Patel, R. SPSS Exact Tests 7.0 for Windows; SPSS Inc.: Chicago, IL, USA, 1996; pp. 135–140. [Google Scholar]
- Lindhe, J.; Westfelt, E.; Nyman, S.; Socransky, S.S.; Haffajee, A.D. Long-term effect of surgical/non-surgical treatment of periodontal disease. J. Clin. Periodontol. 1984, 11, 448–458. [Google Scholar] [CrossRef] [PubMed]
- Ramfjord, S.; Caffesse, R.; Morrison, E.; Hill, R.W.; Kerry, G.J.; Appleberry, E.A.; Nissle, R.R.; Stults, D. Four modalities of periodontal treatment compared over 5 years. J. Clin. Periodontol. 1987, 14, 445–452. [Google Scholar] [CrossRef] [PubMed]
- Isidor, F.; Karring, T. Long-term effect of surgical and nonsurgical periodontal treatment. A 5 year clinical study. J. Periodontal Res. 1986, 21, 462–472. [Google Scholar] [CrossRef] [PubMed]
- Kaldahl, W.B.; Kalkwarf, K.L.; Patil, K.D.; Molvar, M.P.; Dyer, J.K. Long-Term Evaluation of Periodontal Therapy: I. Response to 4 Therapeutic Modalities. J. Periodontol. 1996, 67, 93–102. [Google Scholar] [CrossRef] [PubMed]
- Sischo, L.; Broder, H.L. Oral health-related quality of life: What, why, how, and future implications. J. Dent. Res. 2011, 90, 1264–1270. [Google Scholar] [CrossRef]
- Hodacová, L.; Smejkalová, J.; Cermáková, E.; Slezák, R.; Jacob, V.; Hlavácková, E. Oral health-related quality of life in Czech population. Cent. Eur. J. Public Health 2010, 18, 76–80. [Google Scholar] [CrossRef]
- Tonetti, M.S.; D’Aiuto, F.; Nibali, L.; Donald, A.; Storry, C.; Parkar, M.; Suvan, J.; Hingorani, A.D.; Vallance, P.; Deanfield, J. Treatment of periodontitis and endothelial function. N. Engl. J. Med. 2007, 356, 911–920. [Google Scholar] [CrossRef]
- Isola, G.; Polizzi, A.; Alibrandi, A.; Indelicato, F.; Ferlito, S. Analysis of Endothelin-1 Concentrations in Individuals with Periodontitis. Sci. Rep. 2020, 10, 1652. [Google Scholar] [CrossRef]
- Isola, G.; Alibrandi, A.; Rapisarda, E.; Matarese, G.; Williams, R.C.; Leonardi, R. Association of vitamin D in patients with periodontitis: A cross-sectional study. J. Periodontal Res. 2020. [CrossRef]
- Isola, G.; Alibrandi, A.; Currò, M.; Matarese, M.; Ricca, S.; Matarese, G.; Ientile, R.; Kocher, T. Evaluation of salivary and serum ADMA levels in patients with periodontal and cardiovascular disease as subclinical marker of cardiovascular risk. J. Periodontol. 2020. [Google Scholar] [CrossRef]
| Demographic | Count (%) |
|---|---|
| Gender | |
| Male | 27 (36%) |
| Female | 48 (64%) |
| Marital Status | |
| Never married | 13 (17.3%) |
| Married | 50 (66.7%) |
| Separated/divorced | 7 (9.3%) |
| Widowed | 5 (6.7%) |
| Education status | |
| Primary | 7 (9.3%) |
| Secondary | 16 (21.3%) |
| Tertiary (non-degree) | 28 (37.3%) |
| University degree | 23 (30.7%) |
| Student | 1 (1.3%) |
| Family income (Euro/year) | |
| <6.000 EUR | 13 (17.3%) |
| 6.000–11.999 EUR | 23 (30.3%) |
| 12.000–17.999 EUR | 19 (25.3%) |
| 18.000–23.999 EUR | 1 (1.3%) |
| >24.000 EUR | 1 (1.3%) |
| Smoking (<10 cigarettes) | |
| Yes | 35 (46.7%) |
| No | 40 (53.3%) |
| Systemic disease | |
| Yes | 34 (45.3%) |
| No | 41 (54.7%) |
| Daily use of toothbrush | |
| Yes | 60 (80%) |
| No | 15 (20%) |
| Daily use of interdental cleaning methods | |
| Yes | 32 (42.7%) |
| No | 43 (57.3%) |
| Frequency of prophylaxis visits yearly | |
| None | 28 (37.3%) |
| Once | 30 (40%) |
| Twice | 12 (16%) |
| More | 5 (6.7%) |
| Total | 75 (100%) |
| Min | Median | Max | Mean * | SD ** | N | |
|---|---|---|---|---|---|---|
| Total score t0 | 0 | 16 | 40 | 16.33 a | 7.91 | 75 |
| Total score t1 | 3 | 11 | 35 | 11.96 b | 5.89 | 75 |
| Total score t2 | 1 | 11 | 27 | 11.06 b | 5.48 | 31 |
| OHIP-14 | Min | Median | Max | Mean * | SD ** | N | |
| Functional limitation | F1 (t0) | 0 | 2 | 8 | 2.7 a | 2.2 | 75 |
| F1 (t1) | 0 | 2 | 7 | 1.6 b | 1.4 | 75 | |
| F1 (t2) | 0 | 1 | 7 | 1.5 b | 1.7 | 31 | |
| Physical pain | F2 (t0) | 0 | 3 | 8 | 3.6 a | 2.0 | 75 |
| F2 (t1) | 0 | 2 | 7 | 2.5 b | 1.5 | 75 | |
| F2 (t2) | 0 | 2 | 5 | 2.2 b | 1.2 | 31 | |
| psychological discomfort | F3 (t0) | 0 | 1 | 7 | 1.7 a | 1.9 | 75 |
| F3 (t1) | 0 | 1 | 4 | 1.0 b | 1.1 | 75 | |
| F3 (t2) | 0 | 1 | 4 | 1.0 b | 1.1 | 31 | |
| Physical disability | F4 (t0) | 0 | 3 | 7 | 2.7 a | 1.8 | 75 |
| F4 (t1) | 0 | 2 | 5 | 2.1 b | 1.5 | 75 | |
| F4 (t2) | 0 | 1 | 7 | 1.8 b | 1.8 | 31 | |
| Psychological disability | F5 (t0) | 0 | 2 | 8 | 2.2 a | 1.9 | 75 |
| F5 (t1) | 0 | 1 | 7 | 1.3 b | 1.4 | 75 | |
| F5 (t2) | 0 | 1 | 4 | 1.3 b | 1.0 | 31 | |
| Social disability | F6 (t0) | 0 | 0 | 6 | 0.9 a | 1.9 | 75 |
| F6 (t1) | 0 | 0 | 4 | 0.7 a | 1.4 | 75 | |
| F6 (t2) | 0 | 0 | 2 | 0.5 a | 1.0 | 31 | |
| Handicap | F7 (t0) | 0 | 2 | 7 | 2.3 a | 1.7 | 75 |
| F7 (t1) | 0 | 1 | 7 | 1.6 b | 1.4 | 75 | |
| F7 (t2) | 0 | 1 | 6 | 1.3 b | 1.4 | 31 |
| Min | Median | Max | Mean* | SD ** | N | |
|---|---|---|---|---|---|---|
| PD (t0) | 0.044 | 0.317 | 0.887 | 0.364 a | 0.218 | 75 |
| PD (t1) | 0.007 | 0.130 | 0.607 | 0.184 b | 0.142 | 75 |
| PD (t2) | 0.000 | 0.097 | 0.413 | 0.121 c | 0.100 | 31 |
| PI (t0) | 0.154 | 0.500 | 1.000 | 0.560 a | 0.243 | 75 |
| PI (t1) | 0.047 | 0.219 | 0.535 | 0.229 b | 0.108 | 75 |
| PI (t2) | 0.060 | 0.121 | 0.296 | 0.135 c | 0.057 | 31 |
| BOP (t0) | 0.106 | 0.593 | 1.000 | 0.606 a | 0.230 | 75 |
| BOP (t1) | 0.061 | 0.237 | 0.675 | 0.241 b | 0.122 | 75 |
| BOP (t2) | 0.040 | 0.115 | 0.333 | 0.136 c | 0.075 | 31 |
| Base Line (t0) | Phase I (t1) | Phase II (t2) | |
|---|---|---|---|
| PD (t0) | PD (t1) | PD (t2) | |
| Total OHIP-14 score at t0 | rho = 0.167, p = 0.153 | rho = 0.048, p = 0.685 | rho = 0.210, p = 0.256 |
| PI (t0) | PI (t1) | PI (t0) | |
| Total OHIP-14 score at t1 | rho = 0.028, p = 0.808 | rho = 0.091, p = 0.437 | rho = 0.095, p = 0.611 |
| BOP (t0) | BOP (t1) | BOP (t2) | |
| Total OHIP-14 score at t2 | rho = 0.145, p = 0.216 | rho = 0.141, p = 0.227 | rho = 0.146, p = 0.434 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Theodoridis, C.; Violesti, A.; Nikiforidou, M.; Menexes, G.C.; Vouros, I.D. Short-Term Impact of Non-Surgical and Surgical Periodontal Therapy on Oral Health-Related Quality of Life in a Greek Population—A Prospective Cohort Study. Dent. J. 2020, 8, 54. https://doi.org/10.3390/dj8020054
Theodoridis C, Violesti A, Nikiforidou M, Menexes GC, Vouros ID. Short-Term Impact of Non-Surgical and Surgical Periodontal Therapy on Oral Health-Related Quality of Life in a Greek Population—A Prospective Cohort Study. Dentistry Journal. 2020; 8(2):54. https://doi.org/10.3390/dj8020054
Chicago/Turabian StyleTheodoridis, Charis, Anastasia Violesti, Maria Nikiforidou, Georgios C. Menexes, and Ioannis D. Vouros. 2020. "Short-Term Impact of Non-Surgical and Surgical Periodontal Therapy on Oral Health-Related Quality of Life in a Greek Population—A Prospective Cohort Study" Dentistry Journal 8, no. 2: 54. https://doi.org/10.3390/dj8020054
APA StyleTheodoridis, C., Violesti, A., Nikiforidou, M., Menexes, G. C., & Vouros, I. D. (2020). Short-Term Impact of Non-Surgical and Surgical Periodontal Therapy on Oral Health-Related Quality of Life in a Greek Population—A Prospective Cohort Study. Dentistry Journal, 8(2), 54. https://doi.org/10.3390/dj8020054






