Influence of Ultrasonic Activation of Endodontic Irrigants on Microbial Reduction and Postoperative Pain: A Scoping Review of In Vivo Studies
Abstract
1. Introduction
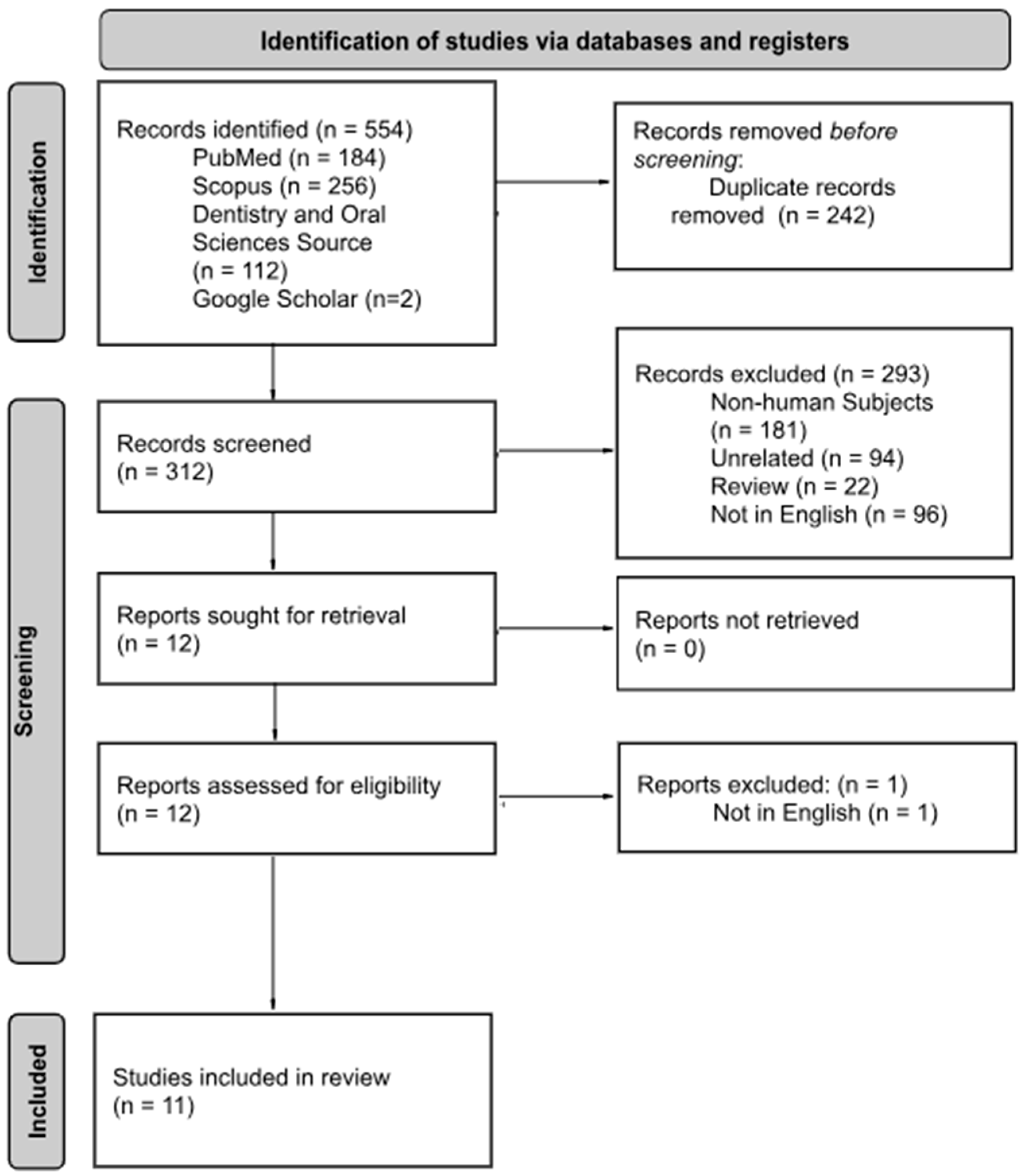
2. Methods
3. Results
4. Microbial Reduction
5. Post Operative Pain
6. Mechanisms Explaining Improved Outcomes
7. Discussion
7.1. Implications
7.2. Limitations and Strengths
7.3. Future Directions
8. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Goldberg, M. Root canal treatment (RCT): From traditional endodontic therapies to innovating pulp regeneration. J. Dent. Oral. Disord. Ther. 2016, 4, 1–6. [Google Scholar] [CrossRef]
- Chalub, L.O.; Nunes, G.P.; Strazzi-Sahyon, H.B.; Ferrisse, T.M.; dos Santos, P.H.; Gomes-Filho, J.E.; Cintra, L.T.A.; Sivieri-Araujo, G. Antimicrobial effectiveness of ultrasonic irrigation in root canal treatment: A systematic review of randomized clinical trials and meta-analysis. Clin. Oral Investig. 2023, 27, 1343–1361. [Google Scholar] [CrossRef]
- Mampilly, J.; Shetty, V.; Shetty, H. Endodontic irrigating solutions, disinfection devices and techniques: A review. IOSR J. Dent. Med. Sci. 2020, 19, 986–997. [Google Scholar] [CrossRef] [PubMed]
- Gomes, B.P.F.A.; Aveiro, E.; Kishen, A. Irrigants and irrigation activation systems in Endodontics. Braz. Dent. J. 2023, 34, 1–33. [Google Scholar] [CrossRef] [PubMed]
- Drews, D.J.; Nguyen, A.D.; Diederich, A.; Gernhardt, C.R. The Interaction of Two Widely Used Endodontic Irrigants, Chlorhexidine and Sodium Hypochlorite, and Its Impact on the Disinfection Protocol during Root Canal Treatment. Antibiotics 2023, 12, 589. [Google Scholar] [CrossRef] [PubMed]
- Khoury, R.D.; de Carvalho, L.S.; do Nascimento, M.F.R.; Alhussain, F.; Abu Hasna, A. Endodontic irrigants from a comprehensive perspective. World J. Clin. Cases 2024, 12, 4460–4468. [Google Scholar] [CrossRef]
- Boutsioukis, C.; Kastrinakis, E.; Lambrianidis, T.; Verhaagen, B.; Versluis, M.; Van Der Sluis, L.W.M. Formation and removal of apical vapor lock during syringe irrigation: A combined experimental and Computational Fluid Dynamics approach. Int. Endod. J. 2014, 47, 191–201. [Google Scholar] [CrossRef]
- Gluskin, A.H.; Lai, G.; Peters, C.I.; Peters, O.A. The double-edged sword of calcium hydroxide in endodontics: Precautions and preventive strategies for extrusion injuries into neurovascular anatomy. J. Am. Dent. Assoc. 2020, 151, 317–326. [Google Scholar] [CrossRef]
- Ali, A.; Bhosale, A.; Pawar, S.; Kakti, A.; Bichpuriya, A.; Agwan, M.A.; Agwan, M.A.S. Current trends in root canal irrigation. Cureus 2022, 14, e24833. [Google Scholar] [CrossRef]
- Boutsioukis, C.; Arias-Moliz, M.T. Present status and future directions—Irrigants and irrigation methods. Int. Endod. J. 2022, 55, 588–612. [Google Scholar] [CrossRef]
- Mozo, S.; Llena, C.; Forner, L. Review of ultrasonic irrigation in endodontics: Increasing action of irrigating solutions. Med. Oral Patol. Oral Cir. Bucal 2012, 17, e512–e516. [Google Scholar] [CrossRef]
- Vyas, N.; Manmi, K.; Wang, Q.; Jadhav, A.J.; Barigou, M.; Sammons, R.L.; Kuehne, S.A.; Walmsley, A.D. Which Parameters Affect Biofilm Removal with Acoustic Cavitation? A Review. Ultrasound Med. Biol. 2019, 45, 1044–1055. [Google Scholar] [CrossRef]
- van der Sluis, L.W.M.; Verhaagen, B.; Macedo, R.; Versluis, M. The Role of Irrigation in Endodontics. In Lasers in Endodontics: Scientific Background and Clinical Applications; Olivi, G., De Moor, R., DiVito, E., Eds.; Springer International Publishing: Cham, Switzerland, 2016; pp. 45–69. [Google Scholar]
- Lee, S.J.; Wu, M.K.; Wesselink, P. The effectiveness of syringe irrigation and ultrasonics to remove debris from simulated irregularities within prepared root canal walls. Int. Endod. J. 2004, 37, 672–678. [Google Scholar] [CrossRef]
- Rödig, T.; Sedghi, M.; Konietschke, F.; Lange, K.; Ziebolz, D.; Hülsmann, M. Efficacy of syringe irrigation, RinsEndo and passive ultrasonic irrigation in removing debris from irregularities in root canals with different apical sizes. Int. Endod. J. 2010, 43, 581–589. [Google Scholar] [CrossRef] [PubMed]
- Nagendrababu, V.; Jayaraman, J.; Suresh, A.; Kalyanasundaram, S.; Neelakantan, P. Effectiveness of ultrasonically activated irrigation on root canal disinfection: A systematic review of in vitro studies. Clin. Oral Investig. 2018, 22, 655–670. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.; Horsley, T.; Weeks, L. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Ali, A.; Hashem, A.; Roshdy, N.N.; Abdelwahed, A. The Effect of Final Irrigation Agitation Techniques on Postoperative Pain after Single Visit Root Canal Treatment of Symptomatic Irreversible Pulpitis: A Randomised Clinical Trial. Eur. Endod. J. 2023, 8, 187–193. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Liu, J.; Dong, G.; Peng, B.; Yang, P.; Chen, Z.; Yang, F.; Guo, D. Comparison between ultrasonic irrigation and syringe irrigation in clinical and laboratory studies. J. Oral Sci. 2016, 58, 373–378. [Google Scholar] [CrossRef]
- Herrera, D.R.; Martinho, F.C.; de-Jesus-Soares, A.; Zaia, A.A.; Ferraz, C.C.R.; Almeida, J.F.A.; Gomes, B. Clinical efficacy of EDTA ultrasonic activation in the reduction of endotoxins and cultivable bacteria. Int. Endod. J. 2017, 50, 933–940. [Google Scholar] [CrossRef]
- Jambagi, N.; Kore, P.; Dhaded, N.S.; Patil, S.A.; Shankar, M. Comparison of Antimicrobial Efficacy of Diode Laser, Ultrasonic Activated and Conventional Irrigation with 2.5% NaOCl during RCT: An Interventional Study. J. Contemp. Dent. Pract. 2021, 22, 669–673. [Google Scholar]
- Kathiria, N.V.; Attur, K.; Bagda, K.M.; Venkataraghavan, K.P.; Patel, K.; Mustafa, M.B.; Attur, S.K. Postendodontic Pain Using Single File System with Different Irrigation Protocols in Single-visit Root Canal Treatment: A Randomized Control Trial. J. Contemp. Dent. Pract. 2024, 25, 180–185. [Google Scholar] [CrossRef]
- Mathevanan, S.; Sureshbabu, N.M.; Solete, P.; Teja, K.V.; Jose, J. Comparison of postoperative pain reduction following laser, ultrasonic activation and conventional needle irrigation after root canal treatment—A randomized clinical trial. J. Clin. Exp. Dent. 2023, 15, e1045–e1053. [Google Scholar] [CrossRef]
- Mittal, N.; Baranwal, H.C.; Gupta, S.; Shankari, T.; Gupta, S.; Kharat, S. Comparative analysis of reduction in pain scores after single visit root canal treatment using endodontic irrigation protocols, namely, Conventional needle irrigation, PUI, PIPS and SWEEPS: A randomized control trial. J. Conserv. Dent. Endod. 2023, 26, 143–149. Available online: https://journals.lww.com/jcde/fulltext/2023/26020/comparative_analysis_of_reduction_in_pain_scores.4.aspx (accessed on 22 August 2025).
- Orozco, E.I.F.; Toia, C.C.; Cavalli, D.; Khoury, R.D.; Cardoso, F.G.d.R.; Bresciani, E.; Valera, M.C. Effect of passive ultrasonic activation on microorganisms in primary root canal infection: A randomized clinical trial. J. Appl. Oral Sci. 2020, 28, e20190100. [Google Scholar] [CrossRef] [PubMed]
- Palanisamy, R.; Anirudhan, S.; Roja, R.J.S.; Koshy, M. Comparison of ultrasonic versus side-vented needle irrigation for reductions in bacterial growth and postoperative pain: A randomized controlled trial. J. Conserv. Dent. Endod. 2023, 26, 616–620. Available online: https://journals.lww.com/jcde/fulltext/2023/26060/comparison_of_ultrasonic_versus_side_vented_needle.3.aspx (accessed on 22 August 2025). [CrossRef] [PubMed]
- Parvez, B.; Sinha, D.J.; Sharma, N.; Nagesh, H.M.; Rawat, M.; Pranshu, P. Comparative Evaluation of Post-Operative Pain Following Single Visit Root Canal Treatment. Ann. Dent. Spec. 2022, 10, 39–44. [Google Scholar] [CrossRef]
- Tang, Z.; Wang, H.; Jiang, S. Clinical study of single-visit root canal treatment with a nickel-titanium (Ni-Ti) rotary instrument combined with different ultrasonic irrigation solutions for elderly patients with chronic apical periodontitis. Biomed. Mater. Eng. 2015, 26 (Suppl. S1), S311–S318. [Google Scholar] [CrossRef] [PubMed]
- Kato, A.S.; Cunha, R.S.; da Silveira Bueno, C.E.; Pelegrine, R.A.; Fontana, C.E.; de Martin, A.S. Investigation of the Efficacy of Passive Ultrasonic Irrigation Versus Irrigation with Reciprocating Activation: An Environmental Scanning Electron Microscopic Study. J. Endod. 2016, 42, 659–663. [Google Scholar] [CrossRef]
- American Association of Endodontists. Root Canal Irrigants and Disinfectants, Endodontics Colleagues for Excellence; American Association of Endodontists: Chicago, IL, USA, 2011. [Google Scholar]
- Prada, I.; Micó-Muñoz, P.; Giner-Lluesma, T.; Micó-Martínez, P.; Collado-Castellano, N.; Manzano-Saiz, A. Influence of microbiology on endodontic failure. Literature review. Med. Oral Patol. Oral Cir. Bucal 2019, 24, e364–e372. [Google Scholar] [CrossRef]
- Sakamoto, M.; Siqueira, J.F.; Rôças, I.N.; Benno, Y. Bacterial reduction and persistence after endodontic treatment procedures. Oral Microbiol. Immunol. 2007, 22, 19–23. [Google Scholar] [CrossRef]
- Patel, N.; Khan, I.; Jarad, F.; Zavattini, A.; Koller, G.; Pimentel, T.; Mahmood, K.; Mannocci, F. The short-term postoperative pain and impact upon quality of life of pulpotomy and root canal treatment, in teeth with symptoms of irreversible pulpitis: A randomized controlled clinical trial. Int. Endod. J. 2025, 58, 55–70. [Google Scholar] [CrossRef]
- Versiani, M.; Martins, J.; Ordinola-Zapata, R. Anatomical complexities affecting root canal preparation: A narrative review. Aust. Dent. J. 2023, 68, S5–S23. [Google Scholar] [CrossRef]
- Wong, J.; Manoil, D.; Näsman, P.; Belibasakis, G.N.; Neelakantan, P. Microbiological Aspects of Root Canal Infections and Disinfection Strategies: An Update Review on the Current Knowledge and Challenges. Front. Oral Health 2021, 2, 672887. [Google Scholar] [CrossRef]
- Khaidarov, A.; Alyavi, M.; Alieva, M. Irrigation in Modern Endodontics. World Bull. Public Health 2024, 32, 22–24. Available online: https://www.researchgate.net/publication/378935744_IRRIGATION_IN_MODERN_ENDODONTICS (accessed on 22 August 2025).
- Al-Ali, M.; Sathorn, C.; Parashos, P. Root canal debridement efficacy of different final irrigation protocols. Int. Endod. J. 2012, 45, 898–906. [Google Scholar] [CrossRef]
- Van Der Vyver, P.; Vorster, M.; Paleker, F.; De Wet, F. Errors in root canal preparation: A review of the literature and clinical case reports. S. Afr. Dent. J. 2019, 74, 246–254. [Google Scholar] [CrossRef]
- İriboz, E.; Bayraktar, K.; Türkaydın, D.; Tarçın, B. Comparison of apical extrusion of sodium hypochlorite using 4 different root canal irrigation techniques. J. Endod. 2015, 41, 380–384. [Google Scholar] [CrossRef] [PubMed]
- Velardi, J.P.; Alquria, T.A.; Alfirdous, R.A.; Corazza, B.J.M.; Gomes, A.P.M.; Silva, E.G.; Griffin, I.L.; Tordik, P.A.; Martinho, F.C. Comparison of GentleWave system and passive ultrasonic irrigation with minimally invasive and conventional instrumentation against LPS in infected root canals. Sci. Rep. 2022, 12, 4894. [Google Scholar] [CrossRef]
- Shon, W.J. Introducing the GentleWave System. Restor. Dent. Endod. 2016, 41, 235. [Google Scholar] [CrossRef] [PubMed]
- Coaguila-Llerena, H.; Gaeta, E.; Faria, G. Outcomes of the GentleWave system on root canal treatment: A narrative review. Restor. Dent. Endod. 2022, 47, e11. [Google Scholar] [CrossRef]
| Database (Date of Search) | Search Strategies | Number of Articles Found |
|---|---|---|
| PubMed (18 August 2025) | (“root canal” [tiab] OR “root canal therapy” [mesh] OR pulpectomy [tiab]) AND (acoustic [tiab] OR ultrasonic [tiab] OR multisonic [tiab] OR gentlewave [tiab]) AND (“side vented needle” [tiab] OR “syringe” [tiab] OR “conventional techniq*” [tiab] OR “conventional irriga*” [tiab]) AND (“efficacy” [tiab] OR “outcome*” [tiab] OR “failure” [tiab] OR “success” [tiab] OR “clinical outcome*” [tiab] OR “compar*” [tiab] OR “bacteria reduc*” [tiab] OR “post op pain” [tiab] OR “post operative pain” [tiab] OR “longevity” [tiab]) | 184 |
| Scopus (18 August 2025) | TITLE-ABS-KEY ((“root canal” OR “root canal therapy” OR “pulpectomy”) AND (“acoustic” OR “ultrasonic” OR “multisonic” OR “gentlewave”) AND (“side vented needle” OR “syringe” OR “conventional techniq*” OR “conventional irriga*”) AND (“efficacy” OR “outcome*” OR “failure” OR “success” OR “clinical outcome*” OR “compar*” OR “bacteria reduc*” OR “post op pain” OR “post operative pain” OR “longevity”)) | 256 |
| Dentistry and Oral Sciences Source (18 August 2025) | (AB (“root canal” OR SU “root canal treatment” OR “pulpectomy”) AND (“acoustic” OR “ultrasonic” OR “multisonic” OR “gentlewave”) AND (“side vented needle” OR “syringe” OR “conventional techniq*” OR “conventional irriga*”) AND (“efficacy” OR “outcome*” OR “failure” OR “success” OR “clinical outcome*” OR “compar*” OR “bacteria reduc*” OR “post op pain” OR “post operative pain” OR “longevity”)) OR (TI (“root canal” OR SU “root canal treatment” OR “pulpectomy”) AND (“acoustic” OR “ultrasonic” OR “multisonic” OR “gentlewave”) AND (“side vented needle” OR “syringe” OR “conventional techniq*” OR “conventional irriga*”) AND (“efficacy” OR “outcome*” OR “failure” OR “success” OR “clinical outcome*” OR “compar*” OR “bacteria reduc*” OR “post op pain” OR “post operative pain” OR “longevity”)) | 112 |
| Google (18 August 2025) | “Ultrasonic Activation EDTA” AND “passive ultrasonic activation randomized clinical trial” | 2 |
| Inclusion Criteria | Exclusion Criteria |
|---|---|
|
|
| Author (Year) | Tooth Type/Diagnosis | Sample Size (Teeth) | Irrigation Methods Compared | Insrumentation Protocol of the Study | Ultrasonic Irrigation Protocol | CNI Protocol | Irrigant Concentrations | Deposition Distances from Working Length Activation Frequency |
|---|---|---|---|---|---|---|---|---|
| Ali (2023) [18] | Mandibular first molars Symptomatic irreversible pulpitis | 78 | XP Endo Finisher UltraX (Ultrasonic) Side Vented Needle | ProTaper Next (PTN) instruments were used to mechanically prepare the root canals in a crown-down technique using an endodontic motor with an adjusted torque of 2 Ncm and speed of 300 rpm according to the manufacturer’s instructions. The PTN rotary system was used as follows: X1, X2, followed by X3 as the master apical file. All files were used in a pecking motion. | 3 mL of 2.5% NaOCl solution was passively introduced in each canal, Ultra X at the maximum power of 45 kHz with flexible and soft silver tip (21 mm, size 20 taper 2) was fitted passively reaching 2 mm short from the working length in short vertical strokes. The irrigation solution was activated for 1 min in each canal. | 3 mL of 2.5% NaOCl solution was passively introduced in each canal by a side-vented needle that was passively placed at 2 mm short from the working length and was constantly pulsed in 1–2 mm vertical strokes for 1 min in each canal. | 2.5% NaOCL | 2 mm Short of Working Length 45 kHz |
| Chen (2016) [19] | Mandibular premolars with a single straight canal Periapical Periodontitis | 60 | Syringe Irrigation Ultrasonic Irrigation | Series of K-files using the step-back enlargement technique. The master apical file, which was three sizes larger than the initial apical file, was used for each pre-molar. | 40 mL of 2.5% NaOCl and Odontonson-M ultrasonic instruments. #15 ultrasonic file was placed at the border between the lower third and middle third of the root canals. The oscillation was performed in bucco-lingual direction for 2 min without the ultrasonic file binding to the canals walls. The 2.5% NaOCl solution was delivered at a rate of 20 mL/min through the ultrasonic file. | (40 mL) of 2.5% NaOCl solution using a 5 mL syringe and a 27-gauge needle. The tip of the needle was placed at the border between the lower third and middle third of the root canals. | 2.5% NaOCl | Border of Lower and Middle Third Manufacturers Reccomended Power Setting |
| Herrera (2017) [20] | Maxillary single-rooted teeth with one root canal per root Pulp necrosis and apical periodontitis | 24 | EDTA with Ultrasonic Activation EDTA Flushing | The cervical and middle thirds of the root canals were prepared with the crown-down technique using Gates Glidden burs. A size 10 K-file was used to obtain the full length of the root canal, using an apex locator. Next, root canals were instrumented using the Mtwo rotary nickel-titanium system according to the manufacturer’s instructions. The instrumentation sequence was as follows: size 10, 0.04 taper, size 15, 0.05 taper, size 20, 0.06 taper, size 25, 0.06 taper, size 30, 0.05 taper, size 35, 0.04 taper and size 40, 0.04 taper. | The root canal was flooded with 1 mL of EDTA and immediately activated for 30 s using an ultrasonic tip that was inserted 2 mm short of the root canal length. The power setting of the ultrasonic device was 30%); then, EDTA was aspirated and refreshed repeating the procedure twice. | The root canal was flooded with 1 mL of EDTA for 30 s; then, EDTA was aspirated and refreshed, repeating the procedure twice. Finally, the root canals were irrigated with 5 mL of saline. | 2.5% NaOCl 2% Chlorohexidine 17% EDTA | 2 mm Short of Working Length 30% Power of Ultrasonic Device |
| Jambagi (2021) [21] | Maxillary and mandibular single-rooted canals (permanent incisors, laterals, canines, premolars) Non-Vital | 60 | High Power Diode Laser Ultrasonic Irrigation Syringe (26 gauge) | ProTaper Universal rotary system using the crown down technique. | The root canal was ultrasonically irrigated (P5 Booster) for 3 min with a continuous flow of 50 mL with 2.5% NaOCl. | 2 mL of 2.5% NaOCl, after each instrumentation with a disposable syringe of 26 gauge needle. | 2.5% NaOCL 17% EDTA | Not Stated |
| Kathiria (2024) [22] | Permanent maxillary and mandibular molars Asymptomatic irreversible pulpitis | 150 | Side Vented Needle EndoActivator UltraX (Ultrasonic) | Canals were prepared with F-One single file system in crown down technique according to the manufacturer’s instruction, i.e., 2.5 controlled torque and at 500 RPM with X Smart EndoMotor. Orifice enlargement followed by cleaning and shaping was performed using 17/12 and 25/06 rotary files, respectively. Apical diameter was prepared up to #25 file. | 2 mL of 3% NaOCl was flushed in the canal and irrigated using ultrasonic tip (Ultra X) at 2–3 mm to the working length. The solution was activated by vertical up and down strokes for 20 s. Repeat the cycle for 3–4 times. | 4 mL of 3% NaOCl was flushed into all the canals using a side-vented 30-Gauge needle, 2 mm short from working length. | 3% NaOCl 17% EDTA | 2–3 mm Short of the Working Length Not Stated |
| Mathevanan (2023) [23] | Mandibular first molars Symptomatic irreversible pulpitis | 75 | Conventional Needle Irrigation Passive Ultrasonic Irrigation Laser Activated Irrigation | The glide path preparation was performed using continuous rotary instrumentation. All the canals were prepared using a continuous rotary system (ProTaper Gold). | Irrigants were dispensed into the canal using a 31G single port side vented needle and the final irrigant activation was performed using IRR 25/25 IrriSafeTM file driven by a P5 piezoelectric ultrasonic unit at a power setting of 5 while placing 2 mm short of working length. 3 mL of 3% NaOCl was used for each activation cycle for 30 s for a total of two cycles. and 3 mL 17% EDTA was activated for 30 s for two cycles followed by a final rinse of 3 mL of physiological saline to neutralize the effects of EDTA. | 27 mm single side-port needle, 3 mL of 3% NaOCl was delivered subsequently into each prepared canal such that the needle was not bound and was placed 2 mm short of the working length and moved up and down with 2 mm amplitude for a total time of 30 s. An intermittent flush of 2 mL of physiological saline was carried out after the usage of NaOCl. 3 mL of 17% ethylenediaminetetraacetic acid (EDTA) was used as a final rinse for 1 min followed by irrigation using 5 mL of physiological saline to neutralize the effects of EDTA. | 3% NaOCl 17% EDTA | 2 mm Short of the Working Length Power Setting 5 |
| Mittal (2023) [24] | Maxillary and mandibular molars Symptomatic irreversible pulpitis | 60 | New laser irrigation activation system shock wave-enhanced emission photoacoustic streaming (SWEEPS) Photon-induced photoacoustic streaming (PIPS) Passive ultrasonic irrigation activation techniques Conventional irrigation (CI) method. | Hyflex EDM files were used for root canal preparation according to the manufacturer’s instructions with canalPro endomotor. | Irrigation solution was activated using an ultrasonic tip (Ultra X) to an ultrasonic device (Ultra X). The activation of the tip was activated for around three times, with each cycle for 20 s along involving the use of 1 mL of 3% NaOCl. 2 mL of 17% EDTA solution was then activated for 1 min. Without touching the canal walls, the ultrasonic tip was placed 2 mm short of the working length of canal. | 2 mL of saline with 2% povidone–iodine was used as the initial irrigant and this was followed by the NaOCl, and EDTA, as mid–rinses using 1 mL for each canal, followed by 2 mL of 2% chlorhexidine as last irrigant using 29–G side vented irrigation needle. The process of recapitulation was performed at each file change with a size #10 K–file. | 10% EDTA 15% Carbamide Peroxide 2% Provodone Iodine 3% NaOCl 2% Chlorohexidine | 2 mm Short of the Working Length Not Stated |
| Orozco (2020) [25] | Upper and lower single rooted teeth Pulp necrosis with radiographic evidence of apical periodontitis and intact pulp chamber walls | 20 | Passive Ultrasonic Activation Conventional Needle Irrigation | Instrumentation was performed by one single operator using single-file reciprocation technique. Initial apical instrument was ISO size #20 hand file, which reached passively to working length. The file was adapted to an electric motor using preset adjustments. The instrument was introduced into the root canal until resistance was felt and then activated. Next, the instrument was apically moved using in-and-out pecking motions, with approximately 3 mm in amplitude by using light apical pressure. After 3 pecking motions, the instrument was removed and cleaned. Between each third (cervical, middle, and apical), 8 mL of 2.5% NaOCl was used to neutralize the content inside the root canal. The working length (−1 mm) was determined by using an apex locator and confirmed by a periapical digital radiograph. Likewise, apical debridement was performed with a K-file size #30, which was extended 1 mm beyond this area. The root canal instrumentation was completed in a single visit in all cases, with a total of 24 mL of 2.5% NaOCl in both groups. | The root canals were irrigated with 4 mL of 2.5% NaOCl delivered by using a 31 gauge × 27 mm side port needle inserted up to 1 mm short of the WL, with PUA being performed for 30 s. The irrigating solution was renewed with 4 mL of 2.5% NaOCl and PUA was resumed for 30 additional seconds. For inactivation of 2.5% NaOCl, the canal was irrigated with 5 mL of 5% sodium thiosulfate, followed by irrigation with 10 mL of saline solution. The ultrasonic activation was performed with a #20:01 non-cutting tip (E1 Irrisonic) and piezoelectric ultrasonic device (ALT—Equipamentos Médicos e Odontológicos) at 1000 Hz low power. The ultrasonic instrument was used at 1 mm short of the WL, avoiding contact with the root canal walls. | The root canals were irrigated with 8 mL of 2.5% NaOCl by using a 31 gauge × 27 mm side port needle, inserted up to 1 mm short of the WL, and 17% EDTA remained inside the root canal for 4 min and manually agitated for 1 additional minute. The 2.5% NaOCl inactivation and 17% EDTA removal were performed in the same manner as described for PUA group. No ultrasonic activation was performed in this group. | 2.5% NaOCL 17% EDTA | 1 mm Short of the Working Length 1000 Hz |
| Palanisamy (2023) [26] | Single–rooted teeth Pulpal necrosis | 80 | Passive Ultrasonic Irrigation Side Vented Needle Irrigation | Canal instrumentation was accomplished using rotary and hand files, as well as 5.25% sodium hypochlorite irrigation. All teeth were prepared with ProTaper rotary instruments. | Agitated with a 150 μm, noncutting, stainless steel wire (Irrisafe) attached to an ultrasonic device (P5 Newtron unit) set to 10 (frequency, 30 kHz). The irrigation protocol was similar to that used in Group CNI, but the irrigants were passively agitated using Irrisafe tips (#15 ultrasonic file) for 30 s before changing the solution. | 6 mL of 2.5% NaOCl and a 31G, 27 mm NaviTip Sideport needle, 1 mm from the working length for 3 min (flow rate, 2 mL/min). This was followed by irrigation with 1 mL of 17% EDTA for 1 min and 1 mL of 2% chlorhexidine for 1 min. | 2.5% NaOCL 17% EDTA 2% Chlorohexidine | 1 mm Short of the Working Length 30 kHz |
| Parvez (2022) [27] | Permanent molars Asymptomatic irreversible pulpitis, periapical periodontitis | 120 | Side Vented Needle Passive Ultrasonic Irrigation | Group 1: The canal was cleaned and shaped by hand, using K-files and the step-back technique. Group 2: The ProTaper Next crown down technique was used for cleaning and shaping. Glyde was used to lubricate the canals during the preparation process. Preparation began with X1, then X2, then X3, with apical rotation at 300 rpm and torque of 2–5.2 N/s using the X smart plus endo-motor. Group 3: Cleaning and shaping were carried out with Wave One Gold reciprocating files using gentle inward motion. During preparation, canals were lubricated with glyde. Withdrawing the file every 3 mm to remove debris. Shaping was achieved at the definitive working length with X smart plus endomotor. | Group 1B: Irrigation with 2.5 percent NaOCl and 17 percent EDTA was performed during the preparation, the canals were kept filled with 2.5 percent NaOCl, and the ultrasonic file (Mani Inc.) was kept short by 2 mm from the working length and free from the canals before passive ultrasonic irrigation was performed for 1 min. Group 2B: Irrigation with 2.5 percent NaOCl and 17 percent EDTA was performed during the preparation, the canal was kept filled with 2.5 percent NaOCl, and the ultrasonic file was kept short by 2 mm from the working length and free from the canals, then passive ultrasonic irrigation was performed for 1 min. Group 3B: Irrigation with 2.5 percent NaOCl and 17 percent EDTA was performed during the preparation. The canal was kept filled with 2.5 percent NaOCl and the ultrasonic file was kept short by 2 mm from the working length and free from the canals, after which passive ultrasonic irrigation was performed for 1 min. | Group 1A: Irrigation was performed with 2.5 percent NaOCl using a 27 gauge side vented needle (Acteon) and 17 percent EDTA during the preparation, followed by final irrigation with normal saline (0.9% w/v). Group 2A: Irrigation with 2.5 percent NaOCl and 17 percent EDTA was performed throughout the preparation, and final irrigation was done with normal saline using a 27 gauge side vented needle. Group 3A: During the preparation, irrigation was done with 2.5% NaOCl using a 27 gauge side vented needle and with 17% EDTA, final irrigation was carried out with normal saline. | 2.5% NaOCL 17% EDTA | 2 mm Short of the Working Length Not Stated |
| Tang (2015) [28] | Incisors, Premolars, Molars Periapical Periodontitis | 360 | Ultrasonic Irrigation Syringe Irrigation | Mtwo NiTi files were used for the canal preparation. | Group A: 2.5% sodium hypochlorite solution in ultrasonic irrigation. Group B: Active silver ion antibacterial solution in ultrasonic irrigation. | Syringe irrigation with 2.5% sodium hypochlorite solution. | 2.5% NaOCl | Not Stated |
| Author (Year) | Irrigation Methods Compared | Comparison in Bacterial/Endotoxin Reduction | Pain Scales Utilized | Comparison of Post Operative Pain | Proposed Mechanisms |
|---|---|---|---|---|---|
| Ali (2023) [18] | XP Endo Finisher UltraX (Ultrasonic) Side Vented Needle | Not Applicable | Verbal Rating Scale | No statistically significant difference was found between all groups regarding the incidence and intensity of pain at different time intervals (p > 0.05). | Not Applicable |
| Chen (2016) [19] | Syringe Irrigation Ultrasonic Irrigation | Not Applicable | Incidence of Pain | No significant difference in the incidence of pain was observed between the syringe irrigation and ultrasonic irrigation groups. | Not Applicable |
| Herrera (2017) [20] | EDTA with Ultrasonic Activation EDTA Flushing | A statistically significant difference was found in the median percentage values for the reduction in cultivable bacteria (p < 0.05) between CNI (23.56%) and PUA (98.37%), producing 30% and 80% root canals free of cultivable bacteria in CNI and PUA group, respectively, in endodontic treatment The number of cultivable bacteria significantly decreased in PUA group, with 98.37% reduction percentage when comparing with CNI group, which only reduced 23.56%. | Not Applicable | Not Applicable | The energy transmitted might lead to an acoustic streaming, cavitation, and/or warming of the irrigating substance, expanding its spectrum of action, especially on microorganisms in difficult-to-reach areas. |
| Jambagi (2021) [21] | High Power Diode Laser Ultrasonic Irrigation Syringe (26 gauge) | Highest reduction in the microbial count was seen in diode laser group (60.92%), ultrasonic group was second with (47.22%), and least reduction was observed in conventional irrigation (37.97%). | Not Applicable | Not Applicable | Flow of the irrigant at a high velocity which was achieved due to passive ultrasonic activation thus facilitating the removal of debrisfrom the root canal irregularities and oval-shaped canals. |
| Kathiria (2024) [22] | Side Vented Needle EndoActivator UltraX (Ultrasonic) | Not Applicable | Visual Analog Scale | Side vented needle had more pain when compared with Endoactivator and Ultrasonic groups at 6 h, but there was no statistically significant difference in pain after the intial 6 h. | Damage to microorganisms and physical destruction of biofilm is the result of explosive and implosion, which is created by sheer stress. This might be the reason for less pain after 6 h of follow-up with UX. |
| Mathevanan (2023) [23] | Conventional Needle Irrigation Passive Ultrasonic Irrigation Laser Activated Irrigation | Not Applicable | Visual Analog Scale | The pairwise comparison showed that PUI and LAI group had a significant reduction in pain scores at all experimental periods when compared to CNI (p < 0.05), with no significant difference in PUI and LAI in postoperative pain scores at all the assessed time intervals. The consumption of analgesic was assessed and participants who received CNI were subjected to more incidence of analgesic consumption followed by LAI and PUI, respectively (p < 0.05). | Insufficient pulpal debridement with CNI leading to more post-operative pain scores |
| Mittal (2023) [24] | New laser irrigation activation system shock wave-enhanced emission photoacoustic streaming (SWEEPS) Photon-induced photoacoustic streaming (PIPS) Passive ultrasonic irrigation activation techniques Conventional irrigation (CI) method. | Not Applicable | Visual Analog Scale | Significant difference (p < 0.05) between all study groups. Post hoc statistical analysis revealed that pain score decreased significantly in Group 4 (SWEEPS), followed by Group 3 (PIPS), Group 2 (ultrasonic activation), and Group 1 (conventional needle irrigation) | The oscillatory movement in ultrasonic system pushes the irrigants laterally to the canal walls, whereas with CI with syringe, irrigants constantly move apically. This causes irrigants to extrude apically, leading to increased incidence of postoperative pain. |
| Orozco (2020) [25] | Passive Ultrasonic Activation Conventional Needle Irrigation | A statistically significant difference was found in the median percentage values for the reduction in cultivable bacteria (p < 0.05) between CNI (23.56%) and PUA (98.37%), producing 30% and 80% root canals free of cultivable bacteria in CNI and PUA group, respectively, in endodontic treatment The number of cultivable bacteria significantly decreased in PUA group, with 98.37% reduction percentage when comparing with CNI group, which only reduced 23.56%. | Not Applicable | Not Applicable | The energy transmitted might lead to an acoustic streaming, cavitation, and/or warming of the irrigating substance, expanding its spectrum of action, especially on microorganisms in difficult-to-reach areas. |
| Palanisamy (2023) [26] | Passive Ultrasonic Irrigation Side Vented Needle Irrigation | Ultrasonic irrigation had a higher proportion of bacteria-free samples than Side Vented Needle irrigation. The passive ultrasonic irrigation group reduced positive bacterial culture by 57%, while the side-vented needle irrigation group reduced it by 22.5% | Visual Analog Scale | Ultrasonic showed a significant reduction in pain at 6 and 12 h compared to side vented needle (p < 0.05), but there were no significant differences observed at 24 and 48 h time-points. | Acoustic streaming and cavitation during passive ultrasonic irrigation. |
| Parvez (2022) [27] | Side Vented Needle Passive Ultrasonic Irrigation | Not Applicable | Numeric Pain Scale | The use of a needle versus passive ultrasonic irrigation had no statistically significant differences. | Not Applicable |
| Tang (2015) [28] | Ultrasonic Irrigation Syringe Irrigation | Not Applicable | Visual Analog Scale | Self-assessed pain levels 24 h after the procedure are significantly lower for Ultrasonic than for Syringe (p < 0.05). Ultrasonic showed lower incidences of postoperative acute reactions. | Not Applicable |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marx, J.; Ward, C.; Gunnell, B.; Marx, Z.; Parry, A.; Dyal, S.; Mohajeri, A.; Hung, M. Influence of Ultrasonic Activation of Endodontic Irrigants on Microbial Reduction and Postoperative Pain: A Scoping Review of In Vivo Studies. Dent. J. 2025, 13, 459. https://doi.org/10.3390/dj13100459
Marx J, Ward C, Gunnell B, Marx Z, Parry A, Dyal S, Mohajeri A, Hung M. Influence of Ultrasonic Activation of Endodontic Irrigants on Microbial Reduction and Postoperative Pain: A Scoping Review of In Vivo Studies. Dentistry Journal. 2025; 13(10):459. https://doi.org/10.3390/dj13100459
Chicago/Turabian StyleMarx, Jacob, Corban Ward, Bayler Gunnell, Zachary Marx, Alicia Parry, Samuel Dyal, Amir Mohajeri, and Man Hung. 2025. "Influence of Ultrasonic Activation of Endodontic Irrigants on Microbial Reduction and Postoperative Pain: A Scoping Review of In Vivo Studies" Dentistry Journal 13, no. 10: 459. https://doi.org/10.3390/dj13100459
APA StyleMarx, J., Ward, C., Gunnell, B., Marx, Z., Parry, A., Dyal, S., Mohajeri, A., & Hung, M. (2025). Influence of Ultrasonic Activation of Endodontic Irrigants on Microbial Reduction and Postoperative Pain: A Scoping Review of In Vivo Studies. Dentistry Journal, 13(10), 459. https://doi.org/10.3390/dj13100459








