Synergistic Effect of Sodium Hypochlorite and Carbon Dioxide Against Enterococcus faecalis Biofilm
Abstract
1. Introduction
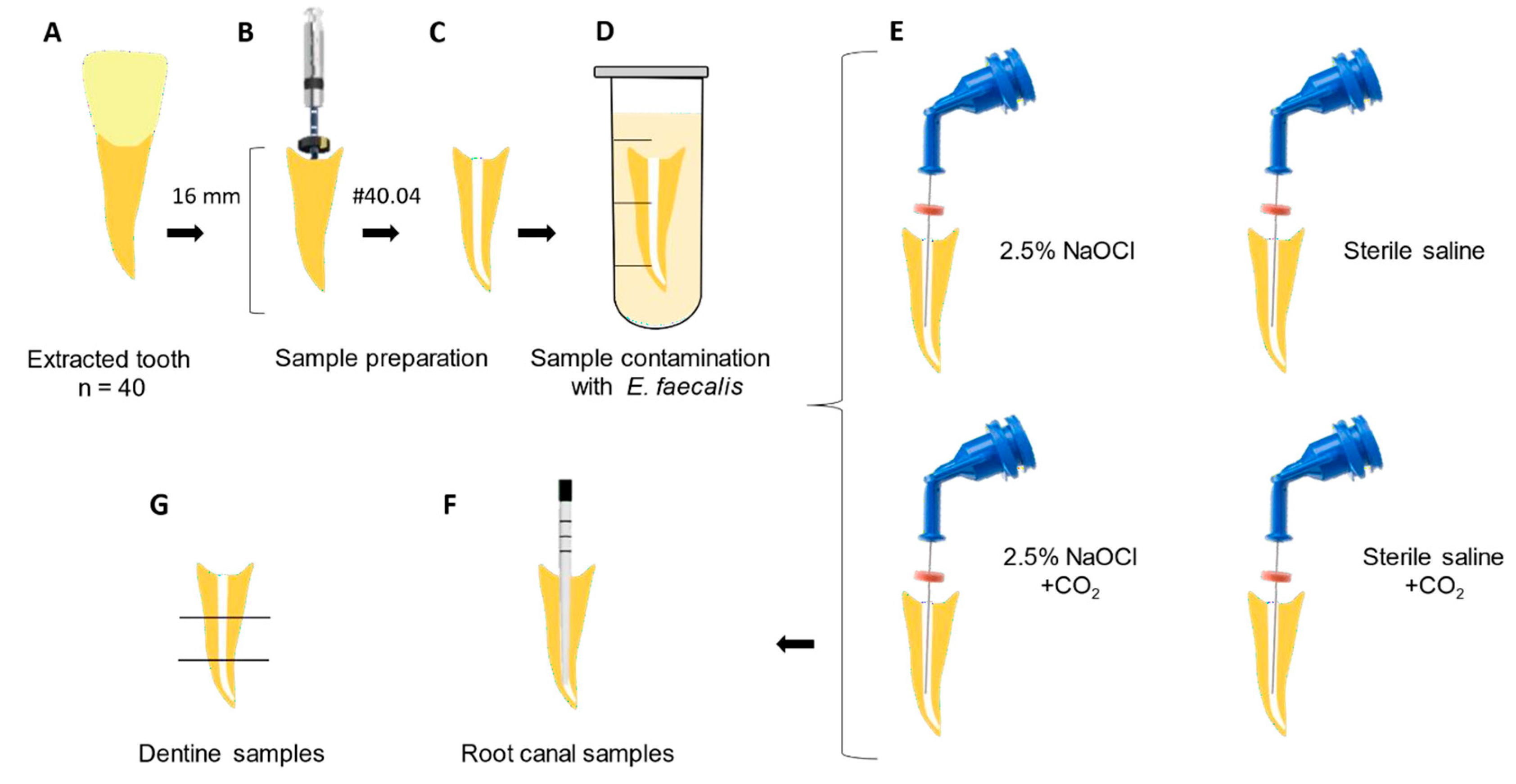
2. Materials and Methods
2.1. Sample Selection and Preparation
2.2. Cultivation of E. faecalis and Specimen Contamination
2.3. Experimental Groups
- The 2.5% NaOCl group: Root canals were irrigated and manually agitated with a #15 K-file using 15 mL of 2.5% NaOCl, 5 mL of 17% EDTA, and a final 5 mL of 2.5% NaOCl for 20 s each. Subsequently, 1 mL of 5% sodium thiosulfate was used for 1 min to inactivate NaOCl. A total of 20 mL of 2.5% NaOCl was used for irrigation [36,40].
- The 2.5% NaOCl + CO2 group: Root canals were irrigated and manually agitated with a #15 K-file using 15 mL of 2.5% NaOCl + CO2 (NaOCl was carbonated using a jet aeration device -Sodastream Industries LTD, Kfar Saba, Israel), 5 mL of 17% EDTA, and a final 5 mL of 2.5% NaOCl + CO2 for 20 s each. Subsequently, 1 mL of 5% sodium thiosulfate was used for 1 min to inactivate NaOCl. A total of 20 mL of 2.5% NaOCl + CO2 was used for irrigation [36,40].
- Sterile saline group: Root canals were irrigated and manually agitated with a #15 K-file using 15 mL of sterile saline solution, 5 mL of 17% EDTA, and a final 5 mL of sterile saline solution for 20 s each. Subsequently, 1 mL of 5% sodium thiosulfate was used for 1 min. A total of 20 mL of sterile saline solution was used for irrigation [36,40].
- Sterile saline + CO2 group: Root canals were irrigated and manually agitated with a #15 K-file using 15 mL of sterile saline solution + CO2 using the jet aeration system, 5 mL of 17% EDTA, and a final 5 mL of sterile saline solution + CO2 solution for 20 s each. Subsequently, 1 mL of 5% sodium thiosulfate was used for 1 min. A total of 20 mL of sterile saline solution + CO2 was used for irrigation [36,40].
2.4. Microbiological Collection
2.5. Dentine Samples
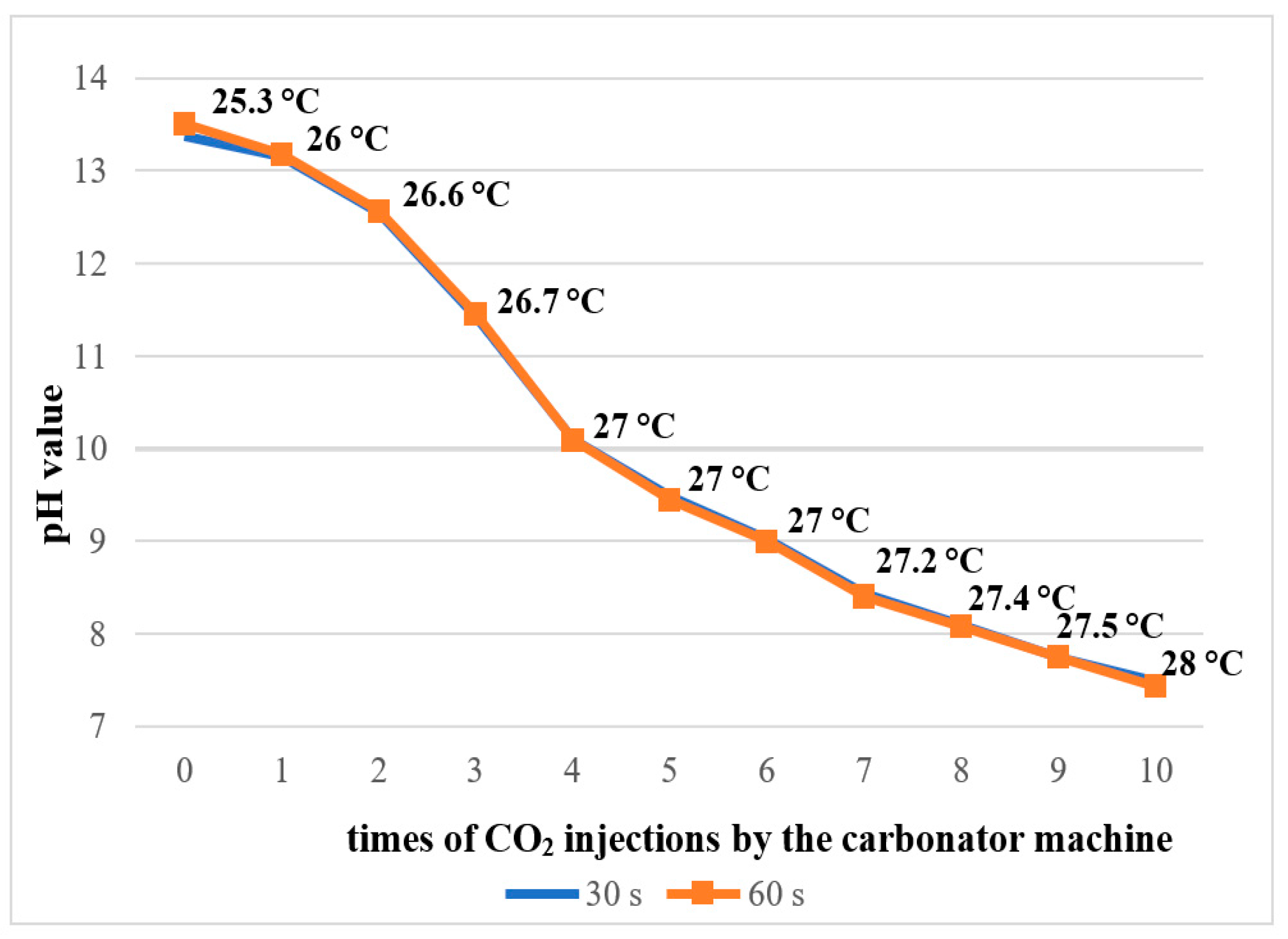
2.6. pH Measurement
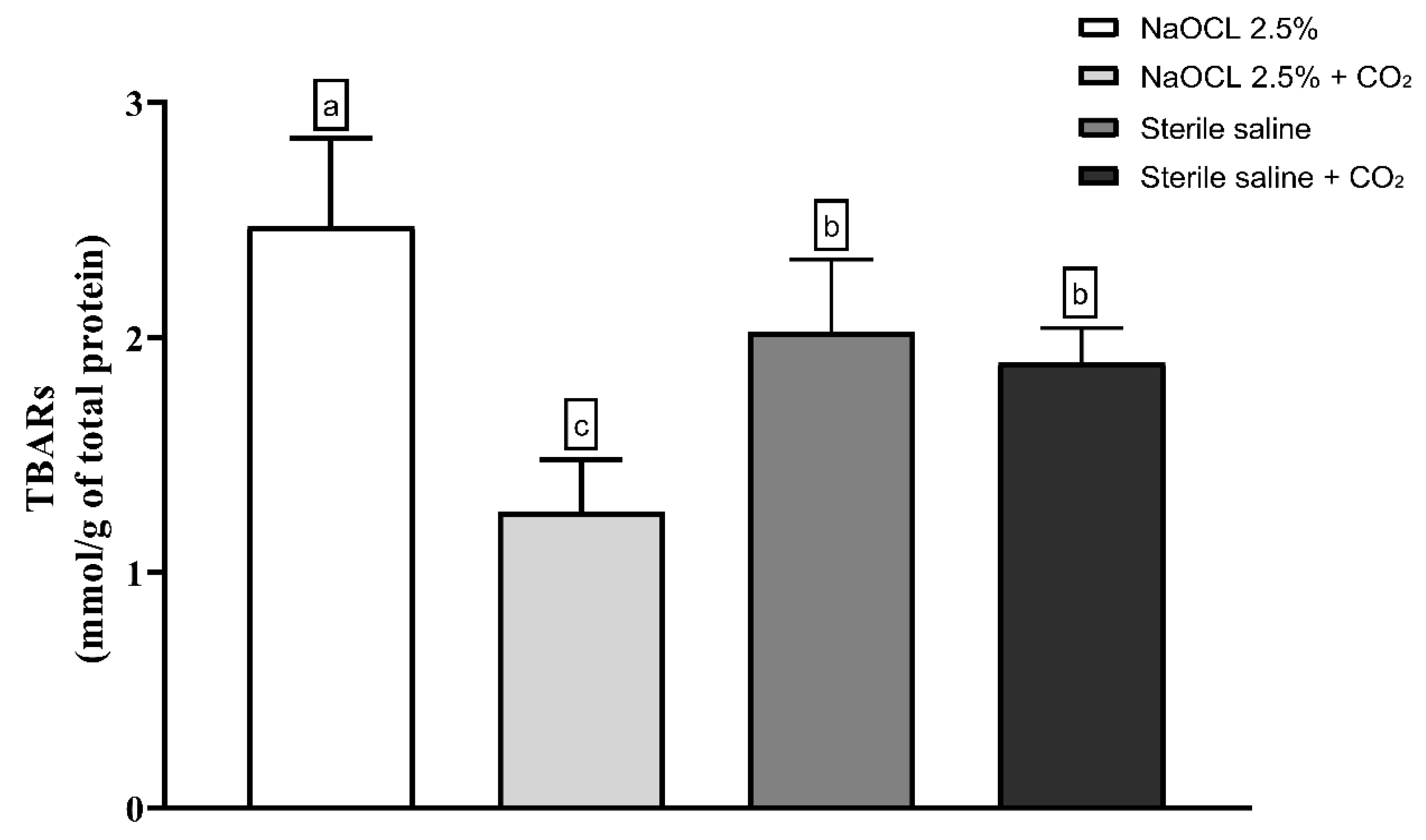
2.7. Assessment of Oxidative Damage Products
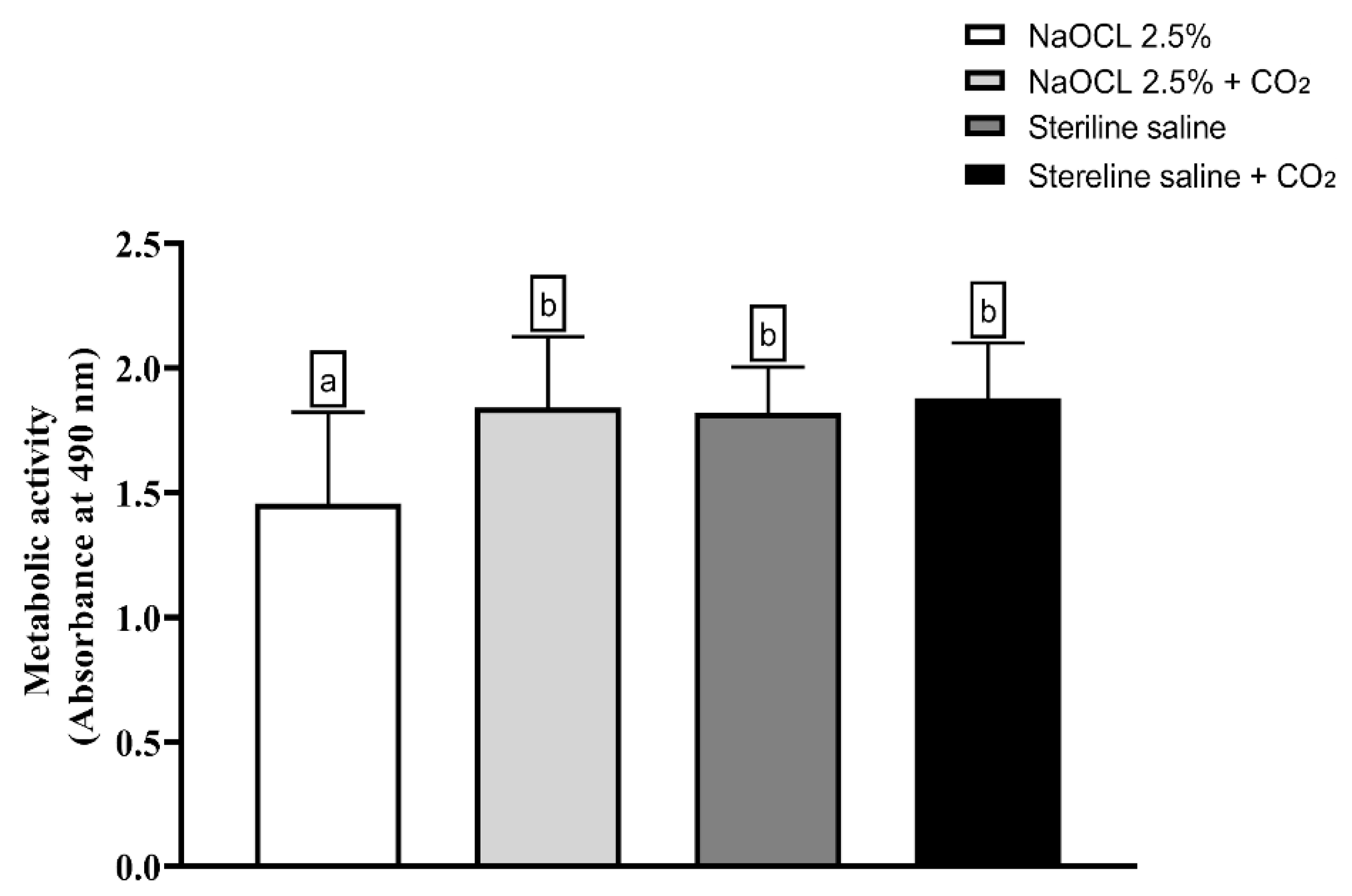
2.8. Metabolic Activity Assessment
2.9. Statistical Analysis
3. Results
3.1. Results of pH Measurement
3.2. Oxidative Damage
3.3. Evaluation of Metabolic Activity
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ahmed, S.; Hassan, S.J.; Gajdhar, S.; Alhazmi, L.S.; Khalifah, R.Y.; Alrifai, J.A.; Aljhdali, S.S.; Maqbul, M.S. Prevalence of Enterococcus faecalis and Candida albicans in endodontic retreatment Cases: A comprehensive study. Saudi Dent. J. 2024, 36, 539–545. [Google Scholar] [CrossRef] [PubMed]
- Alghamdi, F.; Shakir, M. The Influence of Enterococcus faecalis as a Dental Root Canal Pathogen on Endodontic Treatment: A Systematic Review. Cureus 2020, 12, e7257. [Google Scholar] [CrossRef]
- Barbosa-Ribeiro, M.; Arruda-Vasconcelos, R.; Louzada, L.M.; dos Santos, D.G.; Andreote, F.D.; Gomes, B.P.F.A. Microbiological analysis of endodontically treated teeth with apical periodontitis before and after endodontic retreatment. Clin. Oral Investig. 2020, 25, 2017–2027. [Google Scholar] [CrossRef]
- Pinheiro, E.T.; Gomes, B.P.F.A.; Ferraz, C.C.R.; Teixeira, F.B.; Zaia, A.A.; Filho, F.J.S. Evaluation of root canal microorganisms isolated from teeth with endodontic failure and their antimicrobial susceptibility. Oral Microbiol. Immunol. 2003, 18, 100–103. [Google Scholar] [CrossRef]
- Siqueira, J.F., Jr.; Rôças, I.N. Polymerase chain reaction–based analysis of microorganisms associated with failed endodontic treatment. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2004, 97, 85–94. [Google Scholar] [CrossRef]
- Distel, J.; Hatton, J.; Gillespie, M. Biofilm formation in medicated root canals. J. Endod. 2002, 28, 689–693. [Google Scholar] [CrossRef]
- Guerreiro-Tanomaru, J.M.; de Faria-Júnior, N.B.; Duarte, M.A.H.; Ordinola-Zapata, R.; Graeff, M.S.Z.; Tanomaru-Filho, M. Comparative Analysis of Enterococcus faecalis Biofilm Formation on Different Substrates. J. Endod. 2013, 39, 346–350. [Google Scholar] [CrossRef]
- Sedgley, C.M.; Molander, A.; Flannagan, S.E.; Nagel, A.C.; Appelbe, O.K.; Clewell, D.B.; Dahlén, G. Virulence, phenotype and genotype characteristics of endodontic Enterococcus spp. Oral Microbiol. Immunol. 2004, 20, 10–19. [Google Scholar] [CrossRef]
- Gomes, B.P.F.A.; Souza, S.F.C.; Ferraz, C.C.R.; Teixeira, F.B.; Zaia, A.A.; Valdrighi, L.; Souza-Filho, F.J. Effectiveness of 2% chlorhexidine gel and calcium hydroxide against Enterococcus faecalis in bovine root dentine in vitro. Int. Endod. J. 2003, 36, 267–275. [Google Scholar] [CrossRef]
- Weckwerth, P.H.; Zapata, R.O.; Vivan, R.R.; Filho, M.T.; Maliza, A.G.A.; Duarte, M.A.H. In Vitro Alkaline pH Resistance of Enterococcus faecalis. Braz. Dent. J. 2013, 24, 474–476. [Google Scholar] [CrossRef] [PubMed]
- Barbosa-Ribeiro, M.; De-Jesus-Soares, A.; Zaia, A.A.; Ferraz, C.C.; Almeida, J.F.; Gomes, B.P. Antimicrobial Susceptibility and Characterization of Virulence Genes of Enterococcus faecalis Isolates from Teeth with Failure of the Endodontic Treatment. J. Endod. 2016, 42, 1022–1028. [Google Scholar] [CrossRef]
- Figdor, D.; Davies, J.K.; Sundqvist, G. Starvation survival, growth and recovery of Enterococcus faecalis in human serum. Oral Microbiol. Immunol. 2003, 18, 234–239. [Google Scholar] [CrossRef]
- Carvalho, A.S.; Camargo, C.H.R.; Valera, M.C.; Camargo, S.E.A.; Mancini, M.N.G. Smear Layer removal by auxiliary chemical substances in biomechanical preparation: A scanning electron microscope study. J. Endod. 2008, 34, 1396–1400. [Google Scholar] [CrossRef] [PubMed]
- Mohammadi, Z. Sodium hypochlorite in endodontics: An update review. Int. Dent. J. 2008, 58, 329–341. [Google Scholar] [CrossRef]
- Aveiro, E.; Chiarelli-Neto, V.M.; De-Jesus-Soares, A.; Zaia, A.A.; Ferraz, C.C.R.; Almeida, J.F.A.; Marciano, M.A.; Feres, M.; Gomes, B.P.F.A. Efficacy of reciprocating and ultrasonic activation of 6% sodium hypochlorite in the reduction of microbial content and virulence factors in teeth with primary endodontic infection. Int. Endod. J. 2019, 53, 604–618. [Google Scholar] [CrossRef] [PubMed]
- Wong, D.T.; Cheung, G.S. Extension of bactericidal effect of sodium hypochlorite into dentinal tubules. J. Endod. 2014, 40, 825–829. [Google Scholar] [CrossRef] [PubMed]
- Gazzaneo, I.; Vieira, G.C.; Pérez, A.R.; Alves, F.R.; Gonçalves, L.S.; Mdala, I.; Siqueira, J.F.; Rôças, I.N. Root Canal Disinfection by Single- and Multiple-instrument Systems: Effects of Sodium Hypochlorite Volume, Concentration, and Retention Time. J. Endod. 2019, 45, 736–741. [Google Scholar] [CrossRef]
- Ma, J.; Wang, Z.; Shen, Y.; Haapasalo, M. A new noninvasive model to study the effectiveness of dentin disinfection by using confocal laser scanning microscopy. J. Endod. 2011, 37, 1380–1385. [Google Scholar] [CrossRef]
- Wang, Z.; Shen, Y.; Haapasalo, M. Effectiveness of endodontic disinfecting solutions against young and old enterococcus faecalis biofilms in dentin canals. J. Endod. 2012, 38, 1376–1379. [Google Scholar] [CrossRef]
- Haapasalo, M.; Shen, Y.; Wang, Z.; Gao, Y. Irrigation in endodontics. Br. Dent. J. 2014, 216, 299–303. [Google Scholar] [CrossRef]
- Rossi-Fedele, G.; Guastalli, A.R.; Doğramacı, E.J.; Steier, L.; De Figueiredo, J.A.P. Influence of pH changes on chlorine-containing endodontic irrigating solutions. Int. Endod. J. 2011, 44, 792–799. [Google Scholar] [CrossRef]
- Yared, G.; Ramli, G.A.A. Antibacterial Ability of Sodium Hypochlorite Heated in the Canals of Infected Teeth: An Ex Vivo Study. Cureus 2020, 12, e6975. [Google Scholar] [CrossRef]
- Hage, W.; De Moor, R.J.G.; Hajj, D.; Sfeir, G.; Sarkis, D.K.; Zogheib, C. Impact of Different Irrigant Agitation Methods on Bacterial Elimination from Infected Root Canals. Dent. J. 2019, 7, 64. [Google Scholar] [CrossRef]
- Penukonda, R.; Teja, K.V.; Kacharaju, K.R.; Xuan, S.Y.; Mohan, D.A.; Sheun, L.Y.; Cernera, M.; Iaculli, F. Comparative evaluation of smear layer removal with Ultra-X device and XP-Endo Finisher file system: An ex-vivo study: Smear removal on using various activation devices. G. Ital. Endod. 2023, 37. [Google Scholar] [CrossRef]
- Zeng, C.; Meghil, M.M.; Miller, M.; Gou, Y.; Cutler, C.W.; Bergeron, B.E.; Niu, L.; Ma, J.; Tay, F.R. Antimicrobial efficacy of an apical negative pressure root canal irrigation system against intracanal microorganisms. J. Dent. 2018, 72, 71–75. [Google Scholar] [CrossRef]
- Abdellatif, D.; Pisano, M.; Cecere, L.; Natoli, V.; Mancino, D.; Euvrard, E.; Iandolo, A. Activation of Irrigants in Root Canals with Open Apices: A Narrative Review. J. Clin. Med. 2024, 13, 6611. [Google Scholar] [CrossRef] [PubMed]
- Teja, K.V.; Mustafa, M.; Esposito, L.; Iaculli, F.; Cernera, M. Novel non-obturation based concept of regeneration: Apical debris extrusion. G. Ital. Endod. 2024, 38. [Google Scholar] [CrossRef]
- Dang, T.-L.T.; Imai, T.; Van Le, T.; Nguyen, D.-M.K.; Higuchi, T.; Kanno, A.; Yamamoto, K.; Sekine, M. Synergistic effect of pressurized carbon dioxide and sodium hypochlorite on the inactivation of Enterococcus sp. in seawater. Water Res. 2016, 106, 204–213. [Google Scholar] [CrossRef]
- Dehghani, F.; Annabi, N.; Titus, M.; Valtchev, P.; Tumilar, A. Sterilization of ginseng using a high pressure CO2 at moderate temperatures. Biotechnol. Bioeng. 2008, 102, 569–576. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.R.; Park, H.J.; Yim, D.S.; Kim, H.T.; Choi, I.-G.; Kim, K.H. Analysis of survival rates and cellular fatty acid profiles of Listeria monocytogenes treated with supercritical carbon dioxide under the influence of cosolvents. J. Microbiol. Methods 2008, 75, 47–54. [Google Scholar] [CrossRef]
- Vo, H.T.; Imai, T.; Teeka, J.; Sekine, M.; Kanno, A.; Van Le, T.; Higuchi, T.; Phummala, K.; Yamamoto, K. Comparison of disinfection effect of pressurized gases of CO2, N2O, and N2 on Escherichia coli. Water Res. 2013, 47, 4286–4293. [Google Scholar] [CrossRef]
- Hernández-Ríos, P.; Pussinen, P.J.; Vernal, R.; Hernández, M. Oxidative Stress in the Local and Systemic Events of Apical Periodontitis. Front. Physiol. 2017, 8, 869. [Google Scholar] [CrossRef]
- Georgiou, A.C.; Cornejo Ulloa, P.; Van Kessel, G.M.H.; Crielaard, W.; Van der Waal, S.V. Reactive oxygen species can be traced locally and systemically in apical periodontitis: A systematic review. Arch. Oral. Biol. 2021, 129, 105167. [Google Scholar] [CrossRef]
- Castelo-Baz, P.; Martín-Biedma, B.; Cantatore, G.; Ruíz-Piñón, M.; Bahillo, J.; Rivas-Mundiña, B.; Varela-Patiño, P. In vitro comparison of passive and continuous ultrasonic irrigation in simulated lateral canals of extracted teeth. J. Endod. 2012, 38, 688–691. [Google Scholar] [CrossRef] [PubMed]
- Ferraz, C.C.R.; Gomes, B.P.F.A.; Zaia, A.A.; Teixeira, F.B.; Souza-Filho, F.J. In vitro assessment of the antimicrobial action and the mechanical ability of chlorhexidine gel as an endodontic irrigant. J. Endod. 2001, 27, 452–455. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, M.C.; Zuolo, M.L.; Arruda-Vasconcelos, R.; Marinho, A.C.S.; Louzada, L.M.; Francisco, P.A.; Pecorari, V.G.A.; Gomes, B.P.F.d.A. Effectiveness of XP-Endo Finisher in the reduction of bacterial load in oval-shaped root canals. Braz. Oral Res. 2019, 33, e021. [Google Scholar] [CrossRef]
- Yamamoto, L.Y.; Loureiro, C.; Cintra, L.T.A.; Leonardo, R.d.T.; Banci, H.A.; Ribeiro, A.P.F.; Sivieri-Araujo, G.; Jacinto, R.d.C. Antibiofilm activity of laser ablation with indocyanine green activated by different power laser parameters compared with photodynamic therapy on root canals infected with Enterococcus faecalis. Photodiagn. Photodyn. Ther. 2021, 35, 102377. [Google Scholar] [CrossRef]
- Asnaashari, M.; Veshveshadi, O.; Aslani, F.; Hakimiha, N. Evaluation the antibacterial efficacy of sodium hypochlorite in combination with two different photodynamic therapy protocols against Enterococcus Faecalis in Infected root canals: An in-vitro experiment. Photodiagn. Photodyn. Ther. 2023, 43, 103722. [Google Scholar] [CrossRef] [PubMed]
- Lile, I.E.; Hajaj, T.; Veja, I.; Hosszu, T.; Vaida, L.L.; Todor, L.; Stana, O.; Popovici, R.-A.; Marian, D. Comparative Evaluation of Natural Mouthrinses and Chlorhexidine in Dental Plaque Management: A Pilot Randomized Clinical Trial. Healthcare 2025, 13, 1181. [Google Scholar] [CrossRef]
- Marinho, A.C.S.; Martinho, F.C.; Gonçalves, L.M.; Rabang, H.R.C.; Gomes, B.P.F.A. Does the Reciproc file remove root canal bacteria and endotoxins as effectively as multifile rotary systems? Int. Endod. J. 2014, 48, 542–548. [Google Scholar] [CrossRef]
- Berber, V.B.; Gomes, B.P.F.A.; Sena, N.T.; Vianna, M.E.; Ferraz, C.C.R.; Zaia, A.A.; Souza-Filho, F.J. Efficacy of various concentrations of NaOCl and instrumentation techniques in reducing Enterococcus faecalis within root canals and dentinal tubules. Int. Endod. J. 2006, 39, 10–17. [Google Scholar] [CrossRef]
- Rodrigues, G.W.L.; Gouveia, S.D.B.V.; Oliveira, L.C.; de Freitas, R.N.; Dourado, N.G.; Sacoman, C.A.; Ribeiro, A.P.F.; Chaves-Neto, A.H.; Sivieri-Araújo, G.; Leonardo, R.d.T.; et al. Comparative analysis of antimicrobial activity and oxidative damage induced by laser ablation with indocyanine green versus aPDT with methylene blue and curcumin on E. coli biofilm in root canals. Odontology 2025, 1–9. [Google Scholar] [CrossRef]
- Jacob, V.P.; Paião, L.I.; da Silva, A.C.G.; Magario, M.K.W.; Kaneko, T.Y.; Martins, C.M.; Monteiro, D.R.; Mori, G.G. Antimicrobial action of NeoMTA Plus on mono- and dual-species biofilms of Enterococcus faecalis and Candida albicans: An in vitro study. Arch. Oral Biol. 2020, 120, 104925. [Google Scholar] [CrossRef]
- Zehnder, M. Root Canal Irrigants. J. Endod. 2006, 32, 389–398. [Google Scholar] [CrossRef]
- Mohammadi, Z.; Shalavi, S.; Giardino, L.; Palazzi, F.; Mashouf, R.Y.; Soltanian, A. Antimicrobial effect of three new and two established root canal irrigation solutions. Gen. Dent. 2012, 60, 534. [Google Scholar]
- Fukuzaki, S. Mechanisms of actions of sodium hypochlorite in cleaning and disinfection processes. Biocontrol Sci. 2006, 11, 147–157. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Gonzalez, L.; Geeraerd, A.H.; Spilimbergo, S.; Elst, K.; Van Ginneken, L.; Debevere, J.; Van Impe, J.; Devlieghere, F. High pressure carbon dioxide inactivation of microorganisms in foods: The past, the present and the future. Int. J. Food Microbiol. 2007, 117, 1–28. [Google Scholar] [CrossRef] [PubMed]
- Ballal, N.V.; Gandhi, P.; Shenoy, P.A.; Dummer, P.M.H. Evaluation of various irrigation activation systems to eliminate bacteria from the root canal system: A randomized controlled single blinded trial. J. Dent. 2020, 99, 103412. [Google Scholar] [CrossRef]
- Orozco, E.I.F.; Toia, C.C.; Cavalli, D.; Khoury, R.D.; Cardoso, F.G.d.R.; Bresciani, E.; Valera, M.C. Effect of passive ultrasonic activation on microorganisms in primary root canal infection: A randomized clinical trial. J. Appl. Oral Sci. 2020, 28, e20190100. [Google Scholar] [CrossRef] [PubMed]


| Irrigation Protocol | Before IP | After IP |
|---|---|---|
| 2.5% NaOCl | 6.5 Aa | 1.2 Ba |
| (±0.5) | (±1.2) | |
| 2.5% NaOCl + CO2 | 6.3 Aa | 0.4 Bb |
| (±0.4) | (±0.7) | |
| Sterile saline | 6.7 Aa | 5.0 Bc |
| (±0.4) | (±0.2) | |
| Sterile saline + CO2 | 6.9 Aa | 4.9 Bc |
| (±0.3) | (±0.2) |
| Thirds | Irrigation Protocol | |||
|---|---|---|---|---|
| 2.5% NaOCl | 2.5% NaOCl + CO2 | Sterile Saline | Sterile Saline + CO2 | |
| Cervical | 0.8 Aa | 0.2 Aa | 3.9 Ba | 4.1 Ba |
| (±1.3) | (±0.5) | (±0.6) | (±0.6) | |
| Medium | 0.7 Aa | 1.0 Ab | 4.2 Ba | 3.9 Ba |
| (±1.6) | (±1.4) | (±0.4) | (±0.9) | |
| Apical | 2.7 Ab | 3.5 Ac | 4.5 Ba | 4.5 Ba |
| (±1.8) | (±0.6) | (±0.3) | (±0.5) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
de Andrade, J.G.; Natali, A.F.F.; Loureiro, C.; Rodrigues, G.W.L.; Ribeiro, A.P.F.; de Freitas, R.N.; Barzotti, R.J.; Oliveira, L.C.; de Moraes, Y.G.C.; Gomes, N.A.; et al. Synergistic Effect of Sodium Hypochlorite and Carbon Dioxide Against Enterococcus faecalis Biofilm. Dent. J. 2025, 13, 417. https://doi.org/10.3390/dj13090417
de Andrade JG, Natali AFF, Loureiro C, Rodrigues GWL, Ribeiro APF, de Freitas RN, Barzotti RJ, Oliveira LC, de Moraes YGC, Gomes NA, et al. Synergistic Effect of Sodium Hypochlorite and Carbon Dioxide Against Enterococcus faecalis Biofilm. Dentistry Journal. 2025; 13(9):417. https://doi.org/10.3390/dj13090417
Chicago/Turabian Stylede Andrade, Júlia Guerra, Ana Flávia Folhas Natali, Caroline Loureiro, Gladiston William Lobo Rodrigues, Ana Paula Fernandes Ribeiro, Rayara Nogueira de Freitas, Renan Jose Barzotti, Laura Cesário Oliveira, Yuri Gabriel Chamorro de Moraes, Natália Amanda Gomes, and et al. 2025. "Synergistic Effect of Sodium Hypochlorite and Carbon Dioxide Against Enterococcus faecalis Biofilm" Dentistry Journal 13, no. 9: 417. https://doi.org/10.3390/dj13090417
APA Stylede Andrade, J. G., Natali, A. F. F., Loureiro, C., Rodrigues, G. W. L., Ribeiro, A. P. F., de Freitas, R. N., Barzotti, R. J., Oliveira, L. C., de Moraes, Y. G. C., Gomes, N. A., Chaves-Neto, A. H., Martinho, F. C., & Jacinto, R. d. C. (2025). Synergistic Effect of Sodium Hypochlorite and Carbon Dioxide Against Enterococcus faecalis Biofilm. Dentistry Journal, 13(9), 417. https://doi.org/10.3390/dj13090417








