Modified Coronally Advanced Flaps: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
- (1)
- ((multiple recessions[Title/Abstract]) OR (multiple recession-type defects[Title/Abstract])) AND (treatment[Title/Abstract]);
- (2)
- Modified Coronally Advanced Flap[Title/Abstract].
- (1)
- ((TITLE-ABS-KEY (multiple AND recessions) OR TITLE-ABS-KEY (multiple AND recession-type AND defects)) AND TITLE-ABS-KEY (treatment));
- (2)
- TITLE-ABS-KEY(modified AND coronally AND advanced AND flap).
- (1)
- ((TI = (multiple recessions)) OR TI = (multiple recession-type defects)) AND TI = (treatment);
- (2)
- TI = (Modified Coronally Advanced Flap).
- (1)
- TI multiple recessions OR TI multiple recession-type defects AND TI treatment;
- (2)
- TI Modified Coronally Advanced Flap.
Focused Question
2.2. Inclusion Criteria and Selection Process
2.2.1. Types of Participants
2.2.2. Types of Interventions
- mCAF (Modified Coronally Advanced Flap): An envelope type of flap proposed by Zucchelli and De Sanctis [27], characterized by a horizontal incision consisting of oblique submarginal incisions in the interdental areas, which continued with the intra-sulcular incision at the recession defects. This kind of design anticipates the rotation of the surgical papilla;
- mCAF + placental membrane: A placental allograft deriving from amnion and chorion was used for the first time to compare mCAF + placental membrane to mCAF alone in the treatment of gingival recession [39];
- mCAF + EMD (Enamel Matrix Derivatives): EMD was evaluated for its potential both in regeneration of intrabony defects and in root coverage surgical procedures [52].
2.2.3. Types of Studies
2.2.4. Types of Measures: Primary and Secondary Outcomes
- Complete root coverage (CRC) [53,54]: A percentage value describing the number of sites, with respect to the total number of sites treated, that obtained a complete radicular covering at a given time of follow-up. The formula is reported as CRC = (n. of sites with CRC)/(total n. of sites treated) × 100%;
- Root esthetic score (RES) [55,56,57]: A score evaluating level of the gingival margin, marginal tissue contour, soft tissue texture, mucogingival junction alignment, and gingival color. Regarding assessment of the final position of the gingival margin, 3 points are given for partial root coverage and 6 points for complete root coverage, 0 points are assigned when the final position of the gingival margin is equal or apical to the previous recession. One point is assigned for each of the other four variables. Thus, 10 points is the perfect score;
- Mean root coverage (MRC) [60]: A percentage value that describes the rate of reduction in the recession compared to the initial recession;
- Duration of surgery, measured in minutes.
2.3. Data Collection, Extraction, and Management
2.3.1. Assessment of Risk of Bias of the Included Studies
2.3.2. Quantitative Data Synthesis Method
2.3.3. Certainty Assessment
3. Results
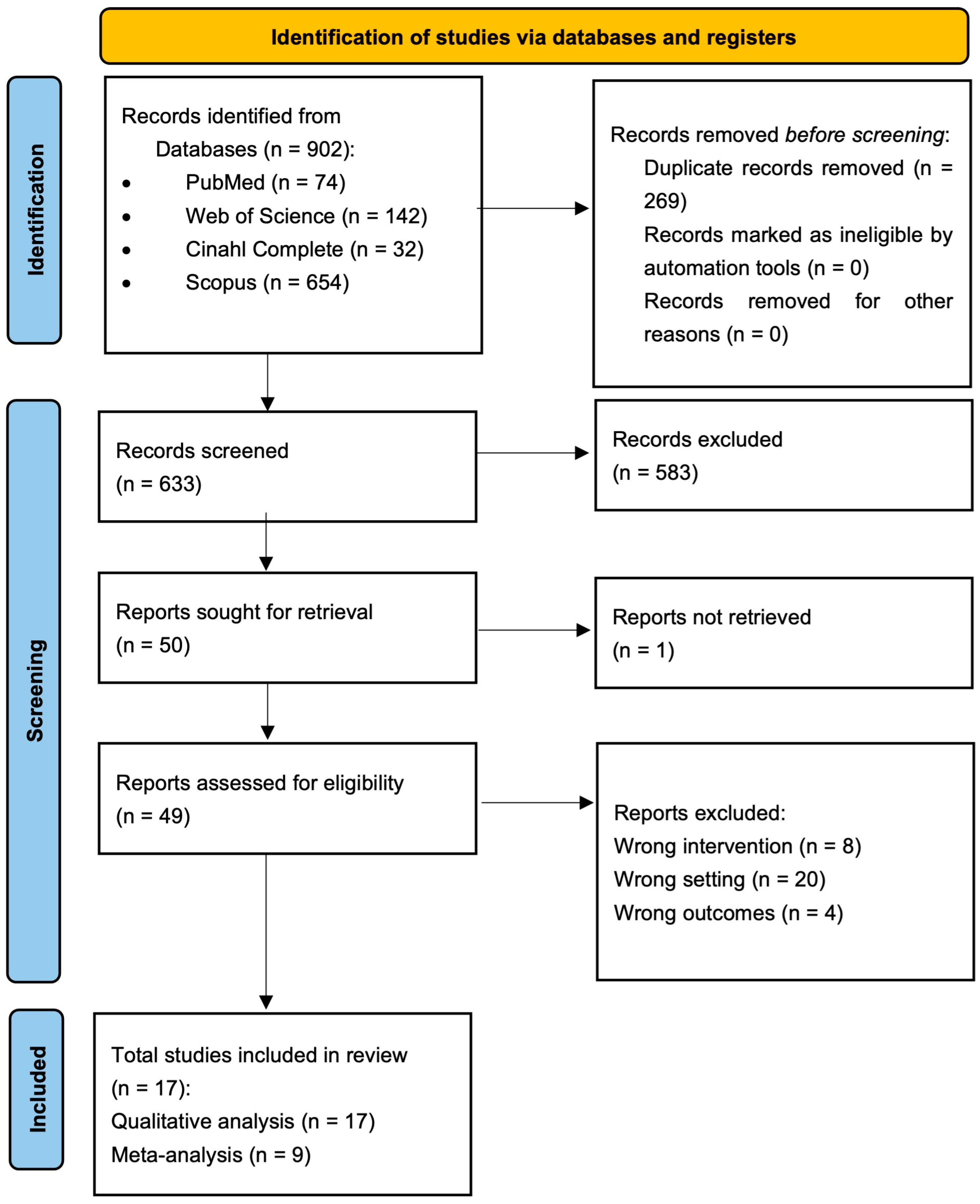
3.1. Results of the Study Search
3.2. Characteristics of the Included Studies
3.3. Risk of Bias
3.4. Synthesis of Results of Meta-Analysis
- -
- mCAF + sCTG (control) vs. mCAF + XADM (test);
- -
- mCAF + sCTG (control) vs. mCAF + CM (test);
- -
- mCAF + sCTG (control) vs. mCAF + PRF (test);
- -
- mCAF + sCTG (control) vs. mCAF + EMD (test);
- -
- mCAF + sCTG (de-epithelialized) (control) vs. mCAF + CTG (harvested double blade scalpel) (test).
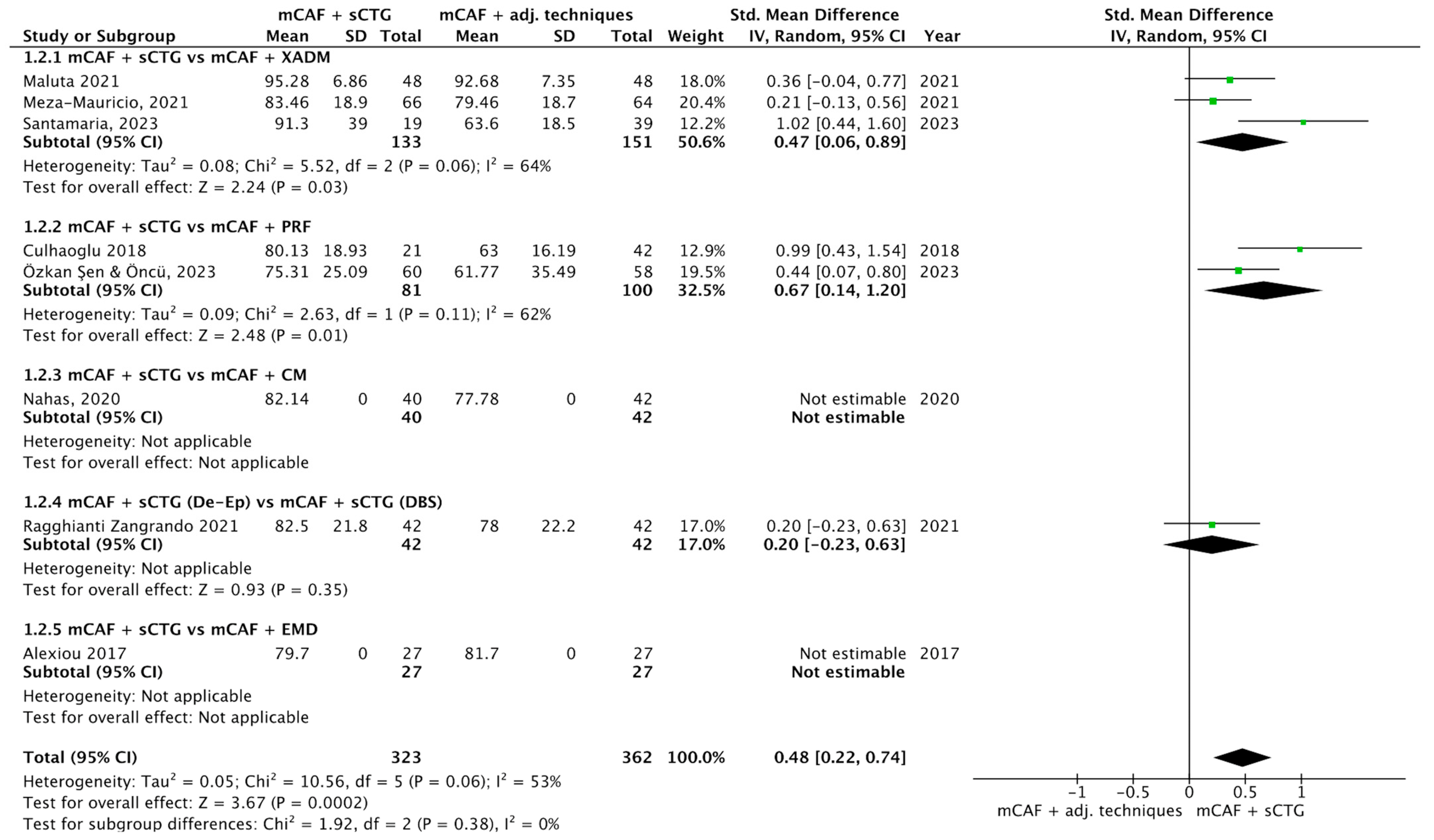
3.4.1. CRC
3.4.2. MRC
3.4.3. RDR
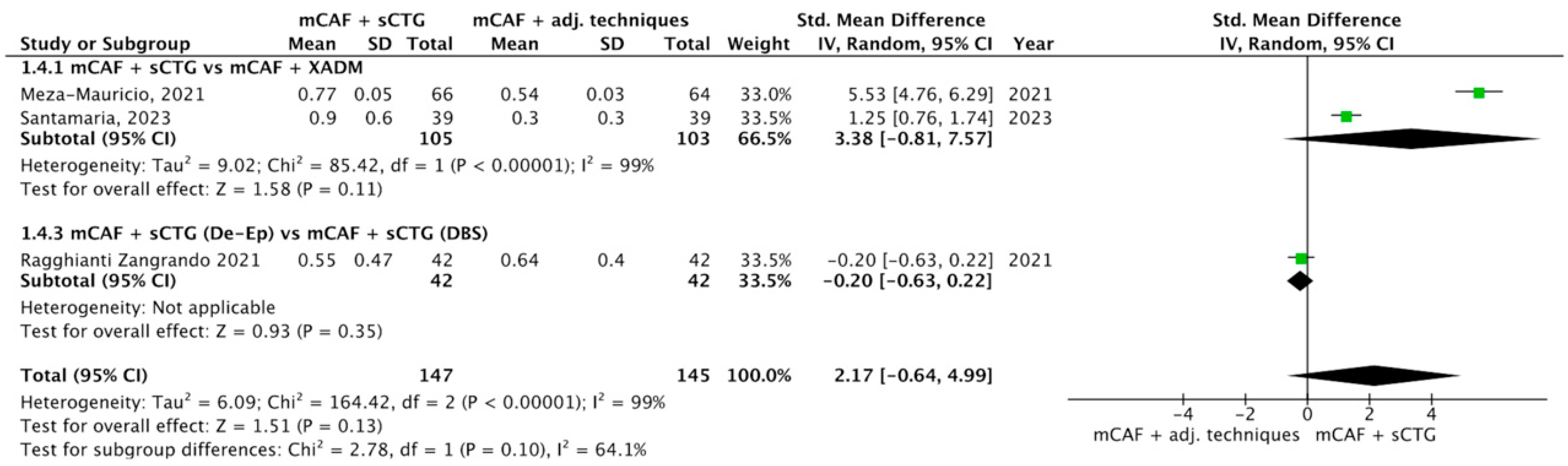
3.4.4. ∆GT
3.4.5. ∆KTW
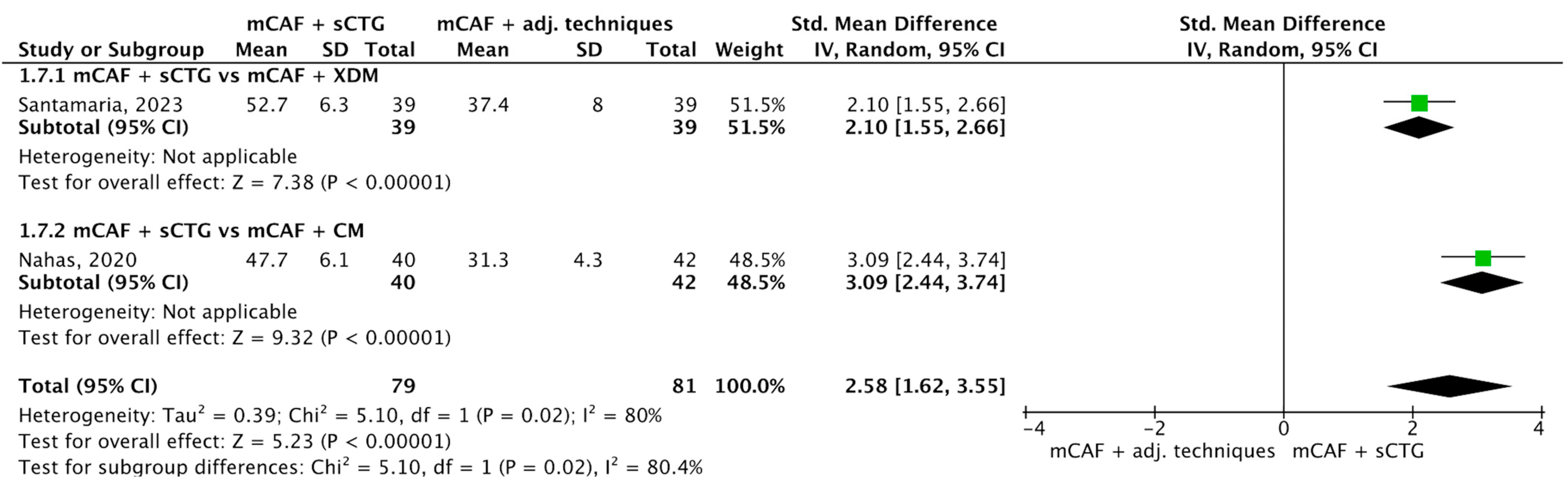
3.4.6. RES
3.4.7. Duration of Surgery
3.5. Certainty Assessement
4. Discussion
Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ADM | Acellular Dermal Matrix |
| CAF | Coronally Advanced Flap |
| CAT | Coronally Advanced Tunnel |
| CI | Confidence Interval |
| CM | Collagen Matrix |
| CRC | Complete Root Coverage |
| CTG | Connective Tissue Graft |
| DBS | Double Blade Scalpel |
| df | Degree of Freedom |
| EMD | Enamel Matrix Derivatives |
| GR | Gingival Recession |
| GRADEpro | GDT Guideline Development Tool |
| GT | Gingival Thickness |
| HA | Hyaluronic Acid |
| I2 | Index of Higgings |
| KT | Keratinized Tissue |
| KTW | Keratinized Tissue Width |
| MAGRs | Multiple Adjacent Gingival Recessions |
| MCAF | Modified Coronally Advanced Flap |
| MRC | Mean Root Coverage |
| NCCLs | Non-Carious Cervial Lesions |
| OB | Orthodontic Button |
| OR | Odds Ratio |
| PICOS | Population, Intervention, Comparison, Outcomes, and Study Design |
| PRF | Platelet-Rich Fibrin |
| RC | Root Coverage |
| RCPPS | Root Coverage Periodontal Plastic Surgery |
| RCSPs | Root Coverage Surgical Procedures |
| RCTs | Randomized Clinical Trials |
| RDR | Recession Depth Reduction |
| RES | Root Coverage Esthetic Score |
| Robvis tool | Risk of Bias Visualization Tool |
| RoB2 | Risk of Bias 2 |
| RR | Risk Ratio |
| RT | Recession Type |
| sCTG | Subepithelial Connective Tissue Graft |
| SMD | Standardized Mean Difference |
| SRs | Systematic Reviews |
| VAS | Visual Analogue Scale |
| T-PRF | Titanium Platelet-Rich Fibrin |
| XADM | Xenogeneic Acellular Dermal Matrix |
References
- Camargo, P.M.; Melnick, P.R.; Kenney, E.B. The use of free gingival grafts for aesthetic purposes. Periodontol. 2000 2001, 27, 72–96. [Google Scholar] [CrossRef]
- Wennström, J.L. Mucogingival therapy. Ann. Periodontol. 1996, 1, 671–701. [Google Scholar] [CrossRef] [PubMed]
- Cairo, F.; Pagliaro, U.; Nieri, M. Treatment of gingival recession with coronally advanced flap procedures: A systematic review. J. Clin. Periodontol. 2008, 35, 136–162. [Google Scholar] [CrossRef] [PubMed]
- Nieri, M.; Pini Prato, G.P.; Giani, M.; Magnani, N.; Pagliaro, U.; Rotundo, R. Patient perceptions of buccal gingival recessions and requests for treatment. J. Clin. Periodontol. 2013, 40, 707–712. [Google Scholar] [CrossRef] [PubMed]
- Löe, H.; Anerud, A.; Boysen, H. The natural history of periodontal disease in man: Prevalence, severity, and extent of gingival recession. J. Periodontol. 1992, 63, 489–495. [Google Scholar] [CrossRef]
- Nocini, R.; Favaloro, E.J.; Sanchis-Gomar, F.; Lippi, G. Periodontitis, coronary heart disease and myocardial infarction: Treat one, benefit all. Blood Coagul. Fibrinolysis 2020, 31, 339–345. [Google Scholar] [CrossRef]
- Nocini, R.; Lippi, G.; Mattiuzzi, C. Periodontal disease: The portrait of an epidemic. J. Public Health Emerg. 2020, 4, 10. [Google Scholar] [CrossRef]
- Prato, G.P.; Rotundo, R.; Magnani, C.; Ficarra, G. Viral etiology of gingival recession. A case report. J. Periodontol. 2002, 73, 110–114. [Google Scholar] [CrossRef]
- Smukler, H.; Landsberg, J. The toothbrush and gingival traumatic injury. J. Periodontol. 1984, 55, 713–719. [Google Scholar] [CrossRef]
- Toker, H.; Ozdemir, H. Gingival recession: Epidemiology and risk indicators in a university dental hospital in Turkey. Int. J. Dent. Hyg. 2009, 7, 115–120. [Google Scholar] [CrossRef]
- Olsson, M.; Lindhe, J. Periodontal characteristics in individuals with varying form of the upper central incisors. J. Clin. Periodontol. 1991, 18, 78–82. [Google Scholar] [CrossRef]
- Stoner, J.E.; Mazdyasna, S. Gingival recession in the lower incisor region of 15-year-old subjects. J. Periodontol. 1980, 51, 74–76. [Google Scholar] [CrossRef]
- Ericsson, I.; Lindhe, J. Recession in sites with inadequate width of the keratinized gingiva. An experimental study in the dog. J. Clin. Periodontol. 1984, 11, 95–103. [Google Scholar] [CrossRef] [PubMed]
- Parma-Benfenali, S.; Fugazzoto, P.A.; Ruben, M.P. The effect of restorative margins on the postsurgical development and nature of the periodontium. Part I. Int. J. Periodontics Restor. Dent. 1985, 5, 30–51. [Google Scholar]
- Wennström, J.L.; Lindhe, J.; Sinclair, F.; Thilander, B. Some periodontal tissue reactions to orthodontic tooth movement in monkeys. J. Clin. Periodontol. 1987, 14, 121–129. [Google Scholar] [CrossRef] [PubMed]
- Yared, K.F.; Zenobio, E.G.; Pacheco, W. Periodontal status of mandibular central incisors after orthodontic proclination in adults. Am. J. Orthod. Dentofac. Orthop. 2006, 130, 6.e1–6.e8. [Google Scholar] [CrossRef]
- Chambrone, L.; Chambrone, L.A. Gingival recessions caused by lip piercing: Case report. J. Can. Dent. Assoc. 2003, 69, 505–508. [Google Scholar]
- Graziani, F.; Gennai, S.; Roldán, S.; Discepoli, N.; Buti, J.; Madianos, P.; Herrera, D. Efficacy of periodontal plastic procedures in the treatment of multiple gingival recessions. J. Clin. Periodontol. 2014, 41 (Suppl. 15), S63–S76. [Google Scholar] [CrossRef]
- Cairo, F.; Nieri, M.; Pagliaro, U. Efficacy of periodontal plastic surgery procedures in the treatment of localized facial gingival recessions. A systematic review. J. Clin. Periodontol. 2014, 41 (Suppl. 15), S44–S62. [Google Scholar] [CrossRef]
- Chambrone, L.; Barootchi, S.; Avila-Ortiz, G. Efficacy of biologics in root coverage and gingival augmentation therapy: An American Academy of Periodontology best evidence systematic review and network meta-analysis. J. Periodontol. 2022, 93, 1771–1802. [Google Scholar] [CrossRef]
- Tavelli, L.; Barootchi, S.; Nguyen, T.V.N.; Tattan, M.; Ravidà, A.; Wang, H.L. Efficacy of tunnel technique in the treatment of localized and multiple gingival recessions: A systematic review and meta-analysis. J. Periodontol. 2018, 89, 1075–1090. [Google Scholar] [CrossRef]
- Toledano-Osorio, M.; Muñoz-Soto, E.; Toledano, M.; Vallecillo-Rivas, M.; Vallecillo, C.; Ramos-García, P.; Osorio, R. Treating Gingival Recessions Using Coronally Advanced Flap or Tunnel Techniques with Autografts or Polymeric Substitutes: A Systematic Review and Meta-Analysis. Polymers 2022, 14, 1453. [Google Scholar] [CrossRef]
- Moraschini, V.; Calasans-Maia, M.D.; Dias, A.T.; de Carvalho Formiga, M.; Sartoretto, S.C.; Sculean, A.; Shibli, J.A. Effectiveness of connective tissue graft substitutes for the treatment of gingival recessions compared with coronally advanced flap: A network meta-analysis. Clin. Oral Investig. 2020, 24, 3395–3406. [Google Scholar] [CrossRef]
- Chambrone, L.; Botelho, J.; Machado, V.; Mascarenhas, P.; Mendes, J.J.; Avila-Ortiz, G. Does the subepithelial connective tissue graft in conjunction with a coronally advanced flap remain as the gold standard therapy for the treatment of single gingival recession defects? A systematic review and network meta-analysis. J. Periodontol. 2022, 93, 1336–1352. [Google Scholar] [CrossRef]
- Tavelli, L.; Barootchi, S.; Cairo, F.; Rasperini, G.; Shedden, K.; Wang, H.L. The Effect of Time on Root Coverage Outcomes: A Network Meta-analysis. J. Dent. Res. 2019, 98, 1195–1203. [Google Scholar] [CrossRef]
- Bhatia, A.; Yadav, V.S.; Tewari, N.; Kumar, A.; Sharma, R.K. Efficacy of modified coronally advanced flap in the treatment of multiple adjacent gingival recessions: A systematic review and meta-analysis. Acta Odontol. Scand. 2021, 79, 562–572. [Google Scholar] [CrossRef] [PubMed]
- Zucchelli, G.; De Sanctis, M. Treatment of multiple recession-type defects in patients with esthetic demands. J. Periodontol. 2000, 71, 1506–1514. [Google Scholar] [CrossRef] [PubMed]
- Zucchelli, G.; Amore, C.; Sforza, N.M.; Montebugnoli, L.; De Sanctis, M. Bilaminar techniques for the treatment of recession-type defects. A comparative clinical study. J. Clin. Periodontol. 2003, 30, 862–870. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, P.F.; da Silva, R.C.; Cury, P.R.; Joly, J.C. Modified coronally advanced flap associated with a subepithelial connective tissue graft for the treatment of adjacent multiple gingival recessions. J. Periodontol. 2006, 77, 1901–1906. [Google Scholar] [CrossRef]
- Ahmedbeyli, C.; Dirikan Ipçi, S.; Cakar, G.; Yılmaz, S.; Chambrone, L. Coronally advanced flap and envelope type of flap plus acellular dermal matrix graft for the treatment of thin phenotype multiple recession defects. A randomized clinical trial. J. Clin. Periodontol. 2019, 46, 1024–1029. [Google Scholar] [CrossRef]
- Santamaria, M.P.; Rossato, A.; Fernanda Ferreira Ferraz, L.; Maria Viana Miguel, M.; Venturoso Simões, B.; Pereira Nunes, M.; Bresciani, E.; de Sanctis, M.; Mathias-Santamaria, I.F. Multiple gingival recessions associated with non-carious cervical lesions treated by partial restoration and modified coronally advanced flap with either connective tissue graft or xenogeneic acellular dermal matrix: A randomized clinical trial. J. Periodontol. 2023, 94, 731–741. [Google Scholar] [CrossRef]
- Meza-Mauricio, J.; Cortez-Gianezzi, J.; Duarte, P.M.; Tavelli, L.; Rasperini, G.; de Faveri, M. Comparison between a xenogeneic dermal matrix and connective tissue graft for the treatment of multiple adjacent gingival recessions: A randomized controlled clinical trial. Clin. Oral Investig. 2021, 25, 6919–6929. [Google Scholar] [CrossRef]
- Gürlek, Ö.; Gümüş, P.; Nizam, N.; Buduneli, N. Coronally advanced flap with connective tissue graft or xenogeneic acellular dermal matrix in the treatment of multiple gingival recessions: A split-mouth randomized clinical trial. J. Esthet. Restor. Dent. 2020, 32, 380–388. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, K.T.; de Jesus Hernandez Martinez, C.; Suemi, M.I.; Palioto, D.B.; Messora, M.R.; de Souza, S.L.S.; Novaes, A.B.; Chaves Furlaneto, F.A.; Taba, M. Root coverage using coronally advanced flap with porcine-derived acellular dermal matrix or subepithelial connective tissue graft: A randomized controlled clinical trial. Clin. Oral Investig. 2020, 24, 4077–4087. [Google Scholar] [CrossRef] [PubMed]
- Öncü, E. The Use of Platelet-Rich Fibrin Versus Subepithelial Connective Tissue Graft in Treatment of Multiple Gingival Recessions: A Randomized Clinical Trial. Int. J. Periodontics Restor. Dent. 2017, 37, 265–271. [Google Scholar] [CrossRef] [PubMed]
- Nahas, R.; Gondim, V.; Carvalho, C.V.; Calderero, L.M.; Rosa, E.F.; Sakiyama, T.; César Neto, J.B.; Pannuti, C.M.; Romito, G.A. Treatment of multiple recessions with collagen matrix versus connective tissue: A randomized clinical trial. Braz. Oral Res. 2020, 33, e123. [Google Scholar] [CrossRef]
- De Santis, D.; Luciano, U.; Pancera, P.; Castegnaro, G.; Alberti, C.; Gelpi, F. A New Matrix for Soft Tissue Management. J. Clin. Med. 2022, 11, 4486. [Google Scholar] [CrossRef]
- Aroca, S.; Keglevich, T.; Barbieri, B.; Gera, I.; Etienne, D. Clinical evaluation of a modified coronally advanced flap alone or in combination with a platelet-rich fibrin membrane for the treatment of adjacent multiple gingival recessions: A 6-month study. J. Periodontol. 2009, 80, 244–252. [Google Scholar] [CrossRef]
- George, S.G.; Kanakamedala, A.K.; Mahendra, J.; Kareem, N.; Mahendra, L.; Jerry, J.J. Treatment of gingival recession using a coronally-advanced flap procedure with or without placental membrane. J. Investig. Clin. Dent. 2018, 9, e12340. [Google Scholar] [CrossRef]
- Rojas, M.A.; Marini, L.; Sahrmann, P.; Pilloni, A. Hyaluronic Acid as an Adjunct to Coronally Advanced Flap Procedures for Gingival Recessions: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. J. Pers. Med. 2022, 12, 1593. [Google Scholar] [CrossRef]
- Pilloni, A.; Schmidlin, P.R.; Sahrmann, P.; Sculean, A.; Rojas, M.A. Effectiveness of adjunctive hyaluronic acid application in coronally advanced flap in Miller class I single gingival recession sites: A randomized controlled clinical trial. Clin. Oral Investig. 2019, 23, 1133–1141. [Google Scholar] [CrossRef] [PubMed]
- Pardo, A.; Magnani, V.; Montagna, P.; Ala, A.; Brancato, G.; Melloni, F.; Lombardo, G.; De Santis, D. Clinical, Microbiological, and Biochemical Outcomes of Hyaluronic Acid in Non-Surgical Periodontal Therapy: A Systematic Review and Meta-Analysis. Appl. Sci. 2025, 15, 5975. [Google Scholar] [CrossRef]
- Rajendran, V.; Uppoor, A.; Kadakampally, D.; Mannava, Y. Comparison of minimally invasive coronally advanced flap and modified coronally advanced flap for the management of multiple adjacent gingival recession defects: A split mouth randomized control trial. J. Esthet. Restor. Dent. 2018, 30, 509–515. [Google Scholar] [CrossRef] [PubMed]
- Khobragade, S.; Kolte, A.; Kolte, R.; Shrirao, T.; Potey, A. Modified coronally advanced flap with and without orthodontic button application in management of multiple proximate gingival recession defects: A randomized clinical trial. Contemp. Clin. Dent. 2016, 7, 544–549. [Google Scholar] [CrossRef] [PubMed]
- Savithri, N.K.; Subramanian, S.; Prakash, P.S.G.; Appukuttan, D. Effect of microsurgical technique for root coverage using modified coronally advanced flap with connective tissue graft- Randomized controlled clinical trial. Dent. Res. J. 2022, 19, 87. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Group, P. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. J. Clin. Epidemiol. 2009, 62, 1006–1012. [Google Scholar] [CrossRef]
- Hoogendam, A.; de Vries Robbé, P.F.; Overbeke, A.J. Comparing patient characteristics, type of intervention, control, and outcome (PICO) queries with unguided searching: A randomized controlled crossover trial. J. Med. Libr. Assoc. 2012, 100, 121–126. [Google Scholar] [CrossRef]
- Miller, P.D. A classification of marginal tissue recession. Int. J. Periodontics Restor. Dent. 1985, 5, 8–13. [Google Scholar]
- Cairo, F.; Nieri, M.; Cincinelli, S.; Mervelt, J.; Pagliaro, U. The interproximal clinical attachment level to classify gingival recessions and predict root coverage outcomes: An explorative and reliability study. J. Clin. Periodontol. 2011, 38, 661–666. [Google Scholar] [CrossRef]
- Özkan Şen, D.; Öncü, E. Splith mouth randomized control trial comparison of T-PRF and subepithelial connective tissue graft in the treatment of maxillar multiple gingival recessions. J. Esthet. Restor. Dent. 2023, 35, 449–456. [Google Scholar] [CrossRef]
- Rokn, A.; Zare, H.; Haddadi, P. Use of Mucograft Collagen Matrix. Front. Dent. 2020, 17, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Alexiou, A.; Vouros, I.; Menexes, G.; Konstantinidis, A. Comparison of enamel matrix derivative (Emdogain) and subepithelial connective tissue graft for root coverage in patients with multiple gingival recession defects: A randomized controlled clinical study. Quintessence Int. 2017, 48, 381–389. [Google Scholar] [CrossRef]
- Fernández-Jiménez, A.; García-De-La-Fuente, A.M.; Estefanía-Fresco, R.; Marichalar-Mendia, X.; Aguirre-Urizar, J.M.; Aguirre-Zorzano, L.A. Complete root coverage in the treatment of Miller class III or RT2 gingival recessions: A systematic review and meta-analysis. BMC Oral Health 2021, 21, 145. [Google Scholar] [CrossRef]
- Pini-Prato, G.; Magnani, C.; Zaheer, F.; Buti, J.; Rotundo, R. Critical Evaluation of Complete Root Coverage as a Successful Endpoint of Treatment for Gingival Recessions. Int. J. Periodontics Restor. Dent. 2015, 35, 655–663. [Google Scholar] [CrossRef]
- Cairo, F.; Rotundo, R.; Miller, P.D.; Pini Prato, G.P. Root coverage esthetic score: A system to evaluate the esthetic outcome of the treatment of gingival recession through evaluation of clinical cases. J. Periodontol. 2009, 80, 705–710. [Google Scholar] [CrossRef]
- Sørdahl, A.J.; Verket, A. Patient and professional use of the root coverage esthetic score (RES) and how it relates to patient satisfaction following periodontal plastic surgery. BMC Oral Health 2022, 22, 295. [Google Scholar] [CrossRef]
- Isaia, F.; Gyurko, R.; Roomian, T.C.; Hawley, C.E. The root coverage esthetic score: Intra-examiner reliability among dental students and dental faculty. J. Periodontol. 2018, 89, 833–839. [Google Scholar] [CrossRef]
- Akcan, S.K.; Ünsal, B. Gingival recession treatment with concentrated growth factor membrane: A comparative clinical trial. J. Appl. Oral Sci. 2020, 28, e20190236. [Google Scholar] [CrossRef]
- Cardaropoli, D.; Tamagnone, L.; Roffredo, A.; Gaveglio, L. Treatment of gingival recession defects using coronally advanced flap with a porcine collagen matrix compared to coronally advanced flap with connective tissue graft: A randomized controlled clinical trial. J. Periodontol. 2012, 83, 321–328. [Google Scholar] [CrossRef]
- Malhotra, S.; Tewari, S.; Sharma, R.; Sharma, R.K.; Tanwar, N.; Arora, R. Clinical evaluation of root coverage in Miller class III/RT2 labial gingival recession treated with interdisciplinary periodontal-orthodontic therapy: A randomized controlled clinical trial. J. Periodontal Implant. Sci. 2024, 54, 265–279. [Google Scholar] [CrossRef]
- Chambrone, L.; Salinas Ortega, M.A.; Sukekava, F.; Rotundo, R.; Kalemaj, Z.; Buti, J.; Pini Prato, G.P. Root coverage procedures for treating localised and multiple recession-type defects. Cochrane Database Syst. Rev. 2018, 10, CD007161. [Google Scholar] [CrossRef]
- Tatakis, D.N.; Trombelli, L. Gingival recession treatment: Guided tissue regeneration with bioabsorbable membrane versus connective tissue graft. J. Periodontol. 2000, 71, 299–307. [Google Scholar] [CrossRef]
- Chapter 8: Assessing Risk of Bias in a Randomized Trial. Available online: https://www.cochrane.org/authors/handbooks-and-manuals/handbook/current/chapter-08 (accessed on 1 July 2025).
- McGuinness, L.A.; Higgins, J.P.T. Risk-of-bias VISualization (robvis): An R package and Shiny web app for visualizing risk-of-bias assessments. Res. Synth. Methods 2021, 12, 55–61. [Google Scholar] [CrossRef]
- RevMan Web. The Cochrane Collaboration. 2023. Available online: https://revman.cochrane.org (accessed on 1 July 2025).
- Richardson, M.; Garner, P.; Donegan, S. Interpretation of subgroup analyses in systematic reviews: A tutorial. Clin. Epidemiol. Glob. Health 2019, 7, 192–198. [Google Scholar] [CrossRef]
- McMaster University and Evidence Prime, GRADEpro GDT: GRADEpro Guideline Development Tool. 2023. Available online: https://gradepro.org (accessed on 1 July 2025).
- Cairo, F.; Cortellini, P.; Pilloni, A.; Nieri, M.; Cincinelli, S.; Amunni, F.; Pagavino, G.; Tonetti, M.S. Clinical efficacy of coronally advanced flap with or without connective tissue graft for the treatment of multiple adjacent gingival recessions in the aesthetic area: A randomized controlled clinical trial. J. Clin. Periodontol. 2016, 43, 849–856. [Google Scholar] [CrossRef]
- Culhaoglu, R.; Taner, L.; Guler, B. Evaluation of the effect of dose-dependent platelet-rich fibrin membrane on treatment of gingival recession: A randomized, controlled clinical trial. J. Appl. Oral Sci. 2018, 26, e20170278. [Google Scholar] [CrossRef]
- Maluta, R.; Monteiro, M.F.; Peruzzo, D.C.; Joly, J.C. Root coverage of multiple gingival recessions treated with coronally advanced flap associated with xenogeneic acellular dermal matrix or connective tissue graft: A 6-month split-mouth controlled and randomized clinical trial. Clin. Oral Investig. 2021, 25, 5765–5773. [Google Scholar] [CrossRef]
- Ozcelik, O.; Haytac, M.C.; Seydaoglu, G. Treatment of multiple gingival recessions using a coronally advanced flap procedure combined with button application. J. Clin. Periodontol. 2011, 38, 572–580. [Google Scholar] [CrossRef]
- Zangrando, M.S.R.; Eustachio, R.R.; de Rezende, M.L.R.; Sant’ana, A.C.P.; Damante, C.A.; Greghi, S.L.A. Clinical and patient-centered outcomes using two types of subepithelial connective tissue grafts: A split-mouth randomized clinical trial. J. Periodontol. 2021, 92, 814–822. [Google Scholar] [CrossRef]
- Rotundo, R.; Genzano, L.; Patel, D.; D’Aiuto, F.; Nieri, M. Adjunctive benefit of a xenogenic collagen matrix associated with coronally advanced flap for the treatment of multiple gingival recessions: A superiority, assessor-blind, randomized clinical trial. J. Clin. Periodontol. 2019, 46, 1013–1023. [Google Scholar] [CrossRef]
- Zucchelli, G.; Mounssif, I.; Mazzotti, C.; Stefanini, M.; Marzadori, M.; Petracci, E.; Montebugnoli, L. Coronally advanced flap with and without connective tissue graft for the treatment of multiple gingival recessions: A comparative short- and long-term controlled randomized clinical trial. J. Clin. Periodontol. 2014, 41, 396–403. [Google Scholar] [CrossRef]
- Hofmänner, P.; Alessandri, R.; Laugisch, O.; Aroca, S.; Salvi, G.E.; Stavropoulos, A.; Sculean, A. Predictability of surgical techniques used for coverage of multiple adjacent gingival recessions--A systematic review. Quintessence Int. 2012, 43, 545–554. [Google Scholar]
- Zangani, A.; Gualtieri, M.; Pardo, A.; Signoriello, A.; Faccioni, P.; Colapinto, G.; Goker, F.; Lombardo, G.; Del Fabbro, M.; Albanese, M. Collagen Matrix Versus Subepithelial Connective Tissue for Recession Coverage: A Systematic Review. Oral Dis. 2024, 31, 1092–1106. [Google Scholar] [CrossRef]
- Zucchelli, G.; Mounssif, I.; Mazzotti, C.; Montebugnoli, L.; Sangiorgi, M.; Mele, M.; Stefanini, M. Does the dimension of the graft influence patient morbidity and root coverage outcomes? A randomized controlled clinical trial. J. Clin. Periodontol. 2014, 41, 708–716. [Google Scholar] [CrossRef]
- D’Ambrosio, F.; Caggiano, M.; Chiacchio, A.; Acerra, A.; Giordano, F. Palatal Graft Harvesting Site Healing and Pain Management: What Is the Best Choice? An Umbrella Review. Appl. Sci. 2024, 14, 5614. [Google Scholar] [CrossRef]
- Xiang, C.; Zhang, L.; Tao, E. Research progress of enamel matrix derivative on periodontal tissue regeneration: A narrative review. Front. Dent. Med. 2025, 6, 1611402. [Google Scholar] [CrossRef]
- Cairo, F.; Barootchi, S.; Tavelli, L.; Barbato, L.; Wang, H.L.; Rasperini, G.; Graziani, F.; Tonetti, M. Aesthetic-And patient-related outcomes following root coverage procedures: A systematic review and network meta-analysis. J. Clin. Periodontol. 2020, 47, 1403–1415. [Google Scholar] [CrossRef]
- Hajibagheri, P.; Basirat, M.; Tabari-Khomeiran, Z.; Asadi-Aria, A. The efficacy of platelet-rich fibrin (PRF) in post-extraction hard and soft tissue healing and associated complications: A systematic review and meta-analysis of split-mouth randomized clinical trials. BMC Oral Health 2025, 25, 869. [Google Scholar] [CrossRef]
- Baeyens, W.; Glineur, R.; Evrard, L. [The use of platelet concentrates: Platelet-rich plasma (PRP) and platelet-rich fibrin (PRF) in bone reconstruction prior to dental implant surgery]. Rev. Med. Brux. 2010, 31, 521–527. [Google Scholar]
- Valenzuela-Mencia, J.; Manzano-Moreno, F.J. Applications of Platelet-Rich Fibrin (PRF) Membranes Alone or in Combination with Biomimetic Materials in Oral Regeneration: A Narrative Review. Biomimetics 2025, 10, 172. [Google Scholar] [CrossRef]
- Yang, H.; Yu, J.; Wu, D. Platelet-rich fibrin application after mandibular third molar extraction: An umbrella review. Clin. Oral Investig. 2024, 29, 34. [Google Scholar] [CrossRef] [PubMed]
- Dadlani, S. Porcine Acellular Dermal Matrix: An Alternative to Connective Tissue Graft-A Narrative Review. Int. J. Dent. 2021, 2021, 1652032. [Google Scholar] [CrossRef]
- Pabst, A.M.; Happe, A.; Callaway, A.; Ziebart, T.; Stratul, S.I.; Ackermann, M.; Konerding, M.A.; Willershausen, B.; Kasaj, A. In vitro and in vivo characterization of porcine acellular dermal matrix for gingival augmentation procedures. J. Periodontal Res. 2014, 49, 371–381. [Google Scholar] [CrossRef] [PubMed]
- Pabst, A.M.; Lehmann, K.M.; Walter, C.; Krüger, M.; Stratul, S.I.; Kasaj, A. Influence of porcine-derived collagen matrix on endothelial progenitor cells: An in vitro study. Odontology 2016, 104, 19–26. [Google Scholar] [CrossRef]
- Papi, P.; Pompa, G. The Use of a Novel Porcine Derived Acellular Dermal Matrix (Mucoderm) in Peri-Implant Soft Tissue Augmentation: Preliminary Results of a Prospective Pilot Cohort Study. Biomed. Res. Int. 2018, 2018, 6406051. [Google Scholar] [CrossRef]
- Rotundo, R.; Pancrazi, G.L.; Grassi, A.; Ceresoli, L.; Di Domenico, G.L.; Bonafede, V. Soft Tissue Substitutes in Periodontal and Peri-Implant Soft Tissue Augmentation: A Systematic Review. Materials 2024, 17, 1221. [Google Scholar] [CrossRef]






| Authors | Year | Country | Design | N° Patients | N° Sites | Surgery Test vs. Control | Clinical Outcomes | Follow-Up |
|---|---|---|---|---|---|---|---|---|
| Alexiou et al. [52] | 2017 | Greece | RCT (split mouth) | 12 | 54 | mCAF + sCTG vs. mCAF + EMD | CRC, MRC | 6 months |
| Aroca et al. [38] | 2009 | France | RCT (split mouth) | 20 | 67 | mCAF + sCTG vs. mCAF | CRC, MRC | 6 months |
| Cairo et al. [68] | 2016 | Italy | RCT (parallel groups) | 32 | 74 | mCAF vs. mCAF + sCTG | CRC, RDR, KTW, GT, duration of surgery, RES | 12 months |
| Culhaoglu et al. [69] | 2018 | Turkey | RCT (parallel groups) | 22 | 63 | mCAF + sCTG vs. mCAF + PRF (2 and 4 layers) | MRC | 6 months |
| George et al. [39] | 2018 | India | RCT (split mouth) | 15 | 60 | mCAF + placental membrane vs. mCAF | RDR, KTW | 6 months |
| Gurlek et al. [33] | 2019 | Turkey | RCT (split mouth) | 12 | 82 | mCAF + XADM vs. mCAF + sCTG | CRC, RDR, KTW | 1,5 years |
| Khobragade et al. [44] | 2016 | India | RCT (split mouth) | 20 | 116 | mCAF + OB application vs. mCAF | CRC, MRC, RES | 6 months |
| Maluta et al. [70] | 2021 | Brazil | RCT (split mouth) | 15 | 94 | mCAF + sCTG vs. mCAF + XDM | CRC, MRC, RDR, KTW | 6 months |
| Meza-Mauricio et al. [32] | 2021 | Brazil | RCT (parallel groups) | 41 | 130 | mCAF + XADM vs. mCAF + sCTG | CRC, MRC, RDR, KTW, GT, RES | 12 months |
| Nahas et al. [36] | 2020 | Brazil | RCT (split mouth) | 15 | 82 | mCAF + CM vs. mCAF + sCTG | CRC, MRC, RDR, KTW, duration of surgery | 12 months |
| Öncü, E. [35] | 2017 | Turkey | RCT (split mouth) | 30 | 60 | mCAF + Platelet-Rich Fibrin (PRF) vs. mCAF + sCTG | CRC, MRC | 6 months |
| Ozcelik et al. [71] | 2011 | Turkey | RCT (parallel groups) | 41 | 155 | mCAF vs. mCAF + OB | CRC, MRC, RDR, KTW, RES | 6 months |
| Özkan Şen, D. and Öncü, E. [50] | 2023 | Turkey | RCT (parallel groups) | 20 | 118 | mCAF + T-PRF (Titanium Platelet-Rich Fibrin) vs. mCAF + sCTG | MRC | 6 months |
| Ragghianti Zangrando et al. [72] | 2021 | Brazil | RCT (split mouth) | 21 | 84 | mCAF + sCTG (harvested de-epithelialized) vs. mCAF + sCTG (harvested double blade scalpel DBS) | CRC, MRC, RDR, KTW, GT, RES | 6 months |
| Rotundo et al. [73] | 2019 | Italy | RCT (parallel groups) | 24 | 61 | mCAF vs. mCAF + CM | CRC, MRC, RDR, KTW, GT, duration of surgery | 12 months |
| Santamaria et al. [31] | 2023 | Brazil | RCT (parallel groups) | 38 | 78 | mCAF + XADM (NCCLs) vs. mCAF + sCTG (NCCLs) | CRC, MRC, RDR, KTW, GT, duration of surgery | 6 months |
| Zucchelli et al. [74] | 2014 | Italy | RCT (parallel groups) | 50 | 149 | mCAF vs. CAF | CRC, duration of surgery | 5 years |
| Study | Surgical Technique | CRC (%) | MRC (%) | RDR (mm) | ∆KTW (mm) | ∆GT (mm) | RES (0–10) | Duration of Surgery (min) |
|---|---|---|---|---|---|---|---|---|
| Alexiou et al. [52] | MCAF + EMD | 55 | 81.7 | / | 0.58 | / | / | / |
| MCAF + CTG | 63 | 79.7 | / | 1.23 | / | / | / | |
| Aroca et al. [38] | MCAF | 74.62 | 80.7 | / | / | / | / | / |
| MCAF + PRF | 52.23 | 91.5 | / | / | / | / | / | |
| Cairo et al. [68] | MCAF | 47 | / | 2.4 | −0.4 | 0.002 | 7.9 | 54.7 |
| MCAF + CTG | 83 | / | 3.0 | 1.8 | 0.66 | 7.9 | 79.4 | |
| Culhaoglu et al. [69] | MCAF + PRF (2 and 4 layers) | / | 63.00 | / | / | / | / | / |
| MCAF + CTG | / | 80.13 | / | / | / | / | / | |
| George et al. [39] | MCAF + Placental membrane | / | / | 1.206 | 2.133 | / | / | / |
| MCAF | / | / | 1.225 | 0.677 | / | / | / | |
| Gurlek et al. [33] | MCAF + XADM | 70.7 | / | 2.40 | 0.92 | / | / | / |
| MCAF + CTG | 87.8 | / | 2.50 | 0.75 | / | / | / | |
| Khobragade et al. [44] | MCAF | 43.8 | 78,3 | / | / | / | 7.57 | / |
| MCAF + OB | 77.9 | 92.23 | / | / | / | 8.76 | / | |
| Maluta et al. [70] | MCAF + XADM | 75.5 | 92.68 | 2.43 | 0.74 | / | / | / |
| MCAF + CTG | 82.6 | 95.28 | 2.54 | 0.91 | / | / | / | |
| Meza-Mauricio et al. [32] | MCAF + XADM | 70.3 | 80.19 | 2.39 | 0.63 | 0.54 | 8.12 | / |
| MCAF + CTG | 83.3 | 91.79 | 2.75 | 0.99 | 0.77 | 8.31 | / | |
| Nahas et al. [36] | MCAF + CM | 60 | 77.78 | 2.00 | 0.3 | / | / | 31.3 |
| MCAF + CTG | 68 | 82.14 | 2.20 | 1.2 | / | / | 47.7 | |
| Öncü, E. [35] | MCAF + PRF | 50 | 77.12 | / | / | / | / | / |
| MCAF + CTG | 60 | 84 | / | / | / | / | / | |
| Ozcelik et al. [71] | MCAF | 61 | 89.1 | 3.89 | 0.66 | / | 7.43 | / |
| MCAF + OB | 84.6 | 96.2 | 4.65 | 0.48 | / | 8.65 | / | |
| Özkan Şen, D. and Öncü, E. [50] | MCAF + PRF | / | 61.77 | / | / | / | / | / |
| MCAF + CTG | / | 75.31 | / | / | / | / | / | |
| Ragghianti Zangrando et al. [72] | MCAF + CTG (de-epithelialized) | 38 | 82.5 | 2.07 | 0.62 | 0.55 | 8.04 | / |
| MCAF + CTG (double blade scalpel) | 38 | 78 | 2.09 | 0.84 | 0.64 | 8.36 | / | |
| Rotundo et al. [73] | MCAF + CM | 63 | 87 | 2.0 | 0.6 | 0.2 | / | 36.1 |
| MCAF | 52 | 75 | 2.0 | 1.1 | −0.3 | / | 47.3 | |
| Santamaria et al. [31] | MCAF + XADM | 50.7 | 63.6 | 1.57 | 0.3 | 0.30 | / | 37.4 |
| MCAF + CTG | 72.9 | 91.3 | 2.30 | 0.96 | 0.90 | / | 52.7 | |
| Zucchelli et al. [74] | MCAF | 78.08 | / | / | / | / | / | 29.8 |
| MCAF + CTG | 90.78 | / | / | / | / | / | 40.2 |
| Outcomes | № of Participants (Studies) Follow-Up | Certainty of the Evidence (GRADE) | Comments |
|---|---|---|---|
| CRC (%) | 604 (7 RCTs) | ⨁⨁⨁⨁ High | sCTG shows a stat. sig. higher CRC than adjunctive technique, with a high level of evidence. |
| CRC (%)—mCAF + sCTG vs. mCAF + XADM | 384 (4 RCTs) | ⨁⨁⨁⨁ High | sCTG shows a stat. sig. higher CRC than XADM, with a high level of evidence. |
| CRC (%)—mCAF + sCTG vs. mCAF + CM | 82 (1 RCT) | ⨁⨁◯◯ Low a | sCTG shows a non-stat. sig. higher CRC than CM, with a low level of evidence. |
| CRC (%)—mCAF + sCTG (de-ep) vs. mCAF + sCTG (DBS) | 84 (1 RCT) | ⨁⨁◯◯ Low b | sCTG (de-ep) and sCTG (DBS) showed no difference in CRC, with a low level of evidence. |
| CRC (%)—mCAF + sCTG vs. mCAF + EMD | 54 (1 RCT) | ⨁⨁◯◯ Low | sCTG shows a non-stat. sig. lower CRC than EMD, with a low level of evidence. |
| KTW gain (mm) | 557 (7 RCTs) | ⨁⨁⨁⨁ High | sCTG shows a stat. sig. higher KTW gain than adjunctive technique, with a high level of evidence. |
| KTW gain (mm)—mCAF + sCTG vs. mCAF + XADM | 337 (4 RCTs) | ⨁⨁⨁⨁ High | sCTG shows a stat. sig. higher KTW gain than XADM, with high level of evidence. |
| KTW gain (mm)—mCAF + sCTG vs. mCAF + CM | 82 (1 RCT) | ⨁⨁⨁◯ Moderate b | sCTG shows a stat. sig. higher KTW gain than CM, with a moderate level of evidence. |
| KTW gain (mm)—mCAF + sCTG (de-ep) vs. mCAF + sCTG (DBS) | 84 (1 RCT) | ⨁⨁⨁◯ Moderate b | sCTG (de-ep) shows a non-stat. sig. slightly lower KTW gain than sCTG (DBS), with a moderate level of evidence. |
| KTW gain (mm)—mCAF + sCTG vs. mCAF + EMD | 54 (1 RCT) | ⨁◯◯◯ Very low b,c | The SMD between sCTG and EMD was not estimable because no standard deviation was reported. This comparison, based solely on mean values, provided very low level of evidence. |
| RES | 214 (2 RCTs) | ⨁⨁⨁⨁ High | There is no stat. sig. difference between the RES of sCTG and that of adjunctive techniques, with a high level of evidence. |
| RES—mCAF + sCTG vs. mCAF + XADM | 130 (1 RCT) | ⨁⨁⨁◯ Moderate b | sCTG shows a non-stat. sig. slightly higher RES than XADM, with a moderate level of evidence. |
| RES—mCAF + sCTG (de-ep) vs. mCAF + sCTG (DBS) | 84 (1 RCT) | ⨁⨁⨁◯ Moderate b | sCTG (de-ep) shows a non-stat. sig. slightly lower RES than sCTG (DBS), with a moderate level of evidence. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gualtieri, M.; Signoriello, A.; Pardo, A.; Muresan, D.A.; Zangani, A.; Faccioni, P.; Corrocher, G.; Lombardo, G. Modified Coronally Advanced Flaps: A Systematic Review and Meta-Analysis. Dent. J. 2025, 13, 477. https://doi.org/10.3390/dj13100477
Gualtieri M, Signoriello A, Pardo A, Muresan DA, Zangani A, Faccioni P, Corrocher G, Lombardo G. Modified Coronally Advanced Flaps: A Systematic Review and Meta-Analysis. Dentistry Journal. 2025; 13(10):477. https://doi.org/10.3390/dj13100477
Chicago/Turabian StyleGualtieri, Miriana, Annarita Signoriello, Alessia Pardo, Diana Andreea Muresan, Alessandro Zangani, Paolo Faccioni, Giovanni Corrocher, and Giorgio Lombardo. 2025. "Modified Coronally Advanced Flaps: A Systematic Review and Meta-Analysis" Dentistry Journal 13, no. 10: 477. https://doi.org/10.3390/dj13100477
APA StyleGualtieri, M., Signoriello, A., Pardo, A., Muresan, D. A., Zangani, A., Faccioni, P., Corrocher, G., & Lombardo, G. (2025). Modified Coronally Advanced Flaps: A Systematic Review and Meta-Analysis. Dentistry Journal, 13(10), 477. https://doi.org/10.3390/dj13100477







