Tooth Agenesis Patterns in Orofacial Clefting Using Tooth Agenesis Code: A Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Eligibility and Exclusion Criteria
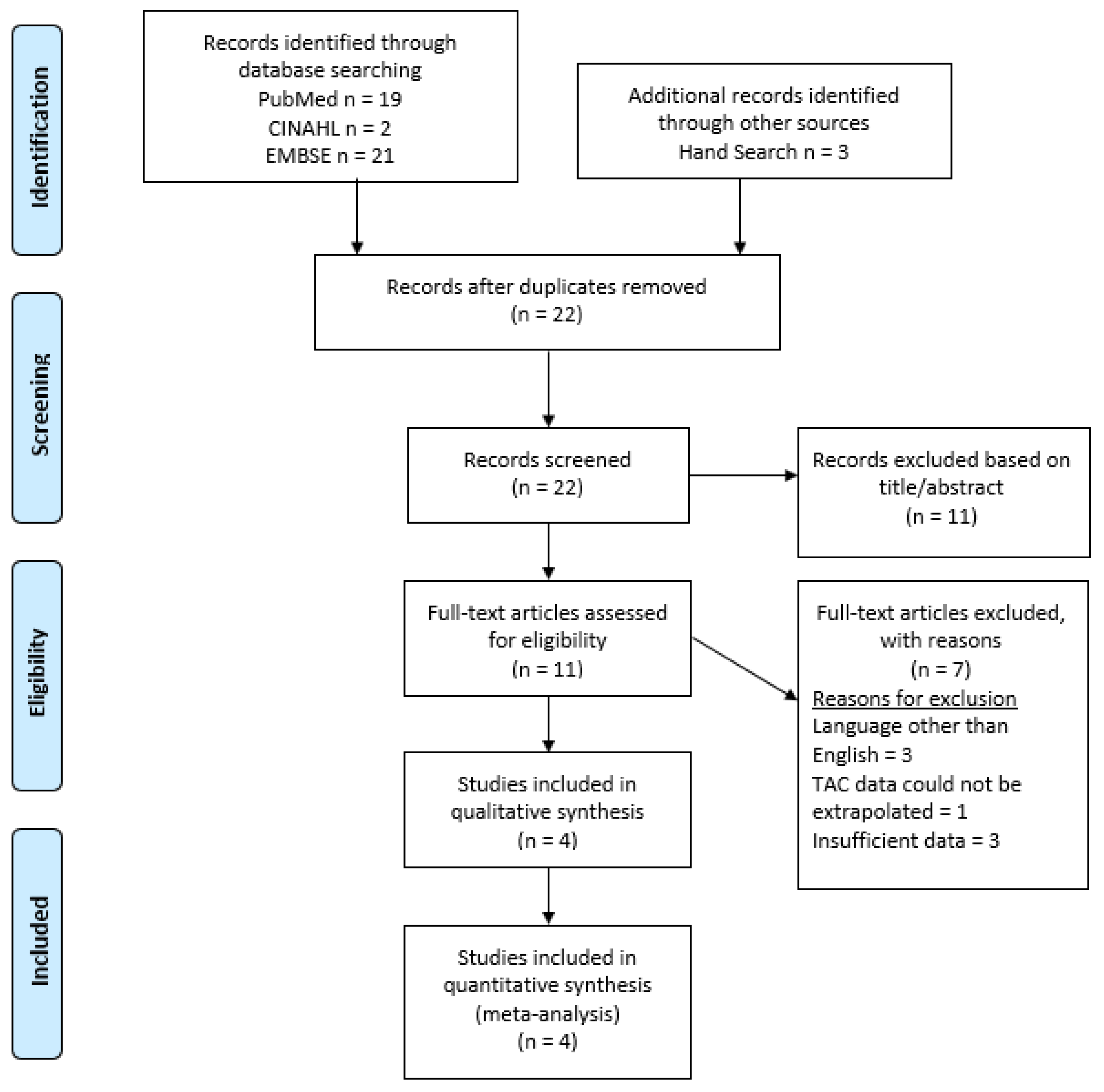
2.3. Study Selection
2.4. Data Collection
2.5. Meta-Analysis
3. Results
3.1. Study Selection
3.2. Study Characteristics
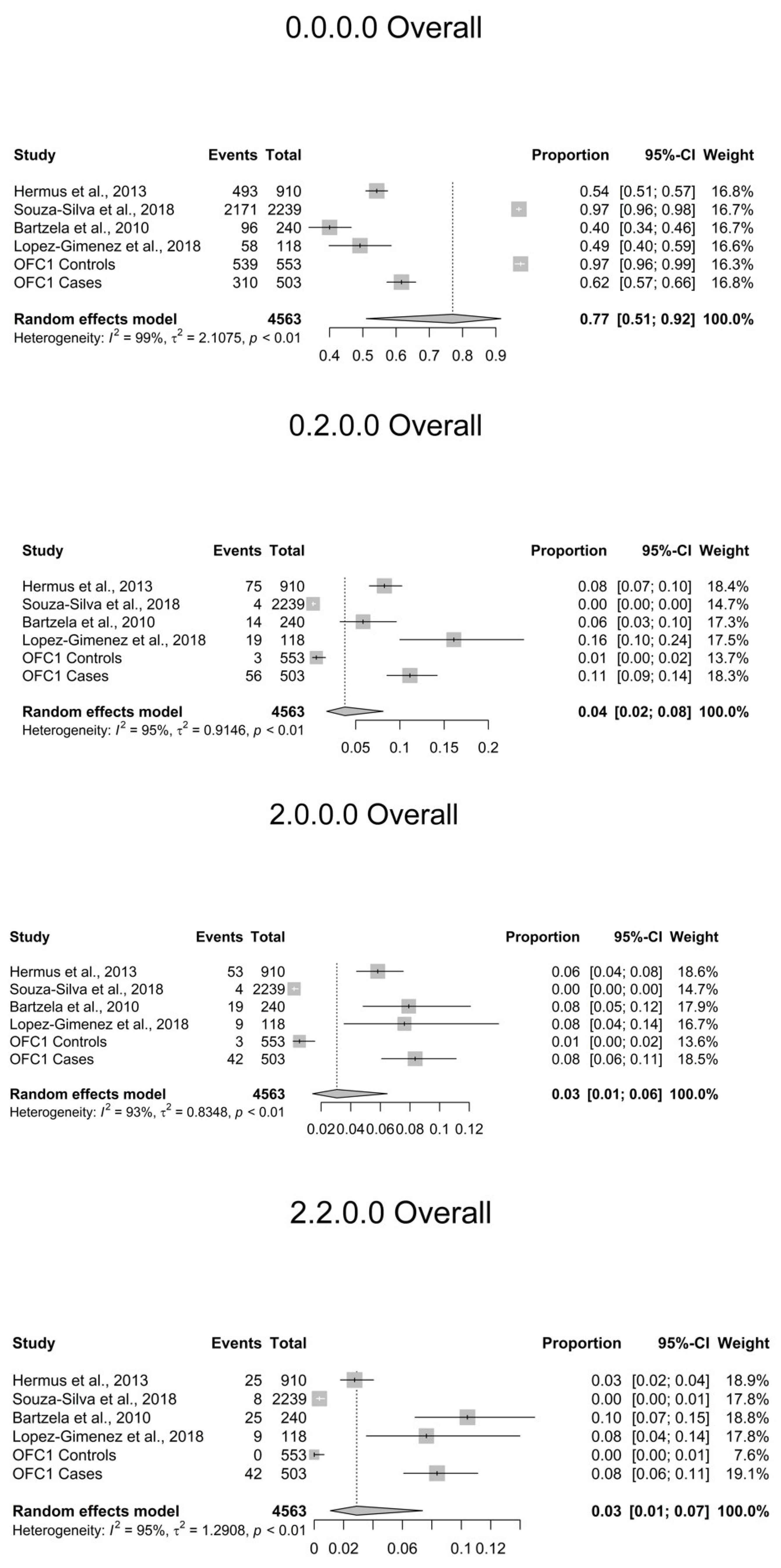
3.3. TAC Patterns
3.4. Sex
3.5. Cleft Type
3.6. Laterality
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Letra, A.; Menezes, R.; Granjeiro, J.; Vieira, A. Defining Subphenotypes for Oral Clefts Based on Dental Development. J. Dent. Res. 2007, 86, 986–991. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Walker, S.C.; Mattick, C.R.; Hobson, R.S.; Steen, I.N. Abnormal tooth size and morphology in subjects with cleft lip and/or palate in the north of England. Eur. J. Orthod. 2009, 31, 68–75. [Google Scholar] [CrossRef] [PubMed]
- Rawashdeh, M.A.; Abu Sirdaneh, E.O. Crown morphologic abnormalities in the permanent dentition of patients with cleft lip and palate. J. Craniofacial Surg. 2009, 20, 465. [Google Scholar] [CrossRef] [Green Version]
- Wu, T.-T.; Chen, P.K.T.; Lo, L.-J.; Cheng, M.-C.; Ko, E.W.-C. The characteristics and distribution of dental anomalies in patients with cleft. Chang Gung Med. J. 2011, 34, 306. [Google Scholar]
- Howe, B.; Cooper, M.E.; Vieira, A.R.; Weinberg, S.; Resick, J.M.; Nidey, N.; Wehby, G.L.; Marazita, M.L.; Uribe, L.M. Spectrum of Dental Phenotypes in Nonsyndromic Orofacial Clefting. J. Dent. Res. 2015, 94, 905–912. [Google Scholar] [CrossRef] [PubMed]
- Jordan, R.E.; Kraus, B.S.; Neptune, C.M. Dental abnormalities associated with cleft lip and/or palate. Cleft Palate J. 1966, 3, 22–55. [Google Scholar] [CrossRef] [PubMed]
- Ranta, R.; Stegars, T.; Rintala, A.E. Correlations of hypodontia in children with isolated cleft palate. Cleft Palate J. 1983, 20, 163. [Google Scholar]
- Schroeder, D.C.; Green, L.J. Frequency of Dental Trait Anomalies in Cleft, Sibling, and Noncleft Groups. J. Dent. Res. 1975, 54, 802–807. [Google Scholar] [CrossRef]
- Fan, L.; Kan, S.; Yang, F.; Xu, H.; Li, H.; Zhu, G.; Ma, L.; Zhang, C.; Lou, S.; Li, D.; et al. Non-syndromic cleft lip with or without palate susceptible loci is associated with tooth agenesis. Oral Dis. 2019, 25, 803–811. [Google Scholar] [CrossRef]
- Phan, M.; Conte, F.; Khandelwal, K.D.; Ockeloen, C.W.; Bartzela, T.; Kleefstra, T.; van Bokhoven, H.; Rubini, M.; Zhou, H.; Carels, C.E. Tooth agenesis and orofacial clefting: Genetic brothers in arms? Hum. Genet. 2016, 135, 1299–1327. [Google Scholar] [CrossRef] [Green Version]
- Ranta, R. A review of tooth formation in children with cleft lip/palate. Am. J. Orthod. Dentofac. Orthop. 1986, 90, 11–18. [Google Scholar] [CrossRef]
- Korolenkova, M.V.; Starikova, N.V.; Udalova, N.V. The role of external aetiological factors in dental anomalies in non-syndromic cleft lip and palate patients. Eur. Arch. Paediatr. Dent. 2019, 20, 105–111. [Google Scholar] [CrossRef] [PubMed]
- Bartzela, T.N.; Carels, C.E.; Bronkhorst, E.M.; Rønning, E.; Rizell, S.; Kuijpers-Jagtman, A.M. Tooth agenesis patterns in bilateral cleft lip and palate. Eur. J. Oral Sci. 2010, 118, 47–52. [Google Scholar] [CrossRef] [PubMed]
- Hermus, R.R.; van Wijk, A.J.; Tan, S.P.K.; Kramer, G.J.C.; Ongkosuwito, E.M. Patterns of tooth agenesis in patients with orofacial clefts. Eur. J. Oral Sci. 2013, 121, 328–332. [Google Scholar] [CrossRef]
- López-Giménez, A.; Silvestre-Rangil, J.; Silvestre, F.J.; Paredes-Gallardo, V. Tooth agenesis code (TAC) in complete unilateral and bilateral cleft lip and palate patients. Odontology 2017, 106, 257–265. [Google Scholar] [CrossRef]
- Silva, B.; Vieira, W.; Bernardino, Í.D.M.; Batista, M.J.; Bittencourt, M.A.V.; Paranhos, L.R. Non-syndromic tooth agenesis patterns and their association with other dental anomalies: A retrospective study. Arch. Oral Biol. 2018, 96, 26–32. [Google Scholar] [CrossRef]
- van Wijk, A.J.; Tan, S.P. A numeric code for identifying patterns of human tooth agenesis: A new approach. Eur. J. Oral Sci. 2006, 114, 97–101. [Google Scholar] [CrossRef]
- Bartzela, T.N.; Carels, C.E.; Bronkhorst, E.M.; Jagtman, A.M.K. Tooth agenesis patterns in unilateral cleft lip and palate in humans. Arch. Oral Biol. 2013, 58, 596–602. [Google Scholar] [CrossRef]
- De Stefani, A.; Bruno, G.; Balasso, P.; Mazzoleni, S.; Baciliero, U.; Gracco, A. Teeth agenesis evaluation in an Italian sample of complete unilateral and bilateral cleft lip and palate patients. Minerva Stomatol. 2018, 67, 156–164. [Google Scholar] [CrossRef]
- Dreesen, K.; Swinnen, S.; Devriendt, K.; Carels, C. Tooth agenesis patterns and phenotype variation in a cohort of Belgian patients with hypodontia and oligodontia clustered in 79 families with their pedigrees. Eur. J. Orthod. 2013, 36, 99–106. [Google Scholar] [CrossRef] [Green Version]
- Antonarakis, G.S.; Suri, S. Prevalence and patterns of permanent tooth agenesis in patients with nonsyndromic Pierre Robin sequence. Am. J. Orthod. Dentofac. Orthop. 2014, 145, 452–460. [Google Scholar] [CrossRef] [PubMed]
- Stavropoulos, D.; Bartzela, T.; Bronkhorst, E.; Mohlin, B.; Hagberg, C. Dental agenesis patterns of permanent teeth in Apert syndrome. Eur. J. Oral Sci. 2011, 119, 198–203. [Google Scholar] [CrossRef] [PubMed]
- Stavropoulos, D.; Bartzela, T.; Tarnow, P.; Mohlin, B.; Kahnberg, K.-E.; Hagberg, C. Dental agenesis patterns in Crouzon syndrome. Swed. Dent. J. 2011, 35, 195–201. [Google Scholar] [PubMed]
- de Smalen, A.; van Nunen, D.P.F.; Hermus, R.R.; Ongkosuwito, E.M.; van Wijk, A.J.; Griot, J.P.W.D.; Breugem, C.C.; Kramer, G.J.C. Permanent tooth agenesis in non-syndromic Robin sequence and cleft palate: Prevalence and patterns. Clin. Oral Investig. 2017, 21, 2273–2281. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shamseer, L.; Moher, D.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: Elaboration and explanation. BMJ 2015, 350, g7647. [Google Scholar] [CrossRef] [Green Version]
- Ranta, R. Hypodontia and delayed development of the second premolars in cleft palate children. Eur. J. Orthod. 1983, 5, 145–148. [Google Scholar] [CrossRef]
- Konstantonis, D.; Nassika, M.; Athanasiou, M.; Vastardis, H. Subphenotypes in Non-Syndromic Orofacial Cleft Patients Based on the Tooth Agenesis Code (TAC). Children 2022, 9, 437. [Google Scholar] [CrossRef]
| Maxillary Right (Q1) | Maxillary Left (Q2) | |||||||||||||
| Maxillary | 17 | 16 | 15 | 14 | 13 | 12 | 11 | 21 | 22 | 23 | 24 | 25 | 26 | 27 |
| AV | 64 | 32 | 16 | 8 | 4 | 2 | 1 | 1 | 2 | 4 | 8 | 16 | 32 | 64 |
| Mandibular | 47 | 46 | 45 | 44 | 43 | 42 | 41 | 31 | 32 | 33 | 34 | 35 | 36 | 37 |
| Mandibular Right (Q4) | Mandibular Left (Q3) | |||||||||||||
| Study Title | Authors | Publication Date | Control Group | Outcome Assessed | Sample Size | Sample | Sex Provided |
|---|---|---|---|---|---|---|---|
| Tooth agenesis patterns in bilateral cleft lip and palate [18] | Theodosia N. Bartzela, Carine E.L. Carels, Ewald M. Bronkhorst, Elisabeth Rønning, Sara Rizell, Anne Marie Kuijpers-Jagtman | 2010 | No | TAC patterns | 240 | CL/P | No |
| Patterns of tooth agenesis in patients with orofacial clefts [14] | Ruurd R. Hermus, Arjen J. van Wijk, Stephan P. K. Tan, Gem J. C. Kramer, Edwin M. Ongkosuwito | 2013 | No | TAC patterns | 910 | CL/P | Yes |
| Tooth agenesis code (TAC) in complete unilateral and bilateral cleft lip and palate patients [15] | Ana López-Giménez, Javier Silvestre-Rangil, Francisco Javier Silvestre, Vanessa Paredes-Gallardo | 2017 | No | TAC patterns | 118 | CL/P | No |
| Non-syndromic tooth agenesis patterns and their association with other dental anomalies: A retrospective study [16] | Bianca Núbia Souza-Silva, Walbert de Andrade Vieira, Ítalo de Macedo Bernardino, Marília Jesus Batistad, Marcos Alan Vieira Bittencourt, Luiz Renato Paranhos | 2018 | No | TAC patterns | 2239 | Non-CL/P | No |
| OFC1 Data | Unpublished | Yes | TAC patterns | 1056 | CL/P and Non-CL/P | Yes |
| Combined Data Proportion (95% CI) | I2: Combined | Case Data Proportion (95% CI) | I2: Cases | Control Data Proportion (95% CI) | I2: Controls | |
|---|---|---|---|---|---|---|
| 0.0.0.0 | 0.77 (0.51, 0.915) | 99.36% | 0.516 (0.432, 0.599) | 90.4% | 0.971 (0.964, 0.976) | 0% |
| 0.2.0.0 | 0.038 (0.017, 0.081) | 95.06% | 0.097 (0.07, 0.135) | 76.37% | 0.003 (0.001, 0.009) | 52.85% |
| 2.0.0.0 | 0.031 (0.014, 0.065) | 93.43% | 0.071 (0.058, 0.086) | 19.07% | 0.003 (0.001, 0.009) | 52.85% |
| 2.2.0.0 | 0.029 (0.011, 0.074) | 95.12% | 0.066 (0.035, 0.119) | 89.54% | 0.003 (0.002, 0.006) | 0% |
| 0.16.0.0 | 0.005 (0.002, 0.015) | 71.07% | 0.012 (0.005, 0.025) | 44.28% | 0.001 (0, 0.006) | 31.51% |
| 0.0.16.16 | 0.003 (0.001, 0.011) | 66.22% | 0.009 (0.004, 0.018) | 15.08% | 0.001 (0, 0.004) | 0% |
| 0.0.0.16 | 0.005 (0.002, 0.009) | 37.02% | 0.007 (0.004, 0.013) | 0% | 0.002 (0.001, 0.005) | 0% |
| 16.16.0.0 | 0.004 (0.001, 0.012) | 71.33% | 0.008 (0.003, 0.021) | 51.68% | 0.001 (0, 0.003) | 0% |
| 16.16.16.16 | 0.003 (0.001, 0.007) | 46.54% | 0.006 (0.003, 0.012) | 0% | 0.001 (0, 0.004) | 0% |
| 0.0.16.0 | 0.004 (0.002, 0.01) | 59.28% | 0.008 (0.004, 0.015) | 14.71% | 0.001 (0, 0.003) | 0% |
| 16.0.0.0 | 0.005 (0.002, 0.012) | 54.64% | 0.008 (0.005, 0.014) | 0% | 0.001 (0, 0.006) | 31.51% |
| 0.18.0.0 | 0.003 (0.001, 0.009) | 50.54% | 0.006 (0.002, 0.013) | 18.98% | 0 (0, 0.003) | 0% |
| 16.2.0.0 | 0.003 (0.001, 0.008) | 51.36% | 0.005 (0.002, 0.013) | 30.72% | 0 (0, 0.003) | 0% |
| 2.16.0.0 | 0.003 (0.001, 0.011) | 68.77% | 0.005 (0.001, 0.02) | 66.83% | 0 (0, 0.003) | 0% |
| 0.0.2.0 | 0.002 (0.001, 0.005) | 0% | 0.004 (0.002, 0.009) | 0% | 0.001 (0, 0.004) | 0% |
| 0.1.0.0 | 0.003 (0.001, 0.006) | 15.53% | 0.004 (0.002, 0.009) | 0% | 0.001 (0, 0.003) | 0% |
| 0.2.16.0 | 0.002 (0.001, 0.008) | 54.41% | 0.004 (0.001, 0.015) | 50.02% | 0 (0, 0.003) | 0% |
| 16.18.16.16 | 0.002 (0.001, 0.006) | 23.5% | 0.004 (0.002, 0.009) | 0% | 0 (0, 0.003) | 0% |
| 18.0.0.0 | 0.002 (0, 0.01) | 71.05% | 0.004 (0.001, 0.022) | 71.06% | 0 (0, 0.003) | 0% |
| 18.18.0.0 | 0.005 (0.001, 0.015) | 72.51% | 0.009 (0.003, 0.024) | 65.58% | 0 (0, 0.003) | 0% |
| 2.18.0.0 | 0.003 (0.001, 0.008) | 51.66% | 0.004 (0.002, 0.013) | 36.91% | 0 (0, 0.003) | 0% |
| 2.2.16.16 | 0.002 (0.001, 0.006) | 24.42% | 0.004 (0.002, 0.009) | 0% | 0.001 (0, 0.003) | 0% |
| 0.0.0.2 | 0.001 (0.001, 0.003) | 0% | 0.002 (0, 0.006) | 0% | 0.001 (0, 0.003) | 0% |
| 0.2.16.16 | 0.001 (0.001, 0.004) | 0% | 0.002 (0.001, 0.007) | 0% | 0 (0, 0.003) | 0% |
| 0.4.0.0 | 0.002 (0.001, 0.004) | 0% | 0.003 (0.001, 0.007) | 0% | 0.001 (0, 0.003) | 0% |
| 0.8.0.0 | 0.001 (0.001, 0.003) | 0% | 0.002 (0.001, 0.007) | 0% | 0.001 (0, 0.003) | 0% |
| 1.0.0.0 | 0.003 (0.001, 0.007) | 43.62% | 0.005 (0.002, 0.011) | 0% | 0.001 (0, 0.003) | 0% |
| 16.18.0.0 | 0.002 (0.001, 0.005) | 15.81% | 0.003 (0.001, 0.008) | 0% | 0 (0, 0.003) | 0% |
| 18.18.16.16 | 0.003 (0.001, 0.01) | 67.84% | 0.005 (0.001, 0.019) | 62.8% | 0 (0, 0.003) | 0% |
| 0.0.32.32 | 0.001 (0, 0.003) | 0% | 0.001 (0, 0.006) | 0% | 0.001 (0, 0.004) | 0% |
| 1.1.0.0 | 0.001 (0.001, 0.004) | 4.2% | 0.002 (0.001, 0.008) | 2.78% | 0.001 (0, 0.003) | 0% |
| Control Percent with Pattern | Case Percent with Pattern | Odds Ratio (95% CI) | p-Value | |
|---|---|---|---|---|
| 0.0.0.0 | 97.47% | 61.63% | 23.91 (13.6, 45.38) | <2 × 10−16 |
| 0.2.0.0 | 0.54% | 11.13% | 0.04 (0.01, 0.14) | 1.3 × 10−15 |
| 2.0.0.0 | 0.54% | 8.35% | 0.06 (0.01, 0.19) | 3.3 × 10−11 |
| 2.2.0.0 | 0% | 8.35% | 0 (0, 0.08) | 1.2 × 10−14 |
| 0.16.0.0 | 0.18% | 0.2% | 0.91 (0.01, 71.49) | >0.99 |
| 0.0.16.16 | 0.18% | 0% | Inf (0.02, Inf) | >0.99 |
| 0.0.0.16 | 0% | 0.4% | 0 (0, 4.84) | 0.23 |
| 16.16.0.0 | 0% | 0.2% | 0 (0, 35.47) | 0.48 |
| 16.16.16.16 | 0.18% | 0% | Inf (0.02, Inf) | >0.99 |
| 0.0.16.0 | 0.18% | 0% | Inf (0.02, Inf) | >0.99 |
| 16.0.0.0 | 0.18% | 0.6% | 0.3 (0.01, 3.78) | 0.35 |
| 0.18.0.0 | 0% | 0% | 0 (0, Inf) | >0.99 |
| 16.2.0.0 | 0% | 0% | 0 (0, Inf) | >0.99 |
| 2.16.0.0 | 0% | 0.2% | 0 (0, 35.47) | 0.48 |
| 0.0.2.0 | 0% | 0.2% | 0 (0, 35.47) | 0.48 |
| 0.1.0.0 | 0.18% | 0.6% | 0.3 (0.01, 3.78) | 0.35 |
| 0.2.16.0 | 0% | 0% | 0 (0, Inf) | >0.99 |
| 16.18.16.16 | 0% | 0.2% | 0 (0, 35.47) | 0.48 |
| 18.0.0.0 | 0% | 0% | 0 (0, Inf) | >0.99 |
| 18.18.0.0 | 0% | 0.6% | 0 (0, 2.2) | 0.11 |
| 2.18.0.0 | 0% | 0.2% | 0 (0, 35.47) | 0.48 |
| 2.2.16.16 | 0% | 0.2% | 0 (0, 35.47) | 0.48 |
| 0.0.0.2 | 0.18% | 0% | Inf (0.02, Inf) | >0.99 |
| 0.2.16.16 | 0% | 0% | 0 (0, Inf) | >0.99 |
| 0.4.0.0 | 0% | 0.4% | 0 (0, 4.84) | 0.23 |
| 0.8.0.0 | 0% | 0% | 0 (0, Inf) | >0.99 |
| 1.0.0.0 | 0% | 0.6% | 0 (0, 2.2) | 0.11 |
| 16.18.0.0 | 0% | 0% | 0 (0, Inf) | >0.99 |
| 18.18.16.16 | 0% | 0.2% | 0 (0, 35.47) | 0.48 |
| 0.0.32.32 | 0.18% | 0% | Inf (0.02, Inf) | >0.99 |
| 1.1.0.0 | 0% | 0% | 0 (0, Inf) | >0.99 |
| CL | I2 | CLP | I2 | CP | I2 | CL vs. CLP OR | CL vs. CP OR | CLP vs. CP OR | |
|---|---|---|---|---|---|---|---|---|---|
| 0.0.0.0 | 0.693 (0.642, 0.74) | 0% | 0.45 (0.412, 0.488) | 33.54% | 0.879 (0.281, 0.993) | 93.98% | 2.829 (2.151, 3.722) p = 6.4 × 10−14 | Failed BD Test | Failed BD Test |
| 0.2.0.0 | 0.067 (0.037, 0.119) | 27.35% | 0.102 (0.064, 0.16) | 83.6% | 0.014 (0.005, 0.039) | 0% | 0.489 (0.303, 0.788) p = 0.0041 | 6.194 (1.84, 20.847) p = 0.0017 | 13.134 (4.07, 42.384) p = 9.3 × 10−8 |
| 0.0.16.16 | 0.012 (0.004, 0.034) | 0% | 0.006 (0.003, 0.014) | 0% | 0.028 (0.006, 0.116) | 37.12% | Failed BD Test | Failed BD Test | Failed BD Test |
| 0.1.0.0 | 0.025 (0.011, 0.059) | 7.37% | 0.004 (0.002, 0.011) | 0% | 0.004 (0.001, 0.029) | 0% | 8.528 (1.129, 64.421) p = 0.026 | Failed BD Test | Failed BD Test |
| 0.16.0.0 | 0.013 (0.005, 0.034) | 0% | 0.02 (0.012, 0.031) | 0% | 0.006 (0.001, 0.028) | 0% | 0.337 (0.074, 1.545) p = 0.24 | Failed BD Test | 4.477 (0.57, 35.156) p = 0.22 |
| 16.2.0.0 | 0.012 (0.004, 0.034) | 0% | 0.008 (0.004, 0.016) | 0% | 0.004 (0.001, 0.029) | 0% | Failed BD Test | Failed BD Test | Failed BD Test |
| 2.0.0.0 | 0.067 (0.029, 0.146) | 61.14% | 0.093 (0.059, 0.144) | 80.34% | 0.014 (0.005, 0.039) | 0% | Failed BD Test | 4.48 (1.321, 15.194) p = 0.016 | 9.221 (2.832, 30.029) p = 2.1 × 10−5 |
| 2.2.0.0 | 0.037 (0.011, 0.111) | 61.61% | 0.081 (0.05, 0.127) | 72.74% | 0.019 (0.008, 0.045) | 0% | 0.407 (0.189, 0.879) p = 0.029 | 1.239 (0.402, 3.823) p = 0.93 | 3.147 (1.227, 8.072) p = 0.02 |
| 0.0.0.16 | 0.021 (0.009, 0.049) | 0% | 0.006 (0.003, 0.014) | 0% | 0.023 (0.01, 0.052) | 0% | 13.304 (1.174, 150.774) p = 0.045 | 0.604 (0.161, 2.264) p = 0.68 | Failed BD Test |
| 0.16.16.16 | 0.013 (0.005, 0.036) | 0% | 0.006 (0.003, 0.013) | 0% | 0.004 (0.001, 0.029) | 0% | Failed BD Test | Failed BD Test | Failed BD Test |
| 16.0.0.0 | 0.012 (0.004, 0.036) | 0% | 0.012 (0.007, 0.022) | 0% | 0.01 (0.003, 0.033) | 0% | Failed BD Test | Failed BD Test | 1.206 (0.24, 6.07) p = 0.82 |
| 16.16.0.0 | 0.012 (0.004, 0.036) | 0% | 0.014 (0.008, 0.024) | 0% | 0.01 (0.003, 0.033) | 0% | Failed BD Test | Failed BD Test | 1.164 (0.23, 5.903) p = 0.86 |
| 16.18.16.16 | 0.012 (0.004, 0.036) | 0% | 0.007 (0.003, 0.015) | 0% | 0.004 (0.001, 0.029) | 0% | Failed BD Test | Failed BD Test | Failed BD Test |
| 0.0.16.0 | 0.012 (0.004, 0.036) | 0% | 0.006 (0.002, 0.013) | 0% | 0.023 (0.01, 0.052) | 0% | Failed BD Test | Failed BD Test | Failed BD Test |
| 0.18.0.0 | 0.012 (0.004, 0.036) | 0% | 0.011 (0.006, 0.02) | 0% | 0.004 (0.001, 0.029) | 0% | Failed BD Test | Failed BD Test | Failed BD Test |
| 16.16.16.16 | 0.012 (0.004, 0.036) | 0% | 0.006 (0.002, 0.013) | 0% | 0.014 (0.005, 0.039) | 0% | Failed BD Test | Failed BD Test | Failed BD Test |
| 2.2.16.16 | 0.012 (0.004, 0.036) | 0% | 0.007 (0.003, 0.014) | 0% | 0.004 (0.001, 0.029) | 0% | Failed BD Test | Failed BD Test | Failed BD Test |
| 2.16.0.0 | 0.012 (0.004, 0.036) | 0% | 0.008 (0.004, 0.018) | 0% | 0.004 (0.001, 0.029) | 0% | Failed BD Test | Failed BD Test | Failed BD Test |
| 1.0.0.0 | 0.012 (0.004, 0.036) | 0% | 0.009 (0.005, 0.019) | 0% | 0.004 (0.001, 0.029) | 0% | Failed BD Test | Failed BD Test | Failed BD Test |
| 3.0.0.0 | 0.012 (0.004, 0.036) | 0% | 0.006 (0.002, 0.014) | 0% | 0.004 (0.001, 0.029) | 0% | Failed BD Test | Failed BD Test | Failed BD Test |
| 18.18.0.0 | 0.012 (0.004, 0.036) | 0% | 0.014 (0.008, 0.024) | 0% | 0.004 (0.001, 0.029) | 0% | Failed BD Test | Failed BD Test | Failed BD Test |
| 2.18.0.0 | 0.012 (0.004, 0.036) | 0% | 0.009 (0.005, 0.018) | 0% | 0.004 (0.001, 0.029) | 0% | Failed BD Test | Failed BD Test | Failed BD Test |
| 18.18.16.16 | 0.012 (0.004, 0.036) | 0% | 0.01 (0.005, 0.02) | 0% | 0.004 (0.001, 0.029) | 0% | Failed BD Test | Failed BD Test | Failed BD Test |
| 0.0.2.0 | 0.012 (0.004, 0.036) | 0% | 0.006 (0.003, 0.013) | 0% | 0.01 (0.003, 0.033) | 0% | Failed BD Test | Failed BD Test | 0.125 (0.009, 1.821) p = 0.32 |
| 18.2.0.0 | 0.012 (0.004, 0.036) | 0% | 0.009 (0.004, 0.019) | 0% | 0.004 (0.001, 0.029) | 0% | Failed BD Test | Failed BD Test | Failed BD Test |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Howe, B.J.; Pendleton, C.; Withanage, M.H.H.; Childs, C.A.; Zeng, E.; van Wijk, A.; Hermus, R.; Padilla, C.; Hecht, J.T.; Poletta, F.A.; et al. Tooth Agenesis Patterns in Orofacial Clefting Using Tooth Agenesis Code: A Meta-Analysis. Dent. J. 2022, 10, 128. https://doi.org/10.3390/dj10070128
Howe BJ, Pendleton C, Withanage MHH, Childs CA, Zeng E, van Wijk A, Hermus R, Padilla C, Hecht JT, Poletta FA, et al. Tooth Agenesis Patterns in Orofacial Clefting Using Tooth Agenesis Code: A Meta-Analysis. Dentistry Journal. 2022; 10(7):128. https://doi.org/10.3390/dj10070128
Chicago/Turabian StyleHowe, Brian J., Chandler Pendleton, Miyuraj Harishchandra Hikkaduwa Withanage, Christopher A. Childs, Erliang Zeng, Arjen van Wijk, Ruurd Hermus, Carmencita Padilla, Jacqueline T. Hecht, Fernando A. Poletta, and et al. 2022. "Tooth Agenesis Patterns in Orofacial Clefting Using Tooth Agenesis Code: A Meta-Analysis" Dentistry Journal 10, no. 7: 128. https://doi.org/10.3390/dj10070128
APA StyleHowe, B. J., Pendleton, C., Withanage, M. H. H., Childs, C. A., Zeng, E., van Wijk, A., Hermus, R., Padilla, C., Hecht, J. T., Poletta, F. A., Orioli, I. M., Buxó-Martínez, C. J., Deleyiannis, F., Vieira, A. R., Butali, A., Valencia-Ramirez, C., Restrepo Muñeton, C., Wehby, G. L., Weinberg, S. M., ... Xie, X.-J. (2022). Tooth Agenesis Patterns in Orofacial Clefting Using Tooth Agenesis Code: A Meta-Analysis. Dentistry Journal, 10(7), 128. https://doi.org/10.3390/dj10070128