Fatigue Behavior of Multi/Unit-Supported Dental Restorations: Implant Platform vs. Prosthetic Platform
Abstract
1. Introduction
2. Materials and Methods
| Ti6Al4V ELI (Ti Gr5) | Ti CP4 | ||
|---|---|---|---|
| Composition | Wt. % | Composition | Wt. % |
| Al | 5.5–6.5 | N(max) | 0.05 |
| V | 3.5–4.5 | C(max) | 0.08 |
| Fe(max) | 0.25 | Fe(max) | 0.5 |
| O(max) | 0.13 | O(max) | 0.4 |
| C(max) | 0.08 | H(max) | 0.0125 |
| N(max) | 0.05 | - | - |
| H(max) | 0.012 | - | - |
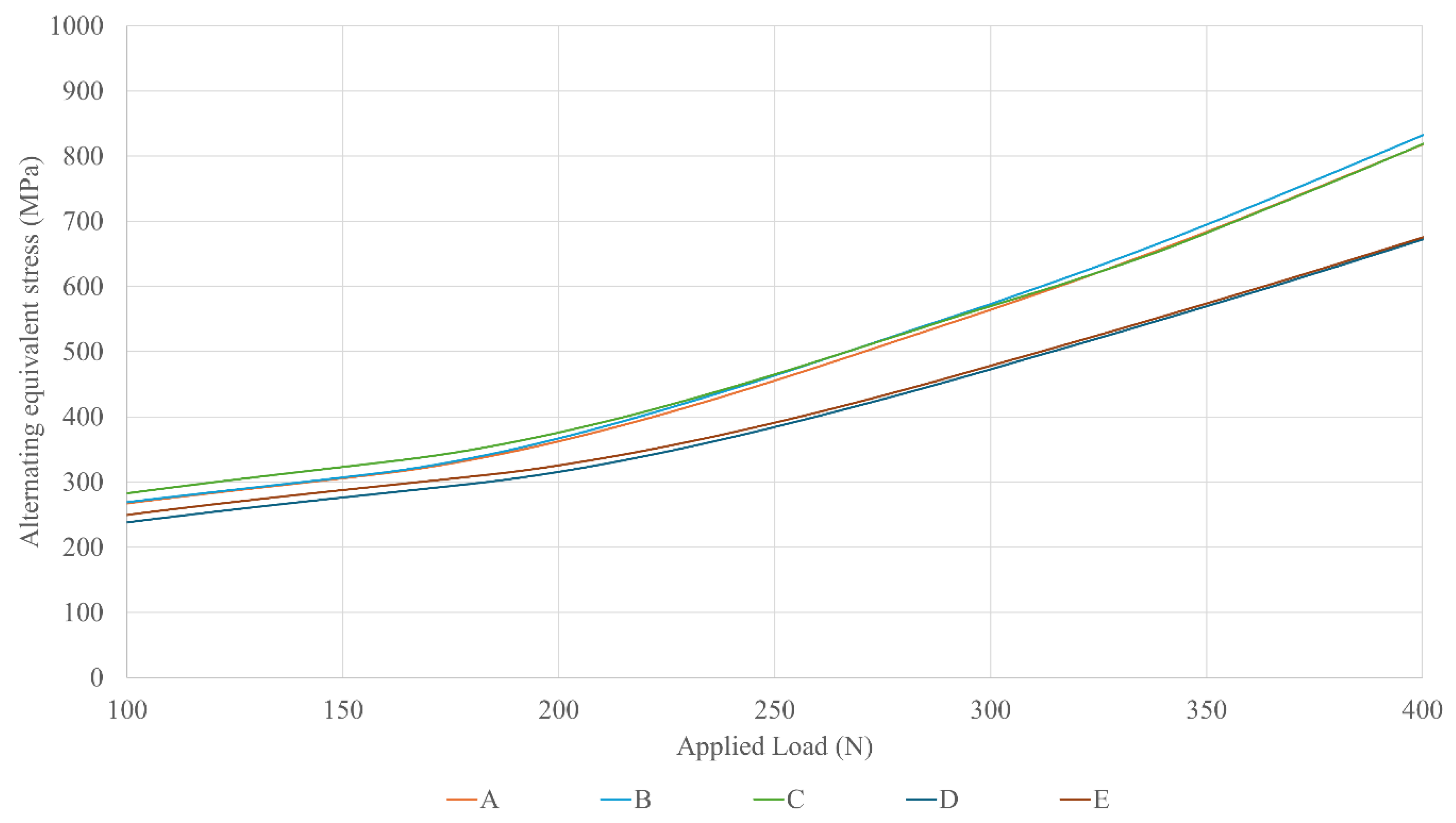
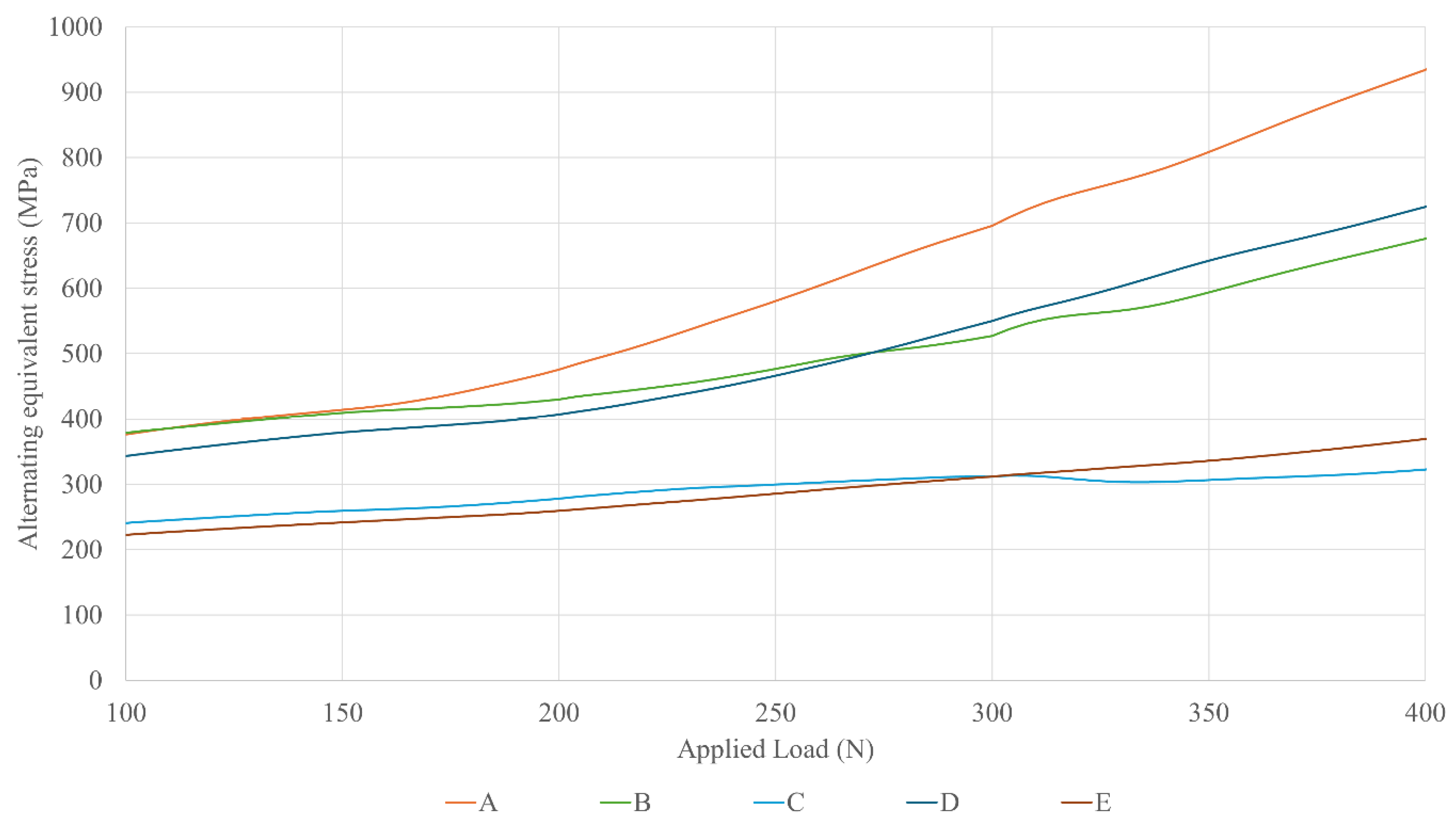
3. Results
4. Discussion
5. Conclusions
- Use Multi/Unit abutments to shift the mechanical fuse away from the bone level.
- The implant platform diameter has little mechanical influence on screw fatigue.
- The prosthetic platform diameter has a strong mechanical impact: expanded prosthetic emergence profiles are recommended to improve the mechanical performance of the restoration.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| IAC | Implant-Abutment Connection |
| FEM | Finite Element Method |
| FEA | Finite Element Analysis |
| DoF | Degrees of Freedom |
References
- Warreth, A.; Fesharaki, H.; McConville, R.; McReynolds, D. An Introduction to Single Implant Abutments. Dent. Update 2013, 40, 7–17. [Google Scholar] [CrossRef]
- Bickford, J.H. Introduction to the Design and Behavior of Bolted Joints, 4th ed.; CRC Press: New York, NY, USA, 2008. [Google Scholar]
- Stüker, R.A.; Teixeira, E.R.; Beck, J.C.P.; Da Costa, N.P. Preload and Torque Removal Evaluation of Three Different Abutment Screws for Single Standing Implant Restorations. J. Appl. Oral. Sci. 2008, 16, 55–58. [Google Scholar] [CrossRef]
- Barbosa, G.S.; da Silva-Neto, J.P.; Simamoto-Júnior, P.C.; das Neves, F.D.; da Gloria Chiarello de Mattos, M.; Ribeiro, R.F. Evaluation of Screw Loosening on New Abutment Screws and after Successive Tightening. Braz. Dent. J. 2011, 22, 51–55. [Google Scholar] [CrossRef]
- Lambrechts, T.; Doornewaard, R.; De Bruyckere, T.; Matthijs, L.; Deschepper, E.; Cosyn, J. A Multicenter Cohort Study on the Association of the One-Abutment One-Time Concept with Marginal Bone Loss around Bone Level Implants. Clin. Oral. Implant. Res. 2021, 32, 192–202. [Google Scholar] [CrossRef]
- Nicolás-Silvente, A.I.; Rivas-Pérez, A.; García-López, R.; Alemán-Marín, J.; Chiva-García, F.; Sánchez-Pérez, A. La Utilización de Pilares Transmucosos Definitivos de Colocación Inmediata. Av. Odontoestomatol. 2020, 36, 99–106. [Google Scholar] [CrossRef]
- Canullo, L.; Pesce, P.; Tronchi, M.; Fiorellini, J.; Amari, Y.; Penarrocha, D. Marginal Soft Tissue Stability around Conical Abutments Inserted with the One Abutment-One Time Protocol after 5 Years of Prosthetic Loading. Clin. Implant. Dent. Relat. Res. 2018, 20, 976–982. [Google Scholar] [CrossRef] [PubMed]
- Atieh, M.A.; Tawse-Smith, A.; Alsabeeha, N.H.M.; Ma, S.; Duncan, W.J. The One Abutment-One Time Protocol: A Systematic Review and Meta-Analysis. J. Periodontol. 2017, 88, 1173–1185. [Google Scholar] [CrossRef] [PubMed]
- Henao, P.; Queija, L.; Linder, S.; Dard, M.; González, A.; Carrión, J. Clinical and Radiographic Outcomes of a New Fully Tapered Implant with the One-Abutment One-Time Approach: In-Line Clinical Case Series with a 1-Year Follow-Up. Int. J. Oral. Maxillofac. Implant. 2023, 38, 943–953. [Google Scholar] [CrossRef]
- Pjetursson, B.; Asgeirsson, A.; Zwahlen, M.; Sailer, I. Improvements in Implant Dentistry over the Last Decade: Comparison of Survival and Complication Rates in Older and Newer Publications. Int. J. Oral. Maxillofac. Implant. 2014, 29, 308–324. [Google Scholar] [CrossRef]
- Dhima, M.; Paulusova, V.; Lohse, C.; Salinas, T.J.; Carr, A.B. Practice-Based Evidence from 29-Year Outcome Analysis of Management of the Edentulous Jaw Using Osseointegrated Dental Implants. J. Prosthodont. 2014, 23, 173–181. [Google Scholar] [CrossRef]
- Anitua, E.; Díez, P.T.; Velasco, J.P.; Larrazabal, N.; Armentia, M.; Seco-Calvo, J. Mechanical Behavior of Dental Restorations: A Finite Element Pilot Study of Implant-Supported vs. Multiunit-Supported Restorations. Prosthesis 2024, 6, 413–428. [Google Scholar] [CrossRef]
- Topkaya, H.; Kaman, M.O. Effect of Dental Implant Dimensions on Fatigue Behaviour: A Numerical Approach. Uludag Univ. J. Fac. Eng. 2018, 23, 249–260. [Google Scholar] [CrossRef]
- Anitua, E.; Tapia, R.; Luzuriaga, F.; Orive, G. Influence of Implant Length, Diameter, and Geometry on Stress Distribution: A Finite Element Analysis. Int. J. Periodontics Restor. Dent. 2010, 30, 89–95. [Google Scholar]
- Georgiopoulos, B.; Kalioras, K.; Provatidis, C.; Manda, M.; Koidis, P. The Effects of Implant Length and Diameter Prior to and after Osseointegration: A 2-D Finite Element Analysis. J. Oral. Implant. 2007, 33, 243–256. [Google Scholar] [CrossRef]
- Baggi, L.; Cappelloni, I.; Di Girolamo, M.; Maceri, F.; Vairo, G. The Influence of Implant Diameter and Length on Stress Distribution of Osseointegrated Implants Related to Crestal Bone Geometry: A Three-Dimensional Finite Element Analysis. J. Prosthet. Dent. 2008, 100, 422–431. [Google Scholar] [CrossRef]
- Santiago Junior, J.F.; Pellizzer, E.P.; Verri, F.R.; De Carvalho, P.S.P. Stress Analysis in Bone Tissue around Single Implants with Different Diameters and Veneering Materials: A 3-D Finite Element Study. Mater. Sci. Eng. C 2013, 3, 4700–4714. [Google Scholar] [CrossRef]
- Chang, S.H.; Lin, C.L.; Hsue, S.S.; Lin, Y.S.; Huang, S.R. Biomechanical Analysis of the Effects of Implant Diameter and Bone Quality in Short Implants Placed in the Atrophic Posterior Maxilla. Med. Eng. Phys. 2012, 34, 153–160. [Google Scholar] [CrossRef] [PubMed]
- Raaj, G.; Manimaran, P.; Kumar, C.; Sadan, D.; Abirami, M. Comparative Evaluation of Implant Designs: Influence of Diameter, Length, and Taper on Stress and Strain in the Mandibular Segment-A Three-Dimensional Finite Element Analysis. J. Pharm. Bioallied Sci. 2019, 16, 486–494. [Google Scholar] [CrossRef]
- Shemtov-Yona, K.; Rittel, D.; Machtei, E.E.; Levin, L.; Machtei, E.E.; Levin, L.; Machtei, E.E. Effect of Dental Implant Diameter on Fatigue Performance. Part I: Mechanical Behavior. Clin. Implant. Dent. Relat. Res. 2014, 16, 172–177. [Google Scholar] [CrossRef]
- Fan, H.; Gan, X.; Zhu, Z. Evaluation of Dental Implant Fatigue Performance under Loading Conditions in Two Kinds of Physiological Environment. Int. J. Clin. Exp. Med. 2017, 10, 6369–6377. [Google Scholar]
- Armentia, M.; Abasolo, M.; Coria, I.; Sainitier, N. Effect of the Geometry of Butt-Joint Implant-Supported Restorations on the Fatigue Life of Prosthetic Screws. J. Prosthet. Dent. 2022, 127, 477.e1–477.e9. [Google Scholar] [CrossRef] [PubMed]
- Ryu, H.S.; Namgung, C.; Lee, J.H.; Lim, Y.J. The Influence of Thread Geometry on Implant Osseointegration under Immediate Loading: A Literature Review. J. Adv. Prosthodont. 2014, 6, 547–554. [Google Scholar] [CrossRef] [PubMed]
- Khened, V.; Bhandarkar, S.; Dhatrak, P. Dental Implant Thread Profile Optimization Using Taguchi Approach. Mater. Today Proc. 2022, 62, 3344–3349. [Google Scholar] [CrossRef]
- Minatel, L.; Verri, F.R.; Kudo, G.A.H.; de Faria Almeida, D.A.; de Souza Batista, V.E.; Lemos, C.A.A.; Pellizzer, E.P.; Santiago, J.F. Effect of Different Types of Prosthetic Platforms on Stress-Distribution in Dental Implant-Supported Prostheses. Mater. Sci. Eng. C 2017, 71, 35–42. [Google Scholar] [CrossRef]
- Shadid, R.; Sadaqah, N.; Al-Omari, W.; Abu-Naba’a, L. Comparison between the Butt-Joint and Morse Taper Implant-Abutment Connection: A Literature Review. J. Implant. Adv. Clin. Dent. 2013, 5, 33–40. [Google Scholar]
- Mishra, S.K.; Chowdhary, R.; Kumari, S. Microleakage at the Different Implant Abutment Interface: A Systematic Review. J. Clin. Diagn. Res. 2017, 11, ZE10–ZE15. [Google Scholar] [CrossRef]
- Shafie, H.R.; White, B.A. Different Implant–Abutment Connections. In Clinical and Laboratory Manual of Dental Implant Abutments; Shafie, H.R., Ed.; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2014; pp. 33–46. [Google Scholar]
- Yamaguchi, S.; Yamanishi, Y.; Machado, L.S.; Matsumoto, S.; Tovar, N.; Coelho, P.G.; Thompson, V.P.; Imazato, S. In Vitro Fatigue Tests and in Silico Finite Element Analysis of Dental Implants with Different Fixture/Abutment Joint Types Using Computer-Aided Design Models. J. Prosthodont. Res. 2018, 62, 24–30. [Google Scholar] [CrossRef]
- Khraisat, A.; Stegaroiu, R.; Nomura, S.; Miyakawa, O. Fatigue Resistance of Two Implant/Abutment Joint Designs. J. Prosthet. Dent. 2002, 88, 604–610. [Google Scholar] [CrossRef]
- Fernández-Asián, I.; Martínez-González, Á.; Torres-Lagares, D.; Serrera-Figallo, M.-Á.; Gutiérrez-Pérez, J.-L. External Connection versus Internal Connection in Dental Implantology. A Mechanical in vitro Study. Metals 2019, 9, 1106. [Google Scholar] [CrossRef]
- ISO 14801:2007; Dentistry-Implants-Dynamic Fatigue Test for Endosseous Dental Implants. International Organization for Standardization: Geneva, Switzerland, 2007.
- Armentia, M.; Abasolo, M.; Coria, I.; Albizuri, J. Fatigue Design of Dental Implant Assemblies: A Nominal Stress Approach. Metals 2020, 10, 744. [Google Scholar] [CrossRef]
- Armentia, M.; Abasolo, M.; Coria, I.; Bouzid, A.-H. On the Use of a Simplified Slip Limit Equation to Predict Screw Self-Loosening of Dental Implants Subjected to External Cycling Loading. Appl. Sci. 2020, 10, 6748. [Google Scholar] [CrossRef]
- ASTM F67-13; Standard Specification for Unalloyed Titanium, for Surgical Implant Applications. ASTM International: West Conshohocken, PA, USA, 2017.
- ASTM F136; Standard Specification for Wrought Titanium-6Aluminum-4Vanadium ELI (Extra Low Interstitial) Alloy for Surgical Implant Applications. ASTM International: West Conshohocken, PA, USA, 2021.
- Walker, K. The Effect of Stress Ratio During Crack Propagation and Fatigue for 2024-T3 and 7075-T6 Aluminum. In Effects of Environment and Complex Load History on Fatigue Life; ASTM International: West Conshohocken, PA, USA, 2009. [Google Scholar]
- Dowling, N.E.; Calhoun, C.A.; Arcari, A. Mean Stress Effects in Stress-Life Fatigue and the Walker Equation. Fatigue Fract. Eng. Mater. Struct. 2009, 32, 163–179. [Google Scholar] [CrossRef]
- Pérez, M.A. Life Prediction of Different Commercial Dental Implants as Influence by Uncertainties in Their Fatigue Material Properties and Loading Conditions. Comput. Methods Programs Biomed. 2012, 108, 1277–1286. [Google Scholar] [CrossRef]
- Wang, R.R.; Fenton, A. Titanium for Prosthodontic Applications: A Review of the Literature. Quintessence Int. 1996, 27, 401–408. [Google Scholar] [PubMed]
- Elias, C.N.; Figueira, D.C.; Rios, P.R. Influence of the Coating Material on the Loosing of Dental Implant Abutment Screw Joints. Mater. Sci. Eng. C 2006, 26, 1361–1366. [Google Scholar] [CrossRef]
- Armentia, M.; Abasolo, M.; Coria, I.; Albizuri, J.; Aguirrebeitia, J. Fatigue Performance of Prosthetic Screws Used in Dental Implant Restorations: Rolled versus Cut Threads. J. Prosthet. Dent. 2021, 126, 406.e1–406.e8. [Google Scholar] [CrossRef] [PubMed]
- Nicolas-Silvente, A.I.; Velasco-Ortega, E.; Ortiz-Garcia, I.; Jimenez-Guerra, A.; Monsalve-Guil, L.; Ayuso-Montero, R.; Gil, J.; Lopez-Lopez, J. Influence of Connection Type and Platform Diameter on Titanium Dental Implants Fatigue: Non-Axial Loading Cyclic Test Analysis. Int. J. Environ. Res. Public. Health 2020, 17, 8988. [Google Scholar] [CrossRef]



| A | B | C | D | E | |
|---|---|---|---|---|---|
| Implant | IIPECA4075 | IIPECA4075 | IIPECA4075 | IIPUCA4075 | IIPUCA4075 |
| Body Ø (mm) | 4.0 | 4.0 | 4.0 | 4.0 | 4.0 |
| Implant platform Ø (mm) | 3.5 | 3.5 | 3.5 | 4.1 | 4.1 |
| Multi/Unit abutment | INTMIUPE3530 | INTMIUPE30 | INTMIUPEEX30 | INTMIUPU30 | INTMIUPUEX30 |
| Tightening torque (Ncm) | 35 | 35 | 35 | 35 | 35 |
| Prosthetic platform Ø (mm) * | 3.5 | 4.1 | 5.5 | 4.1 | 5.5 |
| Cylinder | CPMIUPE | CPMIUPU | CPMIUPA | CPMIUPU | CPMIUPA |
| Prosthetic screw | TTMIR | TTMIR | TTMIUPA | TTMIR | TTMIUPA |
| Screw metric | M1.4 | M1.4 | M1.8 | M1.4 | M1.8 |
| Tightening torque (Ncm) | 20 | 20 | 30 | 20 | 30 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Anitua, E.; Armentia, M.; Mallat, E.; Anitua, B. Fatigue Behavior of Multi/Unit-Supported Dental Restorations: Implant Platform vs. Prosthetic Platform. Dent. J. 2025, 13, 374. https://doi.org/10.3390/dj13080374
Anitua E, Armentia M, Mallat E, Anitua B. Fatigue Behavior of Multi/Unit-Supported Dental Restorations: Implant Platform vs. Prosthetic Platform. Dentistry Journal. 2025; 13(8):374. https://doi.org/10.3390/dj13080374
Chicago/Turabian StyleAnitua, Eduardo, Mikel Armentia, Ernest Mallat, and Beatriz Anitua. 2025. "Fatigue Behavior of Multi/Unit-Supported Dental Restorations: Implant Platform vs. Prosthetic Platform" Dentistry Journal 13, no. 8: 374. https://doi.org/10.3390/dj13080374
APA StyleAnitua, E., Armentia, M., Mallat, E., & Anitua, B. (2025). Fatigue Behavior of Multi/Unit-Supported Dental Restorations: Implant Platform vs. Prosthetic Platform. Dentistry Journal, 13(8), 374. https://doi.org/10.3390/dj13080374





