Is a White Diet Necessary for Tooth Bleaching Procedures? A Systematic Review and Meta-Analysis
Abstract
1. Introduction
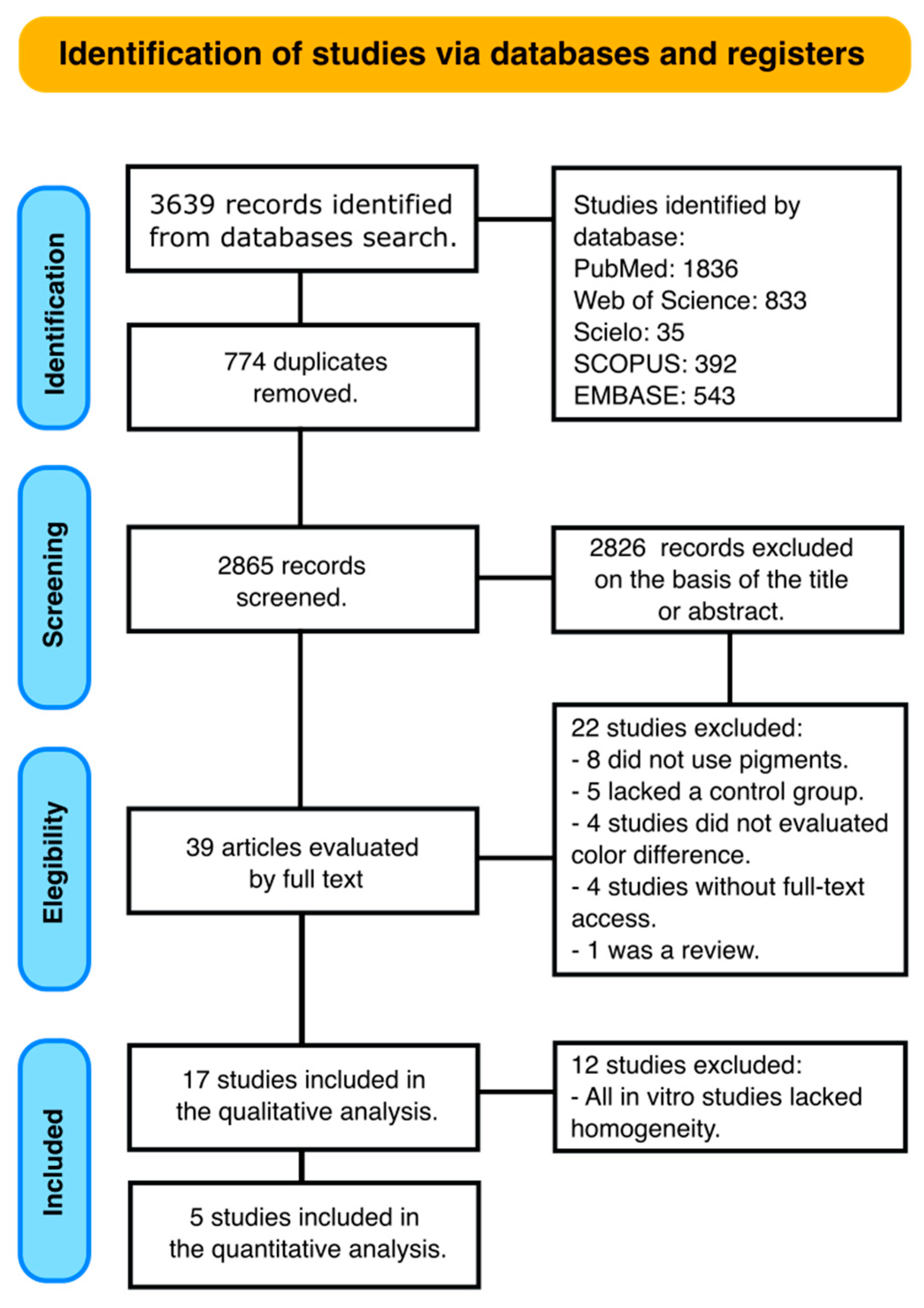
2. Materials and Methods
2.1. Data Sources
2.2. Search Strategy
2.3. Eligibility Criteria
2.4. Data Extraction
2.5. Quality Assessment
2.6. Statistical Analysis
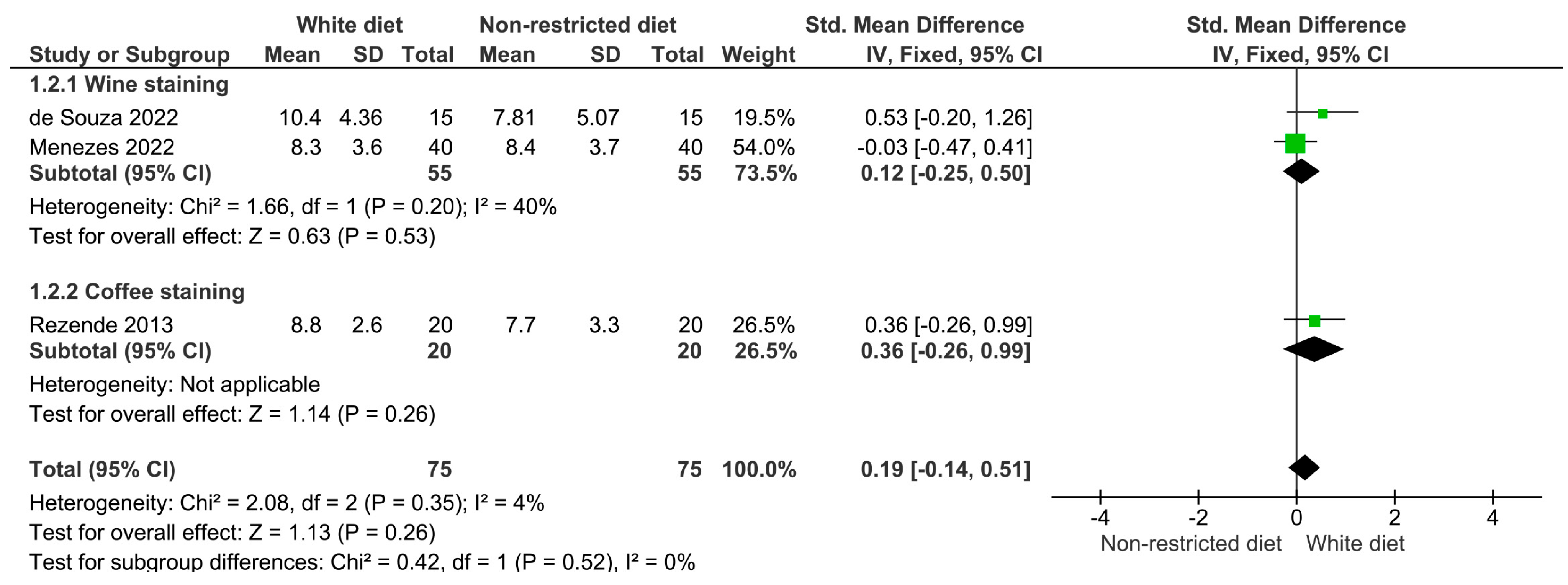
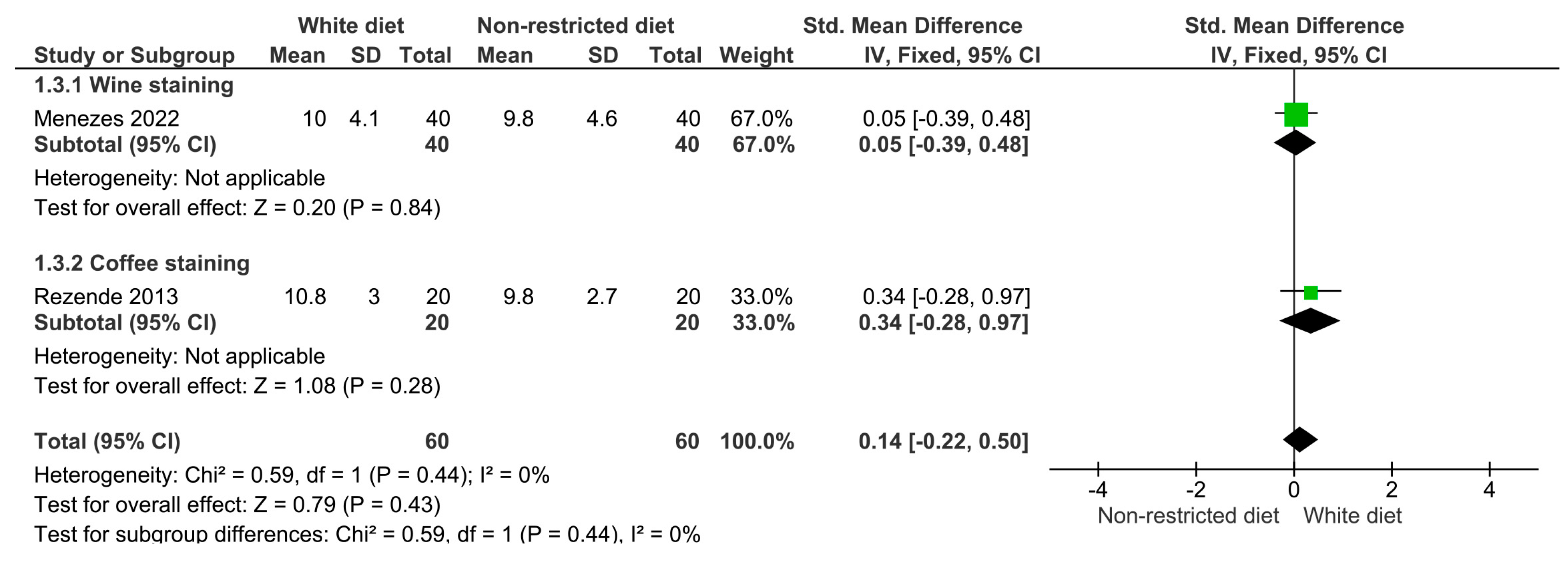
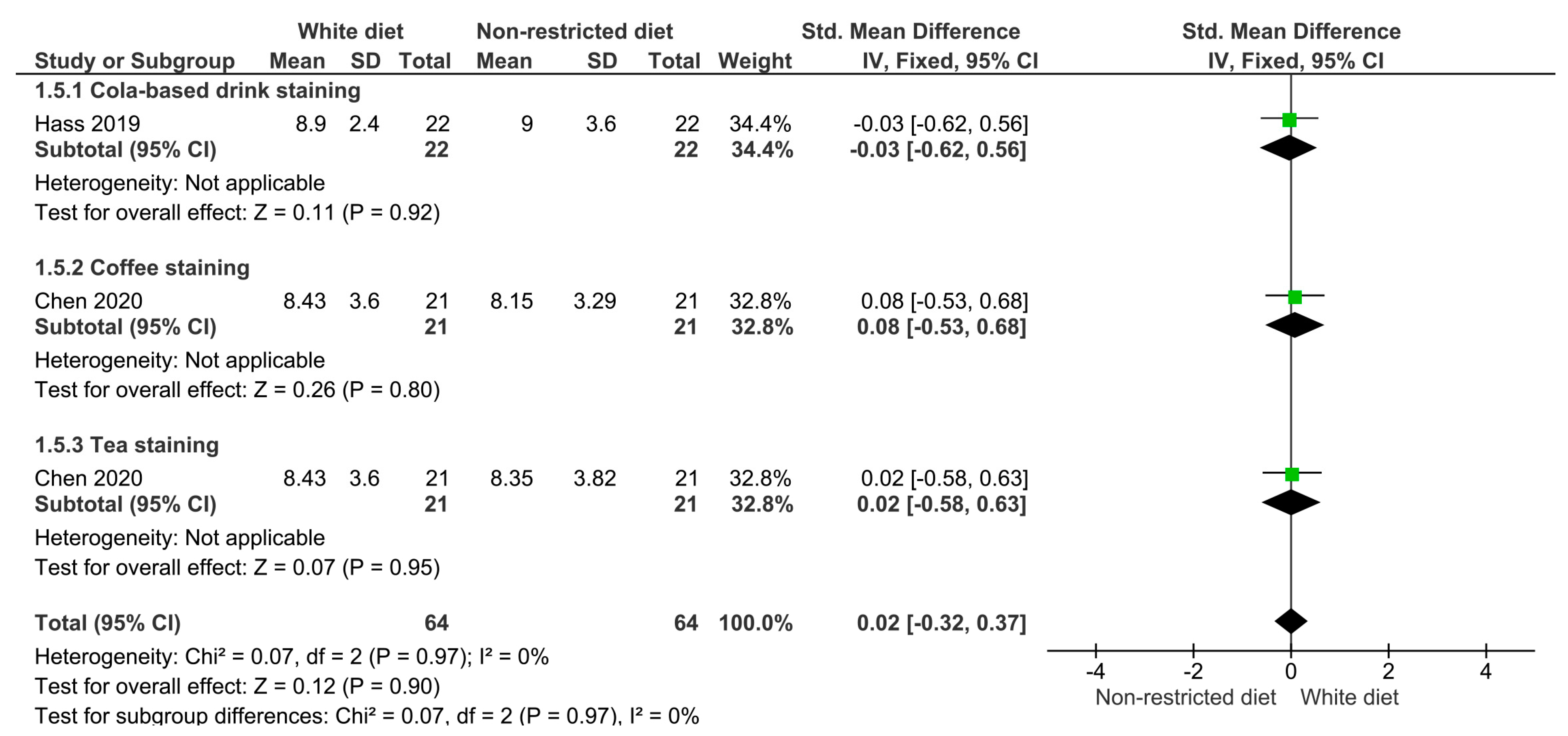
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kose, C.; Calixto, A.L.; Bauer, J.R.O.; Reis, A.; Loguercio, A.D. Comparison of the Effects of In-Office Bleaching Times on Whitening and Tooth Sensitivity: A Single Blind, Randomized Clinical Trial. Oper. Dent. 2016, 41, 138–145. [Google Scholar] [CrossRef] [PubMed]
- Carey, C.M. Tooth Whitening: What We Now Know. J. Evid. Based Dent. Pract. 2014, 14, 70–76. [Google Scholar] [CrossRef] [PubMed]
- Karadas, M.; Tahan, E.; Demirbuga, S.; Seven, N. Influence of Tea and Cola on Tooth Color after Two In-Office Bleaching Applications. J. Restor. Dent. 2014, 2, 83. [Google Scholar] [CrossRef]
- Côrtes, G.; Pini, N.P.; Lima, D.A.N.L.; Liporoni, P.C.S.; Munin, E.; Ambrosano, G.M.B.; Aguiar, F.H.B.; Lovadino, J.R. Influence of Coffee and Red Wine on Tooth Color during and after Bleaching. Acta Odontol. Scand. 2013, 71, 1475–1480. [Google Scholar] [CrossRef] [PubMed]
- Minoux, M.; Serfaty, R. Vital Tooth Bleaching: Biologic Adverse Effects—A Review. Quintessence Int. 2008, 39, 645–659. [Google Scholar] [PubMed]
- Addy, M.; Moran, J. Mechanisms of Stain Formation on Teeth, in Particular Associated with Metal Ions and Antiseptics. Adv. Dent. Res. 1995, 9, 450–456. [Google Scholar] [CrossRef]
- Joiner, A. The Bleaching of Teeth: A Review of the Literature. J. Dent. 2006, 34, 412–419. [Google Scholar] [CrossRef] [PubMed]
- Kirk, R.E.; Othmer, D.F.; Mann, C.A. Encyclopedia of Chemical Technology. Vol. II. J. Phys. Chem. 1949, 53, 591. [Google Scholar] [CrossRef]
- Benahmed, A.G.; Gasmi, A.; Menzel, A.; Hrynovets, I.; Chirumbolo, S.; Shanaida, M.; Lysiuk, R.; Shanaida, Y.; Dadar, M.; Bjørklund, G. A Review on Natural Teeth Whitening. J. Oral Biosci. 2021, 64, 49–58. [Google Scholar] [CrossRef]
- Maran, B.M.; Burey, A.; de Paris Matos, T.; Loguercio, A.D.; Reis, A. In-Office Dental Bleaching with Light vs. without Light: A Systematic Review and Meta-Analysis. J. Dent. 2018, 70, 1–13. [Google Scholar] [CrossRef]
- Baroudi, K.; Hassan, N.A. The Effect of Light-Activation Sources on Tooth Bleaching. Niger. Med. J. 2014, 55, 363. [Google Scholar] [CrossRef] [PubMed]
- Chemin, K.; Rezende, M.; Milan, F.M.; Dantas, T.B.; Gomes, K.; Kossatz, S. Clinical Evaluation of 10% Hydrogen Peroxide on Tooth Sensitivity and Effectiveness in at Home Dental Bleaching. J. Contemp. Dent. Pract. 2018, 19, 1376–1380. [Google Scholar] [CrossRef] [PubMed]
- de Almeida, E.N.M.; Bessegato, J.F.; dos Santos, D.D.L.; de Souza Rastelli, A.N.; Bagnato, V.S. Violet LED for Non-Vital Tooth Bleaching as a New Approach. Photodiagnosis Photodyn. Ther. 2019, 28, 234–237. [Google Scholar] [CrossRef] [PubMed]
- Pirolo, R.; Mondelli, R.F.L.; Correr, G.M.; Gonzaga, C.C.; Furuse, A.Y. Effect of Coffe and a Cola-Based Soft Drink on the Color Stability of Bleached Bovine Incisors Considering the Time Elapsed after Bleaching. J. Appl. Oral Sci. 2014, 22, 534–540. [Google Scholar] [CrossRef] [PubMed]
- Bazzi, J.Z.; Bindo, M.J.F.; Rached, R.N.; Mazur, R.F.; Vieira, S.; de Souza, E.M. The Effect of At-Home Bleaching and Toothbrushing on Removal of Coffee and Cigarette Smoke Stains and Color Stability of Enamel. J. Am. Dent. Assoc. 2012, 143, e1–e7. [Google Scholar] [CrossRef] [PubMed]
- Arévalo Pineda, M.; Larrucea Verdugo, C. Recidiva Del Color Dentario Por Té, Café y Vino: In Vitro. Rev. Clínica Periodoncia Implantol. Rehabil. Oral 2012, 5, 57–65. [Google Scholar]
- Devigus, A. The Perfect Smile. Int. J. Esthet. Dent. 2014, 9, 465. [Google Scholar] [PubMed]
- Lee, R.; Bayne, A.; Tiangco, M.; Garen, G.; Chow, A. Prevention of Tea-induced Extrinsic Tooth Stain. Int. J. Dent. Hyg. 2014, 12, 267–272. [Google Scholar] [CrossRef] [PubMed]
- de Medeiros Melo, C.F.; Manfroi, F.B.; Spohr, A.M. Microhardness and Roughness of Enamel Bleached with 10% Carbamide Peroxide and Brushed with Different Toothpastes: An in Situ Study. J. Int. Oral Health JIOH 2014, 6, 18. [Google Scholar]
- Monteiro, D.; Moreira, A.; Cornacchia, T.; Magalhães, C. Evaluation of the Effect of Different Enamel Surface Treatments and Waiting Times on the Staining Prevention after Bleaching. J. Clin. Exp. Dent. 2017, 9, e677. [Google Scholar] [CrossRef][Green Version]
- de Araújo, L.S.N.; dos Santos, P.H.; Anchieta, R.B.; Catelan, A.; Fraga Briso, A.L.; Fraga Zaze, A.C.S.; Sundfeld, R.H. Mineral Loss and Color Change of Enamel after Bleaching and Staining Solutions Combination. J. Biomed. Opt. 2013, 18, 108004. [Google Scholar] [CrossRef] [PubMed]
- Farawati, F.A.; Hsu, S.-M.; O’Neill, E.; Neal, D.; Clark, A.; Esquivel-Upshaw, J. Effect of Carbamide Peroxide Bleaching on Enamel Characteristics and Susceptibility to Further Discoloration. J. Prosthet. Dent. 2019, 121, 340–346. [Google Scholar] [CrossRef] [PubMed]
- Matis, B.; Wang, G.; Matis, J.; Cook, N.; Eckert, G. White Diet: Is It Necessary during Tooth Whitening? Oper. Dent. 2015, 40, 235–240. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. Syst. Rev. 2021, 10, 89. [Google Scholar] [CrossRef] [PubMed]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan—A Web and Mobile App for Systematic Reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.-Y.; Corbett, M.S.; Eldridge, S.M. RoB 2: A Revised Tool for Assessing Risk of Bias in Randomised Trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [PubMed]
- Delgado, A.H.; Sauro, S.; Lima, A.F.; Loguercio, A.D.; Della Bona, A.; Mazzoni, A.; Collares, F.M.; Staxrud, F.; Ferracane, J.; Tsoi, J. RoBDEMAT: A Risk of Bias Tool and Guideline to Support Reporting of Pre-Clinical Dental Materials Research and Assessment of Systematic Reviews. J. Dent. 2022, 127, 104350. [Google Scholar] [CrossRef]
- de Geus, J.L.; De Lara, M.; Hanzen, T.; Fernández, E.; Loguercio, A.D.; Kossatz, S.; Reis, A. One-Year Follow-up of at-Home Bleaching in Smokers before and after Dental Prophylaxis. J. Dent. 2015, 43, 1346–1351. [Google Scholar] [CrossRef] [PubMed]
- Karakaya, İ.; Cengiz-Yanardag, E. Effects of Staining Beverages and Office Bleaching Agents on the Optical Characteristics and Surface Topography of Maxillary Incisor Teeth. Cyprus J. Med. Sci. 2022, 7, 395–403. [Google Scholar] [CrossRef]
- Karpinia, K.; Magnusson, I.; Barker, M.L.; Gerlach, R.W. Clinical Comparison of Two Self-directed Bleaching Systems. J. Prosthodont. 2003, 12, 242–248. [Google Scholar] [CrossRef]
- Meireles, S.; Heckmann, S.; Santos, I.; Della Bona, A.; Demarco, F. A Double Blind Randomized Clinical Trial of At-Home Tooth Bleaching Using Two Carbamide Peroxide Concentrations: 6-Month Follow-Up. J. Dent. 2008, 36, 878–884. [Google Scholar] [CrossRef] [PubMed]
- Meireles, S.; Santos, I.; Della Bona, A.; Demarco, F. A Double-Blind Randomized Clinical Trial of Two Carbamide Peroxide Tooth Bleaching Agents: 2-Year Follow-Up. J. Dent. 2010, 38, 956–963. [Google Scholar] [CrossRef] [PubMed]
- Meireles, S.S.; dos Santos, I.d.S.; Della Bona, Á.; Demarco, F.F. A Double-Blind Randomized Controlled Clinical Trial of 10 Percent versus 16 Percent Carbamide Peroxide Tooth-Bleaching Agents: One-Year Follow-Up. J. Am. Dent. Assoc. 2009, 140, 1109–1117. [Google Scholar] [CrossRef] [PubMed]
- Gasparri, F.; Schemehorn, B.R.; Zanardi, A. Efficacy of Teeth Whitening with a Mouthwash: In Vitroand In Vivo Approaches. J. Clin. Dent. 2018, 29, 13–17. [Google Scholar]
- Azer, S.S.; Hague, A.L.; Johnston, W.M. Effect of Bleaching on Tooth Discolouration from Food Colourant in Vitro. J. Dent. 2011, 39, e52–e56. [Google Scholar] [CrossRef] [PubMed]
- Al-Angari, S.S.; Eckert, G.J.; Sabrah, A.H. Color Stability, Roughness, and Microhardness of Enamel and Composites Submitted to Staining/Bleaching Cycles. Saudi Dent. J. 2021, 33, 215–221. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, R.F.; da Mata Galvão, A.; Campolina, M.G.; de Mendonça, L.C.; Soares, C.J.; Carvalho, C.N.; da Silva, G.R. Does Polishing of Bleached Enamel Affect Roughness and Tooth Color Stability after Exposure to Coffee? J. Esthet. Restor. Dent. 2022, 34, 351–359. [Google Scholar] [CrossRef]
- Ermis, R.B.; Celik, E.U.; Yildiz, G.; Yazkan, B. Effect of Tooth Discolouration Severity on the Efficacy and Colour Stability of Two Different Trayless At-Home Bleaching Systems. J. Dent. Res. Dent. Clin. Dent. Prospect. 2018, 12, 120. [Google Scholar] [CrossRef]
- Liporoni, P.C.S.; Souto, C.M.C.; Pazinatto, R.B.; Cesar, I.C.R.; de Rego, M.A.; Mathias, P.; Cavalli, V. Enamel Susceptibility to Coffee and Red Wine Staining at Different Intervals Elapsed from Bleaching: A Photoreflectance Spectrophotometry Analysis. Photomed. Laser Surg. 2010, 28, S105-9. [Google Scholar] [CrossRef]
- Catelan, A. Chemical Composition and Roughness of Enamel and Composite after Bleaching, Acidic Beverages and Toothbrushing. J. Clin. Exp. Dent. 2019, 11, e1175. [Google Scholar]
- Berger, S.B.; Coelho, A.S.; Oliveira, V.A.P.; Cavalli, V.; Giannini, M. Enamel Susceptibility to Red Wine Staining after 35% Hydrogen Peroxide Bleaching. J. Appl. Oral Sci. 2008, 16, 201–204. [Google Scholar] [CrossRef] [PubMed]
- Attia, M.L.; Aguiar, F.; Mathias, P.; Ambrosano, G.; Fontes, C.M.; Liporoni, P. The Effect of Coffee Solution on Tooth Color during Home Bleaching Applications. Am. J. Dent. 2009, 22, 175–179. [Google Scholar]
- Borges, J.; Soares, C.; de Bragança, G.; Vilela, A.; Soares, P. Effect of Activated Charcoal Toothpaste on Color Stability of Bleached Teeth Immersed in Different Drinks. Oper. Dent. 2023, 48, 207–217. [Google Scholar] [CrossRef] [PubMed]
- da Silva, L.; Cintra, L.T.A.; de Oliveira Gallinari, M.; de Alcântara, S.; Dos Santos, P.; Chaves Neto, A.H.; Briso, A.L.F. Influence of Different Dye Substances on the Effectiveness of Bleaching and H2O2 Diffusion. Oper. Dent. 2022, 47, 648–657. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Lee, S.S.; Cartwright, S.; Wilson, A.C.; DeVizio, W.; Petrone, M.; Volpe, A.R.; Zhang, Y.P. Comparative Tooth Whitening Efficacy of 18% Carbamide Peroxide Liquid Whitening Gel Using Three Different Regimens. J. Clin. Dent. 2004, 15, 11–16. [Google Scholar] [PubMed]
- Chen, Y.; Yang, S.; Hong, D.; Attin, T.; Yu, H. Short-Term Effects of Stain-Causing Beverages on Tooth Bleaching: A Randomized Controlled Clinical Trial. J. Dent. 2020, 95, 103318. [Google Scholar] [CrossRef] [PubMed]
- Souza, J.M.; Aguiar, J.; Neves, W.; Espíndola-Castro, L.F.; Costa, D.; Silva, C. Influence of Diet and Red Wine Exposure on the Velocity of at Home Bleaching: A Randomized Controlled Clinical Trial. Am. J. Dent. 2022, 35, 191–196. [Google Scholar] [PubMed]
- Hass, V.; Carvalhal, S.T.; Lima, S.N.L.; Viteri-Garcia, A.A.; Maia Filho, E.M.; Bandeca, M.C.; Reis, A.; Loguercio, A.D.; Tavarez, R.R.D.J. Effects of Exposure to Cola-Based Soft Drink on Bleaching Effectiveness and Tooth Sensitivity of in-Office Bleaching: A Blind Clinical Trial. Clin. Cosmet. Investig. Dent. 2019, 11, 383–392. [Google Scholar] [CrossRef]
- Lucas Lage Menezes, D.; Lima, S.N.L.; Maia-Filho, E.M.; Fernandes, E.S.; Mendes, S.J.F.; Machado, L.; Gonçalves, D.; Bandeca, M.C.; Reis, A.; Loguercio, A.D. Clinical Effects of the Exposure to Red Wine during At-Home Bleaching. Quintessence Int. 2022, 53, 48–57. [Google Scholar]
- Rezende, M.; Loguercio, A.; Reis, A.; Kossatz, S. Clinical Effects of Exposure to Coffee during At-Home Vital Bleaching. Oper. Dent. 2013, 38, E229–E236. [Google Scholar] [CrossRef]
- Attin, T.; Manolakis, A.; Buchalla, W.; Hannig, C. Influence of Tea on Intrinsic Colour of Previously Bleached Enamel. J. Oral Rehabil. 2003, 30, 488–494. [Google Scholar] [CrossRef] [PubMed]
- Barbosa, I.F.; Câmara, J.V.F.; Pierote, J.J.A.; Menezes, L.R.; de Freitas, P.F.; Santos, L.A.; Martini, T.; Paulillo, L.A.M.S.; Aguiar, F.H.B. The in Vitro Effect of Solutions with or without Sugar in Dental Bleaching. J. Mech. Behav. Biomed. Mater. 2023, 142, 105821. [Google Scholar] [CrossRef]
- Briso, A.; Fagundes, T.; Gallinari, M.; Moreira, J.; De Almeida, L.; Rahal, V.; Gonçalves, R.; dos Santos, P. An in Situ Study of the Influence of Staining Beverages on Color Alteration of Bleached Teeth. Oper. Dent. 2016, 41, 627–633. [Google Scholar] [CrossRef] [PubMed]
- Câmara, J.V.F.; de Paiva Pereira Santos de Souza, L.; Vargas, D.O.A.; Barbosa, I.F.; da Silveira Pereira, G.D. Effect of Tooth Enamel Staining by Coffee Consumption during At-Home Tooth Bleaching with Carbamide Peroxide. Rev. Odontol. UNESP 2020, 49, e20200024. [Google Scholar] [CrossRef]
- Carlos, N.; Pinto, A.; Do Amaral, F.; França, F.; Turssi, C.; Basting, R. Influence of Staining Solutions on Color Change and Enamel Surface Properties during At-Home and in-Office Dental Bleaching: An in Situ Study. Oper. Dent. 2019, 44, 595–608. [Google Scholar] [CrossRef]
- Correia, A.M.d.O.; Melo, B.E.D.; Cedraz, J.d.S.B.; Rocha, D.M.d.; dos Santos, N.B.; de Mendonça Fragoso, L.S. Influence of Solutions with Pigmentation Potential on Tooth Color after Bleaching Using 22% Carbamide Peroxide. Biosci. J. Online 2017, 33, 1106–1112. [Google Scholar] [CrossRef]
- Karadas, M.; Seven, N. The Effect of Different Drinks on Tooth Color after Home Bleaching. Eur. J. Dent. 2014, 8, 249–253. [Google Scholar] [CrossRef] [PubMed]
- Mori, A.A.; Lima, F.F.; Benetti, A.R.; Terada, R.S.S.; Fujimaki, M.; Pascotto, R.C. Susceptibility to Coffee Staining during Enamel Remineralization Following the In-office Bleaching Technique: An in Situ Assessment. J. Esthet. Restor. Dent. 2016, 28, S23–S31. [Google Scholar] [CrossRef]
- Lins-Filho, P.-C.; Dias, M.-F.; Silva, M.-F.; Guimarães, R.-P. Does Comsumption of Staining Drinks Compromise the Result of Tooth Whitening? J. Clin. Exp. Dent. 2019, 11, e1012. [Google Scholar]
- Rezende, M.; Kapuchczinski, A.C.; Vochikovski, L.; Demiate, I.M.; Loguercio, A.D.; Kossatz, S. Staining Power of Natural and Artificial Dyes after At-Home Dental Bleaching. J. Contemp. Dent. Pract. 2019, 20, 425. [Google Scholar]
- Russo, D.S.; Viano, M.; Bambi, C.; Nieri, M.; Giachetti, L. Color Stability of Bleached Teeth over Time: An in Vitro Study. Eur. J. Esthet. Dent. 2010, 5, 300–310. [Google Scholar]
- Zekonis, R.; Matis, B.A.; Cochran, M.A.; Shetri, S.A.; Eckert, G.J.; Carlson, T.J. Clinical Evaluation of In-Office and at-Home Bleaching Treatments. Oper. Dent. 2003, 28, 114–121. [Google Scholar]
- Deliperi, S.; Bardwell, D.N.; Papathanasiou, A. Clinical Evaluation of a Combined In-Office and Take-Home Bleaching System. J. Am. Dent. Assoc. 2004, 135, 628–634. [Google Scholar] [CrossRef]
- Ghavamnasiri, M.; Bidar, M.; Rad, A.H.; Namazikhah, M.S. The Effect of 16 Percent Carbamide Peroxide on Enamel Staining Susceptibility. J. Calif. Dent. Assoc. 2006, 34, 873–876. [Google Scholar] [CrossRef] [PubMed]
- Setien, V.; Roshan, S.; Cala, C.; Ramirez, R. Pigmentation Susceptibility of Teeth after Bleaching with 2 Systems: An in Vitro Study. Quintessence Int. 2009, 40, 47–52. [Google Scholar] [PubMed]
- Adeyemi, A.; Pender, N.; Higham, S. The Susceptibility of Bleached Enamel to Staining as Measured by Quantitative Light-induced Fluorescence (QLF). Int. Dent. J. 2008, 58, 208–212. [Google Scholar] [CrossRef]
- Sulieman, M.; Macdonald, E.; Rees, J.S.; Newcombe, R.g.; Addy, M. Tooth Bleaching by Different Concentrations of Carbamide Peroxide and Hydrogen Peroxide Whitening Strips: An in Vitro Study. J. Esthet. Restor. Dent. 2006, 18, 93–100. [Google Scholar] [CrossRef]
- Featherstone, J.; Goodman, P.; McLean, J. Electron Microscope Study of Defect Zones in Dental Enamel. J. Ultrastruct. Res. 1979, 67, 117–123. [Google Scholar] [CrossRef]
- Gerlach, R.; Zhou, X. Vital Bleaching with Whitening Strips: Summary of Clinical Research on Effectiveness and Tolerability. J. Contemp. Dent. Pract. 2001, 2, 28–42. [Google Scholar] [CrossRef]
- Putt, M.S.; Milleman, J.L.; Jenkins, W.; Schmitt, P.; Master, A.S.; Strate, J. A Randomized Crossover-Design Study to Investigate the Plaque Removal Efficacy of Two Power Toothbrushes: Philips Sonicare Flexcare and Oral-B Triumph. Compend. Contin. Educ. Dent. Jamesburg NJ 1995 2008, 29, 56–58. [Google Scholar]
- García-Godoy, F.; Ellacuria, J. Effectiveness of Sonicare Power Toothbrush to Remove Chlorhexidine Stains. Am. J. Dent. 2002, 15, 290–292. [Google Scholar] [PubMed]
- Kugel, G.; Aboushala, A.; Sharma, S.; Ferreira, S.; Anderson, C. Maintenance of Whitening with a Power Toothbrush after Bleaching Treatment. Compend. Contin. Educ. Dent. Jamesburg NJ 1995 2004, 25, 119–131. [Google Scholar]
- Horn, B.A.; Bittencourt, B.F.; Gomes, O.M.M.; Farhat, P.A. Clinical Evaluation of the Whitening Effect of Over-the-Counter Dentifrices on Vital Teeth. Braz. Dent. J. 2014, 25, 203–206. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Dantas, A.A.R.; Bortolatto, J.F.; Roncolato, A.; Merchan, H.; Floros, M.C.; Kuga, M.C.; de Oliveira, O.B., Jr. Can a Bleaching Toothpaste Containing Blue Covarine Demonstrate the Same Bleaching as Conventional Techniques? An in Vitro, Randomized and Blinded Study. J. Appl. Oral Sci. 2015, 23, 609–613. [Google Scholar] [CrossRef] [PubMed]
- Roselino, L.d.M.R.; Tirapelli, C.; Pires-de-Souza, F. Randomized Clinical Study of Alterations in the Color and Surface Roughness of Dental Enamel Brushed with Whitening Toothpaste. J. Esthet. Restor. Dent. 2018, 30, 383–389. [Google Scholar] [CrossRef]
- Santana Jorge, O.; Noronha Ferraz de Arruda, C.; Tonani Torrieri, R.; Geng Vivanco, R.; de Carvalho Panzeri Pires-de-Souza, F. Over-the-Counter Bleaching Agents Can Help with Tooth Whitening Maintenance. J. Esthet. Restor. Dent. 2022, 34, 328–334. [Google Scholar] [CrossRef] [PubMed]
- Attin, T.; Albrecht, K.; Becker, K.; Hannig, C.; Wiegand, A. Influence of Carbamide Peroxide on Enamel Fluoride Uptake. J. Dent. 2006, 34, 668–675. [Google Scholar] [CrossRef]
- Kim, Y.; Kwon, H.; Kim, B. Effect of Nano-Carbonate Apatite to Prevent Re-Stain after Dental Bleaching in Vitro. J. Dent. 2011, 39, 636–642. [Google Scholar] [CrossRef] [PubMed]
- Moosavi, H.; Darvishzadeh, F. The Influence of Post Bleaching Treatments in Stain Absorption and Microhardness. Open Dent. J. 2016, 10, 69. [Google Scholar] [CrossRef]
- Van der Burgt, T.P.; Ten Bosch, J.J.; Borsboom, P.C.F.; Kortsmit, W. A Comparison of New and Conventional Methods for Quantification of Tooth Color. J. Prosthet. Dent. 1990, 63, 155–162. [Google Scholar] [CrossRef]
- Watts, A.; Addy, M. Tooth Discolouration and Staining: A Review of the Literature. Br. Dent. J. 2001, 190, 309–316. [Google Scholar] [CrossRef] [PubMed]
- Jiang, T.; Guo, Y.R.; Feng, X.W.; Sa, Y.; Yang, X.; Wang, M.; Li, P.; Wang, Y.N. Hydrogen Peroxide Might Bleach Natural Dentin by Oxidizing Phosphoprotein. Dent. J. 2019, 7, 43. [Google Scholar] [CrossRef] [PubMed]
- Matis, B.A. A clinical evaluation of carbamide peroxide and hydrogen peroxide whitening agents during daytime use. J. Am. Dent. Assoc. 2000, 131, 1269–1277. [Google Scholar]
- Feiz, A. Influence of bleaching agents on the surface morphology and chemical composition of enamel and dentin: A literature review. J. Contemp. Dent. Pract. 2019, 20, 636–642. [Google Scholar]
- Tavares, M. Effects of peroxide bleaching on the organic structure of enamel and dentin matrix. J. Dent. 2013, 41 (Suppl. S5), e98–e105. [Google Scholar]



| Search | Terms |
|---|---|
| #1 | Dental bleaching OR at-home bleaching OR bleached teeth OR tooth bleaching OR tooth whitening OR bleaching OR vital bleaching OR bleached enamel |
| #2 | Cola-based soft drink O carbonated beverages OR cola OR soda OR diet OR red wine OR coffee OR staining beverage OR dyes OR food coloring agents OR staining drinks OR pigmenting agents OR staining solutions OR drink OR tea OR staining beverages OR food colorant |
| #3 | Bleaching effectiveness OR staining OR color alteration OR color change OR staining power OR clinical effect OR tooth color OR intrinsic color OR color stability OR tooth discoloration |
| #4 | #1 and #2 and #3 |
| Study and Year | Bleaching Agent | Bleaching Protocol | Staining Agents | Staining Protocol | Color Measurement Device | Primary Outcome | Secondary Outcome | Main Results |
|---|---|---|---|---|---|---|---|---|
| Attin, 2003 [51] | 10% carbamide peroxide—VivaStyle (Vivadent, Schaan, Liechtenstein) | 8 h application over 8 days | Tea | Immersion for 10 min for 8 days | Spectrophotometer (Pikkio, Medical High Technologies, Verona, Italy) | Color difference | The immersion of the specimens in tea did not affect the bleaching. | |
| Barbosa, 2023 [52] | 10% carbamide peroxide—Pola- night 10% (SDI) 37.5% hydrogen peroxide—Polaoffice + (SDI) | 2 h application over 30 days 3 applications of 8 min with a 7-day interval | Red wine Coffee | Immersion for 45 min for 30 days | Vita Easyshade® Advance 4.0 (Vita Zahnfabrik H. RauterGmbH & Co, Bad Säckingen, Germany) | Color difference | Roughness Surface elemental analysis | Immersion in red wine or coffee did not affect the bleaching process. |
| Briso, 2016 [53] | 10% carbamide peroxide—Whiteness Perfect (FGM Produtos Odontologicos Ltd., Santa Catarina, Brazil) | 4 h application over 14 days | Coffee Grape juice | Immersion for 10 min for 14 days | Ultraviolet–visible reflection spec- trophotometer (UV-2450, Shimadzu Corporation, Kyoto, Japan) | Color difference | Bleaching outcome was not affected by the consumption of staining agents. | |
| Camara, 2018 [54] | 16% carbamide peroxide—Whiteness Perfect (FGM Dental Products, Joinville, Brazil) | 4 h application over 21 days | Coffee | Immersion for 15 min for 21 days | Vita Easyshade™ Advance 4.0 spectrophotometer (VITA Zahnfabrik H. RauterGmbH & Co, BadSäckingen, Germany) | Color difference | Coffee did not affect the bleaching outcome. | |
| Carlos, 2016 [55] | 40% hydrogen peroxide—Opalescence Boost PF 40% (Ultradent South Jordan, UT, USA) 10% carbamide peroxide—Opalescence PF10% (Ultradent) | 3 applications of 40 min with a 7-day interval 1 h application over 15 days | Cola Coffee | Immersion for 30 min for 15 days | Easyshade Advance (VITA, Bad Säckingen, Germany) | Color difference | Roughness Microhardness | The staining solution either cola or coffee negatively affected the results of bleaching. |
| Correia, 2017 [56] | 22% carbamide peroxide—Whiteness Perfect (FGM Dental Products, Joinville, Brazil) | 1 h application over 15 days | Coffee Cola Tea Red wine Chocolate milk Soya sauce | Immersion for 5 min twice a day for 15 days | Spectrophotometer (Minolta CR-321, Japan) | Color difference | Only soya sauce negatively affected the bleaching outcomes. | |
| de Araújo, 2013 [21] | 10% carbamide peroxide—Whiteness Perfect (FGM Produtos Odontologicos Ltd., Santa Catarina, Brazil) | 6 h application over 21 days | Cola soft drink Melted chocolate Red wine | Immersion for 1 h for 21 days | Spectrophotometer (UV-2450; Shimadzu Corp.) | Color difference | Mineral loss Microhardness | Staining solutions did not affect the bleaching outcomes. |
| Karadas, 2014 [57] | 10% carbamide peroxide—Opalescence 10%, (Ultradent Products, USA) | 6 h application over 14 days | Red wine Coffee Cola Tea | Immersion for 15 min, 6 h, 1 week and 1 month | Spectrophotometer (Shadepilot, DeguDent GmbH, Hanau, Germany | Color difference | Staining agents decreased the bleaching effectiveness. | |
| Mori, 2015 [58] | 35% hydrogen peroxide gel—Lase Peroxide Sensy (DMC, São Carlos, Brazil) | 2 applications of 15 min with a 3-day interval | Coffee | Immersion for 30 min for 7 or 14 days | Easyshade® (Vita-Zahnfabrik, Bad Säckingen, Germany) | Whiteness index and closeness to white | Enamel remineralization | The whiteness index was not influenced by coffee. |
| Lins-Filho, 2019 [59] | 35% hydrogen peroxide—Whiteness HP 35% (FGM Dental Products) | 3 applications of 40 min with a 7-day interval | Coffee Wine | Immersion for 5 min for 7 days | Easyshade (Vita, Brea, California, USA) | Color difference | The staining agents did not affect the color change. | |
| Rezende, 2019 [60] | 16% carbamide peroxide—Whiteness Perfect (FGM, Joinville, Santa Catarina, Brazil) | 3 h application over 21 days | Beet Carmine Caramel Red 40 dye | Immersion for 5 min, twice a day, for 21 days | Spectrophotometer (Vita Zahnfabrik, BadSäckingen, Germany) | Color difference | Exposure to staining agents did not affect the bleaching efficacy. | |
| Russo, 2010 [61] | 25% hydrogen peroxide—Zoom 2 (Discus Dental, Culver City, CA, USA) | 3 applications of 20 min | Coffee | Immersion for 1 h, 12 times per day, for 6 days | VITA Easyshade (VITA Zahnfabrik, Bad Säckingen, Germany) | Color difference | The staining with coffee did not affect the bleaching outcome |
| Study and Year | Type of Clinical Trial | Registration | Number of Participants | Bleaching Agent | Bleaching Protocol | Staining Agents | Staining Protocol | Color Measurement Device | Primary Outcome | Secondary Outcome | Main Results |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Chen, 2020 [46] | Randomized double-blinded clinical trial | Clinical Trials Registry #NCT03933527 | 61 participants | 40% hydrogen peroxide -Opalescence BOOST PF 40%, (Ultradent, USA) | 2 sessions of 2 applications of 20 min with a 7-day interval | Coffee Tea | Rinse for 30 s, 4 times daily for 28 days. | Easyshade (Vita ZahnFabrik) | Whiteness index Color difference | Tooth sensitivity | Coffee or tea did not interfere with the color change in bleaching treatment |
| De Souza, 2022 [47] | Randomized clinical trial | ReBEC # RBR-7sv2g8r | 45 participants | 16% carbamide peroxide—Magic White | 4 h application over 14 days | Red wine | Rinse for 5 min 3 times dailyfor 14 days. | Vita Easyshade (Vita Zahnfabrik, Bad Säckingen, Germany) | Color difference | Postoperative sensitivity Satisfaction of patients | Colorant-rich diets did not influence the performance of the bleaching treatment. |
| Hass, 2019 [48] | Randomized single-blinded clinical trial | ReBEC # RBR-2nz5s2 | 44 participants | 35% hydrogen peroxide—Whiteness HP Automixx 35 (FGM Dental Products) | 2 sessions of 3 applications of 15 min with a 7-day interval15 min of HP application (2 sessions and 3 applications each) | Coca- Cola | Rinse for 30 s, 4 times daily for 30 days | Vita Easyshade (Vident, Brea, CA, USA). | Color difference | Tooth sensitivity | Cola-based soft drinks did not affect the bleaching outcome. |
| Menezes, 2022 [49] | Non-randomized clinical trial | ReBEC #RBR-3 × 9m5j | 80 participants | 10% carbamide peroxide—Whiteness Perfect (FGM Dental Products, Joinville, Brazil) | 4 h application over 21 days | Red wine | Rinse for 30 s, 4 times daily for 21 days. | Vita Easyshade (Vita Zahnfabrik, Bad Säckingen, Germany) | Color difference | Tooth sensitivity Nitric oxide levels in saliva | Red wine does not influence the bleaching outcome |
| Rezende, 2013 [50] | Non-randomized clinical trial | Not mentioned | 40 participants | 16% carbamide peroxide—Whiteness Perfect, (FGM Dental Products, Joinville, Brazil) | 3 h application over 21 days | Coffee | Rinse for 30 s, 4 times daily for 21 days. | Easyshade (Vita Zahnfabrik) | Color difference | Tooth sensitivity | Coffee consumption during dental bleaching did not influence the efficacy of bleaching |
| Author | D1: Bias in Planning and Allocation | D2: Bias in Specimen Preparation | D3: Bias in Outcome Assessment | D4: Bias in Data Treatment and Reporting | |||||
|---|---|---|---|---|---|---|---|---|---|
| Control Group | Randomization of Samples | Sample Size | Standardization of Samples and Material | Identical Experimental Conditions Across Groups | Adequate and Standardized Testing procedures and Outcomes | Blinding of the Test Operator | Statistical Analysis | Reporting Study Outcomes | |
| Attin, 2003 [51] | √ | Χ | Χ | √ | √ | √ | Χ | Insufficient √ | √ |
| Barbosa, 2023 [52] | √ | √ | Χ | √ | √ | √ | Χ | √ | √ |
| Briso, 2016 [53] | √ | √ | Χ | √ | √ | √ | √ | √ | √ |
| Camara, 2018 [54] | √ | Χ | Χ | √ | √ | √ | Χ | √ | √ |
| Carlos, 2016 [55] | √ | √ | √ | √ | √ | √ | √ | Insufficient √ | √ |
| Correia, 2017 [56] | √ | Χ | √ | √ | √ | √ | Χ | Insufficient √ | √ |
| de Araújo, 2013 [21] | √ | Χ | Χ | √ | √ | √ | Χ | Insufficient √ | √ |
| Karadas, 2014 [57] | √ | √ | Χ | √ | √ | √ | Χ | Insufficient √ | √ |
| Mori, 2015 [58] | √ | √ | Χ | √ | √ | √ | Χ | √ | √ |
| Lins-Filho, 2019 [59] | √ | √ | Χ | √ | √ | √ | Χ | √ | √ |
| Rezende, 2019 [60] | √ | √ | Χ | √ | √ | √ | Χ | Insufficient √ | √ |
| √ | √ | Χ | √ | √ | √ | Χ | √ | √ | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hardan, L.; Bourgi, R.; Flores-Ledesma, A.; Devoto, W.; Devoto, E.; Fernández-Barrera, M.Á.; Kharouf, N.; Cuevas-Suárez, C.E. Is a White Diet Necessary for Tooth Bleaching Procedures? A Systematic Review and Meta-Analysis. Dent. J. 2024, 12, 118. https://doi.org/10.3390/dj12040118
Hardan L, Bourgi R, Flores-Ledesma A, Devoto W, Devoto E, Fernández-Barrera MÁ, Kharouf N, Cuevas-Suárez CE. Is a White Diet Necessary for Tooth Bleaching Procedures? A Systematic Review and Meta-Analysis. Dentistry Journal. 2024; 12(4):118. https://doi.org/10.3390/dj12040118
Chicago/Turabian StyleHardan, Louis, Rim Bourgi, Abigailt Flores-Ledesma, Walter Devoto, Emma Devoto, Miguel Ángel Fernández-Barrera, Naji Kharouf, and Carlos Enrique Cuevas-Suárez. 2024. "Is a White Diet Necessary for Tooth Bleaching Procedures? A Systematic Review and Meta-Analysis" Dentistry Journal 12, no. 4: 118. https://doi.org/10.3390/dj12040118
APA StyleHardan, L., Bourgi, R., Flores-Ledesma, A., Devoto, W., Devoto, E., Fernández-Barrera, M. Á., Kharouf, N., & Cuevas-Suárez, C. E. (2024). Is a White Diet Necessary for Tooth Bleaching Procedures? A Systematic Review and Meta-Analysis. Dentistry Journal, 12(4), 118. https://doi.org/10.3390/dj12040118










