Craniofacial and Dental Complications Following Total Glossectomy Without Multidisciplinary Follow-Up: A Case Report
Abstract
1. Introduction
2. Case Presentation
2.1. Patient Background
2.2. Functional Examination
2.2.1. Speech
2.2.2. Chewing
2.2.3. Breathing
2.2.4. Swallowing
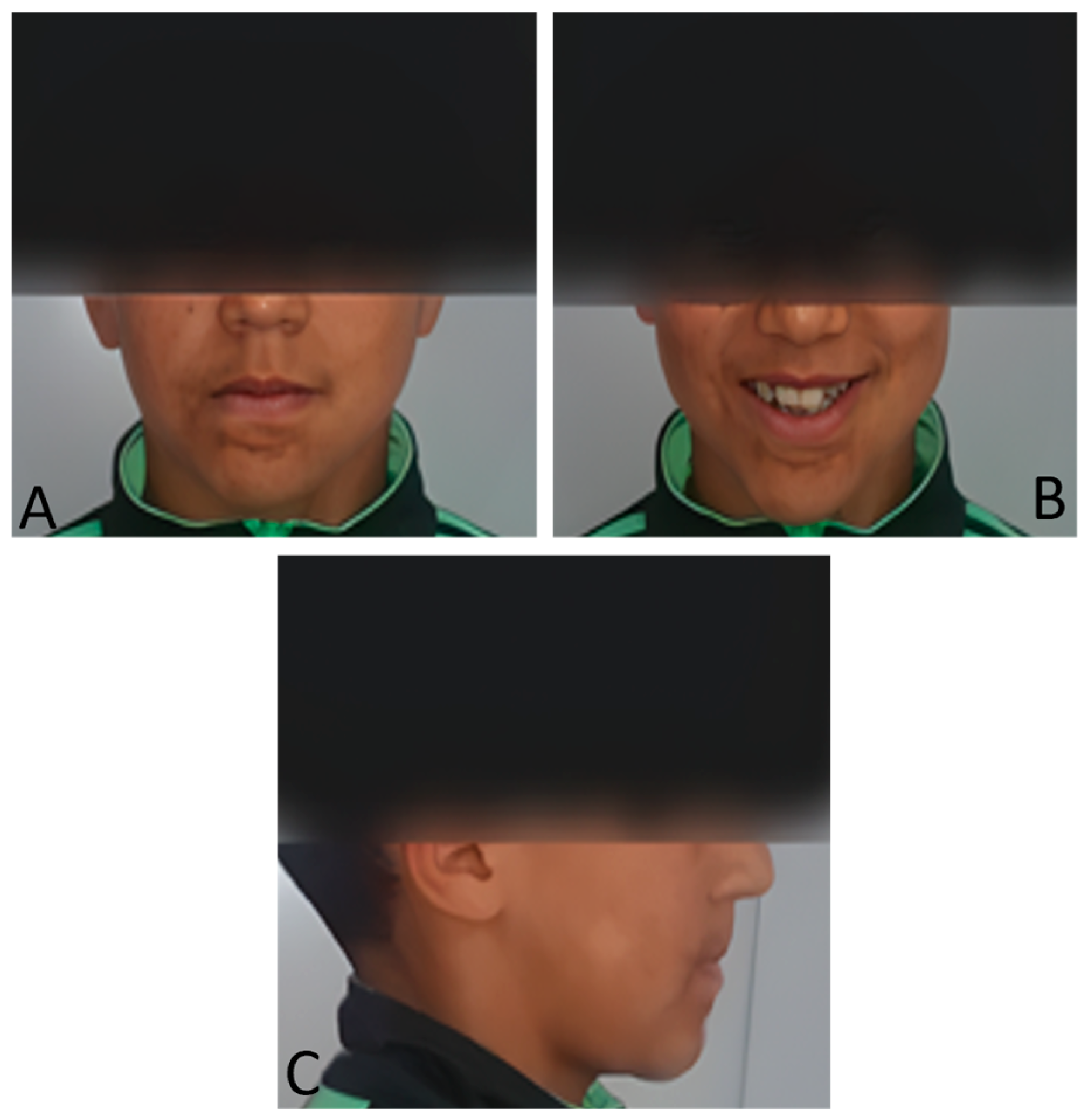
2.3. Extraoral Clinical Examination
- -
- A slight deviation of the chin to the right and an increase in the height of the lower part of the face give it a distinct oval appearance.
- -
- Convex subnasal profile with an open nasolabial angle marked by a subtle scar under the lower lip.
- -
- A disharmonious smile, with a deviation of the upper midline interincisal line to the right from the midsagittal plane.
2.4. Intraoral Clinical Examination (Figure 2)
- -
- Maxillary arch: Crowding of the anterior teeth and a distinctive V-shaped arch are associated with the absence of teeth 14 and 24. Notably, the buccal positions of teeth 13 and 23 and the lingual positions of teeth 12 and 22 demonstrate difficulty in finding space and maintaining good symmetry.
- -
- Mandibular arch: Similar crowding and a V-shape in the mandibular arch are accompanied by the absence of teeth 31, 36, and 45, as well as poor positioning of the incisors, reinforcing the skeletal adaptations caused by the lack of lingual function.
- -
- Interarch relationships: Class III canine and molar relationships characterize a reverse overjet between teeth 26 and 36, with both maxillary and mandibular arches showing endognathia, a hallmark of altered growth patterns.

2.5. Radiographic Examination
- Sagittal Skeletal Relationship: The SNA angle (70°) indicates significant maxillary retro position. The SNB angle (71°) confirms true mandibular retrognathia. Despite this retrognathic mandible, the ANB angle is on the lower end of normal (1°), and the AoBo measurement is severely negative (−7 mm). This combination unequivocally establishes a skeletal Class III relationship.
- Vertical Skeletal Relationship: The most striking finding is a severely hyperdivergent growth pattern, evidenced by the drastically increased GoGn-SN angle (53° compared to a norm of 32° ± 5).
- Dental Compensations: The incisor analysis revealed compensatory adaptations. The upper incisors are proclined (I/NA: 24°) and protruded (itoNA: 7 mm), while the lower incisors are retroclined (I/NB: 19°) and retruded (itoNB: 1 mm), classic mechanisms in skeletal Class III cases.
3. Discussion
Clinical Relevance
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| SNA | The maxilla (point A) is related to the cranial base (SN) |
| SNB | The mandible (point B) is related to the cranial base (SN) |
| AoBo | Represents the projection of the points A and B on the occlusal plane |
| ANB | Is the difference between SNA and SNB |
| I/to NA (mm) | Maxillary incisor position |
| I/to NA | Maxillary incisor version |
| i/ to NB (mm) | Lower incisor position |
| i/ to NB | Lower incisor version |
| Po to NB | Most anterior part of the symphysis of the mandible to line NB |
| GoGnSN | Mandibular plane to cranial base |
References
- Farronato, M.; Fama, A.; Lanteri, V.; Nucci, F.; Farronato, G.; Maspero, C. Lymphangioma of the tongue associated with open bite: Case report. Eur. J. Paediatr. Dent. 2019, 20, 311–314. [Google Scholar] [CrossRef] [PubMed]
- Sharma, S.; Sharma, S. Infected lymphangioma tongue presenting as macroglossia—A case report. Sch. J. Otolaryngol. 2021, 6, 658–660. [Google Scholar] [CrossRef]
- Bektaş-Kayhan, K.; Keskin, Y.; Kesimli, M.C.; Ulusan, M.; Ünür, M. Lymphangioma of the tongue: Report of four cases with dental aspects. Kulak Burun Bogaz Ihtis. Derg. 2014, 24, 172–176. [Google Scholar] [CrossRef]
- Hajeer, M.Y.; Millett, D.T.; Ayoub, A.F.; Siebert, J.P. Applications of 3D imaging in orthodontics: Part I. J. Orthod. 2004, 31, 62–70. [Google Scholar] [CrossRef]
- Chiou, W.-C.; Men, X.; Zhang, K.; Jiang, X.; Chen, S. Three-dimensional evaluation of tongue position and volume in adult patients with different skeletal malocclusions. J. Prev. Treat. Stomatol. Dis. 2025, 33, 33–40. [Google Scholar] [CrossRef]
- Yamaguchi, H.; Sueishi, K. Malocclusion associated with abnormal posture. Bull. Tokyo Dent. Coll. 2003, 44, 43–54. [Google Scholar] [CrossRef]
- Chouchene, F.; Masmoudi, F.; Baaziz, A.; Maatouk, F.; Ghedira, H. Oral manifestations and dental care management of a young patient with lymphangioma of the tongue: A case report. Clin. Case Rep. 2021, 9, e04537. [Google Scholar] [CrossRef]
- Enderby, P. Frenchay Dysarthria Assessment; College-Hill Press: San Diego, CA, USA, 1983. [Google Scholar]
- Tarkowska, A.; Katzer, L.; Ahlers, M.O. Assessment of masticatory performance by means of a color-changeable chewing gum. J. Prosthodont. Res. 2017, 61, 9–19. [Google Scholar] [CrossRef]
- Roithmann, R. Specific tests for nasal permeability. Braz. J. Otorhinolaryngol. 2007, 73, 2. [Google Scholar] [CrossRef] [PubMed]
- Logemann, J.A. Dysphagia: Evaluation and treatment. Folia Phoniatr. Logop. 1995, 47, 140–164. [Google Scholar] [CrossRef] [PubMed]
- Yoon, A.J.; Zaghi, S.; Ha, S.; Law, C.S.; Guilleminault, C.; Liu, S.Y. Ankyloglossia as a risk factor for maxillary hypoplasia and soft palate elongation: A functional-morphological study. Orthod. Craniofac Res. 2017, 20, 237–244. [Google Scholar] [CrossRef]
- Primozic, J.; Farčnik, F.; Perinetti, G.; Richmond, S.; Ovsenik, M. The association of tongue posture with the dentoalveolar maxillary and mandibular morphology in Class III malocclusion: A controlled study. Eur. J. Orthod. 2013, 35, 388–393. [Google Scholar] [CrossRef]
- Mew, J. The influence of the tongue on dentofacial growth. Angle Orthod. 2015, 85, 715–721. [Google Scholar] [CrossRef]
- AlGhamdi, A.; AlBaqami, M. Lymphangioma of the tongue in a pediatric patient. J. Pediatr. Surg. Case Rep. 2021, 75, 102053. [Google Scholar] [CrossRef]
- Deshkar, M.; Thosar, N.R.; Kabra, S.P.; Yeluri, R.; Rathi, N.V. The influence of the tongue on the development of dental malocclusion. Cureus 2024, 16, e61281. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.-J.; Shcherbatyy, V.; Gu, G.; Perkins, J.A. Effects of tongue volume reduction on craniofacial growth: A longitudinal study on orofacial skeletons and dental arches. Arch. Oral Biol. 2008, 53, 919–927. [Google Scholar] [CrossRef]
- Uysal, T.; Yagci, A.; Ucar, F.I.; Veli, I.; Ozer, T. Cone-beam computed tomography evaluation of relationship between tongue volume and lower incisor irregularity. Eur. J. Orthod. 2013, 35, 555–562. [Google Scholar] [CrossRef] [PubMed]
- Nemade, H.; Thaduri, A.; Gondi, J.T.; Chava, S.; Kumar, A.; Raj, P.; Neelap, U.; Akalankam, P.; Rukmangatham, T.M.; Sekara Rao S, L.M.C. Five-year long-term functional and quality of life outcomes in total glossectomy survivors. Eur. Arch. Otorhinolaryngol. 2025, 282, 2063–2070. [Google Scholar] [CrossRef]
- Dzioba, A.; Aalto, D.; Papadopoulos-Nydam, G.; Seikaly, H.; Rieger, J.; Wolfaardt, J.; Osswald, M.; Harris, J.R.; O’COnnell, D.A.; Lazarus, C.; et al. Functional and quality of life outcomes after partial glossectomy: A multi-institutional longitudinal study of the head and neck research network. J. Otolaryngol. Head Neck Surg. 2017, 46, 56. [Google Scholar] [CrossRef]
- Harvold, E.P. The role of function in the etiology and treatment of malocclusion. Am. J. Orthod. 1968, 54, 883–898. [Google Scholar] [CrossRef]
- Schumacher, G.H.; Becker, R.; Hubner, A.; Pommerenke, F. The tongue as a factor in craniofacial growth. Anat. Anz. 1988, 166, 309–315. [Google Scholar] [PubMed]
- Defabianis, P.; Carli, E.; Cogo, C.; Ninivaggi, R. Mechanics of facial growth in young patients. Eur. J. Paediatr. Dent. 2022, 23, 265–270. [Google Scholar] [CrossRef]
- Piancino, M.G.; Talpone, F.; Dalmasso, P.; Debernardi, C.; Lewin, A.; Bracco, P. Reverse-sequencing chewing patterns before and after treatment of children with a unilateral posterior cross-bite. Eur. J. Orthod. 2006, 28, 480–484. [Google Scholar] [CrossRef]
- Cayley, A.S.; Tindall, A.P.; Sampson, W.J.; Butcher, A.R. Electropalatographic and cephalometric assessment of tongue function in open bite and non-open bite subjects. Eur. J. Orthod. 2000, 22, 463–474. [Google Scholar] [CrossRef]
- Fuhrmann, R.A.; Diedrich, P.R. B-mode ultrasound scanning of the tongue during swallowing. Dentomaxillofac. Radiol. 1994, 23, 211–2115. [Google Scholar] [CrossRef] [PubMed]
- Bommarito, S.; Zanato, L.E.; Vieira, M.M.; Angelieri, F. Aglossia: Case report. Int. Arch. Otorhinolaryngol. 2016, 20, 95–97. [Google Scholar] [CrossRef]
- Kharade, P.; Dholam, K.; Bachher, G. Appraisal of function after rehabilitation with tongue prosthesis. J. Craniofacial Surg. 2018, 29, e41–e44. [Google Scholar] [CrossRef] [PubMed]
- Schneider-Moser, U.E.M.; Moser, L. Very early orthodontic treatment: When, why and how? Dent. Press J. Orthod. 2022, 27, e22spe2. [Google Scholar] [CrossRef]
- Artese, F. A broader look at interceptive orthodontics: What can we offer. Dent. Press J. Orthod. 2019, 24, 7–8. [Google Scholar] [CrossRef]


| Parameter | Patient | Norm | Interpretation |
|---|---|---|---|
| SNA | 82° ± 2 | 70° | Maxillary retroposition |
| SNB | 80° ± 2 | 71° | Mandibular retrognathia |
| ANB | 2° ± 2 | 1° | Normal sagittal relationship |
| AoBo | 0 ± 2 | −7 mm | Skeletal Class III |
| GoGn/SN | 32° ± 5 | 53° | Hyperdivergent vertical growth |
| I/NA | 22° | 24° | Upper incisor proclination |
| itoNA | 4 mm | 7 mm | Upper incisor protrusion |
| I/NB | 25° | 19° | Lower incisor retroclination |
| itoNB | 4 mm | 1 mm | Lower incisor retrusion |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Salek, F.; Bahije, L.; Zaoui, F. Craniofacial and Dental Complications Following Total Glossectomy Without Multidisciplinary Follow-Up: A Case Report. Dent. J. 2025, 13, 559. https://doi.org/10.3390/dj13120559
Salek F, Bahije L, Zaoui F. Craniofacial and Dental Complications Following Total Glossectomy Without Multidisciplinary Follow-Up: A Case Report. Dentistry Journal. 2025; 13(12):559. https://doi.org/10.3390/dj13120559
Chicago/Turabian StyleSalek, Fatima, Loubna Bahije, and Fatima Zaoui. 2025. "Craniofacial and Dental Complications Following Total Glossectomy Without Multidisciplinary Follow-Up: A Case Report" Dentistry Journal 13, no. 12: 559. https://doi.org/10.3390/dj13120559
APA StyleSalek, F., Bahije, L., & Zaoui, F. (2025). Craniofacial and Dental Complications Following Total Glossectomy Without Multidisciplinary Follow-Up: A Case Report. Dentistry Journal, 13(12), 559. https://doi.org/10.3390/dj13120559




