MIH and Cavities as Markers of Oral Health Inequality in Children from Southwest Andalusia (Spain)
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Participants
2.3. Variables
2.3.1. Dependent Variables
2.3.2. Independent Variables
2.3.3. Secondary Variables
2.4. Data Sources
2.5. Sample Size
2.6. Statistical Analysis
2.7. Ethical Considerations
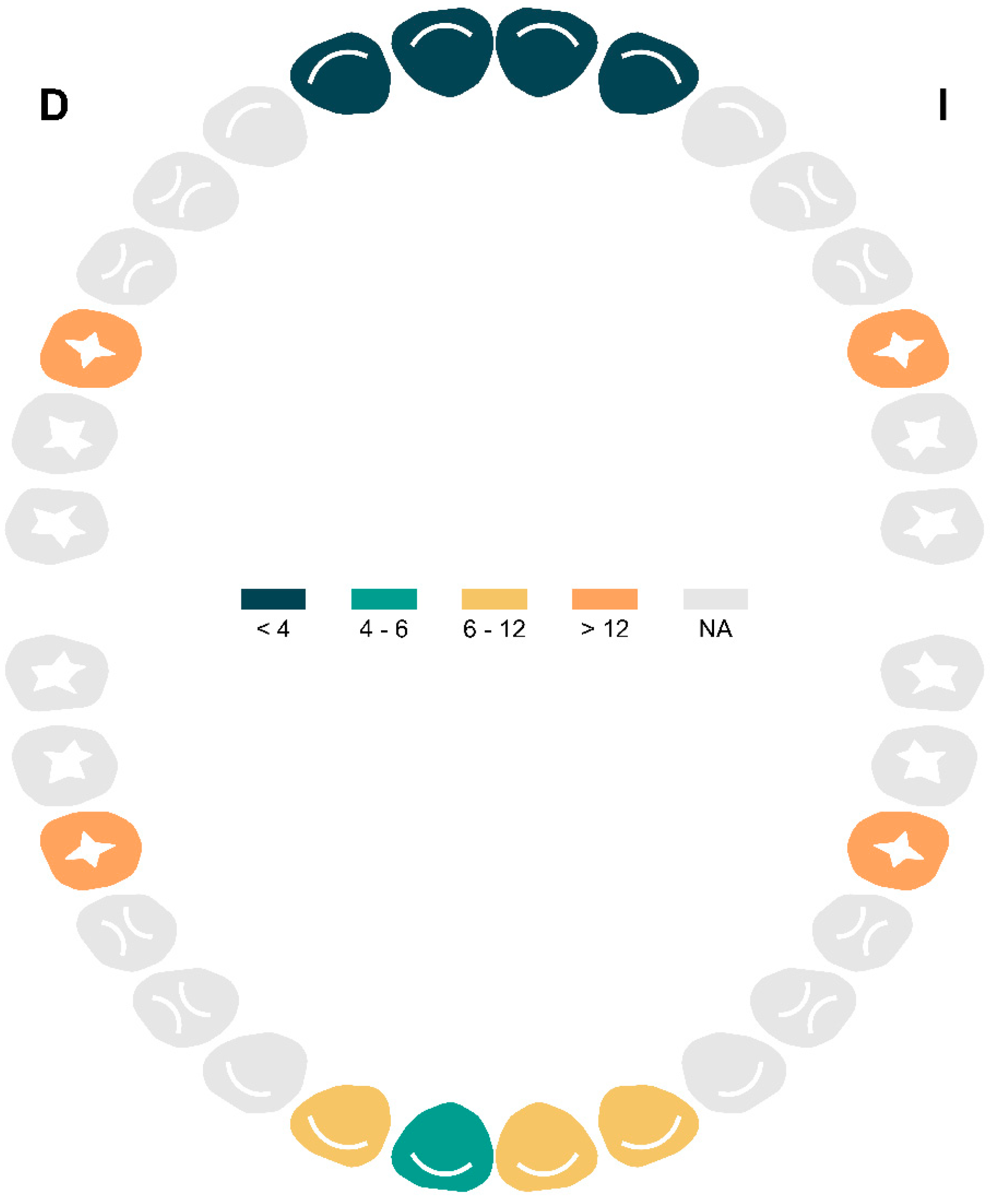
3. Results
3.1. Participant Characteristics
3.2. Prevalence of Caries and Associated Factors
3.3. Indices
3.4. Prevalence of MIH and Associated Factors
4. Discussion
4.1. Main Findings
4.2. Comparison with the Literature
4.3. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Krol, D.M.; Whelan, K.; Section on Oral Health. Maintaining and Improving the Oral Health of Young Children. Pediatrics 2023, 151, e2022060417. [Google Scholar] [CrossRef] [PubMed]
- Watt, S.; Dyer, T.A.; Marshman, Z.; Jones, K. Does poor oral health impact on young children’s development? A rapid review. Br. Dent. J. 2024, 237, 255–260. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Guarnizo-Herreño, C.C.; Wehby, G.L. Children’s dental health, school performance, and psychosocial well-being. J. Pediatr. 2012, 161, 1153–1159. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bravo Pérez, M.; Almerich Silla, J.; Canorea Díaz, E.; Casals Peidró, E.; Cortés Martinicorena, F.; Expósito Delgado, A.; Gómez Santos, G.; Hidalgo Olivares, G.; Lamas Oliveira, M.; Martínez Beneyto, Y.; et al. Encuesta de Salud Oral en España 2020. Rev. Del Iluestre Cons. Gen. Col. De Odontólogos Y Estomatólogos España 2020, 25, 1–35. [Google Scholar]
- Machiulskiene, V.; Campus, G.; Carvalho, J.C.; Dige, I.; Ekstrand, K.R.; Jablonski-Momeni, A.; Maltz, M.; Manton, D.J.; Martignon, S.; Martinez-Mier, E.A.; et al. Terminology of Dental Caries and Dental Caries Management: Consensus Report of a Workshop Organized by ORCA and Cariology Research Group of IADR. Caries Res. 2020, 54, 7–14. [Google Scholar] [CrossRef] [PubMed]
- Kirthiga, M.; Murugan, M.; Saikia, A.; Kirubakaran, R. Risk Factors for Early Childhood Caries: A Systematic Review and Meta-Analysis of Case Control and Cohort Studies. Pediatr. Dent. 2019, 41, 95–112. [Google Scholar] [PubMed] [PubMed Central]
- Lam, P.P.Y.; Chua, H.; Ekambaram, M.; Lo, E.C.M.; Yiu, C.K.Y. Risk predictors of early childhood caries increment-a systematic review and meta-analysis. J. Evid. Based Dent. Pract. 2022, 22, 101732. [Google Scholar] [CrossRef] [PubMed]
- Schwendicke, F.; Dörfer, C.E.; Schlattmann, P.; Foster Page, L.; Thomson, W.M.; Paris, S. Socioeconomic inequality and caries: A systematic review and meta-analysis. J. Dent. Res. 2015, 94, 10–18. [Google Scholar] [CrossRef] [PubMed]
- Ozsin Ozler, C.; Cocco, P.; Cakir, B. Dental caries and quality of life among preschool children: A hospital-based nested case-control study. Br. Dent. J. 2020. [Google Scholar] [CrossRef] [PubMed]
- Benelli, K.D.R.G.; Chaffee, B.W.; Kramer, P.F.; Knorst, J.K.; Ardenghi, T.M.; Feldens, C.A. Pattern of caries lesions and oral health-related quality of life throughout early childhood: A birth cohort study. Eur. J. Oral Sci. 2022, 130, e12889. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Fernandez, M.D.S.; Pauli, L.A.; da Costa, V.P.P.; Azevedo, M.S.; Goettems, M.L. Dental caries severity and oral health-related quality-of-life in Brazilian preschool children. Eur. J. Oral Sci. 2022, 130, e12836. [Google Scholar] [CrossRef] [PubMed]
- Lopes, L.B.; Machado, V.; Mascarenhas, P.; Mendes, J.J.; Botelho, J. The prevalence of molar-incisor hypomineralization: A systematic review and meta-analysis. Sci. Rep. 2021, 11, 22405. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Almuallem, Z.; Busuttil-Naudi, A. Molar incisor hypomineralisation (MIH)—An overview. Br. Dent. J. 2018, 225, 601–609. [Google Scholar] [CrossRef] [PubMed]
- Nisii, F.; Mazur, M.; De Nuccio, C.; Martucci, C.; Spuntarelli, M.; Labozzetta, S.; Fratini, A.; Sozzi, S.; Maruotti, A.; Vozza, I.; et al. Prevalence of molar incisor hypomineralization among school children in Rome, Italy. Sci. Rep. 2022, 12, 7343. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Al-Nerabieah, Z.; AlKhouli, M.; Dashash, M. Prevalence and clinical characteristics of molar-incisor hypomineralization in Syrian children: A cross-sectional study. Sci. Rep. 2023, 13, 8582. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Garcia-Margarit, M.; Catalá-Pizarro, M.; Montiel-Company, J.M.; Almerich-Silla, J.M. Epidemiologic study of molar-incisor hypomineralization in 8-year-old Spanish children. Int. J. Paediatr. Dent. 2014, 24, 14–22. [Google Scholar] [CrossRef] [PubMed]
- Hernández, M.; Boj, J.R.; Espasa, E.; Peretz, B. Prevalencija molarno-incizivne hipomineralizacije u skupini španjolske školske djece. Acta Stomatol. Croat. Int. J. Oral Sci. Dent. Med. 2018, 52, 4–11. Available online: https://cris.tau.ac.il/en/publications/prevalencija-molarno-incizivne-hipomineralizacije-u-%C5%A1kupini-%C5%A1panj (accessed on 25 May 2025). [CrossRef]
- Afzal, S.H.; Skaare, A.B.; Wigen, T.I.; Brusevold, I.J. Molar-Incisor Hypomineralisation: Severity, caries and hypersensitivity. J. Dent. 2024, 142, 104881. [Google Scholar] [CrossRef] [PubMed]
- Juárez-López, M.L.A.; Salazar-Treto, L.V.; Hernández-Monjaraz, B.; Molina-Frechero, N. Etiological Factors of Molar Incisor Hypomineralization: A Systematic Review and Meta-Analysis. Dent. J. 2023, 11, 111. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Jiménez Moreno, E. Salud Bucodental de la Cohorte de 6 años en Lebrija y El Cuervo: Prevalencia de la Hipoplasia Incisivo-Molar y Valoración del Grado de Satisfacción y Mejora de la Asistencia Dental Infantil; Universidad de Sevilla: Sevilla, Spain, 2015. [Google Scholar]
- Petersen, P.E.; Baez, R.; World Health Organization. Assessment of oral status. In Oral Health Surveys Basic Methods; World Health Organization: Geneva, Switzerland, 2013; p. 47. [Google Scholar]
- Lygidakis, N.A.; Garot, E.; Somani, C.; Taylor, G.D.; Rouas, P.; Wong, F.S.L. Best clinical practice guidance for clinicians dealing with children presenting with molar-incisor-hypomineralisation (MIH): An updated European Academy of Paediatric Dentistry policy document. Eur. Arch. Paediatr. Dent. 2022, 23, 3–21. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Riley, R.D.; Ensor, J.; Snell, K.I.E.; Harrell, F.E., Jr.; Martin, G.P.; Reitsma, J.B.; Moons, K.G.M.; Collins, G.; van Smeden, M. Calculating the sample size required for developing a clinical prediction model. BMJ 2020, 368, m441. [Google Scholar] [CrossRef] [PubMed]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2025. [Google Scholar]
- Blanco, L. Encuesta Poblacional: La Salud Bucodental en España 2020; Llodra Calvo, J.C., Ed.; Grupo ICM de Comunicación: Madrid, Spain, 2020. [Google Scholar]
- Bravo Pérez, M.; Cabrera León, A.; Llodra Calvo, J.C. V Estudio Epidemiológico de la Salud Bucodental Escolar en Andalucía. Andalucía. 2022. Available online: https://www.juntadeandalucia.es/export/drupaljda/v_estudio_epidemiologico_salud_oral_escolares_andaluces.pdf (accessed on 25 May 2025).
- Monteagudo, C.; Téllez, F.; Heras-González, L.; Ibañez-Peinado, D.; Mariscal-Arcas, M.; Olea-Serrano, F. Hábitos dietéticos de los escolares e incidencia de caries dental. Nutr. Hosp. 2015, 32, 383–388. Available online: https://pubmed.ncbi.nlm.nih.gov/26262743/ (accessed on 25 May 2025).
- Portero de la Cruz, S.; Cebrino, J. Oral Health Problems and Utilization of Dental Services Among Spanish and Immigrant Children and Adolescents. Int. J. Environ. Res. Public. Health 2020, 17, 738. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Almerich-Silla, J.M.; Montiel-Company, J.M. Influence of immigration and other factors on caries in 12- and 15-yr-old children. Eur. J. Oral Sci. 2007, 115, 378–383. [Google Scholar] [CrossRef] [PubMed]
- Silla, J.M.A.; Montiel Company, J.M. Oral health survey of the child population in the Valencia Region of Spain (2004). Med. Oral Patol. Oral Cir. Bucal 2006, 11, E369–E381. [Google Scholar]
- Ribas-Pérez, D.; Sevillano Garcés, D.; Rodriguez Menacho, D.; Hernandez-Franch, P.V.; Barbero Navarro, I.; Castaño Séiquer, A. Cross-Sectional Study on Oral Health-Related Quality of Life Using OHIP-14 in Migrants Children in Melilla (Spain). Children 2023, 10, 1168. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Banihashem Rad, S.A.; Esteves-Oliveira, M.; Maklennan, A.; Douglas, G.V.A.; Castiglia, P.; Campus, G. Oral health inequalities in immigrant populations worldwide: A scoping review of dental caries and periodontal disease prevalence. BMC Public Health 2024, 24, 1968. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Esteban-Gonzalo, L.; Veiga, O.L.; Gómez-Martínez, S.; Regidor, E.; Martínez, D.; Marcos, A.; Calle, M.E. Adherence to dietary recommendations among Spanish and immigrant adolescents living in Spain; the AFINOS study. Nutr. Hosp. 2013, 28, 1926–1936. [Google Scholar] [PubMed]
- Kizi, G.; Raquel Barata, A.; Ventura, I.; Flores-Fraile, J.; Ribas-Perez, D.; Castaño-Seiquer, A. Oral Health in migrants children in Melilla, Spain. Children 2023, 10, 888. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wu, Y.; Li, G.; Lyu, C.H.; Zhou, N.; Wong, H.M. Oral microbiota in preschoolers with rampant caries: A matched case-control study. Appl. Microbiol. Biotechnol. 2024, 108, 533. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Skeie, M.S.; Riordan, P.J.; Klock, K.S.; Espelid, I. Parental risk attitudes and caries-related behaviours among immigrant and western native children in Oslo. Community Dent. Oral Epidemiol. 2006, 34, 103–113. [Google Scholar] [CrossRef] [PubMed]
- Oreano, M.D.; Santos, P.S.; Borgatto, A.F.; Bolan, M.; Cardoso, M. Association between dental caries and molar-incisor hypomineralisation in first permanent molars: A hierarchical model. Community Dent. Oral Epidemiol. 2023, 51, 436–442. [Google Scholar] [CrossRef] [PubMed]
- Gevert, M.V.; Wambier, L.M.; Ito, L.Y.; Feltrin de Souza, J.; Chibinski, A.C.R. Which are the clinical consequences of Molar Incisor hypomineralization (MIH) in children and adolescents? Systematic review and meta-analysis. Clin. Oral Investig. 2024, 28, 415. [Google Scholar] [CrossRef] [PubMed]
- Americano, G.C.; Jacobsen, P.E.; Soviero, V.M.; Haubek, D. A systematic review on the association between molar incisor hypomineralization and dental caries. Int. J. Paediatr. Dent. 2017, 27, 11–21. [Google Scholar] [CrossRef] [PubMed]
- Ortega-Luengo, S.; Feijóo-Garcia, G.; Miegimolle-Herrero, M.; Gallardo-López, N.E.; Caleya-Zambrano, A.M. Prevalence and clinical presentation of molar incisor hypomineralisation among a population of children in the community of Madrid. BMC Oral Health 2024, 24, 229. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Cots, E.; Casas, M.; Gregoriano, M.; Busquet-Dura, X.; Bielsa, J.; Chacon, C.; Kragt, L.; Torán, P.; Guinot, F. Ethnic disparities in the prevalence of Molar-Incisor-Hypomineralisation (MIH) and caries among 6–12-year-old children in Catalonia, Spain. Eur. J. Paediatr. Dent. 2024, 25, 188–199. [Google Scholar] [CrossRef] [PubMed]
- Franco, M.M.P.; Ribeiro, C.C.C.; Ladeira, L.L.C.; Thomaz, E.B.A.F.; Alves, C.M.C. Pre- and perinatal exposures associated with molar incisor hypomineralization: Birth cohort, Brazil. Oral Dis. 2024, 30, 3431–3439. [Google Scholar] [CrossRef] [PubMed]
- Silva, M.J.; Scurrah, K.J.; Craig, J.M.; Manton, D.J.; Kilpatrick, N. Etiology of molar incisor hypomineralization-A systematic review. Community Dent. Oral Epidemiol. 2016, 44, 342–353. [Google Scholar] [CrossRef] [PubMed]

| Variable | 6 Years n = 200 1 | 7 Years n = 29 1 | Total n = 229 1 |
|---|---|---|---|
| Gender | |||
| Female | 90 (45.0%) | 16 (55.2%) | 106 (46.3%) |
| Male | 110 (55.0%) | 13 (44.8%) | 123 (53.7%) |
| Municipality | |||
| Mazagón | 40 (20.0%) | 4 (13.8%) | 44 (19.2%) |
| Palos de la Frontera | 107 (53.5%) | 18 (62.1%) | 125 (54.6%) |
| San Bartolomé | 53 (26.5%) | 7 (24.1%) | 60 (26.2%) |
| Parental Origin | |||
| Spain | 148 (74.0%) | 21 (72.4%) | 169 (73.8%) |
| Europe | 14 (7.0%) | 2 (6.9%) | 16 (7.0%) |
| Africa | 34 (17.0%) | 5 (17.2%) | 39 (17.0%) |
| America | 4 (2.0%) | 1 (3.4%) | 5 (2.2%) |
| Weight (kg) | |||
| Min–Max | 15.7–67.5 | 20.1–33.0 | 15.7–67.5 |
| Mean (SD) | 24.5 (6.0) | 24.1 (3.5) | 24.5 (5.7) |
| Height (cm) | |||
| Min–Max | 105.0–138.0 | 118.0–139.0 | 105.0–139.0 |
| Mean (SD) | 122.6 (4.8) | 122.9 (4.4) | 122.6 (4.7) |
| BMI kg/m2 | |||
| Min–Max | 11.8–37.0 | 13.0–20.2 | 11.8–37.0 |
| Mean (SD) | 16.2 (3.1) | 16.0 (1.8) | 16.2 (3.0) |
| Median (Q1–Q3) | 15.5 (14.5–17.2) | 16.0 (14.7–16.9) | 15.6 (14.5–17.1) |
| Category BMI | |||
| Severe Malnutrition | 3 (1.5%) | 1 (3.4%) | 4 (1.7%) |
| Moderate Malnutrition | 7 (3.5%) | 1 (3.4%) | 8 (3.5%) |
| Normal Weight | 157 (78.5%) | 23 (79.3%) | 180 (78.6%) |
| Overweight | 19 (9.5%) | 4 (13.8%) | 23 (10.0%) |
| Obesity | 14 (7.0%) | 0 (0.0%) | 14 (6.1%) |
| Variable | Dft Index | p-Value 2 | |
|---|---|---|---|
| Dft = 0 n = 107 1 | Dft ≥ 1 n = 122 1 | ||
| Gender | 0.235 | ||
| Females | 54 (50.5%) | 52 (42.6%) | |
| Males | 53 (49.5%) | 70 (57.4%) | |
| Parental Origin | <0.001 | ||
| Spain | 96 (89.7%) | 73 (59.8%) | |
| Europe | 3 (2.8%) | 13 (10.7%) | |
| Africa | 5 (4.7%) | 34 (27.9%) | |
| America | 3 (2.8%) | 2 (1.6%) | |
| Municipality | 0.145 | ||
| Mazagón | 26 (24.3%) | 18 (14.8%) | |
| Palos de la Frontera | 57 (53.3%) | 68 (55.7%) | |
| San Bartolomé | 24 (22.4%) | 36 (29.5%) | |
| Weight, kg | 23.4 (21.0, 25.5) | 23.0 (21.5, 26.0) | 0.902 |
| Height, cm | 122.0 (119.5, 125.0) | 121.0 (120.0, 124.5) | 0.429 |
| BMI, kg/m2 | 15.32 (14.55, 16.92) | 15.66 (14.33, 17.24) | 0.997 |
| Oral Hygiene | <0.001 | ||
| Good | 51 (47.7%) | 22 (18.0%) | |
| Poor | 56 (52.3%) | 100 (82.0%) | |
| MIH | <0.001 | ||
| Healthy | 88 (82.2%) | 69 (56.6%) | |
| Present | 19 (17.8%) | 53 (43.4%) | |
| Variable | Univariate Analysis | Multivariate Analysis | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p-Value | OR | 95% CI | p-Value | |
| Gender | ||||||
| Females | — | — | — | — | ||
| Males | 1.37 | 0.81, 2.32 | 0.235 | 1.29 | 0.70, 2.38 | 0.415 |
| Parental Origin | ||||||
| Spain | — | — | — | — | ||
| Europe | 5.70 | 1.76, 25.5 | 0.008 | 4.56 | 1.26, 22.3 | 0.033 |
| Africa | 8.94 | 3.62, 27.1 | <0.001 | 7.47 | 2.84, 23.8 | <0.001 |
| America | 0.88 | 0.11, 5.42 | 0.887 | 1.01 | 0.12, 7.49 | 0.992 |
| Municipality | ||||||
| Mazagón | — | — | — | — | ||
| Palos de la Frontera | 1.72 | 0.86, 3.50 | 0.126 | 2.09 | 0.93, 4.87 | 0.079 |
| San Bartolomé | 2.17 | 0.99, 4.85 | 0.056 | 2.46 | 0.98, 6.38 | 0.059 |
| Oral Hygiene | ||||||
| Good | — | — | — | — | ||
| Poor | 4.14 | 2.30, 7.64 | <0.001 | 3.07 | 1.60, 6.03 | <0.001 |
| MIH | ||||||
| Healthy | — | — | — | — | ||
| Present | 3.56 | 1.96, 6.68 | <0.001 | 3.20 | 1.64, 6.42 | <0.001 |
| Decayed | Missing | Filled | Total (IC 95%) | |
|---|---|---|---|---|
| dft | 369 | - | 39 | 1.78 (1.65, 1.95) |
| DMFT | 62 | 0 | 8 | 0.31 (0.23, 0.38) |
| MIH | p-Value 2 | ||
|---|---|---|---|
| Healthy n = 157 1 | Present n = 72 1 | ||
| Gender | 0.446 | ||
| Females | 70 (44.6%) | 36 (50.0%) | |
| Males | 87 (55.4%) | 36 (50.0%) | |
| Parental Origin | 0.430 | ||
| Spain | 120 (76.4%) | 49 (68.1%) | |
| Europe | 9 (5.7%) | 7 (9.7%) | |
| Africa | 24 (15.3%) | 15 (20.8%) | |
| America | 4 (2.5%) | 1 (1.4%) | |
| Municipality | 0.066 | ||
| Mazagón | 35 (22.3%) | 9 (12.5%) | |
| Palos de la Frontera | 87 (55.4%) | 38 (52.8%) | |
| San Bartolomé | 35 (22.3%) | 25 (34.7%) | |
| Weight, kg | 23.2 (21.0, 26.7) | 23.5 (22.1, 24.8) | 0.424 |
| Height, cm | 121.0 (119.5, 125.0) | 122.0 (120.0, 125.0) | 0.404 |
| BMI, kg/m2 | 15.35 (14.51, 17.16) | 15.89 (14.48, 16.67) | 0.633 |
| Oral Hygiene | 0.069 | ||
| Good | 56 (35.7%) | 17 (23.6%) | |
| Poor | 101 (64.3%) | 55 (76.4%) | |
| Univariate Analysis | Multivariate Analysis | |||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p-Value | OR | 95% CI | p-Value | |
| Province Municipality | ||||||
| Mazagón | — | — | — | — | ||
| Palos de la Frontera | 1.70 | 0.77, 4.07 | 0.209 | 1.81 | 0.81, 4.38 | 0.161 |
| San Bartolomé | 2.78 | 1.17, 7.08 | 0.025 | 2.90 | 1.21, 7.45 | 0.021 |
| Oral Hygiene | ||||||
| Good | — | — | — | — | ||
| Poor | 1.79 | 0.97, 3.45 | 0.071 | 1.85 | 0.99, 3.60 | 0.060 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bech Barcaz, L.; Ribas-Pérez, D.; Villalva Hernandez-Franch, P.; El Khoury-Moreno, L.; Torrejón-Martínez, J.; Castaño-Séiquer, A. MIH and Cavities as Markers of Oral Health Inequality in Children from Southwest Andalusia (Spain). Dent. J. 2025, 13, 345. https://doi.org/10.3390/dj13080345
Bech Barcaz L, Ribas-Pérez D, Villalva Hernandez-Franch P, El Khoury-Moreno L, Torrejón-Martínez J, Castaño-Séiquer A. MIH and Cavities as Markers of Oral Health Inequality in Children from Southwest Andalusia (Spain). Dentistry Journal. 2025; 13(8):345. https://doi.org/10.3390/dj13080345
Chicago/Turabian StyleBech Barcaz, Leidy, David Ribas-Pérez, Paloma Villalva Hernandez-Franch, Luis El Khoury-Moreno, Julio Torrejón-Martínez, and Antonio Castaño-Séiquer. 2025. "MIH and Cavities as Markers of Oral Health Inequality in Children from Southwest Andalusia (Spain)" Dentistry Journal 13, no. 8: 345. https://doi.org/10.3390/dj13080345
APA StyleBech Barcaz, L., Ribas-Pérez, D., Villalva Hernandez-Franch, P., El Khoury-Moreno, L., Torrejón-Martínez, J., & Castaño-Séiquer, A. (2025). MIH and Cavities as Markers of Oral Health Inequality in Children from Southwest Andalusia (Spain). Dentistry Journal, 13(8), 345. https://doi.org/10.3390/dj13080345







