Neuroimaging Signatures of Temporomandibular Disorder and Burning Mouth Syndrome: A Systematic Review
Abstract
1. Introduction
2. Methods
2.1. Literature Search and Identification of Studies
2.2. Eligibility and Paper Selection
2.2.1. Types of Studies
2.2.2. Types of Participants
2.2.3. Primary Outcome Measure
2.2.4. Types of Imaging
2.2.5. Types of Stimulation
2.3. Data Collection
2.3.1. Selection of Studies
- -
- English language, humans, and full text available.
- -
- Neuroimaging of participants definitively diagnosed with a type of COFP.
- -
- Quantitative outcome measures reported.
- -
- Diagnosis of trigeminal neuralgia, acute orofacial pain, e.g., dental pain, chronic pain.
- -
- Ultrasound or planar X-ray imaging.
- -
- Studies that did not include neuroimaging.
- -
- Chronic pain outside of the orofacial area.
- -
- Review papers.
2.3.2. Data Extraction
2.3.3. Data Analysis
2.3.4. Assessment of Study Quality
3. Results
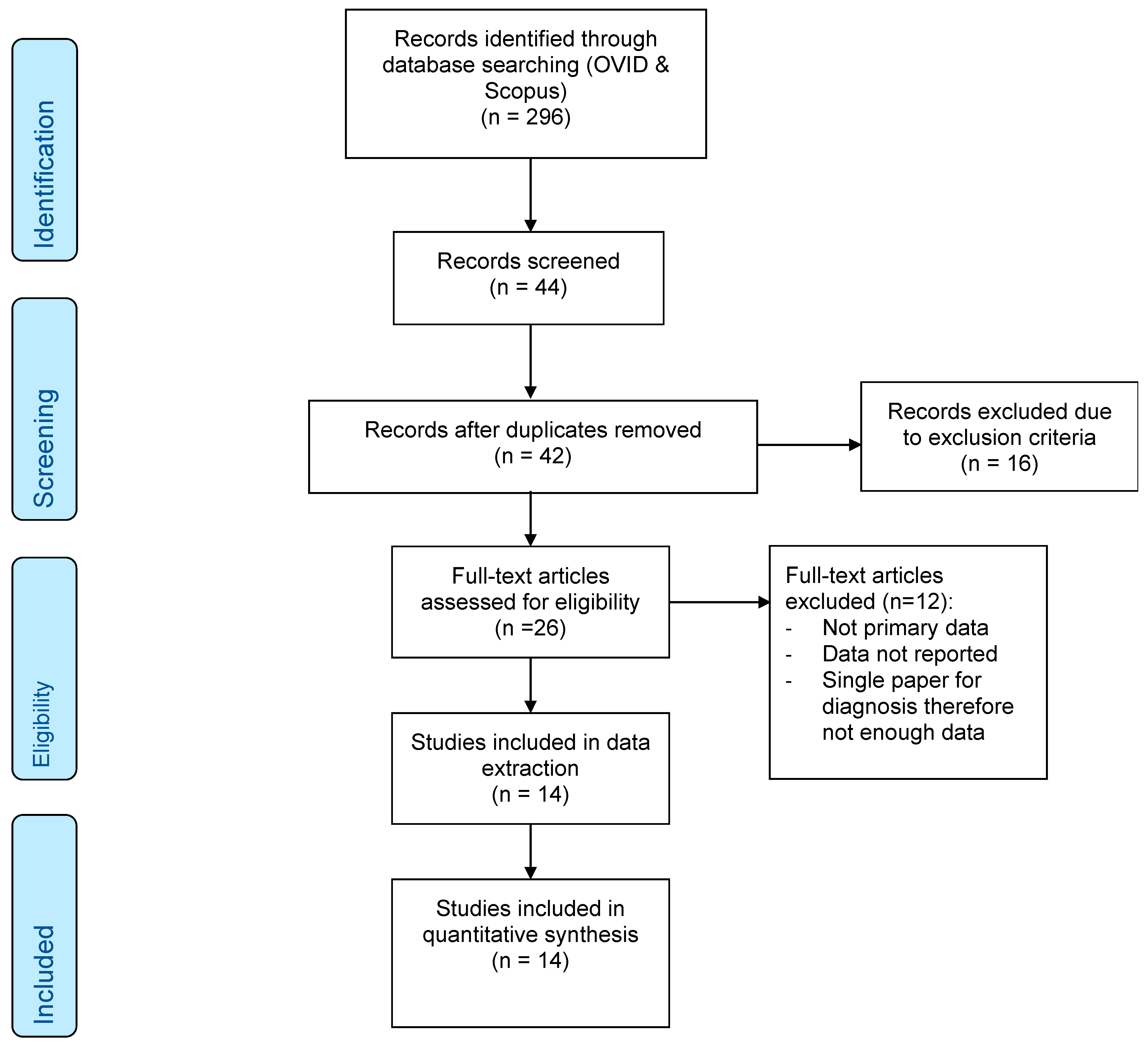
3.1. Included Studies/Search Results
3.2. Demographics/Study Characteristics
3.2.1. Overview
3.2.2. Pain Duration
3.2.3. Confounding
3.2.4. Imaging Modalities
3.3. Risk of Bias Assessment and Quality of Study
3.4. Assessment of Pain
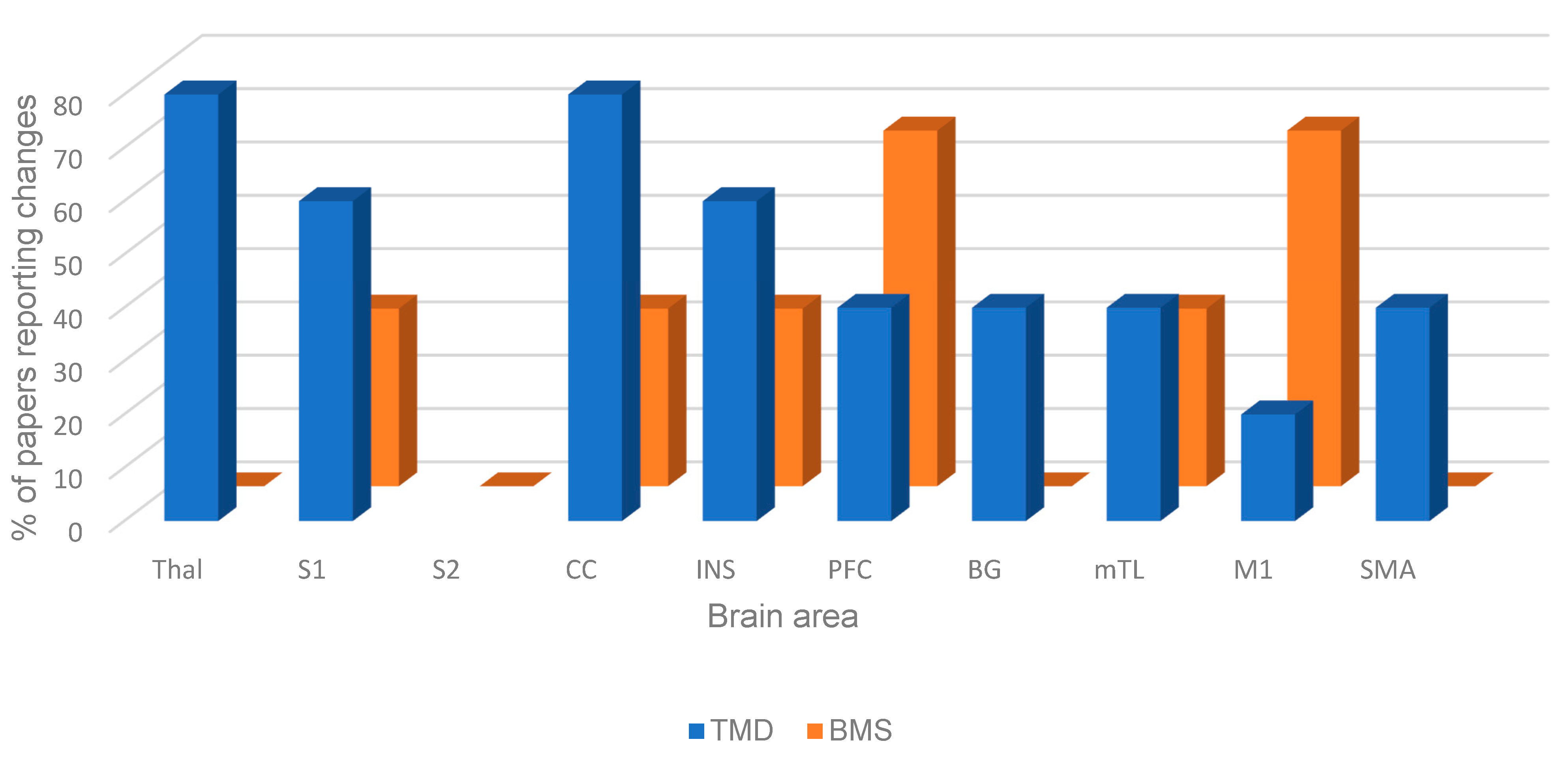
3.5. Resting-State Brain Changes
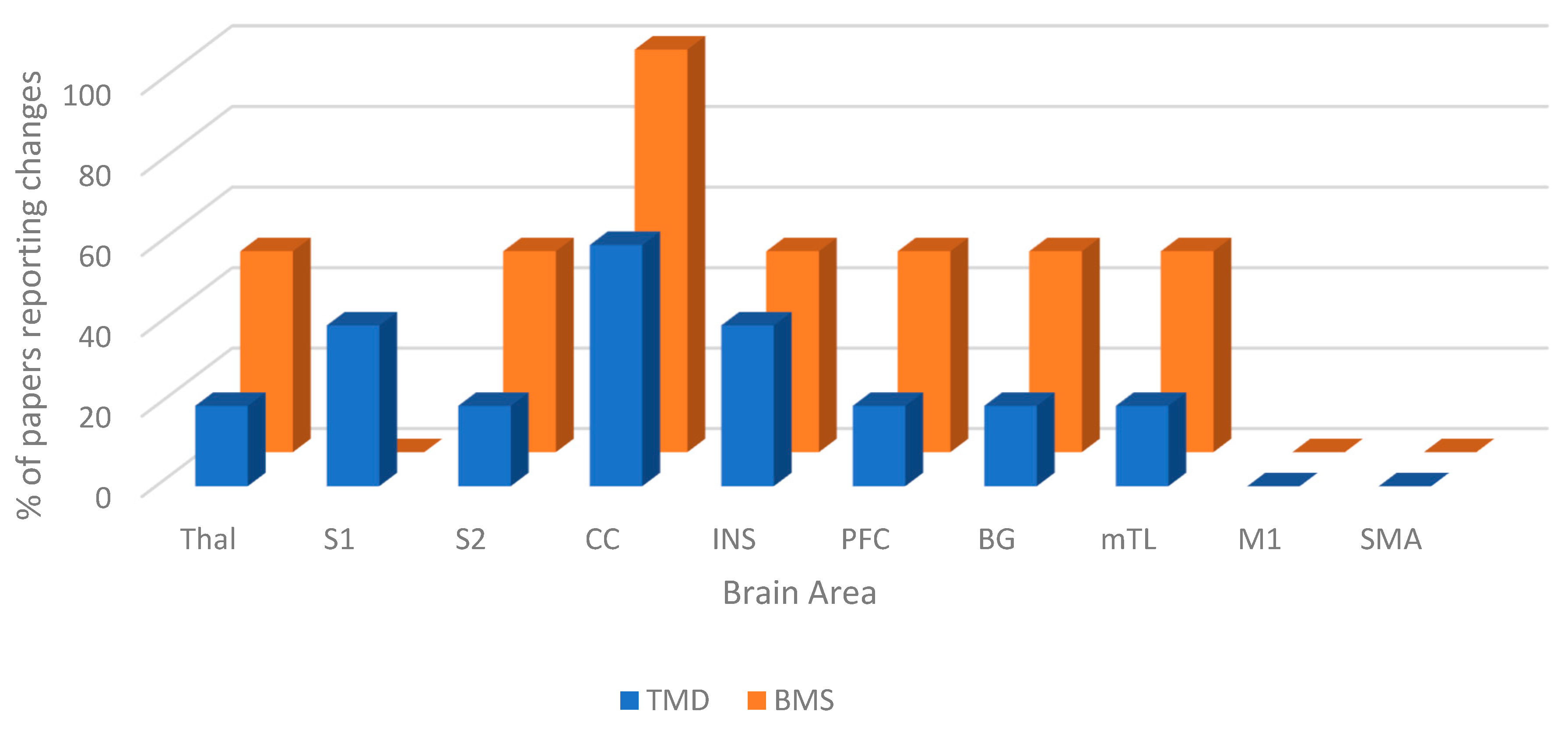
3.6. Task-State Brain Changes
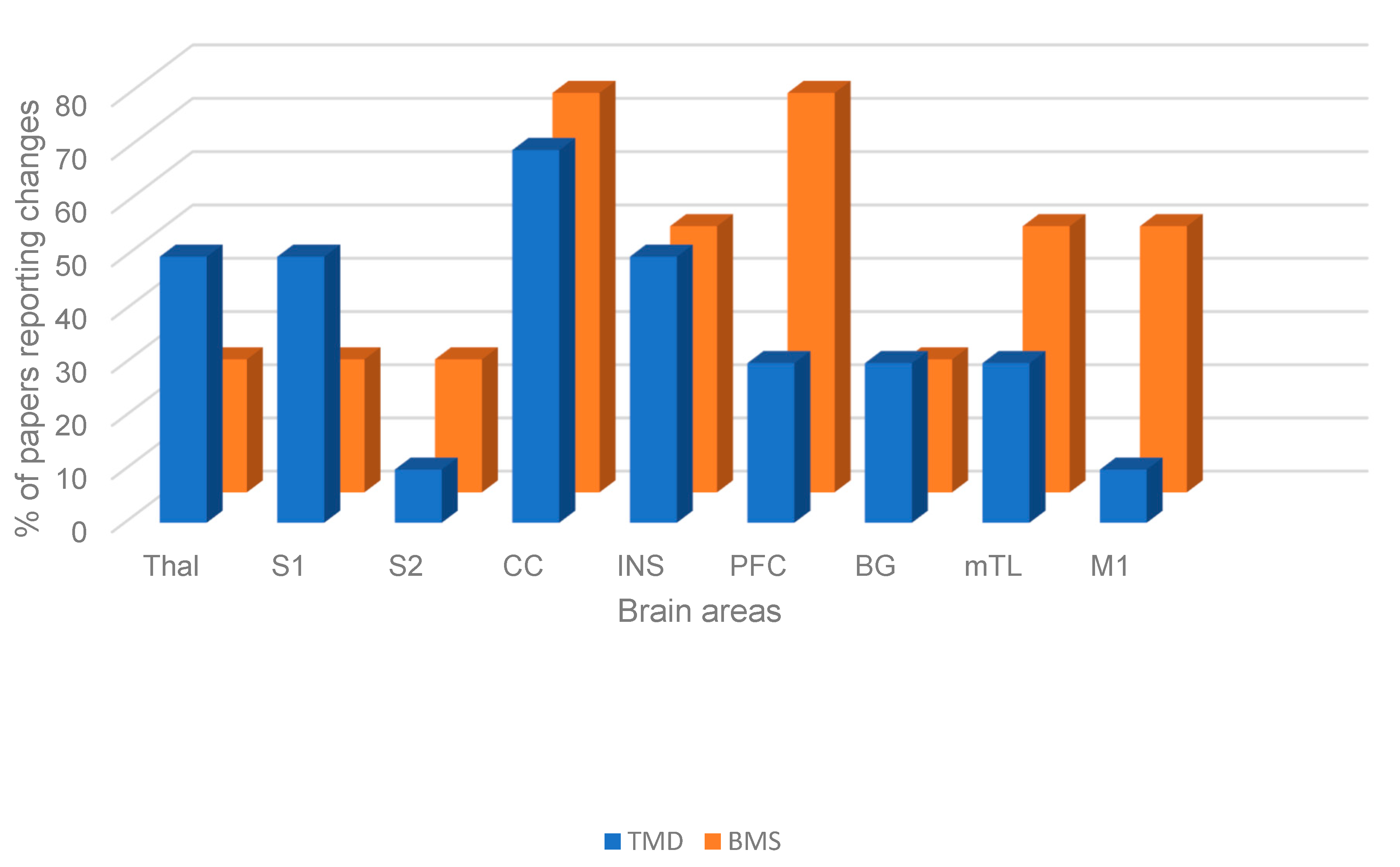
3.7. Shared Brain Area Changes Irrespective of Task or Resting State
4. Discussion
4.1. The Cingulate Cortex (CC) and Insula
4.2. The Prefrontal Cortex (PFC)
4.3. The Limbic System
- Changes may be due to compensatory analgesic adaptations that attempt to reduce the sensation of pain.
- Changes cause an increased transmission of painful signals due to increased or decreased neural connections.
4.4. Motor System Involvement
4.5. Future Research and Limitations of This Review
4.6. Clinical Implications
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Macfarlane, T.; Blinkhorn, A.; Davies, R.; Kincey, J.; Worthington, H. Oro-facial pain in the community: Prevalence and associated impact. Community Dent. Oral Epidemiol. 2002, 30, 52–60. [Google Scholar] [CrossRef] [PubMed]
- Peters, S.; Goldthorpe, J.; McElroy, C.; King, E.; Javidi, H.; Tickle, M.; Aggarwal, V.R. Managing chronic orofacial pain: A qualitative study of patients’, doctors’, and dentists’ experiences. Br. J. Health Psychol. 2015, 20, 777–791. [Google Scholar] [CrossRef] [PubMed]
- Currie, C.C.; Palmer, J.; Stone, S.J.; Brocklehurst, P.; Aggarwal, V.R.; Dorman, P.J.; Pearce, M.S.; Durham, J. Persistent Orofacial Pain Attendances at General Medical Practitioners. J. Dent. Res. 2023, 102, 164–169. [Google Scholar] [CrossRef] [PubMed]
- Beecroft, E.; Durham, J.; Thomson, P. Retrospective examination of the healthcare ‘journey’ of chronic orofacial pain patients referred to oral and maxillofacial surgery. Br. Dent. J. 2013, 214, E12. [Google Scholar] [CrossRef] [PubMed]
- Durham, J.; Shen, J.; Breckons, M.; Steele, J.G.; Araujo-Soares, V.; Exley, C.; Vale, L. Healthcare cost and impact of persistent orofacial pain the deep study cohort. J. Dent. Res. 2016, 95, 1147–1154. [Google Scholar] [CrossRef] [PubMed]
- Breckons, M.; Bissett, S.; Exley, C.; Araujo-Soares, V.; Durham, J. Care Pathways in Persistent Orofacial Pain: Qualitative Evidence from the DEEP Study. J. Dent. Res. Clin. Transl. Res. 2017, 2, 48–57. [Google Scholar] [CrossRef] [PubMed]
- Nicholas, M.; Vlaeyen, J.; Rief, W.; Bark, E.A.; Aziz, Q.; Benoliel, R.; Cohen, M.; Evers, S.; Giamberardino, M.; Goebel, A.; et al. The IASP classification of chronic pain for ICD-11: Chronic primary pain. Pain 2019, 160, 28–37. [Google Scholar] [CrossRef] [PubMed]
- Aggarwal, V.R.; Macfarlane, G.J.; Farragher, T.; McBeth, J. Risk factors for the onset of chronic oro-facial pain—Results from the Cheshire Oro-facial Pain prospective population study. Pain 2010, 149, 354–359. [Google Scholar] [CrossRef] [PubMed]
- Fillingim, R.B.; Ohrbach, R.; Greenspan, J.D.; Knott, C.; Diatchenko, L.; Dubner, R.; Bair, E.; Baraian, C.; Mack, N.; Slade, G.D.; et al. Psychological factors associated with development of TMD: The OPPERA prospective cohort study. J. Pain 2013, 14 (Suppl. S12), T75–T90. [Google Scholar] [CrossRef] [PubMed]
- International Classification of Orofacial Pain, 1st edition (ICOP). Cephalalgia 2020, 40, 129–221. [CrossRef] [PubMed]
- Lin, C.S. Brain signature of chronic orofacial pain: A systematic review and meta-analysis on neuroimaging research of trigeminal neuropathic pain and temporomandibular joint disorders. PLoS ONE 2014, 9, e94300. [Google Scholar] [CrossRef] [PubMed]
- LIberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. J. Clin. Epidemiol. 2009, 62, e1–e34. [Google Scholar] [CrossRef] [PubMed]
- Yin, Y.; He, S.; Xu, J.; You, W.; Li, Q.; Long, J.; Luo, L.; Kemp, G.J.; Sweeney, J.A.; Li, F.; et al. The neuro-pathophysiology of temporomandibular disorders-related pain: A systematic review of structural and functional MRI studies. J. Headache Pain 2020, 21, 78. [Google Scholar] [CrossRef] [PubMed]
- Coleman, B.; Khan, K.; Maffulli, N.; Cook, J.; Wark, J. Studies of surgical outcome after patellar tendinopathy: Clinical significance of methodological deficiencies and guidelines for future studies. Scand. J. Med. Sci. Sports 2000, 10, 2–11. [Google Scholar] [CrossRef] [PubMed]
- Kucyi, A.; Moayedi, M.; Weissman-Fogel, I.; Goldberg, M.B.; Freeman, B.V.; Tenenbaum, H.C.; Davis, K.D. Enhanced medial prefrontal-default mode network functional connectivity in chronic pain and its association with pain rumination. J. Neurosci. 2014, 34, 3969–3975. [Google Scholar] [CrossRef] [PubMed]
- Youssef, A.M.; Gustin, S.M.; Nash, P.G.; Reeves, J.M.; Petersen, E.T.; Peck, C.C.; Murray, G.M.; Henderson, L.A. Differential brain activity in subjects with painful trigeminal neuropathy and painful temporomandibular disorder. Pain 2014, 155, 467–475. [Google Scholar] [CrossRef] [PubMed]
- Younger, J.W.; Shen, Y.F.; Goddard, G.; Mackey, S.C. Chronic myofascial temporomandibular pain is associated with neural abnormalities in the trigeminal and limbic systems. Pain 2010, 149, 222–228. [Google Scholar] [CrossRef] [PubMed]
- Ichesco, E.; Quintero, A.; Clauw, D.J.; Peltier, S.; Sundgren, P.M.; Gerstner, G.E.; Schmidt-Wilcke, T. Altered functional connectivity between the insula and the cingulate cortex in patients with temporomandibular disorder: A pilot study. Headache 2012, 52, 441–454. [Google Scholar] [CrossRef] [PubMed]
- Moayedi, M.; Weissman-Fogel, I.; Salomons, T.V.; Crawley, A.P.; Goldberg, M.B.; Freeman, B.V.; Tenenbaum, H.C.; Davis, K.D. White matter brain and trigeminal nerve abnormalities in temporomandibular disorder. Pain 2012, 153, 1467–1477. [Google Scholar] [CrossRef] [PubMed]
- Gustin, S.M.; Peck, C.C.; Cheney, L.B.; Macey, P.M.; Murray, G.M.; Henderson, L.A. Pain and plasticity: Is chronic pain always associated with somatosensory cortex activity and reorganization? J. Neurosci. 2012, 32, 14874–14884. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.P.; Ma, X.C.; Jin, Z.; Li, K.; Liu, G.; Zeng, Y.W. Cerebral activation during unilateral clenching in patients with temporomandibular joint synovitis and biting pain: An functional magnetic resonance imaging study. Chin. Med. J. 2011, 124, 2136–2143. [Google Scholar] [PubMed]
- Gustin, S.M.; Peck, C.C.; Wilcox, S.L.; Nash, P.G.; Murray, G.M.; Henderson, L.A. Different pain, different brain: Thalamic anatomy in neuropathic and non-neuropathic chronic pain syndromes. J. Neurosci. 2011, 31, 5956–5964. [Google Scholar] [CrossRef]
- Weissman-Fogel, I.; Moayed, I.M.; Tenenbaum, H.C.; Goldberg, M.B.; Freeman, B.V.; Davis, K.D. Abnormal cortical activity in patients with temporomandibular disorder evoked by cognitive and emotional tasks. Pain 2011, 152, 384–396. [Google Scholar] [CrossRef] [PubMed]
- Sinding, C.; Gransjoen, A.; Schlumberger, G.; Grushka, M.; Frasnelli, J.; Singh, P. Grey matter changes of the pain matrix in patients with burning mouth syndrome. Eur. J. Neurosci. 2016, 43, 997–1005. [Google Scholar] [CrossRef] [PubMed]
- Khan, S.A.; Keaser, M.L.; Meiller, T.F.; Seminowicz, D.A. Altered structure and function in the hippocampus and medial prefrontal cortex in patients with burning mouth syndrome. Pain 2014, 155, 1472–1480. [Google Scholar] [CrossRef] [PubMed]
- Albuquerque, R.; De Leeuw, R.; Carlson, C.; Okeson, J.; Miller, C.; Andersen, A. Cerebral activation during thermal stimulation of patients who have burning mouth disorder: An fMRI study. Pain 2006, 122, 223–234. [Google Scholar] [CrossRef] [PubMed]
- Kohashi, R.; Shinozaki, T.; Sekine, N.; Watanabe, K.; Takanezawa, D.; Nishihara, C.; Ozasa, K.; Ikeda, M.; Noma, N.; Okada-Ogawa, A.; et al. Time-dependent responses in brain activity to ongoing hot stimulation in burning mouth syndrome. J. Oral Sci. 2020, 62, 170–174. [Google Scholar] [CrossRef] [PubMed]
- Tennant, P.; Murray, E.J.M.; Arnold, K.F.; Berrie, L.; Fox, M.P.; Gadd, S.C.; Harrison, W.J.; Keeble, C.; Ranker, L.R.; Textor, J.; et al. Use of directed acyclic graphs (DAGs) to identify cofounders in applied health research: Review and recommendations. Int. J. Epidemiol. 2012, 50, 620–632. [Google Scholar] [CrossRef] [PubMed]
- Woolf, C.J. Central sensitization: Implications for the diagnosis and treatment of pain. Pain 2011, 152 (Suppl. S3), S2–S15. [Google Scholar] [CrossRef] [PubMed]
- Svensson, P.; Graven-Nielsen, T. Craniofacial muscle pain: Review of mechanisms and clinical manifestations. J. Oral Rehabil. 2001, 28, 571–579. [Google Scholar]
- Maixner, W.; Fillingim, R.B.; Williams, D.A.; Smith, S.B.; Slade, G.D. Overlapping chronic pain conditions: Implications for diagnosis and classification. J. Pain 2016, 17 (Suppl. S9), T93–T107. [Google Scholar] [CrossRef] [PubMed]
- Karibe, H.; Arakawa, R.; Tateno, A.; Mizumura, S.; Okada, T.; Ishii, T.; Oshima, K.; Ohtsu, M.; Hasegawa, I.; Okubo, Y. Regional cerebral blood flow in patients with orally localized somatoform pain disorder: A single photon emission computed tomography study. Psychiatry Clin. Neurosci. 2010, 64, 476–482. [Google Scholar] [CrossRef] [PubMed]
- National Institute for Health and Care Excellence. Recommendations, Chronic Pain (Primary and Secondary) in over 16s: Assessment of All Chronic Pain and Management of Chronic Primary Pain. Guidance. NICE. 7 April 2021. Available online: https://www.nice.org.uk/guidance/ng193/chapter/Recommendations#managing-chronic-primary-pain (accessed on 4 May 2025).
- National Academies of Sciences, Engineering, and Medicine. Temporomandibular Disorders: Priorities for Research and Care; The National Academies Press: Washington, DC, USA, 2020. [Google Scholar]
- Aggarwal, V.R.; Fu, Y.; Main, C.J.; Wu, J. The effectiveness of self-management interventions in adults with chronic orofacial pain: A systematic review, meta-analysis and meta-regression. Eur. J. Pain 2019, 23, 849–865. [Google Scholar] [CrossRef] [PubMed]
- Aggarwal, V.R.; Wu, J.; Fox, F.; Howdon, D.; Guthrie, E.; Mighell, A. Implementation of biopsychosocial supported self-management for chronic primary oro-facial pain including temporomandibular disorders: A theory, person and evidence-based approach. J. Oral Rehabil. 2021, 48, 1118–1128. [Google Scholar] [CrossRef] [PubMed]

| Patient | Control | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Source | Diagnosis | Imaging Modality | Analysis Method | Resting/Task | Female | Male | Age (Years) | Assessment | Duration of Pain | Female | Male | Age |
| Kucyi 2014 [15] | TMD | MRI (BOLD T2 | FC | Resting | 17 | 33.1 ± 11.9 | NPS, PCS | minimum 3 months | 17 | 32.2 ± 10.2 | ||
| Youssef 2014 [16] | TMD | MRI (STAR labelled T1) | CBF | Resting | 12 | 3 | 44.9 ± 3.1 | VAS, MPQ | 11.4 ± 3.3 years | 41 | 13 | 46.9 ± 2.1 |
| Younger 2010 [17] | TMD | MRI (FAST 3D-SPGR) | GMV | Resting | 14 | 38 ± 13.7 | NRS | 4.4 ± 2.9 years | 15 | age-matched | ||
| Ichesco 2012 [18] | TMD | MRI (T2spiral sequence) | FC | Resting | 8 | 23–31 | VAS, SF-MPQ, BPI, STPI | minimum 3 months | 8 | 22–27 | ||
| Moayedi 2012 [19] | TMD | MRI (T1, DTI) | FA | Resting | 17 | 33.1 ± 11.9 | NPS | 9.8 ± 8.25 years | 17 | 32.2 ± 10.1 | ||
| Gustin 2012 [20] | TMD | MRI (BOLD T1) | BA, CBF, FA | Innocuous brushing of lower lip, little finger, and thumb | 13 | 4 | 44 ± 3 | VAS, MPQ | 10.7 ± 2 years | 27 | 26 | 41 ± 2 |
| Zhao 2011 [21] | TMD | MRI (T2) | BA | Clenching | 11 | 3 | 33.7 ± 13.2 | VAS, SCL−90 | Not reported | 7 | 7 | 23.7 ± 0.9 |
| Ichesco 2012 [18] | TMD | MRI (T2 spiral sequence) | FC | Elicited pain | 8 | 23–31 | VAS, SF-MPQ, BPI, STPI | minimum 3 months | 8 | 22–27 | ||
| Gustin 2011 [22] | TMD | fMRI (QASL, DTI) | GMV, metabolite levels | Innocuous lip brushing | 16 | 4 | 45.7 ± 2.9 | VAS, MPQ, BDI, STATE | 11.4 ± 3.3 years | 25 | 6 | 46.8 ± 3.3 |
| Weissman-Fogel 2011 [23] | TMD | MRI (T1 (structural), T2 (functional)) | Peak activation coordinates | nSTROOP, ncSTROOP, ecSTROOP | 17 | 35.2 ± 11.6 | NPS | 9.3 ± 8.3 years | 17 | 34 ± 9.9 | ||
| Sinding 2016 [24] | BMS | MRI (T1 3d IR/GR sequence) | GMC | Resting | 7 | 5 | 59.4 ± 12.1 | unanchored, unmarked scale | minimum 3 months | 10 | 3 | 59 ± 3.4 |
| Khan 2014 [25] | BMS | MRI | GMV, FA, DTI, FC | Resting | 9 | 54 ± 7.7 | STAI | 4 ± 4.8 years | 9 | age matched | ||
| Albuquerque 2006 [26] | BMS | MRI (EPI sequence) | BA | Thermal stimulation | 8 | 49.1 ± 10.1 | SCL-90R, BDI, STAI | 60.5 ± 38.4 months | 8 | 50 ± 12.3 | ||
| Kohashi 2020 [27] | BMS | MRI (T2) | BA | Thermal stimulation | 15 | 52.6 ± 6.3 | Not reported | not reported | 15 | 49 ± 8.4 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fischer, S.; Tsoumpas, C.; Chana, P.; Feltbower, R.G.; Aggarwal, V.R. Neuroimaging Signatures of Temporomandibular Disorder and Burning Mouth Syndrome: A Systematic Review. Dent. J. 2025, 13, 340. https://doi.org/10.3390/dj13080340
Fischer S, Tsoumpas C, Chana P, Feltbower RG, Aggarwal VR. Neuroimaging Signatures of Temporomandibular Disorder and Burning Mouth Syndrome: A Systematic Review. Dentistry Journal. 2025; 13(8):340. https://doi.org/10.3390/dj13080340
Chicago/Turabian StyleFischer, Sarah, Charalampos Tsoumpas, Pavneet Chana, Richard G. Feltbower, and Vishal R. Aggarwal. 2025. "Neuroimaging Signatures of Temporomandibular Disorder and Burning Mouth Syndrome: A Systematic Review" Dentistry Journal 13, no. 8: 340. https://doi.org/10.3390/dj13080340
APA StyleFischer, S., Tsoumpas, C., Chana, P., Feltbower, R. G., & Aggarwal, V. R. (2025). Neuroimaging Signatures of Temporomandibular Disorder and Burning Mouth Syndrome: A Systematic Review. Dentistry Journal, 13(8), 340. https://doi.org/10.3390/dj13080340









