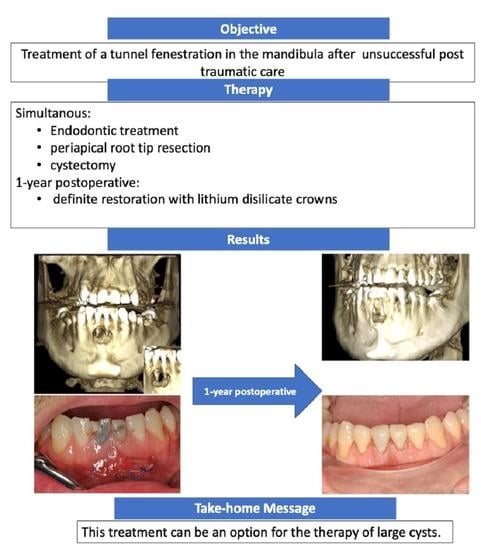
Tunnel Fenestration of the Mandibula after Unsuccessful Post Traumatic Treatment: A Case Report of the One Year Follow-Up
Abstract
:1. Introduction
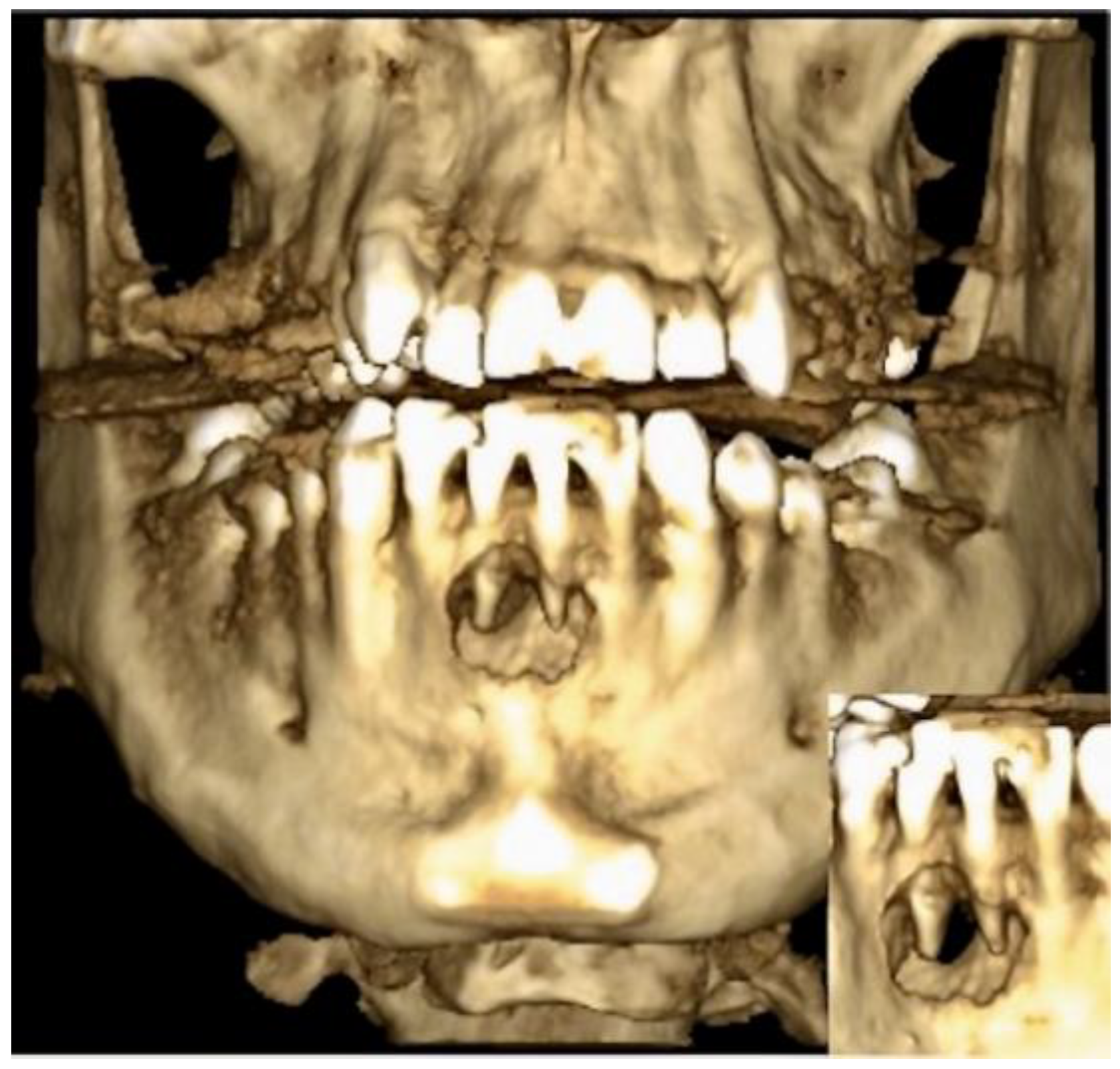
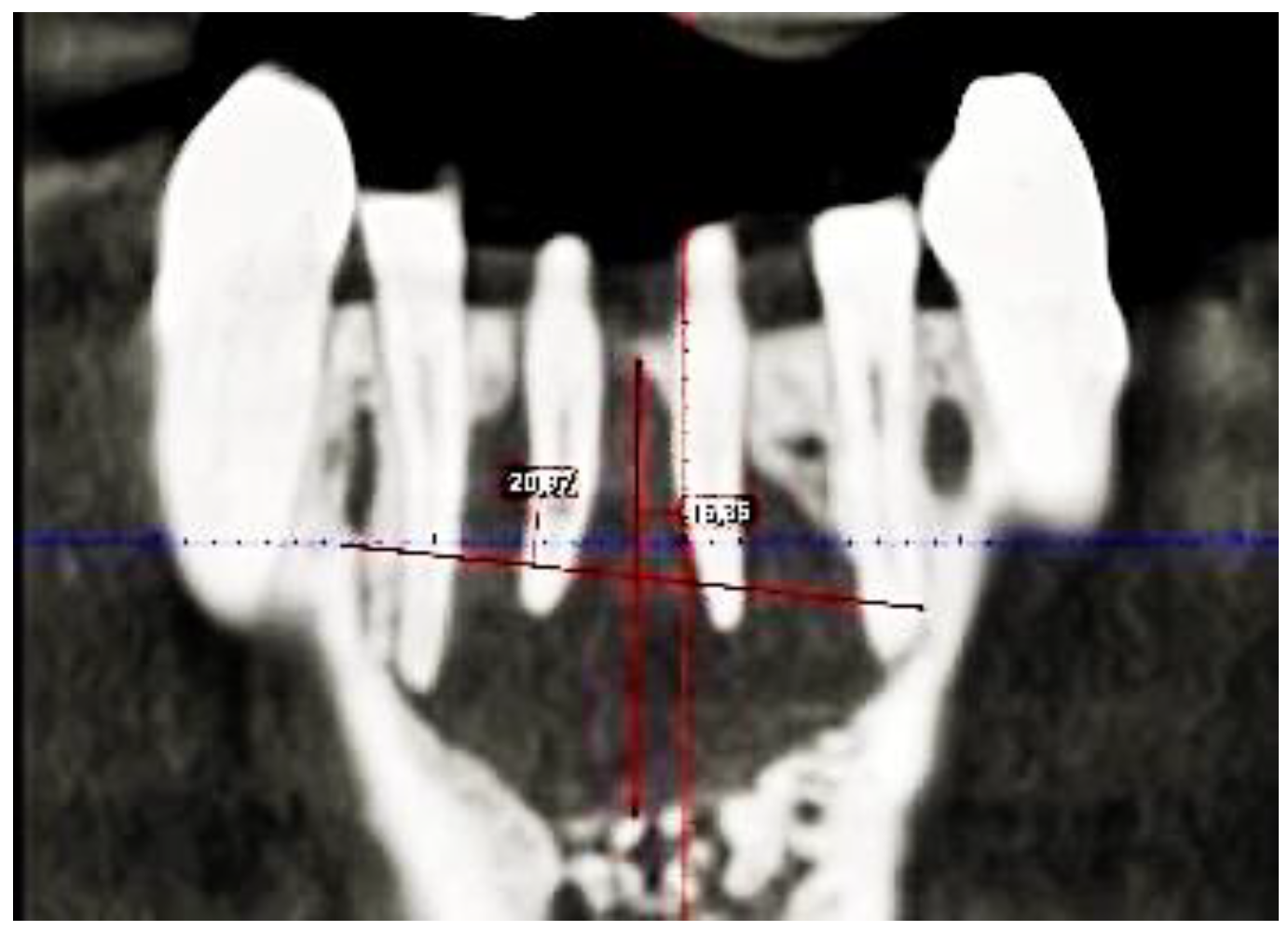
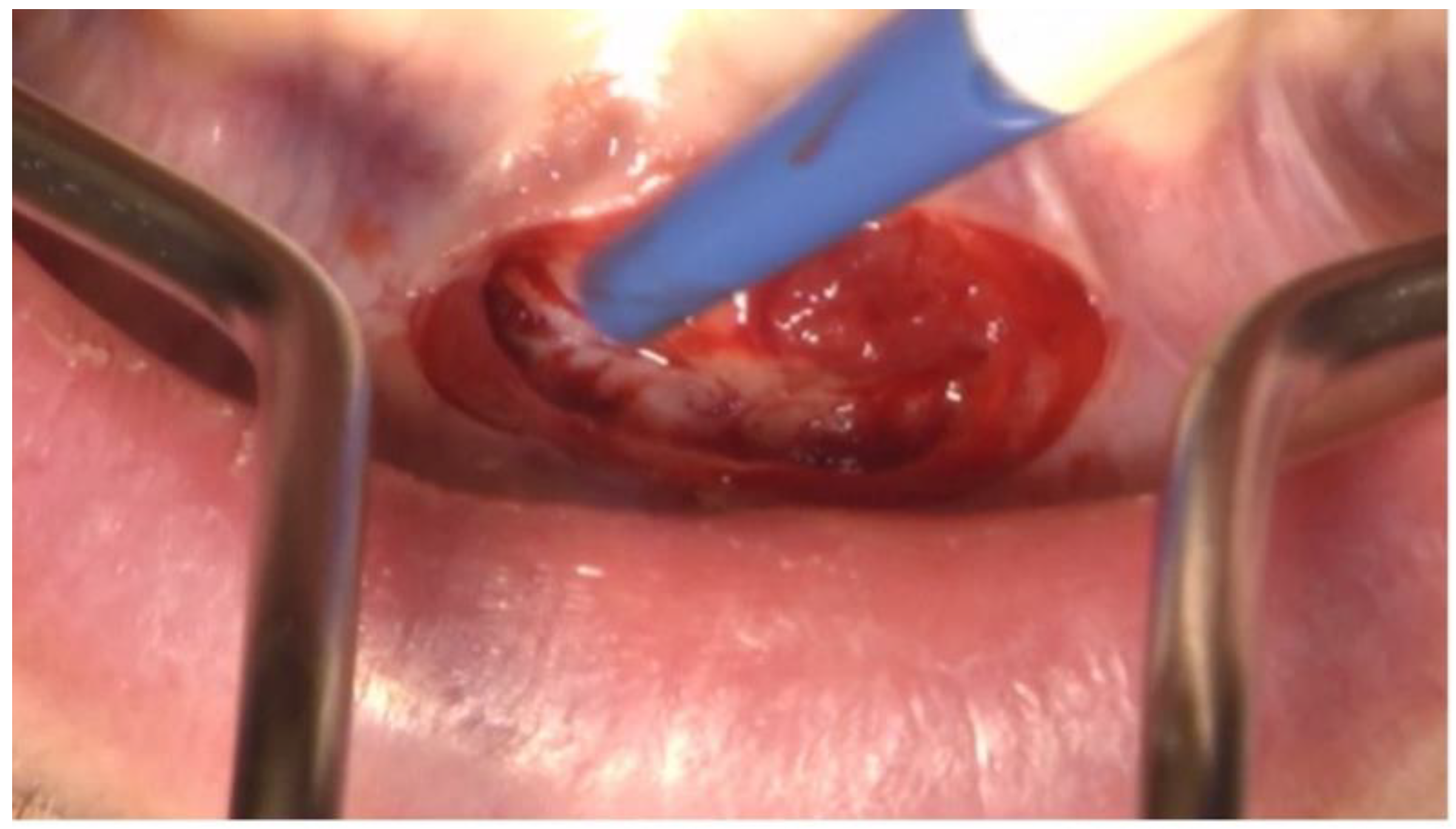
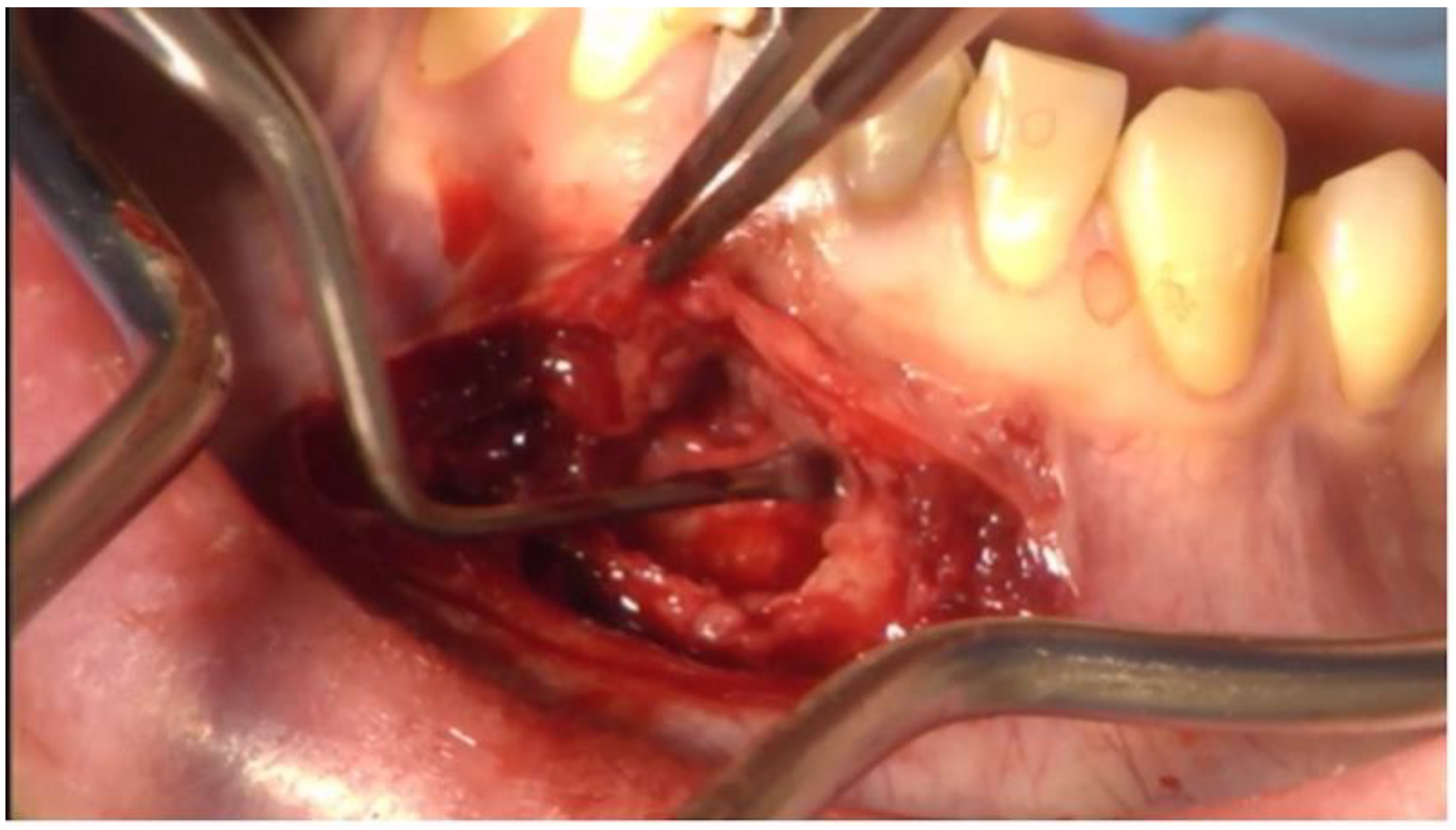
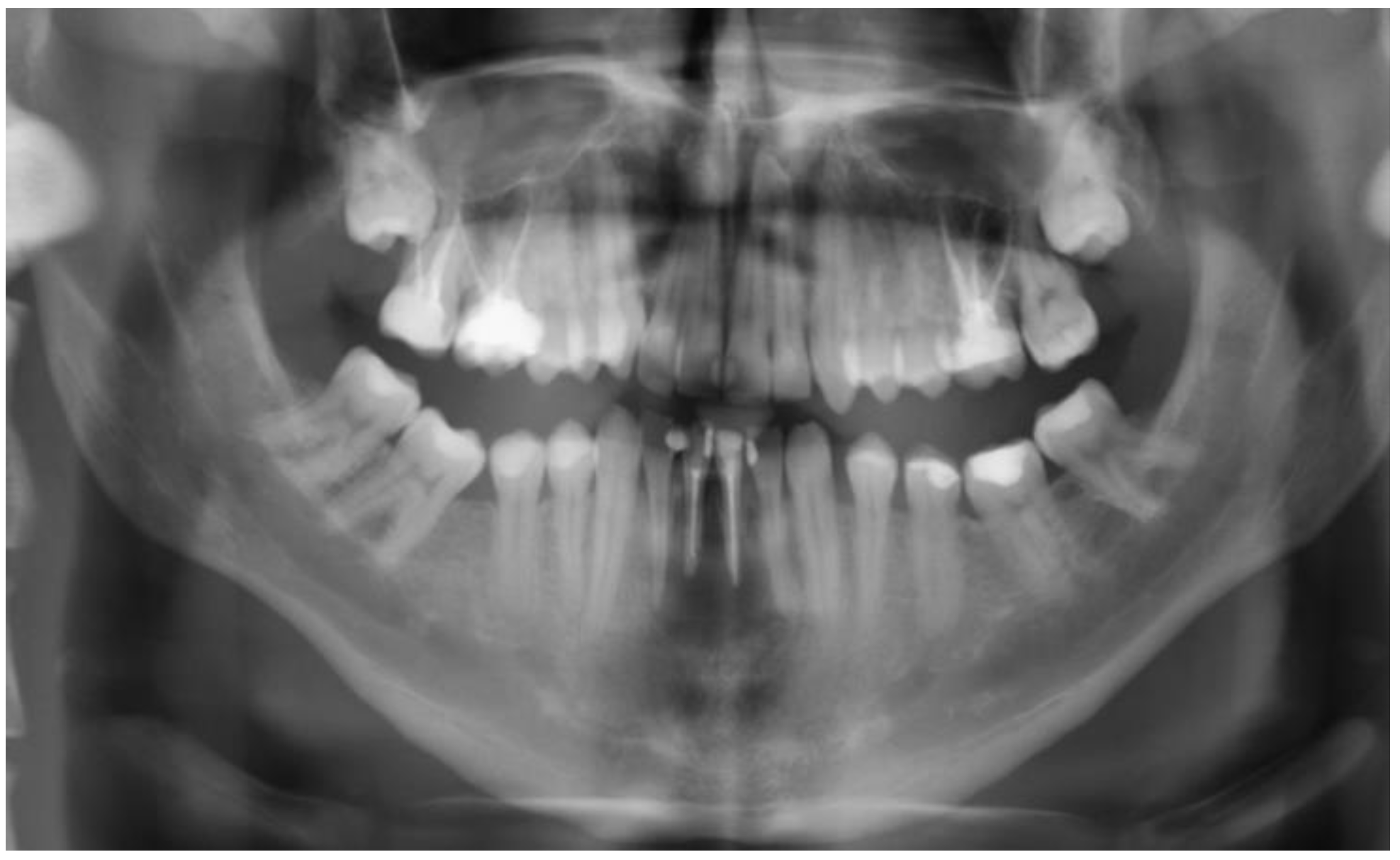
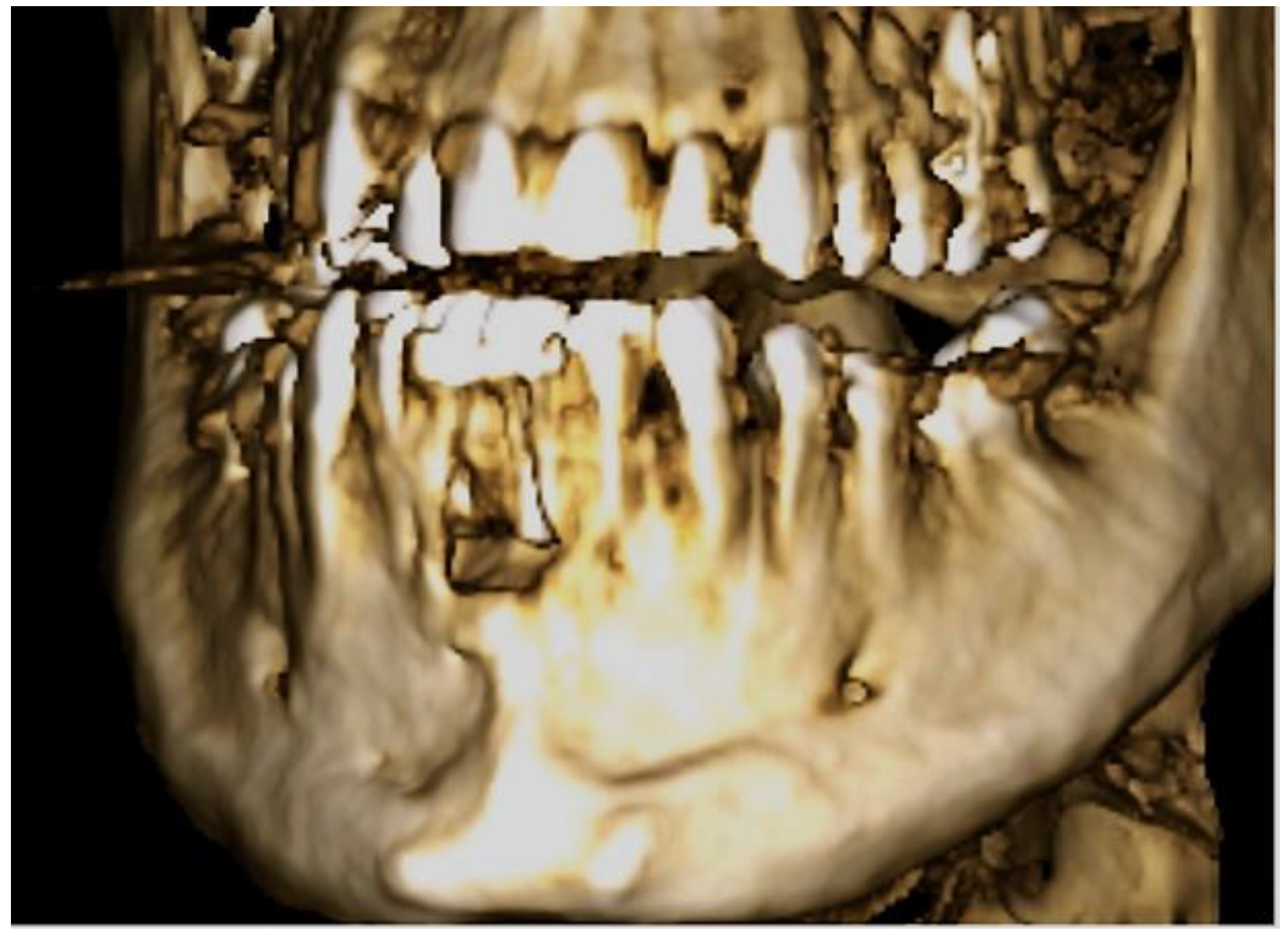
2. Case Description
3. Clinical Procedure and Outcome
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rosenberg, P.A.; Frisbie, J.; Lee, J.; Lee, K.; Frommer, H.; Kottal, S.; Phelan, J.; Lin, L.; Fisch, G. Evaluation of pathologists (histopathology) and radiologists (cone beam computed tomography) differentiating radicular cysts from granulomas. J. Endod. 2010, 36, 423–428. [Google Scholar] [CrossRef] [PubMed]
- Mammadov, K. Spektrum und Verteilung odontogener Zysten–Retrospektive Analyse eines Patientenkollektivs zwischen 2003–2014. Ph.D. Thesis, Ludwig Maximilian University of Munich, Munich, Germany, 2020. [Google Scholar]
- Meningaud, J.-P.; Oprean, N.; Pitak-Arnnop, P.; Bertrand, J.-C. Odontogenic cysts: A clinical study of 695 cases. J. Oral Sci. 2006, 48, 59–62. [Google Scholar] [CrossRef] [PubMed]
- Ochsenius, G.; Escobar, E.; Godoy, L.; Peñafiel, C. Odontogenic cysts: Analysis of 2944 cases in Chile. Med. Oral Patol. Oral Cir. Bucal 2007, 12, E85–E91. [Google Scholar] [PubMed]
- Gutwald, R.; Gellrich, N.-C.; Schmelzeisen, R. (Eds.) Zahnärztliche Chirurgie und Implantologie. Für Studium, Examen und Beruf, 3rd ed.; Deutscher Zahnärzte Verlag: Cologne, Germany, 2019. [Google Scholar]
- Ettl, T.; Gosau, M.; Sader, R.; Reichert, T.E. Jaw cysts-filling or no filling after enucleation? A review. J. Cranio-Maxillo-Facial Surg. Off. Publ. Eur. Assoc. Cranio-Maxillo-Facial Surg. 2012, 40, 485–493. [Google Scholar] [CrossRef]
- Arotiba, G.T.; Arotiba, J.T.; Taiwo, A.O. Biologic, anatomic and clinical considerations in the management of the classic intraosseous ameloblastoma of the jaws. Niger. Q. J. Hosp. Med. 2010, 20, 55–63. [Google Scholar] [CrossRef]
- Nik Abdul Ghani, N.R.; Abdul Hamid, N.F.; Karobari, M.I. Tunnel’ radicular cyst and its management with root canal treatment and periapical surgery: A case report. Clin. Case Rep. 2020, 8, 1387–1391. [Google Scholar] [CrossRef]
- Zhao, R.; Yang, R.; Cooper, P.R.; Khurshid, Z.; Shavandi, A.; Ratnayake, J. Bone Grafts and Substitutes in Dentistry: A Review of Current Trends and Developments. Molecules 2021, 26, 3007. [Google Scholar] [CrossRef]
- Pradeep, K.; Kudva, A.; Narayanamoorthy, V.; Cariappa, K.M.; Saraswathi, M.V. Platelet-rich fibrin combined with synthetic nanocrystalline hydroxy apatite granules in the management of radicular cyst. Niger. J. Clin. Pract. 2016, 19, 688–691. [Google Scholar] [CrossRef]
- Baumann, B.; Saez, P.; Curien, R.; Engels-Deutsch, M. Surgical Treatment of Voluminous Jaw Cysts with a Buccal Plate: A Study of 20 Clinical Cases. J. Contemp. Dent. Pract. 2021, 22, 1069–1075. [Google Scholar] [CrossRef]
- Sayed, M.E.; Jurado, C.A.; Tsujimoto, A.; Garcia-Cortes, J.O. Clinical decision-making regarding endodontic therapy vs extraction and implant-assisted replacement: A systematic review and meta-analysis. Gen. Dent. 2021, 69, 52–57. [Google Scholar]
- Torabinejad, M.; White, S.N. Endodontic treatment options after unsuccessful initial root canal treatment: Alternatives to single-tooth implants. J. Am. Dent. Assoc. 2016, 147, 214–220. [Google Scholar] [CrossRef]
- Naujokat, H. Das Zahntrauma: Sorforttherapie und langfristige Versorgungsmöglichkeiten.AGOKi 21. Jahrestagung. 03.10.2021. Available online: https://www.ag-kiefer.de/online-symposium2021 (accessed on 23 November 2022).
- Nolte, D.; Beck, J.; Berger, C.; Bucher, C.; Chenot, R.; Deppe, H.; Ebeleseder, K.; Esch, J.; Esser, W.; Frank, M.; et al. LeitlinienTEXT (040416)_Dentales Trauma 083-004+SondervotumKZBV-final_sa; AWMF: Duesseldorf, Germany, 2015. [Google Scholar]
- Hülsmann, M. (Ed.) Endodontie; Thieme: Stuttgart, Germany, 2008. [Google Scholar]
- Thomas, P.; Krishna Pillai, R.; Pushparajan Ramakrishnan, B.; Palani, J. An insight into internal resorption. ISRN Dent. 2014, 2014, 759326. [Google Scholar] [CrossRef]
- Harris, M.; Toller, P. The pathogenesis of dental cysts. Br. Med. Bull. 1975, 31, 159–163. [Google Scholar] [CrossRef]
- Covani, U.; Barone, A. Piezosurgical treatment of unicystic ameloblastoma. J. Periodontol. 2007, 78, 1342–1347. [Google Scholar] [CrossRef] [PubMed]
- Fernandez de Grado, G.; Keller, L.; Idoux-Gillet, Y.; Wagner, Q.; Musset, A.-M.; Benkirane-Jessel, N.; Bornert, F.; Offner, D. Bone substitutes: A review of their characteristics, clinical use, and perspectives for large bone defects management. J. Tissue Eng. 2018, 9, 2041731418776819. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Yao, Q.-Y.; Zhu, H.-Y. Efficacy of bone grafts in jaw cystic lesions: A systematic review. World J. Clin. Cases 2022, 10, 2801–2810. [Google Scholar] [CrossRef] [PubMed]
- Yadav, V.S.; Gupta, V.; Chawla, A.; Tewari, N.; Yadav, R. Successful management of a large mucosal fenestration at 18-months follow-up. J. Esthet. Restor. Dent. 2022, 34, 445–450. [Google Scholar] [CrossRef]
- Taschieri, S.; Del Fabbro, M.; Testori, T.; Weinstein, R. Efficacy of xenogeneic bone grafting with guided tissue regeneration in the management of bone defects after surgical endodontics. J. Oral Maxillofac. Surg. Off. J. Am. Assoc. Oral Maxillofac. Surg. 2007, 65, 1121–1127. [Google Scholar] [CrossRef] [PubMed]
- Rath, M. Untersuchung der Einflussfaktoren hinsichtlich der Langzeitprognose nach Wurzelspitzenresektion: Eine retrospektive Fallstudie. Ph.D. Thesis, University of Ulm, Ulm, Germany, 2017. [Google Scholar]
- Hidding, J.; Hemprich, A. Langzeiterfahrungen beim Einsatz von grossen Uberbrückungsplatten nach Unterkiefer-Teilresektion. Long-term experiences with large bridge-work after partial resection of the lower jaw. Stomatol. DDR 1989, 39, 455–458. (In German) [Google Scholar] [PubMed]
- Von Arx, T. Periradikulare Chirurgie-Teil I. Schweiz. Mon. Zahnmed. 2001, 111, 579–585. [Google Scholar]
- Gagliani, M.M.; Gorni, F.G.M.; Strohmenger, L. Periapical resurgery versus periapical surgery: A 5-year longitudinal comparison. Int. Endod. J. 2005, 38, 320–327. [Google Scholar] [CrossRef] [PubMed]
- Wesson, C.M.; Gale, T.M. Molar apicectomy with amalgam root-end filling: Results of a prospective study in two district general hospitals. Br. Dent. J. 2003, 195, 707–714. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tomasi, C.; Wennström, J.L.; Berglundh, T. Longevity of teeth and implants—A systematic review. J. Oral Rehabil. 2008, 35 (Suppl. S1), 23–32. [Google Scholar] [CrossRef] [PubMed]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gillner, P.; Mosch, R.; von See, C. Tunnel Fenestration of the Mandibula after Unsuccessful Post Traumatic Treatment: A Case Report of the One Year Follow-Up. Dent. J. 2023, 11, 37. https://doi.org/10.3390/dj11020037
Gillner P, Mosch R, von See C. Tunnel Fenestration of the Mandibula after Unsuccessful Post Traumatic Treatment: A Case Report of the One Year Follow-Up. Dentistry Journal. 2023; 11(2):37. https://doi.org/10.3390/dj11020037
Chicago/Turabian StyleGillner, Peter, Richard Mosch, and Constantin von See. 2023. "Tunnel Fenestration of the Mandibula after Unsuccessful Post Traumatic Treatment: A Case Report of the One Year Follow-Up" Dentistry Journal 11, no. 2: 37. https://doi.org/10.3390/dj11020037