Advances in Preventive and Therapeutic Approaches for Dental Erosion: A Systematic Review
Abstract
1. Introduction
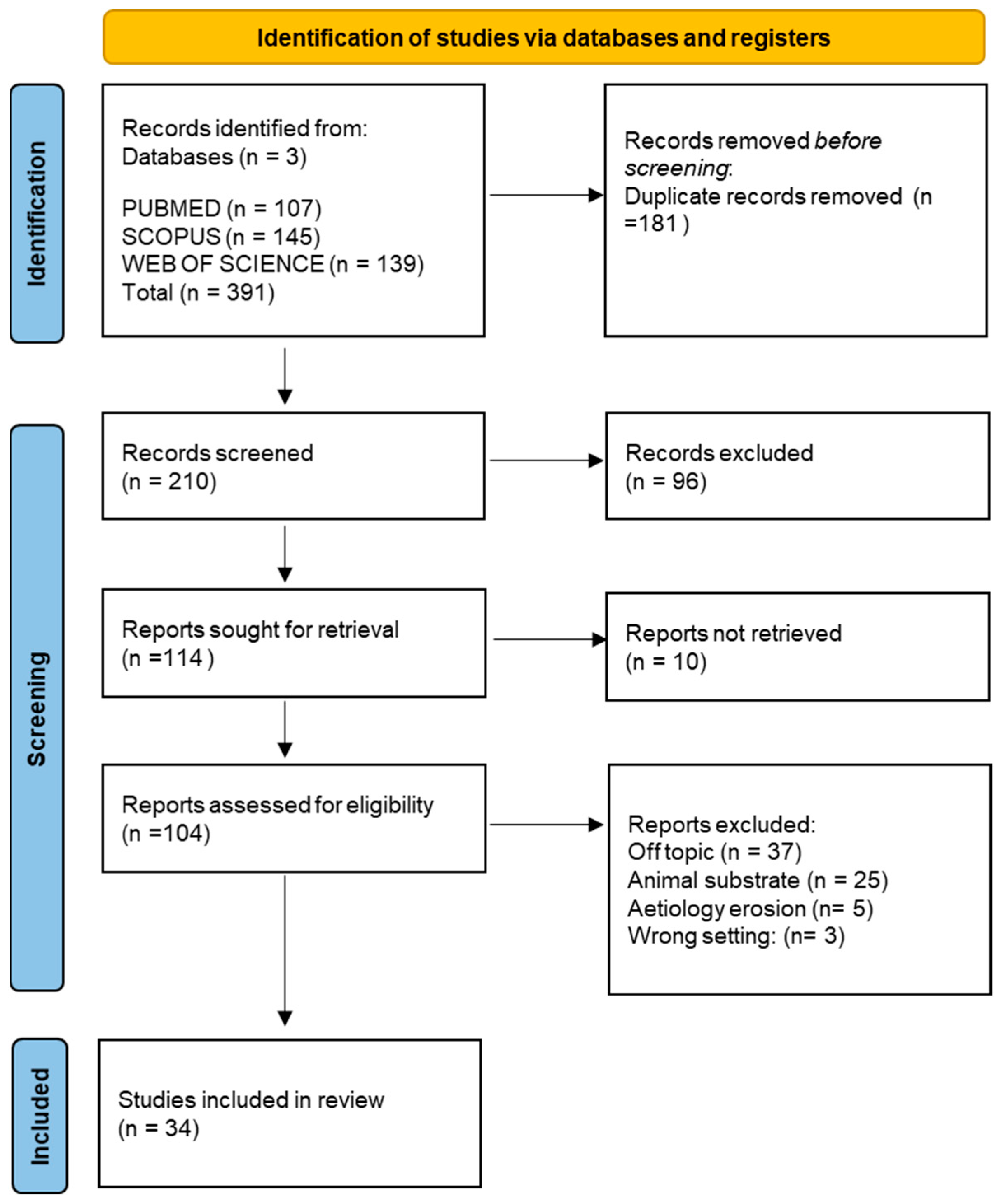
2. Materials and Methods
- Studies in English.
- Articles whose full text is available.
- Clinical studies and in vitro studies were performed only on human teeth.
- Reviews, letters, or commentaries.
- Studies in which animal enamel was used.
- Studies that did not deal with dental erosion.
- Studies that discussed only the diagnosis of the disease.
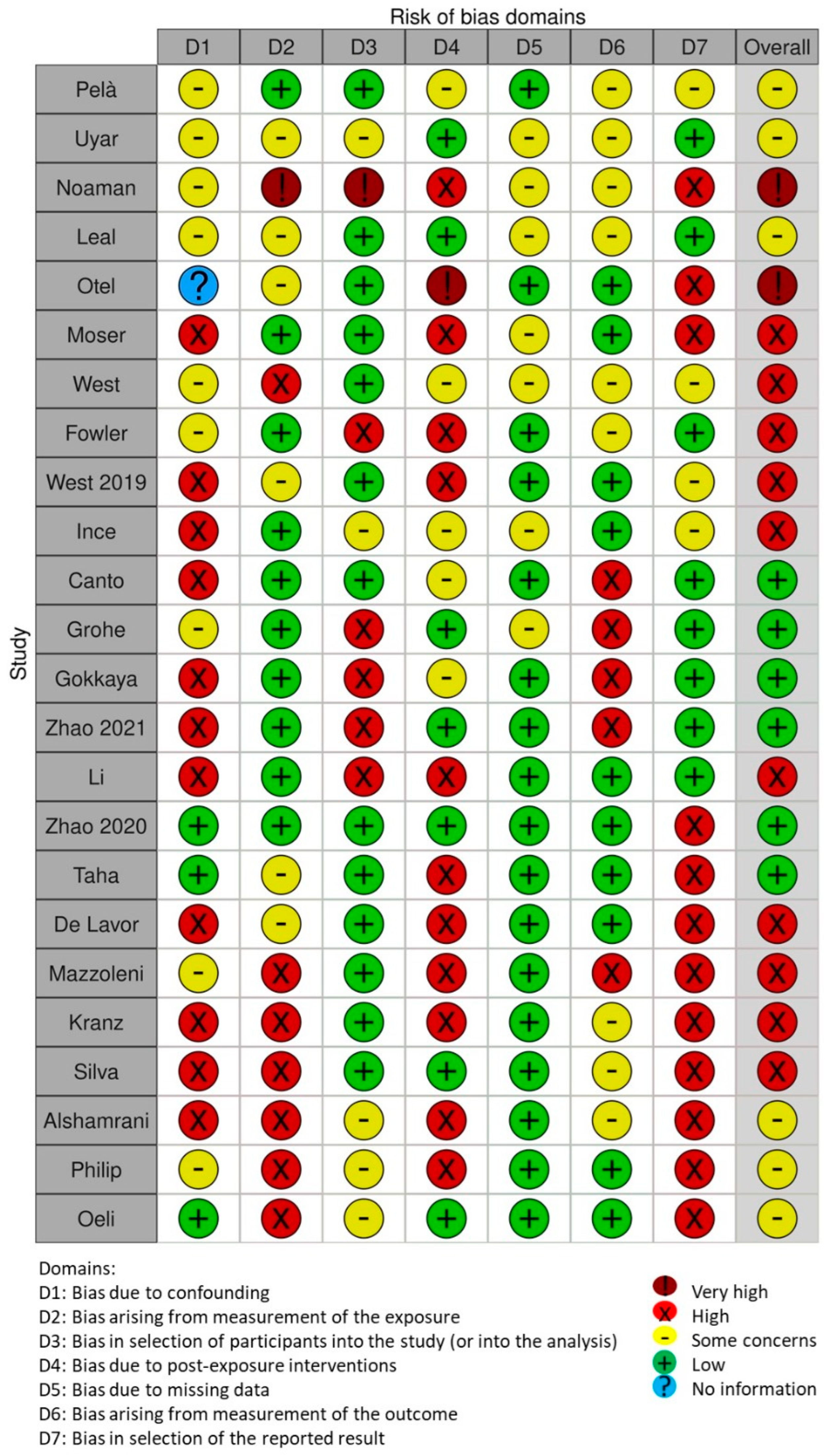
Quality Assessment
3. Results
Quality Assessment and Risk of Bias
4. Discussion
4.1. Preventive Therapy
4.2. Dental Treatment
4.3. Limitation
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
Abbreviations
| AmF | amine fluoride |
| BEWE | basic erosive wear examination |
| Ca2+-MSN | calcium mesoporous silica |
| CaneCPI-5 | sugarcane cystatin |
| CPP | casein phosphopeptide |
| CPP-ACP | casein phosphopeptide-amorphous calcium phosphate |
| CZnHA | zinc-hydroxyapatite carbonate |
| EDL | Dentin erosion |
| EGCG | Fluoride and epigallocatechin gallate |
| ETW | erosive tooth wear |
| GERD | gastroesophageal reflux disease |
| HA | Hydroxyapatite |
| IADR | International Cariology Research Group for Dental Research |
| NaF | Sodium Fluoride |
| NHA | Nano-Hydroxyapatite |
| OHIP-49 | Oral-Health-Impact-Profile-49 |
| ORCA | European Organization for Caries Research |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| RCT | Randomized clinical trial |
| PVM/MA | polyvinyl methyl ether/maleic acid copolymers. |
| SnF2/SnCl2 | stannous fluoride |
| TiF4 | titanium tetrafluoride |
| TP | toothpaste |
References
- Addy, M.; Shellis, R.P. Interaction between Attrition, Abrasion and Erosion in Tooth Wear. Dent. Eros. 2006, 20, 17–31. [Google Scholar] [CrossRef]
- Schlueter, N.; Amaechi, B.T.; Bartlett, D.; Buzalaf, M.A.R.; Carvalho, T.S.; Ganss, C.; Hara, A.T.; Huysmans, M.-C.D.N.J.M.; Lussi, A.; Moazzez, R.; et al. Terminology of Erosive Tooth Wear: Consensus Report of a Workshop Organized by the ORCA and the Cariology Research Group of the IADR. Caries Res. 2020, 54, 2–6. [Google Scholar] [CrossRef] [PubMed]
- Inchingolo, A.M.; Malcangi, G.; Ferrante, L.; Del Vecchio, G.; Viapiano, F.; Mancini, A.; Inchingolo, F.; Inchingolo, A.D.; Di Venere, D.; Dipalma, G.; et al. Damage from Carbonated Soft Drinks on Enamel: A Systematic Review. Nutrients 2023, 15, 1785. [Google Scholar] [CrossRef] [PubMed]
- Ganss, C.; Young, A.; Lussi, A. Tooth Wear and Erosion: Methodological Issues in Epidemiological and Public Health Research and the Future Research Agenda. Community Dent. Health 2011, 28, 191–195. [Google Scholar] [CrossRef] [PubMed]
- Bartlett, D.W.; Fares, J.; Shirodaria, S.; Chiu, K.; Ahmad, N.; Sherriff, M. The Association of Tooth Wear, Diet and Dietary Habits in Adults Aged 18–30 Years Old. J. Dent. 2011, 39, 811–816. [Google Scholar] [CrossRef] [PubMed]
- Inchingolo, F.; Tatullo, M.; Marrelli, M.; Inchingolo, A.M.; Picciariello, V.; Inchingolo, A.D.; Dipalma, G.; Vermesan, D.; Cagiano, R. Clinical Trial with Bromelain in Third Molar Exodontia. Eur. Rev. Med. Pharmacol. Sci. 2010, 14, 771–774. [Google Scholar]
- Cantore, S.; Mirgaldi, R.; Ballini, A.; Coscia, M.F.; Scacco, S.; Papa, F.; Inchingolo, F.; Dipalma, G.; De Vito, D. Cytokine Gene Polymorphisms Associate with Microbiogical Agents in Periodontal Disease: Our Experience. Int. J. Med. Sci. 2014, 11, 674–679. [Google Scholar] [CrossRef]
- Salas, M.M.S.; Nascimento, G.G.; Vargas-Ferreira, F.; Tarquinio, S.B.C.; Huysmans, M.C.D.N.J.M.; Demarco, F.F. Diet Influenced Tooth Erosion Prevalence in Children and Adolescents: Results of a Meta-Analysis and Meta-Regression. J. Dent. 2015, 43, 865–875. [Google Scholar] [CrossRef]
- Bertoldi, C.; Lucchi, A.; Zaffe, D. Effects of Soft-Drinks and Remineralising Treatment on Teeth Assessed by Morphological and Quantitative X-Ray Investigations. Eur. J. Paediatr. Dent. 2015, 16, 263–271. [Google Scholar]
- Mahoney, E.K.; Kilpatrick, N.M. Dental Erosion: Part 1. Aetiology and Prevalence of Dental Erosion. N. Z. Dent. J. 2003, 99, 33–41. [Google Scholar]
- Ramirez, V.; Lussi, A.; Marró Freitte, M.L.; Vasquez, P.; Aránguiz, V. Relationship between Intrinsic and Extrinsic Factors with Erosive Tooth Wear in Adults: A Cross-Sectional Study. Braz. Oral Res. 2022, 36, e0118. [Google Scholar] [CrossRef] [PubMed]
- Meurman, J.H.; Gate, J.M. Pathogenesis and Modifying Factors of Dental Erosion. Eur. J. Oral Sci. 1996, 104, 199–206. [Google Scholar] [CrossRef] [PubMed]
- Benages, A.; Muñoz, J.V.; Sanchiz, V.; Mora, F.; Mínguez, M. Dental Erosion as Extraoesophageal Manifestation of Gastro-oesophageal Reflux. Gut 2006, 55, 1050–1051. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Moazzez, R.; Bartlett, D. Intrinsic Causes of Erosion. Monogr. Oral Sci. 2014, 25, 180–196. [Google Scholar] [CrossRef] [PubMed]
- Bartlett, D.W.; Evans, D.F.; Anggiansah, A.; Smith, B.G. A Study of the Association between Gastro-Oesophageal Reflux and Palatal Dental Erosion. Br. Dent. J. 1996, 181, 125–131. [Google Scholar] [CrossRef] [PubMed]
- Johansson, A.-K.; Omar, R.; Carlsson, G.E.; Johansson, A. Dental Erosion and Its Growing Importance in Clinical Practice: From Past to Present. Int. J. Dent. 2012, 2012, 632907. [Google Scholar] [CrossRef]
- Casas-Apayco, L.C.; Dreibi, V.M.; Hipólito, A.C.; Graeff, M.S.Z.; Rios, D.; Magalhães, A.C.; Buzalaf, M.A.R.; Wang, L. Erosive Cola-Based Drinks Affect the Bonding to Enamel Surface: An in Vitro Study. J. Appl. Oral Sci. 2014, 22, 434–441. [Google Scholar] [CrossRef] [PubMed]
- Alhilou, A.; Beddis, H.P.; Mizban, L.; Seymour, D.W. Basic Erosive Wear Examination: Assessment and Prevention. Dent. Nurs. 2015, 11, 262–267. [Google Scholar] [CrossRef]
- Krishna, M.; Rao, K.; Goyal, K. Prosthodontic Management of Severely Worn Dentition: Including Review of Literature Related to Physiology and Pathology of Increased Vertical Dimension of Occlusion. J. Indian Prosthodont. Soc. 2005, 5, 89. [Google Scholar] [CrossRef]
- Lussi, A.; Schlueter, N.; Rakhmatullina, E.; Ganss, C. Dental Erosion—An Overview with Emphasis on Chemical and Histopathological Aspects. Caries Res. 2011, 45, 2–12. [Google Scholar] [CrossRef]
- West, N.X.; Hughes, J.A.; Addy, M. Erosion of Dentine and Enamel in Vitro by Dietary Acids: The Effect of Temperature, Acid Character, Concentration and Exposure Time. J. Oral Rehabil. 2000, 27, 875–880. [Google Scholar] [CrossRef] [PubMed]
- Barbour, M.E.; Rees, G.D. The Role of Erosion, Abrasion and Attrition in Tooth Wear. J. Clin. Dent. 2006, 17, 88–93. [Google Scholar] [PubMed]
- Shellis, R.P. A Scanning Electron-Microscopic Study of Solubility Variations in Human Enamel and Dentine. Arch. Oral Biol. 1996, 41, 473–484. [Google Scholar] [CrossRef] [PubMed]
- Theuns, H.M.; Driessens, F.C.; van Dijk, J.W.; Groeneveld, A. Experimental Evidence for a Gradient in the Solubility and in the Rate of Dissolution of Human Enamel. Caries Res. 1986, 20, 24–31. [Google Scholar] [CrossRef] [PubMed]
- Haddadin, K.; Rassas, E.; Masarwa, N.; Haddadin, K. Causes for Tooth Surface Loss in a Group of Jordanian Population. Pak. Oral Dent. J. 2015, 35, 129–134. [Google Scholar]
- Abou Neel, E.A.; Bozec, L.; Perez, R.A.; Kim, H.-W.; Knowles, J.C. Nanotechnology in Dentistry: Prevention, Diagnosis, and Therapy. Int. J. Nanomed. 2015, 10, 6371–6394. [Google Scholar] [CrossRef]
- Lussi, A.; Buzalaf, M.A.R.; Duangthip, D.; Anttonen, V.; Ganss, C.; João-Souza, S.H.; Baumann, T.; Carvalho, T.S. The Use of Fluoride for the Prevention of Dental Erosion and Erosive Tooth Wear in Children and Adolescents. Eur. Arch. Paediatr. Dent. 2019, 20, 517–527. [Google Scholar] [CrossRef]
- Belmar da Costa, M.; Delgado, A.H.S.; Pinheiro de Melo, T.; Amorim, T.; Mano Azul, A. Analysis of Laboratory Adhesion Studies in Eroded Enamel and Dentin: A Scoping Review. Biomater. Investig. Dent. 2021, 8, 24–38. [Google Scholar] [CrossRef]
- Colombo, M.; Dagna, A.; Moroni, G.; Chiesa, M.; Poggio, C.; Pietrocola, G. Effect of Different Protective Agents on Enamel Erosion: An in Vitro Investigation. J. Clin. Exp. Dent. 2019, 11, e113–e118. [Google Scholar] [CrossRef] [PubMed]
- da Silva, C.V.; Ramos-Oliveira, T.M.; Mantilla, T.F.; de Freitas, P.M. Frequency of Application of AmF/NaF/SnCl2 Solution and Its Potential in Controlling Human Enamel Erosion Progression: An in Situ Study. Caries Res. 2017, 51, 141–148. [Google Scholar] [CrossRef] [PubMed]
- Bayrak, S.; Tuloglu, N.; Bicer, H.; Sen Tunc, E. Effect of Fluoride Varnish Containing CPP-ACP on Preventing Enamel Erosion. Scanning 2017, 2017, e1897825. [Google Scholar] [CrossRef] [PubMed]
- Inchingolo, A.D.; Di Cosola, M.; Inchingolo, A.M.; Greco Lucchina, A.; Malcangi, G.; Pettini, F.; Scarano, A.; Bordea, I.R.; Hazballa, D.; Lorusso, F.; et al. Correlation between Occlusal Trauma and Oral Microbiota: A Microbiological Investigation. J. Biol. Regul. Homeost. Agents 2021, 35, 295–302. [Google Scholar] [CrossRef] [PubMed]
- Skrtic, D.; Antonucci, J. Effect of Chemical Structure and Composition of the Resin Phase on Vinyl Conversion of Amorphous Calcium Phosphate-Filled Composites. Polym. Int. 2007, 56, 497–505. [Google Scholar] [CrossRef] [PubMed]
- Skrtic, D.; Antonucci, J.M.; Eanes, E.D.; Eichmiller, F.C.; Schumacher, G.E. Physicochemical Evaluation of Bioactive Polymeric Composites Based on Hybrid Amorphous Calcium Phosphates. J. Biomed. Mater. Res. 2000, 53, 381–391. [Google Scholar] [CrossRef] [PubMed]
- Moda, M.D.; Briso, A.L.F.; de Oliveira, R.P.; Pini, N.I.P.; Gonçalves, D.F.M.; dos Santos, P.H.; Fagundes, T.C. Effects of Different Toothpastes on the Prevention of Erosion in Composite Resin and Glass Ionomer Cement Enamel and Dentin Restorations. J. Appl. Oral Sci. 2020, 28, e20200493. [Google Scholar] [CrossRef]
- Braga, R.R. Calcium Phosphates as Ion-Releasing Fillers in Restorative Resin-Based Materials. Dent. Mater. 2019, 35, 3–14. [Google Scholar] [CrossRef]
- Abou Neel, E.A.; Aljabo, A.; Strange, A.; Ibrahim, S.; Coathup, M.; Young, A.M.; Bozec, L.; Mudera, V. Demineralization–Remineralization Dynamics in Teeth and Bone. Int. J. Nanomed. 2016, 11, 4743–4763. [Google Scholar] [CrossRef] [PubMed]
- Washut, K. Treatment of Severe Dental Erosion Utilizing Direct Composite to Phase Treatment. Compend. Contin. Educ. Dent. 2023, 44, 42–47. [Google Scholar]
- Schlichting, L.H.; Resende, T.H.; Reis, K.R.; Raybolt dos Santos, A.; Correa, I.C.; Magne, P. Ultrathin CAD-CAM Glass-Ceramic and Composite Resin Occlusal Veneers for the Treatment of Severe Dental Erosion: An up to 3-Year Randomized Clinical Trial. J. Prosthet. Dent. 2022, 128, 158.e1–158.e12. [Google Scholar] [CrossRef]
- ten Gate, J.M.; Imfeld, T. Dental Erosion, Summary. Eur. J. Oral Sci. 1996, 104, 241–244. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Pelá, V.T.; Niemeyer, S.H.; Baumann, T.; Levy, F.M.; Henrique-Silva, F.; Lussi, A.; Carvalho, T.S.; Buzalaf, M.A.R. Acquired Pellicle Engineering Using a Combination of Organic (Sugarcane Cystatin) and Inorganic (Sodium Fluoride) Components against Dental Erosion. Caries Res. 2022, 56, 138–145. [Google Scholar] [CrossRef] [PubMed]
- Uyar, D.S.; Özgül, B.M.; Tirali, R.E. Efficiency of Fluoride-Free Toothpastes on the Inhibition of Erosive Tooth Wear in Primary and Permanent Teeth. Fluoride 2021, 54, 367–380. [Google Scholar]
- Noaman, Z.; Abdulsahib, A. Evaluating Three Different Gels in Treating and Protecting the Primary Teeth Enamel Surface Erosion. J. Res. Med. Dent. Sci. 2022, 10, 43–50. [Google Scholar]
- Leal, I.D.C.; Costa, W.K.D.F.; Passos, V.F. Fluoride Dentifrice Containing Calcium Silicate and Sodium Phosphate Salts on Dental Erosion: In Vitro Study. Arch. Oral Biol. 2020, 118, 104857. [Google Scholar] [CrossRef] [PubMed]
- Otel, I.; Dias, K.; Pereira, R.; Fonseca, M.; Jesus, A.P.; Mata, A.; Vassilenko, V.; Silveira, J.M.; Pessanha, S. Investigation of the Protective Suitability of a Dental Fluorinated Varnish by Means of X Ray Fluorescence and Raman Spectroscopy. J. Trace Elem. Med. Biol. 2022, 71, 126938. [Google Scholar] [CrossRef] [PubMed]
- Moser, C.; Baumann, T.; Lussi, A.; Carvalho, T.S. Is the Erosion-Protective Effect Still Maintained When Tin Concentrations Are Reduced in Mouth Rinse Solutions? Caries Res. 2021, 55, 108–113. [Google Scholar] [CrossRef] [PubMed]
- West, N.X.; He, T.; Hellin, N.; Claydon, N.; Seong, J.; Macdonald, E.; Farrell, S.; Eusebio, R.; Wilberg, A. Randomized in Situ Clinical Trial Evaluating Erosion Protection Efficacy of a 0.454% Stannous Fluoride Dentifrice. Int. J. Dent. Hyg. 2019, 17, 261–267. [Google Scholar] [CrossRef]
- Fowler, C.E.; Creeth, J.E.; Paul, A.J.; Carson, C.; Tadesse, G.; Brown, A. The Effect of Dentifrice Ingredients on Enamel Erosion Prevention and Repair. Surf. Interface Anal. 2021, 53, 528–539. [Google Scholar] [CrossRef]
- West, N.X.; Hellin, N.; Eusebio, R.; He, T. The Erosion Protection Efficacy of a Stabilized Stannous Fluoride Dentifrice: An in Situ Randomized Clinical Trial. Am. J. Dent. 2019, 32, 138–142. [Google Scholar]
- Ince, S.G.; Banu Ermis, R. The in Situ Potential of Synthetic Nano-Hydroxyapatite for Tooth Enamel Repair. Bioinspired Biomim. Nanobiomaterials 2021, 10, 78–86. [Google Scholar] [CrossRef]
- Canto, F.M.T.; Alexandria, A.K.; Justino, I.B.D.S.; Rocha, G.M.; Cabral, L.M.; Ferreira, R.D.S.; Pithon, M.M.; Maia, L.C. The Use of a New Calcium Mesoporous Silica Nanoparticle versus Calcium and/or Fluoride Products in Reducing the Progression of Dental Erosion. J. Appl. Oral Sci. 2020, 28, e20200131. [Google Scholar] [CrossRef] [PubMed]
- Grohe, B.; Mittler, S. Advanced Non-Fluoride Approaches to Dental Enamel Remineralization: The next Level in Enamel Repair Management. Biomater. Biosyst. 2021, 4, 100029. [Google Scholar] [CrossRef] [PubMed]
- Gokkaya, B.; Ozbek, N.; Guler, Z.; Akman, S.; Sarac, A.S.; Kargul, B. Effect of a Single Application of CPP-ACPF Varnish on the Prevention of Erosive Tooth Wear: An AAS, AFM and SMH Study. Oral Health Prev. Dent. 2020, 18, 311–318. [Google Scholar] [CrossRef] [PubMed]
- Zhao, X.; Wang, L.; Pan, J.; Malmstrom, H.; Ren, Y.-F. Effects of Desensitizing Dentifrices on Dentin Tubule Occlusion and Resistance to Erosive Challenges. BMC Oral Health 2021, 21, 610. [Google Scholar] [CrossRef]
- Li, X.; Lin, X.; Zhong, B.; Yu, H. Effects of the Application Timing of Anti-Erosive Agents on Dentin Erosion. J. Mech. Behav. Biomed. Mater. 2022, 136, 105512. [Google Scholar] [CrossRef]
- Zhao, X.; He, T.; He, Y.; Chen, H. Efficacy of a Stannous-Containing Dentifrice for Protecting Against Combined Erosive and Abrasive Tooth Wear In Situ. Oral Health Prev. Dent. 2020, 18, 619–624. [Google Scholar] [CrossRef]
- Taha, N.S.; Qasim, A.A. Evaluation of the Remineralizing Effect of Elmex Erosion Protection and GC Tooth Mousse Plus on the Eroded Enamel of Primary Teeth Induced by Specific Medicinal Syrup. J. Res. Med. Dent. Sci. 2021, 9, 1–8. [Google Scholar]
- De Lavôr, J.R.; Fernandes, N.L.S.; De Sousa, E.B.G.; Da Cunha, J.L.; Meira, I.A.; Correia Sampaio, F.; De Oliveira, A.F.B. Nanoencapsulated Fluoride as a Remineralization Option for Dental Erosion: An in Vitro Study. Acta Odontol. Scand. 2021, 79, 321–326. [Google Scholar] [CrossRef]
- Mazzoleni, S.; Gargani, A.; Parcianello, R.G.; Pezzato, L.; Bertolini, R.; Zuccon, A.; Stellini, E.; Ludovichetti, F.S. Protection against Dental Erosion and the Remineralization Capacity of Non-Fluoride Toothpaste, Fluoride Toothpaste and Fluoride Varnish. Appl. Sci. 2023, 13, 1849. [Google Scholar] [CrossRef]
- Kranz, S.; Heyder, M.; Mueller, S.; Guellmar, A.; Krafft, C.; Nietzsche, S.; Tschirpke, C.; Herold, V.; Sigusch, B.; Reise, M. Remineralization of Artificially Demineralized Human Enamel and Dentin Samples by Zinc-Carbonate Hydroxyapatite Nanocrystals. Materials 2022, 15, 7173. [Google Scholar] [CrossRef] [PubMed]
- Silva, C.V.; Mantilla, T.F.; Engel, Y.; Tavares, J.P.; Freitas, P.M.; Rechmann, P. The Effect of CO2 9.3 Μm Short-Pulsed Laser Irradiation in Enamel Erosion Reduction with and without Fluoride Applications—A Randomized, Controlled in Vitro Study. Lasers Med. Sci. 2020, 35, 1213–1222. [Google Scholar] [CrossRef] [PubMed]
- AlShamrani, A.; AlHabdan, A.; AlDaweesh, M.; Bin Hamdan, R.; AlRajhi, R. The Effects of Combining Erbium, Chromium: Yttrium-Scandium-Gallium-Garnet Laser Irradiation with Fluoride Application in Controlling the Progression of Enamel Erosion. Saudi Dent. J. 2021, 33, 1126–1132. [Google Scholar] [CrossRef] [PubMed]
- Philip, N. State of the Art Enamel Remineralization Systems: The Next Frontier in Caries Management. Caries Res. 2019, 53, 284–295. [Google Scholar] [CrossRef]
- Qeli, E.; Toti, Ç.; Odorici, A.; Blasi, E.; Tragaj, E.; Tepedino, M.; Masedu, F.; Kaçani, G.; Hysi, D.; Meto, A.; et al. Effectiveness of Two Different Fluoride-Based Agents in the Treatment of Dentin Hypersensitivity: A Prospective Clinical Trial. Materials 2022, 15, 1266. [Google Scholar] [CrossRef]
- Luo, T.; Zhang, J.; Fan, L.; Huang, Y.; Yu, J.; Yu, H. A Digital Workflow with the Virtual Enamel Evaluation and Stereolithographic Template for Accurate Tooth Preparation to Conservatively Manage a Case of Complex Exogenous Dental Erosion. J. Esthet. Restor. Dent. 2022, 34, 733–740. [Google Scholar] [CrossRef]
- Salem, M.N.; Hafez, S. Aesthetic Management of Erosive Tooth Wear in a Young Egyptian Swimmer: A Case Report. Clin. Cosmet. Investig. Dent. 2021, 13, 201–209. [Google Scholar] [CrossRef]
- Menezes-Silva, R.; Fernandes, P.; Bueno, L.S.; Vertuan, M.; Rios, D.; Bresciani, E.; Borges, A.; de Lima Navarro, M.F. Crown Reconstruction of Erosive Wear Using High-Viscosity Glass Ionomer Cement: A Case Report. Oper. Dent. 2022, 47, 239–246. [Google Scholar] [CrossRef]
- Hoeppner, M.G.; Salomão, F.M.; Hirose, M.C.; Besegato, J.F.; Sundfeld Neto, D.; Sunfeld, R.H. Direct Composite Resin Restorations for Teeth with Dental Erosion: A Case Report. Gen. Dent. 2019, 67, 36–39. [Google Scholar]
- Dallari, G.; Scalzo, I.; Rosati, R.M.; Sampaio, C.S.; Hirata, R. Full-Mouth Adhesive Rehabilitation of a Severe Case of Erosion Treated with v-Shaped Veneers. J. Esthet. Restor. Dent. 2021, 33, 422–431. [Google Scholar] [CrossRef]
- Pini, N.P.; De Marchi, L.M.; Ramos, A.L.; Pascotto, R.C. Minimally Invasive Adhesive Rehabilitation for a Patient with Tooth Erosion: Seven-Year Follow-Up. Oper. Dent. 2019, 44, E45–E57. [Google Scholar] [CrossRef] [PubMed]
- Torosyan, A.; Vailati, F.; Mojon, P.; Sierra, D.; Sailer, I. Retrospective Clinical Study of Minimally Invasive Full-Mouth Rehabilitations of Patients with Erosions and/or Abrasions Following the 3-Step Technique. Part 1: 6-Year Survival Rates and Technical Outcomes of the Restorations. Int. J. Prosthodont. 2021, 35, 139–151. [Google Scholar] [CrossRef] [PubMed]
- Oudkerk, J.; Eldafrawy, M.; Bekaert, S.; Grenade, C.; Vanheusden, A.; Mainjot, A. The One-Step No-Prep Approach for Full-Mouth Rehabilitation of Worn Dentition Using PICN CAD-CAM Restorations: 2-Yr Results of a Prospective Clinical Study. J. Dent. 2020, 92, 103245. [Google Scholar] [CrossRef] [PubMed]
- Alhammadi, S.; Milosevic, A. The Restoration of Severe Generalized Dental Erosive Wear Using Direct Composite: A Case Report. Open Dent. J. 2021, 15, 520–525. [Google Scholar] [CrossRef]
- Di Cosola, M.; Cazzolla, A.P.; Charitos, I.A.; Ballini, A.; Inchingolo, F.; Santacroce, L. Candida Albicans and Oral Carcinogenesis. A Brief Review. J. Fungi 2021, 7, 476. [Google Scholar] [CrossRef]
- Inchingolo, F.; Tatullo, M.; Abenavoli, F.M.; Marrelli, M.; Inchingolo, A.D.; Inchingolo, A.M.; Dipalma, G. Non-Hodgkin Lymphoma Affecting the Tongue: Unusual Intra-Oral Location. Head Neck Oncol. 2011, 3, 1. [Google Scholar] [CrossRef]
- Ceci, S.; Berate, P.; Candrea, S.; Babtan, A.-M.; Azzollini, D.; Piras, F.; Curatoli, L.; Corriero, A.; Patano, A.; Valente, F.; et al. The Oral and Gut Microbiota: Beyond a Short Communication. Balneo PRM Res. J. 2021, 12, 405–411. [Google Scholar] [CrossRef]
- Bartlett, D.; O’Toole, S. Tooth Wear and Aging. Aust. Dent. J. 2019, 64 (Suppl. S1), S59–S62. [Google Scholar] [CrossRef]
- Loomans, B.; Opdam, N.; Attin, T.; Bartlett, D.; Edelhoff, D.; Frankenberger, R.; Benic, G.; Ramseyer, S.; Wetselaar, P.; Sterenborg, B.; et al. Severe Tooth Wear: European Consensus Statement on Management Guidelines. J. Adhes. Dent. 2017, 19, 111–119. [Google Scholar] [CrossRef]
- Mesko, M.E.; Sarkis-Onofre, R.; Cenci, M.S.; Opdam, N.J.; Loomans, B.; Pereira-Cenci, T. Rehabilitation of Severely Worn Teeth: A Systematic Review. J. Dent. 2016, 48, 9–15. [Google Scholar] [CrossRef]
- Carvalho, T.; Colon, P.; Ganss, C.; Huysmans, M.; Lussi, A.; Schlueter, N.; Schmalz, G.; Shellis, R.; Tveit, A.; Wiegand, A. Consensus Report of the European Federation of Conservative Dentistry: Erosive Tooth Wear—Diagnosis and Management. Swiss Dent. J. 2016, 126, 342–346. [Google Scholar] [CrossRef] [PubMed]
- Tauböck, T.T.; Schmidlin, P.R.; Attin, T. Vertical Bite Rehabilitation of Severely Worn Dentitions with Direct Composite Restorations: Clinical Performance up to 11 Years. J. Clin. Med. 2021, 10, 1732. [Google Scholar] [CrossRef] [PubMed]
- Libonati, A.; Marzo, G.; Klinger, F.G.; Farini, D.; Gallusi, G.; Tecco, S.; Mummolo, S.; De Felici, M.; Campanella, V. Embryotoxicity Assays for Leached Components from Dental Restorative Materials. Reprod. Biol. Endocrinol. 2011, 9, 136. [Google Scholar] [CrossRef] [PubMed]
- Campanella, V.; Gallusi, G.; Nardi, R.; Mea, A.; Di Taranto, V.; Montemurro, E.; Marzo, G.; Libonati, A. Dentinal Substrate Variability and Bonding Effectiveness: SEM Investigation. J. Biol. Regul. Homeost. Agents 2020, 34, 49–54. [Google Scholar]
- Ramos, R.Q.; Coelho, N.F.; Lopes, G.C. Three-Year Follow-up of Conservative Direct Composite Veneers on Eroded Teeth. Oper. Dent. 2022, 47, 131–137. [Google Scholar] [CrossRef]

| Articles screening strategy | Keywords: ‘dental erosion’ AND ‘therapy’ OR ‘treatment’ |
| Electronic Databases: PubMed, Scopus, and Web of Science | |
| Language: English |
| References | Author(s) | Years | Design Study | Subject | Intervention | Outcomes |
|---|---|---|---|---|---|---|
| [42] | Pelà et al. | 2022 | In vitro | 75 Humans | 5 treatment groups: Control, Elmex™ (SnCl2/NaF/AmF), 0.1 mg/mL CaneCPI-5, 500 ppm NaF, CaneCPI-5 + NaF (Combination). | All treatments demonstrated a protective effect on enamel against dental erosion; however, the combination of CaneCPI-5 with NaF showed greater protection |
| [43] | Uyar et al. | 2021 | In vitro | Human (45 teeth) | Three toothpaste groups:
| Primary teeth had statistically higher volumetric surface roughness values in Group-2 and Group 3.
|
| [44] | Noaman et al. | 2022 | In vitro | Human (30 sound buccal segments of primary first or second molars) | Treatment with NHA gel, HA gel, and NaF gel|
| 10% NHA gel demonstrated better treatment and prevention of erosion caused by Pepsi Cola compared to HA and NaF gels |
| [45] | Leal et al. | 2020 | In vitro | Human (48 teeth) | Divided into 4 groups: NF, SnF2, CSSP, CSSP + Serum|—Cyclic experiments (3x/day for 5 days) including erosive challenge with 0.05 M citric acid, treatment with toothpaste slurries, and remineralization with artificial saliva. | Dentifrice containing calcium silicate and sodium phosphate with or without the dual-phase gel was able to prevent erosive tooth wear |
| [46] | Otel et al. | 2022 | In vitro | Human | Analysis of human enamel specimens
2. After varnish (treatment group) or toothpaste (control) application 3. After citric acid cycle | The use of a fluorinated dental varnish suggests a protective effect for human enamel against dental erosion demineralization process |
| [47] | Moser et al. | 2021 | In vitro | 162 enamel specimens from human premolars | Treatments included a humid chamber (negative control), Elmex® Erosion Protection mouth rinse (positive control), and 7 solutions with varying Sn2+ concentrations and/or containing flavouring. | Sn2+ concentrations in mouth rinses may be lowered to 200 ppm without compromising the anti-erosive properties of the solution |
| [48] | West et al. | 2019 | In vitro | 36 participants (33 completed the study) | Two treatment products: 0.454% stabilized stannous fluoride dentifrice (Procter and Gamble) and a marketed dentifrice control containing 0.24% sodium fluoride and 0.3% triclosan (Colgate-Palmolive).
| SnF2 TP more efficient |
| [49] | Fowler et al. | 2021 | In vitro | Human | Dentifrice formulation (NaF/CL) compared to six commercial dentifrices from European and US regulatory regions. | NaF/CL dentifrice provided the highest protection against dental erosion. |
| [50] | West et al. | 2019 | In vitro | 33 humans | Two treatments:
| Stannous fluoride dentifrice provided significantly greater protection against dental erosion compared to NaF/triclosan dentifrice. |
| [51] | Ince et al. | 2021 | In vitro | 21 humans | Subjects wore a palatal appliance containing five sterilized enamel specimens.
| Home use of nano-hydroxyapatite-containing toothpaste may have a protective effect against erosion at the enamel surface.| |
| [52] | Canto et al. | 2020 | In vitro | 60 human teeth | 60 enamel blocks covered with different treatments:
| The Ca2+-MSN and NaF treatments were superior compared with the others and the negative control |
| [53] | B. Grohe, S. Mittler | 2021 | In vitro | Human | Enamel remineralization systems with and without fluoride. | Fluoride treatment gold standard |
| [54] | Gokkaya et al. | 2020 | In vitro | Human | CPP-ACPF varnish, TCP-F varnish, NaF varnish, and deionized water. | Agents that contain CPP-ACP have a good remineralizing effect |
| [55] | Zhao et al. | 2021 | In vitro | Human | Divided into 3 groups:
| Desensitizing dentifrices containing CPP or PVM/MA effectively occluded dentin tubules after brushing. PVM/MA in combination with submicron silicon dioxide exhibited stronger resistance to erosive challenges by acidic beverages |
| [56] | Li et al. | 2022 | In vitro | Human | chlorhexidine, sodium fluoride, and deionized water with quercetin. | A combination of chlorhexidine and quercetin is more efficient |
| [57] | Zhao et al. | 2020 | In vitro | Human | Subjects were randomized to receive either a Sn-containing NaF dentifrice or a conventional NaF dentifrice. | Sn-containing TP better protection |
| [58] | Taha et al. | 2021 | In vitro | Human(40 teeth) | Divided into five groups (8 samples in each group).
| The simultaneous use of GC Tooth Mousse Plus and Elmex erosion protection paste gave better remineralizing effect than the sole use of either GC Tooth Mousse Plus or Elmex erosion protection paste |
| [59] | de Lavor et al. | 2021 | In vitro | Human (72 teeth) | Divided into 6 groups (n = 12):
| TP with nano fluoride had good remineralizing effects |
| [60] | Mazzoleni et al. | 2023 | In vitro | 8 human teeth | Samples were immersed in 5 mL of soft drink for 2 min at room temperature, then rinsed with distilled/deionized water (total of eight minutes).
| Fluoride TP and varnishes efficient on initial acid attack |
| [61] | Kranz et al. | 2022 | In vitro | Human | Test group (n = 20) treated three times a day for 3 min with a zinc carbonate-hydroxyapatite-containing toothpaste (biorepair®).
| Treatment with biorepair® did not affect enamel surfaces as proposed. Minor mineral precipitation and a reduction in surface roughness were detected among dentin surfaces only.| |
| [62] | Silva et al. | 2020 | In vitro | Human | Specific details were provided for TiF4 gel and AmF/NaF/SnCl2 applications, CO2 laser settings, and erosive cycling parameters.|—Surface loss (in μm) measured immediately after treatment, after 5 and 10 days of erosive cycling with citric acid. | Combination efficient |
| [63] | Alshamrani et al. | 2021 | In vitro | 60 human teeth | Specific treatments for each group: Control (C), fluoride (F), laser (L), fluoride followed by laser (F + L), laser followed by fluoride (L + F)—Specimens eroded in citric acid for 10 min | acidulated phosphate fluoride application as well as laser irradiation before fluoride application increased enamel surface microhardness and prevented the progression of enamel erosion |
| [64] | Philip et al. | 2019 | Clinical Trial | Human | fluoride gel and varnish | enamel more resistant to acid attacks |
| [65] | Qeli et al. | 2022 | Clinical Trial | 176 Human | (i) First group (96 patients): Tiefenfluorid® treatment applied in three appointments at 7-day intervals. (ii) Second group (80 patients): EnamelastTM treatment applied seven times at 7-day intervals. | Good results of calcium fluoride |
| References | Author(s) | Years | Design Study | Subject | Intervention | Outcomes |
|---|---|---|---|---|---|---|
| [66] | Tian Luo et al. | 2022 | Case report | Human | Digital approach utilizing a stereolithographic model and virtual evaluation | Virtual inspection of the enamel helps with acquiring the proper treatment plan |
| [67] | Salem M. et al. | 2021 | Case report | Human | Injection moulding technique | Good results |
| [68] | Menezes-Silva et al. | 2022 | Case report | Human | high-viscosity glass ionomer cement | improved function |
| [69] | Hoeppner M.G. et al. | 2019 | Case report | Human | Glass ionomer cement | Improved aesthetics and function of the worn teeth. |
| [70] | Dallari G. et al. | 2021 | Case report | Human | Restoration with v-shaped veneers | Good aesthetic and functional results after 3 years |
| [71] | Pini, N.P. et al. | 2019 | Case report | Human | direct composite resin techniques | Restorations until 7 years of follow-up |
| [72] | Torosyan A. et al. | 2021 | Clinical Trial | Human | 3-step technique | 406 restorations with 6-year survival rates were good for all the categories |
| [73] | Oudkerk J. et al. | 2020 | Clinical trial | Human | 192 restorations with direct composites | 2-year survival rate of restorations was 100% |
| [74] | Alhammadi S. et al. | 2021 | Case report | Human | All direct restorations | Function improved |
| [75] | Schlichting L.H et al. | 2022 | R. C. T. | Human | 11 patients restored in posterior teeth with 24 ceramic and 36 composite resin ultrathin occlusal veneers | No restorations were lost. 5 partial failures |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Inchingolo, F.; Dipalma, G.; Azzollini, D.; Trilli, I.; Carpentiere, V.; Hazballa, D.; Bordea, I.R.; Palermo, A.; Inchingolo, A.D.; Inchingolo, A.M. Advances in Preventive and Therapeutic Approaches for Dental Erosion: A Systematic Review. Dent. J. 2023, 11, 274. https://doi.org/10.3390/dj11120274
Inchingolo F, Dipalma G, Azzollini D, Trilli I, Carpentiere V, Hazballa D, Bordea IR, Palermo A, Inchingolo AD, Inchingolo AM. Advances in Preventive and Therapeutic Approaches for Dental Erosion: A Systematic Review. Dentistry Journal. 2023; 11(12):274. https://doi.org/10.3390/dj11120274
Chicago/Turabian StyleInchingolo, Francesco, Gianna Dipalma, Daniela Azzollini, Irma Trilli, Vincenzo Carpentiere, Denisa Hazballa, Ioana Roxana Bordea, Andrea Palermo, Alessio Danilo Inchingolo, and Angelo Michele Inchingolo. 2023. "Advances in Preventive and Therapeutic Approaches for Dental Erosion: A Systematic Review" Dentistry Journal 11, no. 12: 274. https://doi.org/10.3390/dj11120274
APA StyleInchingolo, F., Dipalma, G., Azzollini, D., Trilli, I., Carpentiere, V., Hazballa, D., Bordea, I. R., Palermo, A., Inchingolo, A. D., & Inchingolo, A. M. (2023). Advances in Preventive and Therapeutic Approaches for Dental Erosion: A Systematic Review. Dentistry Journal, 11(12), 274. https://doi.org/10.3390/dj11120274













