Bonding Orthodontic Attachments to 3D-Printed Photosensitive Definitive Resin: An In Vitro Study
Abstract
1. Introduction
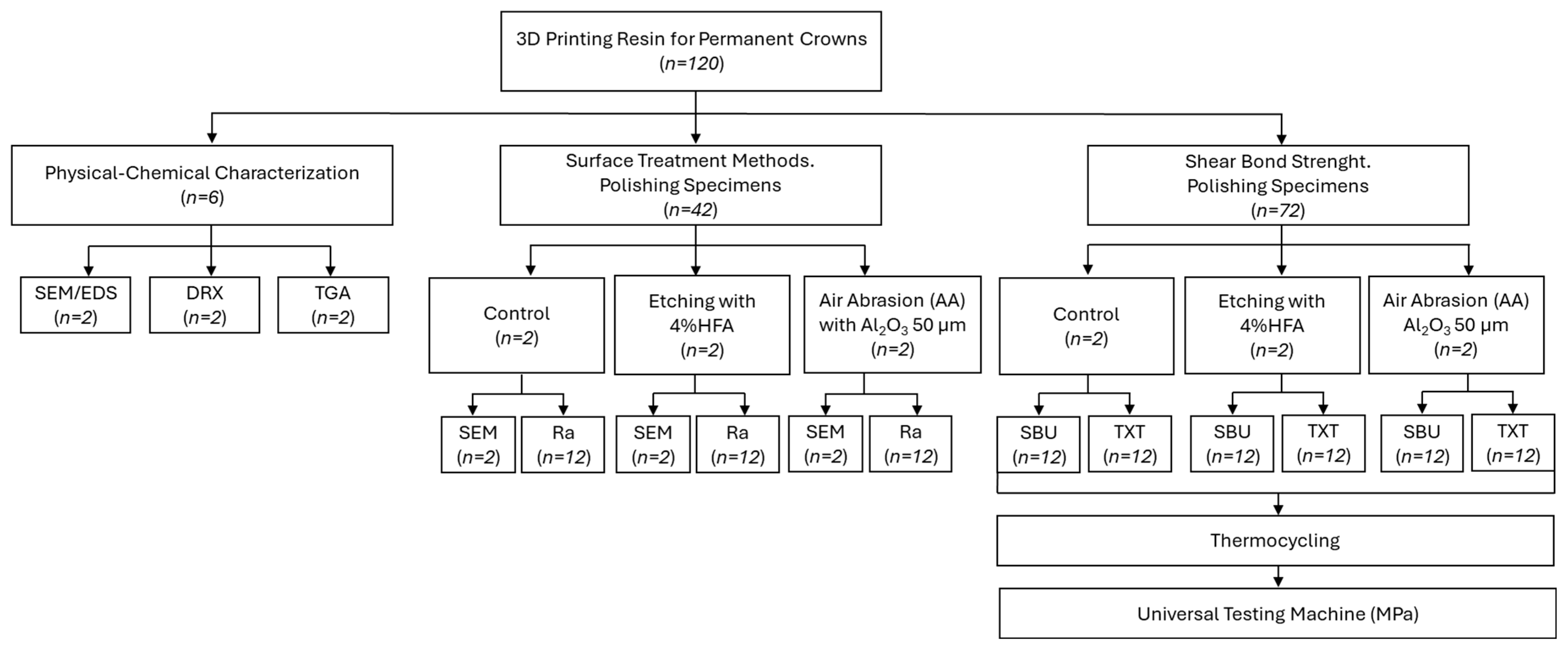
2. Materials and Methods
2.1. Materials Used In Vitro Study
2.2. Preparation of 3D Printed Samples
2.3. Physical–Chemical Characterization
2.3.1. Scanning Electron Microscopy and Energy-Dispersive X-Ray Spectroscopy (SEM/EDS)
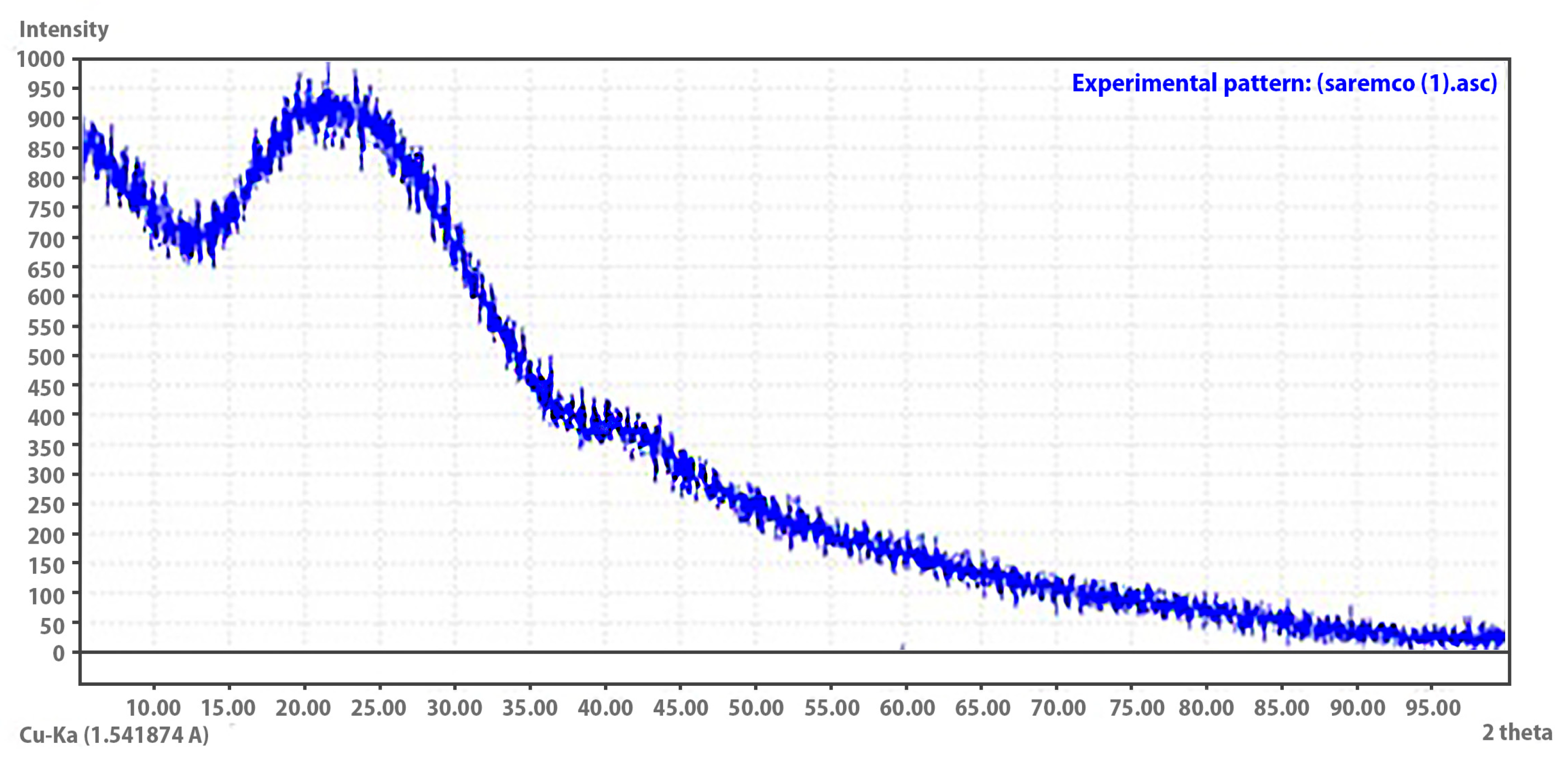
2.3.2. X-Ray Diffraction (XRD)
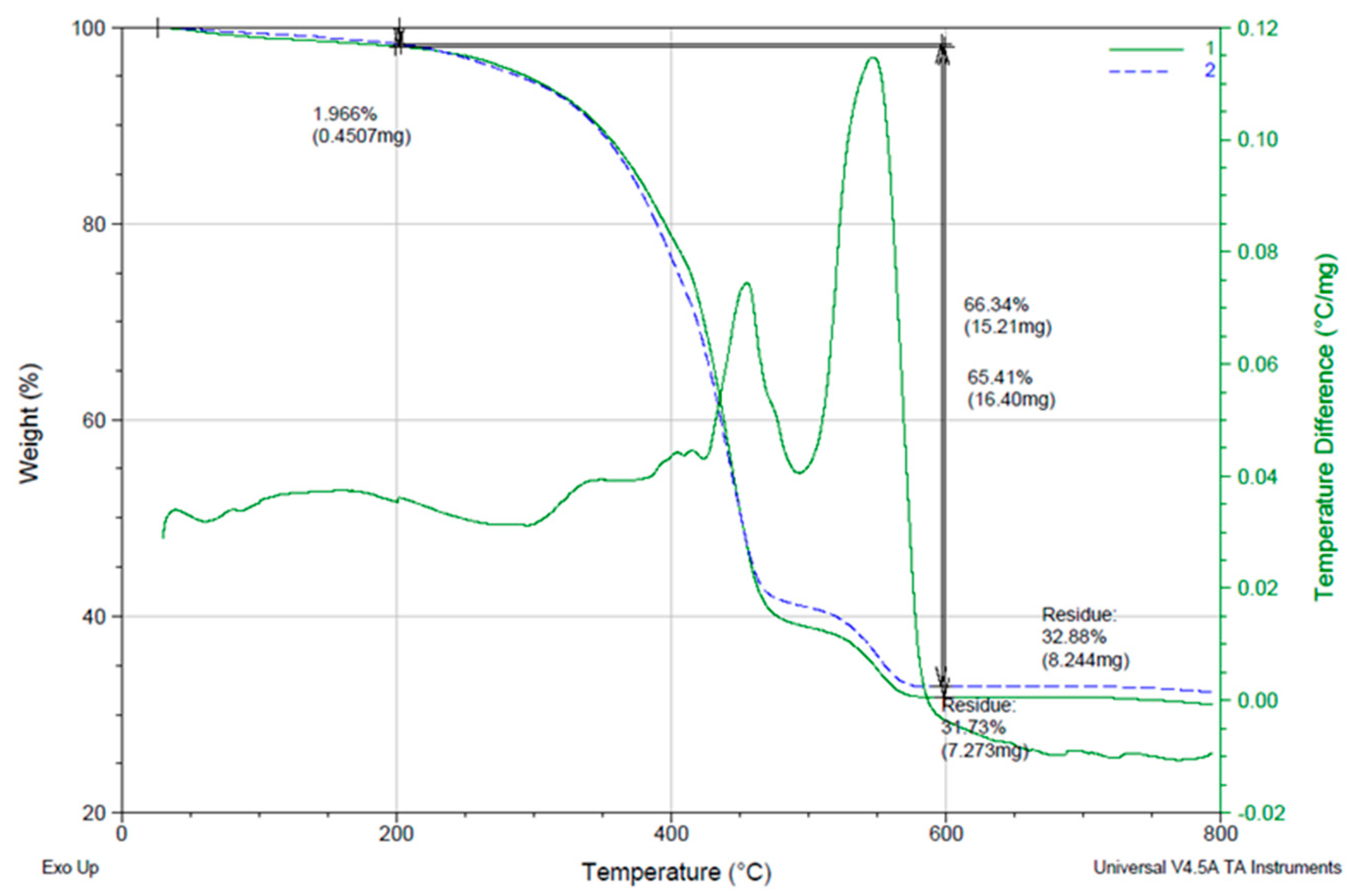
2.3.3. Thermogravimetric Analysis (TGA)
2.4. Surface Treatment Methods—Surface Morphology and Surface Roughness (Ra)
2.5. Shear Bond Strength (SBS) Test
2.5.1. Attachment Fabrication
2.5.2. Preparation and Grouping of Specimens
- TXT—TransbondTM XT Light Cure Adhesive Primer (3MTM UnitekTM—Mexico City, Mexico).
- SBU—Single BondTM Universal Adhesive (3MTM ESPETM—Mexico City, Mexico).
2.5.3. Thermocycling and Mechanical Testing
2.6. Statistical Analysis
3. Results
3.1. Physical–Chemical Characterization
3.1.1. Surface Morphology and Elemental Composition (SEM/EDS)
3.1.2. Crystalline Structure Analysis (XRD)
3.1.3. Thermal Stability and Composition (TGA)
3.2. Surface Treatment Methods
3.2.1. Surface Morphology (SEM Analysis)
3.2.2. Surface Roughness Analysis (Ra Values)
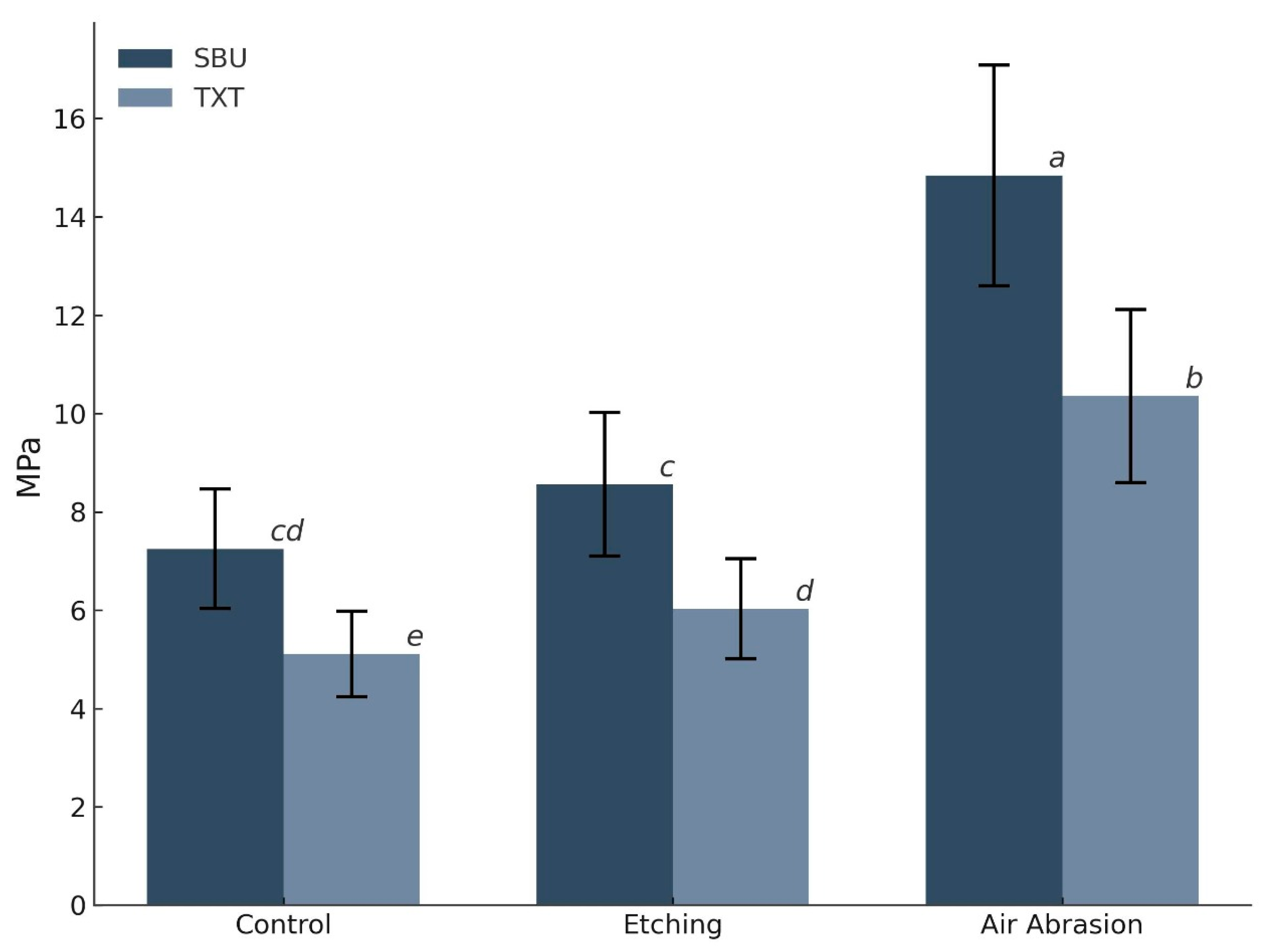
3.3. Shear Bond Strength (SBS) Analysis
4. Discussion
5. Conclusions
- The tested 3D printed definitive resin (Crowntec) demonstrated a hybrid structure composed of an amorphous polymer matrix reinforced with approximately 33% inorganic fillers, as confirmed by EDS, XRD and TGA analyses.
- Among the evaluated protocols, airborne particle abrasion with 50 µm Al2O3 followed by the application of a universal adhesive (containing 10-MDP and silane) achieved the highest shear bond strength, exceeding clinically accepted thresholds for orthodontic retention.
- Polished, untreated resin surfaces exhibited inadequate adhesion for clinical use, highlighting the need for substrate pretreatment in aligner-based orthodontic workflows.
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tian, Y.; Chen, C.; Xu, X.; Wang, J.; Hou, X.; Li, K.; Lu, X.; Shi, H.; Lee, E.-S.; Jiang, H.B.; et al. A Review of 3D Printing in Dentistry: Technologies, Affecting Factors, and Applications. Scanning 2021, 2021, 9950131. [Google Scholar] [CrossRef] [PubMed]
- Alharbi, N.; Wismeijer, D.; Osman, R. Additive Manufacturing Techniques in Prosthodontics: Where Do We Currently Stand? A Critical Review. Int. J. Prosthodont. 2017, 30, 474–484. [Google Scholar] [CrossRef] [PubMed]
- Revilla-León, M.; Özcan, M. Additive Manufacturing Technologies Used for Processing Polymers: Current Status and Potential Application in Prosthetic Dentistry. J. Prosthodont. 2019, 28, 146–158. [Google Scholar] [CrossRef] [PubMed]
- Diken Türksayar, A.A.; Demirel, M.; Donmez, M.B.; Olcay, E.O.; Eyüboğlu, T.F.; Özcan, M. Comparison of wear and fracture resistance of additively and subtractively manufactured screw-retained, implant-supported crowns. J. Prosthet. Dent. 2024, 132, 154–164. Available online: https://www.thejpd.org/action/showFullText?pii=S0022391323004183 (accessed on 26 February 2025). [CrossRef] [PubMed]
- Prause, E.; Malgaj, T.; Kocjan, A.; Beuer, F.; Hey, J.; Jevnikar, P.; Schmidt, F. Mechanical properties of 3D-printed and milled composite resins for definitive restorations: An in vitro comparison of initial strength and fatigue behavior. J. Esthet. Restor. Dent. 2024, 36, 391–401. [Google Scholar] [CrossRef] [PubMed]
- Daher, R.; Ardu, S.; di Bella, E.; Krejci, I.; Duc, O. Efficiency of 3D printed composite resin restorations compared with subtractive materials: Evaluation of fatigue behavior, cost, and time of production. J. Prosthet. Dent. 2024, 131, 943–950. [Google Scholar] [CrossRef] [PubMed]
- Alhotan, A.; Fouda, A.M.; Al-Johani, H.; Yoon, H.I.; Matinlinna, J.P. Physical and mechanical properties of various resins for additively manufactured definitive fixed dental restorations: Effect of material type and thermal cycling. J. Prosthet. Dent. 2025, 134, 238.e1–238.e8. [Google Scholar] [CrossRef] [PubMed]
- Donmez, M.B.; Okutan, Y. Marginal gap and fracture resistance of implant-supported 3D-printed definitive composite crowns: An in vitro study. J. Dent. 2022, 124, 104216. [Google Scholar] [CrossRef] [PubMed]
- Çakmak, G.; Rusa, A.M.; Borga Donmez, M.; Akay, C.; Gdem Kahveci, Ç.; Schimmel, M.; Yilmaz, B. Trueness of crowns fabricated by using additively and subtractively manufactured resin-based CAD-CAM materials. J. Prosthet. Dent. 2024, 131, 951–958. [Google Scholar] [CrossRef] [PubMed]
- Çakmak, G.; Donmez, M.B.; Molinero-Mourelle, P.; Kahveci, Ç.; Abou-Ayash, S.; Peutzfeldt, A.; Yilmaz, B. Fracture resistance of additively or subtractively manufactured resin-based definitive crowns: Effect of restorative material, resin cement, and cyclic loading. Dent. Mater. 2024, 40, 1072–1077. [Google Scholar] [CrossRef] [PubMed]
- Küçükekenci, A.S.; Dönmez, M.B.; Dede, D.Ö.; Çakmak, G.; Yilmaz, B. Bond strength of recently introduced computer-aided design and computer-aided manufacturing resin-based crown materials to polyetheretherketone and titanium. J. Prosthet. Dent. 2024, 132, 1066.e1–1066.e8. [Google Scholar] [CrossRef] [PubMed]
- Donmez, M.B.; Çakmak, G.; Yılmaz, D.; Schimmel, M.; Abou-Ayash, S.; Yilmaz, B.; Peutzfeldt, A. Bond strength of additively manufactured composite resins to dentin and titanium when bonded with dual-polymerizing resin cements. J. Prosthet. Dent. 2023, 132, 1067.e1–1067.e8. [Google Scholar] [CrossRef] [PubMed]
- Kang, Y.J.; Park, Y.; Shin, Y.; Kim, J.H. Effect of Adhesion Conditions on the Shear Bond Strength of 3D Printing Resins after Thermocycling Used for Definitive Prosthesis. Polymers 2023, 15, 1390. [Google Scholar] [CrossRef] [PubMed]
- Di Fiore, A.; Stellini, E.; Alageel, O.; Alhotan, A. Comparison of mechanical and surface properties of two 3D printed composite resins for definitive restoration. J. Prosthet. Dent. 2024, 132, 839.e1–839.e7. Available online: https://www.sciencedirect.com/science/article/abs/pii/S0022391324004529 (accessed on 23 April 2025). [CrossRef] [PubMed]
- Mao, Z.; Schmidt, F.; Beuer, F.; Yassine, J.; Hey, J.; Prause, E. Effect of surface treatment strategies on bond strength of additively and subtractively manufactured hybrid materials for permanent crowns. Clin. Oral. Investig. 2024, 28, 371. [Google Scholar] [CrossRef] [PubMed]
- Shahin, S.Y.; AlQahtani, N.; Abushowmi, T.H.; Siddiqui, I.A.; Akhtar, S.; Nassar, E.A.; Gad, M.M. The effect of surface treatment and thermal aging on the bonding of clear aligner attachments to provisional resin-based material: Shear bond strength analysis. Front. Oral Health 2024, 5, 1449833. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.; Qian, L.; Qian, Y.; Zhang, Z.; Wen, X. Comparative study of three composite materials in bonding attachments for clear aligners. Orthod. Craniofac Res. 2021, 24, 520–527. [Google Scholar] [CrossRef] [PubMed]
- Alsaud, B.A.; Hajjaj, M.S.; Masoud, A.I.; Abou Neel, E.A.; Abuelenain, D.A.; Linjawi, A.I. Bonding of Clear Aligner Composite Attachments to Ceramic Materials: An In Vitro Study. Materials 2022, 15, 4145. [Google Scholar] [CrossRef] [PubMed]
- Biadsee, A.; Rosner, O.; Khalil, C.; Atanasova, V.; Blushtein, J.; Levartovsky, S. Comparative evaluation of shear bond strength of orthodontic brackets bonded to three-dimensionally-printed and milled materials after surface treatment and artificial aging. Korean J. Orthod. 2023, 53, 45–53. [Google Scholar] [CrossRef] [PubMed]
- Bichu, Y.M.; Alwafi, A.; Liu, X.; Andrews, J.; Ludwig, B.; Bichu, A.Y.; Zou, B. Advances in orthodontic clear aligner materials. Bioact. Mater. 2023, 22, 384–403. [Google Scholar] [CrossRef] [PubMed]
- Weir, T. Clear aligners in orthodontic treatment. Aust. Dent. J. 2017, 62, 58–62. [Google Scholar] [CrossRef] [PubMed]
- Jedliński, M.; Mazur, M.; Greco, M.; Belfus, J.; Grocholewicz, K.; Janiszewska-Olszowska, J. Attachments for the Orthodontic Aligner Treatment—State of the Art—A Comprehensive Systematic Review. Int. J. Environ. Res. Public Health 2023, 20, 4481. [Google Scholar] [CrossRef] [PubMed]
- Jindal, P.; Juneja, M.; Siena, F.L.; Bajaj, D.; Breedon, P. Mechanical and geometric properties of thermoformed and 3D printed clear dental aligners. Am. J. Orthod. Dentofac. Orthop. 2019, 156, 694–701. [Google Scholar] [CrossRef] [PubMed]
- Çokakoğlu, S.; Nalçacı, R.; Altıntaş, S.H.; Atıcı, F. Can a Self-etching Primer be Effective in Bonding Aligner Attachments to Different Types of Ceramics? Turk. J. Orthod. 2024, 37, 30–35. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, T.; Fareen, N.; Alam, M.K. The effect of surface treatment and thermocycling on the shear bond strength of orthodontic brackets to the Y-TZP zirconia ceramics: A systematic review. Dental Press. J. Orthod. 2021, 26, 212118. [Google Scholar] [CrossRef] [PubMed]
- Alqerban, A. Lithium di silicate ceramic surface treated with Er,Cr:YSGG and other conditioning regimes bonded to orthodontic bracket. Saudi Dent. J. 2021, 33, 188–193. [Google Scholar] [CrossRef] [PubMed]
- Bourgi, R.; Kharouf, N.; Cuevas-Suárez, C.E.; Lukomska-Szymanska, M.; Haikel, Y.; Hardan, L. A Literature Review of Adhesive Systems in Dentistry: Key Components and Their Clinical Applications. Appl. Sci. 2024, 14, 8111. [Google Scholar] [CrossRef]
- Yu, J.; Zhang, Z.; Yang, H.; Wang, Y.; Muhetaer, A.; Lei, J.; Huang, C. Effect of universal adhesive and silane pretreatment on bond durability of metal brackets to dental glass ceramics. Eur. J. Oral. Sci. 2021, 129, e12772. [Google Scholar] [CrossRef] [PubMed]
- Niknam, O.; Shamohammadi, M.; Ataei, Z.; Rakhshan, V. Combined Effects of Different Bracket Bonding Adhesives and Different Resin Removal Methods on Enamel Discoloration: A Preliminary Study. Int. J. Dent. 2023, 2023, 8838264. [Google Scholar] [CrossRef] [PubMed]
- Lima, R.B.W.; de Araújo Ferreira Muniz, I.; Campos, D.E.S.; Murillo-Gómez, F.; de Andrade, A.K.M.; Duarte, R.M.; de Souza, G.M. Effect of universal adhesives and self-etch ceramic primers on bond strength to glass-ceramics: A systematic review and meta-analysis of in vitro studies. J. Prosthet. Dent. 2024, 131, 392–402. Available online: https://www.sciencedirect.com/science/article/abs/pii/S0022391322000555 (accessed on 23 April 2025). [CrossRef] [PubMed]
- Kutalmıs Buyuk, S.; Kucukekenci, A.S. Effects of different etching methods and bonding procedures on shear bond strength of orthodontic metal brackets applied to different CAD/CAM ceramic materials. Angle Orthod. 2018, 88, 221–226. [Google Scholar] [CrossRef] [PubMed]
- Pédemay, C.; François, P.; Fouquet, V.; Abdel-Gawad, S.; Attal, J.P.; Dantagnan, C.A. Shear bond strength and ARI scores of metal brackets to glazed glass ceramics and zirconia: An in vitro study investigating surface treatment protocols. BMC Oral Health 2024, 24, 1567. [Google Scholar] [CrossRef] [PubMed]
- Farkas, A.Z.; Galatanu, S.V.; Nagib, R. The Influence of Printing Layer Thickness and Orientation on the Mechanical Properties of DLP 3D-Printed Dental Resin. Polymers 2023, 15, 1113. [Google Scholar] [CrossRef] [PubMed]
- Alsarani, M.M. Influence of aging process and restoration thickness on the fracture resistance of provisional crowns: A comparative study. Saudi Dent. J. 2023, 35, 939–945. [Google Scholar] [CrossRef] [PubMed]
- May, M.M.; Fraga, S.; May, L.G. Effect of milling, fitting adjustments, and hydrofluoric acid etching on the strength and roughness of CAD-CAM glass-ceramics: A systematic review and meta-analysis. J. Prosthet. Dent. 2022, 128, 1190–1200. [Google Scholar] [CrossRef] [PubMed]
- Murillo-Gómez, F.; Hernández-Víquez, J.R.; Sauma-Montes de Oca, J.R.; Vargas-Vargas, C.; González-Vargas, N.; Vega-Baudrit, J.R.; Chavarría-Bolaños, D. Mechanical, Adhesive and Surface Properties of a Zirconia-Reinforced Lithium Silicate CAD/CAM Ceramic Exposed to Different Etching Protocols. Materials 2024, 17, 5039. [Google Scholar] [CrossRef] [PubMed]
- Kang, Y.J.; Kim, H.; Lee, J.; Park, Y.; Kim, J.H. Effect of airborne particle abrasion treatment of two types of 3D-printing resin materials for permanent restoration materials on flexural strength. Dent. Mater. 2023, 39, 648–658. [Google Scholar] [CrossRef]
- Ersöz, B.; Aydın, N.; Ezmek, B.; Karaoğlanoğlu, S.; Çal, İ.K. Effect of Surface Treatments Applied to 3D Printed Permanent Resins on Shear Bond Strength. J. Clin. Exp. Dent. 2024, 16, e1059–e1066. [Google Scholar] [CrossRef] [PubMed]
- ISO 21920-2:2021; Geometrical Product Specifications (GPS)—Surface Texture: Profile—Part 2: Terms, Definitions and Surface Texture Parame-ters. Available online: https://www.iso.org/ (accessed on 30 April 2025).
- Fotovat, F.; Shishehian, A.; Alijani, S.; Alafchi, B.; Parchami, P. Comparison of shear bond strength of orthodontic stainless-steel brackets on temporary crowns fabricated by three different methods: An in vitro study. Int. Orthod. 2022, 20, 100641. [Google Scholar] [CrossRef] [PubMed]
- Al Jabbari, Y.S.; Al Taweel, S.M.; Rifaiy MAl Alqahtani, M.Q.; Koutsoukis, T.; Zinelis, S. Effects of surface treatment and artificial aging on the shear bond strength of orthodontic brackets bonded to four different provisional restorations. Angle Orthod. 2014, 84, 649–655. [Google Scholar] [CrossRef] [PubMed]
- ISO/TS 11405:2015; Dentistry—Testing of Adhesion to Tooth Structure. Available online: https://www.iso.org/ (accessed on 30 April 2025).
- Lankes, V.; Reymus, M.; Liebermann, A.; Stawarczyk, B. Bond strength between temporary 3D printable resin and conventional resin composite: Influence of cleaning methods and air-abrasion parameters. Clin. Oral Investig. 2023, 27, 31–43. [Google Scholar] [CrossRef] [PubMed]
- Hammamy, M.; Rueda, S.R.; Pio, A.; Rizzante, F.A.P.; Lawson, N.C. Effect of Air Particle Abrasion and Primers on Bond Strength to 3D-Printed Crown Materials. Materials 2025, 18, 265. [Google Scholar] [CrossRef] [PubMed]
- Gorassini, F.; Fiorillo, L.; Marrapodi, M.M.; D’Amico, C.; Basile, M.; Cicciù, M.; Cervino, G. Debonding issues in orthodontics: An RCTs systematic review. Explor. Med. 2024, 5, 477–491. [Google Scholar] [CrossRef]



| Material | Chemical Composition | Manufacturer |
|---|---|---|
| 3D Printed composite resins for definitive restoration | ||
| Crowntec® (additively manufactured composite resin) | Esterification products of 4.4′-isopropylphenol, ethoxylated and 2-methylprop-2enoic acid, silanized dental glass, pyrogenic silica, initiator. Total content of inorganic fillers: 30–50 wt% | SAREMCO Dental AG |
| Surface Conditioning Methods | ||
| Porcelain etchant (4% HFA) | Hydrofluoric Acid 5–10% Sodium Fluoride < 1 | BISCO Inc. |
| Rhino (Al2O3) | Aluminum oxide particles White Alumina WA-200 (50 μm) | MDC Dental |
| Bonding agents | ||
| Single bond universal adhesive (SBU) | MDP phosphate monomer, Dimethacrylate resins, HEMA, Vitrebond copolymer, filler, ethanol, water, initiators, silane. | 3MTM ESPETM |
| Transbond XT Light Cure Adhesive Primer | Bisphenol a diglycidyl ether dimethacrylate, Triethylene glycol dimethacrylate (TEGDMA) | 3MTM UnitekTM |
| Composite resin | ||
| 3M FiltekTM Z350 XT composite | Matrix: Bis-GMA, UDMA, Bis-EMA Filler: Silica, zirconia nanoparticles (20 µm) (72.5 wt%/55.9 vol%) | 3MTM ESPETM |
| Type III Sum of Squares | df | Mean Square | F | |
|---|---|---|---|---|
| Surface Treatment | 564.9 | 2 | 282.45 | 125.41 |
| Adhesive | 167.45 | 1 | 167.45 | 74.35 |
| Surface Treatment x Adhesive Interaction | 18.86 | 2 | 9.43 | 4.19 |
| Error | 148.65 | 66 | 2.25 |
| Comparison | ΔMPa | p-Value |
|---|---|---|
| SBU (Air Abrasion)—TXT (Air Abrasion) | 4.48 | <0.001 |
| SBU (Air Abrasion)—SBU (Etching) | 6.28 | <0.001 |
| SBU (Air Abrasion)—SBU (Control) | 7.59 | <0.001 |
| TXT (Air Abrasion)—TXT (Etching) | 4.33 | <0.001 |
| TXT (Air Abrasion)—TXT (Control) | 5.25 | <0.001 |
| SBU (Etching)—TXT (Etching) | 2.53 | <0.001 |
| SBU (Control)—TXT (Control) | 2.14 | <0.001 |
| SBU (Etching)—SBU (Control) | 1.31 | 0.545 |
| TXT (Etching)—TXT (Control) | 0.92 | 0.759 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Criollo-Barrios, O.V.; Luna-Domínguez, C.R.; Luna-Lara, C.A.; Figueroa-López, R.d.J.; Cozza, R.C.; Luna-Domínguez, J.H. Bonding Orthodontic Attachments to 3D-Printed Photosensitive Definitive Resin: An In Vitro Study. Dent. J. 2025, 13, 341. https://doi.org/10.3390/dj13080341
Criollo-Barrios OV, Luna-Domínguez CR, Luna-Lara CA, Figueroa-López RdJ, Cozza RC, Luna-Domínguez JH. Bonding Orthodontic Attachments to 3D-Printed Photosensitive Definitive Resin: An In Vitro Study. Dentistry Journal. 2025; 13(8):341. https://doi.org/10.3390/dj13080341
Chicago/Turabian StyleCriollo-Barrios, Omaika Victoria, Carlos Roberto Luna-Domínguez, Carlos Alberto Luna-Lara, Ricardo de Jesus Figueroa-López, Ronaldo Câmara Cozza, and Jorge Humberto Luna-Domínguez. 2025. "Bonding Orthodontic Attachments to 3D-Printed Photosensitive Definitive Resin: An In Vitro Study" Dentistry Journal 13, no. 8: 341. https://doi.org/10.3390/dj13080341
APA StyleCriollo-Barrios, O. V., Luna-Domínguez, C. R., Luna-Lara, C. A., Figueroa-López, R. d. J., Cozza, R. C., & Luna-Domínguez, J. H. (2025). Bonding Orthodontic Attachments to 3D-Printed Photosensitive Definitive Resin: An In Vitro Study. Dentistry Journal, 13(8), 341. https://doi.org/10.3390/dj13080341








