An Enigmatic Soft-Tissue Creeping Phenomenon: The Spontaneous Peri-Implant Mucosa Margin and Papilla Growth, Part Two—A Scientifically Supported Hypothesis Article
Abstract
1. Introduction
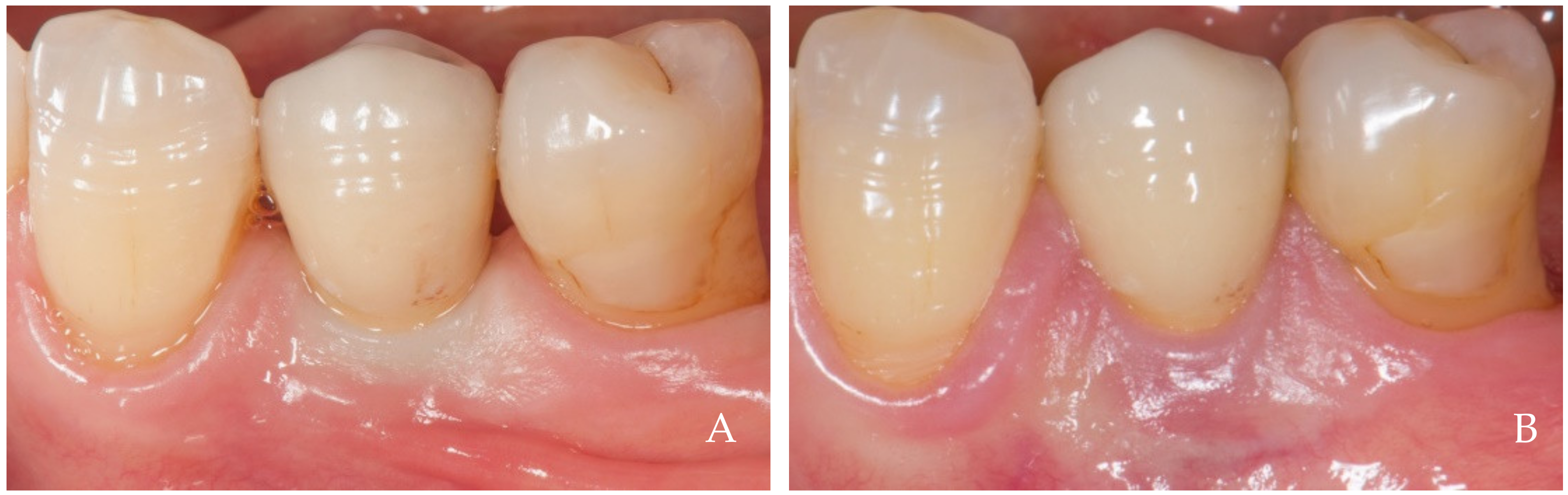
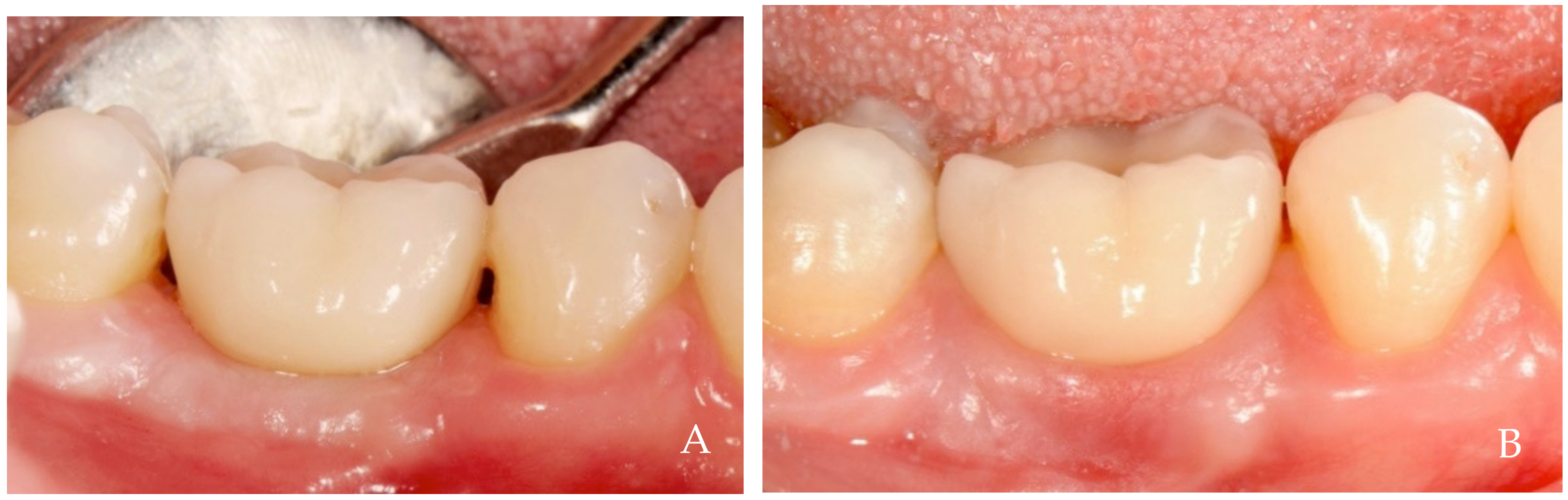
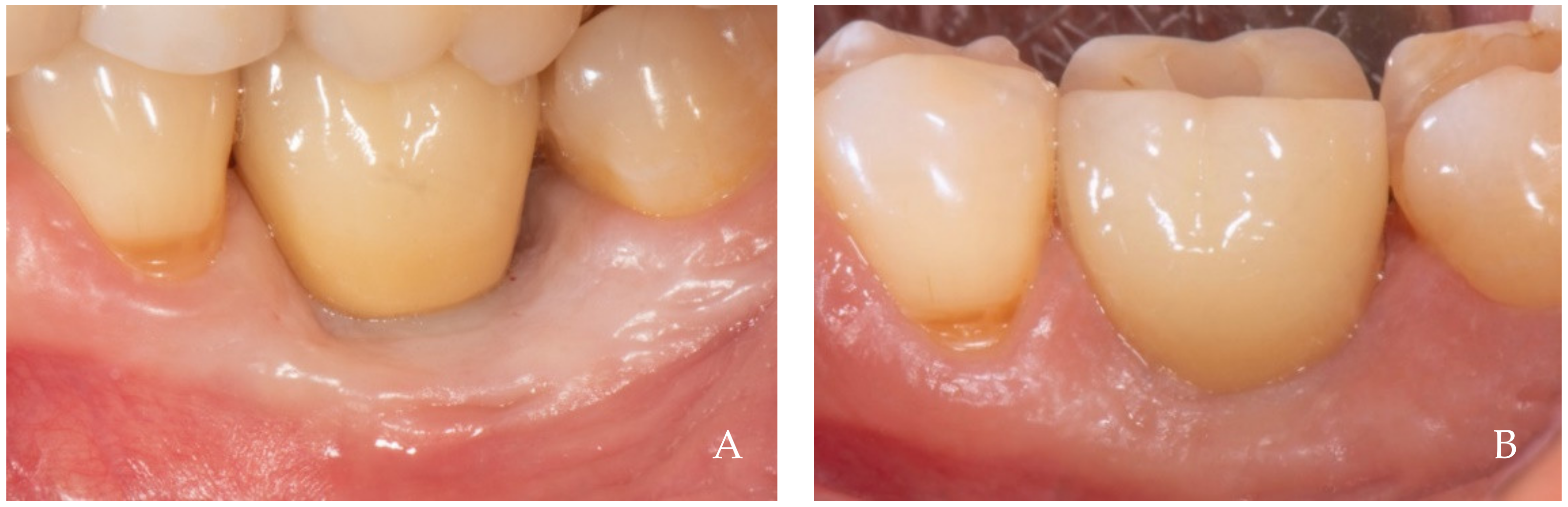
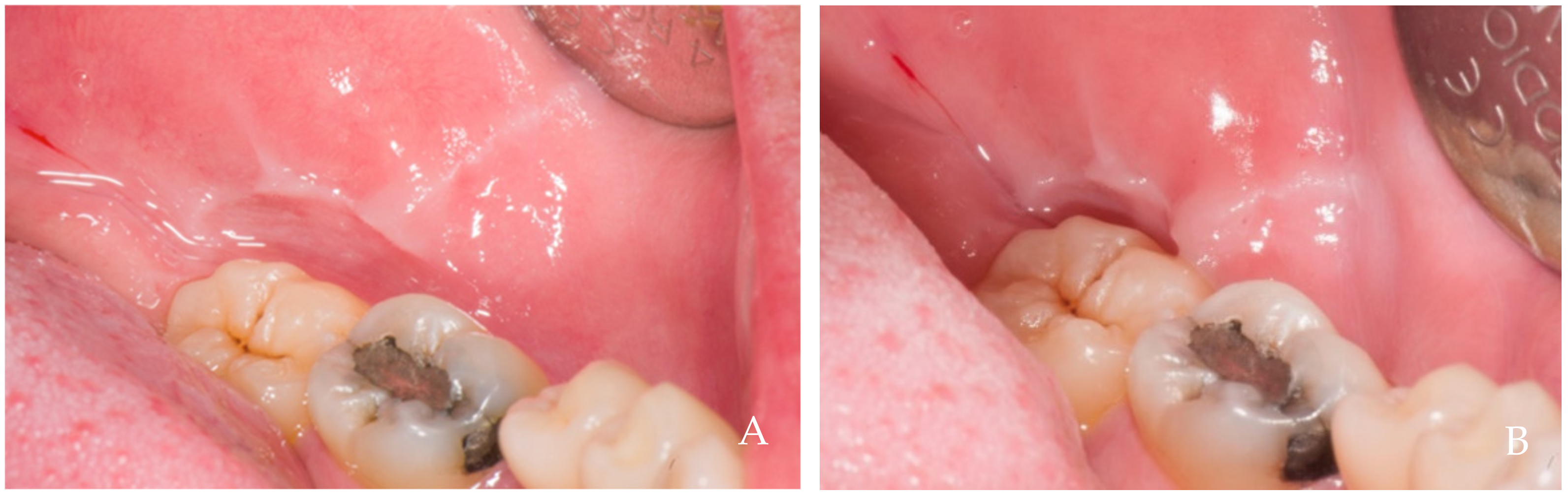
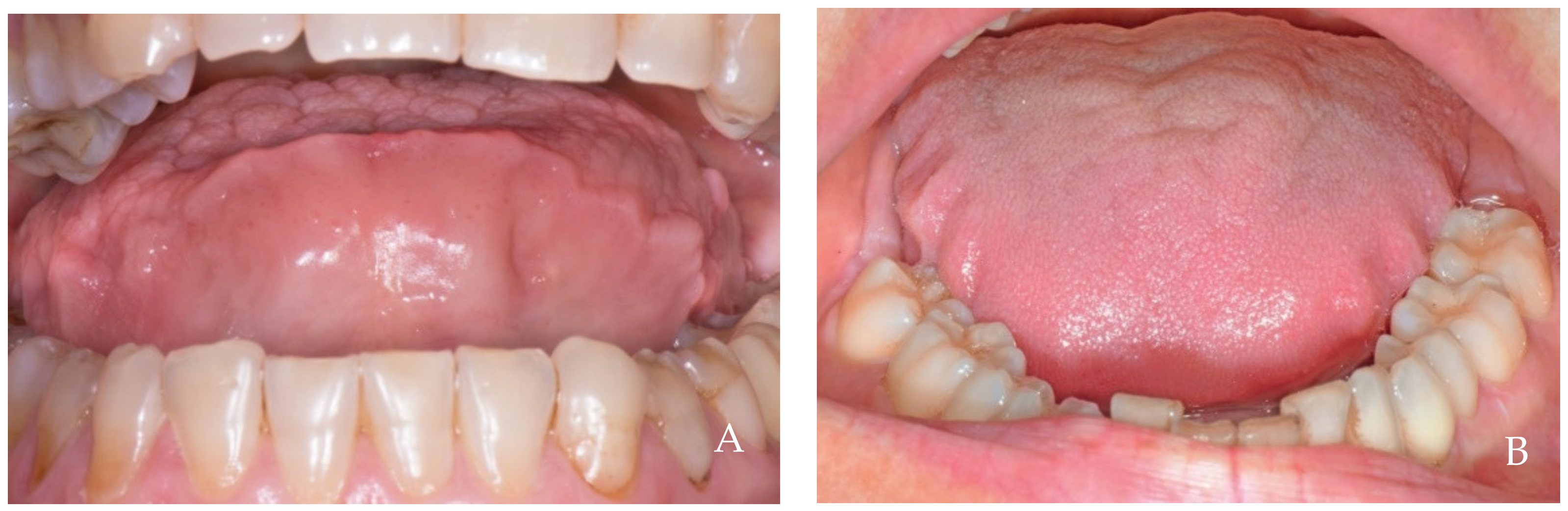
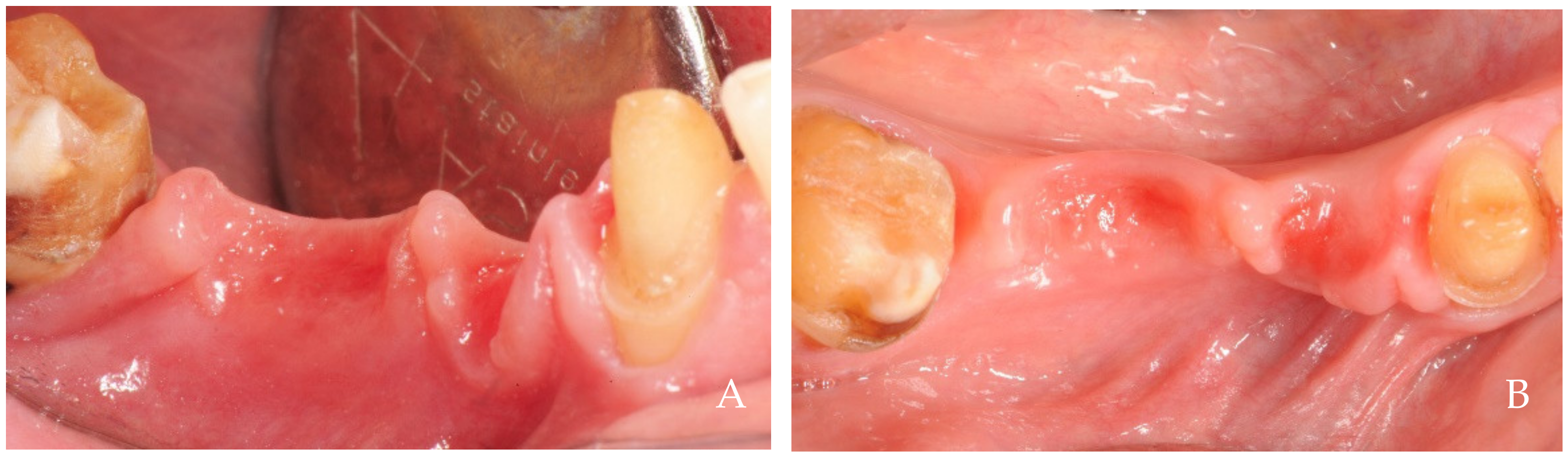
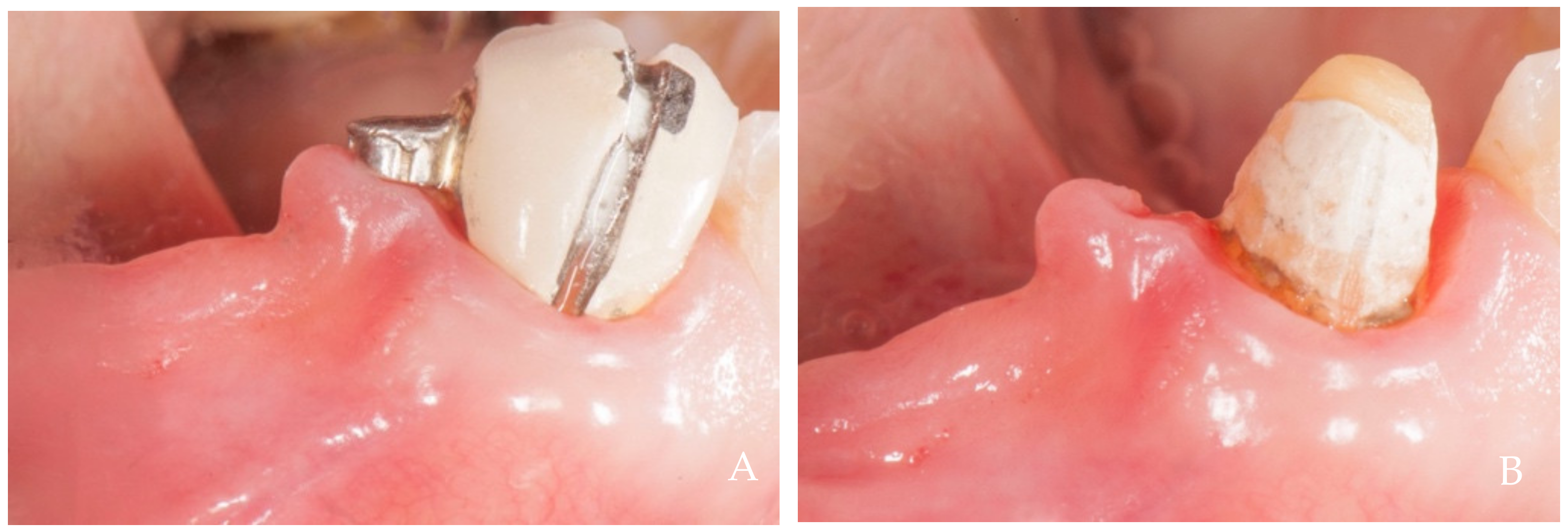
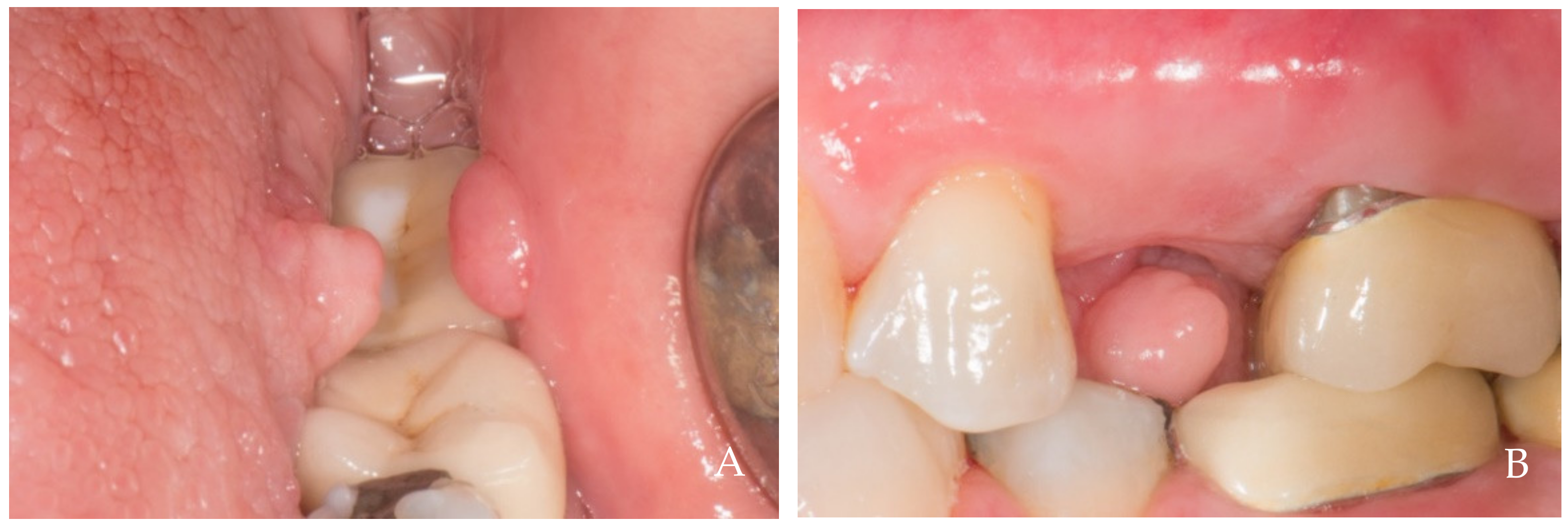
2. Clinical Examples of Oral Soft Tissue Growth
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Agabiti, I.; Apaza Alccayhuaman, K.A.; Nakajima, Y.; Botticelli, D. An enigmatic soft tissue creeping phenomenon: The spontaneous peri-implant mucosa margin and papilla growth. A retrospective clinical study. Clin. Exp. Dent. Res. 2021, 7, 474–483. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Tarnow, D.; Elian, N.; Fletcher, P.; Froum, S.; Magner, A.; Cho, S.; Salama, M.; Salama, H.; Garber, D.A. Vertical distance from the crest of bone to the height of the interproximal papilla between adjacent implants. J. Periodontol. 2003, 74, 1785–1788. [Google Scholar] [CrossRef]
- Chang, L.C. Factors associated with the interdental papilla height between two maxillary central incisors: A radiographic study. J. Periodontol. 2012, 83, 43–49. [Google Scholar] [CrossRef] [PubMed]
- Tarnow, D.P.; Cho, S.C.; Wallace, S.S. The effect of inter-implant distance on the height of inter-implant bone crest. J. Periodontol. 2000, 71, 546–549. [Google Scholar] [CrossRef]
- Cardaropoli, G.; Wennström, J.L.; Lekholm, U. Peri-implant bone alterations in relation to inter-unit distances. A 3-year retrospective study. Clin. Oral Implants Res. 2003, 14, 430–436. [Google Scholar] [CrossRef] [PubMed]
- Chang, M.; Wennström, J.L. Soft tissue topography and dimensions lateral to single implant-supported restorations. a cross-sectional study. Clin. Oral Implants Res. 2013, 24, 556–562. [Google Scholar] [CrossRef]
- Harster, P. Tissue modeling: The oral pump. Quintessence Int. 2005, 36, 633–640. [Google Scholar]
- Jemt, T. Regeneration of gingival papillae after single-implant treatment. Int. J. Periodontics Restor. Dent. 1997, 17, 326–333. [Google Scholar]
- Donders, F.C. Under den Mechanismus des Saugens. Pflug. Arch. 1875, 10, 91–94. [Google Scholar] [CrossRef]
- Körbitz, A. Kursus der Systematischen Orthodontik; Johann Ambrosius Barth: Leipzig, Germany, 1914. [Google Scholar]
- Barclay, A.E. The normal mechanism of swallowing. Brit. J. Radiol. 1930, 3, 534–546. [Google Scholar] [CrossRef]
- Noltemeier, H. Einführung in die Allgemeine Kiefer- und Gesichtsorthopädie; Buchdruckerei P. Dobler GmbH & Co KG.: Hannover, Germany, 1949. [Google Scholar]
- Eckert Möbius, A. Die Bedeutung der Zunge für die Nasen- und Mundatmung. Fortschritte Kieferorthopädie 1953, 14, 229–239. [Google Scholar] [CrossRef]
- Faigenblum, M.J. Negative oral pressures. A research report. Dent. Pract. Dent. Rec. 1966, 16, 214–216. [Google Scholar]
- Fränkel, R. A functional approach to orofacial orthopaedics. Br. J. Orthod. 1980, 7, 41–51. [Google Scholar] [CrossRef]
- Shaker, R.; Cook, I.J.; Dodds, W.J.; Hogan, W.J. Pressure-flow dynamics of the oral phase of swallowing. Dysphagia 1988, 3, 79–84. [Google Scholar] [CrossRef] [PubMed]
- Thuer, U.; Sieber, R.; Ingervall, B. Cheek and tongue pressure in the molar areas and the atmospheric pressure in the palatal vault in young adults. Eur. J. Orthod. 1999, 21, 299–309. [Google Scholar] [CrossRef]
- Kennedy, D.; Kieser, J.; Bolter, C.; Swain, M.; Singh, B.; Waddell, J.N. Tongue pressure patterns during water swallowing. Dysphagia 2010, 25, 11–19. [Google Scholar] [CrossRef]
- Engelke, W.; Jung, K.; Knosel, M. Intra-oral compartment pressures: A biofunctional model and experimental measurements under different conditions of posture. Clin. Oral Investig. 2011, 15, 165–176. [Google Scholar] [CrossRef]
- Hiraki, K.; Yamada, Y.; Kurose, M.; Ofusa, W.; Sugiyama, T.; Ishida, R. Application of a barometer for assessment of oral functions: Donders space. J. Oral Rehabil. 2017, 44, 65–72. [Google Scholar] [CrossRef] [PubMed]
- Engelke, W.G.; Mendoza, M.; Repetto, G. Preliminary radiographic observations of the tongue-repositioning manoeuvre. Eur. J. Orthod. 2006, 28, 618–623. [Google Scholar] [CrossRef] [PubMed]
- Santander, P.; Engelke, W.; Olthoff, A.; Völter, C. Intraoral pressure patterns during swallowing. Eur. Arch. Otorhinolaryngol. 2013, 270, 1019–1025. [Google Scholar] [CrossRef][Green Version]
- Morris, M.L. Artificial crown contours and gingival health. J. Prosthet. Dent. 1962, 12, 1146–1156. [Google Scholar] [CrossRef]
- Mew, J.R. The postural basis of malocclusion: A philosophical overview. Am. J. Orthod. Dentofac. Orthop. 2004, 126, 729–738. [Google Scholar] [CrossRef] [PubMed]
- Kieser, J.A.; Farland, M.G.; Jack, H.; Farella, M.; Wang, Y.; Rohrle, O. The role of oral soft tissues in swallowing function: What can tongue pressure tell us? Aust. Dent. J. 2014, 59 (Suppl. 1), 155–161. [Google Scholar] [CrossRef] [PubMed]
- Mosher, H.P. X-ray study of movements of the tongue, epiglottis and hyoid bone in swallowing, followed by a discussion of difficulty in swallowing caused by retropharyngeal diverticulum, post-cricoid webs and exostoses of cervical vertebrae. Laryngoscope 1927, 37, 235–262. [Google Scholar] [CrossRef]
- Vincent-Bugnas, S.; Borsa, L.; Gruss, A.; Lupi, L. Prioritization of predisposing factors of gingival hyperplasia during orthodontic treatment: The role of amount of biofilm. BMC Oral Health 2021, 21, 84. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kampe, T.; Tagdae, T.; Bader, G.; Edman, G.; Karlsson, S. Reported symptoms and clinical findings in a group of subjects with longstanding bruxing behavior. J. Oral Rehabil. 1997, 24, 581–587. [Google Scholar] [CrossRef] [PubMed]
- Long, J.H., Jr. A device to prevent jaw clenching. J. Prosthet. Dent. 1998, 79, 353–354. [Google Scholar] [CrossRef] [PubMed]
- Sapiro, S.M. Tongue indentations as an indicator of clenching. Clin. Prev. Dent. 1992, 14, 21–24. [Google Scholar]
- Morita, K.; Tsuka, H.; Kuremoto, K.I.; Kimura, H.; Kawano, H.; Yokoi, M.; Yasuda, K.; Yoshida, M.; Tsuga, K. Association between buccal mucosa ridging and oral feature/symptom and its effects on occlusal function among dentate young adults in a cross-sectional study of Japan. Cranio 2021, 39, 24–28. [Google Scholar] [CrossRef] [PubMed]
- Morita, K.; Mori, T.; Maruyama, M.; Hiraoka, A.; Higa, C.; Kuroki, A.; Yoshida, M.; Tsuga, K. Association between buccal mucosa ridging and oral or occlusal status among older people. Oral Dis. 2018, 24, 778–783. [Google Scholar] [CrossRef] [PubMed]
- Mizutani, S.; Ekuni, D.; Tomofuji, T.; Azuma, T.; Irie, K.; Machida, T.; Yoneda, T.; Iwasaki, Y.; Morita, M. Factors related to the formation of buccal mucosa ridging in university students. Acta Odontol. Scand. 2014, 72, 58–63. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Takagi, I.; Sakurai, K. Investigation of the factors related to the formation of the buccal mucosa ridging. J. Oral Rehabil. 2003, 30, 565–572. [Google Scholar] [CrossRef] [PubMed]
- Piquero, K.; Ando, T.; Sakurai, K. Buccal mucosa ridging and tongue indentation. Bull. Tokyo Dent. Coll. 1999, 40, 71–78. [Google Scholar] [CrossRef] [PubMed]
- Gould, M.S.; Picton, D.C. A study of pressures exerted by the lips and cheeks on the teeth of subjects with angle’s class II division 1, class II division 2 and class III malocclusions compared with those of subjects with normal occlusions. Arch. Oral Biol. 1968, 13, 527–541. [Google Scholar] [CrossRef]
- Yanagisawa, K.; Takagi, I.; Sakurai, K. Influence of tongue pressure and width on tongue indentation formation. J. Oral Rehabil. 2007, 34, 827–834. [Google Scholar] [CrossRef] [PubMed]




Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Agabiti, I.; Apaza Alccayhuaman, K.A.; Taniguchi, Z.; Kuwano, K.; Botticelli, D. An Enigmatic Soft-Tissue Creeping Phenomenon: The Spontaneous Peri-Implant Mucosa Margin and Papilla Growth, Part Two—A Scientifically Supported Hypothesis Article. Dent. J. 2024, 12, 216. https://doi.org/10.3390/dj12070216
Agabiti I, Apaza Alccayhuaman KA, Taniguchi Z, Kuwano K, Botticelli D. An Enigmatic Soft-Tissue Creeping Phenomenon: The Spontaneous Peri-Implant Mucosa Margin and Papilla Growth, Part Two—A Scientifically Supported Hypothesis Article. Dentistry Journal. 2024; 12(7):216. https://doi.org/10.3390/dj12070216
Chicago/Turabian StyleAgabiti, Ivo, Karol Alí Apaza Alccayhuaman, Zenzaburo Taniguchi, Kazuhisa Kuwano, and Daniele Botticelli. 2024. "An Enigmatic Soft-Tissue Creeping Phenomenon: The Spontaneous Peri-Implant Mucosa Margin and Papilla Growth, Part Two—A Scientifically Supported Hypothesis Article" Dentistry Journal 12, no. 7: 216. https://doi.org/10.3390/dj12070216
APA StyleAgabiti, I., Apaza Alccayhuaman, K. A., Taniguchi, Z., Kuwano, K., & Botticelli, D. (2024). An Enigmatic Soft-Tissue Creeping Phenomenon: The Spontaneous Peri-Implant Mucosa Margin and Papilla Growth, Part Two—A Scientifically Supported Hypothesis Article. Dentistry Journal, 12(7), 216. https://doi.org/10.3390/dj12070216







