Mortality Associated with Orofacial Clefts in Brazil
Abstract
1. Introduction
2. Materials and Methods
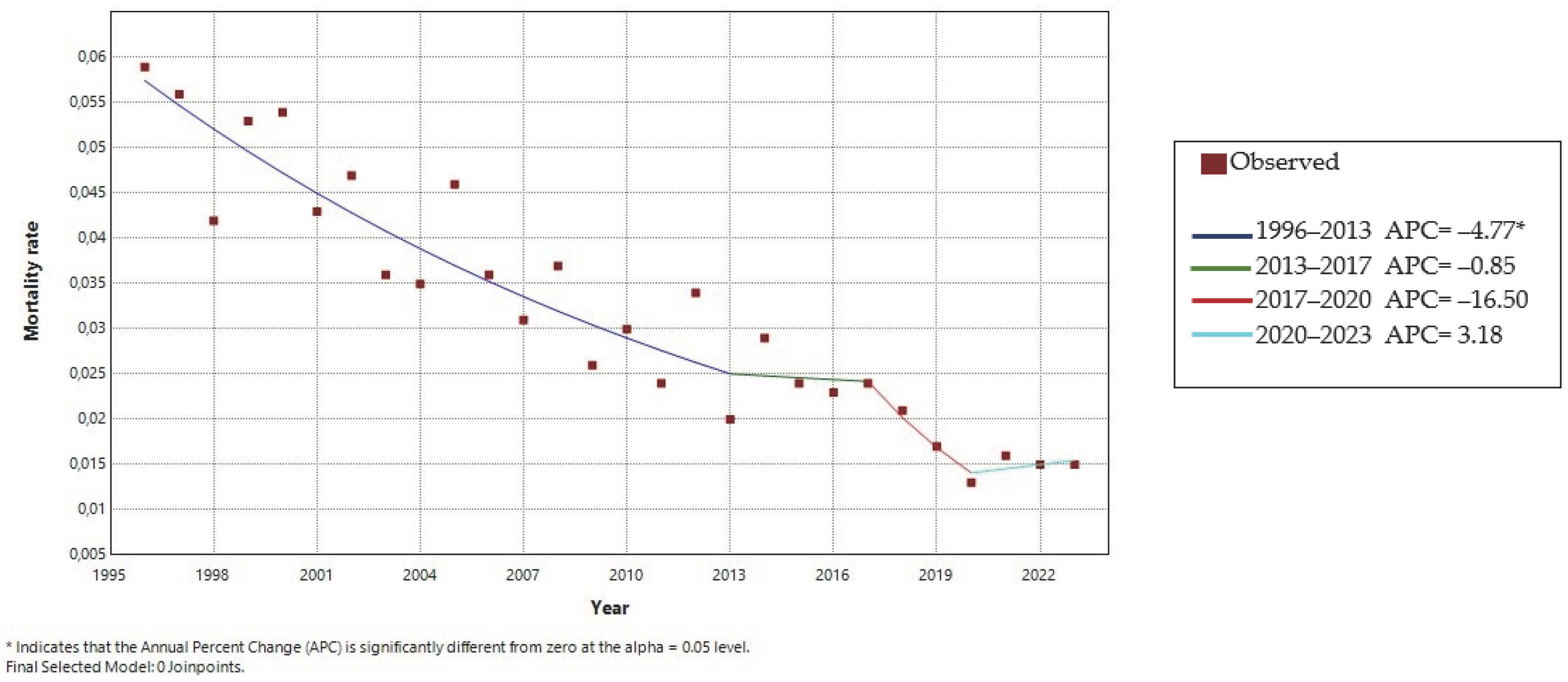
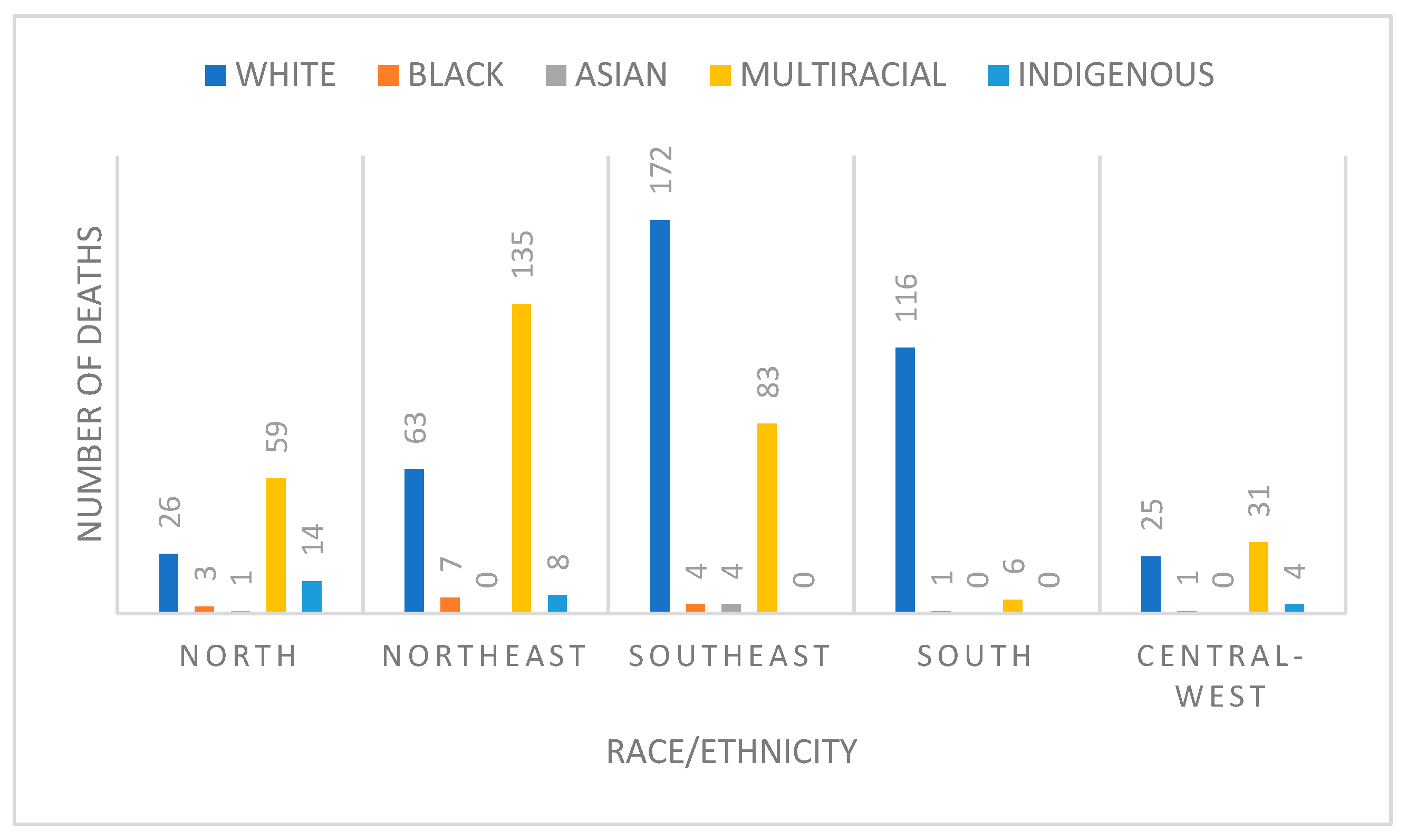
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| SUS | Unified Health System |
| CLP | Cleft lip and palate |
| CLO | Cleft lip only |
| CPO | Cleft palate only |
| DATASUS | Department of Informatics of the Brazilian Unified Health System |
| SINASC | Live Birth Information System |
| ICD-10 | International Classification of Diseases, Tenth Revision |
| DC | Death certificate |
References
- Machado, R.A.; Martelli-Junior, H.; Reis, S.R.A.; Küchler, E.C.; Scariot, R.; das Neves, L.T.; Coletta, R.D. Identification of novel variants in cleft palate-associated genes in Brazilian patients with non-syndromic cleft palate only. Front. Cell Dev. Biol. 2021, 9, 638522. [Google Scholar] [CrossRef] [PubMed]
- Hlongwa, P.; Levin, J.; Rispel, L.C. Epidemiologia e perfil clínico de indivíduos com fissura labiopalatina que utilizam centros de tratamento acadêmico especializados na África do Sul. PLoS ONE 2019, 14, e0215931. [Google Scholar] [CrossRef]
- Martelli-Júnior, H.; Orsi Júnior, J.; Chaves, M.R.; Barros, L.M.; Bonan, P.R.F.; Freitas, J.A. Epidemiological study of cleft lip and palate in Alfenas-Minas Gerais-1986 to 1998. RPG 2006, 13, 31–35. (In Portuguese) [Google Scholar]
- Vyas, T.; Gupta, P.; Kumar, S.; Gupta, R.; Gupta, T.; Singh, H.P. Cleft of lip and palate: A review. J. Family Med. Prim. Care 2020, 9, 2621–2625. [Google Scholar] [CrossRef]
- Hujoel, P.P.; Bollen, A.M.; Mueller, B.A. First-year mortality among infants with facial clefts. Cleft Palate Craniofac. J. 1992, 29, 451–455. [Google Scholar] [CrossRef]
- Christensen, K.; Juel, K.; Herskind, A.M.; Murray, J.C. Long term follow up study of survival associated with cleft lip and palate at birth. BMJ 2004, 328, 1405. [Google Scholar] [CrossRef]
- Ngai, C.W.; Martin, W.L.; Tonks, A.; Wyldes, M.P.; Kilby, M.D. Are isolated facial cleft lip and palate associated with increased perinatal mortality? A cohort study from the West Midlands Region, 1995–1997. J. Matern. Fetal Neonatal Med. 2005, 17, 203–206. [Google Scholar] [CrossRef]
- Carlson, L.; Hatcher, K.W.; Burg, R.V. Elevated infant mortality rates among oral cleft and isolated oral cleft cases: A meta-analysis of studies from 1943 to 2010. Cleft Palate Craniofac. J. 2013, 50, 2–12. [Google Scholar] [CrossRef]
- Malic, C.C.; Lam, M.; Donelle, J.; Richard, L.; Vigod, S.N.; Benchimol, E.I. Incidence, risk factors, and mortality associated with orofacial cleft among children in Ontario, Canada. JAMA Netw. Open 2020, 3, e1921036. [Google Scholar] [CrossRef]
- van Nunen, D.P.F.; van den Boogaard, M.-J.H.; Don Griot, J.P.W.; Rüttermann, M.; van der Veken, L.; Breugem, C.C. Elevated infant mortaity rate among Dutch oral cleft cases: A retrospective analysis from 1997 to 2011. Front. Surg. 2014, 1, 48. [Google Scholar] [CrossRef]
- Huang, R.S.; Mihalache, A.; Riff, K.W.Y.W. Cleft lip and/or palate mortality trends in the USA: A retrospective population-based study. BMJ Paediatr. Open 2024, 8, e002305. [Google Scholar] [CrossRef] [PubMed]
- Goldrick, N.M.; Revie, G.; Groisman, B.; Hurtado-Villa, P.; Sipek, A.; Khoshnood, B.; Rissmann, A.; Dastgiri, S.; Landau, D.; Tagliabue, G.; et al. A multi-program analysis of cleft lip with cleft palate prevalence and mortality using data from 22 International Clearinghouse for Birth Defects Surveillance and Research programs, 1974–2014. Birth Defects Res. 2023, 115, 980–997. [Google Scholar] [CrossRef] [PubMed]
- IPEA, Institute for Applied Economic Research. [Sustainable Development Goals]. 2019. Available online: https://www.ipea.gov.br/ods/ods3.html#:~:text=At%C3%A9%202030%2C%20acabar%20com%20as,25%20por%201.000%20nascidos%20vivos.Acesso%20em%2028%20de%20junho%20de%202024 (accessed on 22 March 2024). (In Portuguese)
- Silveira, D.M.M.L.; Martelli, D.R.B.; Dias, V.O.; Silveira, M.S.C.; Almeida, I.L.F.; Martelli Júnior, H. Surgical rehabilitation of cleft lip and/or palate: Evaluation of the Brazilian public health system. Braz. J. Otorhinolaryngol. 2022, 88, S126–S132. [Google Scholar] [CrossRef] [PubMed]
- CNES. National Register of Health Facilities. [Reports: Accreditations]. Available online: https://cnes2.datasus.gov.br/Mod_Ind_Habilitacoes_Listar.asp?VTipo=0401&VListar=1&VEstado=00&VMun=&VComp=&VContador=34&VTitulo=H (accessed on 22 March 2024). (In Portuguese)
- DATASUS. Tabnet. Available online: https://datasus.saude.gov.br/informacoes-de-saude-tabnet/ (accessed on 21 June 2024).
- World Health Organization. International Statistical Classification of Diseases and Related Health Problems, 10th Revision; University of São Paulo Press: São Paulo, Brazil, 2012; Volume 3. (In Portuguese) [Google Scholar]
- Ishitani, L.H.; França, E. Uso das Causas Múltiplas de Morte em Saúde Pública. Inf. Epidemiológico Do SUS 2001, 10, 163–175. [Google Scholar] [CrossRef]
- Higashi, H.; Barendregt, J.J.; Kassebaum, N.J.; Weiser, T.G.; Bickler, S.W.; Vos, T. The burden of selected congenital anomalies amenable to surgery in low and middle-income regions: Cleft lip and palate, congenital heart anomalies and neural tube defects. Arch. Dis. Child 2015, 100, 233–238. [Google Scholar] [CrossRef]
- Mullassery, D.; Llewellyn, R.S.; Almond, S.L.; Jesudason, E.C.; Losty, P.D. Oesophageal atresia with cleft lip and palate: A marker for associated lethal anomalies? Pediatr. Surg. Int. 2008, 24, 815–817. [Google Scholar] [CrossRef]
- Kang, S.L.; Narayanan, S.B.; Kelsall, W. Oral/perioral reactions to injectable soft tissue fillers: A clinicopathological multicentric study. Cleft Palate Craniofac. J. 2012, 49, 508–511. [Google Scholar] [CrossRef]
- Ryu, J.Y.; Park, T.H.; Cho, B.C.; Choi, K.Y. The prevalence, risk of premature births, mortality and causes of death of cleft lip with or without palate in South Korea: A nationwide population-based cohort study. Int. J. Epidemiol. 2022, 51, 974–983. [Google Scholar] [CrossRef]
- Mugisha, N.; Uwishema, O.; Noureddine, R.; Ghanem, L.; Manoel, A.Z.; Shariff, S. Utilization of mobile surgical units to address surgical needs in remote African communities: A narrative review. BMC Surg. 2024, 24, 304. [Google Scholar] [CrossRef]
- Bedi, G.; Vyas, K.S.; Chung, M.T.; Morrison, S.D.; Asaad, M.; Mardini, S. Telemedicine in International Cleft Care: A Systematic Review. Cleft Palate Craniofacial J. 2021, 58, 1547–1555. [Google Scholar] [CrossRef]
- CEARÁ. Secretaria de Saúde do Estado do Ceará. Linha de Cuidado Para Pessoas com Fissura Labiopalatina; Secretaria de Saúde do Ceará: Fortaleza, Brazil, 2024; 29p. [Google Scholar]
- Molen, M.V.; Breugel, J.M.M.V.; Janssen, N.G.; Admiraal, R.J.C.; van Adrichem, L.N.A.; Bierenbroodspot, F.; Bittermann, D.; van den Boogaard, M.-J.H.; Broos, P.H.; DijkstraPutkamer, J.J.M. Clinical practice guidelines on the treatment of patients with cleft lip, alveolus, and palate: An executive summary. J. Clin. Med. 2021, 10, 4813. [Google Scholar] [CrossRef]
- Wehby, G.L.; Castilla, E.E.; Goco, N.; Rittler, M.; Cosentino, V.; Javois, L.; Kindem, M.; Chakraborty, H.; Dutra, G.; López-Camelo, J.S.; et al. The effect of systematic pediatric care on neonatal mortality and hospitalizations of infants born with oral clefts. BMC Pediatr. 2011, 11, 121. [Google Scholar] [CrossRef] [PubMed]
- Bell, J.C.; Nassar, N.; Bower, C.; Turner, R.M.; Raynes-Greenow, C. Long-term survival for infants born with orofacial clefts in Western Australia. Birth Defects Res. A Clin. Mol. Teratol. 2016, 106, 172–177. [Google Scholar] [CrossRef] [PubMed]
- Zhou, X.; Jiang, Y.; Fang, J.; Wang, H.; Xie, D.; Kuang, H.; Li, T.; Liu, Q.; He, J. Incidence of cleft lip and palate, and epidemiology of perinatal deaths related to cleft lip and palate in Hunan Province, China, 2016–2020. Sci. Rep. 2023, 13, 10304. [Google Scholar] [CrossRef]
- Fertonani, H.P.; Pires, D.E.P.; Biff, D.; Scherer, M.D.A. [Healthcare model: Concepts and challenges for Brazilian primary care]. Ciência Saúde Coletiva 2015, 20, 1869–1878. [Google Scholar] [CrossRef]
- Brazil. Presidency of the Republic. Civil House. Subdepartment for Legal Affairs. Law No. 8,080 of September 19, 1990; Presidency of the Republic. Civil House. Subdepartment for Legal Affairs: Brasilia, Brazil, 1990; Volume 128, pp. 18055–18059. [Google Scholar]
- Operation Smile. [Report on Services Provided in Brazil]. Available online: https://www.operacaosorriso.org.br/wp-content/uploads/2024/04/Relatorio-de-atendimentos-final-2024.pdf (accessed on 22 March 2024). (In Portuguese).


| Age | N |
|---|---|
| 0–27 days | 477 |
| 28–364 days | 403 |
| 1–4 years | 68 |
| 5–9 years | 8 |
| 10–14 years | 6 |
| 15–19 years | 3 |
| 25–29 years | 2 |
| 30–34 years | 4 |
| 40–44 years | 1 |
| 45–49 years | 1 |
| 50–54 years | 4 |
| 65–69 years | 1 |
| 70–74 years | 3 |
| 75–79 years | 2 |
| ≥80 years | 3 |
| Unknown | 1 |
| Sex | n |
| Male | 533 |
| Female | 446 |
| Race | n |
| Caucasian | 402 |
| Multiracial | 314 |
| Unknown | 224 |
| Indigenous | 26 |
| Black | 16 |
| Asian | 5 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Costa, A.d.A.; Farias, H.M.T.; Martelli, D.R.B.; Dias, V.O.; Brazilian Oral Cleft Group; Coletta, R.D.; Martelli Junior, H. Mortality Associated with Orofacial Clefts in Brazil. Dent. J. 2025, 13, 282. https://doi.org/10.3390/dj13070282
Costa AdA, Farias HMT, Martelli DRB, Dias VO, Brazilian Oral Cleft Group, Coletta RD, Martelli Junior H. Mortality Associated with Orofacial Clefts in Brazil. Dentistry Journal. 2025; 13(7):282. https://doi.org/10.3390/dj13070282
Chicago/Turabian StyleCosta, Amanda de Andrade, Hildeth Maisa Torres Farias, Daniella Reis B. Martelli, Verônica Oliveira Dias, Brazilian Oral Cleft Group, Ricardo D. Coletta, and Hercílio Martelli Junior. 2025. "Mortality Associated with Orofacial Clefts in Brazil" Dentistry Journal 13, no. 7: 282. https://doi.org/10.3390/dj13070282
APA StyleCosta, A. d. A., Farias, H. M. T., Martelli, D. R. B., Dias, V. O., Brazilian Oral Cleft Group, Coletta, R. D., & Martelli Junior, H. (2025). Mortality Associated with Orofacial Clefts in Brazil. Dentistry Journal, 13(7), 282. https://doi.org/10.3390/dj13070282






