Race to the Moon or the Bottom? Applications, Performance, and Ethical Considerations of Artificial Intelligence in Prosthodontics and Implant Dentistry
Abstract
:1. Introduction
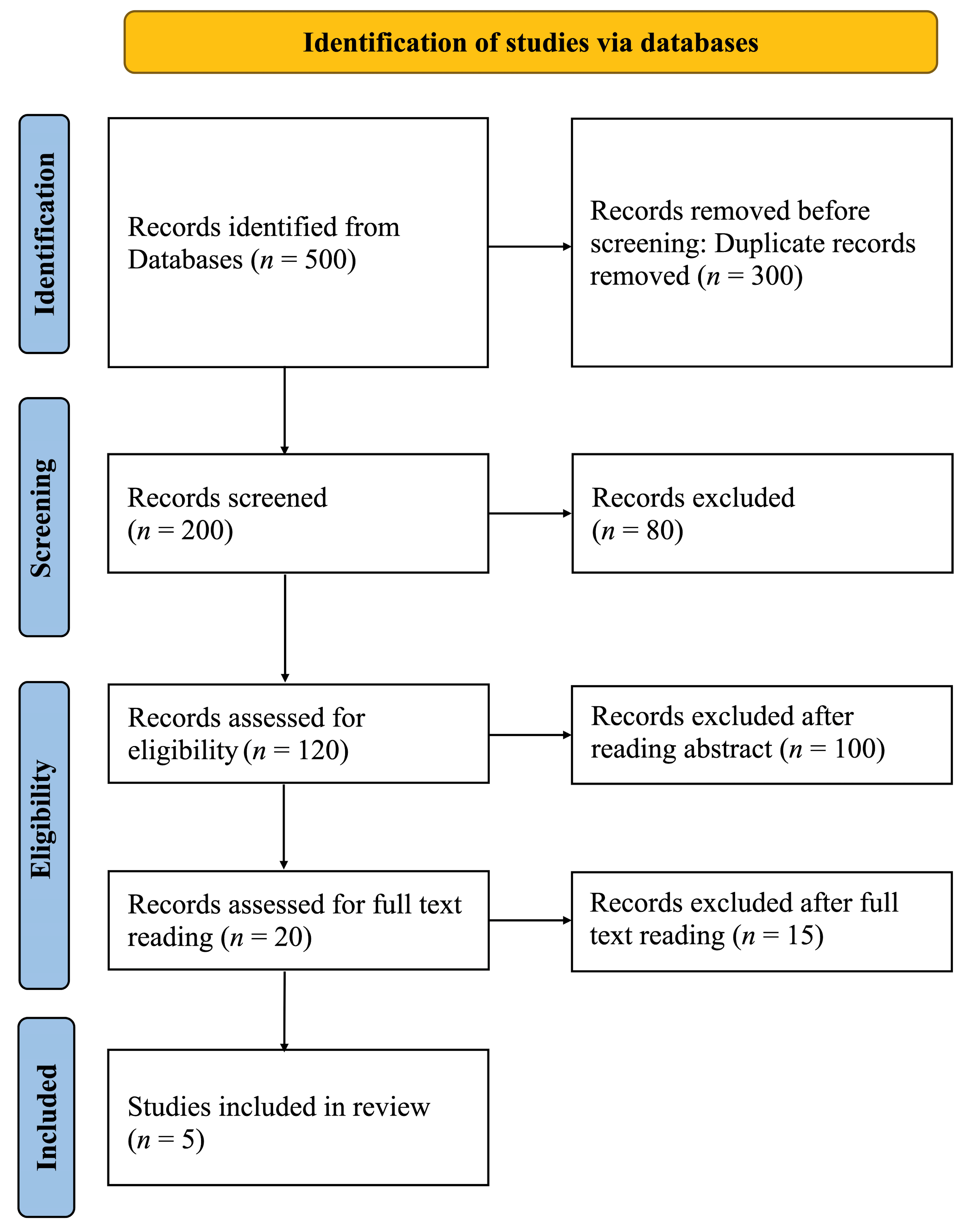
2. Materials and Methods
3. Results
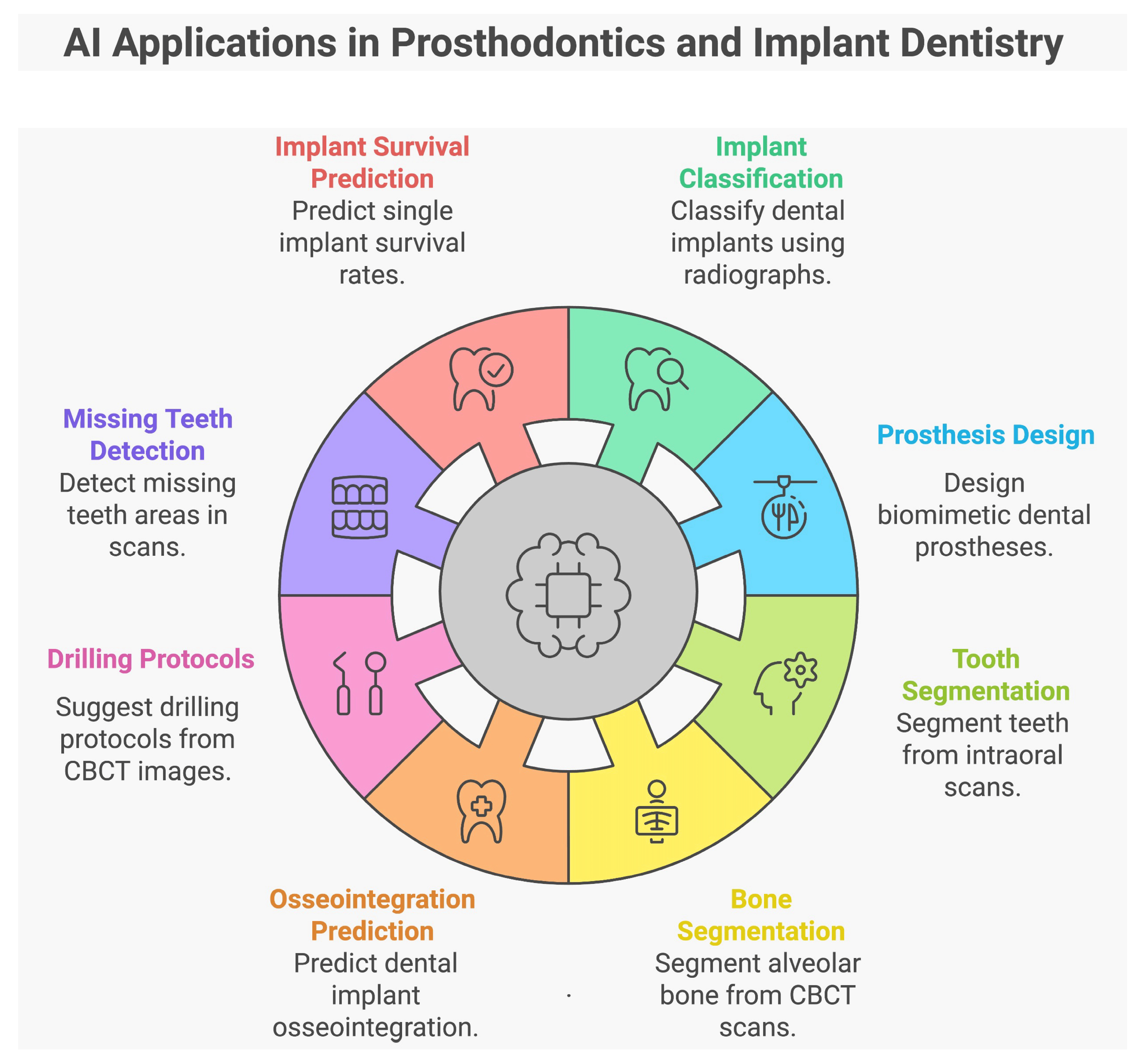
3.1. Applications of AI in Prosthodontics and Implant Dentistry
3.1.1. Characteristics of the Included Studies
3.1.2. Type of Dataset Utilized to Extract Data
3.1.3. Total Number of Datasets Extracted and Utilized for Training and Testing AI
3.1.4. Object Validation Method Utilized
3.1.5. Experts Involved in Data Validation
3.1.6. Performance Metrics Evaluation
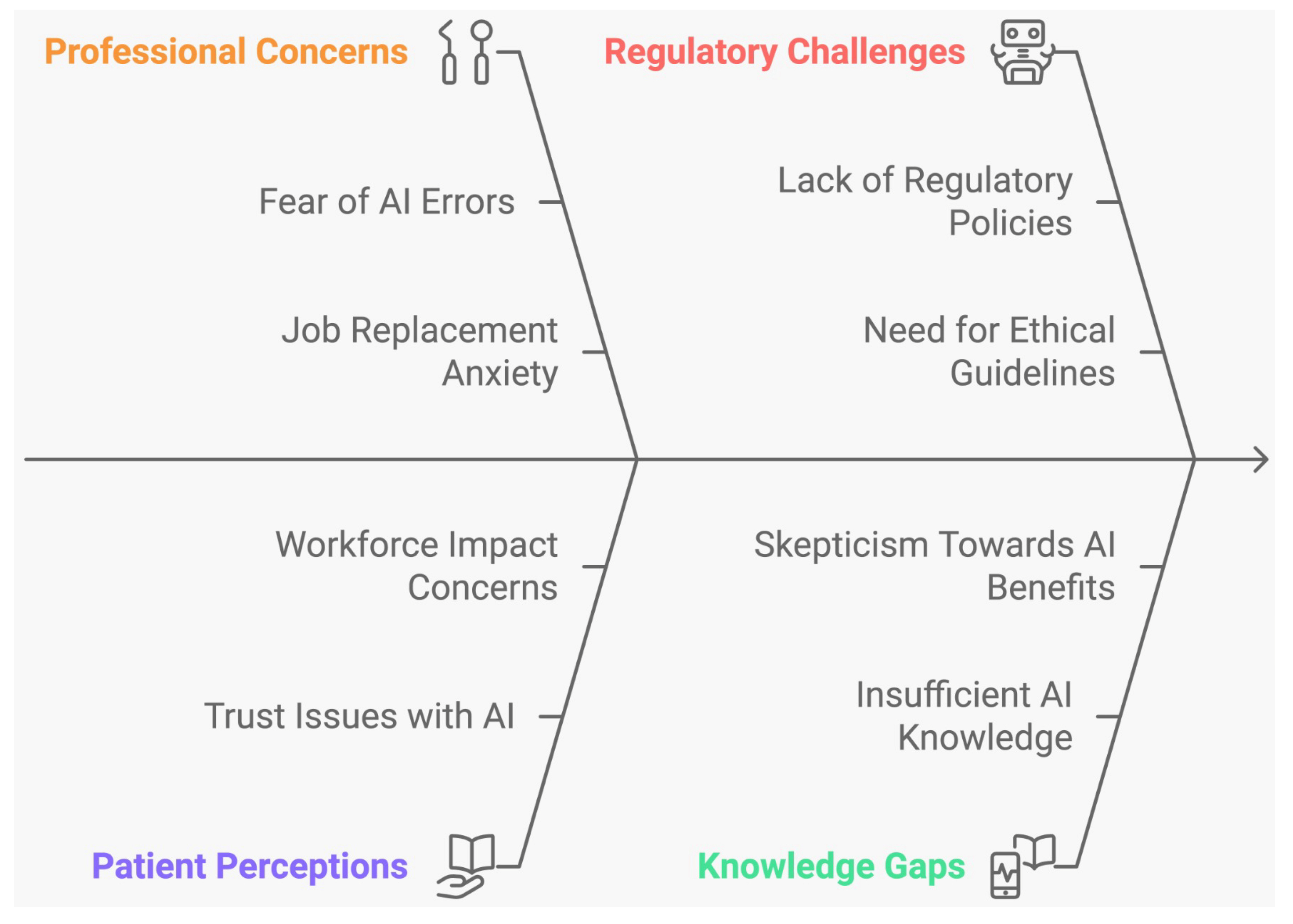
3.2. Ethical Issues Associated with the Use of AI in Dentistry
Characteristics of Included Studies
4. Discussion
4.1. Applications of AI in Prosthodontics and Implant Dentistry
Limitations of Studies
4.2. Ethical Issues Associated with the Use of AI in Dentistry
Limitations of Studies
4.3. Ethical Framework in Dentistry
4.3.1. Privacy and Data Security
4.3.2. Bias and Fairness
4.3.3. Transparency
4.3.4. Clinical Validation and Regulation
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Altalhi, A.M.; Alharbi, F.S.; Alhodaithy, M.A.; Almarshedy, B.S.; Al-Saaib, M.Y.; Al Jfshar, R.M.; Aljohani, A.S.; Alshareef, A.H.; Muhayya, M.; Al-Harbi, N.H. The Impact of Artificial Intelligence on Dental Implantology: A Narrative Review. Cureus 2023, 15, e47941. [Google Scholar] [CrossRef]
- Ramesh, A.N.; Kambhampati, C.; Monson, J.R.; Drew, P.J. Artificial intelligence in medicine. Ann. R. Coll. Surg. Engl. 2004, 86, 334–338. [Google Scholar] [CrossRef] [PubMed]
- Reyes, L.T.; Knorst, J.K.; Ortiz, F.R.; Ardenghi, T.M. Scope and challenges of machine learning-based diagnosis and prognosis in clinical dentistry: A literature review. J. Clin. Transl. Res. 2021, 7, 523–539. [Google Scholar] [PubMed]
- Semerci, Z.M.; Yardımcı, S. Empowering Modern Dentistry: The Impact of Artificial Intelligence on Patient Care and Clinical Decision Making. Diagnostics 2024, 14, 1260. [Google Scholar] [CrossRef] [PubMed]
- Alshadidi, A.A.; Alshahrani, A.A.; Aldosari, L.I.; Chaturvedi, S.; Saini, R.S.; Hassan, S.A.; Cicciù, M.; Minervini, G. Investigation on the application of artificial intelligence in prosthodontics. Appl. Sci. 2023, 13, 5004. [Google Scholar] [CrossRef]
- Singi, S.R.; Sathe, S.; Reche, A.R.; Sibal, A.; Mantri, N. Extended Arm of Precision in Prosthodontics: Artificial Intelligence. Cureus 2022, 14, e30962. [Google Scholar] [CrossRef]
- Zhang, B.; Dai, N.; Tian, S.; Yuan, F.; Yu, Q. The extraction method of tooth preparation margin line based on S-Octree CNN. Int. J. Numer. Method. Biomed. Eng. 2019, 35, e3241. [Google Scholar] [CrossRef] [PubMed]
- Lerner, H.; Mouhyi, J.; Admakin, O.; Mangano, F. Artificial intelligence in fixed implant prosthodontics: A retrospective study of 106 implant-supported monolithic zirconia crowns inserted in the posterior jaws of 90 patients. BMC Oral Health 2020, 20, 80. [Google Scholar] [CrossRef]
- Alqutaibi, A.Y.; Algabri, R.; Ibrahim, W.I.; Alhajj, M.N.; Elawady, D. Dental implant planning using artificial intelligence: A systematic review and meta-analysis. J. Prosthet. Dent. 2024; in press. [Google Scholar] [CrossRef]
- Safdar, N.M.; Banja, J.D.; Meltzer, C.C. Ethical considerations in artificial intelligence. Eur. J. Radiol. 2020, 122, 108768. [Google Scholar] [CrossRef] [PubMed]
- Wells, G.A.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. 2024. Available online: https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 19 September 2024).
- Kong, H.J.; Yoo, J.Y.; Lee, J.H.; Eom, S.H.; Kim, J.H. Performance evaluation of deep learning models for the classification and identification of dental implants. J. Prosthet. Dent. 2023; in press. [Google Scholar] [CrossRef] [PubMed]
- Alsomali, M.; Alghamdi, S.; Alotaibi, S.; Alfadda, S.; Altwaijry, N.; Alturaiki, I.; Al-Ekrish, A. Development of a deep learning model for automatic localization of radiographic markers of proposed dental implant site locations. Saudi Dent. J. 2022, 34, 220–225. [Google Scholar] [CrossRef] [PubMed]
- Kurtulus, I.L.; Lubbad, M.; Yilmaz, O.M.D.; Kilic, K.; Karaboga, D.; Basturk, A.; Akay, B.; Nalbantoglu, U.; Yilmaz, S.; Ayata, M.; et al. A robust deep learning model for the classification of dental implant brands. J. Stomatol. Oral Maxillofac. Surg. 2024, 8, 101818. [Google Scholar] [CrossRef]
- Wang, X.; Alqahtani, K.A.; Van den Bogaert, T.; Shujaat, S.; Jacobs, R.; Shaheen, E. Convolutional neural network for automated tooth segmentation on intraoral scans. BMC Oral Health 2024, 24, 804. [Google Scholar] [CrossRef]
- Al-Asali, M.; Alqutaibi, A.Y.; Al-Sarem, M.; Saeed, F. Deep learning-based approach for 3D bone segmentation and prediction of missing tooth region for dental implant planning. Sci. Rep. 2024, 14, 13888. [Google Scholar] [CrossRef] [PubMed]
- Fontenele, R.C.; Gerhardt, M.D.N.; Picoli, F.F.; Van Gerven, A.; Nomidis, S.; Willems, H.; Freitas, D.Q.; Jacobs, R. Convolutional neural network-based automated maxillary alveolar bone segmentation on cone-beam computed tomography images. Clin. Oral Implant. Res. 2023, 34, 565–574. [Google Scholar] [CrossRef]
- Oh, S.; Kim, Y.J.; Kim, J.; Jung, J.H.; Lim, H.J.; Kim, B.C.; Kim, K.G. Deep learning-based prediction of osseointegration for dental implant using plain radiography. BMC Oral Health 2023, 23, 208. [Google Scholar] [CrossRef] [PubMed]
- Moufti, M.A.; Trabulsi, N.; Ghousheh, M.; Fattal, T.; Ashira, A.; Danishvar, S. Developing an Artificial Intelligence Solution to Autosegment the Edentulous Mandibular Bone for Implant Planning. Eur. J. Dent. 2023, 17, 1330–1337. [Google Scholar] [CrossRef] [PubMed]
- Park, W.; Huh, J.K.; Lee, J.H. Automated deep learning for classification of dental implant radiographs using a large multi-center dataset. Sci. Rep. 2023, 13, 4862. [Google Scholar]
- Park, J.H.; Moon, H.S.; Jung, H.I.; Hwang, J.; Choi, Y.H.; Kim, J.E. Deep learning and clustering approaches for dental implant size classification based on periapical radiographs. Sci. Rep. 2023, 13, 16856. [Google Scholar] [CrossRef]
- Kim, H.S.; Ha, E.G.; Kim, Y.H.; Jeon, K.J.; Lee, C.; Han, S.S. Transfer learning in a deep convolutional neural network for implant fixture classification: A pilot study. Imaging Sci. Dent. 2022, 52, 219–224. [Google Scholar] [CrossRef] [PubMed]
- Sukegawa, S.; Yoshii, K.; Hara, T.; Tanaka, F.; Yamashita, K.; Kagaya, T.; Nakano, K.; Takabatake, K.; Kawai, H.; Nagatsuka, H.; et al. Is attention branch network effective in classifying dental implants from panoramic radiograph images by deep learning? PLoS ONE 2022, 17, e0269016. [Google Scholar] [CrossRef] [PubMed]
- Kong, H.J. Classification of dental implant systems using cloud-based deep learning algorithm: An experimental study. J. Yeungnam Med. Sci. 2023, 40, S29–S36. [Google Scholar] [CrossRef] [PubMed]
- Al-Sarem, M.; Al-Asali, M.; Alqutaibi, A.Y.; Saeed, F. Enhanced Tooth Region Detection Using Pretrained Deep Learning Models. Int. J. Environ. Res. Public. Health 2022, 19, 15414. [Google Scholar] [CrossRef] [PubMed]
- Altan, B.; Gunec, H.G.; Cinar, S.; Kutal, S.; Gulum, S.; Aydin, K.C. Detecting Prosthetic Restorations Using Artificial Intelligence on Panoramic Radiographs. Sci. Program. 2022, 2022, 6384905. [Google Scholar] [CrossRef]
- Sakai, T.; Li, H.; Shimada, T.; Kita, S.; Iida, M.; Lee, C.; Nakano, T.; Yamaguchi, S.; Imazato, S. Development of artificial intelligence model for supporting implant drilling protocol decision making. J. Prosthodont. Res. 2023, 67, 360–365. [Google Scholar] [CrossRef]
- Lyakhov, P.A.; Dolgalev, A.A.; Lyakhova, U.A.; Muraev, A.A.; Zolotayev, K.E.; Semerikov, D.Y. Neural network system for analyzing statistical factors of patients for predicting the survival of dental implants. Front. Neuroinform 2022, 16, 1067040. [Google Scholar] [CrossRef]
- Chau, R.C.W.; Hsung, R.T.; McGrath, C.; Pow, E.H.N.; Lam, W.Y.H. Accuracy of artificial intelligence-designed single-molar dental prostheses: A feasibility study. J. Prosthet. Dent. 2024, 131, 1111–1117. [Google Scholar] [CrossRef] [PubMed]
- Kosan, E.; Krois, J.; Wingenfeld, K.; Deuter, C.E.; Gaudin, R.; Schwendicke, F. Patients’ Perspectives on Artificial Intelligence in Dentistry: A Controlled Study. J. Clin. Med. 2022, 11, 2143. [Google Scholar] [CrossRef]
- Hamd, Z.; Elshami, W.; Al Kawas, S.; Aljuaid, H.; Abuzaid, M.M. A closer look at the current knowledge and prospects of artificial intelligence integration in dentistry practice: A cross-sectional study. Heliyon 2023, 9, e17089. [Google Scholar] [CrossRef]
- Ayad, N.; Schwendicke, F.; Krois, J.; van den Bosch, S.; Bergé, S.; Bohner, L.; Hanisch, M.; Vinayahalingam, S. Patients’ perspectives on the use of artificial intelligence in dentistry: A regional survey. Head. Face Med. 2023, 19, 23. [Google Scholar] [CrossRef] [PubMed]
- Roganović, J.; Radenković, M.; Miličić, B. Responsible Use of Artificial Intelligence in Dentistry: Survey on Dentists’ and Final-Year Undergraduates’ Perspectives. Healthcare 2023, 11, 1480. [Google Scholar] [CrossRef] [PubMed]
- Rokhshad, R.; Karteva, T.; Chaurasia, A.; Richert, R.; Mörch, C.; Tamimi, F.; Ducret, M. Artificial intelligence and smile design: An e-Delphi consensus statement of ethical challenges. J. Prosthodont. 2024, 33, 730–735. [Google Scholar] [CrossRef] [PubMed]
- Rajkumar, N.M.R.; Muzoora, M.R.; Thun, S. Dentistry and Interoperability. J. Dent. Res. 2022, 101, 1258–1262. [Google Scholar] [CrossRef] [PubMed]
- Rahim, A.; Khatoon, R.; Khan, T.A.; Syed, K.; Khan, I.; Khalid, T.; Khalid, B. Artificial intelligence-powered dentistry: Probing the potential, challenges, and ethicality of artificial intelligence in dentistry. Digit. Health 2024, 10, 20552076241291345. [Google Scholar] [CrossRef]
- Keskinbora, K.H. Medical ethics considerations on artificial intelligence. J. Clin. Neurosci. 2019, 64, 277–282. [Google Scholar] [CrossRef]
- Fiske, A.; Henningsen, P.; Buyx, A. Your Robot Therapist Will See You Now: Ethical Implications of Embodied Artificial Intelligence in Psychiatry, Psychology, and Psychotherapy. J. Med. Internet Res. 2019, 21, e13216. [Google Scholar] [CrossRef] [PubMed]
- Char, D.S.; Shah, N.H.; Magnus, D. Implementing Machine Learning in Health Care—Addressing Ethical Challenges. N. Engl. J. Med. 2018, 378, 981–983. [Google Scholar] [CrossRef]
- Mörch, C.M.; Atsu, S.; Cai, W.; Li, X.; Madathil, S.A.; Liu, X.; Mai, V.; Tamimi, F.; Dilhac, M.A.; Ducret, M. Artificial Intelligence and Ethics in Dentistry: A Scoping Review. J. Dent. Res. 2021, 100, 1452–1460. [Google Scholar] [CrossRef]
- Currie, G.; Hawk, K.E.; Rohren, E.M. Ethical principles for the application of artificial intelligence (AI) in nuclear medicine. Eur. J. Nucl. Med. Mol. Imaging 2020, 47, 748–752. [Google Scholar] [CrossRef] [PubMed]
- Hauser-Ulrich, S.; Künzli, H.; Meier-Peterhans, D.; Kowatsch, T. A Smartphone-Based Health Care Chatbot to Promote Self-Management of Chronic Pain (SELMA): Pilot Randomized Controlled Trial. JMIR Mhealth Uhealth 2020, 8, e15806. [Google Scholar] [CrossRef]
- Harishbhai Tilala, M.; Kumar Chenchala, P.; Choppadandi, A.; Kaur, J.; Naguri, S.; Saoji, R.; Devaguptapu, B. Ethical Considerations in the Use of Artificial Intelligence and Machine Learning in Health Care: A Comprehensive Review. Cureus 2024, 16, e62443. [Google Scholar] [CrossRef] [PubMed]
- Duggal, I.; Tripathi, T. Ethical principles in dental healthcare: Relevance in the current technological era of artificial intelligence. J. Oral. Biol. Craniofac Res. 2024, 14, 317–321. [Google Scholar] [CrossRef]
- Bertolaccini, L.; Falcoz, P.E.; Brunelli, A.; Batirel, H.; Furak, J.; Passani, S.; Szanto, Z. The significance of general data protection regulation in the compliant data contribution to the European Society of Thoracic Surgeons database. Eur. J. Cardiothorac. Surg. 2023, 64, ezad289. [Google Scholar] [CrossRef] [PubMed]
- Naik, N.; Hameed, B.M.Z.; Shetty, D.K.; Swain, D.; Shah, M.; Paul, R.; Aggarwal, K.; Ibrahim, S.; Patil, V.; Smriti, K.; et al. Legal and Ethical Consideration in Artificial Intelligence in Healthcare: Who Takes Responsibility? Front. Surg. 2022, 9, 862322. [Google Scholar] [CrossRef] [PubMed]
- Panch, T.; Mattie, H.; Atun, R. Artificial intelligence and algorithmic bias: Implications for health systems. J. Glob. Health 2019, 9, 010318. [Google Scholar] [CrossRef]
- Nazer, L.H.; Zatarah, R.; Waldrip, S.; Ke, J.X.C.; Moukheiber, M.; Khanna, A.K.; Hicklen, R.S.; Moukheiber, L.; Moukheiber, D.; Ma, H.; et al. Bias in artificial intelligence algorithms and recommendations for mitigation. PLoS Digit. Health 2023, 2, e0000278. [Google Scholar] [CrossRef]
- Di Martino, F.; Delmastro, F. Explainable AI for clinical and remote health applications: A survey on tabular and time series data. Artif. Intell. Rev. 2023, 56, 5261–5315. [Google Scholar] [CrossRef]
- Gerke, S.; Babic, B.; Evgeniou, T.; Cohen, I.G. The need for a system view to regulate artificial intelligence/machine learning-based software as medical device. NPJ Digit. Med. 2020, 3, 53. [Google Scholar] [CrossRef] [PubMed]
- Macrì, M.; D’Albis, V.; D’Albis, G.; Forte, M.; Capodiferro, S.; Favia, G.; Alrashadah, A.O.; García, V.D.; Festa, F. The Role and Applications of Artificial Intelligence in Dental Implant Planning: A Systematic Review. Bioengineering 2024, 11, 778. [Google Scholar] [CrossRef]
- Ducret, M.; Wahal, E.; Gruson, D.; Amrani, S.; Richert, R.; Mouncif-Moungache, M.; Schwendicke, F. Trustworthy Artificial Intelligence in Dentistry: Learnings from the EU AI Act. J. Dent. Res. 2024, 103, 1051–1056. [Google Scholar] [CrossRef] [PubMed]
- US Food and Drug Administration (FDA). Artificial Intelligence and Machine Learning (AI/ML)-Enabledmedical Devices. 2024. Available online: https://www.fda.gov/medical-devices/software-medical-device-samd/artificial-intelligence-and-machine-learning-aiml-enabled-medical-devices (accessed on 6 October 2024).


| Author, Year, and Country | Type of Study | Purpose of the Study | Total Number and Type of Dataset Utilized to Extract Data | AI Method | Method Used for Validation (Object Detection Algorithms) | Conclusion |
|---|---|---|---|---|---|---|
| Kurtulus et al. (2024) [14] Turkey | Retrospective | To evaluate the performance of deep learning techniques for classifying dental implant systems using panoramic radiographs. | 1258 panoramic radiographs from 6586 implant systems. | Convolutional neural network (CNN) models | VGG16, ResNet-50, EfficientNet, Vovnet 57, Vovnet 39, and ConvNeXt. | All the proposed CNN models demonstrated capability to accurately classify dental implant systems from panoramic radiographs. |
| Chau, R.C.W. et al. (2024) [29] Hong Kong | Feasibility | To evaluate the accuracy of a new AI system in designing biomimetic single-molar dental prostheses and compare them to natural molar teeth. | 169 participants | Convolutional neural network | 3D Generative Adversarial Network (GAN) | 3D GAN AI system successfully designed a single molar dental prosthesis that replicated the morphology of a naturally healthy tooth by learning the characteristics of the remaining dentition. |
| Wang et al. (2024) [15] Belgium | Retrospective | To evaluate the performance of a convolutional neural network (CNN) model for automatic tooth segmentation on intraoral scanner (IOS) images. | 761 IOS images (380 upper jaws, 381 lower jaws) by Trios 3Shape intraoral scanner | Convolutional neural network | 3D U-Net and CNN model | 3D U-Net pipeline outperformed current methods for automated tooth segmentation on IOS images by providing accurate, efficient, and consistent results. |
| Al-Asali M. et al. (2024) [16] Saudi Arabia | Retrospective | To use U-Net models to segment missing bone areas in CBCT scans and predict implant positions. | 150 CBCT images | Convolutional neural networks | U-net model 1 and 2 | These models offer promising automated dental implant planning for dental implantologists. |
| Kong, H.J. et al. (2023) Republic of Korea [12] | Retrospective | To assess deep learning models’ performance in classifying and identifying 103 dental implant designs using panoramic radiographs. | 14,037 images from Panoramic radiographs | Deep learning model | Versions 5 and 7 of You Only Look Once (YOLO) algorithm | A deep learning model for implant design achieved high performance, with mAP influenced by algorithm type, image processing, and design details. |
| Seok Oh et al. (2023) [18] Republic of Korea | Retrospective | To evaluate if deep learning can predict dental implant osseointegration using plain radiography. | Panoramic and periapical radiographs of 580 patients with 1206 implants | Deep learning model | ResNet-18,34,50, DenseNet-121,201 MobileNet-V2, and MobileNet-V3 | Deep learning can help predict dental implant osseointegration using plain radiography to some extent |
| Park et al. (2023) [20] Republic of Korea | Retrospective | To assess the accuracy of automated deep learning model for identifying and classifying various types of dental implant systems (DIS). | Panoramic images: 116,756 Periapical images: 40,209 Total combined images: 156,965 | Deep learning model | Automated DL algorithm | Automated deep learning demonstrated reliable classification accuracy with large datasets. However, no significant difference in accuracy between panoramic and periapical images was evident |
| Fontenele, C.R. et al. (2023) [17] Belgium | Retrospective | To develop and evaluate the efficacy of a new AI-driven CNN tool for automatically segmenting 3D maxillary alveolar bone from CBCT images. | 141 CBCT Scans | Convolutional neural network | Virtual Patient Creator | Manual segmentation was slightly better than the CNN-based tool. However, newly introduced tool had higher accuracy and was 116 times faster than the manual tool. |
| Kong, H.J. et al. (2023) Republic of Korea [24] | Retrospective | To assess the accuracy and clinical usability of implant system classification using automated machine learning on the Google Cloud platform. | 4800 periapical radiographs of 4 implant systems (Osstem TSIII, Osstem USII, Biomet 3i Osseotite External, and Dentsply Sirona Xive) | Deep machine | AutoML | The study demonstrated that AutoML AI model on a cloud platform is useful for the classification of dental implant systems with high accuracy. |
| Moufti, M.A. et al. (2023) [19] UAE | Retrospective | To develop and assess the efficacy of an AI tool to identify and outline areas of missing teeth on CBCT images before placing implants. | 43 CBCT images | Convolutional neural network | U-Net | The model demonstrated high accuracy in segmenting edentulous bone areas compared to human investigators, potentially reducing the time and cost of implant treatment through automated CBCT image analysis. |
| Park, J.H. et al. (2023) [21] Republic of Korea | Retrospective | To assess two AI methods for automatically classifying dental implant diameter and length from periapical radiographs. | 1320 images from 927 periapical radiographs and 874 patients | Deep learning and clustering analysis | Deep learning: VGG16 Clustering analysis: k-means++ algorithm | Both AI models demonstrated reliable classification performance. |
| Sakai, T. et al. (2023) [27] Japan | Retrospective | Develop an AI model to create a suitable implant drilling protocol from CBCT images. | 1200 | Convolutional neural network | LeNet-5 | The AI model effectively predicts drilling protocols from CBCT images before surgery, suggesting it could support decision-making for achieving primary stability. |
| Alsomali, M. et al. (2022) [13] Saudi Arabia | Retrospective | To develop an AI model that automatically locates radiographic stent gutta percha markers in CBCT images to identify implant sites for treatment planning. | 34 CBCT cases, 16,272 images | Deep learning neural network | Mask R-CNN | Training an AI program with only axial images is insufficient for accurate performance. |
| Lyakhov, P.A. et al. (2022) [28] Russia | Descriptive | To predict single implant survival rates using artificial intelligence. | 1646 patient histories (91.64% successful implant cases (1490), 8.36% rejection cases (136) | Convolutional neural network (CNN) | PyTorch machine learning framework | The proposed neural network system offers higher accuracy than similar systems by analyzing patient data. It can only predict single dental implant outcomes and cannot be considered a complete decision support tool. |
| Al-Sarem et al. (2022) [25] Saudi Arabia | Retrospective | To create and analyze a deep learning model that detects missing teeth positions from segmented CBCT images. | 500 CBCT images | Convolutional neural network (CNN) models | AlexNet, VGG16, VGG19, ResNet50, DenseNet169, and MobileNetV3 | Among the proposed DL models, DenseNet169 performed best and can be considered a promising, time-saving tool for automated dental implant planning. |
| Kim et al. (2022) [22] Republic of Korea | Retrospective | To assess transfer learning in a deep convolutional neural network for classifying implant fixtures. | 263 periapical radiographs with 355 implant fixtures | Deep convolutional neural network | YOLOv3 | Transfer learning with YOLOv3 enabled high performance even with a small amount of data. |
| Sukegawa, et al. (2022) [23] Yemen | Retrospective | To evaluate the performance of the attention branch network (ABN) for implant classification using convolutional neural networks (CNNs). | 10,191 dental implant images from digital panoramic radiographs (of 13 implant brands) | Convolutional neural network | ABN, ResNet 18,50,152 | ResNet18 with the ABN model reported excellent performance and high compatibility in dental implant classification. |
| Altan et al. (2022) [26] Turkey | Retrospective | To develop and evaluate CNN (convolutional neural network) to automatically detect prosthetic restorations in panoramic radiographs using deep learning. | 5126 panoramic radiographs (2988 crowns and 2969 bridges) | Convolutional neural network | YOLOv4 model | Prosthetic restorations were detected with high accuracy using the deep learning method. |
| Study | Selection | Comparability | Outcome | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Representativeness of the Exposed Cohort | Selection of the Nonexposed Cohort | Ascertainment of Exposure | Demonstration That Outcome of Interest Was Not Present at Start of Study | Control for Main Factor | Control for Additional Factor | Assessment of Outcome | Follow-up Long Enough for Outcomes to Occur | Adequacy of Follow-up of Cohorts | Total Scores | |
| Kurtulus et al. [14] | 0 | * | * | * | * | 0 | * | 0 | 0 | 5 |
| Chau, R.C.W. et al. [29] | 0 | * | * | * | * | 0 | * | 0 | 0 | 5 |
| Wang et al. [15] | 0 | * | * | * | * | 0 | * | 0 | 0 | 5 |
| Al Asali M. et al. [16] | 0 | * | * | * | * | 0 | * | 0 | 0 | 5 |
| Kong, H.J. et al. [12] | 0 | * | * | * | * | 0 | * | 0 | 0 | 5 |
| Seok Oh et al. [18] | * | * | * | * | * | 0 | * | 0 | 0 | 6 |
| Park et al. [20] | * | * | * | * | * | 0 | * | 0 | 0 | 6 |
| Fontenele, C.R. et al. [17] | * | 0 | * | * | * | 0 | * | 0 | 0 | 5 |
| Kong, H.J. et al. [24] | * | * | * | * | * | 0 | * | 0 | 0 | 6 |
| Moufti, M.A. et al. [19] | * | * | * | * | * | 0 | * | 0 | 0 | 6 |
| Park J H. et al. [21] | 0 | * | * | * | * | 0 | * | 0 | 0 | 5 |
| Sakai, T. et al. [27] | 0 | * | * | * | * | 0 | * | 0 | 0 | 5 |
| Alsomali, M. et al. [13] | 0 | * | * | * | * | 0 | * | 0 | 0 | 5 |
| Lyakhov, P.A. et al. [28] | 0 | * | * | * | * | 0 | * | 0 | 0 | 5 |
| Al-Sarem et al. [25] | 0 | 0 | * | * | * | 0 | * | 0 | 0 | 4 |
| Kim et al. [22] | 0 | * | * | * | * | 0 | * | 0 | 0 | 5 |
| Sukegawa et al. [23] | 0 | * | * | * | * | 0 | * | 0 | 0 | 5 |
| Altan et al. [26] | 0 | * | * | * | * | * | * | * | * | 8 |
| Author, Year, and Country | Type of Study | Objective | Sample Size | AI Used in Study | Conclusion | Ethical Issue Discussed |
|---|---|---|---|---|---|---|
| Hamd, Z.Y. et al. (2023), Saudi Arabia [31] | Cross-sectional study | Willingness, knowledge, and attitude of dental professionals and students regarding use of AI in dentistry | 134 | NA | 85.5% of dental professionals agreed on the importance of the role of AI in their practice while 31.3% stated that AI would threaten/disrupt their profession. | Professionals concerned using AI in clinical practice fearing error |
| Ayad, N. et al. (2023), Germany [32] | Observational study | Patient’s perception of AI in dentistry | 265 | DentalXrai Pro | 52.5% of the population had average or above-average knowledge of AI and 47.5% had no or below-average knowledge. But their overall perception was positive toward AI use in dentistry. | Patients concerned that AI may affect workforce need and trust between dentist and patient |
| Roganovi’c J et al. (2023) Serbia [33] | Cross-sectional survey | Dentist’s and final-year student’s familiarity and attitude toward AI use in dentistry | 193 | NA | The dentists as well as the students were skeptical about AI use. Students were more anxious fearing that AI could replace dentists and also regarding the lack of regulatory policies. | Dental professionals fearing AI replacing them in the future |
| Rokhshad, R. et al. (2023) Multiple countries [34] | Cross-sectional | To identify the ethical challenges in using AI for smile designing | 28 | NA | 53.6% of them had used smile designing software routinely or sometimes, 10.7% of them had used it rarely, and 35.7% had never used it. | Patient wellness, respect for autonomy, privacy protection, solidarity, governance, equity, diversity, expertise/prudence, accountability/responsibility, sustainability, and transparency |
| Kosan, E. et al. (2022), Germany [30] | Observational study | Patient’s perception of use of AI dentistry | 140 | DentalXrai | Patients showed positive perception toward use of AI in dentistry. They were able to understand what the dentist tried to explain more clearly with the help of AI. | Patients’ concern and fear about AI |
| Study | Selection | Comparability | Outcome | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Representativeness of the Exposed Cohort | Selection of the Nonexposed Cohort | Ascertainment of Exposure | Demonstration That Outcome of Interest Was Not Present at Start of Study | Control for Main Factor | Control for Additional Factor | Assessment of Outcome | Follow-up Long Enough for Outcomes to Occur | Adequacy of Follow-up of Cohorts | Total Scores | |
| Hamd, Z.Y. et al. [31] | 0 | * | * | * | 0 | 0 | * | 0 | 0 | 4 |
| Ayad, N. et al. [32] | 0 | * | * | * | 0 | 0 | * | 0 | 0 | 4 |
| Roganovic, J. et al. [33] | 0 | * | * | * | 0 | 0 | * | 0 | 0 | 4 |
| Rokhshad, R. et al. [34] | 0 | * | * | * | 0 | 0 | * | 0 | 0 | 4 |
| Kosan, E. et al. [30] | 0 | * | * | * | * | 0 | * | 0 | 0 | 5 |
| AI Technology | Description | Applications |
|---|---|---|
| Convolutional Neural Networks (CNNs) | Deep learning models specialized for image analysis, particularly in feature extraction and classification. | Classification of dental radiographs, implant system identification, and bone analysis. |
| Generative Adversarial Networks (GANs) | AI models designed for generating new data that mimics existing datasets. | Designing dental prostheses and simulating natural tooth morphology. |
| U-Net | A neural network architecture for image segmentation, especially for medical imaging tasks. | Tooth segmentation, bone segmentation, and implant site assessment from CBCT or 3D scans. |
| YOLO (You Only Look Once) | Object detection algorithm optimized for real-time processing and detection. | Detection of dental prosthetics, restorations, and implant fixtures in radiographic images. |
| ResNet (Residual Networks) | Deep learning architecture designed to overcome vanishing gradient problems in deep neural networks. | Osseointegration prediction and implant classification. |
| DenseNet (Dense Convolutional Networks) | AI models focus on efficient parameter sharing to improve performance with fewer computations. | Prediction of implant outcomes and bone density assessment. |
| Support Vector Machines (SVMs) | A supervised learning model for classification and regression analysis. | Classifying dental materials and differentiating between healthy and diseased tissue. |
| Random Forests | Ensemble learning techniques that combine multiple decision trees for classification and regression. | Predicting implant success rates and analyzing patient-specific prosthodontic outcomes. |
| Attention Mechanisms (e.g., Attention Branch Network) | Models that focus computational resources on relevant parts of input data for improved accuracy. | Dental implant classification and anomaly detection in imaging data. |
| 3D Neural Networks | Extensions of CNNs for analyzing volumetric data. | 3D segmentation of bone structures, implant planning, and prosthesis fitting. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alfaraj, A.; Nagai, T.; AlQallaf, H.; Lin, W.-S. Race to the Moon or the Bottom? Applications, Performance, and Ethical Considerations of Artificial Intelligence in Prosthodontics and Implant Dentistry. Dent. J. 2025, 13, 13. https://doi.org/10.3390/dj13010013
Alfaraj A, Nagai T, AlQallaf H, Lin W-S. Race to the Moon or the Bottom? Applications, Performance, and Ethical Considerations of Artificial Intelligence in Prosthodontics and Implant Dentistry. Dentistry Journal. 2025; 13(1):13. https://doi.org/10.3390/dj13010013
Chicago/Turabian StyleAlfaraj, Amal, Toshiki Nagai, Hawra AlQallaf, and Wei-Shao Lin. 2025. "Race to the Moon or the Bottom? Applications, Performance, and Ethical Considerations of Artificial Intelligence in Prosthodontics and Implant Dentistry" Dentistry Journal 13, no. 1: 13. https://doi.org/10.3390/dj13010013
APA StyleAlfaraj, A., Nagai, T., AlQallaf, H., & Lin, W.-S. (2025). Race to the Moon or the Bottom? Applications, Performance, and Ethical Considerations of Artificial Intelligence in Prosthodontics and Implant Dentistry. Dentistry Journal, 13(1), 13. https://doi.org/10.3390/dj13010013








