Malocclusion Complexity in Patients with Dental Anomalies—A Case–Control Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Method of Error Control
2.2. Statistical Analysis
3. Results
4. Discussion
4.1. Assessment of the Impact of the Presence of Dental Anomalies on the ICON’s Aesthetic and Upper Arch Crowding or Spacing Components
4.2. Assessment of the Impact of the Presence of Dental Anomalies on the ICON’s Crossbite and Overbite Components
4.3. Assessment of the Impact of the Presence of Dental Anomalies on the ICON’s Sagittal Relationship Component
4.4. Limitations of This Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ICON | Index of Complexity, Outcome, and Need |
References
- Cobourne, M.T.; Sharpe, P.T. Diseases of the tooth: The genetic and molecular basis of inherited anomalies affecting the dentition. Wiley Interdiscip. Rev. Dev. Biol. 2013, 2, 183–212. [Google Scholar] [CrossRef]
- Balija, N.D.; Aurer, B.; Meštrović, S.; Varga, M.L. Prevalence of Dental Anomalies in Orthodontic Patients. Acta Stomatol. Croat. 2022, 56, 61–68. [Google Scholar] [CrossRef]
- Mahjoub, D.T.; Jarwan, R.K.; Filimban, L.A.Z.; Bahatheq, J.K.; Alsharif, F.S.; Alsharif, O.A.M.; Albalawi, S.H.; Rawas, A.E.; Najjar, R.S. The prevalence of dental anomalies among Saudi Population in Makkah, Saudi Arabia. J. Orthod. Sci. 2024, 13, 46. [Google Scholar] [CrossRef]
- Herrera-Atoche, J.R.; Diaz-Morales, S.; Colome-Ruiz, G.; Escoffie-Ramirez, M.; Orellana, M.F. Prevalence of dental anomalies in a Mexican population. Dentistry 2014, 3000, 1. [Google Scholar] [CrossRef]
- Montasser, M.A.; Taha, M. Prevalence and distribution of dental anomalies in orthodontic patients. Orthodontics 2012, 13, 52–59. [Google Scholar]
- Gupta, S.K.; Saxena, P.; Jain, S.; Jain, D. Prevalence and distribution of selected developmental dental anomalies in an Indian population. J. Oral Sci. 2011, 53, 231–238. [Google Scholar] [CrossRef] [PubMed]
- Uslu, O.; Akcam, M.O.; Evirgen, S.; Cebeci, I. Prevalence of dental anomalies in various malocclusions. Am. J. Orthod. Dentofac. Orthop. 2009, 135, 328–335. [Google Scholar] [CrossRef] [PubMed]
- Baron, C.; Houchmand-Cuny, M.; Enkel, B.; Lopez-Cazaux, S. Prevalence of dental anomalies in French orthodontic patients: A retrospective study. Arch. Pediatr. 2018, 25, 426–430. [Google Scholar] [CrossRef]
- Baccetti, T. A controlled study of associated dental anomalies. Angle Orthod. 1998, 68, 267–274. [Google Scholar]
- Nangia, T.; Kalra, G.; Langpoklakpam, C. Comprehensive Management of an Impacted Maxillary Central Incisor: A Case Report. Cureus 2024, 16, e71547. [Google Scholar] [CrossRef] [PubMed]
- Fekonja, A. Prevalence of dental developmental anomalies of permanent teeth in children and their influence on esthetics. J. Esthet. Restor. Dent. 2017, 29, 276–283. [Google Scholar] [CrossRef] [PubMed]
- Jha, K.; Adhikari, M. Surgical orthodontic intervention for impacted maxillary permanent central incisors: A case series. Clin. Case Rep. 2023, 11, e8199. [Google Scholar] [CrossRef] [PubMed]
- Dipalma, G.; Inchingolo, A.M.; Lauria, P.; Marotti, P.; Chieppa, S.; Di Venere, D.; Palermo, A.; Corsalini, M.; Inchingolo, F.; Inchingolo, A.D. Unilateral Agenesis of the Upper Permanent Lateral Incisors in Growing Patients: Gap Closure or Gap Opening? A Systematic Review. Int. Dent. J. 2025, 75, 100815. [Google Scholar] [CrossRef]
- Ku, J.H.; Han, B.; Kim, J.; Oh, J.; Kook, Y.A.; Kim, Y. Common dental anomalies in Korean orthodontic patients: An update. Korean J. Orthod. 2022, 52, 324–333. [Google Scholar] [CrossRef] [PubMed]
- Daniels, C.; Richmond, S. The development of the Index of Complexity, Outcome and Need (ICON). J. Orthod. 2000, 27, 149–162. [Google Scholar] [CrossRef]
- González-Pérez, N.A.; Herrera-Atoche, J.R.; López-González, P.; Pacheco-Arjona, R.; Rangel-Méndez, J.; Canul-May, J.E.; Sosa-Escalante, J.E.; Zúńiga-Herrer, I.D.; Aguilar-Ayala, F.J.; González-Herrera, L. Genetic Variants of MSX1, PAX9, and AXIN2 in Mayan Probands with Dental Agenesis from Yucatan, Mexico. ODOVTOS Int. J. Dent. Sci. 2024, 26, 266–282. [Google Scholar] [CrossRef]
- Kerekes-Máthé, B.; Mártha, K.; Bănescu, C.; O’Donnell, M.B.; Brook, A.H. Genetic and Morphological Variation in Hypodontia of Maxillary Lateral Incisors. Genes 2023, 14, 231. [Google Scholar] [CrossRef]
- Alhammadi, M.S.; Asiri, H.A.; Almashraqi, A.A. Incidence, severity and orthodontic treatment difficulty index of impacted canines in Saudi population. J. Clin. Exp. Dent. 2018, 10, e327–e334. [Google Scholar] [CrossRef]
- Modak, S.; Choudhury, P.P.; Chattaraj, S.; Lahoti, E.; Chowdhury, S.M.; Sheet, S. Prevalence and Etiological Distribution of Midline Diastema- An Institutional Study. J. Pharm. Bioallied Sci. 2025, 17, S1301–S1303. [Google Scholar] [CrossRef]
- Kiliç, N.; Oktay, H. Orthodontic Intervention to Impacted and Transposed Lower Canines. Case Rep. Dent. 2017, 2017, 4105713. [Google Scholar] [CrossRef]
- Vorloeper, J.; Coenen, F.A.; Lang, N.A.; Niederau, C.; Knaup, I.; Craveiro, R.B.; Wolf, M. Digital analyses of Bolton tooth size ratios and their association to gender, angle class, and other occlusal traits: A study using a partially automated digital 3D model analysis. Eur. J. Orthod. 2024, 46, cjae046. [Google Scholar] [CrossRef]
- Cai, J.; Chen, S.; Chen, L.; Yang, X.; Dai, X.; Dai, Z.; Xu, L. Digital-assisted diagnosis and orthodontic management of an impacted mandibular lateral incisor: A case report. BMC Oral Health 2024, 24, 1210. [Google Scholar] [CrossRef]
- Turtinen, H.; Sarja, M.; Hyvärinen, J.; Pirhonen, P.; Pesonen, P.; Pirttiniemi, P.; Silvola, A.S. Associations between Bolton ratio and overjet deviations in a Finnish adult population. Acta Odontol. Scand. 2021, 79, 593–599. [Google Scholar] [CrossRef]
- Nguyen, V.A.; Nguyen, T.T.; Nguyen, T.T.H. Management of an adult patient with missing one mandibular incisor, severe overjet, and midline discrepancy with asymmetric extraction, lingual appliance, and skeletal anchorage: A case report. J. World Fed. Orthod. 2020, 9, 86–94. [Google Scholar] [CrossRef]
- Alam, M.K.; Iida, J. Overjet, overbite and dental midline shift as predictors of tooth size discrepancy in a Bangladeshi population and a graphical overview of global tooth size ratios. Acta Odontol. Scand. 2013, 71, 1520–1531. [Google Scholar] [CrossRef]
- Oliveira, D.D.; De Oliveira, B.F.; Da Mata Cid Pinto, L.S.; Figueiredo, D.S.F.; Pithon, M.M.; Seraidarian, P.I. Interdisciplinary treatment of a class III patient with congenitally absent maxillary lateral incisors. J. Esthet. Restor. Dent. 2013, 25, 242–253. [Google Scholar] [CrossRef] [PubMed]
- Tausche, E.; Harzer, W. Treatment of a patient with Class II malocclusion, impacted maxillary canine with a dilacerated root, and peg-shaped lateral incisors. Am. J. Orthod. Dentofac. Orthop. 2008, 133, 762–770. [Google Scholar] [CrossRef]
- Eid, F.Y.; Elkalza, A.R.; Madian, A.M.; Yacout, Y.M. Buccolingual and arch distribution patterns of permanent teeth impactions in an Egyptian population: A CBCT-based retrospective analysis. BMC Oral Health 2025, 25, 1510. [Google Scholar] [CrossRef] [PubMed]
- Cinelli, F.; Paolini, E.; Nieri, M.; Di Paola, L.; Fiorentini, G.; Menesini, E.; Franchi, L. Bullying, cyberbullying, self-esteem, psychological distress and relationship with oral health related quality of life: A cross-sectional survey in adolescents. Eur. J. Orthod. 2025, 47, cjaf058. [Google Scholar] [CrossRef]
- Mucedero, M.; Pezzuto, C.; Rozzi, M.; Ricchiuti, M.R.; Cozza, P. Young adult patient with two palatally maxillary impacted canines and forced traction on rigid arches of stabilization. Case Rep. Oral Implantol. 2016, 9, 17–26. [Google Scholar]
- Mallineni, S.K.; Aldhuwayhi, S.; Deeban, Y.; Almutairi, K.S.; Alhabrdi, S.N.; Almidaj, M.A.; Alrumi, B.A.; Assalman, A.S.; Joseph, A.M.; Thakare, A.A.; et al. Prevalence, Occurrence, and Characteristics of Supernumerary Teeth Among the Saudi Arabian Population Using Panoramic Radiographs. Diagnostics 2024, 14, 2542. [Google Scholar] [CrossRef] [PubMed]
- Yüksel, S.; Üçem, T. The effect of tooth agenesis on dentofacial structures. Eur. J. Orthod. 1997, 19, 71–78. [Google Scholar] [CrossRef]
- Avelar Fernandez, C.C.; Cruz Alves Pereira, C.V.; Luiz, R.R.; Vieira, A.R.; De Castro Costa, M. Dental anomalies in different growth and skeletal malocclusion patterns. Angle Orthod. 2018, 88, 195–201. [Google Scholar] [CrossRef] [PubMed]
- Cacciatore, G.; Poletti, L.; Sforza, C. Early diagnosed impacted maxillary canines and the morphology of the maxilla: A three-dimensional study. Prog. Orthod. 2018, 19, 20. [Google Scholar] [CrossRef]
- Sokmen, T.; Bagcı, N.; Balos Tuncer, B. Buccolingual inclination of posterior dentition in maxillary impacted canine patients using quadrant analysis—A cone-beam computed tomographic study. BMC Oral Health 2024, 24, 1012. [Google Scholar] [CrossRef] [PubMed]
- Yan, B.; Sun, Z.; Fields, H.; Wang, L.; Luo, L. Etiologic factors for buccal and palatal maxillary canine impaction: A perspective based on cone-beam computed tomography analyses. Am. J. Orthod. Dentofac. Orthop. 2013, 143, 527–534. [Google Scholar] [CrossRef]
- Ceraulo, S.; Barbarisi, A.; Oliva, B.; Moretti, S.; Caccianiga, G.; Lauritano, D.; Biagi, R. Treatment options in impacted maxillary canines: A literature review. Dent. J. 2025, 13, 433. [Google Scholar] [CrossRef]
- Saade, M.; Arai, K.; Motro, M.; Saade, A.; Will, L.A. Maxillary dimensions and arch shape with palatally displaced canines. Eur. J. Orthod. 2023, 45, 338–345. [Google Scholar] [CrossRef]
- Peck, S.; Peck, L.; Kataja, M. The palatally displaced canine as a dental anomaly of genetic origin. Angle Orthod. 1994, 64, 249–256. [Google Scholar]
- Athanasiou, M.; Papadopoulou, C.; Alamoudi, R.; Halazonetis, D.; Verna, C.; Gkantidis, N.; Kanavakis, G. Palatal canine impaction is associated with craniofacial shape in humans. Eur. J. Orthod. 2024, 46, cjae051. [Google Scholar] [CrossRef]
- Herrera-Atoche, J.R.; Medina-Mazariegos, C.R.; Zúñiga-Herrera, I.D.; Colomé-Ruiz, G.E.; Aguilar-Ayala, F.J.; Pinzón-Te, A.L.; Aguilar-Pérez, F.J. Growth differences in patients with dental agenesis, how its location impacts facial morphology. J. Dent. Sci. 2020, 15, 336–344. [Google Scholar] [CrossRef] [PubMed]
- Williams, R.; Park, J.H.; Chae, J.M.; Vaden, J.L. The congenitally missing second premolar: Space closure. A viable option. Am. J. Orthod. Dentofac. Orthop. 2020, 157, 571–583.e16. [Google Scholar] [CrossRef] [PubMed]
- Grauer, D.; Heymann, G.C.; Swift, E.J. Clinical management of tooth size discrepancies. J. Esthet. Restor. Dent. 2012, 24, 155–159. [Google Scholar] [CrossRef]
- Pinho, T.; Amaral, R. Transposed Maxillary Canines: Narrative Review with Clinical Case Report. Dent. J. 2025, 13, 251. [Google Scholar] [CrossRef]
- Altug-Atac, A.T.; Erdem, D. Prevalence and distribution of dental anomalies in orthodontic patients. Am. J. Orthod. Dentofac. Orthop. 2007, 131, 510–514. [Google Scholar] [CrossRef] [PubMed]
| Number Anomalies | |
| Dental agenesis | When there is no identifiable mineralization of the tooth crown on radiographic records, and no evidence of extraction. |
| Supernumerary teeth | A tooth is considered supernumerary when it appears in addition to the normal number of teeth. |
| Shape Anomalies | |
| Microdontic upper lateral incisors | An upper lateral incisor is considered microdontic when its mesiodistal width is equal to or smaller than that of its mandibular counterpart. |
| Barrel shaped upper lateral incisors | An upper lateral incisor is considered to be barrel-shaped when the operator identifies a pronounced manifestation of a thickened or elevated cingulum on the gingival aspect of its lingual surface. |
| Peg shaped upper lateral incisors | An upper lateral incisor is considered to be peg-shaped when its width is greatest at the cervical margin. |
| Eruption Anomalies | |
| Impacted teeth | The operator classifies a tooth as impacted when it is not expected to erupt fully into its regular functional position based on clinical and radiographic examinations. |
| Dental transposition | Dental transposition is defined as the “positional interchange of two adjacent teeth, or the development or eruption of a tooth in a position normally occupied by a non-adjacent tooth.” |
| Dental transmigration | A tooth is considered in dental transmigration when its “eruption path had been altered and the tooth had drifted to the opposite side of the arch with at least half of the crown length crossing the midline.” |
| ICON Levels | p | |||||
|---|---|---|---|---|---|---|
| Easy | Mild | Moderate | Difficult | Very Difficult | ||
| % (N) | % (N) | % (N) | % (N) | % (N) | ||
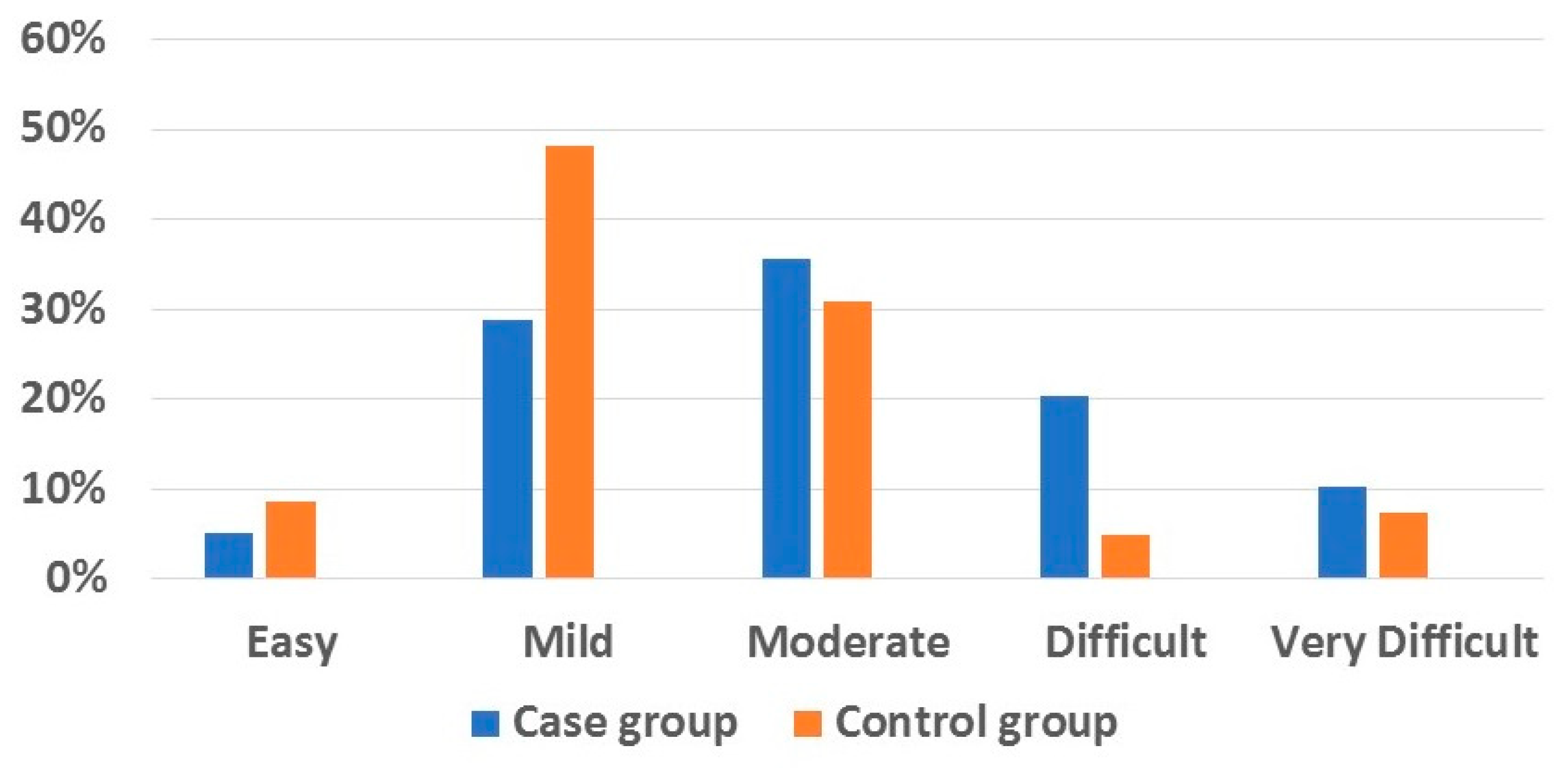
| Case group | 5.1 (3) | 28.8 (17) | 35.6 (21) | 20.3 (12) | 10.2 (6) | 0.022 * |
| Control group | 8.6 (7) | 48.1 (39) | 30.9 (25) | 4.9 (4) | 7.4 (6) | |
| Groups | p | ||||
|---|---|---|---|---|---|
| Control | Number | Shape | Eruption | ||
| Mean SD (95% CI) N = 81 | Mean SD (95% CI) N = 10 | Mean SD (95% CI) N = 10 | Mean SD (95% CI) N = 21 | ||
| ICON Score | 47.44 ±17.54 a (43.56–51.32) | 45.9 ±17.66 a (33.26–58.53) | 41.9 ±12.52 a (32.93–50.86) | 63.23 ±14.26 b (56.74 -69.72) | 0.001 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Romero-Noh, M.F.; Herrera-Atoche, J.R.; Zúñiga-Herrera, I.D.; Carrillo-Ávila, B.A.; Martínez-Aguilar, V.M.; Pérez-Traconis, L.B. Malocclusion Complexity in Patients with Dental Anomalies—A Case–Control Study. Dent. J. 2025, 13, 506. https://doi.org/10.3390/dj13110506
Romero-Noh MF, Herrera-Atoche JR, Zúñiga-Herrera ID, Carrillo-Ávila BA, Martínez-Aguilar VM, Pérez-Traconis LB. Malocclusion Complexity in Patients with Dental Anomalies—A Case–Control Study. Dentistry Journal. 2025; 13(11):506. https://doi.org/10.3390/dj13110506
Chicago/Turabian StyleRomero-Noh, María Fernanda, José Rubén Herrera-Atoche, Iván Daniel Zúñiga-Herrera, Bertha Arelly Carrillo-Ávila, Víctor Manuel Martínez-Aguilar, and Laura Beatriz Pérez-Traconis. 2025. "Malocclusion Complexity in Patients with Dental Anomalies—A Case–Control Study" Dentistry Journal 13, no. 11: 506. https://doi.org/10.3390/dj13110506
APA StyleRomero-Noh, M. F., Herrera-Atoche, J. R., Zúñiga-Herrera, I. D., Carrillo-Ávila, B. A., Martínez-Aguilar, V. M., & Pérez-Traconis, L. B. (2025). Malocclusion Complexity in Patients with Dental Anomalies—A Case–Control Study. Dentistry Journal, 13(11), 506. https://doi.org/10.3390/dj13110506






