The Effect of Zirconia Material and the Height of the Ceramic Coping on the Strength of Hybrid Ti-Ceramic Abutments
Abstract
1. Introduction
Aim
2. Materials and Methods
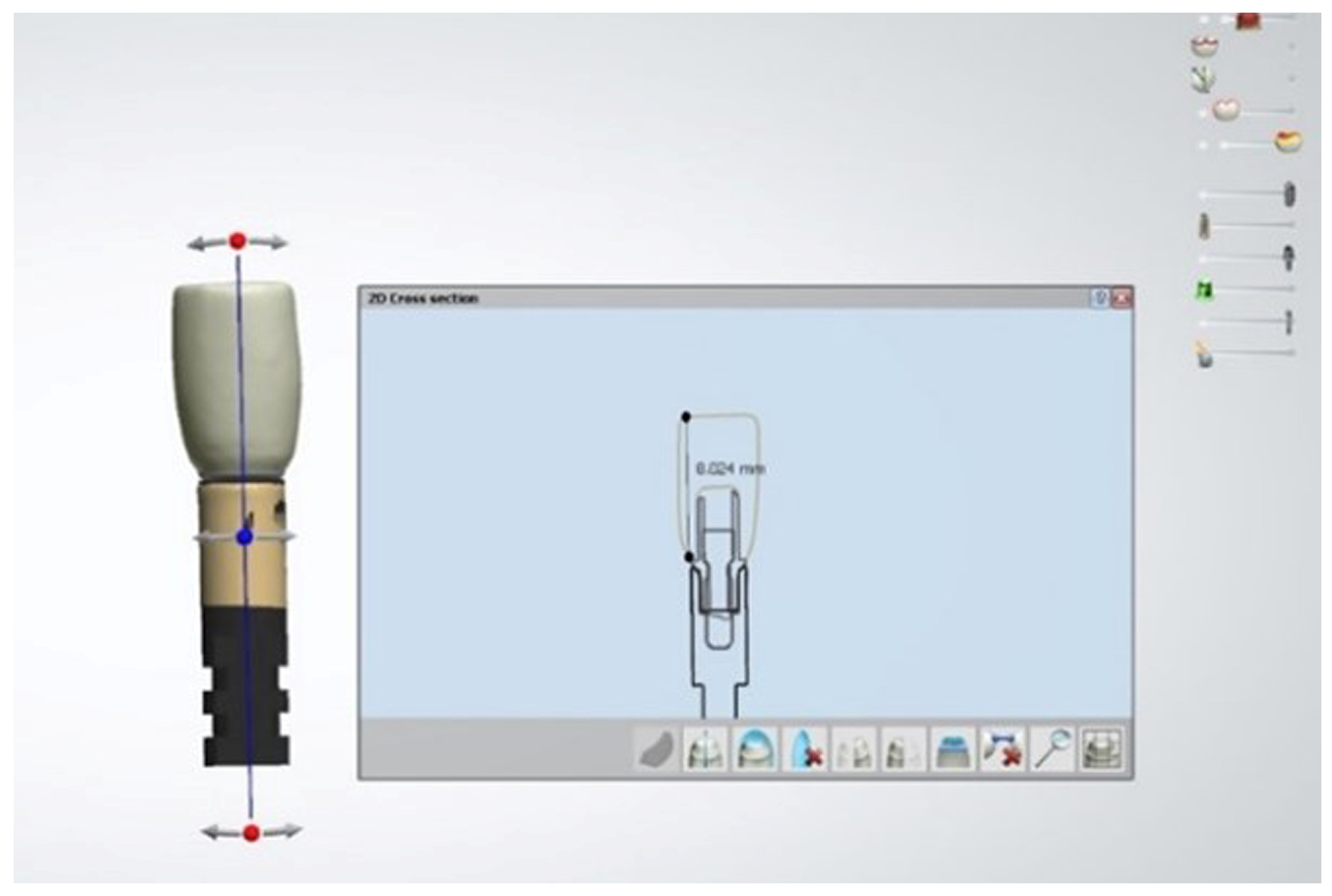
2.1. Fabrication of Zirconia Copings
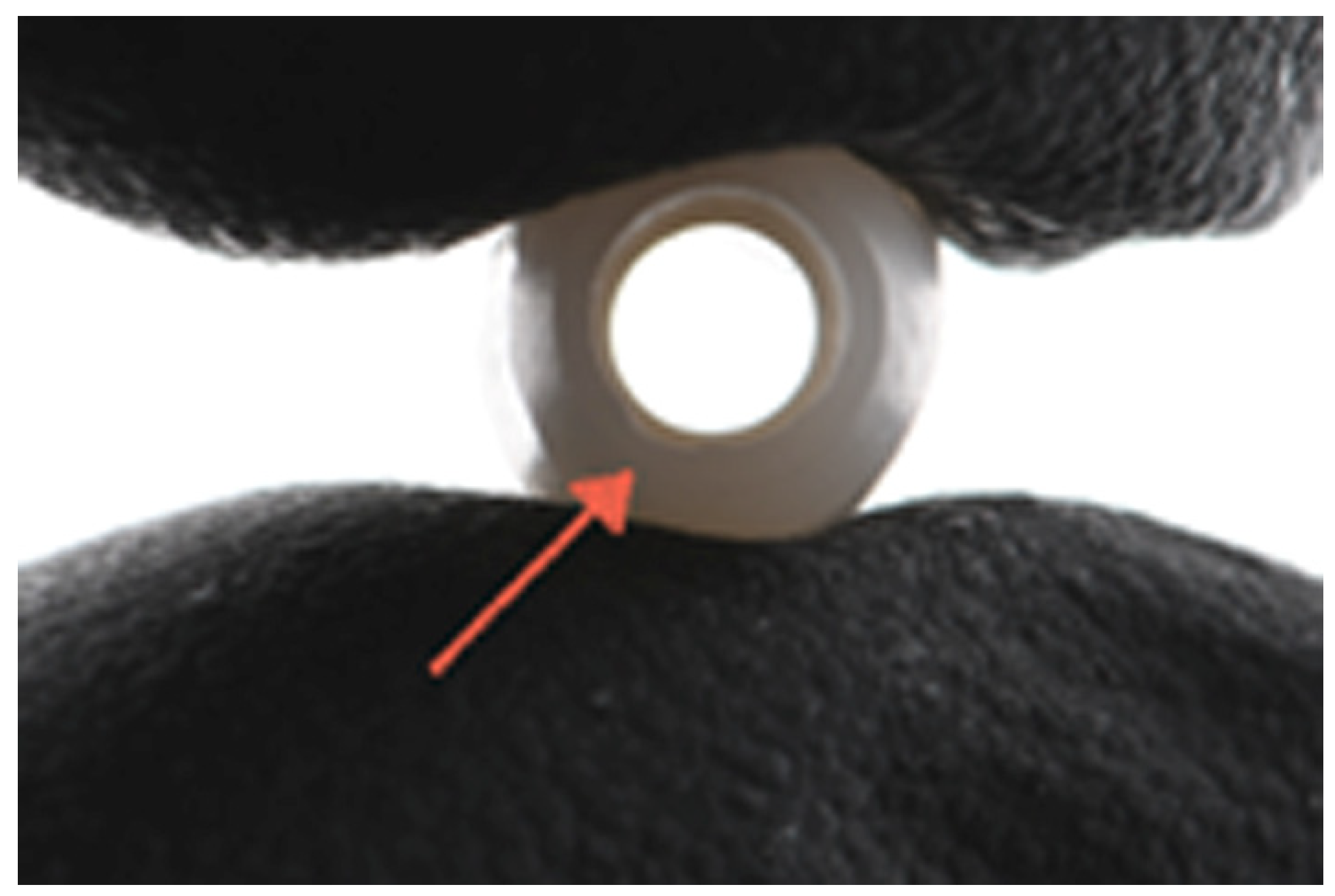
2.2. Fatigue Loading
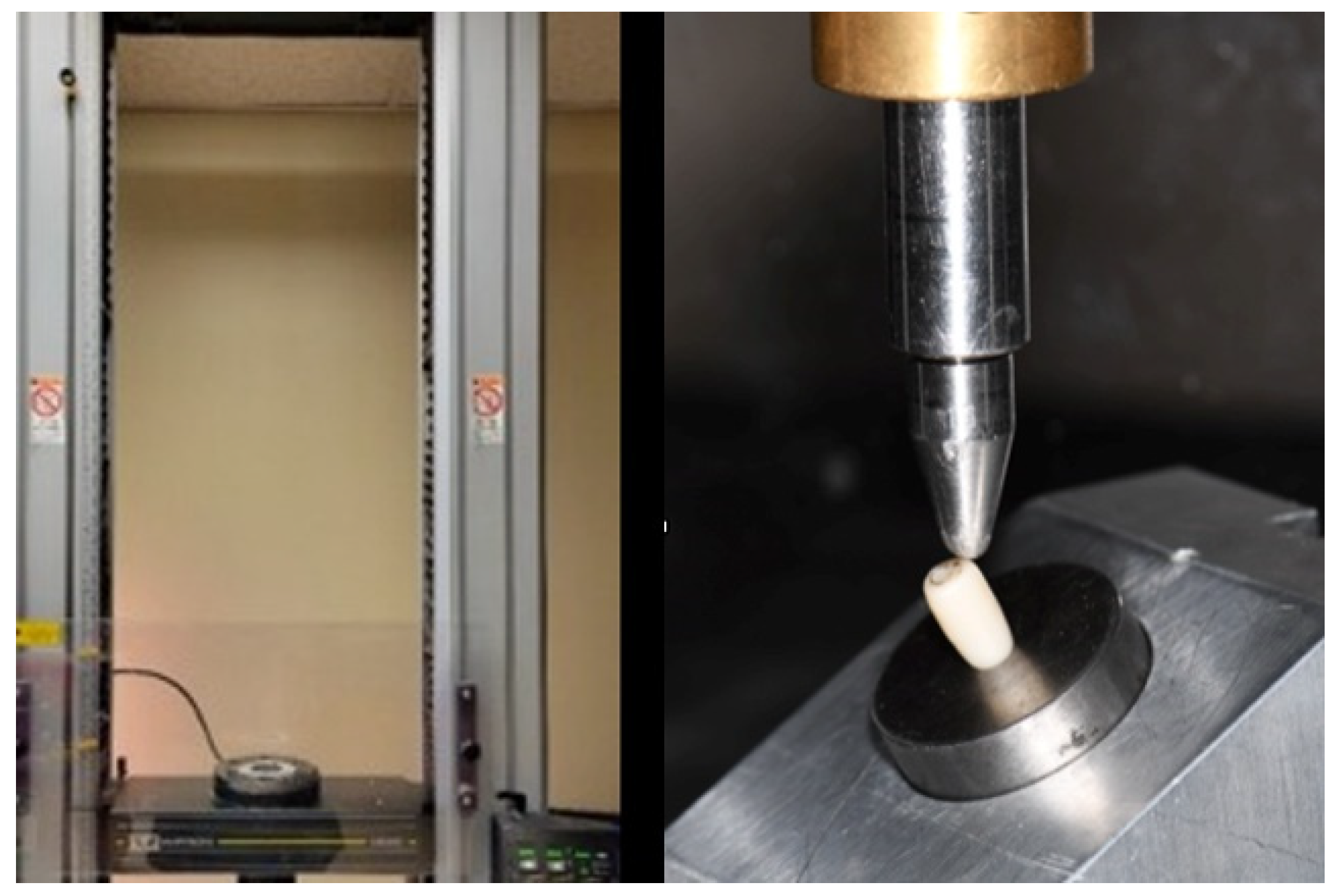
2.3. Compressive Loading Tests
3. Results
Failure Modes
4. Discussion
5. Conclusions
- The height of the ceramic coping negatively affected the strength of the tested titanium base hybrid abutment. Short ceramic copings showed higher failure forces in both tested zirconia materials.
- The 3Y zirconia copings showed increased strength compared to 5Y zirconia in all height groups.
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sailer, I.; Philipp, A.; Zembic, A.; Pjetursson, B.E.; Hämmerle, C.H.; Zwahlen, M. A systematic review of the performance of ceramic and metal implant abutments supporting fixed implant reconstructions. Clin. Oral Implants Res. 2009, 20 (Suppl. S4), 4–31. [Google Scholar] [CrossRef] [PubMed]
- Moreno, A.L.M.; Dos Santos, D.M.; Bertoz, A.P.M.; Goiato, M.C. Abutment on Titanium-Base Hybrid Implant: A Literature Review. Eur. J. Dent. 2023, 17, 261–269. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Al-Thobity, A.M. Titanium Base Abutments in Implant Prosthodontics: A Literature Review. Eur. J. Dent. 2022, 16, 49–55. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kongkiatkamon, S.; Rokaya, D.; Kengtanyakich, S.; Peampring, C. Current classification of zirconia in dentistry: An updated review. PeerJ 2023, 11, e15669. [Google Scholar] [CrossRef]
- Kontonasaki, E.; Rigos, A.E.; Ilia, C.; Istantsos, T. Monolithic zirconia: An update to current knowledge, optical properties, wear, and clinical performance. Dent. J. 2019, 7, 90. [Google Scholar] [CrossRef] [PubMed]
- Alqutaibi, A.Y.; Ghulam, O.; Krsoum, M.; Binmahmoud, S.; Taher, H.; Elmalky, W.; Zafar, M.S. Revolution of current dental zirconia: A comprehensive review. Molecules 2022, 27, 1699. [Google Scholar] [CrossRef]
- Gou, M.; Chen, H.; Fu, M.; Wang, H. Fracture of Zirconia Abutments in Implant Treatments: A Systematic Review. Implant Dent. 2019, 28, 378–387. [Google Scholar] [CrossRef] [PubMed]
- Bharate, V.; Kumar, Y.; Koli, D.; Pruthi, G.; Jain, V. Effect of different abutment materials (zirconia or titanium) on the crestal bone height in 1 year. J. Oral Biol. Craniofac. Res. 2020, 10, 372–374. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Halim, F.C.; Pesce, P.; De Angelis, N.; Benedicenti, S.; Menini, M. Comparison of the Clinical Outcomes of Titanium and Zirconia Implant Abutments: A Systematic Review of Systematic Reviews. J. Clin. Med. 2022, 11, 5052. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bonyatpour, M.; Giti, R.; Erfanian, B. Implant angulation and fracture resistance of one-piece screw-retained hybrid monolithic zirconia ceramic restorations. PLoS ONE 2023, 18, e0280816. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chmielewski, M.; Dąbrowski, W.; Ordyniec-Kwaśnica, I. The Fracture Resistance Comparison between Titanium and Zirconia Implant Abutments with and without Ageing: Systematic Review and Meta-Analysis. Dent. J. 2024, 12, 274. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Linkevicius, T.; Vaitelis, J. The effect of zirconia or titanium as abutment material on soft peri-implant tissues: A systematic review and meta-analysis. Clin. Oral Implants Res. 2015, 26 (Suppl. S11), 139–147. [Google Scholar] [CrossRef] [PubMed]
- Sailer, I.; Zembic, A.; Jung, R.E.; Siegenthaler, D.; Holderegger, C.; Hämmerle, C.H. Randomized controlled clinical trial of customized zirconia and titanium implant abutments for canine and posterior single-tooth implant reconstructions: Preliminary results at 1 year of function. Clin. Oral Implants Res. 2009, 20, 219–225. [Google Scholar] [CrossRef] [PubMed]
- Cao, Y.; Yu, C.; Wu, Y.; Li, L.; Li, C. Long-Term Survival and Peri-Implant Health of Titanium Implants with Zirconia Abutments: A Systematic Review and Meta-Analysis. J. Prosthodont. 2019, 28, 883–892. [Google Scholar] [CrossRef] [PubMed]
- Lopes, A.C.O.; Machado, C.M.; Bonjardim, L.R.; Bergamo, E.T.P.; Ramalho, I.S.; Witek, L.; Coelho, P.G.; Bonfante, E.A. The effect of CAD/CAM crown material and cement type on retention to implant abutments. J. Prosthodont. 2019, 28, e552–e556. [Google Scholar] [CrossRef]
- Al-Zordk, W.; Elmisery, A.; Ghazy, M. Hybrid-abutment-restoration: Effect of material type on torque maintenance and fracture resistance after thermal aging. Int. J. Implant Dent. 2020, 6, 24. [Google Scholar] [CrossRef]
- Arce, C.; Lawson, N.C.; Liu, P.R.; Lin, C.P.; Givan, D.A. Retentive Force of Zirconia Implant Crowns on Titanium Bases Following Different Surface Treatments. Int. J. Oral Maxillofac. Implants 2018, 33, 530–535. [Google Scholar] [CrossRef] [PubMed]
- Wiedenmann, F.; Liebermann, A.; Spintzyk, S.; Eichberger, M.; Stawarczyk, B. Influence of Different Cleaning Procedures on Tensile Bond Strength Between Zirconia Abutment and Titanium Base. Int. J. Oral Maxillofac. Implants 2019, 34, 1318–1327. [Google Scholar] [CrossRef] [PubMed]
- Bankoğlu Güngör, M.; Karakoca Nemli, S. The Effect of Resin Cement Type and Thermomechanical Aging on the Retentive Strength of Custom Zirconia Abutments Bonded to Titanium Inserts. Int. J. Oral Maxillofac. Implants 2018, 33, 523–529. [Google Scholar] [CrossRef] [PubMed]
- Gehrke, P.; Alius, J.; Fischer, C.; Erdelt, K.J.; Beuer, F. Retentive strength of two-piece CAD/CAM zirconia implant abutments. Clin. Implant Dent. Relat. Res. 2014, 16, 920–925. [Google Scholar] [CrossRef] [PubMed]
- Abbo, B.; Razzoog, M.E.; Vivas, J.; Sierraalta, M. Resistance to dislodgement of zirconia copings cemented onto titanium abutments of different heights. J. Prosthet. Dent. 2008, 99, 25–29. [Google Scholar] [CrossRef] [PubMed]
- Bergamo, E.; Zahoui, A.; Luri Amorin Ikejiri, L.; Marun, M.; Peixoto da Silva, K.; Coelho, P.G.; Soares, S.; Bonfante, E.A. Retention of zirconia crowns to Ti-base abutments: Effect of luting protocol, abutment treatment and autoclave sterilization. J. Prosthodont. Res. 2021, 65, 171–175. [Google Scholar] [CrossRef] [PubMed]
- Silva, C.E.P.; Soares, S.; Machado, C.M.; Bergamo, E.T.P.; Coelho, P.G.; Witek, L.; Ramalho, I.S.; Jalkh, E.B.B.; Bonfante, E.A. Effect of CAD/CAM Abutment Height and Cement Type on the Retention of Zirconia Crowns. Implant Dent. 2018, 27, 582–587. [Google Scholar] [CrossRef] [PubMed]
- Muñoz, M.; Vilarrasa, J.; Ruíz-Magaz, V.; Albertini, M.; Nart, J. Influence of the abutment height on marginal bone level changes around two-piece dental implants: Meta-analysis and trial sequential analysis of randomized clinical trials. Clin. Oral Implants Res. 2023, 34, 81–94. [Google Scholar] [CrossRef]
- Chen, Z.; Lin, C.Y.; Li, J.; Wang, H.L.; Yu, H. Influence of abutment height on peri-implant marginal bone loss: A systematic review and meta-analysis. J. Prosthet. Dent. 2019, 122, 14–21.e2. [Google Scholar] [CrossRef] [PubMed]
- Emfietzoglou, R.; Dereka, X. Survival Rates of Short Dental Implants (≤6 mm) Used as an Alternative to Longer (>6 mm) Implants for the Rehabilitation of Posterior Partial Edentulism: A Systematic Review of RCTs. Dent. J. 2024, 12, 185. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Rajkumar, G.C.; Aher, V.; Ramaiya, S.; Manjunath, G.S.; Kumar, D.V. Implant placement in the atrophic posterior maxilla with sinus elevation without bone grafting: A 2-year prospective study. Int. J. Oral Maxillofac. Implants 2013, 28, 526–530. [Google Scholar] [CrossRef]
- Jung, R.E.; Al-Nawas, B.; Araujo, M.; Avila-Ortiz, G.; Barter, S.; Brodala, N.; Chappuis, V.; Chen, B.; De Souza, A.; Almeida, R.F.; et al. Group 1 ITI Consensus Report: The influence of implant length and design and medications on clinical and patient-reported outcomes. Clin. Oral Implants Res. 2018, 29 (Suppl. S16), 69–77. [Google Scholar] [CrossRef]
- Carosi, P.; Lorenzi, C.; Lio, F.; Laureti, M.; Ferrigno, N.; Arcuri, C. Short implants (≤6 mm) as an alternative treatment option to maxillary sinus lift. Int. J. Oral Maxillofac. Surg. 2021, 50, 1502–1510. [Google Scholar] [CrossRef]
- Quaranta, A.; Piemontese, M.; Rappelli, G.; Sammartino, G.; Procaccini, M. Technical and biological complications related to crown to implant ratio: A systematic review. Implant Dent. 2014, 23, 180–187. [Google Scholar] [CrossRef] [PubMed]
- Blanes, R.J. To what extent does the crown-implant ratio affect the survival and complications of implant-supported reconstructions? A systematic review. Clin. Oral Implants Res. 2009, 20 (Suppl. S4), 67–72. [Google Scholar] [CrossRef] [PubMed]
- Gehrke, S.A. Importance of Crown Height Ratios in Dental Implants on the Fracture Strength of Different Connection Designs: An In Vitro Study. Clin. Implant. Dent. Relat. Res. 2015, 17, 790–797. [Google Scholar] [CrossRef] [PubMed]
- Cárdenas, R.; Sánchez, D.; Euán, R.; Flores, A.M. Effect of fatigue loading and failure mode of different ceramic implant abutments. J. Prosthet. Dent. 2022, 127, 875–881. [Google Scholar] [CrossRef] [PubMed]
- Graf, T.; Völler, E.; Erdelt, K.; Stimmelmayr, M.; Schubert, O.; Güth, J.F. Monolithic hybrid abutment crowns: Influence of crown height, crown morphology and material on the implant-abutment complex. J. Prosthodont. Res. 2024, 68, 606–614. [Google Scholar] [CrossRef] [PubMed]
- Malchiodi, L.; Cucchi, A.; Ghensi, P.; Consonni, D.; Nocini, P.F. Influence of crown–implant ratio on implant success rates and crestal bone levels: A 36-month follow-up prospective study. Clin. Oral Implants Res. 2014, 25, 240–251. [Google Scholar] [CrossRef]
- Esfahrood, Z.R.; Ahmadi, L.; Karami, E.; Asghari, S. Short dental implants in the posterior maxilla: A review of the literature. J. Korean Assoc. Oral Maxillofac. Surg. 2017, 43, 70–76. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Song, S.R.; Park, K.M.; Jung, B.Y. Fracture strength analysis of titanium insert-reinforced zirconia abutments according to the axial height of the titanium insert with an internal connection. PLoS ONE 2021, 16, e0249208. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zhang M, Lun DK, Pelekos G, Fok MR Clinical performance of implant supported single hybrid abutment crown restoration: A sysyematic review and meta-analysis. J. Prosthod. Res. 2023, 68, 63–77. [CrossRef]
- Takano, R.; Honda, J.; Kobayashi, T.; Kubochi, K.; Takata, H.; Komine, F. Fracture strength of implant-supported hybrid abutment crowns in premolar region fabricated using different restorative CAD/CAM materials. Dent. Mater. J. 2023, 42, 187–192. [Google Scholar] [CrossRef] [PubMed]
- Strasding, M.; Hicklin, S.P.; Todorovic, A.; Fehmer, V.; Mojon, P.; Sailer, I. A multicenter randomized controlled clinical pilot study of buccally micro-veneered lithium-disilicate and zirconia crowns supported by titanium base abutments: 1-year outcomes. Clin. Oral Implants Res. 2023, 34, 56–65. [Google Scholar] [CrossRef]
- Belli, R.; Hurle, K.; Schürrlen, J.; Petschelt, A.; Werbach, K.; Peterlik, H.; Rabe, T.; Mieller, B.; Lohbauer, U. A revised relationship between fracture toughness and Y2O3 content in modern dental zirconias. J. Eur. Ceram. Soc. 2021, 41, 7771–7782. [Google Scholar] [CrossRef]
- Liao, Y.; Gruber, M.; Lukic, H.; McLees, J.; Chen, S.; Boghosian, A.; Megremis, S. Survey of the mechanical and physical behaviors of yttria-stabilized zirconia from multiple dental laboratories. JADA Found. Sci. 2023, 2, 100018. [Google Scholar] [CrossRef]
- Leib, E.W.; Vainio, U.; Pasquarelli, R.M.; Kus, J.; Czaschke, C.; Walter, N.; Janssen, R.; Müller, M.; Schreyer, A.; Weller, H.; et al. Synthesis and thermal stability of zirconia and yttria-stabilized zirconia microspheres. J. Colloid Interface Sci. 2015, 448, 582–592. [Google Scholar] [CrossRef] [PubMed]
- Grech J, Antunes E: Zirconia in dental prosthetics: A literature review. J. Mater. Res. Technol. 2019, 8, 4956–4964. [CrossRef]
- Zhang, F.; Vanmeensel, K.; Inokoshi, M.; Batuk, M.; Hadermann, J.; Van Meerbeek, B.; Naert, I.; Vleugels, J. Critical influence of alumina content on the low temperature degradation of 2–3 mol% yttria-stabilized TZP for dental restorations. J. Eur. Ceram. Soc. 2015, 35, 741–750. [Google Scholar] [CrossRef]
- Yilmaz, B.; Gouveia, D.; Seghi, R.R.; Johnston, W.M.; Lang, L.A. Effect of crown height on the screw joint stability of zirconia screw-retained crowns. J. Prosthet. Dent. 2022, 128, 13. [Google Scholar] [CrossRef]
- Zahoui, A.; Bergamo, E.T.; Marun, M.M.; Silva, K.P.; Coelho, P.G.; Bonfante, E.A. Cementation protocol for bonding zirconia crowns to titanium base CAD/CAM abutments. Int. J. Prosthodont. 2020, 33, 527–535. [Google Scholar] [CrossRef] [PubMed]
- Karasan, D.; Pitta, J.; Zarauz, C.; Strasding, M.; Liu, X.; Fehmer, V.; Sailer, I. Theinfluence of titanium-base abutment geometry and height onmechanical stability of implant-supported single crowns. Clin. Oral Implant. Res. 2024, 35, 1033–1041. [Google Scholar] [CrossRef]
- Favasuli, L.; Mascarenhas, P.S.; Mauricio, P. Laboratory Fracture Resilience of Hybrid Abutments Used in Oral Rehabilitation: A Systematic Review. J. Funct. Biomater. 2022, 13, 120. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chantler, G.M.J.; Evans, D.J.C.; Derksen, W. Clinical performance of single screw-retained implant prostheses restored using titanium base abutments: A systematic review and meta-analysis. Clin. Oral Implant. Res. 2023, 34, 64–85. [Google Scholar] [CrossRef]
- Derksen, W.; Joda, T.; Chantler, J.; Fehmer, V.; Gallucci, G.O.; Gierthmuehlen, P.C.; Ioannidis, A.; Karasan, D.; Lanis, A.; Pala, K.; et al. Group 2 ITI Consensus Report: Technological developments in implant prosthetics. Clin. Oral Implants Res. 2023, 34 (Suppl. S26), 104–111. [Google Scholar] [CrossRef] [PubMed]
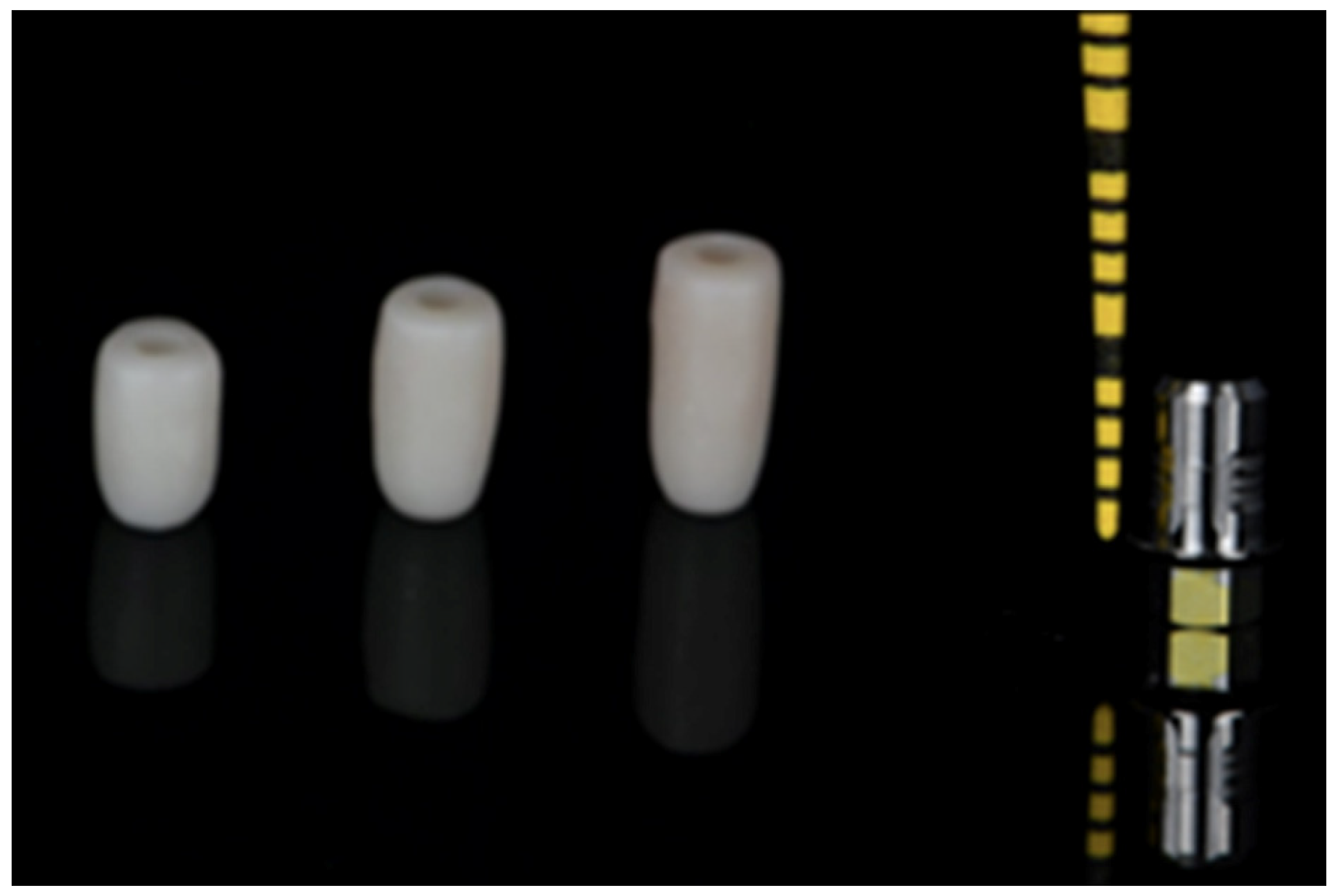




| 3YZ | 8 mm Group 1 | 10 mm Group 2 | 12 mm Group 3 |
| 5YZ | 8 mm Group 4 | 10 mm Group 5 | 12 mm Group 6 |
| Tests of Between-Subjects Effects | |||||
|---|---|---|---|---|---|
| Dependent Variable: Load | |||||
| Source | Type III Sum of Squares | df | Mean Square | F | Sig. |
| Corrected Model | 19,677,166.995 a | 5 | 3,935,433.399 | 37.947 | 0.000 |
| Intercept | 129,883,362.548 | 1 | 129,883,362.548 | 1252.381 | 0.000 |
| Height | 17,107,829.702 | 2 | 8,553,914.851 | 82.480 | 0.000 |
| Material | 1,923,269.165 | 1 | 1,923,269.165 | 18.545 | 0.000 |
| Height * Material | 646,068.128 | 2 | 323,034.064 | 3.115 | 0.052 |
| Error | 5,600,294.524 | 54 | 103,709.158 | ||
| Total | 155,160,824.066 | 60 | |||
| Corrected Total | 25,277,461.518 | 59 | |||
| Tukey B a,b | ||||
|---|---|---|---|---|
| Height (mm) | N | Subset | ||
| 1 | 2 | 3 | ||
| 12 | 20 | 869.6035 | ||
| 10 | 20 | 1376.9680 | ||
| 8 | 20 | 2167.3275 | ||
| Means for groups in homogeneous subsets are displayed. a,b Based on observed means. The error term is mean square (error) = 103,709.158. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Anastasaki, A.; Bora, P.; Kourtis, S.; Fu, C.C. The Effect of Zirconia Material and the Height of the Ceramic Coping on the Strength of Hybrid Ti-Ceramic Abutments. Dent. J. 2025, 13, 284. https://doi.org/10.3390/dj13070284
Anastasaki A, Bora P, Kourtis S, Fu CC. The Effect of Zirconia Material and the Height of the Ceramic Coping on the Strength of Hybrid Ti-Ceramic Abutments. Dentistry Journal. 2025; 13(7):284. https://doi.org/10.3390/dj13070284
Chicago/Turabian StyleAnastasaki, Aikaterini, Pranit Bora, Stefanos Kourtis, and Chin Chuan Fu. 2025. "The Effect of Zirconia Material and the Height of the Ceramic Coping on the Strength of Hybrid Ti-Ceramic Abutments" Dentistry Journal 13, no. 7: 284. https://doi.org/10.3390/dj13070284
APA StyleAnastasaki, A., Bora, P., Kourtis, S., & Fu, C. C. (2025). The Effect of Zirconia Material and the Height of the Ceramic Coping on the Strength of Hybrid Ti-Ceramic Abutments. Dentistry Journal, 13(7), 284. https://doi.org/10.3390/dj13070284







