Oral Health Status Among Children and Adolescents from Vulnerable Populations: A Cross-Sectional Study in Seville, Spain
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Eligibility Criteria
- Risk of severe poverty or severe material deprivation: Household income below the extreme poverty threshold.
- Very low work intensity within the household.
- Complex family situation: single-parent families with low income; large families with all members unemployed; immigrant families in an irregular administrative situation or recent arrivals.
- Recipients of social aid programs: families receiving the Minimum Vital Income (IMV) or the Minimum Social Insertion Income of Andalusia (RMISA).
- Children or adolescents eligible for free school meal grants due to socioeconomic reasons.
2.3. Clinical Examination
- For caries experience, dft (decayed, filled, and extracted teeth in primary dentition) and DMFT (decayed, missing, and filled teeth in permanent dentition) were recorded as dft in primary teeth and DMFT in permanent teeth. In mixed dentition, both indices were recorded separately, following WHO recommendations.
- Pulp therapy needs were determined based on clinical diagnosis. Pulp therapy needs were determined clinically following WHO and AAPD guidance: deep carious lesions with clinical signs of irreversible pulpitis (spontaneous/nocturnal pain, tenderness to percussion), presence of fistula/abscess, or extensive cavitated lesions with pulp exposure. Radiographs were not systematically available; diagnosis was primarily clinical.
- Oral hygiene practices, including brushing frequency, use of fluoridated toothpaste, and dental floss, were recorded. Toothbrushing frequency was recorded as <1/day, 1/day, 2/day, or >2/day; “infrequent brushing” was defined as ≤1/day.
- Dietary habits, specifically the frequency of free-sugar consumption, were recorded. Free-sugar intake was captured in four categories (≤1/week, 2–4/week, 1/day, and ≥2/day). For regression, it was dichotomized into low (≤1/day) vs. high (≥2/day).
2.4. Sociodemographic Variables
2.5. Statistical Analysis
2.6. Ethical Considerations
3. Results
3.1. Sociodemographic Characteristics
3.2. Caries Indices
3.2.1. Primary Dentition (Dft Index)
3.2.2. Permanent Dentition (DMFT Index)
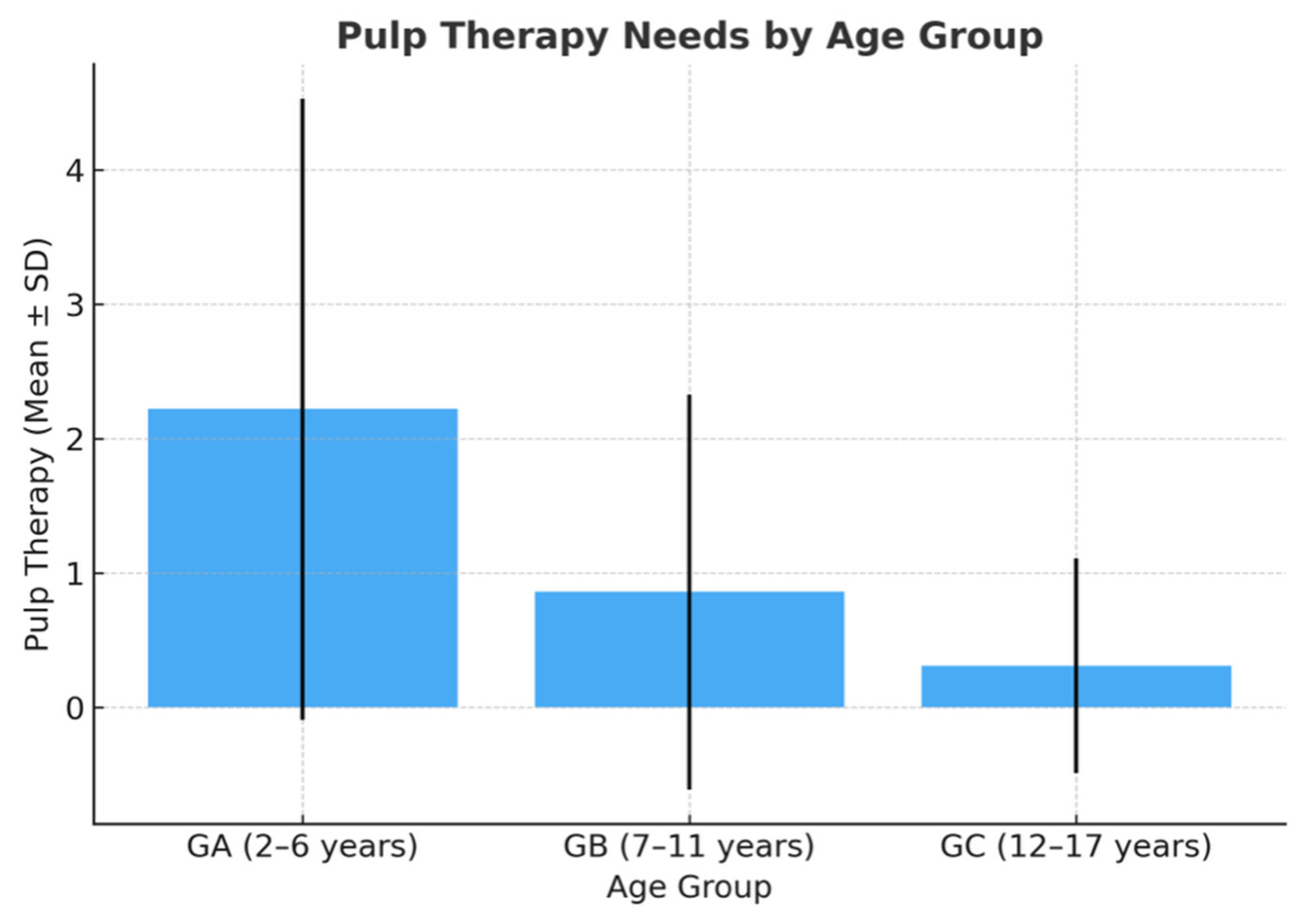
3.2.3. Pulp Therapy Needs
3.3. Oral Hygiene Habits
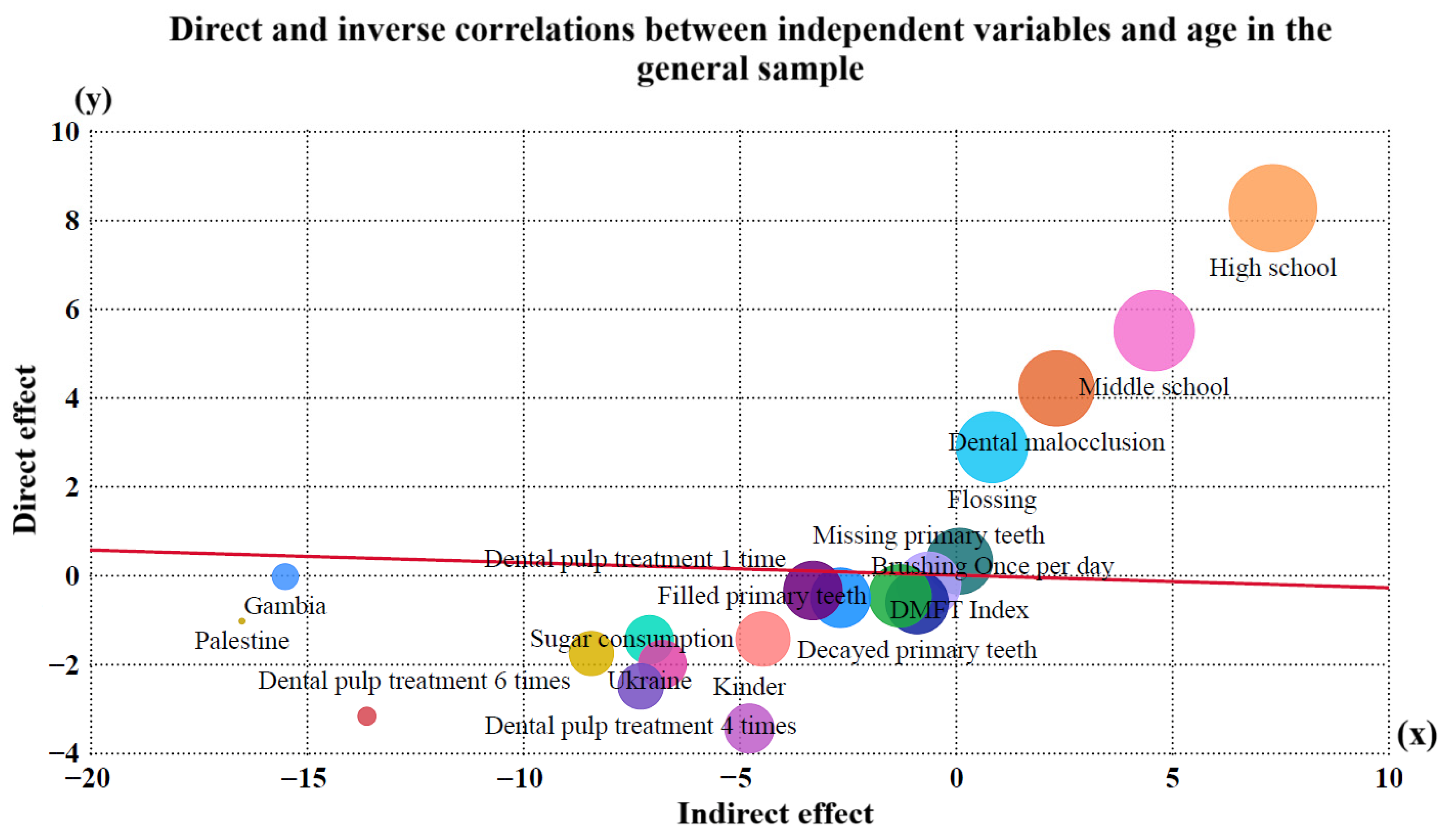
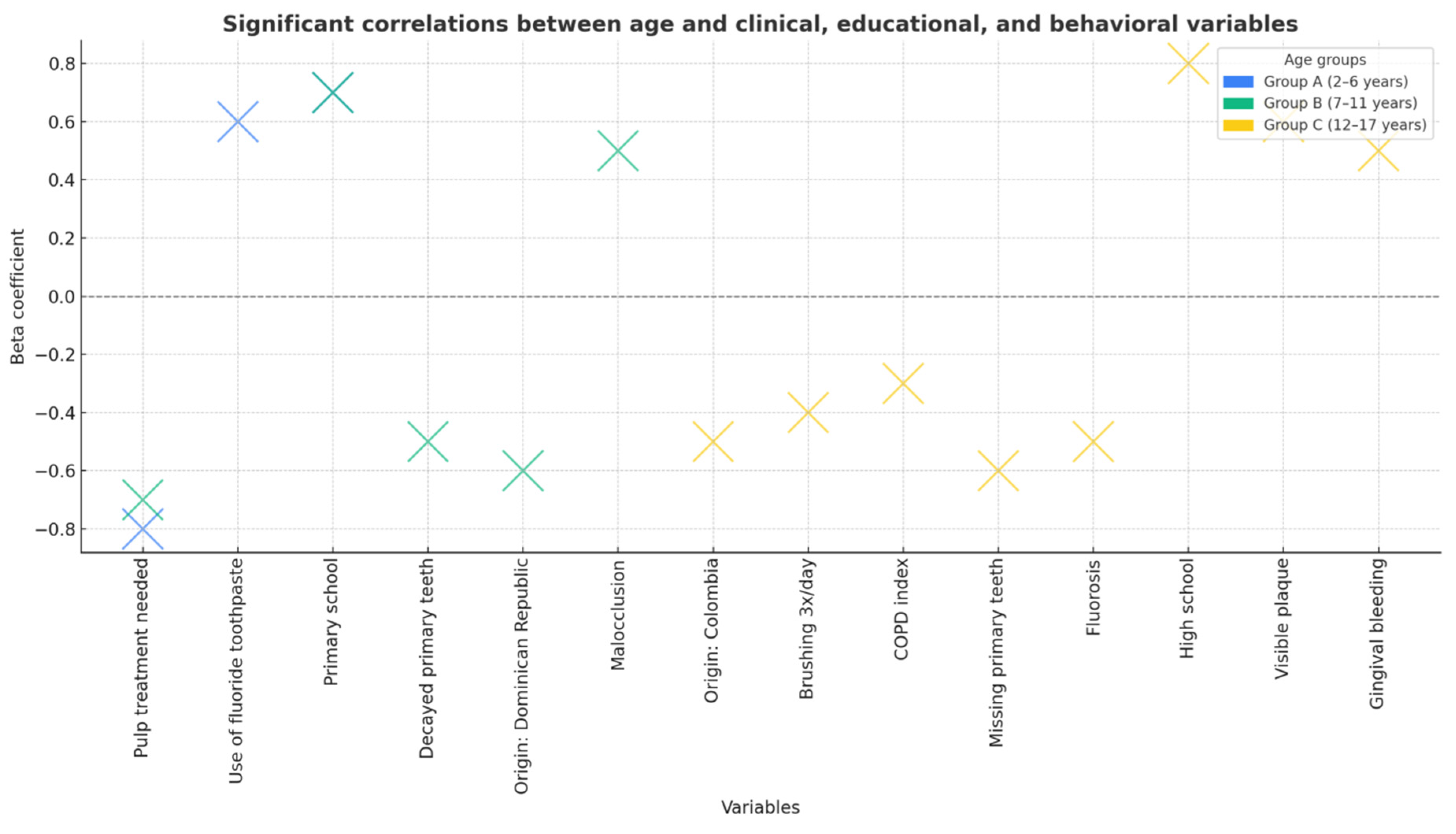
3.4. Multivariate Analysis
4. Discussion
4.1. Impact of Migrant Status on Oral Health
4.2. Educational Level and Health Inequalities
4.3. Behavioral and Dietary Determinants
4.4. Access to Dental Care Services
4.5. Comparison with European and Global Data
4.6. Strengths and Limitations
4.7. Public Health Implications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Peres, M.A.; Macpherson, L.M.D.; Weyant, R.J.; Daly, B.; Venturelli, R.; Mathur, M.R.; Listl, S.; Celeste, R.K.; Guarnizo-Herreño, C.C.; Kearns, C.; et al. Oral diseases: A global public health challenge. Lancet 2019, 394, 249–260. [Google Scholar] [CrossRef]
- Watt, R.G.; Sheiham, A. Integrating the common risk factor approach into a social determinants framework. Community Dent. Oral Epidemiol. 2012, 40, 289–296. [Google Scholar] [CrossRef]
- World Health Organization. Global Oral Health Strategy and Action Plan 2023–2030; WHO: Geneva, Switzerland, 2024; Available online: https://www.who.int/publications/i/item/9789240090538 (accessed on 10 September 2025).
- Institutos Odontológicos. El Barómetro de la Salud Bucodental en España 2025 Alerta de los Malos Hábitos de Higiene Dental Infantil. Immedicohospitalario.es. 2025. Available online: https://www.immedicohospitalario.es/noticia/50378/el-barometro-de-la-salud-bucodental-en-espana-2025-alerta-de-los-mal.html (accessed on 10 September 2025).
- Consejo General de Dentistas de España. Uno de Cada Cinco Menores Sufre Dolores Dentales Frecuentes Debido al Estado de su Boca. Consejodentistas.es; 2025. Available online: https://www.consejodentistas.es (accessed on 10 September 2025).
- Ministerio de Sanidad. Plan para la Ampliación de la Cartera Común de Servicios de Salud Bucodental en el Sistema Nacional de Salud; Ministerio de Sanidad: Madrid, Spain, 2022; Available online: https://www.sanidad.gob.es (accessed on 10 September 2025).
- Bravo Pérez, M.; Llodra, J.C.; Cortés-Martinicorena, F.J.; Baca, P.; Castillo, R.; Cuenca, E. Encuesta de salud oral en población infantil española 2010. Rev. Cons. Odontoestomatol. España (RCOE) 2012, 17, 5–20. [Google Scholar]
- Cubero Santos, A.; Lorido Cano, I.; González Huéscar, A.; Ferrer García, M.; Zapata Carrasco, M.; Ambel Sánchez, J.L. Prevalencia de caries dental en escolares de educación infantil de la Comunidad de Madrid. Pediatr. Aten. Primaria 2019, 24, 93–101. [Google Scholar]
- Gonçalves Riatto, S. Estudio Epidemiológico de Salud Oral en una Población Infantil del Área de Salud de Salamanca. Ph.D Thesis, Universidad de Salamanca, Salamanca, Spain, 2015. [Google Scholar]
- Blomma, C.; De Boever, A.; Vanobbergen, J.; De Clercq, M.; De Visschere, L.; Bottenberg, P. Persistent oral health inequality in children—Repeated cross-sectional study. BMC Public Health 2024, 24, 597. [Google Scholar] [CrossRef]
- Sanz, M.; Bravo, M.; Llodra, J.C. Prevalencia de hábitos bucodentales saludables en la población infantil española. An. Pediatría 2011, 75, 121–126. [Google Scholar]
- Donte Group. Salud Bucodental y Exclusión Económica; Donte Group: Madrid, Spain, 2023. [Google Scholar]
- Goldfeld, S.; Francis, K.L.; O’Connor, E.; Ludvigsson, J.; Faresjö, T.; Nikiema, B.; Gauvin, L.; Yang-Huang, J.; Awad, Y.A.; McGrath, J.J.; et al. Comparative inequalities in child dental caries across four countries: Examination of international birth cohorts and implications for oral health policy. PLoS ONE 2022, 17, e0268899. [Google Scholar] [CrossRef] [PubMed]
- Fletcher, R.H.; Fletcher, S.W.; Fletcher, G.S. Clinical Epidemiology: The Essentials, 5th ed; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2013. [Google Scholar]
- Marmot, M. Social determinants of health inequalities. Lancet 2005, 365, 1099–1104. [Google Scholar] [CrossRef]
- Bravo Pérez, M.; Almerich Silla, J.M.; Canorea Díaz, E.; Casals Peidró, E.; Cortés Martinicorena, F.J.; Expósito Delgado, A.; Gómez Santos, G.; Hidalgo Olivares, G.; Lamas Oliveira, M.; Martínez Beneyto, Y.; et al. Encuesta de Salud Oral en España 2020; Consejo General de Dentistas: Madrid, Spain, 2020. [Google Scholar]
- EAPN Andalucía. Report on the State of Poverty in Andalusia 2023: Monitoring of Indicators; EAPN Andalucía: Seville, Spain, 2024; Available online: https://www.eapn-andalucia.org (accessed on 10 September 2025).
- National Institute of Statistics (INE). Active Population Survey (EPA). Unemployment Rates by Province; INE: Madrid, Spain, 2024; Available online: https://www.ine.es (accessed on 10 September 2025).
- Prieto-Regueiro, B.; Gómez-Santos, G.; Grini, D.; Burgueño-Torres, L.; Diéguez-Pérez, M. Relevance of sociocultural inequalities and parents’ origins in relation to the oral health of preschoolers in Lanzarote, Spain. Healthcare 2023, 11, 2344. [Google Scholar] [CrossRef] [PubMed]
- Vallejos, D.; Coll, I.; López-Safont, N. Association between oral health status and sociodemographic factors among 5–15-year-old schoolchildren from Mallorca, Spain: A cross-sectional study. Children 2025, 12, 527. [Google Scholar] [CrossRef]
- Klein, H.; Palmer, C.E.; Knutson, J.W. Studies on dental caries. Public Health Rep. 1938, 53, 751–765. [Google Scholar] [CrossRef]
- Silness, J.; Löe, H. Periodontal disease in pregnancy II. Acta Odontol. Scand. 1964, 22, 121–135. [Google Scholar] [CrossRef]
- Dean, H.T. Classification of mottled enamel diagnosis. J. Am. Dent. Assoc. 1942, 28, 1421–1426. [Google Scholar] [CrossRef]
- Weerheijm, K.L. Molar incisor hypomineralization (MIH). Eur. J. Paediatr. Dent. 2004, 5, 114–120. [Google Scholar]
- World Health Organization. Oral Health Surveys: Basic Methods, 5th ed.; WHO: Geneva, Switzerland, 2013; Available online: https://www.who.int/publications/i/item/9789241548649 (accessed on 10 September 2025).
- Petersen, P.E. World Health Organization global policy for improvement of oral health: World Health Assembly 2007. Int. Dent. J. 2008, 58, 115–121. [Google Scholar] [CrossRef] [PubMed]
- European Academy of Paediatric Dentistry (EAPD). Guidelines on Preventive Oral Care in Children; EAPD: Athens, Greece, 2020; Available online: https://www.eapd.eu (accessed on 10 September 2025).
- Cubero-Santos, A.; Lorido Cano, I.; González Huéscar, A.; Ferrer García, M.A.; Zapata Carrasco, M.D.; Ambel Sánchez, J.L. Prevalencia de caries dental en escolares de educación infantil y primaria en Badajoz: Disparidades socioeconómicas y origen migrante. Rev. Pediatr. Aten. Primaria 2019, 21, e47–e59. [Google Scholar]
- Veloso Duran, A.; Framis-de-Mena, B.; Vázquez Salceda, M.C.; Guinot Jimeno, F. Oral health status comparison between Spanish and immigrant children aged 3 to 12 years in Barcelona. Children 2022, 9, 1389. [Google Scholar] [CrossRef] [PubMed]
- Gallardo, V.P.; Cencillo, C.P.; Plana, B.M. Prevalencia de la caries dental en el niño inmigrante: Estudio comparativo con el niño autóctono. An. Pediatr. 2006, 65, 337–341. [Google Scholar] [CrossRef]
- Navarro Félez, I.; Martínez Angulo, L.; Gascó Eguiluz, M.; Coy Vidal, C.; García Canela, M.; Tajada Vitales, C.; de la Fuente Cadenas, G.A. Influence of nationality on the prevalence of frequent diseases in Primary Health Care. Rev. Pediatr. Aten. Primaria 2020, 22, 1–11. [Google Scholar]
- Kizi, G.; Barata, A.R.; Ventura, I.; Flores-Fraile, J.; Ribas-Pérez, D.; Castaño-Séiquer, A. Oral health in migrant children in Melilla, Spain. Children 2023, 10, 888. [Google Scholar] [CrossRef]
- Ribas-Pérez, D.; Sevillano Garcés, D.; Rodríguez Menacho, D.; Hernández-Franch, P.V.; Barbero Navarro, I.; Castaño-Séiquer, A. Cross-sectional study on oral health-related quality of life using OHIP-14 in migrant children in Melilla (Spain). Children 2023, 10, 1168. [Google Scholar] [CrossRef] [PubMed]
- Gonçalves Riatto, S.; Montero, J.; Ribas Pérez, D.; Castaño-Séiquer, A.; Dib, A. Oral health status of Syrian children in the refugee center of Melilla, Spain. Int. J. Dent. 2018, 2018, 2637508. [Google Scholar] [CrossRef] [PubMed]
- Martín Hernández, J.; Barbero Navarro, I.; Rodríguez Menacho, D.; Villalva Hernández, P.; Barrera Mora, J.M.; Ribas-Pérez, D.; Castaño-Séiquer, A. Social determinants of oral health in migrants at the Spanish border. Front. Public Health. 2025, 13, 1641311. [Google Scholar] [CrossRef]
- Almerich-Torres, T.; Montiel-Company, J.M.; Bellot-Arcís, C.; Almerich-Silla, J.M. Relationship between caries, body mass index and social class in Spanish children. Gac. Sanit. 2017, 31, 499–504. [Google Scholar] [CrossRef] [PubMed][Green Version]
- de Paula, J.S.; Ambrosano, G.M.B.; Mialhe, F.L. The impact of social determinants on schoolchildren’s oral health in Brazil. Braz. Oral Res. 2015, 29, 1–9. [Google Scholar] [CrossRef]
- Téllez, M.; Zini, A.; Estupiñán-Day, S. Social determinants of dental health. Curr. Oral Health Rep. 2014, 1, 149–156. [Google Scholar] [CrossRef]
- Almajed, O.S.; A Aljouie, A.; Alharbi, M.S.; Alsulaimi, L.M. The Impact of Socioeconomic Factors on Pediatric Oral Health: A Review. Cureus 2024, 16, e53567. [Google Scholar] [CrossRef]
- Do, L.G.; Song, Y.H.; Du, M.; Spencer, A.J.; Ha, D.H. Socioecological determinants of child oral health—A scoping review. Community Dent. Oral Epidemiol. 2022, 51, 1024–1036. [Google Scholar] [CrossRef]
- Kateeb, E.; Lim, S.; Amer, S.; Ismail, A. Behavioral and social determinants of early childhood caries among Palestinian preschoolers in Jerusalem area: A cross-sectional study. BMC Oral Heal. 2023, 23, 152. [Google Scholar] [CrossRef]
- World Health Organization. Oral Health: Key Facts; WHO: Geneva, Switzerland, 2025; Available online: https://www.who.int/news-room/fact-sheets/detail/oral-health (accessed on 10 September 2025).
- Morata Alba J, Morata Alba L. Oral health in children. Should we improve their education? Rev. Pediatr. Aten. Primaria 2019, 21, 173–178. [Google Scholar]
- Tapias-Ledesma, M.A.; Garrido, P.C.; Y Peña, M.E.; Hernánez-Barrera, V.; de Miguel, A.G.; Jiménez-Garcia, R. Use of dental care and prevalence of caries among immigrant and Spanish-born children. J. Dent. Child. 2011, 78, 36–42. [Google Scholar]
- Bravo-Pérez, M.; Casals-Peidró, E.; Cortés-Martinicorena, F.J.; Llodra-Calvo, J.C. Encuesta de salud oral en España 2020. RCOE Rev. Ilustre Cons. Gen. Col. Odontólogos Estomatólogos España 2021, 26, 7–45. [Google Scholar]
- Ministerio de Sanidad. Informe de Salud Bucodental Infantil en España 2023; Ministerio de Sanidad: Madrid, Spain, 2023. [Google Scholar]
- Fernández-Cevallos, A.D.; Ribas-Perez, D.; Arenas-González, M.; Elkhoury-Moreno, L.; Torrejón-Martínez, J.; Rosel-Gallardo, E.; Castaño-Seiquer, A.L. Impact of dental aesthetics on self-esteem in students at the Polígono Sur education permanent center in Seville, Spain. Sci. Rep. 2025, 15, 15550. [Google Scholar] [CrossRef]
- Piovesan, C.; Mendes, F.M.; Ferreira, F.V.; Guedes, R.S.; Ardenghi, T.M. Socioeconomic inequalities in the distribution of dental caries in Brazilian preschool children. J. Public Heal. Dent. 2010, 70, 319–326. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Oral Health Status Report: Towards Universal Health Coverage for Oral Health by 2030; WHO: Geneva, Switzerland, 2022; Available online: https://www.who.int/publications/i/item/9789240061484 (accessed on 10 September 2025).
- Petersen, P.E. Global policy for improvement of oral health in the 21st century—Implications to oral health research of World Health Assembly 2007, World Health Organization. Community Dent. Oral Epidemiol. 2009, 37, 1–8. [Google Scholar] [CrossRef]
- Watt, R.G.; Daly, B.; Allison, P.; Macpherson, L.M.; Venturelli, R.; Listl, S.; Weyant, R.J.; Mathur, M.R.; Guarnizo-Herreño, C.C.; Benzian, H. Ending the neglect of oral health: A call for global action. Lancet 2020, 395, 2468–2478. [Google Scholar]
- Bech Barcaz, L.; Ribas-Pérez, D.; Villalva Hernandez-Franch, P.; El Khoury-Moreno, L.; Torrejón-Martínez, J.; Castaño-Séiquer, A. MIH and cavities as markers of oral health inequality in children from Southwest Andalusia (Spain). Dent. J. 2025, 13, 345. [Google Scholar] [CrossRef]
- Rodríguez, L. La Fundación Luis Séiquer afianza su red de clínicas solidarias. Gac. Dent. 2021, 337, 158–163. [Google Scholar]
- Luis Séiquer Social Dentistry Foundation. Who We Are? FOS: Seville, Spain, 2025; Available online: https://fundacionodontologiasocial.org/inicio-pro/ (accessed on 10 September 2025).
- Gudipaneni, R.K.; Alruwaili, M.F.O.; Ganji, K.K.; Karobari, M.I.; Kulkarni, S.; Metta, K.K.; Assiry, A.A.; Israelsson, N.; Bawazir, O.A. Sociobehavioural Factors Associated with Child Oral Health During COVID-19 Pandemic. Saudi Dent J. 2023, 35, 307–312. [Google Scholar]

| Variable | Category | GA (2–6 Years, n = 37) | GB (7–11 Years, n = 107) | GC (12–17 Years, n = 106) | Total (n = 250) | Overall Mean ± SD |
|---|---|---|---|---|---|---|
| Age | 5.08 ± 1.06 | 8.98 ± 1.43 | 14.98 ± 1.67 | 250 | 10.95 ± 3.99 | |
| Sex | Female | 18 (48.6%) | 49 (45.8%) | 56 (52.8%) | 123 (49.2%) | |
| Male | 19 (51.4%) | 58 (54.2%) | 50 (47.2%) | 127 (50.8%) | ||
| Country of Origin | Spanish | 10 (27.0%) | 49 (45.8%) | 56 (52.8%) | 115 (46.0%) | |
| Latin American | 14 (37.8%) | 36 (33.6%) | 31 (29.2%) | 81 (32.4%) | ||
| African | 8 (21.6%) | 19 (17.8%) | 17 (16.0%) | 44 (17.6%) | ||
| Other | 6 (16.2%) | 3 (2.8%) | 2 (1.9%) | 11 (4.4%) | ||
| School Grade | Kindergarten | 19 (51.4%) | 2 (1.9%) | 0 (0.0%) | 21 (8.4%) | |
| Primary School | 18 (48.6%) | 105 (98.1%) | 2 (1.9%) | 125 (50.0%) | ||
| Secondary School | 0 (0.0%) | 0 (0.0%) | 53 (50.0%) | 53 (21.2%) | ||
| Upper Secondary | 0 (0.0%) | 0 (0.0%) | 51 (48.1%) | 51 (20.4%) |
| Group | n | Mean | SD |
|---|---|---|---|
| GA (2–6 years) | 37 | 2.22 | 2.31 |
| GB (7–11 years) | 107 | 0.86 | 1.47 |
| GC (12–17 years) | 106 | 0.31 | 0.80 |
| Predictor (Reference) | B (Unstd.) | β (Std.) | 95% CI (Lower–Upper) | p-Value |
|---|---|---|---|---|
| Decayed primary teeth (yes) | −0.754 | −0.606 | −0.892 to −0.616 | <0.001 |
| Missing primary teeth (yes) | −0.410 | −0.157 | −0.622 to −0.198 | <0.001 |
| Filled primary teeth (yes) | −0.876 | −0.170 | −1.288 to −0.464 | <0.001 |
| Gambia (yes) | −7.765 | −0.123 | −15.498 to −0.033 | 0.049 |
| Palestine (yes) | −8.765 | −0.139 | −16.498 to −1.033 | 0.026 |
| Ukraine (yes) | −4.265 | −0.189 | −7.080 to −1.450 | 0.003 |
| Educational level: Kindergarten (yes) | −4.108 | −0.286 | −4.769 to −3.447 | <0.001 |
| Brushing frequency: once per day (yes) | −1.584 | −0.193 | −2.662 to −0.507 | 0.004 |
| Frequent sugar consumption (yes) | −2.945 | −0.237 | −4.456 to −1.434 | <0.001 |
| Need for pulp therapy: 1 tooth | −1.822 | −0.146 | −3.299 to −0.345 | 0.016 |
| Need for pulp therapy: 3 teeth | −4.391 | −0.216 | −6.780 to −2.002 | <0.001 |
| Need for pulp therapy: 4 teeth | −4.891 | −0.241 | −7.280 to −2.502 | <0.001 |
| Need for pulp therapy: 6 teeth | −5.091 | −0.179 | −8.421 to −1.761 | 0.003 |
| Need for pulp therapy: 8 teeth | −8.391 | −0.188 | −13.610 to −3.172 | 0.002 |
| DMFT Index | 0.203 | 0.186 | 0.089 to 0.316 | 0.001 |
| Educational level: Middle school (yes) | 5.047 | 0.518 | 4.588 to 5.507 | <0.001 |
| Educational level: High school (yes) | 7.799 | 0.789 | 7.334 to 8.265 | <0.001 |
| Flossing (yes) | 1.860 | 0.223 | 0.841 to 2.880 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Reyes-Lara, R.E.; Curto, A.; Ribas-Perez, D.; Barbero-Navarro, I.; Rodriguez-Menacho, D.; Flores-Fraile, J.; Castaño-Séiquer, A. Oral Health Status Among Children and Adolescents from Vulnerable Populations: A Cross-Sectional Study in Seville, Spain. Dent. J. 2025, 13, 522. https://doi.org/10.3390/dj13110522
Reyes-Lara RE, Curto A, Ribas-Perez D, Barbero-Navarro I, Rodriguez-Menacho D, Flores-Fraile J, Castaño-Séiquer A. Oral Health Status Among Children and Adolescents from Vulnerable Populations: A Cross-Sectional Study in Seville, Spain. Dentistry Journal. 2025; 13(11):522. https://doi.org/10.3390/dj13110522
Chicago/Turabian StyleReyes-Lara, Rodolfo Esteban, Adrián Curto, David Ribas-Perez, Ignacio Barbero-Navarro, Diego Rodriguez-Menacho, Javier Flores-Fraile, and Antonio Castaño-Séiquer. 2025. "Oral Health Status Among Children and Adolescents from Vulnerable Populations: A Cross-Sectional Study in Seville, Spain" Dentistry Journal 13, no. 11: 522. https://doi.org/10.3390/dj13110522
APA StyleReyes-Lara, R. E., Curto, A., Ribas-Perez, D., Barbero-Navarro, I., Rodriguez-Menacho, D., Flores-Fraile, J., & Castaño-Séiquer, A. (2025). Oral Health Status Among Children and Adolescents from Vulnerable Populations: A Cross-Sectional Study in Seville, Spain. Dentistry Journal, 13(11), 522. https://doi.org/10.3390/dj13110522







