Adhesion to Zirconia: A Systematic Review of Current Conditioning Methods and Bonding Materials
Abstract
1. Introduction
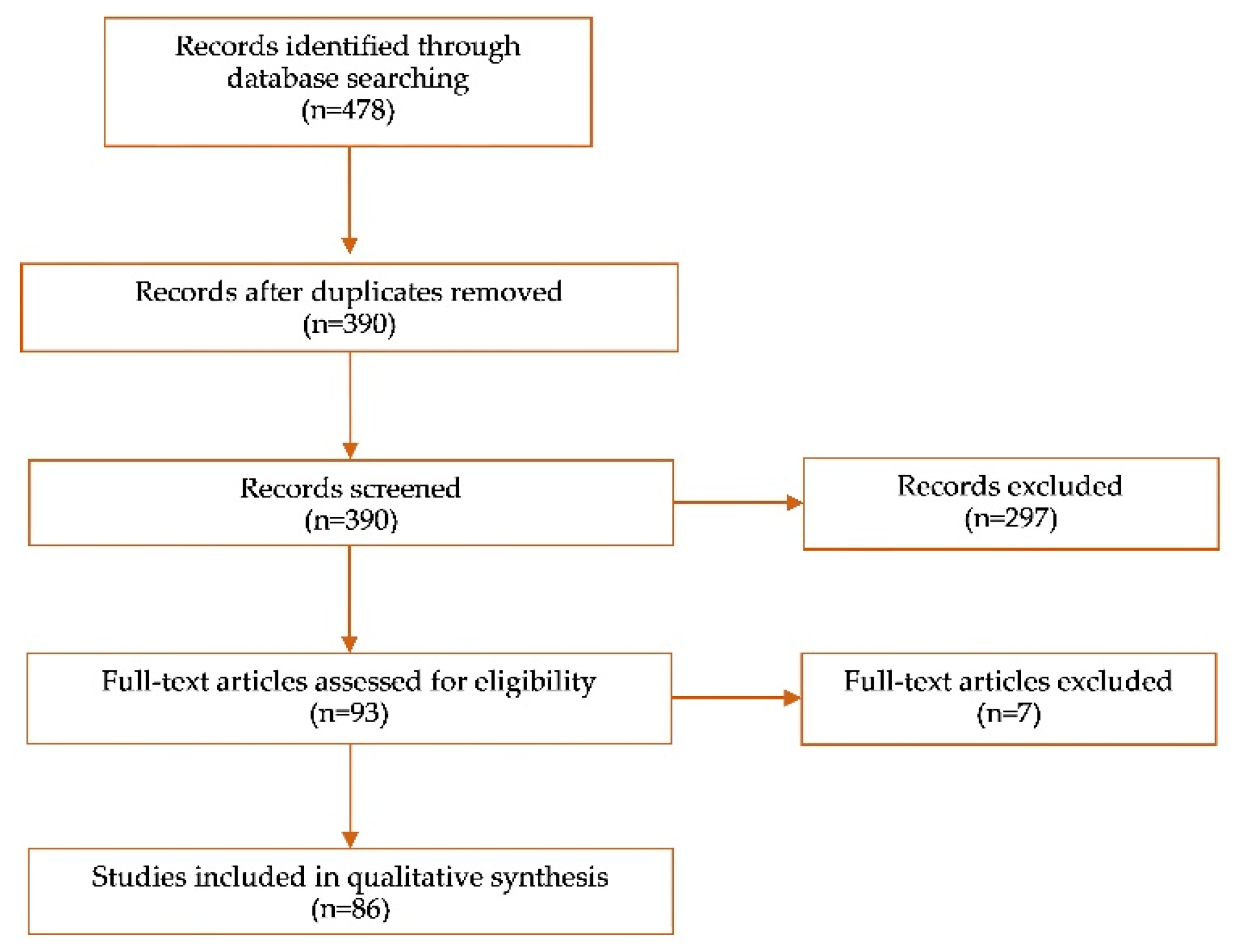
2. Materials and Methods
2.1. Search Strategy
2.2. Eligibility Criteria
3. Results
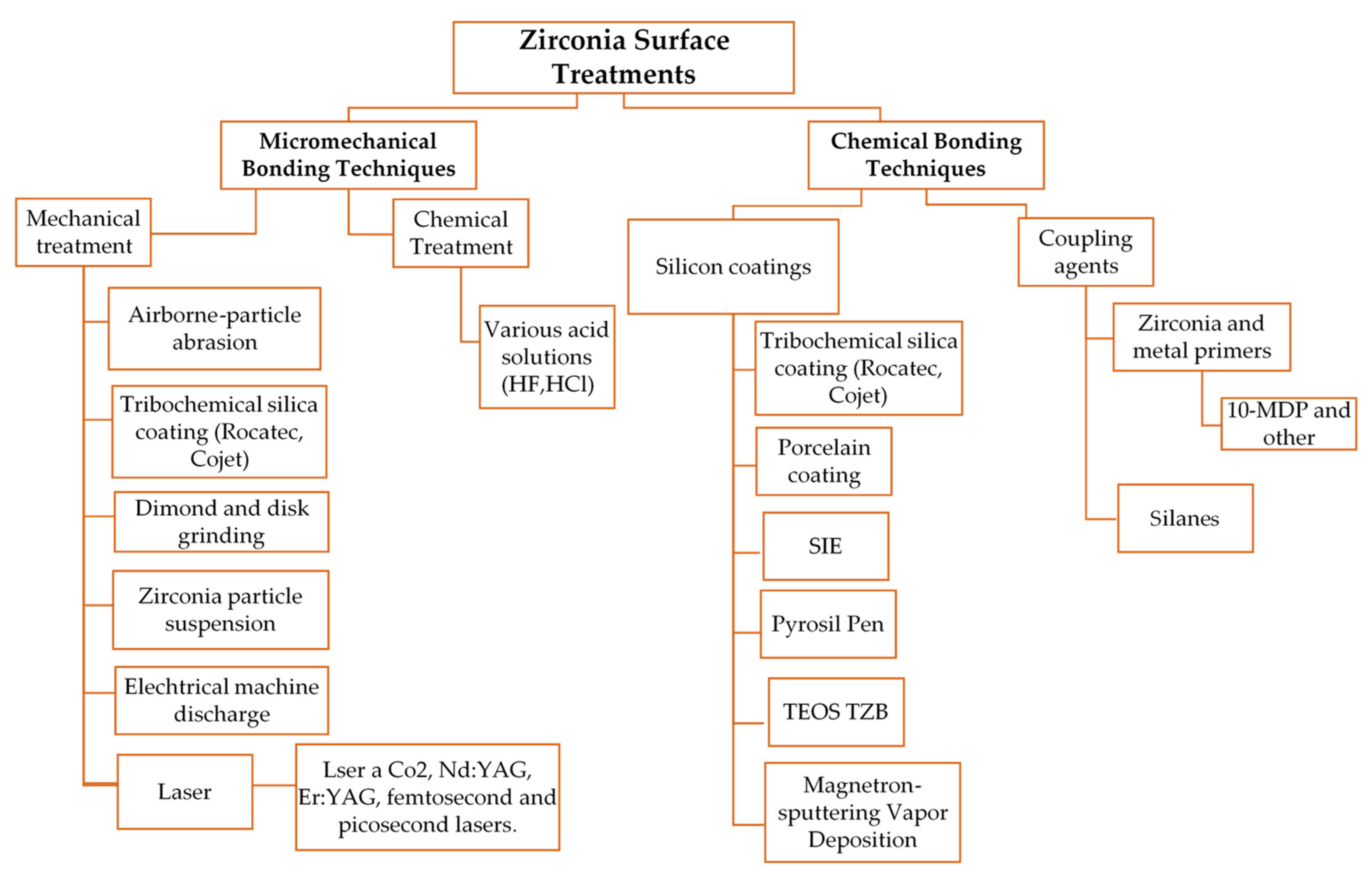
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Colombo, M.; Poggio, C.; Lasagna, A.; Chiesa, M.; Scribante, A. Vickers micro-hardness of new restorative CAD/CAM dental materials: Evaluation and comparison after exposure to acidic drink. Materials (Basel) 2019, 12, 1246. [Google Scholar] [CrossRef] [PubMed]
- Miyazaki, T.; Nakamura, T.; Matsumura, H.; Ban, S.; Kobayashi, T. Current status of zirconia restoration. J. Prosthodont. Res. 2013, 57, 236–261. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Lawn, B.R. Novel Zirconia Materials in Dentistry. J. Dent. Res. 2018, 97, 140–147. [Google Scholar] [CrossRef] [PubMed]
- Shahmiri, R.; Standard, O.C.; Hart, J.N.; Sorrell, C.C. Optical properties of zirconia ceramics for esthetic dental restorations: A systematic review. J. Prosthet. Dent. 2018, 119, 36–46. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Kim, S.H.; Han, J.S.; Yeo, I.L.; Yoon, H.I. Optical and Surface Properties of Monolithic Zirconia after Simulated Toothbrushing. Materials (Basel) 2019, 10, 1158. [Google Scholar] [CrossRef]
- Carrabba, M.; Keeling, A.J.; Aziz, A.; Vichi, A.; Fabian Fonzar, R.; Wood, D. Translucent zirconia in the ceramic scenario for monolithic restorations: A flexural strength and translucency comparison test. J. Dent. 2017, 60, 70–76. [Google Scholar] [CrossRef]
- Ozcan, M.; Bernasconi, M. Adhesion to zirconia used for dental restorations: A systematic review and meta-analysis. J. Adhes Dent. 2015, 17, 7–26. [Google Scholar]
- Tzanakakis, E.G.; Tzoutzas, I.G.; Koidis, P.T. Is there a potential for durable adhesion to zirconia restorations? A systematic review. J. Prosthet. Dent. 2016, 115, 9–19. [Google Scholar] [CrossRef]
- Khan, A.A.; Al Kheraif, A.A.; Jamaluddin, S.; Elsharawy, M.; Divakar, D.D. Recent Trends in Surface Treatment Methods for Bonding Composite Cement to Zirconia: A Reveiw. J. Adhes Dent. 2017, 19, 7–19. [Google Scholar]
- Yang, L.; Xie, H.; Meng, H.; Wu, X.; Chen, Y.; Zhang, H. Effects of Luting Cements and Surface Conditioning on Composite Bonding Performance to Zirconia. J. Adhes Dent. 2018, 20, 549–558. [Google Scholar]
- Thammajaruk, P.; Buranadham, S.; Thanatvarakorn, O.; Ferrari, M.; Guazzato, M. Influence of glass-ceramic coating on composite zirconia bonding and its characterization. Dent. Mater. 2019, 35, 105–113. [Google Scholar] [CrossRef] [PubMed]
- Shimizu, H.; Inokoshi, M.; Takagaki, T.; Uo, M.; Minakuchi, S. Bonding Efficacy of 4-META/MMA-TBB Resin to Surface-treated Highly Translucent Dental Zirconia. J. Adhes Dent. 2018, 20, 453–459. [Google Scholar] [PubMed]
- Piest, C.; Wille, S.; Strunskus, T.; Polonskyi, O.; Kern, M. Efficacy of Plasma Treatment for Decontaminating Zirconia. J. Adhes Dent. 2018, 20, 289–297. [Google Scholar] [PubMed]
- Yang, L.; Chen, B.; Xie, H.; Chen, Y.; Chen, Y.; Chen, C. Durability of Resin Bonding to Zirconia Using Products Containing 10-Methacryloyloxydecyl Dihydrogen Phosphate. J. Adhes Dent. 2018, 20, 279–287. [Google Scholar] [PubMed]
- Moura, D.M.D.; do Nascimento Januario, A.B.; de Araujo, A.M.M.; de Oliveira Dal Piva, A.M.; Ozcan, M.; Bottino, M.A.; Souza, R.O.A. Effect of primer-cement systems with different functional phosphate monomers on the adhesion of zirconia to dentin. J. Mech. Behav. Biomed. Mater. 2018, 88, 69–77. [Google Scholar] [CrossRef] [PubMed]
- Araujo, A.M.M.; Januario, A.; Moura, D.M.D.; Tribst, J.P.M.; Ozcan, M.; Souza, R.O.A. Can the Application of Multi-Mode Adhesive be a Substitute to Silicatized/Silanized Y-TZP Ceramics? Braz. Dent. J. 2018, 29, 275–281. [Google Scholar] [CrossRef] [PubMed]
- Grasel, R.; Santos, M.J.; Rego, H.C.; Rippe, M.P.; Valandro, L.F. Effect of Resin Luting Systems and Alumina Particle Air Abrasion on Bond Strength to Zirconia. Oper. Dent. 2018, 43, 282–290. [Google Scholar] [CrossRef]
- Dos Santos, A.F.; Sandes de Lucena, F.; Sanches Borges, A.F.; Lisboa-Filho, P.N.; Furuse, A.Y. Incorporation of TiO2 nanotubes in a polycrystalline zirconia: Synthesis of nanotubes, surface characterization, and bond strength. J. Prosthet. Dent. 2018, 120, 589–595. [Google Scholar] [CrossRef]
- Dal Piva, A.M.O.; Carvalho, R.L.A.; Lima, A.L.; Bottino, M.A.; Melo, R.M.; Valandro, L.F. Silica coating followed by heat-treatment of MDP-primer for resin bond stability to yttria-stabilized zirconia polycrystals. J. Biomed. Mater. Res. B Appl. Biomater. 2019, 107, 104–111. [Google Scholar] [CrossRef]
- Yoshida, K. Influence of cleaning methods on resin bonding to saliva-contaminated zirconia. J. Esthet. Restor. Dent. 2018, 30, 259–264. [Google Scholar] [CrossRef]
- Wille, S.; Lehmann, F.; Kern, M. Durability of Resin Bonding to Lithium Disilicate and Zirconia Ceramic using a Self-etching Primer. J. Adhes Dent. 2017, 19, 491–496. [Google Scholar]
- Xie, H.; Cheng, Y.; Chen, Y.; Qian, M.; Xia, Y.; Chen, C. Improvement in the Bonding of Y-TZP by Room-temperature Ultrasonic HF Etching. J. Adhes Dent. 2017, 19, 425–433. [Google Scholar]
- Pitta, J.; Branco, T.C.; Portugal, J. Effect of saliva contamination and artificial aging on different primer/cement systems bonded to zirconia. J. Prosthet. Dent. 2018, 119, 833–839. [Google Scholar] [CrossRef]
- Yagawa, S.; Komine, F.; Fushiki, R.; Kubochi, K.; Kimura, F.; Matsumura, H. Effect of priming agents on shear bond strengths of resin-based luting agents to a translucent zirconia material. J. Prosthodont. Res. 2018, 62, 204–209. [Google Scholar] [CrossRef]
- Noda, Y.; Nakajima, M.; Takahashi, M.; Mamanee, T.; Hosaka, K.; Takagaki, T.; Ikeda, M.; Foxton, R.M.; Tagami, J. The effect of five kinds of surface treatment agents on the bond strength to various ceramics with thermocycle aging. Dent. Mater. J. 2017, 36, 755–761. [Google Scholar] [CrossRef]
- Chuang, S.F.; Kang, L.L.; Liu, Y.C.; Lin, J.C.; Wang, C.C.; Chen, H.M.; Tai, C.K. Effects of silane- and MDP-based primers application orders on zirconia-resin adhesion-A ToF-SIMS study. Dent. Mater. 2017, 33, 923–933. [Google Scholar] [CrossRef]
- Elsayed, A.; Younes, F.; Lehmann, F.; Kern, M. Tensile Bond Strength of So-called Universal Primers and Universal Multimode Adhesives to Zirconia and Lithium Disilicate Ceramics. J. Adhes Dent. 2017, 19, 221–228. [Google Scholar]
- Galvao Ribeiro, B.R.; Galvao Rabelo Caldas, M.R.; Almeida, A.A.; Fonseca, R.G.; Adabo, G.L. Effect of surface treatments on repair with composite resin of a partially monoclinic phase transformed yttrium-stabilized tetragonal zirconia. J. Prosthet. Dent. 2018, 119, 286–291. [Google Scholar] [CrossRef]
- Chen, C.; Chen, Y.; Lu, Z.; Qian, M.; Xie, H.; Tay, F.R. The effects of water on degradation of the zirconia-resin bond. J. Dent. 2017, 64, 23–29. [Google Scholar] [CrossRef]
- Tsujimoto, A.; Barkmeier, W.W.; Takamizawa, T.; Wilwerding, T.M.; Latta, M.A.; Miyazaki, M. Interfacial Characteristics and Bond Durability of Universal Adhesive to Various Substrates. Oper. Dent. 2017, 42, e59–e70. [Google Scholar] [CrossRef]
- Sakrana, A.A.; Ozcan, M. Effect of chemical etching solutions versus air abrasion on the adhesion of self-adhesive resin cement to IPS e.max ZirCAD with and without aging. Int. J. Esthet. Dent. 2017, 12, 72–85. [Google Scholar]
- Akazawa, N.; Koizumi, H.; Nogawa, H.; Nakayama, D.; Kodaira, A.; Matsumura, H. Effect of mechanochemical surface preparation on bonding to zirconia of a tri-n-butylborane initiated resin. Dent. Mater. J. 2017, 36, 19–26. [Google Scholar] [CrossRef]
- Wandscher, V.F.; Fraga, S.; Pozzobon, J.L.; Soares, F.Z.; Foletto, E.L.; May, L.G.; Valandro, L.F. Tribochemical Glass Ceramic Coating as a New Approach for Resin Adhesion to Zirconia. J. Adhes Dent. 2016, 18, 435–440. [Google Scholar]
- Esteves-Oliveira, M.; Jansen, P.; Wehner, M.; Dohrn, A.; Bello-Silva, M.S.; Eduardo, C.P.; Meyer-Lueckel, H. Surface Characterization and Short-term Adhesion to Zirconia after Ultra-short Pulsed Laser Irradiation. J. Adhes Dent. 2016, 18, 483–492. [Google Scholar]
- Rona, N.; Yenisey, M.; Kucukturk, G.; Gurun, H.; Cogun, C.; Esen, Z. Effect of electrical discharge machining on dental Y-TZP ceramic-resin bonding. J. Prosthodont. Res. 2017, 6, 158–167. [Google Scholar] [CrossRef]
- Sawada, T.; Spintzyk, S.; Schille, C.; Zöldföldi, J.; Paterakis, A.; Schweizer, E.; Ingrid, S.; Frank, R.; Jurgen, G.G. Influence of Pre-Sintered Zirconia Surface Conditioning on Shear Bond Strength to Resin Cement. Materials (Basel) 2016, 9, 518. [Google Scholar] [CrossRef]
- Zhao, L.; Jian, Y.T.; Wang, X.D.; Zhao, K. Bond strength of primer/cement systems to zirconia subjected to artificial aging. J. Prosthet. Dent. 2016, 116, 790–796. [Google Scholar] [CrossRef]
- Iwasaki, T.; Komine, F.; Fushiki, R.; Kubochi, K.; Shinohara, M.; Matsumura, H. Shear bond strengths of an indirect composite layering material to a tribochemically silica-coated zirconia framework material. Dent. Mater. J. 2016, 35, 461–469. [Google Scholar] [CrossRef]
- Passia, N.; Mitsias, M.; Lehmann, F.; Kern, M. Bond strength of a new generation of universal bonding systems to zirconia ceramic. J. Mech. Behav. Biomed. Mater. 2016, 62, 268–274. [Google Scholar] [CrossRef]
- Lopes, G.C.; Spohr, A.M.; De Souza, G.M. Different Strategies to Bond Bis-GMA-based Resin Cement to Zirconia. J. Adhes Dent. 2016, 18, 239–246. [Google Scholar]
- Salem, R.; Naggar, G.E.; Aboushelib, M.; Selim, D. Microtensile Bond Strength of Resin-bonded Hightranslucency Zirconia Using Different Surface Treatments. J. Adhes Dent. 2016, 18, 191–196. [Google Scholar]
- Hallmann, L.; Ulmer, P.; Lehmann, F.; Wille, S.; Polonskyi, O.; Johannes, M.; Köbel, S.; Trottenberg, T.; Bornholdt, S.; Haase, F.; et al. Effect of surface modifications on the bond strength of zirconia ceramic with resin cement resin. Dent. Mater. 2016, 32, 631–639. [Google Scholar] [CrossRef] [PubMed]
- Angkasith, P.; Burgess, J.O.; Bottino, M.C.; Lawson, N.C. Cleaning Methods for Zirconia Following Salivary Contamination. J. Prosthodont 2016, 25, 375–379. [Google Scholar] [CrossRef] [PubMed]
- Bomicke, W.; Schurz, A.; Krisam, J.; Rammelsberg, P.; Rues, S. Durability of Resin-Zirconia Bonds Produced Using Methods Available in Dental Practice. J. Adhes Dent. 2018, 18, 17–27. [Google Scholar]
- Xie, H.; Li, Q.; Zhang, F.; Lu, Y.; Tay, F.R.; Qian, M.; Chen, C. Comparison of resin bonding improvements to zirconia between one-bottle universal adhesives and tribochemical silica coating, which is better? Dent. Mater. 2016, 32, 403–411. [Google Scholar] [CrossRef] [PubMed]
- Cheung, G.J.; Botelho, M.G. Zirconia Surface Treatments for Resin Bonding. J. Adhes Dent. 2015, 17, 551–558. [Google Scholar]
- Ahn, J.S.; Yi, Y.A.; Lee, Y.; Seo, D.G. Shear Bond Strength of MDP-Containing Self-Adhesive Resin Cement and Y-TZP Ceramics: Effect of Phosphate Monomer-Containing Primers. Biomed. Res. Int. 2015. [Google Scholar] [CrossRef] [PubMed]
- Alves, M.; Campos, F.; Bergoli, C.D.; Bottino, M.A.; Ozcan, M.; Souza, R. Effect of Adhesive Cementation Strategies on the Bonding of Y-TZP to Human Dentin. Oper. Dent. 2016, 41, 276–283. [Google Scholar] [CrossRef]
- Yenisey, M.; Dede, D.O.; Rona, N. Effect of surface treatments on the bond strength between resin cement and differently sintered zirconium-oxide ceramics. J. Prosthodont. Res. 2016, 60, 36–46. [Google Scholar] [CrossRef]
- Pereira Lde, L.; Campos, F.; Dal Piva, A.M.; Gondim, L.D.; Souza, R.O.; Ozcan, M. Can application of universal primers alone be a substitute for airborne-particle abrasion to improve adhesion of resin cement to zirconia? J. Adhes Dent. 2015, 17, 169–174. [Google Scholar]
- Kim, D.H.; Son, J.S.; Jeong, S.H.; Kim, Y.K.; Kim, K.H.; Kwon, T.Y. Efficacy of various cleaning solutions on saliva-contaminated zirconia for improved resin bonding. J. Adv. Prosthodont. 2015, 7, 85–92. [Google Scholar] [CrossRef] [PubMed]
- Liu, D.; Tsoi, J.K.; Matinlinna, J.P.; Wong, H.M. Effects of some chemical surface modifications on resin zirconia adhesion. J. Mech. Behav. Biomed. Mater. 2015, 46, 23–30. [Google Scholar] [CrossRef]
- Ishii, R.; Tsujimoto, A.; Takamizawa, T.; Tsubota, K.; Suzuki, T.; Shimamura, Y.; Miyazaki, M. Influence of surface treatment of contaminated zirconia on surface free energy and resin cement bonding. Dent. Mater. J. 2015, 34, 91–97. [Google Scholar] [CrossRef]
- Jiang, T.; Chen, C.; Lv, P. Selective infiltrated etching to surface treat zirconia using a modified glass agent. Adhes Dent. 2014, 16, 553–557. [Google Scholar]
- Oliveira-Ogliari, A.; Collares, F.M.; Feitosa, V.P.; Sauro, S.; Ogliari, F.A.; Moraes, R.R. Methacrylate bonding to zirconia by in situ silica nanoparticle surface deposition. Dent. Mater. 2015, 31, 68–76. [Google Scholar] [CrossRef] [PubMed]
- Lung, C.Y.; Liu, D.; Matinlinna, J.P. Silica coating of zirconia by silicon nitride hydrolysis on adhesion promotion of resin to zirconia. Mater. Sci. Eng. C Mater. Biol. Appl. 2015, 46, 103–110. [Google Scholar] [CrossRef] [PubMed]
- Sciasci, P.; Abi-Rached, F.O.; Adabo, G.L.; Baldissara, P.; Fonseca, R.G. Effect of surface treatments on the shear bond strength of luting cements to Y-TZP ceramic. J. Prosthet. Dent. 2015, 113, 212–219. [Google Scholar] [CrossRef] [PubMed]
- Qeblawi, D.M.; Campillo-Funollet, M.; Munoz, C.A. In vitro shear bond strength of two self-adhesive resin cements to zirconia. J Prosthet. Dent. 2015, 113, 122–127. [Google Scholar] [CrossRef]
- Feitosa, S.A.; Patel, D.; Borges, A.L.; Alshehri, E.Z.; Bottino, M.A.; Ozcan, M.; Valandro, L.F.; Bottino, M.C. Effect of cleansing methods on saliva-contaminated zirconia--an evaluation of resin bond durability. Oper. Dent. 2015, 40, 163–171. [Google Scholar] [CrossRef]
- Yi, Y.A.; Ahn, J.S.; Park, Y.J.; Jun, S.H.; Lee, I.B.; Cho, B.H.; Son, H.H.; Seo, D.G. The effect of sandblasting and different primers on shear bond strength between yttria-tetragonal zirconia polycrystal ceramic and a self-adhesive resin cement. Oper. Dent. 2015, 40, 63–71. [Google Scholar] [CrossRef]
- Kim, J.H.; Chae, S.Y.; Lee, Y.; Han, G.J.; Cho, B.H. Effects of multipurpose, universal adhesives on resin bonding to zirconia ceramic. Oper. Dent. 2015, 40, 55–62. [Google Scholar] [CrossRef] [PubMed]
- Klosa, K.; Warnecke, H.; Kern, M. Effectiveness of protecting a zirconia bonding surface against contaminations using a newly developed protective lacquer. Dent. Mater. 2014, 30, 785–792. [Google Scholar] [CrossRef] [PubMed]
- Druck, C.C.; Pozzobon, J.L.; Callegari, G.L.; Dorneles, L.S.; Valandro, L.F. Adhesion to Y-TZP ceramic: Study of silica nanofilm coating on the surface of Y-TZP. J. Biomed. Mater. Res. B Appl. Biomater. 2015, 103, 143–150. [Google Scholar] [CrossRef] [PubMed]
- De Souza, G.; Hennig, D.; Aggarwal, A.; Tam, L.E. The use of MDP-based materials for bonding to zirconia. J. Prosthet. Dent. 2014, 112, 895–902. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Xie, H.; Song, X.; Burrow, M.F.; Chen, G.; Zhang, F. Evaluation of a commercial primer for bonding of zirconia to two different resin composite cements. J. Adhes Dent. 2014, 16, 169–176. [Google Scholar] [PubMed]
- Shin, Y.J.; Shin, Y.; Yi, Y.A.; Kim, J.; Lee, I.B.; Cho, B.H.; Son, H.H.; Seo, D.G. Evaluation of the shear bond strength of resin cement to Y-TZP ceramic after different surface treatments. Scanning 2014, 36, 479–486. [Google Scholar] [CrossRef] [PubMed]
- Da Silva, E.M.; Miragaya, L.; Sabrosa, C.E.; Maia, L.C. Stability of the bond between two resin cements and an yttria-stabilized zirconia ceramic after six months of aging in water. J. Prosthet. Dent. 2014, 112, 568–575. [Google Scholar] [CrossRef]
- Oba, Y.; Koizumi, H.; Nakayama, D.; Ishii, T.; Akazawa, N.; Matsumura, H. Effect of silane and phosphate primers on the adhesive performance of a tri-n-butylborane initiated luting agent bonded to zirconia. Dent. Mater. J. 2014, 33, 226–232. [Google Scholar] [CrossRef]
- Liu, D.; Pow, E.H.N.; Tsoi, J.K.; Matinlinna, J.P. Evaluation of four surface coating treatments for resin to zirconia bonding. J. Mech. Behav. Biomed. Mater. 2014, 32, 300–309. [Google Scholar] [CrossRef]
- Erdem, A.; Akar, G.C.; Erdem, A.; Kose, T. Effects of different surface treatments on bond strength between resin cements and zirconia ceramics. Oper. Dent. 2014, 39, E118–E127. [Google Scholar] [CrossRef]
- Xie, H.; Chen, C.; Dai, W.; Chen, G.; Zhang, F. In vitro short-term bonding performance of zirconia treated with hot acid etching and primer conditioning etching and primer conditioning. Dent. Mater. J. 2013, 32, 928–938. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.; Song, X.; Chen, Y.; Zhu, Q.; Zhang, W. Effect of Er:YAG laser irradiation on bonding property of zirconia ceramics to resin cement. Photomed. Laser Surg. 2013, 31, 619–625. [Google Scholar] [CrossRef] [PubMed]
- Turker, S.B.; Ozcan, M.; Mandali, G.; Damla, I.; Bugurman, B.; Valandro, L.F. Bond strength and stability of 3 luting systems on a zirconia-dentin complex. Gen. Dent. 2013, 61, e10–e13. [Google Scholar] [PubMed]
- Cheung, G.C.; Botelho, M.G.; Matinlinna, J.P. Effect of surface treatments of zirconia ceramics on the bond strength to resin cement. J. Adhes Dent. 2014, 16, 49–56. [Google Scholar] [PubMed]
- Keul, C.; Liebermann, A.; Roos, M.; Uhrenbacher, J.; Stawarczyk, B.; Ing, D. The effect of ceramic primer on shear bond strength of resin composite cement to zirconia: A function of water storage and thermal cycling. J. Am. Dent. Assoc. 2013, 144, 1261–1271. [Google Scholar] [CrossRef]
- Sarmento, H.R.; Campos, F.; Sousa, R.S.; Machado, J.P.; Souza, R.O.; Bottino, M.A.; Ozcan, M. Influence of air-particle deposition protocols on the surface topography and adhesion of resin cement to zirconia. Acta Odontol. Scand. 2014, 72, 346–453. [Google Scholar] [CrossRef]
- Heikkinen, T.T.; Matinlinna, J.P.; Vallittu, P.K.; Lassila, L.V. Long term water storage deteriorates bonding of composite resin to alumina and zirconia short communication. Open. Dent. J. 2013, 7, 123–125. [Google Scholar] [CrossRef]
- Bottino, M.A.; Bergoli, C.; Lima, E.G.; Marocho, S.M.; Souza, R.O.; Valandro, L.F. Bonding of Y-TZP to dentin: Effects of Y-TZP surface conditioning, resin cement type, and aging. Oper. Dent. 2014, 39, 291–300. [Google Scholar] [CrossRef]
- Gomes, A.L.; Ramos, J.C.; Santos-del Riego, S.; Montero, J.; Albaladejo, A. Thermocycling effect on microshear bond strength to zirconia ceramic using Er:YAG and tribochemical silica coating as surface conditioning. Lasers Med. Sci. 2015, 30, 787–795. [Google Scholar] [CrossRef]
- Liu, L.; Liu, S.; Song, X.; Zhu, Q.; Zhang, W. Effect of Nd: YAG laser irradiation on surface properties and bond strength of zirconia ceramics. Lasers Med. Sci. 2015, 30, 627–634. [Google Scholar] [CrossRef]
- Seto, K.B.; McLaren, E.A.; Caputo, A.A.; White, S.N. Fatigue behavior of the resinous cement to zirconia bond. Oper Dent. 2013, 22, 523–528. [Google Scholar] [CrossRef] [PubMed]
- Baldissara, P.; Querzè, M.; Monaco, C.; Scotti, R.; Fonseca, R.G. Efficacy of surface treatments on the bond strength of resin cements to two brands of zirconia ceramic. J. Adhes Dent. 2013, 15, 259–267. [Google Scholar] [PubMed]
- Vanderlei, A.; Bottino, M.A.; Valandro, L.F. Evaluation of resin bond strength to yttria-stabilized tetragonal zirconia and framework marginal fit: Comparison of different surface conditionings. Oper. Dent. 2014, 39, 50–63. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Niu, L.N.; Wang, Y.J.; Jiao, K.; Liu, Y.; Zhou, W.; Shen, L.J.; Fang, M.; Li, M.; Zhang, X.; et al. Bonding of resin cement to zirconia with high pressure primer coating. PLoS ONE 2014, 9, e101174. [Google Scholar] [CrossRef] [PubMed]
- Saker, S.; Ibrahim, F.; Ozcan, M. Effect of different surface treatments on adhesion of In-Ceram Zirconia to enamel and dentin substrates. J. Adhes Dent. 2013, 15, 369–376. [Google Scholar] [PubMed]
- Queiroz, J.R.; Massi, M.; Nogueira, L., Jr.; Sobrinho, A.S.; Bottino, M.A.; Ozcan, M. Silica-based nano-coating on zirconia surfaces using reactive magnetron sputtering: Effect on chemical adhesion of resin cements. J. Adhes Dent. 2013, 15, 151–159. [Google Scholar] [PubMed]
- De Sa Barbosa, W.F.; Aguiar, T.R.; Francescantonio, M.D.; Cavalcanti, A.N.; de Oliveira, M.T.; Giannini, M. Effect of water storage on bond strength of self-adhesive resin cements to zirconium oxide ceramic. J. Adhes Dent. 2013, 15, 145–150. [Google Scholar] [PubMed]
- Lung, C.Y.; Kukk, E.; Matinlinna, J.P. The effect of silica-coating by sol-gel process on resin-zirconia bonding. Dent. Mater. J. 2013, 32, 165–172. [Google Scholar] [CrossRef]
- Subasi, M.G.; Inan, O. Influence of surface treatments and resin cement selection on bonding to zirconia. Lasers Med. Sci. 2014, 29, 19–27. [Google Scholar] [CrossRef]
- Kern, M.; Passia, N.; Sasse, M.; Yazigi, C. Ten-year outcome of zirconia ceramic cantilever resin-bonded fixed dental prostheses and the influence of the reasons for missing incisors. J. Dent. 2017, 65, 51–55. [Google Scholar] [CrossRef]
- Rathmann, F.; Bomicke, W.; Rammelsberg, P.; Ohlmann, B. Veneered zirconia inlay-retained fixed dental prostheses: 10-Year results from a prospective clinical study. J. Dent. 2017, 64, 68–72. [Google Scholar] [CrossRef]
- Chaar, M.S.; Kern, M. Five-year clinical outcome of posterior zirconia ceramic inlay-retained FDPs with a modified design. J. Dent. 2015, 43, 1411–1415. [Google Scholar] [CrossRef]
- Sasse, M.; Kern, M. Survival of anterior cantilevered all-ceramic resin-bonded fixed dental prostheses made from zirconia ceramic. J. Dent. 2014, 42, 660–663. [Google Scholar] [CrossRef] [PubMed]
- Sasse, M.; Kern, M. CAD/CAM single retainer zirconia-ceramic resin-bonded fixed dental prostheses: Clinical outcome after 5 years. Int J. Comput. Dent. 2013, 16, 109–118. [Google Scholar] [PubMed]
- Blatz, M.B.; Vonderheide, M.; Conejo, J. The Effect of Resin Bonding on Long-Term Success of High-Strength Ceramics. J. Dent. Res. 2018, 97, 132–139. [Google Scholar] [CrossRef] [PubMed]
- Luthra, R.; Kaur, P. An insight into current concepts and techniques in resin bonding to high strength ceramics. Aust. Dent. J. 2016, 61, 163–173. [Google Scholar] [CrossRef]
- Inokoshi, M.; De Munck, J.; Minakuchi, S.; Van Meerbeek, B. Meta-analysis of bonding effectiveness to zirconia ceramics. J. Dent. Res. 2014, 93, 329–334. [Google Scholar] [CrossRef]
- Otani, A.; Amaral, M.; May, L.G.; Cesar, P.F.; Valandro, L.F. A critical evaluation of bond strength tests for the assessment of bonding to Y-TZP. Dent. Mater. 2015, 31, 648–656. [Google Scholar] [CrossRef]
- Yun, J.Y.; Ha, S.R.; Lee, J.B.; Kim, S.H. Effect of sandblasting and various metal primers on the shear bond strength of resin cement to Y-TZP ceramic. Dent. Mater. 2010, 26, 650–658. [Google Scholar] [CrossRef]
- Zhang, Y.; Lawn, B.R.; Rekow, E.D.; Thompson, V.P. Effect of sandblasting on the long-term performance of dental ceramics. J. Biomed. Mater. Res. B Appl. Biomater. 2004, 71, 381–386. [Google Scholar] [CrossRef]
- Souza, R.O.; Valandro, L.F.; Melo, R.M.; Machado, J.P.; Bottino, M.A.; Ozcan, M. Air-particle abrasion on zirconia ceramic using different protocols: Effects on biaxial flexural strength after cyclic loading, phase transformation and surface topography. J. Mech. Behav. Biomed. Mater. 2013, 26, 155–163. [Google Scholar] [CrossRef] [PubMed]
- Özcan, M. Air Abrasion of Zirconia Resin-bonded Fixed Dental Prostheses Prior to Adhesive Cementation: Why and How? J. Adhes Dent. 2013, 394. [Google Scholar]
- Thammajaruk, P.; Inokoshi, M.; Chong, S.; Guazzato, M. Bonding of composite cements to zirconia: A systematic review and meta-analysis of in vitro studies. J. Mech. Behav. Biomed. Mater. 2018, 80, 258–268. [Google Scholar] [CrossRef] [PubMed]
| Database | PubMed, Medline; Cochrane Library. |
|---|---|
| Publication date | 1 January 2013–31 December 2018 |
| Keywords | Zirconia, 3Y-TZP, Adhesion, Adhesive cementation, Bonding, Resin, Composite resin, Composite material, Dentin, Enamel. |
| Language | English |
| Type of paper | In vitro studies, clinical articles, systematic reviews. |
| Inclusion criteria | Studies evaluating adhesion between zirconia and composite. |
| Exclusion criteria | In vitro studies: absence of bonding strength evaluation, insufficient aging (TC <5000 or storage <one month), complete crown specimens; Clinical articles: Case Report, Follow up < 5 years, studies on complete crowns. |
| Journal category | All |
| Search | Query | Items Found |
|---|---|---|
| 1 | Zirconia OR 3Y-TZP | 7020 |
| 2 | Adhesion OR adhesive cementation OR bonding | 372,909 |
| 3 | Resin OR composite resin OR composite material | 88,815 |
| 4 | 1 AND 2 AND 3 | 652 |
| 5 | Filters: Publication date from 2013/01/01 to 2018/12/31 | 370 |
| Final string | ||
| (((“zirconium oxide”[Supplementary Concept] OR “zirconium oxide”[All Fields] OR “zirconia”[All Fields]) OR 3Y-TZP[All Fields]) AND (((“J Adhes”[Journal] OR “adhesion”[All Fields]) OR ((“adhesives”[Pharmacological Action] OR “adhesives”[MeSH Terms] OR “adhesives”[All Fields] OR “adhesive”[All Fields]) AND (“cementation”[MeSH Terms] OR “cementation”[All Fields]))) OR (“object attachment”[MeSH Terms] OR (“object”[All Fields] AND “attachment”[All Fields]) OR “object attachment”[All Fields] OR “bonding”[All Fields]))) AND (((“resins, plant”[MeSH Terms] OR (“resins”[All Fields] AND “plant”[All Fields]) OR “plant resins”[All Fields] OR “resin”[All Fields]) OR (“composite resins”[MeSH Terms] OR (“composite”[All Fields] AND “resins”[All Fields]) OR “composite resins”[All Fields] OR (“composite”[All Fields] AND “resin”[All Fields]) OR “composite resin”[All Fields])) OR (composite[All Fields] AND material[All Fields])) AND (“2013/01/01”[PDAT]: “2018/12/31”[PDAT]) | ||
| Search | Query | Items Found |
|---|---|---|
| 1 | Zirconia OR 3Y-TZP | 7020 |
| 2 | Adhesion OR adhesive cementation OR bonding | 372,909 |
| 3 | Dentin OR enamel | 57,574 |
| 4 | 1 AND 2 AND 3 | 158 |
| 5 | Filters: Publication date from 1 January, 2013 to 31 December, 2018 | 77 |
| Final string | ||
| (((“zirconium oxide”[Supplementary Concept] OR “zirconium oxide”[All Fields] OR “zirconia”[All Fields]) OR 3Y-TZP[All Fields]) AND (((“J Adhes”[Journal] OR “adhesion”[All Fields]) OR ((“adhesives”[Pharmacological Action] OR “adhesives”[MeSH Terms] OR “adhesives”[All Fields] OR “adhesive”[All Fields]) AND (“cementation”[MeSH Terms] OR “cementation”[All Fields]))) OR (“object attachment”[MeSH Terms] OR (“object”[All Fields] AND “attachment”[All Fields]) OR “object attachment”[All Fields] OR “bonding”[All Fields]))) AND ((“dentin”[MeSH Terms] OR “dentin”[All Fields]) OR (“dental enamel”[MeSH Terms] OR (“dental”[All Fields] AND “enamel”[All Fields]) OR “dental enamel”[All Fields] OR “enamel”[All Fields])) AND (“2013/01/01”[PDAT]: “2018/12/31”[PDAT]) | ||
| Search | Query | Items Found |
|---|---|---|
| 1 | Zirconia OR 3Y-TZP | 267 |
| 2 | Adhesion OR adhesive cementation OR bonding | 12,030 |
| 3 | Resin OR composite resin OR composite material | 6317 |
| 4 | 1 AND 2 AND 3 | 52 |
| 5 | Cochrane Library publication date from Jan 2013 to Dec 2018 | 31 |
| Final string | ||
| ((zirconia) OR 3Y-TZP):ti,ab,kw AND (((adhesion) OR adhesive cementation) OR bonding):ti,ab,kw AND (((resin) OR composite resin) OR composite material):ti,ab,kw (Word variations have been searched)” with Cochrane Library publication date Between Jan 2013 and Dec 2018 (Word variations have been searched) | ||
| Article | Tested Adhesion Techniques | Results | |
|---|---|---|---|
| 1 | Yang et al., 2018 [10] | Different kinds of cement (RMGIC, self-adhesive, MDP-free). Primers and universal adhesives with 10-MDP. Preliminary APA preliminary. | RMGIC get worse adhesion results. Better bond strength for MDP primer (or adhesive) with traditional composite cement, than MDP cement alone. |
| 2 | Thammajaruk et al., 2019 [11] | Ceramic coating technique (DCM hot bond coating) vs. APA. | APA gives better adhesion and more stable long-term results. |
| 3 | Shimizu et al., 2018 [12] | Mechanical pre-treatment (none, APA, plasma treatment) and chemical pre-treatment (none, 10-MDP primer). | APA improves the bonding strength and the pre-treatment with MDP primer resulted in better adhesion. |
| 4 | Piest et al., 2018. [13] | Efficacy of plasma treatment for contaminated zirconia (saliva and silicone). | Plasma treatment is expensive and not efficacious, especially for silicone contamination. |
| 5 | Yang et al., 2018 [14] | Comparison between two kinds of adhesion protocol: one involves APA followed by MDP- free composite cement, others that involve APA followed by MDP containing product (primer or adhesive or cement). | Product containing 10-MDP (primers, adhesives, and cement) improve zirconia adhesion in comparison APA with MDP-free composite cement. |
| 6 | Moura et al., 2018 [15] | Comparison of three adhesion techniques: -APA+ MDP- composite cement -MDP-primer + MDP-free composite cement (no APA) -APA+ primer with functional monomer + MDP-free composite cement. | The adhesion protocol that involves APA followed the use of MDP-composite cement has worse results. |
| 7 | Araùjo et al., 2018 [16] | Compare the effectiveness of an MDP-adhesive as a substitute for TBC adhesion protocol. | Mechanical pre-treatment included in the TBC technique is necessary for an adequate adhesion. |
| 8 | Grasel et al., 2018 [17] | Evaluation of the effectiveness of mechanical pre-treatment (APA). Comparison of different adhesion systems (universal primer and composite cement) after APA. | Mechanical pre-treatment is necessary for improving adhesion. No substantial differences between the adhesion systems. |
| 9 | Dos Santos et al., 2018 [18] | Effect of incorporation of TiO2 nanotubes in a polycrystalline zirconia on bond strength. | The technique tested has no significant effect. |
| 0 | Dal Piva et al., 2018 [19] | Efficacy of a heat-treatment after TBC protocol. | Heat treatment is not valid in improving adhesion. |
| 1 | Yoshida et al., 2018 [20] | Cleaning methods for saliva contaminated zirconia (Ivoclean, ADG, etching gel, APA). | ADG and APA are effective cleaning methods on the alumina blasted zirconia. |
| 2 | Wille et al., 2017 [21] | Effectiveness comparison of “phosphoric acid esters”-based primer and a self-etching primer applied on sandblasted zirconia. Cementation with composite cement. | Phosphoric acid esters primer gets better results. |
| 3 | Xie et al., 2017 [22] | Different zirconia treatments (APA Al2O3, 40% HF 30 min, 40% HF 10 min in US bath) and different 10-MDP primers. Composite cement. | No differences emerge on the type of primer, nor on the way the acid is applied. Treatment with HF achieves results comparable to sandblasting. |
| 4 | Pitta et al., 2017 [23] | The study evaluates the effect of saliva contamination on the effectiveness of the adhesive system. | Some adhesive systems do not appear to be affected by saliva contamination. |
| 5 | Yagawa et al., 2018 [24] | Comparison of some primers containing different adhesive monomers. Cementation with self-curing or dual composite. | Dual cement ensures better adhesion. Major SBS for samples treated with 10-MDP primer. |
| 6 | Noda et al., 2017 [25] | Comparison of different primers with functional monomers. | Primer containing 10-MDP exhibits higher bond strength than MAC-10 primer. |
| 7 | Chuang et al., 2017 [26] | Comparison of silane, 10-MDP, or both MDP and silane primers on sandblasted samples. | 10-MDP primers get better SBS. |
| 8 | Elsayed et al., 2017 [27] | Sandblasted samples, subjected to the application of different primer/composite cement adhesive systems. | -APA + Monobond Plus (silane/adhesive monomers) + Variolink Esthetic DC. -APA + All Bond universal (10-MDP) + Duo Link Universal. |
| 9 | Galvão Ribeiro et al., 2018 [28] | Comparison between APA and TBC treatment followed by application of silane or silane/10-MDP primers. Self-adhesive composite. | TBC + silane/10-MDP primer + self-adhesive composite. |
| 0 | Chen C et al., 2017 [29] | Effect of storage in aqueous solutions (acid, basic, or neutral) on adhesion. Sandblasted samples, treated with two different MDP primers, cemented with a composite. | Values of SBS greater for samples deposited in alkaline solution. |
| 1 | Tsujimoto e al., 2017 [30] | Bond durability of universal adhesives. | Thermocycling decreases bond strength. |
| 2 | Sakrana and Ozcan, 2017 [31] | Different mechanical treatments (APA, CH2Cl2, HCl). | Better adhesion for HCl e APA. |
| 3 | Akazawa et al., 2017 [32] | Comparison between APA and TBC followed by the application of different primers. MDP-free composite cement. | -TBC + silane/10-MDP primer. -SAPA Al2O3 (50-70 µm) + silano/10-MDP primer. |
| 4 | Wandscher et al., 2016 [33] | Sandblasting with leucite powder, feldspar ceramic or Cojet method. Silane and adhesive cement application. | Better results for leucite powder sandblasting. |
| 5 | Esteves-Oliveira et al., 2016 [34] | Comparison between APA, TBC, ultrashort pulses laser. Self-adhesive composite. | Laser treatment is the more effective one. |
| 6 | Rona et al., 2017 [35] | Comparison between APA, TBS, Er: YAG e EDM (Electric Discharge Machine). MDP/silane or silane primer; MDP- based composite. | Better SBS values for EDM e Rocatec. |
| 7 | Sawada et al., 2016 [36] | Effectiveness of experimental conditioners, based on silica and quartz, applied before sintering. | Experimental solution does not improve significantly adhesion. |
| 8 | Zhao et al., 2016 [37] | Comparison of different primer/cement systems in improving zirconia adhesion. | Using an MDP-primer before cement improves adhesion, regardless of the type of cement (self-adhesive or MDP-free). |
| 9 | Iwasaki et al., 2016 [38] | Zirconia treatment with APA or TBC, followed by primer application with different functional components and traditional composite cement. | -TBC + 10-MDP/silane primer + traditional composite cement. |
| 0 | Passia et al., 2016 [39] | Effectiveness of different primers and composite cements after APA Al2O3. | -APA Al2O3 associated with MDP cement or phosphoric acid methacrylate cement and MDP primer. |
| 1 | Lopes et al., 2016 [40] | Different kinds of primers on sandblasted zirconia. MDP free cement. | MDP-based primers improve adhesion. |
| 2 | Salem et al., 2016 [41] | Different kind of treatments (APA Al2O3, SIE, “Modified fusion sputtering”). Self-adhesive composite. | -SIE or “Modified fusion sputtering” + silane/10-MDP primer. |
| 3 | Hallmann et al., 2016 [42] | Mechanical pre-treatments (APA with alumina or zirconia, abrasive paper, acid solution, plasma, argon-ion bombardment); 10-MDP composite. | The most effective method is APA with Al2O3. Increased adhesion strength even with sandblasting with zirconia particles, which seems to be less harmful. |
| 4 | Angkasith et al., 2016 [43] | Effect of saliva contamination with the use of 10-MDP primers. | If the contamination occurs after the primer, rinsing with water is sufficient. Otherwise, Ivoclean and APA are effective. |
| 5 | Bomicke et al., 2016 [44] | Comparison between different mechanical treatments (APA, Cojet, and Rocatec TBC), and comparison between the adhesive system. | -Rocatec + silane/10-MDP primer + 10-MDP composite. |
| 6 | Xie et al., 2016 [45] | Comparison between TBC and APA with different MDP primers. | -APA + Z-Prime plus+ 10-MDP primer -TBC |
| 7 | Cheung et al., 2015 [46] | Comparison of different surface treatments (vitrification, APA) followed by the application or not of silane/MDP primers and cementation with an MDP composite. | Liner (pre sintering) + HF + silane/MDP primer. |
| 8 | Ahn et al., 2015 [47] | Comparison between sandblasted or not zirconia. Application or not of primers with 10-MDP or other adhesive monomers. 10-MDP cement. | Good adhesion for APA + Primer 10-MDP + 10-MDP cement. Self-adhesive cement without preliminary sandblasting does not guarantee adhesion. |
| 9 | Alves et al., 2016 [48] | Comparison on cement (traditional composite or self-adhesive), and different substrates (Cojet, Rocatec, silane primer/10-MDP). | Better SBS for primer + traditional composite. |
| 0 | Yenisey et al., 2016 [49] | Effectiveness of various surface treatments and their association (APA, Cojet, Rocatec, Er: YAG, silane primer, Silano-Pen). | -APA + Cojet + silane. |
| 1 | Pereira et al., 2015 [50] | Comparison of application of various types of primers with or without sandblasting. | In general, sandblasting increases the bond strength if associated with the use of the primer, except for Scotchbond Universal (universal primer) and MZ Primer (primer with adhesive monomers). |
| 2 | Kim DH et al., 2015 [51] | Different cleaning methods: NaOCl, APA, Ivoclean, H2O2, H2O, and sodium dodecyl sulfate. | Effective for saliva cleansing NaOCl, Ivoclean, and sandblasting. |
| 3 | Liu D et al., 2015 [52] | TBC comparison with application of acid solutions (Nitric and Fluoridric acid) and application of pre-sintering silica particles. Silane/10-MDP primer, 10-MDP composite. | TBC method and silica particle deposition have higher SBS values. |
| 4 | Ishii et al., 2015 [53] | Comparison of saliva cleansing methods: water, sandblasting, Ivoclean, orthophosphoric acid. | Sandblasting and Ivoclean are effective. |
| 5 | Jiang et al., 2014 [54] | APA Al2O3 vs. SIE. 4-META-based composite. | Both methods increase adhesion values when compared to the control. |
| 6 | Oliveira-Ogliari et al., 2015 [55] | Effectiveness of solutions based on zirconia precursors compared with TBC. Silane, adhesive cement. | Promising results for experimental solutions. |
| 7 | Lung et al., 2015 [56] | Comparison of a solution based on silicon nitride with TBC. Silane, adhesive cement. | TBC gets better results. |
| 8 | Sciasci et al., 2015 [57] | Different surface treatments (APA, TBC) in association with different types of cement (modified CVI and adhesive cements). | High adhesion values for TBC with traditional adhesive cements or self-adhesive. |
| 9 | Qeblawi et al., 2015 [58] | Comparison of zirconia treatment (APA and TBC) and adhesive cement type. | -TBC (Cojet) + silane + self-adhesive.-APA (Al2O3 50 µm) + self-adhesive (MDP). |
| 0 | Feitosa et al., 2015 [59] | Different saliva cleansing methods: water, Ivoclean, orthophosphoric acid, isopropanol. | Ivoclean is the most effective of the tested methods. |
| 1 | Yi et al., 2015 [60] | APA and TBC, followed by primer application with different functional components and cementation with 10-MDP composite. | -APA Al2O3 + 10-MDP primer + 10-MDP composite. |
| 2 | Kim JH et al., 2015 [61] | Effectiveness comparison of various 10-MDP based primers. For this purpose, no preliminary treatments are done on zirconia and a traditional composite cement is used. | Primer universali All Bond Universal (10-MDP) and Single Bond Universal (10-MDP/silane) get better results than the Alloy Primer (10-MDP). |
| 3 | Klosa et al., 2014 [62] | Effectiveness of a solution of ethyl cellulose in the removal of contaminants. | The experimental solution improves SBS but does not reach the values of the uncontaminated sample. |
| 4 | Druck et al., 2015 [63] | Comparison of deposition of silica nanofilm (magnetron sputtering PVD) with tribological-chemical treatment. Silane and adhesive cement application. | Similar results (TBS) for TBC and Si nanofilm (5 nm). |
| 5 | De Souza et al., 2014 [64] | Different primers for zirconia, adhesive systems, and MDP- based cements. | Better adhesion values for samples in which the primer is applied. |
| 6 | Chen C et al., 2014 [65] | Comparison between TBC and APA followed or not by application of primer (Z-Prime Plus), both with traditional composite cement and self-adhesive (RelyX Unicem). | -TBC+ silane + traditional composite cement. |
| 7 | Shin et al., 2014 [66] | Two different MDP composites on zirconia treated with various methods (MDP primer, APA + primer, Cojet). | No significant differences on the type of cement. Best SBS for APA followed by the application of the 10-MDP primer. |
| 8 | Da Silva et al., 2014 [67] | Comparison of zirconia treatment (10-MDP primer vs. TBC) and comparison of cement type (traditional composite cement and self-adhesive, with adhesive monomers). | Best result for self-adhesive composite, in association with tribological-chemical treatment. |
| 9 | Oba et al., 2014 [68] | Efficacy of different primers on sandblasted zirconia. | MDP primers get better results, and are indifferent if silane is also present. |
| 0 | Liu et al., 2014 [69] | Comparison between: Rocatec, Glazing Porcelain + HF, pre-sintering silica powder application, pre-sintering zirconia powder application. Composite self-adhesive. | High SBS values for tTBC treatment and zirconia powder. |
| 1 | Erdem et al. 2014 [70] | Comparison of zirconia treatments (APA, TBC, Er: YAG), associated with different cements. | -Air abrasion 110 µm + self-adhesive composite.-Rocatec + silane + both traditional or self-adhesive cement. |
| 2 | Xie et al., 2013 [71] | Comparison of different treatments of zirconia (APA, Cojet, acid etching), followed by application or not of the primer. | -TBC (Cojet) + silane + MDP-free composite. -Hot etching + MDP primer + MDP-free composite. |
| 3 | Lin et al., 2013 [72] | Comparison of different treatments of zirconia (sandblasting with Al2O3 and Er: YAG laser). | The use of the Er: YAG laser is not able to increase the adhesion values. |
| 4 | Turker et al., 2013 [73] | Comparison of adhesion of CVI, CVI modified with resin, and MDP composite cements. Preliminary blasting. | Better adhesion values for self-adhesive cements. |
| 5 | Cheung et al., 2014 [74] | Comparison of different surface treatments (vitrification, APA) followed by the application or not of silane/MDP primers, cementation with MDP composite. | -TBC + silane/MDP + MDP cement.-Vitrification + HF+ silane/MDP+ MDP cement. |
| 6 | Keul et al., 2013 [75] | Comparison of the use of self-adhesive cements alone or in combination with primers containing adhesive monomers. | The use of the primer improves the bond strength. |
| 7 | Sarmento et al., 2014 [76] | APA and TBC comparison. Silane/10-MDP primer and 10-MDP composite. | After thermocycling spontaneous de-cementation of all the samples. |
| 8 | Heikkinen et al., 2013 [77] | Effect of different kind of silane on silica-coated alumina blasted zirconia. | Not significant differences. |
| 9 | Bottino et al., 2014 [78] | Comparison of two surface treatments of zirconia (vitrification and TB) associated with two different 10-MDP based resin cements. | Panavia F cement guarantees better adhesion, in particular in association with vitrification. |
| 0 | Gomes et al., 2015 [79] | Confronto trattamento zirconia (TBC, Laser Er: YAG) e tipologia cemento (cemento 10-MDP e cemento autoadesivo con altri monomeri). | -TBC (Rocatec) + silane + 10-MDP composite. |
| 1 | Liu L et al., 2015 [80] | Different zirconnia treatments (APA Al2O3, Nd: YAG laser). MDP-based cement. | -APA Al2O3 + MDP cement. |
| 2 | Seto et al., 2013 [81] | Comparison of different types of adhesive cement on sandblasted samples. | Higher adhesion values for cement with 10-MDP (Panavia 2.0 + Oxiguard primer) and GCem (self-adhesive with other monomers). |
| 3 | Baldissara et al., 2013 [82] | Comparison TBC with ceramic liner, and between self-adhesive composite (Panavia F e Rely X). | TBC achieves superior bond strength, especially in association with RelyX. Panavia F gives better results in association with the liner. |
| 4 | Vanderlei et al., 2014 [83] | Comparison between “glaze on technique and TBC.” MDP composite cement. | -Low fusing porcelain glaze + HF + silane MDPcomposite. |
| 5 | Wang et al., 2014 [84] | Use of MDP-primers (with different air-dried pressure) on sandblasted zirconia. | The pressure can affect the result depending on the primer used. |
| 6 | Saker et al., 2013 [85] | Comparison of different treatments (APA, TBC + silane or 10-MDP based primer, “glaze on” technique). Cementation with MDP composite. | -TBC + MDP primer - “Glaze on” technique + HF + silane. |
| 7 | Queiroz et al., 2013 [86] | Comparison of different zirconia treatments (sandblasting + primer, only primer, silica nanofilm with magnetron sputtering) and different cements (10-MDP, HEMA, other monomers). | -Air abrasion (Al2O3 45µm) + Metal/zirconia primer + self-adhesive composite. |
| 8 | De Sà Barbosa et al., 2013 [87] | Effectiveness comparison of some self-adhesive composite cements containing adhesive monomers other than 10-MDP (RelyX Unicem, BisCem, G-Cem, SeT) with traditional composite cement (RelyX ARC). APA 50 µm. | The only group to maintain higher values after 1 year is the one cemented with G-Cem. |
| 9 | Lung et al., 2013 [88] | Comparison between TEOS sol-gel technique and TBC. | Silica coating method improved adhesion more effectively. |
| 0 | Subasi et al., 2014 [89] | Comparison between mechanical treatments (APA Al2O3, TBC, Er: YAG laser) and between the cement (MDP or other monomers-based). | No differences between APA and TBC, with better results for MDP cements. |
| RMGIC, Resin Modified Glass Ionomer Cement. APA, Air Particle Abrasion. TBC, Tribochemical silica coating. SBS, Shear Bond Strength. TBS, Tensile Bond Strength. | |||
| Article | Type of Restoration | Adhesion Protocol | Follow-Up | Overall Survival Rate | |
|---|---|---|---|---|---|
| 1 | Kern et al., 2017 [90] | Single-retainer RBFDP | -APA Al2O3 50 µm, 10-MDP self-adhesive cement -Zirconia primer MDP-free composite cement. | 10 years | 98.2% |
| 2 | Rathmann et al., 2017 [91] | IRFDP | Tribochemical silica coating, silane, 10-MDP self-adhesive cement or MDP-free. | 5 years | 21.2% |
| 3 | Chaar et Kern, 2015 [92] | IRFDP | APA Al2O3 50 µm, self-adhesive 10-MDP cement. | 5 years | 95.8% |
| 4 | Sasse et Kern, 2014 [93] | Single-retainer RBFDP | APA Al2O3 50 µm, self-adhesive 10-MDP cement. | 6 years | 91.1% |
| 5 | Sasse et Kern, 2013 [94] | Single-retainer RBFDP | -APA Al2O3 50 µm, 10-MDP self-adhesive cement -Zirconia primer MDP-free composite cement. | 5 years | 89.4% |
| RBFDP, Resin Bonded Fixed Dental Prosthesis. IRFDP, Inlay Retained Fixed Dental Prosthesis. APA, Air Particle Abrasion. | |||||
| Article | Cause for Exclusion | |
|---|---|---|
| 1 | Blatz et al., 2017 [95] | Review of clinical trials, includes studies on complete crowns. |
| 2 | Khan et al., 2017 [9] | Review of laboratory studies, do not consider the aging factor. |
| 3 | Tzanakakis et al., 2016 [8] | Review of laboratory studies, do not consider the aging factor. |
| 4 | Luthra et kaur, 2016 [96] | Review of laboratory studies, do not consider the aging factor. |
| 5 | Ozcan et Bernasconi, 2015 [7] | Review of laboratory studies, do not consider the aging factor. |
| 6 | Inokoshi et al., 2014 [97] | Review of laboratory studies, does not observe the inclusion criteria relating to aging, and sets an “aging” limit at 1000 TC. |
| 7 | Miyazaki et al., 2013 [2] | Review of laboratory and clinical studies, do not consider the aging factor, and includes studies on complete crowns. |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Scaminaci Russo, D.; Cinelli, F.; Sarti, C.; Giachetti, L. Adhesion to Zirconia: A Systematic Review of Current Conditioning Methods and Bonding Materials. Dent. J. 2019, 7, 74. https://doi.org/10.3390/dj7030074
Scaminaci Russo D, Cinelli F, Sarti C, Giachetti L. Adhesion to Zirconia: A Systematic Review of Current Conditioning Methods and Bonding Materials. Dentistry Journal. 2019; 7(3):74. https://doi.org/10.3390/dj7030074
Chicago/Turabian StyleScaminaci Russo, Daniele, Francesca Cinelli, Chiara Sarti, and Luca Giachetti. 2019. "Adhesion to Zirconia: A Systematic Review of Current Conditioning Methods and Bonding Materials" Dentistry Journal 7, no. 3: 74. https://doi.org/10.3390/dj7030074
APA StyleScaminaci Russo, D., Cinelli, F., Sarti, C., & Giachetti, L. (2019). Adhesion to Zirconia: A Systematic Review of Current Conditioning Methods and Bonding Materials. Dentistry Journal, 7(3), 74. https://doi.org/10.3390/dj7030074






