The Evaluation of the Cervical Marginal Sealing of Direct vs. Indirect Composite Resin Restorations in MOD Cavities
Abstract
1. Introduction
2. Materials and Methods
2.1. Sample Preparation
2.2. Sample Preparation for Marginal Sealing Evaluation
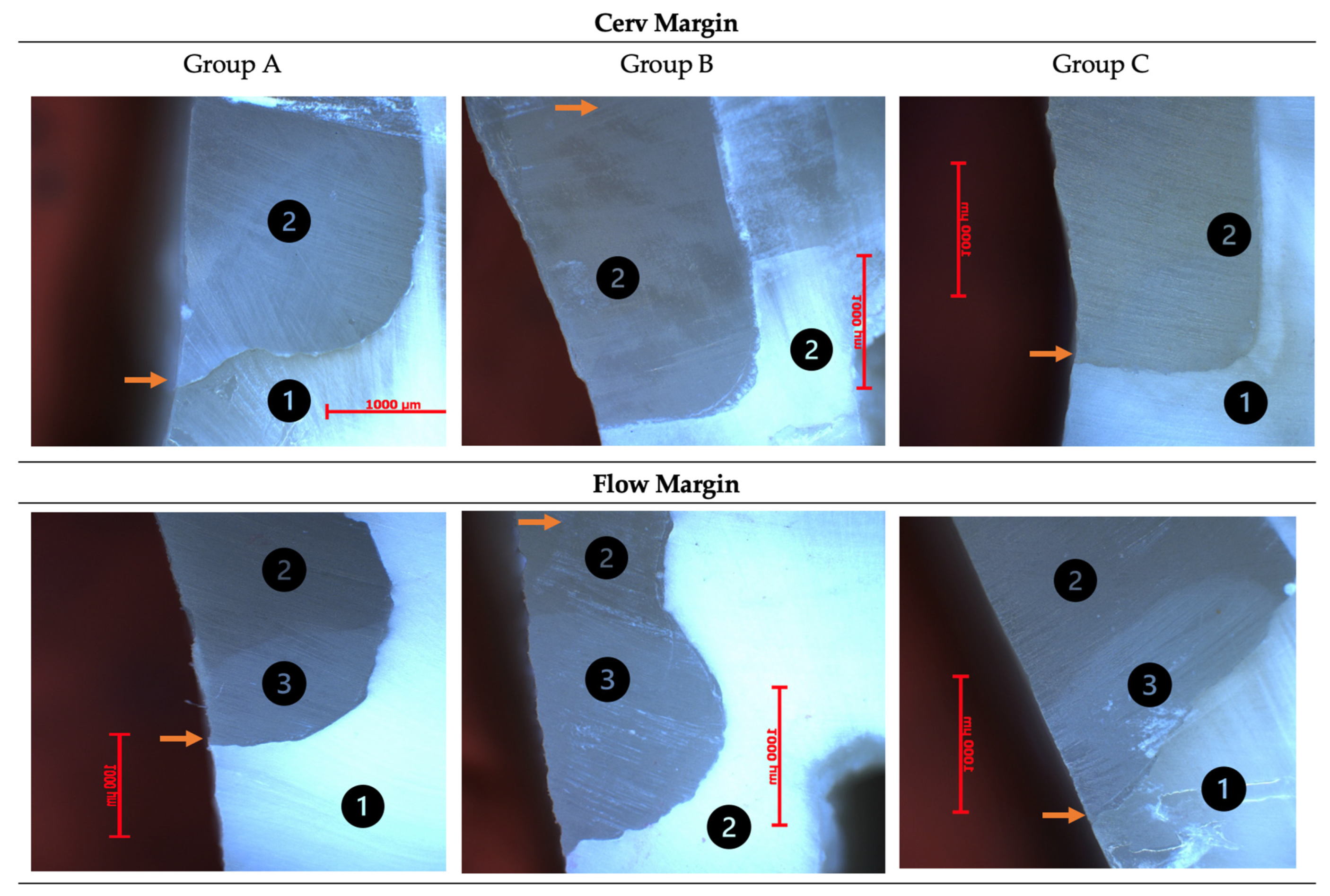
2.3. Evaluation of Marginal Sealing by Optical Microscopy
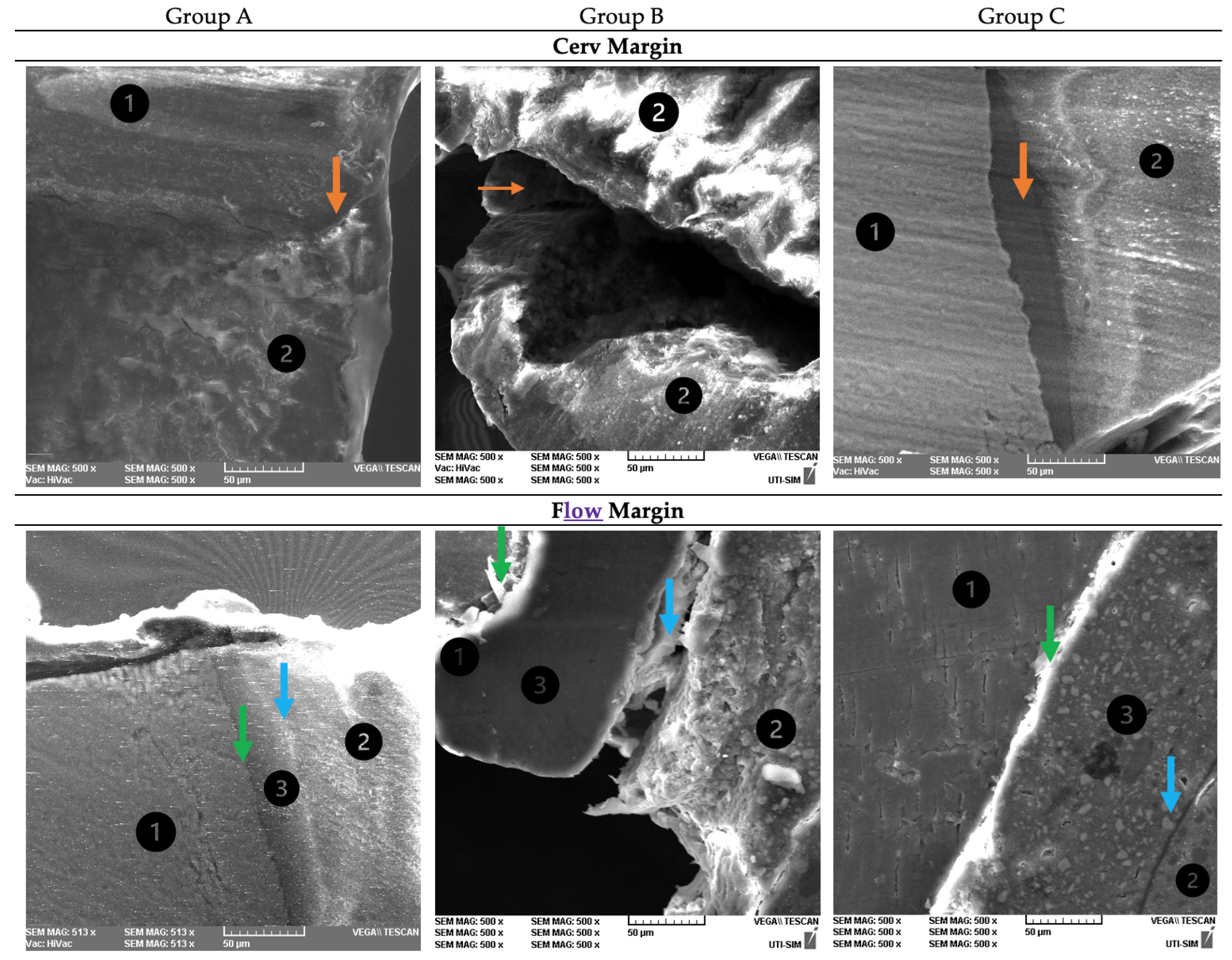
2.4. Evaluation of the Adhesive Interface by Scanning Electron Microscopy (SEM)
2.5. Statistical Analysis
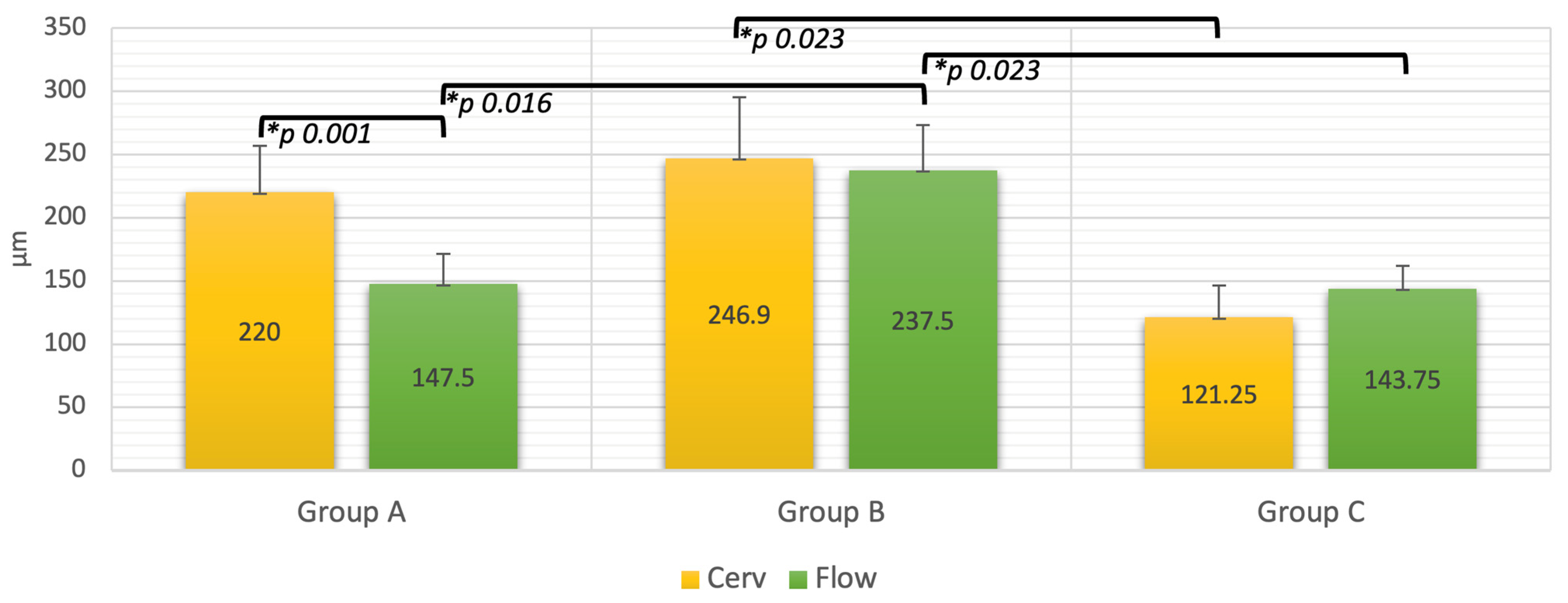
3. Results
4. Discussion
5. Conclusions
- Composite resin inlay mesio-occluso-distal restorations present a more effective marginal sealing compared to composite resin applied through the direct technique.
- The adaptation of the materials to cervical margins relocated using flow composite resin is less effective compared to the adaptation at the cervical margins without relocation in mesio-occluso-distal cavities restored by the direct technique, using the etch-and-rinse strategy.
- Relocation of the cervical margins using flow composite resin does not improve marginal adaptation.
- The adhesive strategy in direct restoration technique is not relevant for marginal sealing.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Frankenberger, R.; Sindel, J.; Kramer, N.; Petschelt, A. Dentin bond strength and marginal adaptation: Direct composite resins vs. ceramic inlays. Oper. Dent. 1999, 24, 147–155. [Google Scholar] [PubMed]
- Lange, R.T.; Pfeiffer, P. Clinical evaluation of ceramic inlays compared to composite restorations. Oper. Dent. 2009, 34, 263–272. [Google Scholar] [CrossRef] [PubMed]
- Angeletaki, F.; Gkogkos, A.; Papazoglou, E.; Kloukos, D. Direct versus indirect inlay/onlay composite restorations in posterior teeth. A systematic review and meta-analysis. J. Dent. 2016, 53, 12–21. [Google Scholar] [CrossRef] [PubMed]
- Dejak, B.; Młotkowski, A. A comparison of stresses in molar teeth restored with inlays and direct restorations, including polymerization shrinkage of composite resin and tooth loading during mastication. Dent. Mater. 2015, 31, 77–87. [Google Scholar] [CrossRef] [PubMed]
- Watts, D.C.; Satterthwaite, J.D. Axial shrinkage-stress depends upon both C-factor and composite mass. Dent. Mater. 2008, 24, 1–8. [Google Scholar] [CrossRef]
- Ghiorghe, C.A.; Iovan, G.; Andrian, S.; Nica, I.; Topoliceanu, C.; Pancu, G. Studies on Adhesion of Composite Resins and Glass-Ionomer Cements in Open-Sandwich Technique. Rev. Chim. 2017, 68, 1890–1894. [Google Scholar] [CrossRef]
- Pallesen, U.; Qvist, V. Composite resin fillings and inlays. An 11-year evaluation. Clin. Oral Investig. 2003, 7, 71–79. [Google Scholar] [CrossRef] [PubMed]
- Forster, A.; Braunitzer, G.; Tóth, M.; Szabó, B.P.; Fráter, M. In vitro fracture resistance of adhesively restored molar teeth with different MOD cavity dimensions. J. Prosthodont. 2019, 28, 325–331. [Google Scholar] [CrossRef] [PubMed]
- Satterthwaite, J.D.; Vogel, K.; Watts, D.C. Effect of resin-composite filler particle size and shape on shrinkage-strain. Dent. Mater. 2009, 25, 1612–1615. [Google Scholar] [CrossRef]
- Murariu, A.L.; Dinu, C.; Forna, D.A.; Stefanescu, V.; Topor, G.; Forna, N.C.; Fotea, S.; Gurau, G.; Iordache, C. Composite Resins-Multifunctional Restorative Material and Practical Approaches in Dental Field. Mater. Plast. 2020, 57, 276–284. [Google Scholar] [CrossRef]
- Deliperi, S.; Bardwell, D.N. An alternative method to reduce polymerization shrinkage in direct posterior composite restorations. J. Am. Dent. Assoc. 2002, 133, 1387–1398. [Google Scholar] [CrossRef] [PubMed]
- Cramer, N.B.; Stansbury, J.W.; Bowman, C.N. Recent advances and developments in composite dental restorative materials. J. Dent. Res. 2011, 90, 402–416. [Google Scholar] [CrossRef] [PubMed]
- Tatarciuc, M.; Maftei, G.A.; Vitalariu, A.; Luchian, I.; Martu, I.; Diaconu-Popa, D. Inlay-Retained Dental Bridges—A Finite Element Analysis. Appl. Sci. 2021, 11, 3770. [Google Scholar] [CrossRef]
- Boaro, L.C.; Goncalves, F.; Guimarães, T.C.; Ferracane, J.L.; Versluis, A.; Braga, R.R. Polymerization stress, shrinkage and elastic modulus of current low-shrinkage restorative composites. Dent. Mater. 2010, 12, 1144–1150. [Google Scholar] [CrossRef] [PubMed]
- Neppelenbroek, K.H. The clinical challenge of achieving marginal adaptation in direct and indirect restorations. J. Appl. Oral Sci. 2015, 23, 448–449. [Google Scholar] [CrossRef] [PubMed]
- Şenol, A.A.; Atali, P.Y.; Kahramanoğlu, E. Microleakage and Marginal Integrity of Direct and Indirect Composite Resin Restorations in MOD Cavities After Thermo-Mechanical Loading. Clin. Exp. Health Sci. 2021, 11, 564–574. [Google Scholar] [CrossRef]
- Taraboanta, I.; Stoleriu, S.; Iovan, G.; Moldovanu, A.; Georgescu, A.; Negraia, M.; Andrian, S. Evaluation of pre-heating effects on marginal adaptation of resin-based materials. Mater. Plast. 2018, 55, 238–242. [Google Scholar] [CrossRef]
- Erdilek, D.; Dörter, C.; Koray, F.; Kunzelmann, K.H.; Efes, B.G.; Gomec, Y. Effect of thermo-mechanical load cycling on microleakage in class II ormocer restorations. Eur. J. Dent. 2009, 3, 200–205. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Tjaderhane, L. Dentin Bonding: Can We Make it Last? Oper. Dent. 2015, 40, 4–18. [Google Scholar] [CrossRef]
- Kozma, A.; Bodnar, C.; Dobre, M.; Agop-Forna, D.; Topoliceanu, C.; Lăzărescu, H.; Forna, N. The recovery of the esthetic and masticatory functions by minimal invazive restorations: A review. Rom. J. Oral Rehabil. 2019, 11, 15–21. [Google Scholar]
- Van Ende, A.; De Munck, J.; Mine, A.; Lambrechts, P.; Van Meerbeek, B. Does a low-shrinking composite induce less stress at the adhesive interface? Dent. Mater. 2010, 26, 215–222. [Google Scholar] [CrossRef] [PubMed]
- Sharma, S.; Padda, B.K.; Choudhary, V. Comparative evaluation of residual monomer content and polymerization shrinkage of a packable composite and an ormocer. J. Conserv. Dent. 2012, 15, 161–165. [Google Scholar] [CrossRef] [PubMed]
- Mendonça, J.S.; Neto, R.G.; Santiago, S.L.; Lauris, J.R.; Navarro, M.F.; de Carvalho, R.M. Direct resin composite restorations versus indirect composite inlays: One-year results. J. Contemp. Dent. Pract. 2010, 11, 25–32. [Google Scholar] [CrossRef]
- da Rosa Rodolpho, P.A.; Cenci, M.S.; Donassollo, T.A.; Loguércio, A.D.; Demarco, F.F. A clinical evaluation of posterior composite restorations: 17-year findings. J. Dent. 2006, 34, 427–435. [Google Scholar] [CrossRef] [PubMed]
- Spreafico, R.C.; Krejci, I.; Dietschi, D. Clinical performance and marginal adaptation of class II direct and semidirect composite restorations over 3.5 years in vivo. J. Dent. 2005, 33, 499–507. [Google Scholar] [CrossRef]
- Wassell, R.W.; Walls, A.W.; McCabe, J.F. Direct composite inlays versus conventional composite restorations: 5-year follow-up. J. Dent. 2000, 28, 375–382. [Google Scholar] [CrossRef]
- Barone, A.; Derchi, G.; Rossi, A.; Marconcini, S.; Covani, U. Longitudinal clinical evaluation of bonded composite inlays: A 3-year study. Quintessence Int. 2008, 39, 65. [Google Scholar]
- Garapati, S.; Das, M.; Mujeeb, A.; Dey, S.; Kiswe, S.P. Cuspal movement and microleakage in premolar teeth restored with posterior restorative materials. J. Int. Oral Health 2014, 6, 47. [Google Scholar] [PubMed]
- Tărăboanță, I.; Stoleriu, S.; Gurlui, S.; Nica, I.; Tărăboanță-Gamen, A.C.; Iovan, A.; Andrian, S. The Influence of Abrasive and Acidic Aggressions on the Surface Condition of Flow Composite Resin. Materials 2022, 15, 1000. [Google Scholar] [CrossRef]
- Hodobet, C.; Pangica, A.M.; Florescu, A.; Hancu, V.; Biclesanu, C.F. In vitro Comparative study on the marginal adaptation of direct, semi-direct and indirect composite resins restorations to dentine and dental cementum. Rev. Chim. 2018, 69, 3138–3145. [Google Scholar] [CrossRef]
- Fronza, B.M.; Rueggeberg, F.A.; Braga, R.R.; Mogilevych, B.; Soares, L.E.; Martin, A.A.; Ambrosano, G.; Giannini, M. Monomer conversion, microhardness, internal marginal adaptation, and shrinkage stress of bulk-fill resin composites. Dent Mater 2015, 31, 1542–1551. [Google Scholar] [CrossRef]
- Juloski, J.; Köken, S.; Ferrari, M. Cervical margin relocation in indirect adhesive restorations: A literature review. J. Prosthodont. Res. 2018, 62, 273–280. [Google Scholar] [CrossRef] [PubMed]
- Cicciù, M.; Fiorillo, L.; D’Amico, C.; Gambino, D.; Amantia, E.M.; Laino, L.; Crimi, S.; Campagna, P.; Bianchi, A.; Herford, A.S.; et al. 3D digital impression systems compared with traditional techniques in dentistry: A recent data systematic review. Materials 2020, 13, 1982. [Google Scholar] [CrossRef] [PubMed]
- Kalra, S.; Singh, A.; Gupta, M.; Chadha, V. Ormocer: An aesthetic direct restorative material; An in vitro study comparing the marginal sealing ability of organically modified ceramics and a hybrid composite using an ormocer-based bonding agent and a conventional fifth-generation bonding agent. Contemp. Clin. Dent. 2012, 3, 48. [Google Scholar] [CrossRef] [PubMed]
- Fleming, G.J.; Hall, D.P.; Shortall, A.C.; Burke, F.J. Cuspal movement and microleakage in premolar teeth restored with posterior filling materials of varying reported volumetric shrinkage values. J. Dent. 2005, 33, 139–146. [Google Scholar] [CrossRef] [PubMed]
- Manchorova-Veleva, N.A.; Vladimirov, S.B.; Keskinova, D.A. Clinical Effect of Dental Adhesive on Marginal Integrity in Class I And Class II Resin-Composite Restorations. Folia Med. 2015, 57, 250–256. [Google Scholar] [CrossRef][Green Version]
- Bhatti, U.A. The phenomenon of postoperative sensitivity and composite restorations—A review. J. Pak. Dent. Assoc. 2019, 28, 33–40. [Google Scholar] [CrossRef]
- Bhatti, U.A.; Ahmed, A.; Javed, Q. Frequency of postoperative sensitivity in posterior class I composite restorations. Pak. Oral Dent. J. 2014, 34, 532–535. [Google Scholar]
- Baldi, A.; Comba, A.; Michelotto Tempesta, R.; Carossa, M.; Pereira, G.K.; Valandro, L.F.; Paolone, G.; Vichi, A.; Goracci, C.; Scotti, N. External marginal gap variation and residual fracture resistance of composite and lithium-silicate CAD/CAM overlays after cyclic fatigue over endodontically-treated molars. Polymers 2021, 13, 3002. [Google Scholar] [CrossRef]

 .
.
 .
.
 ; flowable composite-dentin: green arrow
; flowable composite-dentin: green arrow  ; conventional composite-flowable composite blue arrow
; conventional composite-flowable composite blue arrow  .
.
 ; flowable composite-dentin: green arrow
; flowable composite-dentin: green arrow  ; conventional composite-flowable composite blue arrow
; conventional composite-flowable composite blue arrow  .
.
| Etching Technique | Phosphoric Acid Application | Adhesive Application |
|---|---|---|
| Etch-and-rinse | The acid was applied on the exposed dentin for 15 s, then was rinsed for 15 s with water and air-dried for 5 s using the air-spray from the dental unit. | The adhesive was applied on the air-dried surface for 20 s using an adhesive tip applicator with a rubbing action. Then, a slight air pressure was applied for 5 s and the adhesive was light cured for 20 s. |
| Self-etch | Phosphoric acid was not applied. |
| Name | Type | Manufacturer | Composition |
|---|---|---|---|
| Miris 2 | Nanohybrid composite resin | Coltène Whaledent, Altstaetten, Switzerland | Barium alumino fluoride glass, BisGMA, TEGDMA, UDMA |
| ScotchBond Universal | Adhesive resin | 3M ESPE, St. Paul, MN, USA | Methacryloyloxydecyl, dihydrogen phosphate, phosphate monomer, dimethacrylate resin, hydroxyethyl methacrylate, methacrylate-modified alkenoic acid copolymer, filler, ethanol, water, initiators, silane |
| Enamel Plus HRi Flow | Flow composite resin | Micerium, Avegno, GE, Italy | BisGMA, UDMA, 1,4-butandiol-dimethacrylate, highly dispersed silicone dioxide 53%vol |
| Rely X Unicem | Self-adhesive resin cement | 3M ESPE, St. Paul, MN, USA | Methacrylated phosphoric acid esters, TEGDMA, substituted dimethacrylate, silanized glass powder, silane treated silica, sodium persulfate, substituted pyrimidine, calcium hydroxide, 72%wt |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tiron, B.; Forna, N.C.; Tărăboanță, I.; Stoleriu, S.; Topoliceanu, C.; Sălceanu, M.; Brânzan, R.; Iovan, G. The Evaluation of the Cervical Marginal Sealing of Direct vs. Indirect Composite Resin Restorations in MOD Cavities. Dent. J. 2024, 12, 92. https://doi.org/10.3390/dj12040092
Tiron B, Forna NC, Tărăboanță I, Stoleriu S, Topoliceanu C, Sălceanu M, Brânzan R, Iovan G. The Evaluation of the Cervical Marginal Sealing of Direct vs. Indirect Composite Resin Restorations in MOD Cavities. Dentistry Journal. 2024; 12(4):92. https://doi.org/10.3390/dj12040092
Chicago/Turabian StyleTiron, Bianca, Norina Consuela Forna, Ionuț Tărăboanță, Simona Stoleriu, Claudiu Topoliceanu, Mihaela Sălceanu, Răzvan Brânzan, and Gianina Iovan. 2024. "The Evaluation of the Cervical Marginal Sealing of Direct vs. Indirect Composite Resin Restorations in MOD Cavities" Dentistry Journal 12, no. 4: 92. https://doi.org/10.3390/dj12040092
APA StyleTiron, B., Forna, N. C., Tărăboanță, I., Stoleriu, S., Topoliceanu, C., Sălceanu, M., Brânzan, R., & Iovan, G. (2024). The Evaluation of the Cervical Marginal Sealing of Direct vs. Indirect Composite Resin Restorations in MOD Cavities. Dentistry Journal, 12(4), 92. https://doi.org/10.3390/dj12040092








