Comparing Zirconium Crown Marginal Adaptation in Preparations with Two Different Occlusal Reductions
Abstract
1. Introduction
- Zirconia-Toughened Alumina (ZTA):
- 2.
- Magnesia Partially Stabilized Zirconia (Mg-PSZ):
- 3.
- Yttria Fully Stabilized Tetragonal Zirconia Polycrystal (3Y-TZP):
- Partial-contour zirconia: Veneered zirconia crowns were created using partially sintered Y-TZP blocks. A partial-contour zirconia restoration involves milling a durable zirconia framework and covering it in a more aesthetically pleasing porcelain veneer. These restorations have various names, including veneered, zirconia-based, and bi-layered. Another option is to apply the veneering layer where it is cosmetically necessary; these restorations are known as hybrid or minimally veneered restorations [25].
- Full-contour zirconia: Partially sintered Y-TZP blocks were used to create full-contour anatomical crowns. One material block can mill a monolithic unit for full-contour restorations without porcelain overlays [17,18]. Similar to regular porcelain fused to metal (PFM) crowns, it can be ready for the application of a knife-edge, chamfer, or shoulder finishing line [26]. It is approved for use with crowns over implants, posterior crowns, full-arch bridges up to 14 units, and crowns with limited occlusal clearance. The major candidates are grinders and bruxers who do not want metal occlusal PFM restorations or cast gold.
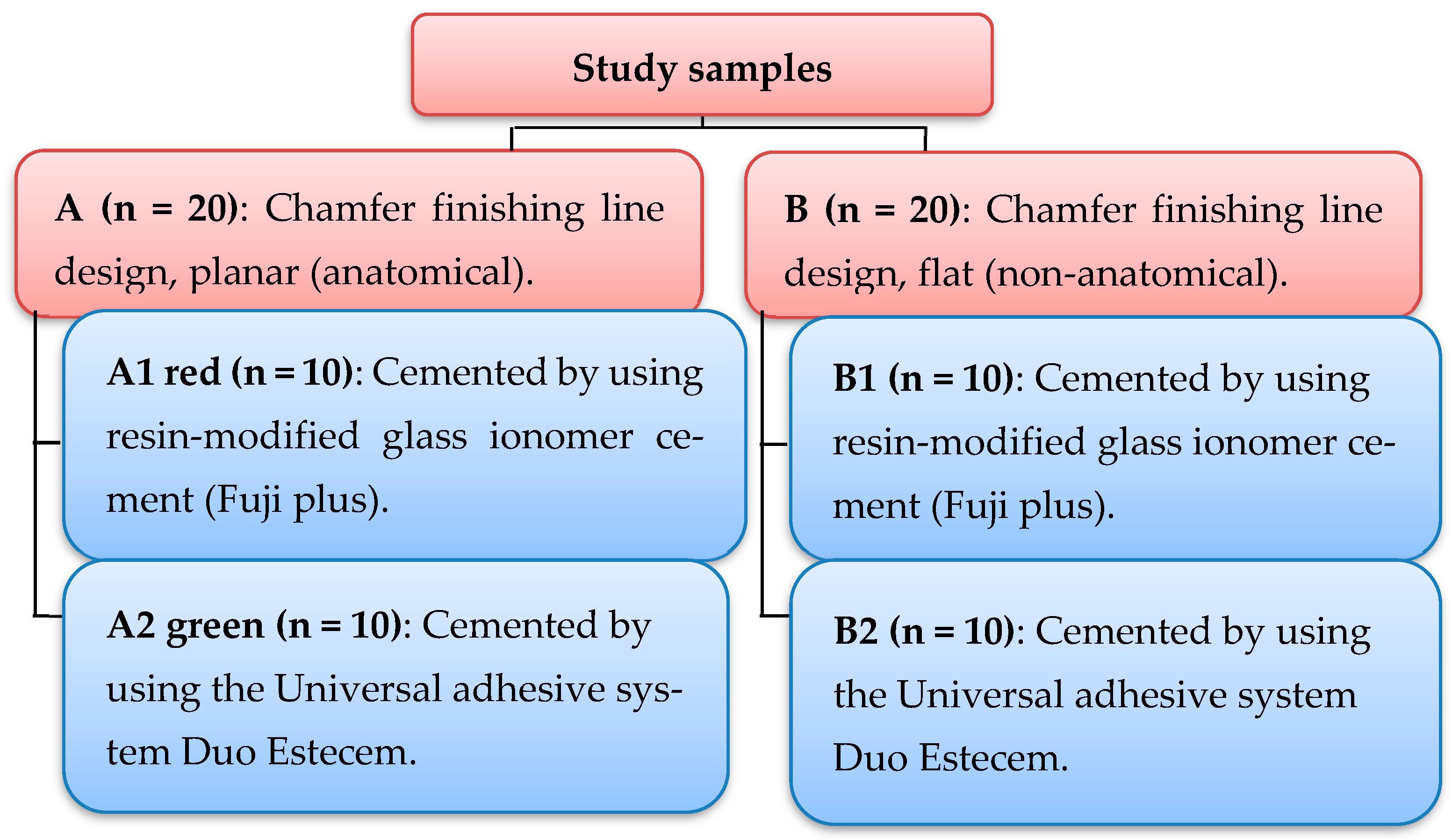
2. Materials and Methods
2.1. Statistical Analysis
2.1.1. Shapiro–Wilk Statistical Analysis
2.1.2. Descriptive Analysis
2.1.3. Inferential Analysis
3. Results
3.1. Pre-Cementation Results
3.2. Descriptive Statistics
3.3. Inferential Statistics
3.4. Post-Cementation Results
3.5. Descriptive Statistics
3.6. Inferential Statistics
3.7. Comparative Statistical Analysis between Pre- and Post-Cementation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- White, S.N.; Ingles, S.; Kipnis, V. Influence of marginal opening on microleakage of cemented artificial crowns. J. Prosthodont. Mater. 1994, 71, 257–264. [Google Scholar] [CrossRef]
- Tan, P.L.; Gratton, D.G.; Diaz-Arnold, A.M.; Holmes, D.C. An in vitro comparison of vertical marginal gaps of CAD/CAM titanium and conventional cast restorations. J. Prosthodont. 2008, 17, 378–383. [Google Scholar] [CrossRef]
- Demir, N.; Ozturk, A.N.; Malkoc, M.A. Evaluation of the marginal fit of full ceramic crowns by the microcomputed tomography (micro-CT) technique. Eur. J. Dent. 2014, 8, 437–444. [Google Scholar] [CrossRef] [PubMed]
- Holmes, J.R.; Bayne, S.C.; Holland, G.A.; Sulik, W.D. Considerations in measurement of marginal fit. J. Prosthet. Dent. 1989, 62, 405–408. [Google Scholar] [CrossRef] [PubMed]
- Suarez, M.J.; Villaumbrosia, D.; González, P.; Pradíes, G.; Lozano, J.F. Comparison of the marginal fit of Procera All Ceram crowns with two finish lines. Int. J. Prosthodont. 2003, 16, 229–232. [Google Scholar]
- Neves, F.D.; Prado, C.J.; Prudente, M.S.; Carneiro, T.A.; Zancopé, K.; Davi, L.R.; Mendonça, G.; Cooper, L.F.; Soares, C.J. Micro-computed tomography evaluation of marginal fit of lithium disilicate crowns fabricated by using chairside CAD/CAM systems or the heat-pressing technique. J. Prosthet. Dent. 2014, 112, 1134–1140. [Google Scholar] [CrossRef]
- Mclean, J.W.; Vonfraunhofer, J.A. The estimation of cement Film thickness by an in vivo technique. Br. J. Dent. 1971, 131, 107–111. [Google Scholar] [CrossRef] [PubMed]
- Akbar, J.H.; Petrie, C.S.; Walker, M.P.; Williams, K.; Eick, J.D. Marginal adaptation of Cerec 3 CAD/CAM composite crowns using two different finish line preparation designs. J. Prosthodont. 2006, 15, 155–163. [Google Scholar] [CrossRef] [PubMed]
- Ural, C.; Burgaz, Y.; Sarac, D. In vitro evaluation of marginal adaptation in five ceramic restoration fabricating techniques. Int. J. Quintessence 2010, 41, 585–590. [Google Scholar]
- Kassem, A.S.; Atta, O.; El-Mowafy, O. Fatigue resistance and microleakage of CAD/CAM ceramic and composite molar crowns. J. Prosthodont. 2012, 21, 28–32. [Google Scholar] [CrossRef]
- Christensen, G.J. Impressions are changing deciding on conventional, digital, or digital plus in office milling. J. Am. Dent. Assoc. 2009, 140, 1301–1304. [Google Scholar] [CrossRef] [PubMed]
- Logozzo, S.; Kilpela, A.; Makynen, A.; Zanetti, E.M. Recent advances in dental optics-part II: Experimental tests for a new intraoral scanner. Opt. Lasers Eng. 2014, 54, 187–196. [Google Scholar] [CrossRef]
- Jorge, R.N.; Campos, J.R.; Vaz, M.A.; Santos, S.M.; Tavares, J.M.R. (Eds.) Proceedings of the Iv International Conference on Biodental Engineering Iv, Porto, Portugal, 21–23 June 2016; CRC Press: Boca Raton, FL, USA, 2017. [Google Scholar]
- Raigrodski, A.J. Contemporary materials and technologies for all ceramic fixed partial dentures: A review of the literature. Int. J. Prosthodont. 2004, 92, 557–562. [Google Scholar] [CrossRef] [PubMed]
- Koutayas, S.O.; Vagkopoulou, T.; Pelekanos, S.; Koidis, P.; Strub, J.R. Zirconia in Dentistry: Part II. Evidence based clinical break through. Eur. J. Esthet Dent. 2009, 4, 348–380. [Google Scholar] [PubMed]
- Ramos, G.F.; Monteiro, E.B.; Bottino, M.A.; Zhang, Y.; Marques, D.E.; Melo, R. Failure probability of three designs of zirconia crowns. Int. J. Periodont. Restor. Dent. 2015, 35, 843–849. [Google Scholar] [CrossRef]
- Beuer, M.; Stimmelmayr, J.F.; Gueth, D.; Edelhoff, M.; Naumann, M. In vitro performance of full contour zirconia single crowns. J. Dent. Mater. 2012, 28, 449–456. [Google Scholar] [CrossRef]
- Reich, S. Tooth colored CAD/CAM monolithic restorations. Int. J. Comput. Dent. 2015, 18, 131–146. [Google Scholar]
- Carden, R.A. A changing direction in dentistry: Full contour zirconia. J. Dent. Tech. 2011, 14–16. [Google Scholar]
- Witkowski, S.; Komine, F.; Gerds, T. Marginal accuracy of titanium copings fabricated by casting and CAD/CAM techniques. J. Prosthet. Dent. 2006, 96, 47–52. [Google Scholar] [CrossRef]
- Nakamura, K.; Harada, A.; Kanno, T.; Inagaki, R.; Niwano, Y.; Milleding, P.; Örtengren, U. The influence of low-temperature degradation and cyclic loading on the fracture resistance of monolithic zirconia molar crowns. J. Mech. Behav. Bio-Med Mater. 2015, 47, 49–56. [Google Scholar] [CrossRef]
- Lameira, D.P.; Buarque e Silva, W.A.; Andrade e Silva, F.; De Souza, G.M. Fracture strength of aged monolithic and bilayer zirconia-based crowns. Biomed. Res. Int. 2015, 2015, 418641. [Google Scholar] [CrossRef]
- Zarone, F.; Russo, S.; Sorrentino, R. From porcelain fused to metal to zirconia: Clinical and experimental considerations. J. Dent. Mater. 2011, 27, 83–96. [Google Scholar] [CrossRef]
- Denry, I.; Kelly, J.R. State of the art of zirconia for dental applications. J. Dent. Mater. 2008, 24, 299–307. [Google Scholar] [CrossRef]
- Miyazaki, T.; Hotta, Y. CAD/CAM systems available for the fabrication of crown and bridge restorations. Aust. J. Dent. 2011, 56, 97–106. [Google Scholar] [CrossRef]
- Rekow, E.D.; Silvia, N.R.; Coehlo, P.G.; Zhang, Y.; Guess, P.; Thompson, V.P. Performance of dental ceramics: Challenges for improvements. J. Dent. Res. 2011, 90, 937–952. [Google Scholar] [CrossRef]
- Edelhoff, D.; Özcan, M. To what extent does the longevity of fixed dental prostheses depend on the function of the cement? Working Group 4 materials: Cementation. Clin. Oral Implant. Res. 2007, 18, 193–204. [Google Scholar] [CrossRef]
- Hitz, T.; Stawarczyk, B.; Fischer, J.; Hämmerle, C.H.; Sailer, I. Are self-adhesive resin cements a valid alternative to conventional resin cements? A laboratory study of the long-term bond strength. Dent. Mater. 2012, 28, 1183–1190. [Google Scholar] [CrossRef] [PubMed]
- Burke, F.J. Trends in indirect dentistry: 3. Luting materials. Dent. Update 2005, 32, 251–260. [Google Scholar] [CrossRef] [PubMed]
- Sunico-Segarra, M.; Segarra, A. Resin cements: Factors affecting clinical performance. In A Practical Clinical Guide to Resin Cements; Springer: Berlin/Heidelberg, Germany, 2015. [Google Scholar]
- Jiang, L.; Liao, Y.; Wan, Q.; Li, W. Effects of sintering temperature and particle size on the translucency of zirconium dioxide dental ceramic. J. Mater. Sci. Mater. Med. 2011, 22, 2429–2435. [Google Scholar] [CrossRef] [PubMed]
- Rosentritt, M.; Behr, M.; Kolbeck, C.; Handel, G. Marginal integrity of CAD/CAM fixed partial dentures. Eur. J. Dent. 2007, 1, 25–30. [Google Scholar] [CrossRef]
- Hoang, L. Accuracy and Precision of Die Spacer Thickness with Combined Computer-Aided Design and 3-D Printing Technology. Master’s Thesis, Marquette University, Milwaukee, WI, USA, 2014; pp. 1–31. [Google Scholar]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.G. Statistical power analyses using G* Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef]
- Soares, C.J.; Martins, L.R.; Fonseca, R.B.; Correr-Sobrinho, L.; Neto, A.J. Influence of cavity preparation design on fracture resistance of posterior leucite reinforced ceramic restorations. J. Prosthet. Dent. 2006, 95, 421–429. [Google Scholar] [CrossRef] [PubMed]
- Kocaagaoglu, H.; Kilinc, H.I.; Al-bayrak, H. Effect of digital impressions and production protocols on the adaptation of zirconia copings. J. Prosthet. Dent. 2017, 117, 102–108. [Google Scholar] [CrossRef]
- El-Helali, R.; Dowling, A.H.; Mcginley, E.L.; Duncan, H.F.; Fleming, G.J. Influence of resin-based composite restoration technique and endodontic access on cuspal deflection and cervical microleakage scores. J. Dent. 2013, 41, 216–222. [Google Scholar] [CrossRef]
- Korkut, L.; Cotert, H.S.; Kurtulumus, H. Marginal, internal fit and microleakage of zirconia infrastructures: An in vitro study. Oper. Dent. 2011, 36, 72–79. [Google Scholar] [CrossRef]
- Rosenstiel, S.F.; Land, M.F.; Fujimoto, J. Contemporary Fixed Prosthodontics, 5th ed.; Elsevier Inc.: Amsterdam, The Netherlands, 2016. [Google Scholar]
- Filser, F.; Kocher, P.; Gauckler, L.J. Net-shaping of ceramic components by direct ceramic machining. Assem. Autom. 2003, 23, 382–390. [Google Scholar] [CrossRef]
- Proussaefs, P. Crowns cemented on crown preparations lacking geometric resistance form. Part II: Effect of cement. J. Prosthodont. 2004, 13, 36–41. [Google Scholar] [CrossRef] [PubMed]
- Anunmana, C.; Charoenchitt, M.; Asvanund, C. Gap comparison between single crown and three-unit bridge zirconia substructures. J. Adv. Prosthodont. 2014, 6, 253. [Google Scholar] [CrossRef]
- Dimashkieh, M. The Effect of Veneering Porcelain on the Marginal Fit of Cercon Zirconia Copings. Ph.D. Thesis, Department of Prosthetic Dental Science Collage of Dentistry, King Saud University, Riyadh, Saudi Arabia, 2010. [Google Scholar]
- Shahrbaf, S.; Van Noort, R.; Mirzakouchaki, B.; Ghassemieh, E.; Martin, N. Fracture strength of machined ceramic crowns as a function of tooth preparation design and the elastic modulus of the cement. Dent. Mater. 2014, 30, 234–241. [Google Scholar] [CrossRef]
- Ortorp, A.; Onsson, D.J.; Mouhsen, A.; Vult Von Steyern, P. The fit of cobalt chromium three unit fixed dental prostheses fabricated with four different techniques: A comparative in vitro study. J. Dent. Mater. 2011, 27, 356–363. [Google Scholar] [CrossRef] [PubMed]
- Holden, J.E.; Goldstein, G.R.; Hittelman, E.L.; Clark, E.A. Comparison of the marginal fit of pressable ceramic to metal ceramic restorations. J. Prosthodont. 2009, 18, 645–648. [Google Scholar] [CrossRef]
- Lombardas, P.; Carbunaru, A.; McAlarney, M.E.; Toothaker, R.W. Dimensional accuracy of castings produced with ringless and metal ring investment systems. J. Prosthet. Dent. 2000, 84, 27–31. [Google Scholar] [CrossRef]
- Romeo, E.; Iorio, M.; Storelli, S.; Camandona, M.; Abati, S. Marginal adaptation of full coverage CAD/CAM restorations: In vitro study using a non-destructive method. J. Minerva Stomatol. 2009, 58, 61–72. [Google Scholar]
- Jonathan, N.G. A Comparison of Crown Marginal Fit Fabricated Using Digital and Conventional. Methods. Master’s Thesis, Department of Maxillofacial Prosthodontics, University of British Columbia, Vancouver, BC, Canada, 2013. [Google Scholar]
- Wolfart, S.; Wegner, S.M.; Al-Halabi, A.; Kern, M. Clinical evaluation of marginal fit of a new experimental all ceramic system before and after cementation. Int. J. Prosthodont. 2003, 16, 587–592. [Google Scholar]
- Aschenbrenner, C.M.; Lang, R.; Handel, G.; Behr, M. Analysis of marginal adaptation and sealing to enamel and dentin of four self-adhesive resin cements. J. Clin. Oral. Investig. 2012, 16, 191–200. [Google Scholar] [CrossRef]
- Contrepois, M.; Soenen, A.; Bartala, M.; Laviole, O. Marginal adaptation of ceramic crowns: A systematic review. J. Prosthet. Dent. 2013, 110, 447–454. [Google Scholar] [CrossRef]
- Podhorsky, A.; Rehmann, P.; Wöstmann, B. Tooth preparation for full-coverage restorations—A literature review. Clin. Oral Investig. 2015, 19, 959–968. [Google Scholar] [CrossRef]
- Ferrini, F.; Paolone, G.; Di Domenico, G.L.; Pagani, N.; Gherlone, E.F. SEM Evaluation of the Marginal Accuracy of Zirconia, Lithium Disilicate, and Composite Single Crowns Created by CAD/CAM Method: Comparative Analysis of Different Materials. Materials 2023, 16, 2413. [Google Scholar] [CrossRef] [PubMed]
- Karatasli, Ö.; Kursoglu, P.; Capa, N.; Kazazoglu, E. Comparison of the marginal fit of different coping materials and designs produced by computer aided manufacturing systems. Dent. Mater. J. 2011, 30, 97–102. [Google Scholar] [CrossRef] [PubMed]
- Malhotra, S.; Bhullar, K.K.; Kaur, S.; Malhotra, M.; Kaur, R.; Handa, A. Comparative evaluation of compressive strength and flexural strength of gc gold hybrid, gic conventional and resin-modified glass-ionomer cement. J. Pharm. Bioallied Sci. 2022, 14 (Suppl. S1), S214. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.J.; Millstein, P.L.; Nathanson, D. Effects of cement, cement space, marginal design, seating aid materials, and seating force on crown cementation. J. Prosthet. Dent. 1992, 67, 786–790. [Google Scholar] [CrossRef] [PubMed]
- D’Souza, R.; Shetty, O.; Puppala, P.; Shetty, N. A better bond: Luting simplified. Int. J. Prsthodont. Restor. Dent. 2012, 2, 77–81. [Google Scholar] [CrossRef]
- Stappert, C.F.; Dai, M.; Chitmongkolsuk, S.; Gerds, T.; Strub, J.R. Marginal adaptation of three unit fixed partial dentures constructed from pressed ceramic systems. Br. J. Dent. 2004, 196, 766–770. [Google Scholar] [CrossRef] [PubMed]
- Okutan, M.; Heydecke, G.; Butz, F.; Strub, J.R. Fracture load and marginal fit of shrinkage free ZrSiO4 all ceramic crowns after chewing simulation. J. Oral Rehabil. 2006, 33, 827–832. [Google Scholar] [CrossRef]
- Gu, X.H.; Kern, M. Marginal discrepancies and leakage of all ceramic crowns: Influence of luting agents and aging conditions. Int. J. Prosthodont. 2003, 16, 109–116. [Google Scholar]
- Suarez, M.J.; Rivera, B.; Pradies, G. Evaluation of the absolute marginal discrepancy of zirconia-based ceramic copings. J. Prosthet. Dent. 2011, 105, 108–114. [Google Scholar]



| Tests of Normality | |||||||
|---|---|---|---|---|---|---|---|
| Tested Groups | Subgroups | Kolmogorov–Smirnov | Shapiro–Wilk | ||||
| Statistic | df | Sig. | Statistic | df | Sig. | ||
| A | AI | 0.180 | 10 | 0.21 | 0.918 | 10 | 0.339 |
| A2 | 0.174 | 10 | 0.23 | 0.926 | 10 | 0.407 | |
| B | B1 | 0.228 | 10 | 0.151 | 0.846 | 10 | 0.052 |
| B2 | 0.221 | 10 | 0.184 | 0.886 | 10 | 0.153 | |
| Groups | Subgroups | N | Pre-Cementation | |||
|---|---|---|---|---|---|---|
| Min. | Max. | Mean | ±SD | |||
| A | A1 | 10 | 47.15 | 111.25 | 80.284 | 23.021 |
| A2 | 10 | 68.35 | 110.85 | 95.372 | 13.407 | |
| B | B1 | 10 | 66.37 | 117.32 | 101.21 | 14.278 |
| B2 | 10 | 104.52 | 136.67 | 118.597 | 9.956 | |
| Paired Samples Test | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Tested Groups/PRE | Paired Differences | t | df | Sig. (2-Tailed) | |||||
| Mean | Std. Deviation | Std. Error Mean | 95% Confidence Interval of the Difference | ||||||
| Lower | Upper | ||||||||
| Pair 1 | A1-A2 | −4.03300 | 29.42142 | 9.30387 | −25.07981 | 17.01381 | −0.433 | 9 | 0.675 |
| Pair 2 | A1-B1 | −20.96700 | 32.56010 | 10.29641 | −44.25909 | 2.32509 | −2.036 | 9 | 0.072 |
| Pair 3 | A1-B2 | −23.76000 | 22.58261 | 7.14125 | −39.91463 | −7.60537- | −3.327 | 9 | 0.009 ** |
| Pair 4 | A2-B1 | −16.93400 | 17.58250 | 5.56007 | −29.51176 | −4.35624- | −3.046 | 9 | 0.01 * |
| Pair 5 | A2-B2 | −19.72700 | 15.64231 | 4.94653 | −30.91684 | −8.53716- | −3.988 | 9 | 0.003 ** |
| Pair 6 | B1-B2 | −2.79300 | 17.11347 | 5.41175 | −15.03524 | 9.44924 | −0.516 | 9 | 0.618 |
| Statistics/PRE | AI | A2 | B1 | B2 |
|---|---|---|---|---|
| N | 10 | 10 | 10 | 10 |
| Mean | A 80.284 | B 95.372 | C 101.21 | D 118.597 |
| ±Std. Deviation | 23.02 | 13.407 | 14.278 | 9.959 |
| LSD | 3.012 | |||
| p value | F = 6.22 p value = 0.002 H.SIG | |||
| Tests of Normality | ||||||
|---|---|---|---|---|---|---|
| Tested Groups Post | Kolmogorov–Smirnov | Shapiro–Wilk | ||||
| Statistic | df | Sig. | Statistic | df | Sig. | |
| A1 | 0.146 | 10 | 0.21 | 0.937 | 10 | 0.515 |
| A2 | 0.165 | 10 | 0.23 | 0.922 | 10 | 0.375 |
| B1 | 0.145 | 10 | 0.12 | 0.932 | 10 | 0.466 |
| B2 | 0.190 | 10 | 0.22 | 0.943 | 10 | 0.592 |
| Groups | Subgroups | N | Descriptive Statistics/Post-Cementation | |||
|---|---|---|---|---|---|---|
| Min. | Max. | Mean | ±SD | |||
| A | A1 | 10 | 73.07 | 122.05 | 95.442 | 17.598 |
| A2 | 10 | 91.45 | 119.30 | 108.424 | 8.807 | |
| B | B1 | 10 | 82.82 | 137.75 | 116.758 | 16.151 |
| B2 | 10 | 119.60 | 146.55 | 134.806 | 8.114 | |
| Paired Samples Test | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Tested Groups/Post | Paired Differences | t | df | Sig. (2-Tailed) | |||||
| Mean | Std. Deviation | Std. Error Mean | 95% Confidence Interval of the Difference | ||||||
| Lower | Upper | ||||||||
| Pair 1 | A1-A2 | −12.98800 | 20.69533 | 6.54444 | −27.79255 | 1.81655 | −1.985 | 9 | 0.078 |
| Pair 2 | A1-B1 | −21.23300 | 29.35672 | 9.28341 | −42.23353 | −0.23247 | −2.287 | 9 | 0.0481 * |
| Pair 3 | A1-B2 | −39.36400 | 18.20305 | 5.75631 | −52.38568 | −26.34232 | −6.838 | 9 | 0.0001 *** |
| Pair 4 | A2-B1 | −8.24500 | 21.88527 | 6.92073 | −23.90078 | 7.41078 | −1.191 | 9 | 0.264 |
| Pair 5 | A2-B2 | −26.37600 | 12.10464 | 3.82782 | −35.03514 | −17.71686 | −6.891 | 9 | 0.0001 *** |
| Pair 6 | B1-B2 | −18.13100 | 20.75647 | 6.56377 | −32.97928 | −3.28272 | −2.762 | 9 | 0.022 ** |
| Statistics/Post | A1 | A2 | B1 | B2 |
|---|---|---|---|---|
| N | 10 | 10 | 10 | 10 |
| Mean | A 95.442 |
B 108.424 |
B 116.758 |
C 134.806 |
| ±Std. Deviation | 17.598 | 8.807 | 16.151 | 8.114 |
| LSD | 5.38 | |||
| p value | F = 15.09 p value = 0.0001 H.SIG | |||
| Statistics | A1 | A2 | B1 | B2 |
|---|---|---|---|---|
| N | 10 | 10 | 10 | 10 |
| pre Mean ± SD | 80.28 ± 23.02 | 95.37 ± 13.41 | 101.21 ± 14.28 | 118.59 ± 9.95 |
| Post Mean ± SD | 95.4 ± 17.6 | 108.4 ± 8.81 | 116.76 ± 16.2 | 134.81 ± 8.1 |
| t test | 2.74 | 29.5 | 5.08 | 75.5 |
| p value | 0.115 | 0.000 * | 0.037 * | 0.000 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khekan, A.; Kordaß, B. Comparing Zirconium Crown Marginal Adaptation in Preparations with Two Different Occlusal Reductions. Dent. J. 2024, 12, 77. https://doi.org/10.3390/dj12030077
Khekan A, Kordaß B. Comparing Zirconium Crown Marginal Adaptation in Preparations with Two Different Occlusal Reductions. Dentistry Journal. 2024; 12(3):77. https://doi.org/10.3390/dj12030077
Chicago/Turabian StyleKhekan, Ali, and Bernd Kordaß. 2024. "Comparing Zirconium Crown Marginal Adaptation in Preparations with Two Different Occlusal Reductions" Dentistry Journal 12, no. 3: 77. https://doi.org/10.3390/dj12030077
APA StyleKhekan, A., & Kordaß, B. (2024). Comparing Zirconium Crown Marginal Adaptation in Preparations with Two Different Occlusal Reductions. Dentistry Journal, 12(3), 77. https://doi.org/10.3390/dj12030077






