Systemic Diseases and Biological Dental Implant Complications: A Narrative Review
Abstract
1. Introduction
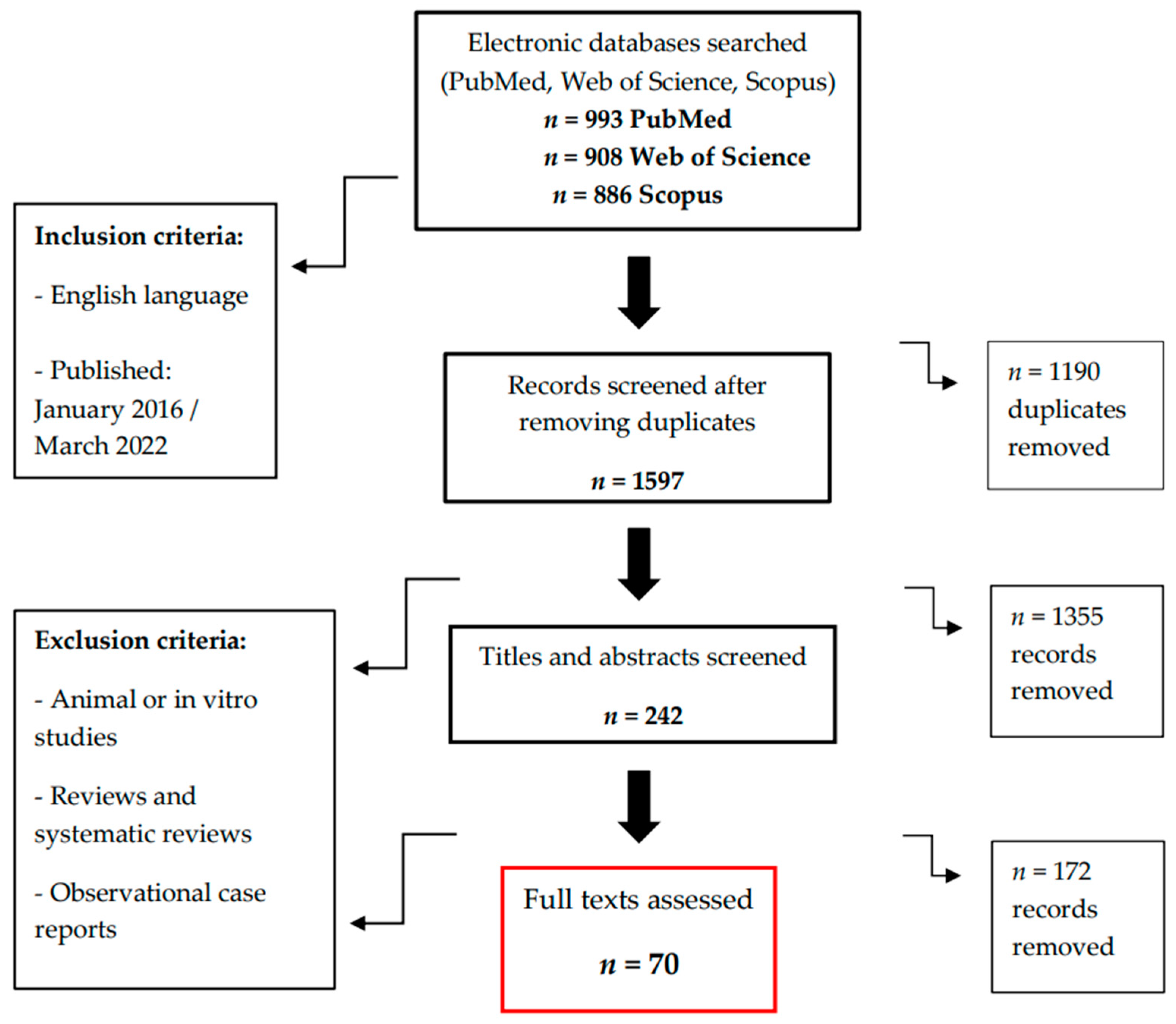
2. Materials and Methods
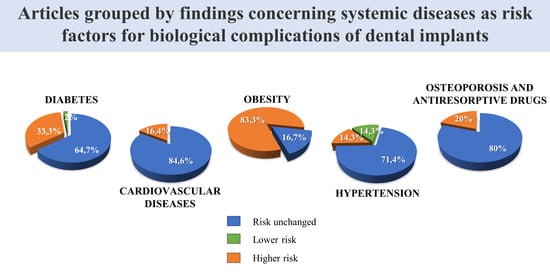
3. Results
4. Types of Study Examined
4.1. Diabetes and Prediabetes
4.2. Obesity
4.3. Cardiovascular Disease
4.4. Hypertension
4.5. Osteoporosis and the Use of Antiresorptive Drugs
5. Discussion
5.1. Diabetes
5.2. Obesity
5.3. Cardiovascular Disease
5.4. Hypertension
5.5. Osteoporosis and the Use of Antiresorptive Drugs
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Berglundh, T.; Armitage, G.; Araujo, M.G.; Avila-Ortiz, G.; Blanco, J.; Camargo, P.M.; Chen, S.; Cochran, D.; Derks, J.; Figuero, E.; et al. Peri-implant diseases and conditions: Consensus report of workgroup 4 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J. Clin. Periodontol. 2018, 45 (Suppl. S20), S286–S291. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.-T.; Huang, Y.-W.; Zhu, L.; Weltman, R. Prevalences of peri-implantitis and peri-implant mucositis: Systematic review and meta-analysis. J. Dent. 2017, 62, 1–12. [Google Scholar] [CrossRef]
- Luo, H.; Pan, W.; Sloan, F.; Feinglos, M.; Wu, B. Forty-Year Trends in Tooth Loss Among American Adults with and Without Diabetes Mellitus: An Age-Period-Cohort Analysis. Prev. Chronic Dis. 2015, 12, E211. [Google Scholar] [CrossRef]
- Elani, H.W.; Starr, J.R.; Da Silva, J.D.; Gallucci, G.O. Trends in Dental Implant Use in the U.S., 1999–2016, and Projections to 2026. J. Dent. Res. 2018, 97, 1424–1430. [Google Scholar] [CrossRef] [PubMed]
- Blanco, C.; Liñares, A.; Dopico, J.; Pico, A.; Sobrino, T.; Leira, Y.; Blanco, J. Peri-implantitis, systemic inflammation, and dyslipidemia: A cross-sectional biochemical study. J. Periodontal Implant Sci. 2021, 51, 342–351. [Google Scholar] [CrossRef] [PubMed]
- Froum, S.J.; Hengjeerajaras, P.; Liu, K.-Y.; Maketone, P.; Patel, V.; Shi, Y. The Link Between Periodontitis/Peri-implantitis and Cardiovascular Disease: A Systematic Literature Review. Int. J. Periodontics Restor. Dent. 2020, 40, e229–e233. [Google Scholar] [CrossRef]
- Suvan, J.; D’Aiuto, F.; Moles, D.; Petrie, A.; Donos, N. Association between overweight/obesity and periodontitis in adults. A systematic review. Obes. Rev. 2011, 12, e381–e404. [Google Scholar] [CrossRef]
- Khan, S.; Barrington, G.; Bettiol, S.; Barnett, T.; Crocombe, L. Is overweight/obesity a risk factor for periodontitis in young adults and adolescents?: A systematic review. Obes. Rev. 2018, 19, 852–883. [Google Scholar] [CrossRef]
- De Moura-Grec, P.G.; Marsicano, J.; De Carvalho, C.A.P.; Sales-Peres, S.H.D.C. Obesity and periodontitis: Systematic review and meta-analysis. Cienc. Saude Coletiva 2014, 19, 1763–1772. [Google Scholar] [CrossRef]
- da Silva, F.G.; Pola, N.M.; Casarin, M.; Muniz, F.W.M.G. Association between clinical measures of gingival inflammation and obesity in adults: Systematic review and meta-analyses. Clin. Oral Investig. 2021, 25, 4281–4298. [Google Scholar] [CrossRef]
- Nascimento, G.G.; Peres, K.G.; Mittinty, M.N.; Mejia, G.C.; Silva, D.A.S.; Gonzalez-Chica, D.; Peres, M.A. Obesity and Periodontal Outcomes: A Population-Based Cohort Study in Brazil. J. Periodontol. 2017, 88, 50–58. [Google Scholar] [CrossRef] [PubMed]
- Elangovan, S.; Brogden, K.A.; Dawson, D.V.; Blanchette, D.; Pagan-Rivera, K.; Stanford, C.M.; Johnson, G.K.; Recker, E.; Bowers, R.; Haynes, W.; et al. Body Fat Indices and Biomarkers of Inflammation: A Cross-Sectional Study with Implications for Obesity and Peri-implant Oral Health. Int. J. Oral Maxillofac. Implant. 2014, 29, 1429–1434. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Gurav, A.N. Periodontitis and Insulin Resistance: Casual or Causal Relationship? Diabetes Metab. J. 2012, 36, 404–411. [Google Scholar] [CrossRef] [PubMed]
- Naujokat, H.; Kunzendorf, B.; Wiltfang, J. Dental implants and diabetes mellitus—A systematic review. Int. J. Implant. Dent. 2016, 2, 5. [Google Scholar] [CrossRef]
- Cabrera-Domínguez, J.J.; Castellanos-Cosano, L.; Torres-Lagares, D.; Pérez-Fierro, M.; Machuca-Portillo, G. Clinical performance of titanium-zirconium implants with a hydrophilic surface in patients with controlled type 2 diabetes mellitus: 2-year results from a prospective case-control clinical study. Clin. Oral Investig. 2020, 24, 2477–2486. [Google Scholar] [CrossRef] [PubMed]
- Alasqah, M.N.; Alrabiah, M.; Al-Aali, K.A.; Mokeem, S.A.; Binmahfooz, A.M.; ArRejaie, A.S.; Abduljabbar, T. Peri-implant soft tissue status and crestal bone levels around adjacent implants placed in patients with and without type-2 diabetes mellitus: 6 years follow-up results. Clin. Implant Dent. Relat. Res. 2018, 20, 562–568. [Google Scholar] [CrossRef] [PubMed]
- Salih, H.M.; Al-Nimer, M.S.; Mohammed, N.B. Assessment of early and late implantation failure of teeth: A single-center experience with 297 implanted teeth. Arch. Venez. De Farmacol. Y Ter. 2021, 40, 340–343. [Google Scholar] [CrossRef]
- Carr, A.; Revuru, V.S.; Lohse, C.M. Association of Systemic Conditions with Dental Implant Failures in 6,384 Patients During a 31-Year Follow-up Period. Int. J. Oral Maxillofac. Implant. 2017, 32, 1153–1161. [Google Scholar] [CrossRef]
- Krennmair, S.; Hunger, S.; Forstner, T.; Malek, M.; Krennmair, G.; Stimmelmayr, M. Implant health and factors affecting peri-implant marginal bone alteration for implants placed in staged maxillary sinus augmentation: A 5-year prospective study. Clin. Implant Dent. Relat. Res. 2019, 21, 32–41. [Google Scholar] [CrossRef]
- Eskow, C.C.; Oates, T.W. Dental Implant Survival and Complication Rate over 2 Years for Individuals with Poorly Controlled Type 2 Diabetes Mellitus. Clin. Implant Dent. Relat. Res. 2017, 19, 423–431. [Google Scholar] [CrossRef]
- Krennmair, S.; Weinländer, M.; Forstner, T.; Krennmair, G.; Stimmelmayr, M. Factors affecting peri-implant bone resorption in four Implant supported mandibular full-arch restorations: A 3-year prospective study. J. Clin. Periodontol. 2016, 43, 92–101. [Google Scholar] [CrossRef] [PubMed]
- Latimer, J.M.; Roll, K.L.; Daubert, D.M.; Zhang, H.; Shalev, T.; Wolff, L.F.; Kotsakis, G.A. ABCD study collaborators Clinical performance of hydrophilic, titanium-zirconium dental implants in patients with well-controlled and poorly controlled type 2 diabetes: One-year results of a dual-center cohort study. J. Periodontol. 2021, 93, 745–757. [Google Scholar] [CrossRef] [PubMed]
- Nobre, M.D.A.; Maló, P. Prevalence of periodontitis, dental caries, and peri-implant pathology and their relation with systemic status and smoking habits: Results of an open-cohort study with 22009 patients in a private rehabilitation center. J. Dent. 2017, 67, 36–42. [Google Scholar] [CrossRef] [PubMed]
- AL Zahrani, S.; AL Mutairi, A.A. Stability and bone loss around submerged and non-submerged implants in diabetic and non-diabetic patients: A 7-year follow-up. Braz. Oral Res. 2018, 32, e57. [Google Scholar] [CrossRef] [PubMed]
- Juncar, R.-I.; Precup, A.-I.; Juncar, M. Immediate implant-prosthetic dental rehabilitation of patients with diabetes using four immediately loaded dental implants: A pilot study. J. Int. Med. Res. 2020, 48, 300060519897195. [Google Scholar] [CrossRef] [PubMed]
- Al Zahrani, S.; Al Mutairi, A.A. Crestal Bone Loss Around Submerged and Non-Submerged Dental Implants in Individuals with Type-2 Diabetes Mellitus: A 7-Year Prospective Clinical Study. Med. Princ. Pract. 2019, 28, 75–81. [Google Scholar] [CrossRef] [PubMed]
- Al-Shibani, N.; Al-Aali, K.A.; Al-Hamdan, R.S.; Alrabiah, M.; Basunbul, G.; Abduljabbar, T. Comparison of clinical peri-implant indices and crestal bone levels around narrow and regular diameter implants placed in diabetic and non-diabetic patients: A 3-year follow-up study. Clin. Implant Dent. Relat. Res. 2019, 21, 247–252. [Google Scholar] [CrossRef]
- Friedmann, A.; Winkler, M.; Diehl, D.; Yildiz, M.S.; Bilhan, H. One-year performance of posterior narrow diameter implants in hyperglycemic and normo-glycemic patients—A pilot study. Clin. Oral Investig. 2021, 25, 6707–6715. [Google Scholar] [CrossRef]
- Alsahhaf, A.; Alshiddi, I.F.; Alshagroud, R.S.; Al-Aali, K.A.; Vohra, F.; Abduljabbar, T. Clinical and radiographic indices around narrow diameter implants placed in different glycemic-level patients. Clin. Implant Dent. Relat. Res. 2019, 21, 621–626. [Google Scholar] [CrossRef]
- Al-Askar, M.; Ajlan, S.; Alomar, N.; Al-Daghri, N.M. Clinical and Radiographic Peri-Implant Parameters and Whole Salivary Interleukin-1β and Interleukin-6 Levels among Type-2 Diabetic and Nondiabetic Patients with and without Peri-Implantitis. Med. Princ. Pract. 2018, 27, 133–138. [Google Scholar] [CrossRef]
- Alshahrani, A.; Al Deeb, M.; Alresayes, S.; Mokeem, S.A.; Al-Hamoudi, N.; Alghamdi, O.; Vohra, F.; Abduljabbar, T. Comparison of peri-implant soft tissue and crestal bone status of dental implants placed in prediabetic, type 2 diabetic, and non-diabetic individuals: A retrospective cohort study. Int. J. Implant. Dent. 2020, 6, 56. [Google Scholar] [CrossRef] [PubMed]
- Mozzati, M.; Gallesio, G.; Menicucci, G.; Manzella, C.; Tumedei, M.; Del Fabbro, M. Dental Implants with a Calcium Ions-Modified Surface and Platelet Concentrates for the Rehabilitation of Medically Compromised Patients: A Retrospective Study with 5-Year Follow-Up. Materials 2021, 14, 2718. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Choi, H.; Park, J.; Jung, H.; Jung, Y. Effects of anti-resorptive drugs on implant survival and peri-implantitis in patients with existing osseointegrated dental implants: A retrospective cohort study. Osteoporos. Int. 2020, 31, 1749–1758. [Google Scholar] [CrossRef] [PubMed]
- Alberti, A.; Morandi, P.; Zotti, B.; Tironi, F.; Francetti, L.; Taschieri, S.; Corbella, S. Influence of Diabetes on Implant Failure and Peri-Implant Diseases: A Retrospective Study. Dent. J. 2020, 8, 70. [Google Scholar] [CrossRef] [PubMed]
- Nobre, M.D.A.; Maló, P.; Gonçalves, Y.; Sabas, A.; Salvado, F.J. Dental implants in diabetic patients: Retrospective cohort study reporting on implant survival and risk indicators for excessive marginal bone loss at 5 years. J. Oral Rehabil. 2016, 43, 863–870. [Google Scholar] [CrossRef] [PubMed]
- Mameno, T.; Wada, M.; Otsuki, M.; Okuno, I.; Ozeki, K.; Tahara, A.; Ikebe, K. Risk indicators for marginal bone resorption around implants in function for at least 4 years: A retrospective longitudinal study. J. Periodontol. 2020, 91, 37–45. [Google Scholar] [CrossRef]
- Neves, J.; Nobre, M.D.A.; Oliveira, P.; Dos Santos, J.M.; Malo, P. Risk Factors for Implant Failure and Peri-Implant Pathology in Systemic Compromised Patients. J. Prosthodont. 2018, 27, 409–415. [Google Scholar] [CrossRef]
- Saminsky, M.; Ben Dor, A.; Horwitz, J. Variables Affecting Peri-Implant Radiographic Bone Loss-8-23 Years Follow-Up. Appl. Sci. 2020, 10, 8591. [Google Scholar] [CrossRef]
- Staedt, H.; Rossa, M.; Lehmann, K.M.; Al-Nawas, B.; Kämmerer, P.W.; Heimes, D. Potential risk factors for early and late dental implant failure: A retrospective clinical study on 9080 implants. Int. J. Implant Dent. 2020, 6, 81. [Google Scholar] [CrossRef]
- French, D.; Ofec, R.; Levin, L. Long term clinical performance of 10 871 dental implants with up to 22 years of follow-up: A cohort study in 4247 patients. Clin. Implant Dent. Relat. Res. 2021, 23, 289–297. [Google Scholar] [CrossRef]
- French, D.; Grandin, H.M.; Ofec, R. Retrospective cohort study of 4,591 dental implants: Analysis of risk indicators for bone loss and prevalence of peri-implant mucositis and peri-implantitis. J. Periodontol. 2019, 90, 691–700. [Google Scholar] [CrossRef]
- De Angelis, P.; Manicone, P.F.; Gasparini, G.; De Filippis, I.; Liguori, M.G.; De Angelis, S.; Cannata, F.; D’addona, A. The Effect of Controlled Diabetes and Hyperglycemia on Implant Placement with Simultaneous Horizontal Guided Bone Regeneration: A Clinical Retrospective Analysis. BioMed Res. Int. 2021, 2021, 9931505. [Google Scholar] [CrossRef] [PubMed]
- Ormianer, Z.; Block, J.; Matalon, S.; Kohen, J. The Effect of Moderately Controlled Type 2 Diabetes on Dental Implant Survival and Peri-implant Bone Loss: A Long-Term Retrospective Study. Int. J. Oral Maxillofac. Implant. 2018, 33, 389–394. [Google Scholar] [CrossRef]
- Hasanoglu Erbasar, G.N.; Hocaoğlu, T.P.; Erbasar, R.C. Risk factors associated with short dental implant success: A long-term retrospective evaluation of patients followed up for up to 9 years. Braz. Oral Res. 2019, 33, e030. [Google Scholar] [CrossRef] [PubMed]
- Sghaireen, M.G.; Alduraywish, A.A.; Srivastava, K.C.; Shrivastava, D.; Patil, S.R.; Al Habib, S.; Hamza, M.; Ab Rahman, S.; Lynch, E.; Alam, M.K. Comparative Evaluation of Dental Implant Failure among Healthy and Well-Controlled Diabetic Patients—A 3-Year Retrospective Study. Int. J. Environ. Res. Public Health 2020, 17, 5253. [Google Scholar] [CrossRef]
- Mayta-Tovalino, F.; Mendoza-Martiarena, Y.; Tapia, P.R.; Alvarez, M.A.; Gálvez-Calla, L.; Calderón-Sánchez, J.; Bolaños-Cardenas, R.; Diaz-Sarabia, A. An 11-Year Retrospective Research Study of the Predictive Factors of Peri-Implantitis and Implant Failure: Analytic-Multicentric Study of 1279 Implants in Peru. Int. J. Dent. 2019, 2019, 3527872. [Google Scholar] [CrossRef]
- Nguyen, T.T.H.; Eo, M.Y.; Cho, Y.J.; Myoung, H.; Kim, S.M. 7-mm-long dental implants: Retrospective clinical outcomes in medically compromised patients. J. Korean Assoc. Oral Maxillofac. Surg. 2019, 45, 260–266. [Google Scholar] [CrossRef]
- Parihar, A.S.; Singh, R.; Vaibhav, V.; Kumar, K.; Singh, R.; Jerry, J.J. A 10 years retrospective study of assessment of prevalence and risk factors of dental implants failures. J. Fam. Med. Prim. Care 2020, 9, 1617–1619. [Google Scholar] [CrossRef]
- Shetty, K.; Parihar, A.S.; Madhuri, S.; Devanna, R.; Sharma, G.; Singh, R. Assessment of failure rate of dental implants in medically compromised patients. J. Fam. Med. Prim. Care 2020, 9, 883–885. [Google Scholar] [CrossRef]
- Manor, Y.; Simon, R.; Haim, D.; Garfunkel, A.; Moses, O. Dental implants in medically complex patients—A retrospective study. Clin. Oral Investig. 2017, 21, 701–708. [Google Scholar] [CrossRef]
- Niedermaier, R.; Stelzle, F.; Riemann, M.; Bolz, W.; Schuh, P.; Wachtel, H. Implant-Supported Immediately Loaded Fixed Full-Arch Dentures: Evaluation of Implant Survival Rates in a Case Cohort of up to 7 Years. Clin. Implant Dent. Relat. Res. 2016, 19, 4–19. [Google Scholar] [CrossRef] [PubMed]
- Alrabiah, M.; Alrahlah, A.; Al-Hamdan, R.S.; Al-Aali, K.A.; Labban, N.; Abduljabbar, T. Survival of adjacent-dental-implants in prediabetic and systemically healthy subjects at 5-years follow-up. Clin. Implant Dent. Relat. Res. 2019, 21, 232–237. [Google Scholar] [CrossRef] [PubMed]
- AbdulAzeez, A.R.; Alkinani, A.A. The Crucial Role of Plaque Control in Peri-Implant Mucositis Initiation as Opposed to the Role of Systemic Health Condition: A Cross-Sectional Study. Clin. Cosmet. Investig. Dent. 2021, 13, 257–268. [Google Scholar] [CrossRef] [PubMed]
- Kissa, J.; El Kholti, W.; Chemlali, S.; Kawtari, H.; Laalou, Y.; Albandar, J.M. Prevalence and risk indicators of peri-implant diseases in a group of Moroccan patients. J. Periodontol. 2020, 92, 1096–1106. [Google Scholar] [CrossRef]
- Al-Sowygh, Z.H.; Ab Ghani, S.M.; Sergis, K.; Vohra, F.; Akram, Z. Peri-implant conditions and levels of advanced glycation end products among patients with different glycemic control. Clin. Implant Dent. Relat. Res. 2018, 20, 345–351. [Google Scholar] [CrossRef]
- Abduljabbar, T.; Javed, F.; Malignaggi, V.; Vohra, F.; Kellesarian, S. Influence of implant location in patients with and without type 2 diabetes mellitus: 2-year follow-up. Int. J. Oral Maxillofac. Surg. 2017, 46, 1188–1192. [Google Scholar] [CrossRef]
- Dalago, H.R.; Filho, G.S.; Rodrigues, M.A.P.; Renvert, S.; Bianchini, M.A. Risk indicators for Peri-implantitis. A cross-sectional study with 916 implants. Clin. Oral Implant. Res. 2017, 28, 144–150. [Google Scholar] [CrossRef]
- Alrabiah, M.; Al-Aali, K.A.; Al-Sowygh, Z.H.; Binmahfooz, A.M.; Mokeem, S.A.; Abduljabbar, T. Association of advanced glycation end products with peri-implant inflammation in prediabetes and type 2 diabetes mellitus patients. Clin. Implant Dent. Relat. Res. 2018, 20, 535–540. [Google Scholar] [CrossRef]
- Mokeem, S.; Alfadda, S.A.; Al-Shibani, N.; Alrabiah, M.; Al-Hamdan, R.S.; Vohra, F.; Abduljabbar, T. Clinical and radiographic peri-implant variables around short dental implants in type 2 diabetic, prediabetic, and non-diabetic patients. Clin. Implant Dent. Relat. Res. 2019, 21, 60–65. [Google Scholar] [CrossRef]
- Al Amri, M.D.; Aldosari, A.M.A.; Al-Johany, S.S.; Al Baker, A.M.; Al Rifaiy, M.Q.; Al-Kheraif, A.A. Comparison of clinical and radiographic status around immediately loaded versus conventional loaded implants placed in patients with type 2 diabetes: 12- and 24-month follow-up results. J. Oral Rehabil. 2017, 44, 220–228. [Google Scholar] [CrossRef]
- Alasqah, M.N.; Al-Shibani, N.; Al-Aali, K.A.; Qutub, O.A.; Abduljabbar, T.; Akram, Z. Clinical indices and local levels of inflammatory biomarkers in per-implant health of obese and nonobese individuals. Clin. Implant Dent. Relat. Res. 2018, 21, 80–84. [Google Scholar] [CrossRef] [PubMed]
- Alqahtani, F.; Alqhtani, N.; Alkhtani, F.; Divakar, D.D.; Al-Kheraif, A.A.; Javed, F. Clinicoradiographic markers of peri-implantitis in cigarette-smokers and never-smokers with type 2 diabetes mellitus at 7-years follow-up. J. Periodontol. 2020, 91, 1132–1138. [Google Scholar] [CrossRef] [PubMed]
- Al Amri, M.D.; Abduljabbar, T.S.; Al-Johany, S.S.; Al Rifaiy, M.Q.; Aldosari, A.M.A.; Al-Kheraif, A.A. Comparison of clinical and radiographic parameters around short (6 to 8 mm in length) and long (11 mm in length) dental implants placed in patients with and without type 2 diabetes mellitus: 3-year follow-up results. Clin. Oral Implant. Res. 2017, 28, 1182–1187. [Google Scholar] [CrossRef] [PubMed]
- Al Amri, M.D.; Abduljabbar, T.S. Comparison of clinical and radiographic status of platform-switched implants placed in patients with and without type 2 diabetes mellitus: A 24-month follow-up longitudinal study. Clin. Oral Implant. Res. 2017, 28, 226–230. [Google Scholar] [CrossRef] [PubMed]
- Al Amri, M.D.; Abduljabbar, T.S.; Al-Kheraif, A.A.; Romanos, G.E.; Javed, F. Comparison of clinical and radiographic status around dental implants placed in patients with and without prediabetes: 1-year follow-up outcomes. Clin. Oral Implant. Res. 2017, 28, 231–235. [Google Scholar] [CrossRef]
- Abduljabbar, T.; Al-Sahaly, F.; Al-Kathami, M.; Afzal, S.; Vohra, F. Comparison of periodontal and peri-implant inflammatory parameters among patients with prediabetes, type 2 diabetes mellitus and non-diabetic controls. Acta Odontol. Scand. 2017, 75, 319–324. [Google Scholar] [CrossRef]
- Vohra, F.; Alkhudhairy, F.; Al-Kheraif, A.A.; Akram, Z.; Javed, F. Peri-implant parameters and C-reactive protein levels among patients with different obesity levels. Clin. Implant Dent. Relat. Res. 2018, 20, 130–136. [Google Scholar] [CrossRef]
- Abduljabbar, T.; Al-Sahaly, F.; Kellesarian, S.V.; Kellesarian, T.V.; Al-Anazi, M.; Al-Khathami, M.; Javed, F.; Vohra, F. Comparison of peri-implant clinical and radiographic inflammatory parameters and whole salivary destructive inflammatory cytokine profile among obese and non-obese men. Cytokine 2016, 88, 51–56. [Google Scholar] [CrossRef]
- Alshiddi, I.F.; Alsahhaf, A.; Alshagroud, R.S.; Al-Aali, K.A.; Vohra, F.; Abduljabbar, T. Clinical, radiographic, and restorative peri-implant measurements of narrow and standard diameter implants in obese and nonobese patients: A 3-year retrospective follow-up study. Clin. Implant Dent. Relat. Res. 2019, 21, 656–661. [Google Scholar] [CrossRef]
- Alkhudhairy, F.; Vohra, F.; Al-Kheraif, A.A.; Akram, Z. Comparison of clinical and radiographic peri-implant parameters among obese and non-obese patients: A 5-year study. Clin. Implant Dent. Relat. Res. 2018, 20, 756–762. [Google Scholar] [CrossRef]
- Hazem, A.; Bissada, N.; Demko, C.; Paes, A.; Lang, L. Comparison of Preprosthetic Implant Complications and Failures Between Obese and Nonobese Patients. Int. J. Oral Maxillofac. Implant. 2016, 31, 1093–1099. [Google Scholar] [CrossRef] [PubMed]
- Wang, I.; Ou, A.; Johnston, J.; Giannobile, W.V.; Yang, B.; Fenno, J.C.; Wang, H. Association between peri-implantitis and cardiovascular diseases: A case-control study. J. Periodontol. 2022, 93, 633–643. [Google Scholar] [CrossRef] [PubMed]
- Tallarico, M.; Canullo, L.; Xhanari, E.; Meloni, S.M. Dental implants treatment outcomes in patient under active therapy with alendronate: 3-year follow-up results of a multicenter prospective observational study. Clin. Oral Implant. Res. 2016, 27, 943–949. [Google Scholar] [CrossRef] [PubMed]
- Khoury, F.; Hidajat, H. Extensive Autogenous Bone Augmentation and Implantation in Patients Under Bisphosphonate Treatment: A 15-Case Series. Int. J. Periodontics Restor. Dent. 2016, 36, 9–18. [Google Scholar] [CrossRef]
- Suvarna, S.; Dutt, P.; Misra, A.; Usmani, N.; Suvarna, C. Intricate Assessment and Evaluation of Dental Implants in Patients on Bisphosphonate Therapy: A Retrospective Analysis. J. Contemp. Dent. Pract. 2016, 17, 414–417. [Google Scholar] [CrossRef]
- Corcuera-Flores, J.R.; Alonso-Domínguez, A.M.; Serrera-Figallo, M.; Torres-Lagares, D.; Castellanos-Cosano, L.; Machuca-Portillo, G. Relationship Between Osteoporosis and Marginal Bone Loss in Osseointegrated Implants: A 2-Year Retrospective Study. J. Periodontol. 2016, 87, 14–20. [Google Scholar] [CrossRef]
- Alsadi, W.; AbouSulaiman, A.; AlSabbagh, M.M. Retrospective Study of Dental Implants Survival Rate in Postmenopausal Women with Osteoporosis. Int. J. Dent. Oral Sci. 2021, 8, 4259. [Google Scholar] [CrossRef]
- Alsadi, W.; AbouSulaiman, A.; AlSabbagh, M.M. Association of dental implants success in bone density classification of postmenopausal women with osteoporosis—A clinical and radiographic prospective study. J. Indian Acad. Oral Med. Radiol. 2021, 33, 428. [Google Scholar] [CrossRef]
- Toy, V.; Uslu, M. Evaluation of long-term dental implant success and marginal bone loss in postmenopausal women. Niger. J. Clin. Pract. 2020, 23, 147–153. [Google Scholar]
- Chow, L.; Chow, T.W.; Chai, J.; Mattheos, N. Bone stability around implants in elderly patients with reduced bone mineral density—A prospective study on mandibular overdentures. Clin. Oral Implant. Res. 2017, 28, 966–973. [Google Scholar] [CrossRef]
- Temmerman, A.; Rasmusson, L.; Kübler, A.; Thor, A.; Merheb, J.; Quirynen, M. A Prospective, Controlled, Multicenter Study to Evaluate the Clinical Outcome of Implant Treatment in Women with Osteoporosis/Osteopenia: 5-Year Results. J. Dent. Res. 2018, 98, 84–90. [Google Scholar] [CrossRef] [PubMed]
- Temmerman, A.; Rasmusson, L.; Kübler, A.; Thor, A.; Quirynen, M. An open, prospective, non-randomized, controlled, multicentre study to evaluate the clinical outcome of implant treatment in women over 60 years of age with osteoporosis/osteopenia: 1-year results. Clin. Oral Implant. Res. 2017, 28, 95–102. [Google Scholar] [CrossRef] [PubMed]
- Heitz-Mayfield, L.J.; Aaboe, M.; Araujo, M.; Carrión, J.B.; Cavalcanti, R.; Cionca, N.; Cochran, D.; Darby, I.; Funakoshi, E.; Gierthmuehlen, P.C.; et al. Group 4 ITI Consensus Report: Risks and biologic complications associated with implant dentistry. Clin. Oral Implant. Res. 2018, 29 (Suppl. S16), 351–358. [Google Scholar] [CrossRef] [PubMed]
- Jiang, X.; Zhu, Y.; Liu, Z.; Tian, Z.; Zhu, S. Association between diabetes and dental implant complications: A systematic review and meta-analysis. Acta Odontol. Scand. 2021, 79, 9–18. [Google Scholar] [CrossRef]
- Dreyer, H.; Grischke, J.; Tiede, C.; Eberhard, J.; Schweitzer, A.; Toikkanen, S.E.; Glöckner, S.; Krause, G.; Stiesch, M. Epidemiology and risk factors of peri-implantitis: A systematic review. J. Periodontal Res. 2018, 53, 657–681. [Google Scholar] [CrossRef]
- Monje, A.; Catena, A.; Borgnakke, W.S. Association between diabetes mellitus/hyperglycaemia and peri-implant diseases: Systematic review and meta-analysis. J. Clin. Periodontol. 2017, 44, 636–648. [Google Scholar] [CrossRef]
- Andrade, C.A.S.; Paz, J.L.C.; de Melo, G.S.; Mahrouseh, N.; Januário, A.L.; Capeletti, L.R. Survival rate and peri-implant evaluation of immediately loaded dental implants in individuals with type 2 diabetes mellitus: A systematic review and meta-analysis. Clin. Oral Investig. 2022, 26, 1797–1810. [Google Scholar] [CrossRef]
- Guobis, Z.; Pacauskienė, I.; Astramskaite, I. General Diseases Influence on Peri-Implantitis Development: A Systematic Review. J. Oral Maxillofac. Res. 2016, 7, e5. [Google Scholar] [CrossRef]
- Monteiro, J.; Pellizzer, E.; Lemos, C.A.; de Moraes, S.; Vasconcelos, B.D.E. Is there an association between overweight/obesity and dental implant complications? A systematic review and meta-analysis. Int. J. Oral Maxillofac. Surg. 2019, 48, 1241–1249. [Google Scholar] [CrossRef]
- Turri, A.; Rossetti, P.; Canullo, L.; Grusovin, M.; Dahlin, C. Prevalence of Peri-implantitis in Medically Compromised Patients and Smokers: A Systematic Review. Int. J. Oral Maxillofac. Implant. 2016, 31, 111–118. [Google Scholar] [CrossRef]
- Nemati, F.; Rahbar-Roshandel, N.; Hosseini, F.; Mahmoudian, M.; Shafiei, M. Anti-Inflammatory Effects of Anti-Hypertensive Agents: Influence on Interleukin-1β Secretion by Peripheral Blood Polymorphonuclear Leukocytes from Patients with Essential Hypertension. Clin. Exp. Hypertens. 2011, 33, 66–76. [Google Scholar] [CrossRef] [PubMed]
- Schimmel, M.; Srinivasan, M.; McKenna, G.; Müller, F. Effect of advanced age and/or systemic medical conditions on dental implant survival: A systematic review and meta-analysis. Clin. Oral Implant. Res. 2018, 29, 311–330. [Google Scholar] [CrossRef] [PubMed]
- Stavropoulos, A.; Bertl, K.; Pietschmann, P.; Pandis, N.; Schiødt, M.; Klinge, B. The effect of antiresorptive drugs on implant therapy: Systematic review and meta-analysis. Clin. Oral Implant. Res. 2018, 29 (Suppl. S18), 54–92. [Google Scholar] [CrossRef] [PubMed]
- Mancini, L.; Americo, L.M.; Pizzolante, T.; Donati, R.; Marchetti, E. Impact of COVID-19 on Periodontitis and Peri-Implantitis: A Narrative Review. Front. Oral Health 2022, 3, 822824. [Google Scholar] [CrossRef]
| Diabetes | Frequencies | % of the Total |
|---|---|---|
| Higher risk | 17 | 33.3 % |
| Risk unchanged | 33 | 64.7 % |
| Lower risk | 1 | 2.0 % |
| Obesity | Frequencies | % of the Total |
|---|---|---|
| Higher risk | 5 | 83.3 % |
| Risk unchanged | 1 | 16.7 % |
| CVD | Frequencies | % of the Total |
|---|---|---|
| Higher risk | 2 | 15.4 % |
| Risk unchanged | 11 | 84.6 % |
| Hypertension | Frequencies | % of the Total |
|---|---|---|
| Higher risk | 1 | 14.3 % |
| Risk unchanged | 5 | 71.4 % |
| Lower risk | 1 | 14.3 % |
| Osteoporosis | Frequencies | % of the Total |
|---|---|---|
| Higher risk | 3 | 21.4 % |
| Risk unchanged | 11 | 78.6 % |
| Antiresorptive Drugs | Frequencies | % of the total |
|---|---|---|
| Higher risk | 1 | 16.7 % |
| Risk unchanged | 5 | 83.3 % |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sbricoli, L.; Bazzi, E.; Stellini, E.; Bacci, C. Systemic Diseases and Biological Dental Implant Complications: A Narrative Review. Dent. J. 2023, 11, 10. https://doi.org/10.3390/dj11010010
Sbricoli L, Bazzi E, Stellini E, Bacci C. Systemic Diseases and Biological Dental Implant Complications: A Narrative Review. Dentistry Journal. 2023; 11(1):10. https://doi.org/10.3390/dj11010010
Chicago/Turabian StyleSbricoli, Luca, Elissar Bazzi, Edoardo Stellini, and Christian Bacci. 2023. "Systemic Diseases and Biological Dental Implant Complications: A Narrative Review" Dentistry Journal 11, no. 1: 10. https://doi.org/10.3390/dj11010010
APA StyleSbricoli, L., Bazzi, E., Stellini, E., & Bacci, C. (2023). Systemic Diseases and Biological Dental Implant Complications: A Narrative Review. Dentistry Journal, 11(1), 10. https://doi.org/10.3390/dj11010010