Abstract
Background: Gingival recession (GR) is defined as the exposure of the root surface due to the gingival margin shifting apically from the cemento-enamel junction. Current effective management of defects related to GR relies on root coverage periodontal plastic surgery (RCPPS), using the Modified Coronally Advanced Flap (mCAF) with an envelope design. Recent literature also reported the association of different biomaterials to the mCAF procedure. In light of these considerations, a systematic review (SR) was conducted to determine and compare the efficacy of all mCAF adjunctive techniques for the treatment of multiple adjacent GR-type (MAGR) defects. Methods: An electronic search was conducted in 2025 on studies published between 2013 and 2025, using PubMed, Scopus, Web of Science, and Cinahl Complete, to address the focused question: “which is the efficacy of different mCAF adjunctive techniques for the treatment of multiple adjacent GR-type defects, in terms of root coverage (RC), esthetic outcomes, and keratinized tissue (KT) augmentation?”. Randomized controlled trials with a minimum follow-up of 6 months with ≥ 5 patients treated for coverage of MAGR were included. Risk of bias was assessed with RoB 2 Tool. A meta-analysis was performed using RevMan5.4 software and the level of evidence of included studies was analyzed with GRADEPro GDT. Results: A total of 17 studies were included in the SR, 9 of which evaluating mCAF + sCTG (subepithelial connective tissue graft) vs. mCAF adjunctive techniques [Collagen Matrix (CM), xenogeneic acellular dermal matrix (XADM), Platelet-Rich Fibrin (PRF), Enamel Matrix Derivatives (EMD), sCTG harvested double blade scalpel] were then included in the meta-analysis. The primary outcomes of complete root coverage (CRC) and keratinized tissue width variation (ΔKTW) were statistically significant ([CRC: Odds Ratio (OR) 1.70; 95% CI (confidence interval) 1.18, 2.44; p = 0.004]; [ΔKTW: SMD (standardized mean difference) 0.37; 95% CI 0.11, 0.63; p = 0.005]) in favor of mCAF + CTG. Meanwhile, no statistically significant difference was observed in terms of RES. The certainty assessment highlighted relevant results: despite the lack of evidence in the long-term, a high level of evidence showed that sCTG was more effective than XADM in terms of CRC (p = 0.002) and ΔKTW (p = 0.0001). A low level of evidence revealed that sCTG achieved a greater ΔKTW compared to CM (p = 0.0006). Although no significant differences were observed, a low level of evidence suggested that mCAF + EMD and mCAF + sCTG (DBS) may provide good results. To date, only one RCT showed long-term stable results of CTG in terms of RC. Conclusions: The association of sCTG to mCAF demonstrated better results in terms of RC and KTW augmentation in short- and medium-term follow-ups. Long-term studies are needed to confirm the efficacy of the other mCAF adjunctive techniques, considering limitations due to heterogeneity in follow-ups, distribution of techniques analyzed, and different study designs. Registration in PROSPERO (International prospective register of systematic reviews) was performed with ID CRD420251085823.
1. Introduction
Gingival recession (GR), defined as the exposure of the root surface due to the apical shift in the gingival margin from the cemento-enamel junction [1,2], is usually associated with impaired esthetics. If left untreated, it can lead to dental hypersensitivity, poor plaque control, root caries, and even loss of periodontal support [2,3]. These functional and esthetic issues are more frequently perceived in younger individuals, especially in the case of deeper GR and involved anterior areas, even in the presence of non-carious cervical lesions [4].
The development of GR is related to various etiological factors, mainly inflammatory, anatomical, or mechanical, such as plaque-induced periodontal disease [5,6,7], viral infections [8], traumatic tooth brushing [9], aberrant frenum attachment [10], thin gingival phenotype [11], malocclusion and dental crowding [12], subgingival restorative margin invading the biological width [13,14], orthodontic treatment [15,16], and lip/tongue piercings [17].
Multiple adjacent recessions are even more challenging defects, as the surgical field is larger and more anatomical variations may be present (prominent roots, shallow vestibules, defect size) [18]. Current effective management of these defects relies on root coverage periodontal plastic surgery (RCPPS). Several randomized clinical trials (RCTs) and systematic reviews (SRs) analyzed the efficacy of the most used RCPPS techniques, e.g., the Coronally Advanced Flap (CAF) with or without subepithelial connective tissue graft (sCTG), and the Coronally Advanced Tunnel technique (CAT) with or without sCTG [19,20,21,22,23]. Successful treatment of GR aims to eliminate etiologic factors related to the onset and progression of the defect, characterizing the phenotype of the recession site and adjacent areas, and selecting the most suitable option [24]. In this context, the CAF is commonly considered the gold standard to treat GR [19,25], as it typically renders the best cost–benefit treatment outcomes in terms of complete root coverage (CRC), mean root coverage (MRC), keratinized tissue width (KTW) gain, and long-term stability of treatment outcomes.
Nevertheless, vertical releasing incisions performed with the CAF may disrupt its vascularity or negatively influence the esthetic outcome due to keloid/scar formation [26]. To address these drawbacks, a Modified Coronally Advanced Flap (mCAF) was proposed, with the employment of an envelope design, characterized by a sub-marginal oblique incision in the papillary area, anticipating the rotational movement of the surgical papilla during coronal advancement [27], without the need for vertical incisions. Further studies reported improved clinical and esthetic outcomes with the additional use of connective tissue graft (CTG) to this novel approach, compared to the conventional bilaminar technique [28,29].
Recent literature focused on the association of different biomaterials as an adjunct to the flap alone: acellular dermal matrix (ADM) [30], xenogenic acellular dermal matrix (mCAF + XADM) [31,32,33,34], Platelet-Rich Fibrin (mCAF + PRF) [35], Collagen Matrix (mCAF + CM) [36,37], barrier membrane (mCAF + PRF membrane, mCAF + placental membrane) [38,39], hyaluronic acid (HA) [40,41,42], other adjunctive techniques, e.g., the orthodontic button application (mCAF + OB) [43,44], or the use of a microsurgical approach [45].
Based on the hypothesis that these mCAF adjunctive techniques may provide efficacy not only in the short-, but also in the long-term treatment of multiple adjacent GR-type defects, a SR was conducted in 2025 to determine and compare their outcomes in terms of root coverage (RC), esthetic outcomes, and keratinized tissue (KT) augmentation. The novelty of this SR lies in its specific clinical focus on these latest mCAF adjunctive techniques, with the aim of enriching comparison between them and mCAF alone.
2. Materials and Methods
This study was conducted in 2025 in accordance with the PRISMA guidelines and checklist (2020) [46]. The review was conducted according to the population, intervention, comparison, outcome, and study design (PICOS) format [47]. Registration in PROSPERO (International prospective register of systematic reviews) was performed with ID CRD420251085823 on 4 July 2025.
2.1. Search Strategy
An electronic search was conducted using the following databases: PubMed, Scopus, Web of Science, and Cinahl Complete, considering studies published between 2013 and 2025.
In MEDLINE (PubMed) the following search terms were used:
- (1)
- ((multiple recessions[Title/Abstract]) OR (multiple recession-type defects[Title/Abstract])) AND (treatment[Title/Abstract]);
- (2)
- Modified Coronally Advanced Flap[Title/Abstract].
In Scopus the following search terms were used:
- (1)
- ((TITLE-ABS-KEY (multiple AND recessions) OR TITLE-ABS-KEY (multiple AND recession-type AND defects)) AND TITLE-ABS-KEY (treatment));
- (2)
- TITLE-ABS-KEY(modified AND coronally AND advanced AND flap).
In Web of Science the following search terms were used:
- (1)
- ((TI = (multiple recessions)) OR TI = (multiple recession-type defects)) AND TI = (treatment);
- (2)
- TI = (Modified Coronally Advanced Flap).
In Cinahl Complete the following search terms were used:
- (1)
- TI multiple recessions OR TI multiple recession-type defects AND TI treatment;
- (2)
- TI Modified Coronally Advanced Flap.
Focused Question
The focused question was defined as follows:
“What is the efficacy of different mCAF adjunctive techniques for the treatment of multiple adjacent GR-type defects, in terms of root coverage (RC), esthetic outcomes, and keratinized tissue (KT) augmentation?”. Furthermore, the aim of the literature search was to evaluate the long-term results of these mCAF adjunctive techniques.
2.2. Inclusion Criteria and Selection Process
Study selection criteria based on the PICOS (Population, Intervention, Comparison, Outcomes, and Study design) framework were as follows.
2.2.1. Types of Participants
Based on the defined focused question, studies with patients with at least two gingival recession (GR) defects were included. Miller classification [48] and recession-type (RT) classification based on the interdental clinical attachment level [49] were considered.
2.2.2. Types of Interventions
The following root coverage surgical procedures for the treatment of multiple gingival recessions were considered:
- mCAF (Modified Coronally Advanced Flap): An envelope type of flap proposed by Zucchelli and De Sanctis [27], characterized by a horizontal incision consisting of oblique submarginal incisions in the interdental areas, which continued with the intra-sulcular incision at the recession defects. This kind of design anticipates the rotation of the surgical papilla;
- mCAF + sCTG (subepithelial connective tissue graft): The envelope type of CAF proposed by Zucchelli and De Sanctis [27], with site-specific subepithelial connective tissue graft [31,32,33,34,35,45,50];
- mCAF + PRF (Platelet-Rich Fibrin): PRF is a second-generation platelet concentrate prepared from centrifuged blood in glass or titanium tube (T-PRF). It is associated with the mCAF technique in the form of PRF membrane [35,38,50];
- mCAF + CM (Collagen Matrix): CM is a resorbable, three-dimensional (3D) matrix of pure type I and III porcine collagen obtained with standardized and controlled manufacturing processes without cross-linking or chemical treatment [36,51];
- mCAF + XADM (xenogeneic acellular dermal matrix): XADM is 3D porcine-derived acellular dermal matrix of collagen and elastin, which undergoes several purification processes that remove the full rejection potential of the tissue [31,32,33,34];
- mCAF + OB (Orthodontic Button) application: After the coronally displacement, sutures were stabilized with orthodontic buttons [43,44];
- mCAF + placental membrane: A placental allograft deriving from amnion and chorion was used for the first time to compare mCAF + placental membrane to mCAF alone in the treatment of gingival recession [39];
- mCAF + EMD (Enamel Matrix Derivatives): EMD was evaluated for its potential both in regeneration of intrabony defects and in root coverage surgical procedures [52].
2.2.3. Types of Studies
Randomized controlled trials with a minimum follow-up of 6 months with ≥5 patients were included. Retrospective studies, prospective studies, in vitro studies, animal studies, case reports, case series, narrative reviews, and systematic reviews were excluded.
2.2.4. Types of Measures: Primary and Secondary Outcomes
The variables sought in each study were defined as follows.
Primary outcomes were as follows:
- Complete root coverage (CRC) [53,54]: A percentage value describing the number of sites, with respect to the total number of sites treated, that obtained a complete radicular covering at a given time of follow-up. The formula is reported as CRC = (n. of sites with CRC)/(total n. of sites treated) × 100%;
- Root esthetic score (RES) [55,56,57]: A score evaluating level of the gingival margin, marginal tissue contour, soft tissue texture, mucogingival junction alignment, and gingival color. Regarding assessment of the final position of the gingival margin, 3 points are given for partial root coverage and 6 points for complete root coverage, 0 points are assigned when the final position of the gingival margin is equal or apical to the previous recession. One point is assigned for each of the other four variables. Thus, 10 points is the perfect score;
- Differential keratinized tissue width (ΔKTW) [58,59], where KTW is the distance from the free gingival margin to the mucogingival junction.
Secondary outcomes were as follows:
- Mean root coverage (MRC) [60]: A percentage value that describes the rate of reduction in the recession compared to the initial recession;
- Recession depth reduction (RDR) [61,62]: A value in mm which describes the difference between the recession depth measure at a given follow-up and the measure of the initial recession depth;
- Differential gingival thickness (ΔGT) [31,34,59], where GT is a measurement in mm which indicates the thickness of the attached gingiva;
- Duration of surgery, measured in minutes.
2.3. Data Collection, Extraction, and Management
Titles of the studies assessed through the search previously described (using the predetermined inclusion and exclusion criteria) were screened by two independent examiners (M.G. and A.S.), to minimize the risk of reviewer bias. Duplicates were deleted. Data collection from the included reports was performed by the two reviewers, who independently worked with an Excel spreadsheet. In the case of disagreement regarding eligibility, the two reviewers analyzed the title jointly to reach a final decision concerning inclusion or exclusion. Articles identified as potentially useful through analysis of the title were then selected for a more in-depth investigation by reading the abstract. In the examination of the abstract, attention was paid to assess the compliance of the study with the inclusion criteria. The selected studies were then saved as a digital version and submitted for full-text reading. In this way, only articles that fulfilled all criteria of the selection process were finally included for data extraction.
Data extraction and management were performed by filling in a table in the Excel spreadsheet with the following data: Titles, Authors, Year, Design, N° Patients, N° Sites, Surgery Test vs. Control, N° Patients in each group, N° Sites in each group, CRC (%), % RC, RDR, ΔKTw, ΔGT, Duration of the surgery (min), RES, Follow-up.
2.3.1. Assessment of Risk of Bias of the Included Studies
According to the Risk of Bias 2 (RoB 2) Tool [63], the following parameters were adopted for the evaluation of risk of bias for RCTs: random sequence generation and allocation concealment (selection bias), blinding of participants and personnel (performance bias), blinding of outcome assessment (detection bias), incomplete outcome data (attrition bias), selective reporting (reporting bias). In the event of a disagreement between the same two reviewers (M.G. and A.S.), additional discussion was used to reach a consensus. All data were represented through a risk of bias graph and a risk of bias summary.
All data were graphically represented through a traffic-light plot and a summary plot by uploading the data into the Robvis web application (visualization tool) [64].
2.3.2. Quantitative Data Synthesis Method
A Meta-Analysis was carried out using RevMan5 software [65].
Primary and secondary outcomes were considered in performing the meta-analysis, examining both dichotomous variables (CRC) and continuous variables (MRC, GT gain, RDR, KTW gain, RES, duration of surgery).
For the dichotomous CRC data, the inverse variance method was applied with the risk ratio (RR) as the main effect measure. The random effects model was adopted, which considers variation between studies in addition to random error, allowing for generalization of results to a broader population. Results were presented with a 95% confidence interval, providing a precise estimate of the effect with a suitable level of certainty.
For continuous data (MRC, GT gain, RDR, KTW gain, and duration of surgery) the inverse variance method was also employed. However, in this case, the effect measure used was the standard mean difference (SMD). The magnitude of the SMD was interpreted as mild if SMD = 0.2, mean if SMD = 0.5 and high if SMD = 0.8.
The heterogeneity between studies was assessed with the heterogeneity index of Higgins (I2). Heterogeneity is considered low if I2 is less than 40%, moderate if I2 is between 40% and 70%, substantial if I2 is between 70% and 90%, and considerable if I2 is more than 90%. When the heterogeneity was low (I2 < 40%), a fixed effects model was applied; otherwise, a random effects model analysis was undertaken to account for variation between studies and obtain more robust estimates. Parallel-group and split-mouth studies were combined in the meta-analyses of treatment effects. The significance level was set at alpha = 0.05. Results were reported with a 95% confidence interval (CI) to indicate the precision of the estimates. All data were graphically represented using a forest plot.
Subgroups analysis was conducted considering the threshold of p-value as less than 0.1 [66]. Results were reported with the significance of subgroup differences at every level of heterogeneity: in case of moderate to high heterogeneity, meta-analysis was included, but the uncertainty in the evidence was acknowledged as inconsistency between individual trial results [66], thus these results were retained but interpreted with caution.
2.3.3. Certainty Assessment
The certainty assessment was conducted using GRADEpro GDT [67].
The same two reviewers (M.G. and A.S.) evaluated the certainty of evidence based on the following factors: risk of bias, inconsistency, indirectness, imprecision, publication bias, large effect, plausible confounding, and dose–response gradient. In the event of disagreement between the two reviewers, additional discussion was used to reach a consensus.
3. Results
3.1. Results of the Study Search
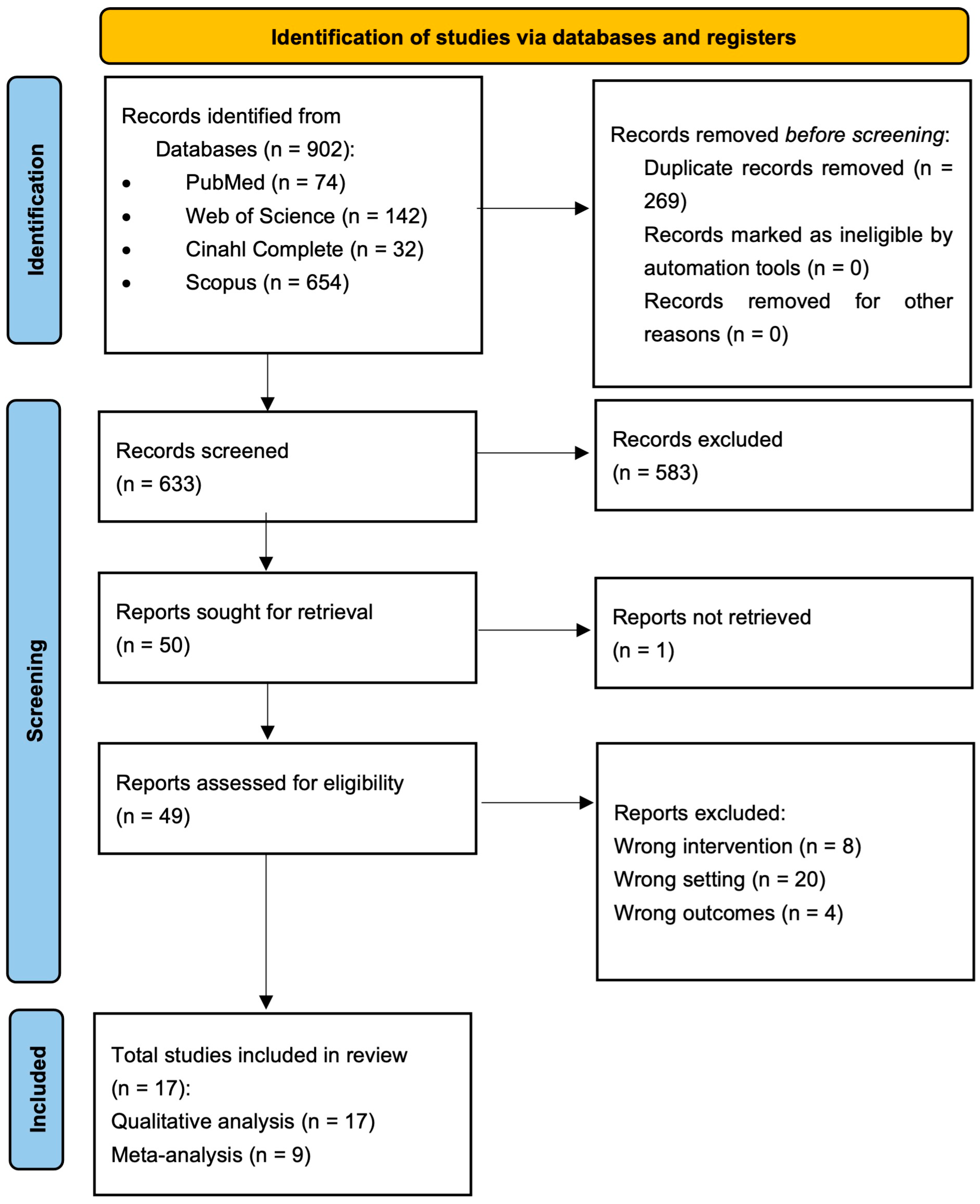
The electronic search through the PubMed database identified 74 publications, the search using the Scopus database identified 654 publications, the Web of Science database identified 142 publications and the Cinahl Complete database identified 32 publications. Following the removal of all duplicates, 633 articles were identified up to the date of search (1 July 2025). Among these, after reading all titles and abstracts, 50 publications were sought for retrieval (one study was not retrieved). The full text analysis led to the exclusion of 32 articles with specified reasons, so the electronic search finally identified 17 articles, whose data are reported in Figure 1.
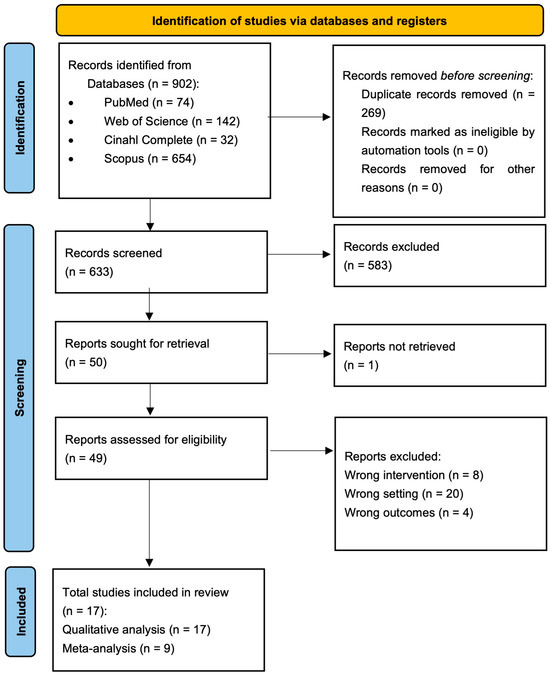
Figure 1.
Flow chart summarizing the study selection procedure, constructed in accordance with PRISMA guidelines (2020).
3.2. Characteristics of the Included Studies
All 17 studies included in the SR (see Table 1) were RCTs. Nine of these articles were performed with a split-mouth design, where each patient received both the test and control surgical interventions; in eight studies, a parallel-groups design was adopted, assigning patients to either the test or control surgery, respectively.

Table 1.
Summary and characteristics of the included studies in the SR.
The number of patients included in each study ranged from 7 to 50 and the number of treated sites (number of GRs) ranged from 14 to 269.
The characteristics of the included studies are described in detail in Table 1.
3.3. Risk of Bias
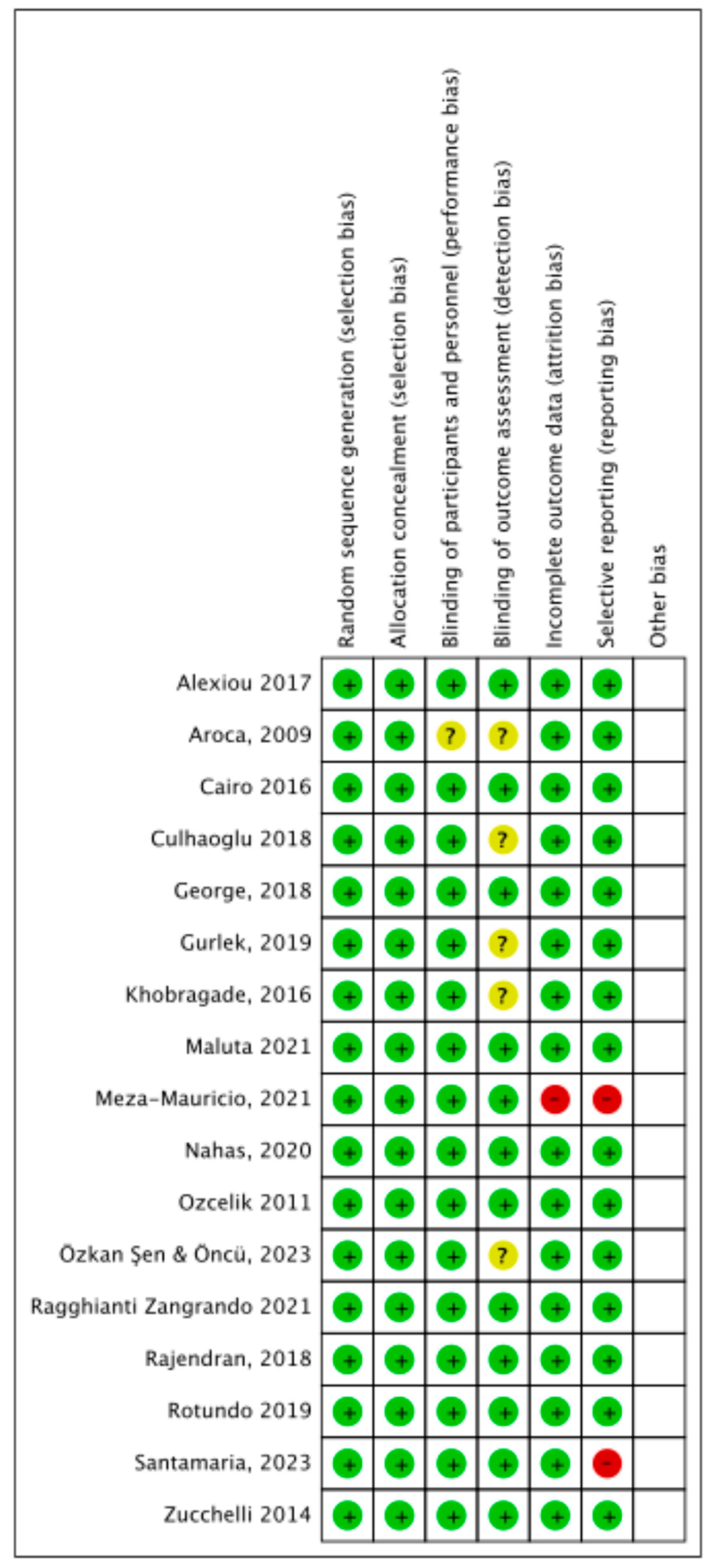
Risk of bias (Figure 2 and Figure 3) in the included RCTs was evaluated using the data extracted from each trial.
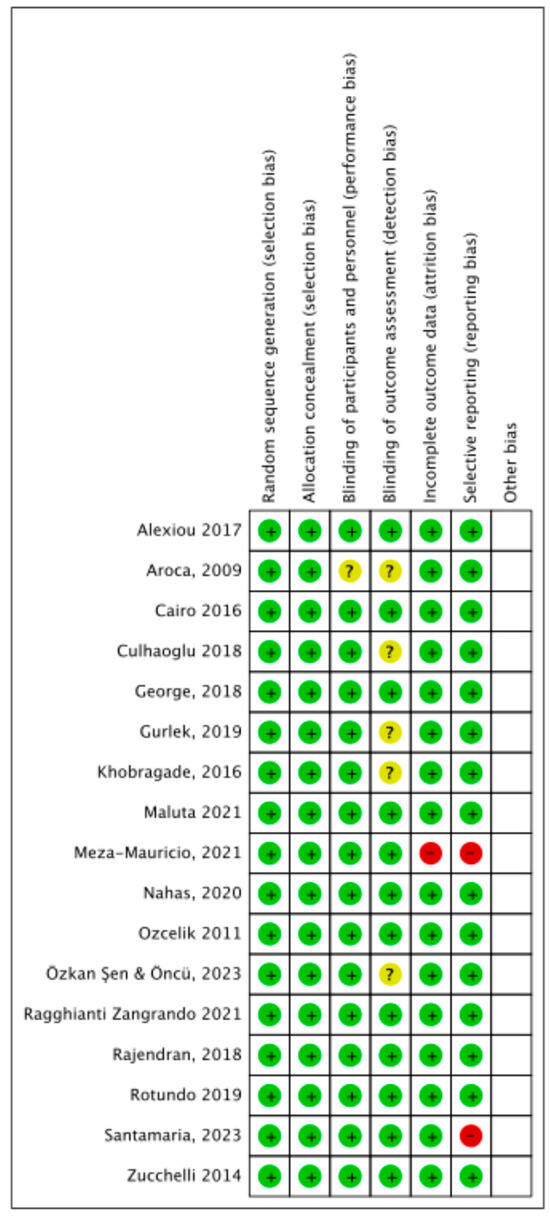
Figure 2.
Risk of bias summary: Review authors’ judgements about each risk of bias item for each included study (RCTs); green color: low risk; yellow color: some concerns or unclear risk; red color: high risk ([31,32,33,36,38,39,43,44,50,52,68,69,70,71,72,73,74]).
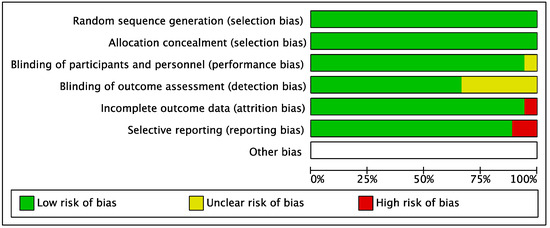
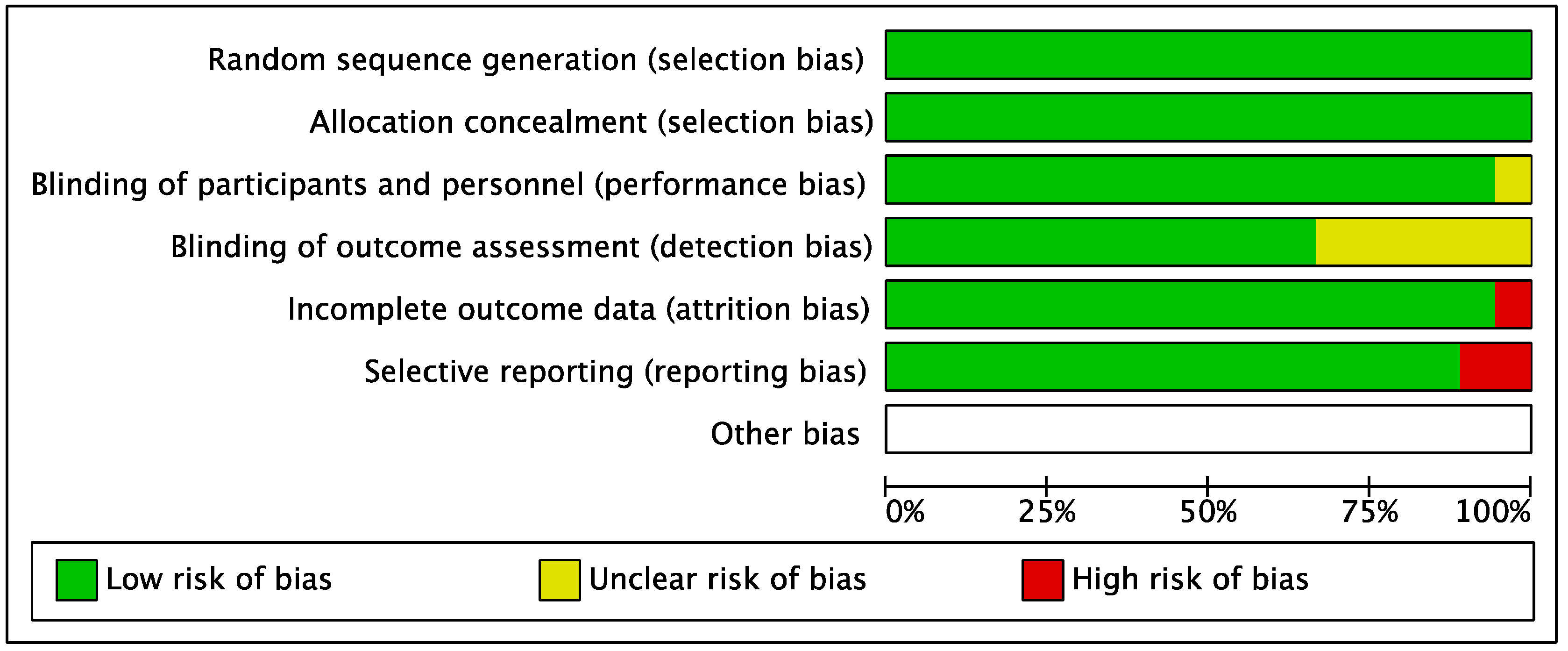
Figure 3.
Risk of bias graph: Review authors’ judgements about each risk of bias item presented as percentages across all included studies.
All trials reported an adequate method of randomization and allocation concealment.
Sixteen trials reported adequate blinding of participants and personnel. One trial [38] was considered unclear as it did not mention the blinding of participants and personnel.
Regarding the blinding of outcomes assessment, 12 trials were considered at low risk of bias, while in 5 trials the blinding of the examiners was not mentioned, thus it was considered as unclear.
Most of the studies were at low risk of bias for incomplete outcomes data domain, except for one trial [32] in which esthetic (VAS) and pain (VAS) values were reported on a graphic scale, without reporting the mean values.
Selective reporting was considered at low risk of bias for 15 studies. The bias from selective outcomes reporting was considered high for 2 studies: respectively, in the first study [32], esthetic (VAS) and pain (VAS) values were reported on a graphic scale, while in the second study [31], the 3-month clinical measurements mentioned were not reported.
Results of individual studies included in the SR are described in Table 2. CRC was reported in 14 studies [31,32,33,35,36,38,44,52,68,70,71,72,73,74]. MRC was reported in 13 studies [31,32,35,36,38,44,50,52,69,70,71,72,73]. RDR was reported in 10 studies [31,32,33,36,39,68,70,71,72,73]. RES was reported by five studies [32,44,68,71,72]. ∆GT was reported in five studies [31,32,68,72,73]. ∆KTW was reported in 10 studies [31,32,33,36,39,68,70,71,72,73]. Duration of surgery was reported in five studies [31,36,68,73,74].

Table 2.
Outcomes of individual studies included in the SR.
3.4. Synthesis of Results of Meta-Analysis
Of the 17 included studies, 9 evaluating mCAF + sCTG vs. mCAF variation (CM, XADM, PRF, EMD, sCTG harvested double blade scalpel) were included in the following meta-analysis (Figures 4–10):
- −
- mCAF + sCTG vs. mCAF + XADM [31,32,33,70];
- −
- mCAF + sCTG vs. mCAF + CM [36];
- −
- mCAF + sCTG vs. mCAF + PRF [35,50,69];
- −
- mCAF + sCTG vs. mCAF + EMD [52];
- −
- mCAF + sCTG (de-epithelialized) vs. mCAF + CTG (harvested double blade scalpel) [72].
The six parameters considered were CRC, MRC, RDR, KTW gain, GT gain, RES, duration of surgery. For each parameter, we created a forest plot to explore the efficacy of mCAF adjunctive techniques (test) compared to mCAF + sCTG (control).
When outcomes were reported, comparisons were divided into subgroups:
- -
- mCAF + sCTG (control) vs. mCAF + XADM (test);
- -
- mCAF + sCTG (control) vs. mCAF + CM (test);
- -
- mCAF + sCTG (control) vs. mCAF + PRF (test);
- -
- mCAF + sCTG (control) vs. mCAF + EMD (test);
- -
- mCAF + sCTG (de-epithelialized) (control) vs. mCAF + CTG (harvested double blade scalpel) (test).
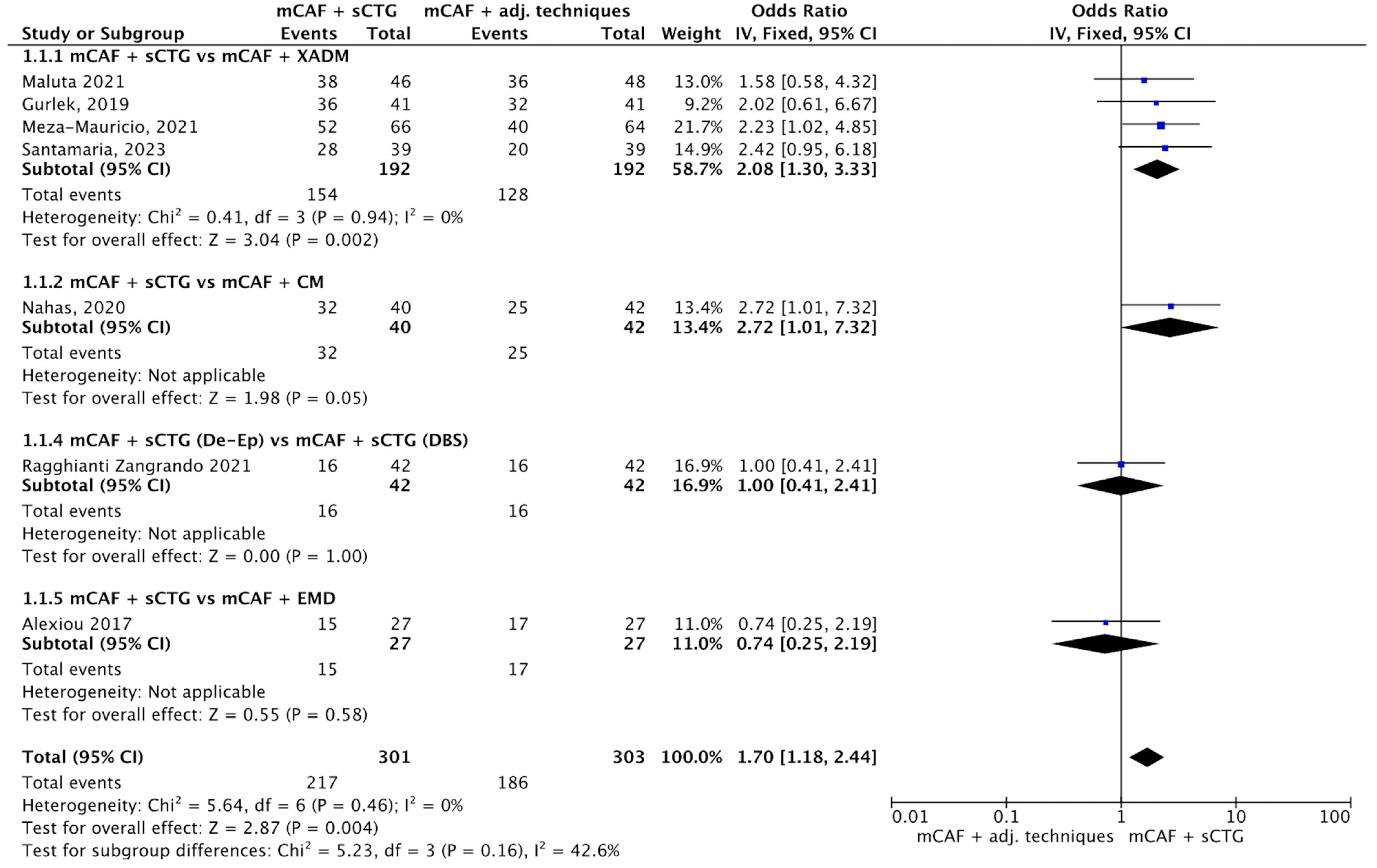
3.4.1. CRC
Eight trials reported this outcome (see Figure 4) [31,32,33,36,52,70,72]. The I2 value was 0%, indicating no observed heterogeneity among studies; therefore, a fixed-effect model was applied. The overall Odds Ratio (OR) was 1.70 [95% CI: 1.18 to 2.44], with a p-value of 0.004, indicating a statistically significant difference in favor of mCAF + sCTG.
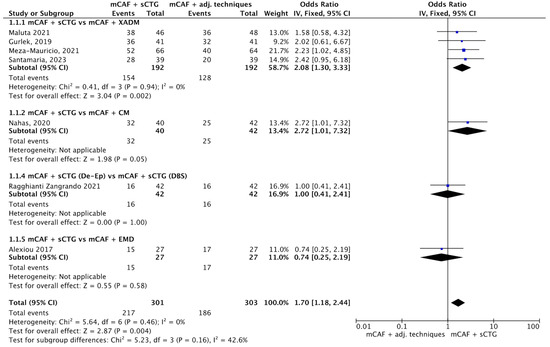
Figure 4.
Forest plot of comparison: mCAF + sCTG vs. mCAF adjunctive techniques, outcome: CRC (%) ([31,32,33,36,52,70,72]).
In the subgroup mCAF + sCTG vs. mCAF + XADM, 192 sites were treated in each group. The I2 was 0%, so heterogeneity was considered low, and a fixed-effect model was used. The difference between groups was statistically significant (p = 0.002) in favor of mCAF + sCTG. In the subgroups mCAF + sCTG vs. mCAF + CM, mCAF + sCTG (de-epithelialized) vs. mCAF + sCTG (DBS), and mCAF + sCTG vs. mCAF + EMD, the differences between groups were not statistically significant, thus the test for heterogeneity was not applicable in these cases.
The test for subgroup differences showed no statistically significant interaction between the subgroups (Chi2 = 5.23, degrees of freedom (df) = 3, p = 0.16), although a moderate degree of heterogeneity was observed (I2 = 42.6%), suggesting that the treatment effect was relatively consistent across the different types of substitutes evaluated.
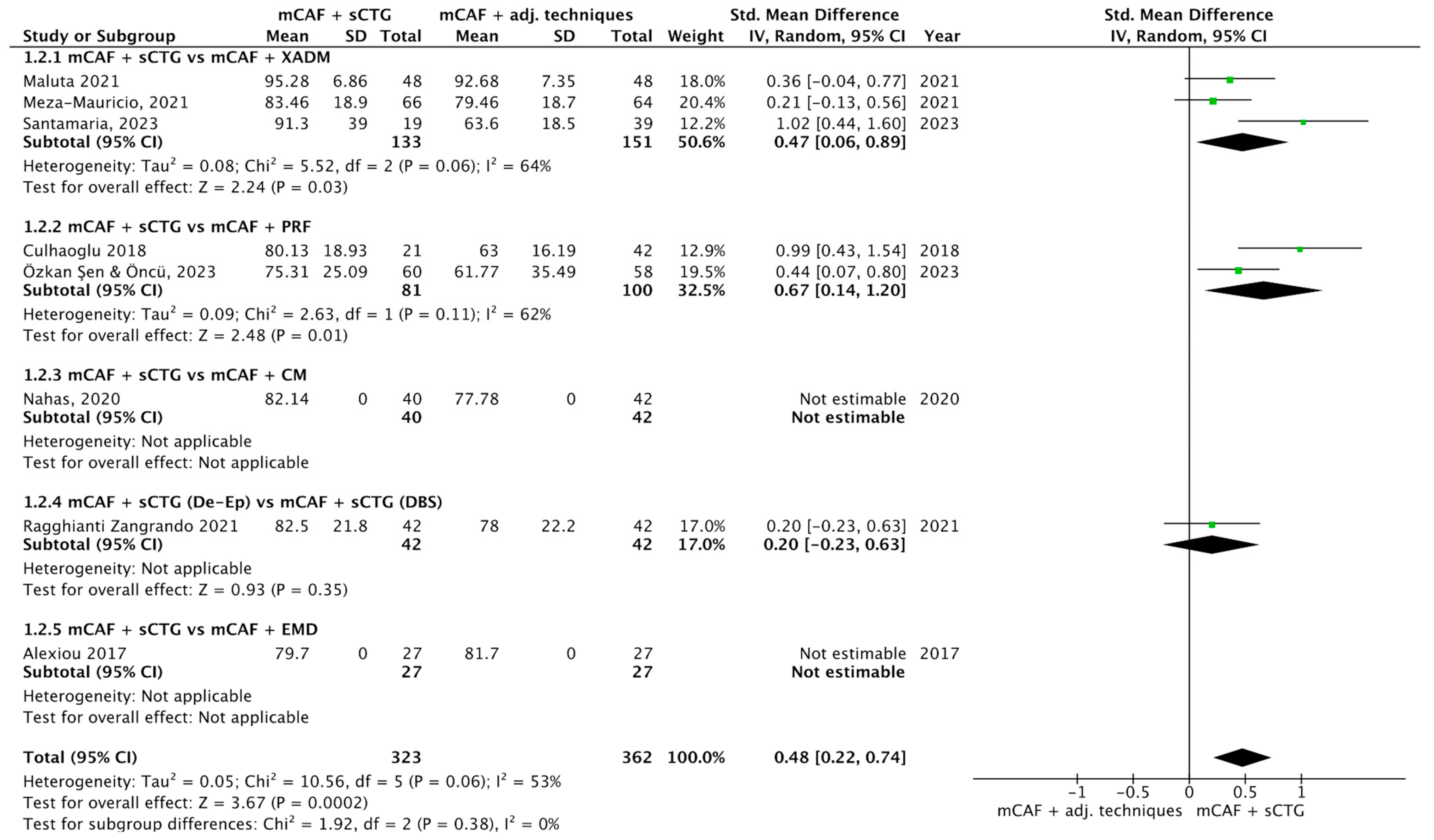
3.4.2. MRC
Nine trials reported this outcome (Figure 5) [31,32,35,36,50,69,70,72,73]. I2 value was 58%, which indicates moderate heterogeneity: for this reason, the random effect model was used. The SMD was 0.48 (95% CI from 0.22 to 0.74) with a p-value of 0.0002, indicating a statistically significant difference in favor of mCAF + sCTG.
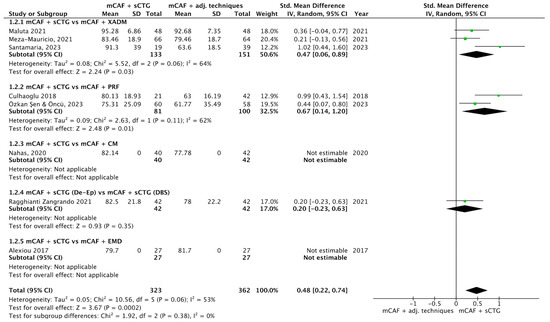
Figure 5.
Forest plot of comparison: mCAF + sCTG vs. mCAF adjunctive techniques, outcome: mean root coverage (MRC) (%) ([31,32,35,36,50,69,70,72,73]).
In the subgroup mCAF + sCTG (151 sites) vs. mCAF + XADM (133 sites), I2 value was 64%, so the heterogeneity was considered moderate. The difference between groups was statistically significant in favor of sCTG (p = 0.03). Even more evident was the analysis of the subgroup mCAF + sCTG vs. mCAF + PRF, which showed a p-value of 0.01. In the subgroups mCAF + sCTG vs. mCAF + CM, mCAF + sCTG (de-epithelialized) vs. mCAF + sCTG (DBS), and mCAF + sCTG vs. mCAF + EMD, no significant difference was found, thus test for heterogeneity was not applicable in these cases.
The test for subgroup differences yielded a Chi2 value of 1.92, with 2 df (p = 0.38), and I2 = 0%, indicating that no statistically significant difference in treatment effects across the subgroups was found. The low I2 value suggests no heterogeneity between subgroups, implying that the treatment effect is consistent across these groups.
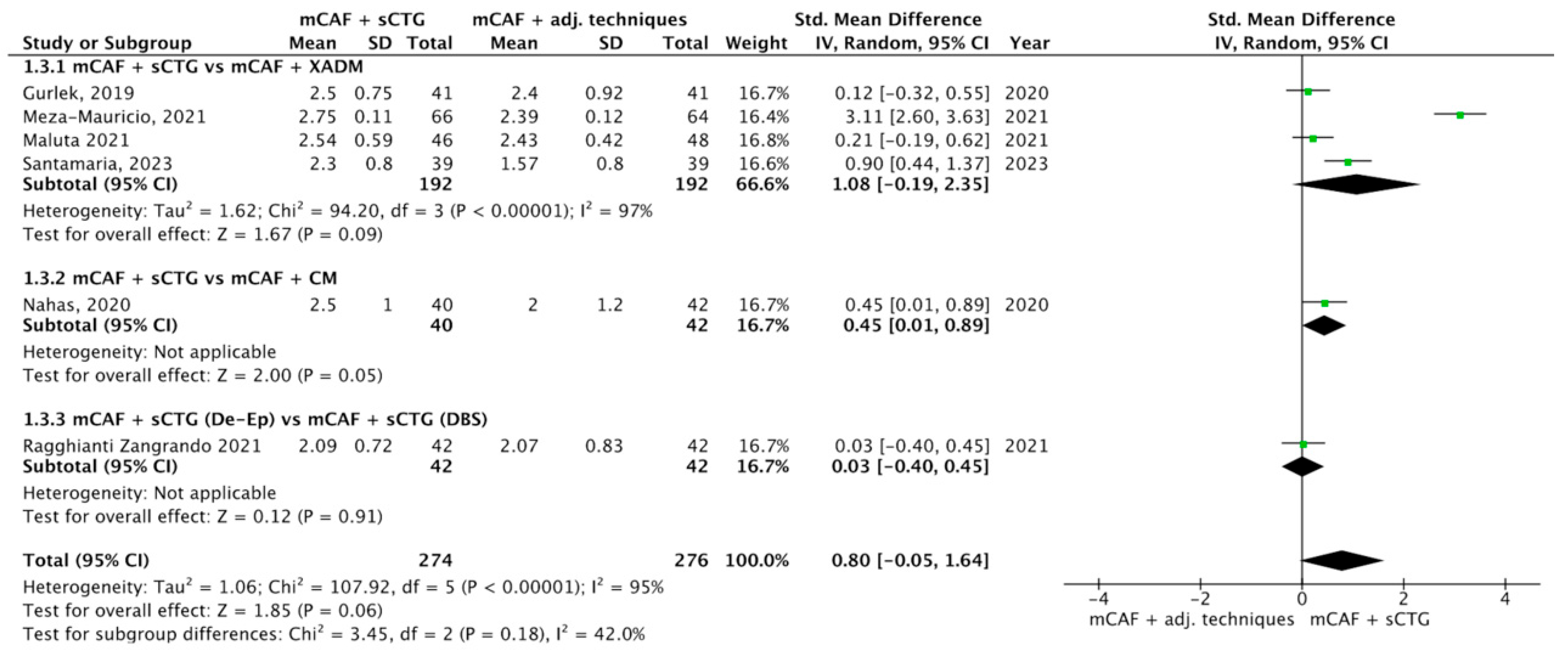
3.4.3. RDR
Five trials reported this outcome (Figure 6) [31,32,33,36,70,72]. I2 value was 95%, which indicates considerable heterogeneity: for this reason, the random effect model was applied. The SMD was 0.80, with 95% CI from −0.05 to 1.64 and p = 0.06 (not statistically significant).
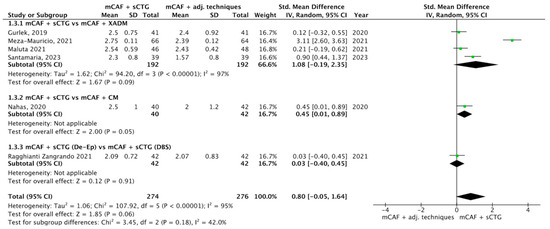
Figure 6.
Forest plot of comparison: mCAF + sCTG vs. mCAF adjunctive techniques, outcome: recession depth reduction (RDR) (mm) ([31,32,33,36,70,72]).
In the subgroup mCAF + sCTG vs. mCAF + XADM, 192 sites were treated with each technique. The difference between groups was not statistically significant, even if a higher value of RDR was recorded with the sCTG. In the subgroups mCAF + sCTG vs. mCAF + CM and mCAF + sCTG (de-epithelialized) vs. mCAF + sCTG (DBS), the differences between groups were not statistically significant, thus test for heterogeneity was not applicable in these cases.
The test for subgroup differences yielded a Chi2 value of 3.45 with 2 df (p = 0.18) and I2 = 42%, indicating a not statistically significant difference in treatment effects across the subgroups analyzed. The moderate I2 value suggests some variability between subgroups; however, this variation is not statistically significant and may be attributed to chance.
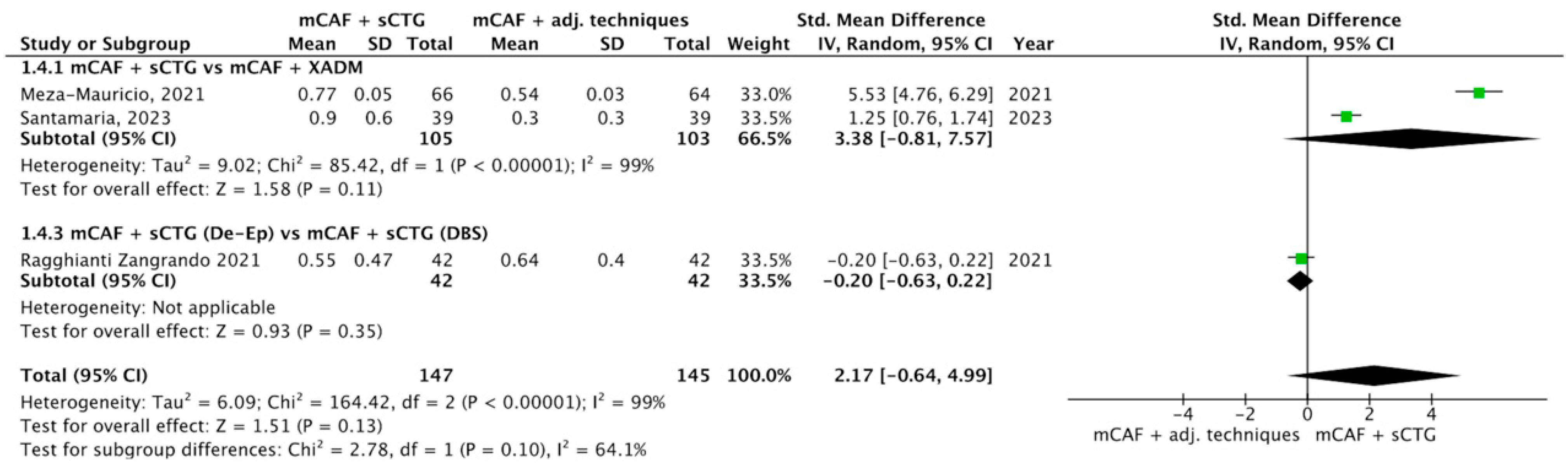
3.4.4. ∆GT
Three trials reported this outcome (Figure 7) [31,32,72]. I2 value was 99%, indicating considerable heterogeneity: the random effect model was thus applied. The difference between groups was not statistically significant (p = 0.10; SMD = 2.17; 95% CI from −0.64 to 4.99).
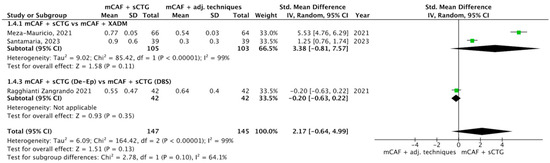
Figure 7.
Forest plot of comparison: mCAF + sCTG vs. mCAF adjunctive techniques, outcome: gingival thickness (GT) gain (mm) ([31,32,72]).
In the subgroups mCAF + sCTG (105 sites) vs. mCAF + XADM (103 sites) and mCAF + sCTG (de-epithelialized) (42 sites) vs. mCAF + sCTG (DBS) (42 sites), the differences were not statistically significant.
The test for subgroup differences yielded a Chi2 value of 2.78 with one df (p = 0.10) and I2 = 64%, indicating that no statistically significant difference was found between subgroups, while the I2 value reflects substantial heterogeneity.
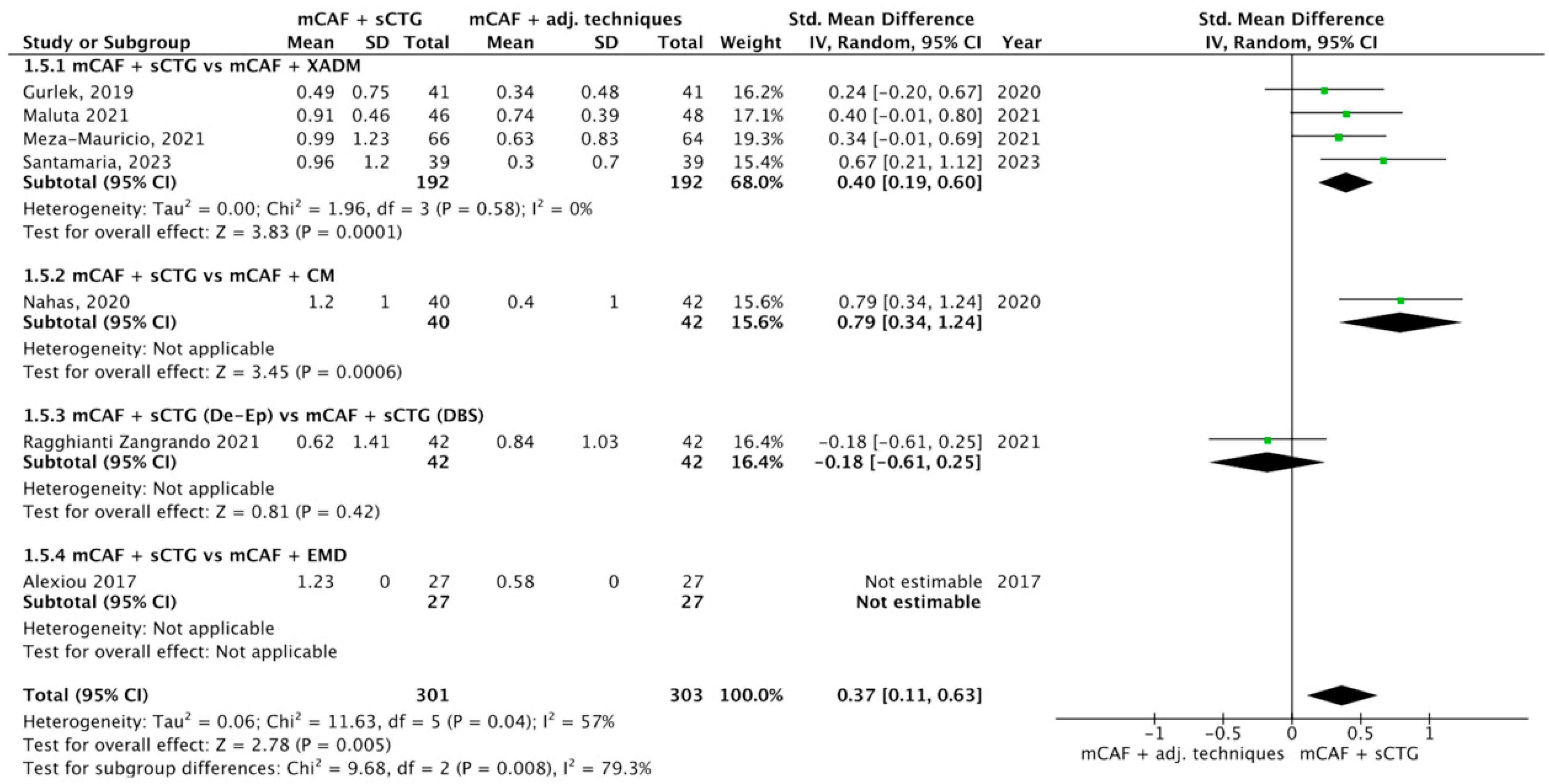
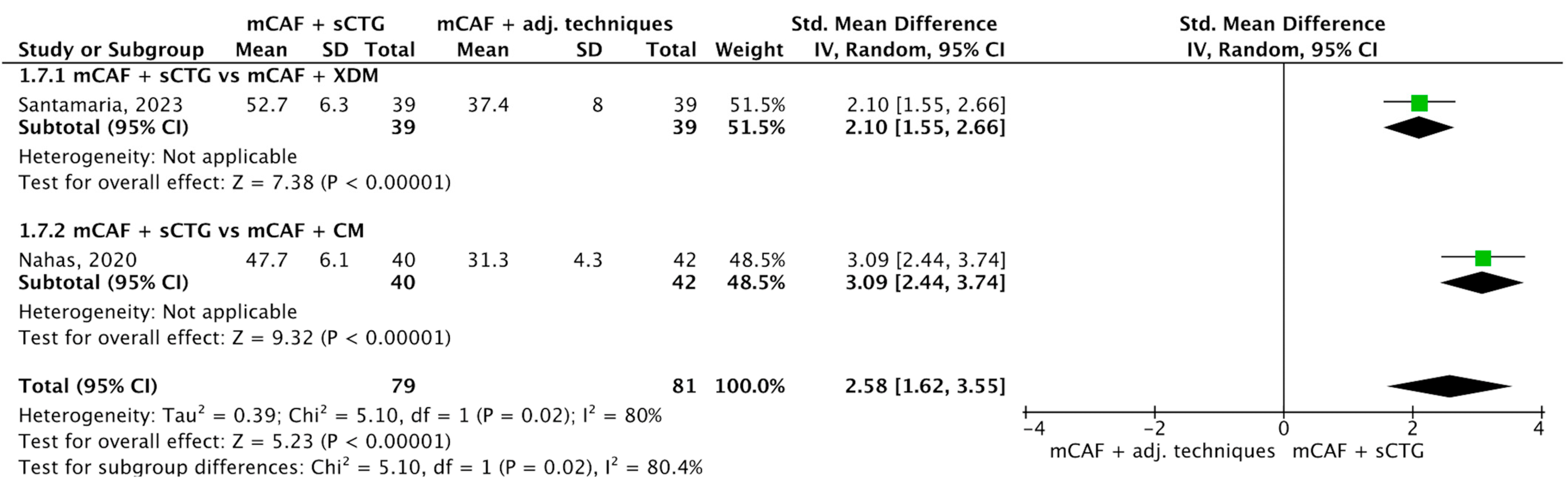
3.4.5. ∆KTW
Seven trials reported this outcome (Figure 8) [31,32,33,36,52,70,72]. I2 value was 99%, so the heterogeneity was considerable, thus a random effect model was applied. The difference between sCTG and its substitutes was statistically significant, with a p-value of 0.005 in favor of mCAF + sCTG.
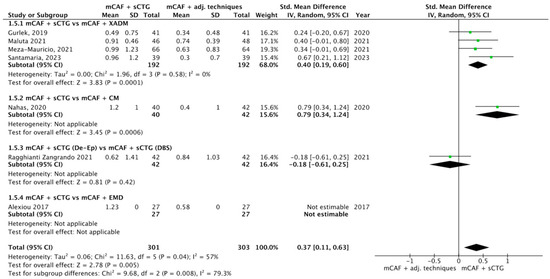
Figure 8.
Forest plot of comparison: mCAF + sCTG vs. mCAF adjunctive techniques, outcome: keratinized tissue width (KTW) gain (mm) ([31,32,33,36,52,70,72]).
The test for overall effect of subgroup mCAF + sCTG vs. mCAF + XADM showed a significant difference between groups (p = 0.0001) and the I2 value was 0%, indicating no observed heterogeneity among the studies.
A statistically significant difference was also observed in mCAF + sCTG vs. mCAF + CM comparison, but the test of heterogeneity was not applicable.
The other comparisons did not show any significant difference between groups.
The test for subgroup differences yielded a Chi2 value of 9.68 with 2 df (p = 0.008) and I2 = 79.3%. This indicates a statistically significant difference between subgroups, with substantial heterogeneity.
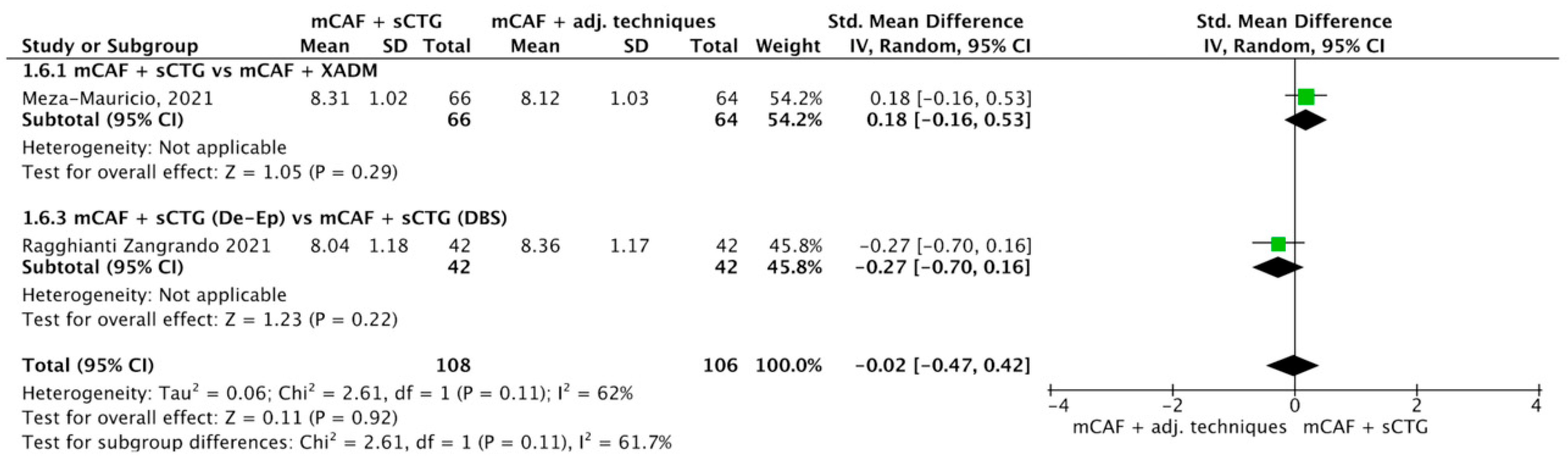
3.4.6. RES
Only two trials recorded this outcome (Figure 9) [32,72]: no statistically significant difference was registered between sCTG and adjunctive techniques.
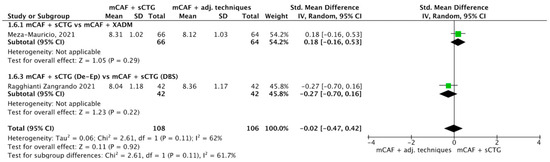
Figure 9.
Forest plot of comparison: mCAF + sCTG vs. mCAF adjunctive techniques, outcome: root esthetic score (RES) ([32,72]).
3.4.7. Duration of Surgery
Only two trials recorded the time of surgery (Figure 10) [31,36]: duration of surgery was statistically significant in favor of mCAF adjunctive techniques groups (p < 0.00001).
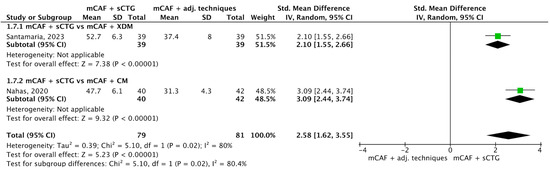
Figure 10.
Forest plot of comparison: mCAF + sCTG vs. mCAF adjunctive techniques, outcome: duration of surgery ([31,36]).
3.5. Certainty Assessement
The quality of evidence was assessed for RCTs comparing primary outcomes of mCAF + sCTG vs. mCAF adjunctive techniques (see Table 3).

Table 3.
Certainty assessment using GRADEpro GDT. Explanations: a The difference between the two groups was statistically significant; however, the test for heterogeneity was not calculated as only one study was included in this subgroup. Therefore, the effect of this intervention cannot be considered generalizable. b the test for heterogeneity was not calculated as only one study was included in this subgroup. Therefore, the effect of this intervention cannot be considered generalizable. c The standard deviation was not reported. d There was a considerable heterogeneity of total events.
4. Discussion
Coverage of multiple GRs is generally more challenging than treatment of single GRs due to the presence of a larger avascular recipient bed, variable root prominence and shallow vestibule, uneven recession depths, and limited residual keratinized tissue [75].
Compared to the traditional CAF approach, the use of additional grafting, flap technique modifications, or tunnel variation with CTG may improve clinical outcomes [18]. The surgical approach of Modified Coronally Advanced Flap (mCAF) combined with subepithelial connective tissue graft (sCTG) is considered the gold standard; however, assessing and comparing the predictability of alternative adjunctive techniques of mCAF for simultaneous root coverage is challenging due to procedural and material heterogeneity [26]. The use of mCAF + sCTG has shown long-term clinical improvement of recession depth, increasing KT and CAL, besides the morbidity of procedure and the issue concerning graft availability [23].
In this proposal, another meta-analysis already analyzed the additional use of CTG and CM to mCAF: Bathia et al. [26] reported that combining mCAF with either CTG or Collagen Matrix (CM) significantly improved CRC and recession reduction compared to mCAF alone. A more recent systematic review [76] directly compared CAF + CM vs. CAF + CTG and reported a statistically significant difference in favor of sCTG, with superior outcomes in terms of recession reduction (p = 0.02) and KTW gain (p = 0.03). However, palatal harvesting causes severe discomfort in the palatal area in patients undergoing harvesting [77]; after CTG, patients usually present a small percentage of postoperative complications, such as dentin hypersensitivity, bleeding, edema, pain, and delayed wound healing. Moreover, postoperative pain is a negative experience that causes difficulty in swallowing and negatively influences patient compliance and confidence in treatment [78].
To avoid those complications, it is essential to investigate and evaluate evidence for alternative approaches. Based on recent literature on the association of mCAF with promising biomaterials or other substitutes/approaches, such as EMD [79], this review was conducted to compare the efficacy of different adjunctive techniques, focusing on the treatment of multiple adjacent GR-type defects in terms of root coverage (RC), esthetic outcomes, and keratinized tissue (KT) augmentation. The selection of specific outcomes for a subsequent metanalysis was necessary for a proper comparison, due to the presence of substitutes of different origins, different techniques, and heterogeneous follow-ups.
Only RCTs with a minimum follow-up of 6 months were included, as this duration is considered sufficient for tissues healing after surgery. Studies with longer follow-ups, up to one year, were also considered to account for complete healing [23]. Several biomaterials investigated in this study were superimposable to others analyzed in different systematic reviews [23]: among the included studies, nine evaluating mCAF + sCTG vs. mCAF + other associations (CM, XADM, PRF, EMD, sCTG harvested double blade scalpel) were included in the meta-analysis, with mCAF + sCTG as control group.
Regarding RC, most of the studies (14 out of 17) reported the evaluation of CRC, which was usually considered in other systematic reviews [21,61] as a primary outcome, in terms of both clinical stability and esthetics. CRC was described with early and long-term follow-ups (between 6 months and 5 years) as between 43% and 93% in the case of traditional approaches of mCAF (mCAF alone or with CTG) [27,31,32,33,35,36,38,44,52,68,70,71,72,73,74]; between 50% and 82% in the case of use of substitutes [31,32,33,35,36,38,44,52,71,72,73]. Nevertheless, results for techniques alternative to sCTG are not available with follow-ups longer than 1,5 years: this issue can be underlined as critical for a proper comparison between different approaches, as longer outcomes, even up to 5 years, are declared as stable only with traditional approaches (percentages of CRC around 90%) [74].
Another parameter frequently considered for RC [22] was percentage of MRC, reported in almost all studies: only a few studies [52,70,71], whose approach was the association to mCAF of OB application, XADM, and EMD, revealed percentage of MRC comparable to those of mCAF alone or mCAF + sCTG, but more evidence of these techniques is needed. Similarly to CRC, MRC values of alternative techniques were comparable to traditional approaches of mCAF only in short-term follow-ups, with outcomes up to 95,28% in case of use of sCTG between 6 and 18 months [70]. On the other hand, in long-term follow-ups, it is not possible to compare them with CTG, which remains stable at 91% after 5 years [74]. It can be thus assumed that CRC and MRC well point out the rate of reduction in the initial recession, showing that use of new biomaterials can lead to promising clinical outcomes, despite sCTG still remaining the gold standard in long-term assessment.
Cairo et al. [80] examined esthetic- and patient-related outcomes, finding that CTG procedures showed highest overall esthetic performance for root coverage, although graft integration might impair soft tissue color and appearance. Additionally, CTG-based techniques were also correlated with greater patient satisfaction and morbidity. In this SR, the esthetic performance was evaluated measuring the RES parameter, which provides an objective attempt both for patients and clinicians to categorize esthetic assessment [55], finding a higher RES specifically in the case of using orthodontic buttons [44,71]. However, a high level of evidence showed no statistically significant difference in RES between sCTG and adjunctive techniques.
The ∆GT parameter [31,32,68,72,73], evaluated in only five studies, presented heterogeneous values for all techniques analyzed. Better indicative of a clear tendency, the evaluation of ∆KTW was reported in almost half of studies (10 out of 17) [26,27,28,31,33,58,60,61,62,63], with similar values in terms of CTG (between 0.62 and 1.8 mm) compared to other approaches (between 0.3 and 2.13 mm) considering earlier follow-ups, with no results at longer follow-up.
Regarding comparison between mCAF + sCTG and mCAF + PRF, MRC was found in favor of the control group (p = 0.01; SMD = −0.67, 95% CI [0.14, 1.20]). Outcomes regarding PRF still represent a controversial issue, as PRF influences the healing process of both soft and hard tissues, releasing, in time, platelets, growth factors, and cytokines [81]. Despite methods of its production not being standardized, PRF does not require anticoagulants, thrombin, or any other gelling agent, making it easily usable [82]. In this regard, PRF was initially employed in implant surgery to improve bone healing, alveolar ridge preservation, 1- and 2-stage sinus floor elevation, horizontal and vertical bone regeneration, periodontal defects regeneration, third molar extractions, and later used also in plastic periodontal surgery [35,50,69,83,84]. The comparison between the use of PRF membranes added to mCAF versus mCAF alone showed no significant benefits [38] in favor of PRF, except for increasing KT thickness.
Regarding comparison between mCAF + sCTG and mCAF + CM, only one trial reported this comparison [36]: CRC did not demonstrate a statistically significant difference (p = 0.05) between groups, while ∆KTW revealed a statistically significant difference (p = 0.0006) in favor of the control group (SMD = 0.79, 95% CI [0.34, 1.24]). In the comparison between mCAF + sCTG and mCAF + XADM the parameter CRC was evaluated in four RCTs [31,32,33,70], and a statistically significant difference (p = 0.002) was found in favor of the control group (OR = 2.08, 95% CI [1.30, 3.33]). Statistically significant differences again in favor of the control group were found also for MRC (three RCTs [31,32,70], p = 0.03) and ∆KTW (four RCTs [31,32,33,70] (p = 0.0001). The potential proliferation of fibroblasts may be due to the presence of important growth factors: different collagen matrices were employed to treat gingival recessions associated with dental wear, as autogenous or xenogeneic substitutes, e.g., porcine acellular dermal matrix [31], which consists of 3D sterilized pure collagen types I and III and elastin, a stable tissue matrix derived from porcine dermis without being posteriorly cross-linked artificially or put under any other chemical treatment [85]. In vitro and in vivo investigations showed an increase growth and proliferation of human gingival fibroblasts, osteoblasts, and endothelial cells, revealing a revascularization of the collagen structure during early healing. Furthermore, other authors suggested that it enhances migration, adhesion, and proliferation of periodontal ligament cells and human oral fibroblasts [86,87,88].
Finally, duration of surgery was significant shorter with mCAF adjunctive techniques (p < 0.00001): as described by other SR [89], it could represent a determining factor in reducing patient morbidity.
In light of these considerations, to ensure appropriate decision-making, the clinicians should consider patients’ anxiety, discomfort, preference, and esthetics, and discuss with them all the advantages and drawbacks of CTG and its substitutes.
Limitations of the Study
Considerable variability across the included RCTs is acknowledged, as studies with a split-mouth design introduce a distortion: one intervention’s effect could contaminate the other side of the mouth, making it difficult to estimate the true effect of each treatment. Furthermore, there is an evident heterogeneity of follow-ups (from a minimum of 6 months to 5 years).
Regarding the heterogeneity of interventions included in this SR, only one RCT [74] showed stable long-term results of CTG in terms of RC, plus the association of sCTG to mCAF also reached better results in the long-term for KTW augmentation. On the other side, a lack of evidence in the long-term emerged regarding the alternative approaches of mCAF for RES, MRC, KTW gain, and GT gain. A low level of evidence suggested that mCAF + EMD and mCAF+ sCTG (DBS) may provide good results.
As the meta-analysis revealed these heterogeneous outcomes, study limitations derive from discrepancy in follow-ups between comparisons, not homogeneous distribution of techniques analyzed, and different study design performed, with unclear blinding of participants or examiners in few cases.
Furthermore, regarding studies on the association with PRF, the investigation by Culhaoglu et al. [59] dealt with the PRF technique employed in two different modalities, two or four layers, respectively. In this case, by the union of the two groups, a single mean and standard deviation were considered to avoid potential bias for data duplication.
Future perspectives in the study search could focus on targeted reviews based on comparable techniques in terms of follow-ups of at least 3 years and similar study design.
5. Conclusions
Based on the findings of this SR and meta-analysis, the combination of the mCAF with a sCTG remains the most effective and evidence-supported approach for the treatment of multiple adjacent gingival recessions, ensuring superior and stable long-term outcomes for RC, RES, and KT gain.
The mCAF combined with biomaterials or adjunctive techniques (such as XADM, PRF, orthodontic button, or EMD) demonstrated promising short-term results in clinical outcomes; however, the lack of long-term data and the high heterogeneity among studies prevent drawing definitive conclusions on their clinical predictability. Despite this, some mCAF adjunctive techniques can be associated with a significant reduction in duration of surgical procedures, which may contribute to decrease patient morbidity and thus improve procedural efficiency. In terms of esthetic outcomes (RES), alternative mCAF approaches also showed favorable results, as no statistically significant differences were found when compared with the use of sCTG.
Further RCTs with a parallel-groups design and a follow-up of more than 5 years are needed to reliably assess the clinical effectiveness and predictability of these alternatives compared to the established use of sCTG.
Author Contributions
Conceptualization, G.L.; methodology, M.G., A.S., A.P.; software, M.G., A.S., A.P.; validation, D.A.M., A.Z., P.F., G.C.; formal analysis, M.G., A.S., A.P.; investigation, D.A.M., A.Z., P.F., G.C.; resources, D.A.M., A.Z., P.F., G.C.; data curation, M.G., A.S., G.L.; writing—original draft preparation, M.G., A.S., G.L. writing—review and editing, M.G., A.S., A.P., D.A.M., A.Z., P.F., G.C.; visualization, G.L.; supervision, G.L.; project administration, G.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data are available from the corresponding author upon reasonable request.
Acknowledgments
Authors would like to thank the independent statistician Luisa Zanolla (University of Verona, Verona, Italy), who reviewed the work for statistical analysis.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| ADM | Acellular Dermal Matrix |
| CAF | Coronally Advanced Flap |
| CAT | Coronally Advanced Tunnel |
| CI | Confidence Interval |
| CM | Collagen Matrix |
| CRC | Complete Root Coverage |
| CTG | Connective Tissue Graft |
| DBS | Double Blade Scalpel |
| df | Degree of Freedom |
| EMD | Enamel Matrix Derivatives |
| GR | Gingival Recession |
| GRADEpro | GDT Guideline Development Tool |
| GT | Gingival Thickness |
| HA | Hyaluronic Acid |
| I2 | Index of Higgings |
| KT | Keratinized Tissue |
| KTW | Keratinized Tissue Width |
| MAGRs | Multiple Adjacent Gingival Recessions |
| MCAF | Modified Coronally Advanced Flap |
| MRC | Mean Root Coverage |
| NCCLs | Non-Carious Cervial Lesions |
| OB | Orthodontic Button |
| OR | Odds Ratio |
| PICOS | Population, Intervention, Comparison, Outcomes, and Study Design |
| PRF | Platelet-Rich Fibrin |
| RC | Root Coverage |
| RCPPS | Root Coverage Periodontal Plastic Surgery |
| RCSPs | Root Coverage Surgical Procedures |
| RCTs | Randomized Clinical Trials |
| RDR | Recession Depth Reduction |
| RES | Root Coverage Esthetic Score |
| Robvis tool | Risk of Bias Visualization Tool |
| RoB2 | Risk of Bias 2 |
| RR | Risk Ratio |
| RT | Recession Type |
| sCTG | Subepithelial Connective Tissue Graft |
| SMD | Standardized Mean Difference |
| SRs | Systematic Reviews |
| VAS | Visual Analogue Scale |
| T-PRF | Titanium Platelet-Rich Fibrin |
| XADM | Xenogeneic Acellular Dermal Matrix |
References
- Camargo, P.M.; Melnick, P.R.; Kenney, E.B. The use of free gingival grafts for aesthetic purposes. Periodontol. 2000 2001, 27, 72–96. [Google Scholar] [CrossRef]
- Wennström, J.L. Mucogingival therapy. Ann. Periodontol. 1996, 1, 671–701. [Google Scholar] [CrossRef] [PubMed]
- Cairo, F.; Pagliaro, U.; Nieri, M. Treatment of gingival recession with coronally advanced flap procedures: A systematic review. J. Clin. Periodontol. 2008, 35, 136–162. [Google Scholar] [CrossRef] [PubMed]
- Nieri, M.; Pini Prato, G.P.; Giani, M.; Magnani, N.; Pagliaro, U.; Rotundo, R. Patient perceptions of buccal gingival recessions and requests for treatment. J. Clin. Periodontol. 2013, 40, 707–712. [Google Scholar] [CrossRef] [PubMed]
- Löe, H.; Anerud, A.; Boysen, H. The natural history of periodontal disease in man: Prevalence, severity, and extent of gingival recession. J. Periodontol. 1992, 63, 489–495. [Google Scholar] [CrossRef]
- Nocini, R.; Favaloro, E.J.; Sanchis-Gomar, F.; Lippi, G. Periodontitis, coronary heart disease and myocardial infarction: Treat one, benefit all. Blood Coagul. Fibrinolysis 2020, 31, 339–345. [Google Scholar] [CrossRef]
- Nocini, R.; Lippi, G.; Mattiuzzi, C. Periodontal disease: The portrait of an epidemic. J. Public Health Emerg. 2020, 4, 10. [Google Scholar] [CrossRef]
- Prato, G.P.; Rotundo, R.; Magnani, C.; Ficarra, G. Viral etiology of gingival recession. A case report. J. Periodontol. 2002, 73, 110–114. [Google Scholar] [CrossRef]
- Smukler, H.; Landsberg, J. The toothbrush and gingival traumatic injury. J. Periodontol. 1984, 55, 713–719. [Google Scholar] [CrossRef]
- Toker, H.; Ozdemir, H. Gingival recession: Epidemiology and risk indicators in a university dental hospital in Turkey. Int. J. Dent. Hyg. 2009, 7, 115–120. [Google Scholar] [CrossRef]
- Olsson, M.; Lindhe, J. Periodontal characteristics in individuals with varying form of the upper central incisors. J. Clin. Periodontol. 1991, 18, 78–82. [Google Scholar] [CrossRef]
- Stoner, J.E.; Mazdyasna, S. Gingival recession in the lower incisor region of 15-year-old subjects. J. Periodontol. 1980, 51, 74–76. [Google Scholar] [CrossRef]
- Ericsson, I.; Lindhe, J. Recession in sites with inadequate width of the keratinized gingiva. An experimental study in the dog. J. Clin. Periodontol. 1984, 11, 95–103. [Google Scholar] [CrossRef] [PubMed]
- Parma-Benfenali, S.; Fugazzoto, P.A.; Ruben, M.P. The effect of restorative margins on the postsurgical development and nature of the periodontium. Part I. Int. J. Periodontics Restor. Dent. 1985, 5, 30–51. [Google Scholar]
- Wennström, J.L.; Lindhe, J.; Sinclair, F.; Thilander, B. Some periodontal tissue reactions to orthodontic tooth movement in monkeys. J. Clin. Periodontol. 1987, 14, 121–129. [Google Scholar] [CrossRef] [PubMed]
- Yared, K.F.; Zenobio, E.G.; Pacheco, W. Periodontal status of mandibular central incisors after orthodontic proclination in adults. Am. J. Orthod. Dentofac. Orthop. 2006, 130, 6.e1–6.e8. [Google Scholar] [CrossRef]
- Chambrone, L.; Chambrone, L.A. Gingival recessions caused by lip piercing: Case report. J. Can. Dent. Assoc. 2003, 69, 505–508. [Google Scholar]
- Graziani, F.; Gennai, S.; Roldán, S.; Discepoli, N.; Buti, J.; Madianos, P.; Herrera, D. Efficacy of periodontal plastic procedures in the treatment of multiple gingival recessions. J. Clin. Periodontol. 2014, 41 (Suppl. 15), S63–S76. [Google Scholar] [CrossRef]
- Cairo, F.; Nieri, M.; Pagliaro, U. Efficacy of periodontal plastic surgery procedures in the treatment of localized facial gingival recessions. A systematic review. J. Clin. Periodontol. 2014, 41 (Suppl. 15), S44–S62. [Google Scholar] [CrossRef]
- Chambrone, L.; Barootchi, S.; Avila-Ortiz, G. Efficacy of biologics in root coverage and gingival augmentation therapy: An American Academy of Periodontology best evidence systematic review and network meta-analysis. J. Periodontol. 2022, 93, 1771–1802. [Google Scholar] [CrossRef]
- Tavelli, L.; Barootchi, S.; Nguyen, T.V.N.; Tattan, M.; Ravidà, A.; Wang, H.L. Efficacy of tunnel technique in the treatment of localized and multiple gingival recessions: A systematic review and meta-analysis. J. Periodontol. 2018, 89, 1075–1090. [Google Scholar] [CrossRef]
- Toledano-Osorio, M.; Muñoz-Soto, E.; Toledano, M.; Vallecillo-Rivas, M.; Vallecillo, C.; Ramos-García, P.; Osorio, R. Treating Gingival Recessions Using Coronally Advanced Flap or Tunnel Techniques with Autografts or Polymeric Substitutes: A Systematic Review and Meta-Analysis. Polymers 2022, 14, 1453. [Google Scholar] [CrossRef]
- Moraschini, V.; Calasans-Maia, M.D.; Dias, A.T.; de Carvalho Formiga, M.; Sartoretto, S.C.; Sculean, A.; Shibli, J.A. Effectiveness of connective tissue graft substitutes for the treatment of gingival recessions compared with coronally advanced flap: A network meta-analysis. Clin. Oral Investig. 2020, 24, 3395–3406. [Google Scholar] [CrossRef]
- Chambrone, L.; Botelho, J.; Machado, V.; Mascarenhas, P.; Mendes, J.J.; Avila-Ortiz, G. Does the subepithelial connective tissue graft in conjunction with a coronally advanced flap remain as the gold standard therapy for the treatment of single gingival recession defects? A systematic review and network meta-analysis. J. Periodontol. 2022, 93, 1336–1352. [Google Scholar] [CrossRef]
- Tavelli, L.; Barootchi, S.; Cairo, F.; Rasperini, G.; Shedden, K.; Wang, H.L. The Effect of Time on Root Coverage Outcomes: A Network Meta-analysis. J. Dent. Res. 2019, 98, 1195–1203. [Google Scholar] [CrossRef]
- Bhatia, A.; Yadav, V.S.; Tewari, N.; Kumar, A.; Sharma, R.K. Efficacy of modified coronally advanced flap in the treatment of multiple adjacent gingival recessions: A systematic review and meta-analysis. Acta Odontol. Scand. 2021, 79, 562–572. [Google Scholar] [CrossRef] [PubMed]
- Zucchelli, G.; De Sanctis, M. Treatment of multiple recession-type defects in patients with esthetic demands. J. Periodontol. 2000, 71, 1506–1514. [Google Scholar] [CrossRef] [PubMed]
- Zucchelli, G.; Amore, C.; Sforza, N.M.; Montebugnoli, L.; De Sanctis, M. Bilaminar techniques for the treatment of recession-type defects. A comparative clinical study. J. Clin. Periodontol. 2003, 30, 862–870. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, P.F.; da Silva, R.C.; Cury, P.R.; Joly, J.C. Modified coronally advanced flap associated with a subepithelial connective tissue graft for the treatment of adjacent multiple gingival recessions. J. Periodontol. 2006, 77, 1901–1906. [Google Scholar] [CrossRef]
- Ahmedbeyli, C.; Dirikan Ipçi, S.; Cakar, G.; Yılmaz, S.; Chambrone, L. Coronally advanced flap and envelope type of flap plus acellular dermal matrix graft for the treatment of thin phenotype multiple recession defects. A randomized clinical trial. J. Clin. Periodontol. 2019, 46, 1024–1029. [Google Scholar] [CrossRef]
- Santamaria, M.P.; Rossato, A.; Fernanda Ferreira Ferraz, L.; Maria Viana Miguel, M.; Venturoso Simões, B.; Pereira Nunes, M.; Bresciani, E.; de Sanctis, M.; Mathias-Santamaria, I.F. Multiple gingival recessions associated with non-carious cervical lesions treated by partial restoration and modified coronally advanced flap with either connective tissue graft or xenogeneic acellular dermal matrix: A randomized clinical trial. J. Periodontol. 2023, 94, 731–741. [Google Scholar] [CrossRef]
- Meza-Mauricio, J.; Cortez-Gianezzi, J.; Duarte, P.M.; Tavelli, L.; Rasperini, G.; de Faveri, M. Comparison between a xenogeneic dermal matrix and connective tissue graft for the treatment of multiple adjacent gingival recessions: A randomized controlled clinical trial. Clin. Oral Investig. 2021, 25, 6919–6929. [Google Scholar] [CrossRef]
- Gürlek, Ö.; Gümüş, P.; Nizam, N.; Buduneli, N. Coronally advanced flap with connective tissue graft or xenogeneic acellular dermal matrix in the treatment of multiple gingival recessions: A split-mouth randomized clinical trial. J. Esthet. Restor. Dent. 2020, 32, 380–388. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, K.T.; de Jesus Hernandez Martinez, C.; Suemi, M.I.; Palioto, D.B.; Messora, M.R.; de Souza, S.L.S.; Novaes, A.B.; Chaves Furlaneto, F.A.; Taba, M. Root coverage using coronally advanced flap with porcine-derived acellular dermal matrix or subepithelial connective tissue graft: A randomized controlled clinical trial. Clin. Oral Investig. 2020, 24, 4077–4087. [Google Scholar] [CrossRef] [PubMed]
- Öncü, E. The Use of Platelet-Rich Fibrin Versus Subepithelial Connective Tissue Graft in Treatment of Multiple Gingival Recessions: A Randomized Clinical Trial. Int. J. Periodontics Restor. Dent. 2017, 37, 265–271. [Google Scholar] [CrossRef] [PubMed]
- Nahas, R.; Gondim, V.; Carvalho, C.V.; Calderero, L.M.; Rosa, E.F.; Sakiyama, T.; César Neto, J.B.; Pannuti, C.M.; Romito, G.A. Treatment of multiple recessions with collagen matrix versus connective tissue: A randomized clinical trial. Braz. Oral Res. 2020, 33, e123. [Google Scholar] [CrossRef]
- De Santis, D.; Luciano, U.; Pancera, P.; Castegnaro, G.; Alberti, C.; Gelpi, F. A New Matrix for Soft Tissue Management. J. Clin. Med. 2022, 11, 4486. [Google Scholar] [CrossRef]
- Aroca, S.; Keglevich, T.; Barbieri, B.; Gera, I.; Etienne, D. Clinical evaluation of a modified coronally advanced flap alone or in combination with a platelet-rich fibrin membrane for the treatment of adjacent multiple gingival recessions: A 6-month study. J. Periodontol. 2009, 80, 244–252. [Google Scholar] [CrossRef]
- George, S.G.; Kanakamedala, A.K.; Mahendra, J.; Kareem, N.; Mahendra, L.; Jerry, J.J. Treatment of gingival recession using a coronally-advanced flap procedure with or without placental membrane. J. Investig. Clin. Dent. 2018, 9, e12340. [Google Scholar] [CrossRef]
- Rojas, M.A.; Marini, L.; Sahrmann, P.; Pilloni, A. Hyaluronic Acid as an Adjunct to Coronally Advanced Flap Procedures for Gingival Recessions: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. J. Pers. Med. 2022, 12, 1593. [Google Scholar] [CrossRef]
- Pilloni, A.; Schmidlin, P.R.; Sahrmann, P.; Sculean, A.; Rojas, M.A. Effectiveness of adjunctive hyaluronic acid application in coronally advanced flap in Miller class I single gingival recession sites: A randomized controlled clinical trial. Clin. Oral Investig. 2019, 23, 1133–1141. [Google Scholar] [CrossRef] [PubMed]
- Pardo, A.; Magnani, V.; Montagna, P.; Ala, A.; Brancato, G.; Melloni, F.; Lombardo, G.; De Santis, D. Clinical, Microbiological, and Biochemical Outcomes of Hyaluronic Acid in Non-Surgical Periodontal Therapy: A Systematic Review and Meta-Analysis. Appl. Sci. 2025, 15, 5975. [Google Scholar] [CrossRef]
- Rajendran, V.; Uppoor, A.; Kadakampally, D.; Mannava, Y. Comparison of minimally invasive coronally advanced flap and modified coronally advanced flap for the management of multiple adjacent gingival recession defects: A split mouth randomized control trial. J. Esthet. Restor. Dent. 2018, 30, 509–515. [Google Scholar] [CrossRef] [PubMed]
- Khobragade, S.; Kolte, A.; Kolte, R.; Shrirao, T.; Potey, A. Modified coronally advanced flap with and without orthodontic button application in management of multiple proximate gingival recession defects: A randomized clinical trial. Contemp. Clin. Dent. 2016, 7, 544–549. [Google Scholar] [CrossRef] [PubMed]
- Savithri, N.K.; Subramanian, S.; Prakash, P.S.G.; Appukuttan, D. Effect of microsurgical technique for root coverage using modified coronally advanced flap with connective tissue graft- Randomized controlled clinical trial. Dent. Res. J. 2022, 19, 87. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Group, P. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. J. Clin. Epidemiol. 2009, 62, 1006–1012. [Google Scholar] [CrossRef]
- Hoogendam, A.; de Vries Robbé, P.F.; Overbeke, A.J. Comparing patient characteristics, type of intervention, control, and outcome (PICO) queries with unguided searching: A randomized controlled crossover trial. J. Med. Libr. Assoc. 2012, 100, 121–126. [Google Scholar] [CrossRef]
- Miller, P.D. A classification of marginal tissue recession. Int. J. Periodontics Restor. Dent. 1985, 5, 8–13. [Google Scholar]
- Cairo, F.; Nieri, M.; Cincinelli, S.; Mervelt, J.; Pagliaro, U. The interproximal clinical attachment level to classify gingival recessions and predict root coverage outcomes: An explorative and reliability study. J. Clin. Periodontol. 2011, 38, 661–666. [Google Scholar] [CrossRef]
- Özkan Şen, D.; Öncü, E. Splith mouth randomized control trial comparison of T-PRF and subepithelial connective tissue graft in the treatment of maxillar multiple gingival recessions. J. Esthet. Restor. Dent. 2023, 35, 449–456. [Google Scholar] [CrossRef]
- Rokn, A.; Zare, H.; Haddadi, P. Use of Mucograft Collagen Matrix. Front. Dent. 2020, 17, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Alexiou, A.; Vouros, I.; Menexes, G.; Konstantinidis, A. Comparison of enamel matrix derivative (Emdogain) and subepithelial connective tissue graft for root coverage in patients with multiple gingival recession defects: A randomized controlled clinical study. Quintessence Int. 2017, 48, 381–389. [Google Scholar] [CrossRef]
- Fernández-Jiménez, A.; García-De-La-Fuente, A.M.; Estefanía-Fresco, R.; Marichalar-Mendia, X.; Aguirre-Urizar, J.M.; Aguirre-Zorzano, L.A. Complete root coverage in the treatment of Miller class III or RT2 gingival recessions: A systematic review and meta-analysis. BMC Oral Health 2021, 21, 145. [Google Scholar] [CrossRef]
- Pini-Prato, G.; Magnani, C.; Zaheer, F.; Buti, J.; Rotundo, R. Critical Evaluation of Complete Root Coverage as a Successful Endpoint of Treatment for Gingival Recessions. Int. J. Periodontics Restor. Dent. 2015, 35, 655–663. [Google Scholar] [CrossRef]
- Cairo, F.; Rotundo, R.; Miller, P.D.; Pini Prato, G.P. Root coverage esthetic score: A system to evaluate the esthetic outcome of the treatment of gingival recession through evaluation of clinical cases. J. Periodontol. 2009, 80, 705–710. [Google Scholar] [CrossRef]
- Sørdahl, A.J.; Verket, A. Patient and professional use of the root coverage esthetic score (RES) and how it relates to patient satisfaction following periodontal plastic surgery. BMC Oral Health 2022, 22, 295. [Google Scholar] [CrossRef]
- Isaia, F.; Gyurko, R.; Roomian, T.C.; Hawley, C.E. The root coverage esthetic score: Intra-examiner reliability among dental students and dental faculty. J. Periodontol. 2018, 89, 833–839. [Google Scholar] [CrossRef]
- Akcan, S.K.; Ünsal, B. Gingival recession treatment with concentrated growth factor membrane: A comparative clinical trial. J. Appl. Oral Sci. 2020, 28, e20190236. [Google Scholar] [CrossRef]
- Cardaropoli, D.; Tamagnone, L.; Roffredo, A.; Gaveglio, L. Treatment of gingival recession defects using coronally advanced flap with a porcine collagen matrix compared to coronally advanced flap with connective tissue graft: A randomized controlled clinical trial. J. Periodontol. 2012, 83, 321–328. [Google Scholar] [CrossRef]
- Malhotra, S.; Tewari, S.; Sharma, R.; Sharma, R.K.; Tanwar, N.; Arora, R. Clinical evaluation of root coverage in Miller class III/RT2 labial gingival recession treated with interdisciplinary periodontal-orthodontic therapy: A randomized controlled clinical trial. J. Periodontal Implant. Sci. 2024, 54, 265–279. [Google Scholar] [CrossRef]
- Chambrone, L.; Salinas Ortega, M.A.; Sukekava, F.; Rotundo, R.; Kalemaj, Z.; Buti, J.; Pini Prato, G.P. Root coverage procedures for treating localised and multiple recession-type defects. Cochrane Database Syst. Rev. 2018, 10, CD007161. [Google Scholar] [CrossRef]
- Tatakis, D.N.; Trombelli, L. Gingival recession treatment: Guided tissue regeneration with bioabsorbable membrane versus connective tissue graft. J. Periodontol. 2000, 71, 299–307. [Google Scholar] [CrossRef]
- Chapter 8: Assessing Risk of Bias in a Randomized Trial. Available online: https://www.cochrane.org/authors/handbooks-and-manuals/handbook/current/chapter-08 (accessed on 1 July 2025).
- McGuinness, L.A.; Higgins, J.P.T. Risk-of-bias VISualization (robvis): An R package and Shiny web app for visualizing risk-of-bias assessments. Res. Synth. Methods 2021, 12, 55–61. [Google Scholar] [CrossRef]
- RevMan Web. The Cochrane Collaboration. 2023. Available online: https://revman.cochrane.org (accessed on 1 July 2025).
- Richardson, M.; Garner, P.; Donegan, S. Interpretation of subgroup analyses in systematic reviews: A tutorial. Clin. Epidemiol. Glob. Health 2019, 7, 192–198. [Google Scholar] [CrossRef]
- McMaster University and Evidence Prime, GRADEpro GDT: GRADEpro Guideline Development Tool. 2023. Available online: https://gradepro.org (accessed on 1 July 2025).
- Cairo, F.; Cortellini, P.; Pilloni, A.; Nieri, M.; Cincinelli, S.; Amunni, F.; Pagavino, G.; Tonetti, M.S. Clinical efficacy of coronally advanced flap with or without connective tissue graft for the treatment of multiple adjacent gingival recessions in the aesthetic area: A randomized controlled clinical trial. J. Clin. Periodontol. 2016, 43, 849–856. [Google Scholar] [CrossRef]
- Culhaoglu, R.; Taner, L.; Guler, B. Evaluation of the effect of dose-dependent platelet-rich fibrin membrane on treatment of gingival recession: A randomized, controlled clinical trial. J. Appl. Oral Sci. 2018, 26, e20170278. [Google Scholar] [CrossRef]
- Maluta, R.; Monteiro, M.F.; Peruzzo, D.C.; Joly, J.C. Root coverage of multiple gingival recessions treated with coronally advanced flap associated with xenogeneic acellular dermal matrix or connective tissue graft: A 6-month split-mouth controlled and randomized clinical trial. Clin. Oral Investig. 2021, 25, 5765–5773. [Google Scholar] [CrossRef]
- Ozcelik, O.; Haytac, M.C.; Seydaoglu, G. Treatment of multiple gingival recessions using a coronally advanced flap procedure combined with button application. J. Clin. Periodontol. 2011, 38, 572–580. [Google Scholar] [CrossRef]
- Zangrando, M.S.R.; Eustachio, R.R.; de Rezende, M.L.R.; Sant’ana, A.C.P.; Damante, C.A.; Greghi, S.L.A. Clinical and patient-centered outcomes using two types of subepithelial connective tissue grafts: A split-mouth randomized clinical trial. J. Periodontol. 2021, 92, 814–822. [Google Scholar] [CrossRef]
- Rotundo, R.; Genzano, L.; Patel, D.; D’Aiuto, F.; Nieri, M. Adjunctive benefit of a xenogenic collagen matrix associated with coronally advanced flap for the treatment of multiple gingival recessions: A superiority, assessor-blind, randomized clinical trial. J. Clin. Periodontol. 2019, 46, 1013–1023. [Google Scholar] [CrossRef]
- Zucchelli, G.; Mounssif, I.; Mazzotti, C.; Stefanini, M.; Marzadori, M.; Petracci, E.; Montebugnoli, L. Coronally advanced flap with and without connective tissue graft for the treatment of multiple gingival recessions: A comparative short- and long-term controlled randomized clinical trial. J. Clin. Periodontol. 2014, 41, 396–403. [Google Scholar] [CrossRef]
- Hofmänner, P.; Alessandri, R.; Laugisch, O.; Aroca, S.; Salvi, G.E.; Stavropoulos, A.; Sculean, A. Predictability of surgical techniques used for coverage of multiple adjacent gingival recessions--A systematic review. Quintessence Int. 2012, 43, 545–554. [Google Scholar]
- Zangani, A.; Gualtieri, M.; Pardo, A.; Signoriello, A.; Faccioni, P.; Colapinto, G.; Goker, F.; Lombardo, G.; Del Fabbro, M.; Albanese, M. Collagen Matrix Versus Subepithelial Connective Tissue for Recession Coverage: A Systematic Review. Oral Dis. 2024, 31, 1092–1106. [Google Scholar] [CrossRef]
- Zucchelli, G.; Mounssif, I.; Mazzotti, C.; Montebugnoli, L.; Sangiorgi, M.; Mele, M.; Stefanini, M. Does the dimension of the graft influence patient morbidity and root coverage outcomes? A randomized controlled clinical trial. J. Clin. Periodontol. 2014, 41, 708–716. [Google Scholar] [CrossRef]
- D’Ambrosio, F.; Caggiano, M.; Chiacchio, A.; Acerra, A.; Giordano, F. Palatal Graft Harvesting Site Healing and Pain Management: What Is the Best Choice? An Umbrella Review. Appl. Sci. 2024, 14, 5614. [Google Scholar] [CrossRef]
- Xiang, C.; Zhang, L.; Tao, E. Research progress of enamel matrix derivative on periodontal tissue regeneration: A narrative review. Front. Dent. Med. 2025, 6, 1611402. [Google Scholar] [CrossRef]
- Cairo, F.; Barootchi, S.; Tavelli, L.; Barbato, L.; Wang, H.L.; Rasperini, G.; Graziani, F.; Tonetti, M. Aesthetic-And patient-related outcomes following root coverage procedures: A systematic review and network meta-analysis. J. Clin. Periodontol. 2020, 47, 1403–1415. [Google Scholar] [CrossRef]
- Hajibagheri, P.; Basirat, M.; Tabari-Khomeiran, Z.; Asadi-Aria, A. The efficacy of platelet-rich fibrin (PRF) in post-extraction hard and soft tissue healing and associated complications: A systematic review and meta-analysis of split-mouth randomized clinical trials. BMC Oral Health 2025, 25, 869. [Google Scholar] [CrossRef]
- Baeyens, W.; Glineur, R.; Evrard, L. [The use of platelet concentrates: Platelet-rich plasma (PRP) and platelet-rich fibrin (PRF) in bone reconstruction prior to dental implant surgery]. Rev. Med. Brux. 2010, 31, 521–527. [Google Scholar]
- Valenzuela-Mencia, J.; Manzano-Moreno, F.J. Applications of Platelet-Rich Fibrin (PRF) Membranes Alone or in Combination with Biomimetic Materials in Oral Regeneration: A Narrative Review. Biomimetics 2025, 10, 172. [Google Scholar] [CrossRef]
- Yang, H.; Yu, J.; Wu, D. Platelet-rich fibrin application after mandibular third molar extraction: An umbrella review. Clin. Oral Investig. 2024, 29, 34. [Google Scholar] [CrossRef] [PubMed]
- Dadlani, S. Porcine Acellular Dermal Matrix: An Alternative to Connective Tissue Graft-A Narrative Review. Int. J. Dent. 2021, 2021, 1652032. [Google Scholar] [CrossRef]
- Pabst, A.M.; Happe, A.; Callaway, A.; Ziebart, T.; Stratul, S.I.; Ackermann, M.; Konerding, M.A.; Willershausen, B.; Kasaj, A. In vitro and in vivo characterization of porcine acellular dermal matrix for gingival augmentation procedures. J. Periodontal Res. 2014, 49, 371–381. [Google Scholar] [CrossRef] [PubMed]
- Pabst, A.M.; Lehmann, K.M.; Walter, C.; Krüger, M.; Stratul, S.I.; Kasaj, A. Influence of porcine-derived collagen matrix on endothelial progenitor cells: An in vitro study. Odontology 2016, 104, 19–26. [Google Scholar] [CrossRef]
- Papi, P.; Pompa, G. The Use of a Novel Porcine Derived Acellular Dermal Matrix (Mucoderm) in Peri-Implant Soft Tissue Augmentation: Preliminary Results of a Prospective Pilot Cohort Study. Biomed. Res. Int. 2018, 2018, 6406051. [Google Scholar] [CrossRef]
- Rotundo, R.; Pancrazi, G.L.; Grassi, A.; Ceresoli, L.; Di Domenico, G.L.; Bonafede, V. Soft Tissue Substitutes in Periodontal and Peri-Implant Soft Tissue Augmentation: A Systematic Review. Materials 2024, 17, 1221. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).