Comparative Dissemination of Aerosol and Splatter Using Suction Device during Ultrasonic Scaling: A Pilot Study
Abstract
:1. Introduction
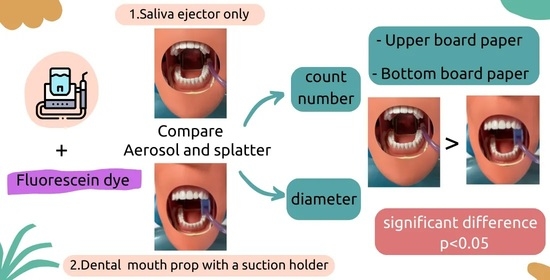
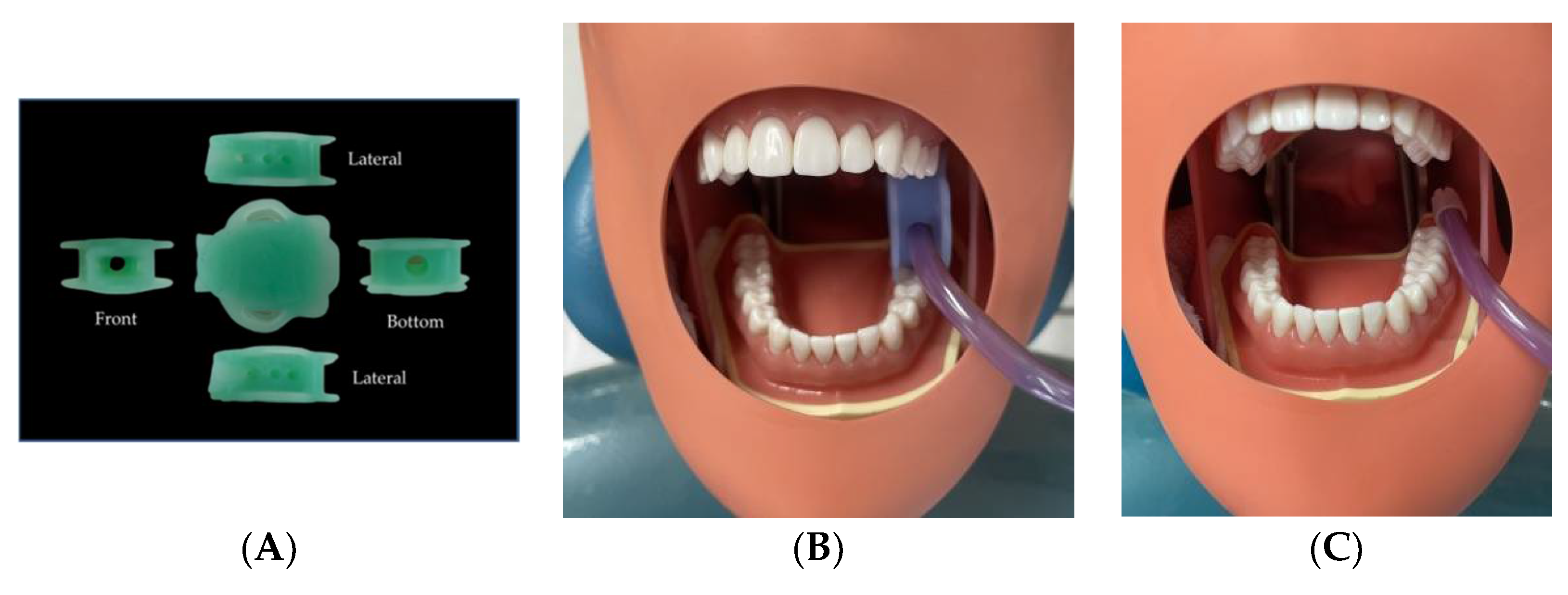
2. Materials and Methods
2.1. Laboratory Platform Setup
2.2. Experimental Design
2.3. Effects of Dental Suction
2.4. Image Processing
2.5. Statistical Analysis
3. Results
3.1. The Size of the Aerosol and Splatter Particles
3.2. Comparison of the Aerosol and Splatter Particle Size on the Upper and Bottom Board Paper
3.3. Comparison of the Aerosol and Splatter Particle Count Number on the Upper and Bottom Board Paper
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gallagher, J.E.; Sukriti, K.C.; Johnson, I.G.; Al-Yaseen, W.; Jones, R.; McGregor, S.; Robertson, M.; Harris, R.; Innes, N.; Wade, W.G. A systematic review of contamination (aerosol, splatter and droplet generation) associated with oral surgery and its relevance to COVID-19. BDJ Open 2020, 6, 25. [Google Scholar] [CrossRef] [PubMed]
- Fennelly, M.; Gallagher, C.; Harding, M.; Hellebust, S.; Wenger, J.; O’Sullivan, N.; O’Connor, D.; Prentice, M. Real-time Monitoring of Aerosol Generating Dental Procedures. J. Dent. 2022, 120, 104092. [Google Scholar] [CrossRef]
- Melzow, F.; Mertens, S.; Todorov, H.; Groneberg, D.A.; Paris, S.; Gerber, A. Aerosol exposure of staff during dental treatments: A model study. BMC Oral Health 2022, 22, 128. [Google Scholar] [CrossRef]
- Allison, J.R.; Currie, C.C.; Edwards, D.C.; Bowes, C.; Coulter, J.; Pickering, K.; Kozhevnikova, E.; Durham, J.; Nile, C.J.; Jakubovics, N.; et al. Evaluating aerosol and splatter following dental procedures: Addressing new challenges for oral health care and rehabilitation. J. Oral Rehabil. 2020, 48, 61–72. [Google Scholar] [CrossRef]
- World Health Organization. Infection Prevention and Control of Epidemic- and Pandemic-Prone Acute Respiratory Infections in Health Care; WHO: Geneva, Switzerland, 2014. [Google Scholar]
- Han, P.; Li, H.; Walsh, L.J.; Ivanovski, S. Splatters and Aerosols Contamination in Dental Aerosol Generating Procedures. Appl. Sci. 2021, 11, 1914. [Google Scholar] [CrossRef]
- Leggat, P.A.; Kedjarune, U. Bacterial aerosols in the dental clinic: A review. Int. Dent. J. 2001, 51, 39–44. [Google Scholar] [CrossRef]
- Rautemaa, R.; Nordberg, A.; Wuolijoki-Saaristo, K.; Meurman, J.H. Bacterial aerosols in dental practice—A potential hospital infection problem? J. Hosp. Infect. 2006, 64, 7681. [Google Scholar] [CrossRef]
- Legnani, P.; Checchi, L.; Pelliccioni, G.A.; D’Achille, C. Atmospheric contamination during dental procedures. Quintessence Int. 1994, 25, 435–439. [Google Scholar]
- Sharma, N.S.; Shrivastav, S.S.; Hazarey, P.V. An Inexpensive Universal Mouth Props, Saliva Ejector and Tongue Retractor. J. Ind. Orthod. Soc. 2012, 46, 169–171. [Google Scholar] [CrossRef]
- Dahlke, W.O.; Cottam, M.R.; Herring, M.C.; Leavitt, J.M.; Ditmyer, M.M.; Walker, R.S. Evaluation of the spatter-reduction effectiveness of two dry-field isolation techniques. J. Am. Dent. Assoc. 2012, 143, 1199–1204. [Google Scholar] [CrossRef]
- Li, X.; Mak, C.M.; Ma, K.W.; Wong, H.M. How the high-volume evacuation alters the flow-field and particle removal characteristics in the mock-up dental clinic. Build. Environ. 2021, 205, 108225. [Google Scholar] [CrossRef] [PubMed]
- Marsh, B.P.; Chada, N.; Gari, R.R.S.; Sigdel, K.P.; King, G.M. The Hessian Blob Algorithm: Precise Particle Detection in Atomic Force Microscopy Imagery. Sci. Rep. 2018, 8, 978. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, M.; Wu, T.; Beeman, S.C.; Cullen-McEwen, L.; Bertram, J.F.; Charlton, J.R.; Baldelomar, E.; Bennett, K.M. Efficient Small Blob Detection Based on Local Convexity, Intensity and Shape Information. IEEE Trans. Med. Imaging 2016, 35, 1127–1137. [Google Scholar] [CrossRef]
- Thurzo, A.; Urbanová, W.; Waczulíková, I.; Kurilová, V.; Mriňáková, B.; Kosnáčová, H.; Gális, B.; Varga, I.; Matajs, M.; Novák, B. Dental Care and Education Facing Highly Transmissible SARS-CoV-2 Variants: Prospective Biosafety Setting: Prospective, Single-Arm, Single-Center Study. Int. J. Environ. Res. 2022, 19, 7693. [Google Scholar] [CrossRef] [PubMed]
- Gross, K.B.; Overman, P.R.; Cobb, C.; Brockmann, S. Aerosol generation by two ultrasonic scalers and one sonic scaler: A comparative study. J. Dent. Hyg. 1992, 66, 314–318. [Google Scholar]
- Veena, H.R.; Mahantesha, S.; Joseph, P.A.; Patil, S.H. Dissemination of aerosol and splatter during ultrasonic scaling: A pilot study. J. Infect. Public Health 2015, 8, 260–265. [Google Scholar] [CrossRef]
- Jacks, M.E. A laboratory comparison of evacuation devices on aerosol reduction. J. Dent. Hyg. 2002, 76, 202–206. [Google Scholar]
- Morawska, L.; Johnsona, G.R.; Ristovski, Z.D.; Hargreaves, M.; Mengersen, K.; Corbett, S.; Chao, C.Y.H.; Li, Y.; Katoshevski, D. Size distribution and sites of origin of droplets expelled from the human respiratory tract during expiratory activities. J. Aerosol. Sci. 2009, 40, 256–269. [Google Scholar] [CrossRef] [Green Version]
- Yan, J.; Grantham, M.; Pantelic, J.; Bueno de Mesquita, P.J.; Albert, B.; Liu, F.; Ehrman, S.; Milton, D.K. Infectious virus in exhaled breath of symptomatic seasonal influenza cases from a college community. Proc. Natl. Acad. Sci. USA 2018, 115, 1081–1086. [Google Scholar] [CrossRef] [Green Version]
- Holloman, J.L.; Mauriello, S.M.; Pimenta, L.; Arnold, R.R. Comparison of suction device with saliva ejector for aerosol and spatter reduction during ultrasonic scaling. J. Am. Dent. Assoc. 2015, 146, 27–33. [Google Scholar] [CrossRef] [PubMed]
- James, R.; Mani, A. Dental aerosols: A silent hazard in dentistry! Int. J. Sci. Res. 2016, 5, 1761–1763. [Google Scholar]
- Fennelly, K.P. Particle sizes of infectious aerosols: Implications for infection control. Lancet Respir. Med. 2020, 8, 914–924. [Google Scholar] [CrossRef]
- Rapaport, B.H.J.; Smith, M.T.; Brown, J.S. An audit of routine practice: A prospective study on the use of mouth props in oral surgery. Br. Dent. J. 2020, 228, 938–942. [Google Scholar] [CrossRef] [PubMed]
- Day, R. A new mouth prop design. Br. Dent. J. 2019, 227, 643. [Google Scholar]
- Szymanska, J. Dental bioaerosol as an occupational hazard in a dentist’s workplace. Ann. Agric. Environ. Med. 2007, 14, 203–207. [Google Scholar] [PubMed]
- Morawska, L.; Milton, D.K. It is time to address airborne transmission of coronavirus disease 2019 (COVID-19). Clin. Infect. Dis. 2020, 71, 2311–2313. [Google Scholar] [CrossRef] [PubMed]
- National Research Council. Rapid Expert Consultation on the Possibility of Bioaerosol Spread of SARS-CoV-2 for the COVID-19 Pandemic (1 April 2020); The National Academies Press: Washington, DC, USA, 2020.
- Tang, S.; Mao, Y.; Jones, R.M.; Tan, Q.; Ji, J.S.; Li, N.; Shen, J.; Lv, Y.; Pan, L.; Ding, P.; et al. Aerosol transmission of SARS-CoV-2? Evidence, prevention and control. Environ. Int. 2020, 144, 106039. [Google Scholar] [CrossRef] [PubMed]


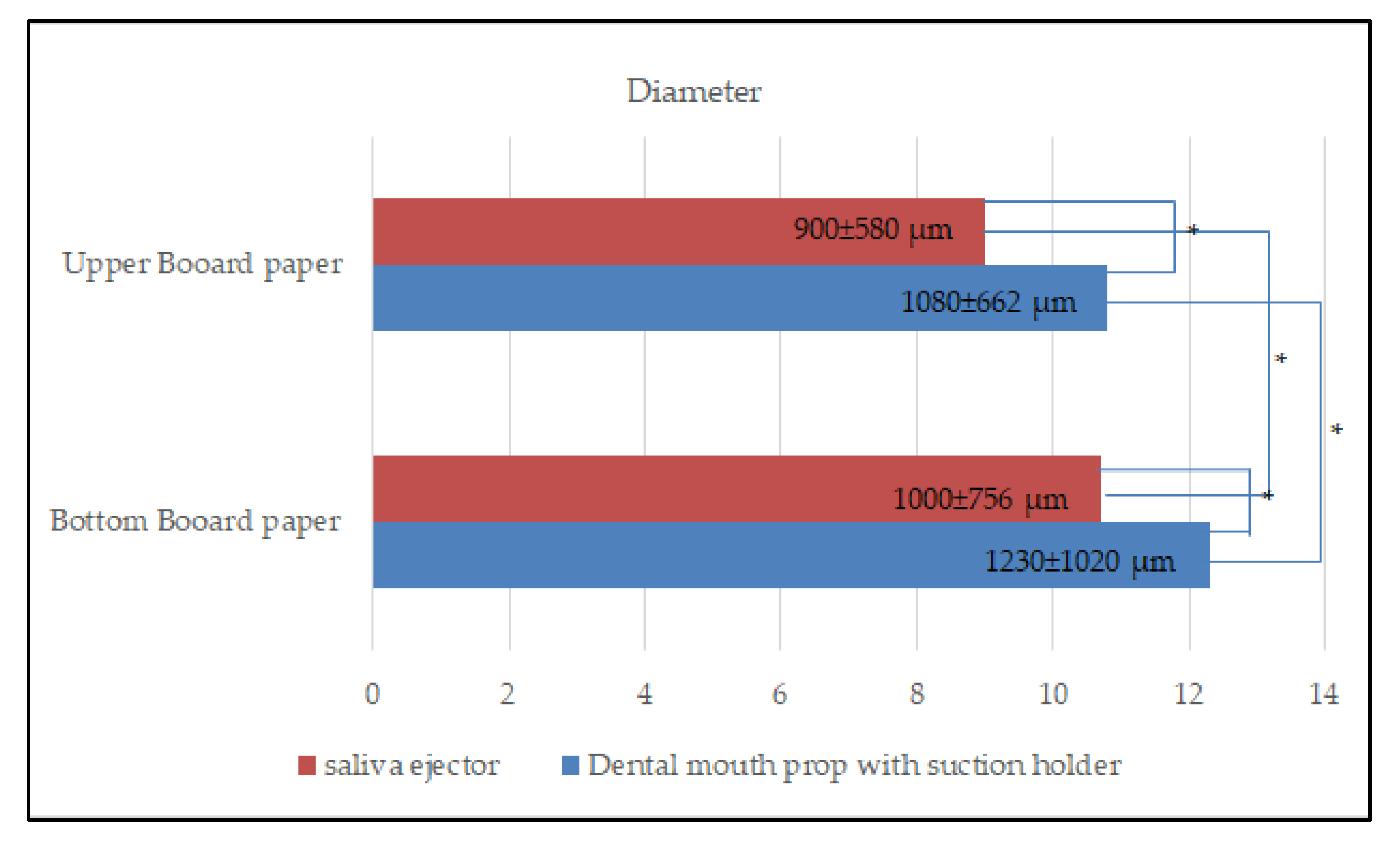
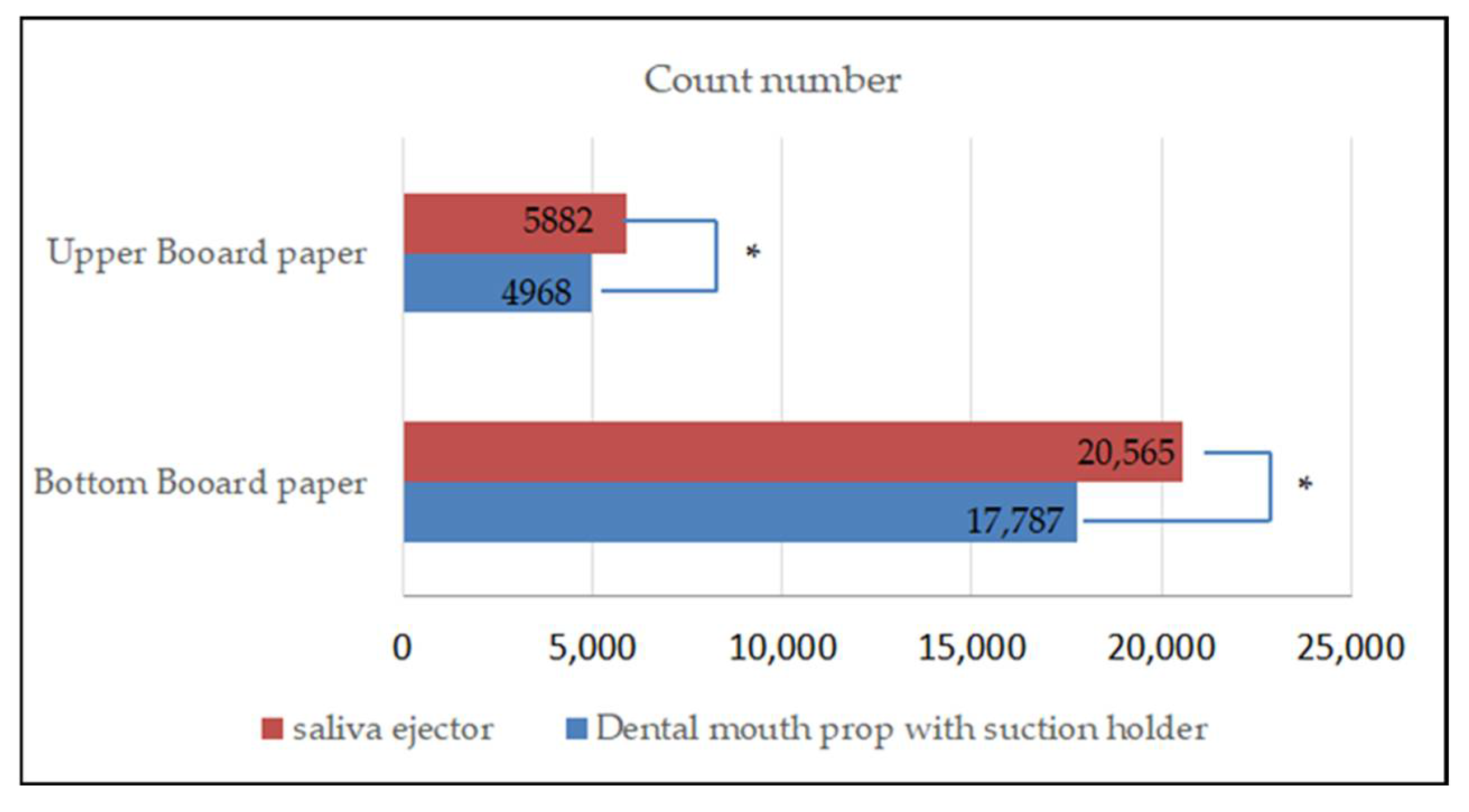
| Device | Time | Upper Board Paper | Bottom Board Paper | ||
|---|---|---|---|---|---|
| Diameter (µm) | Count Number | Diameter (µm) | Count Number | ||
| Dental mouth prop with suction holder | 1 | 990 ± 668 | 9055 | 970 ± 779 | 16,486 |
| 2 | 1170 ± 558 | 2426 | 1720 ± 1253 | 13,956 | |
| 3 | 1290 ± 659 | 3428 | 1120 ± 910 | 22,922 | |
| mean | 1080 ± 662 | 4968 | 1230 ± 1020 | 17,787 | |
| Saliva ejector | 1 | 1340 ± 678 | 3560 | 1090 ± 879 | 24,065 |
| 2 | 820 ± 486 | 8836 | 940 ± 676 | 19,257 | |
| 3 | 730 ± 503 | 5253 | 940 ± 640 | 18,376 | |
| mean | 900 ± 580 | 5882 | 1000 ± 756 | 20,565 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Engsomboon, N.; Pachimsawat, P.; Thanathornwong, B. Comparative Dissemination of Aerosol and Splatter Using Suction Device during Ultrasonic Scaling: A Pilot Study. Dent. J. 2022, 10, 142. https://doi.org/10.3390/dj10080142
Engsomboon N, Pachimsawat P, Thanathornwong B. Comparative Dissemination of Aerosol and Splatter Using Suction Device during Ultrasonic Scaling: A Pilot Study. Dentistry Journal. 2022; 10(8):142. https://doi.org/10.3390/dj10080142
Chicago/Turabian StyleEngsomboon, Nutthawadee, Praewpat Pachimsawat, and Bhornsawan Thanathornwong. 2022. "Comparative Dissemination of Aerosol and Splatter Using Suction Device during Ultrasonic Scaling: A Pilot Study" Dentistry Journal 10, no. 8: 142. https://doi.org/10.3390/dj10080142
APA StyleEngsomboon, N., Pachimsawat, P., & Thanathornwong, B. (2022). Comparative Dissemination of Aerosol and Splatter Using Suction Device during Ultrasonic Scaling: A Pilot Study. Dentistry Journal, 10(8), 142. https://doi.org/10.3390/dj10080142