Interventions to Improve the Oral Hygiene of Individuals with Alzheimer’s Disease: A Systematic Review
Abstract
:1. Introduction
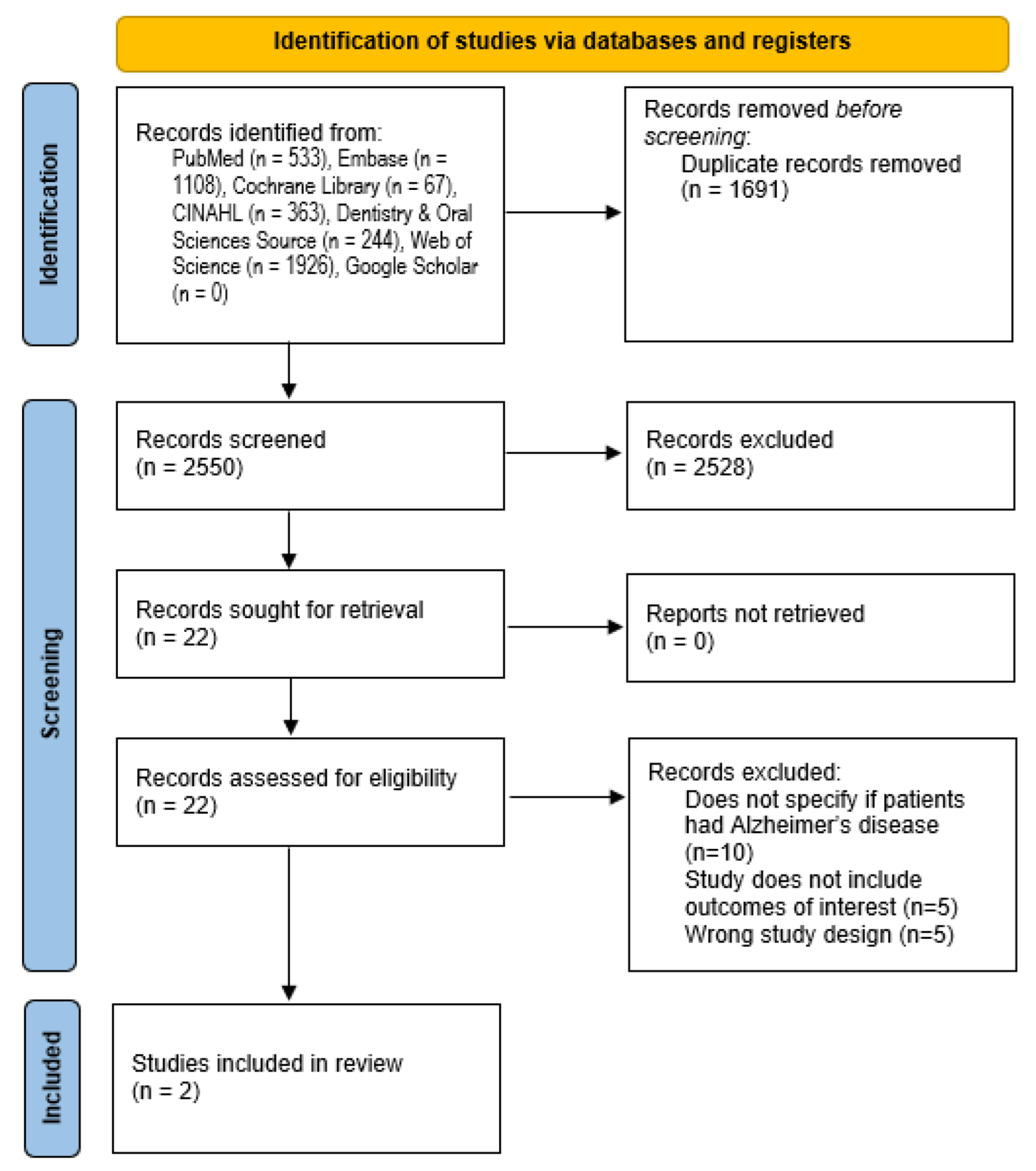
2. Materials and Methods
2.1. Study Inclusion and Exclusion Criteria
2.2. Data Sources
2.3. Search Strategies and Screening
2.4. Data Extraction
2.5. Quality Assessment
2.6. Data Synthesis
2.7. Ethical Considerations
3. Results
3.1. Study Characteristics
3.2. Results of the Plaque Index
3.3. Secondary Outcomes of Interest
3.4. Study Quality
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Holtzman, D.M.; Morris, J.C.; Goate, A.M. Alzheimer’s disease: The challenge of the second century. Sci. Transl. Med. 2011, 3, 77sr1. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization. The Top 10 Causes of Death. 2020. Available online: https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death (accessed on 26 June 2021).
- GBD 2016 Dementia Collaborators. Global, regional, and national burden of Alzheimer’s disease and other dementias, 1990-2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019, 18, 88–106. [Google Scholar] [CrossRef] [Green Version]
- De-Paula, V.J.; Radanovic, M.; Diniz, B.S.; Forlenza, O.V. Alzheimer’s disease. Subcell Biochem. 2012, 65, 329–352. [Google Scholar] [CrossRef] [PubMed]
- Gao, S.S.; Chu, C.H.; Young, F.Y.F. Oral Health and Care for Elderly People with Alzheimer’s Disease. Int. J. Environ. Res. Public Health 2020, 17, 5713. [Google Scholar] [CrossRef]
- Gao, S.S.; Chen, K.J.; Duangthip, D.; Lo, E.C.M.; Chu, C.H. The Oral Health Status of Chinese Elderly People with and without Dementia: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2020, 17, 1913. [Google Scholar] [CrossRef] [Green Version]
- Marchini, L.; Ettinger, R.; Caprio, T.; Jucan, A. Oral health care for patients with Alzheimer’s disease: An update. Spec. Care Dent. 2019, 39, 262–273. [Google Scholar] [CrossRef]
- Delwel, S.; Binnekade, T.T.; Perez, R.S.G.M.; Hertogh, C.M.P.M.; Scherder, E.J.A.; Lobbezoo, F. Oral health and orofacial pain in older people with dementia: A systematic review with focus on dental hard tissues. Clin. Oral. Investig. 2017, 21, 17–32. [Google Scholar] [CrossRef] [Green Version]
- Martande, S.; Pradeep, A.R.; Singh, S.P.; Kumari, M.; Suke, D.K.; Raju, A.P.; Naik, S.B.; Singh, P.; Guruprasad, C.N.; Chatterji, A. Periodontal health condition in patients with Alzheimer’s disease. Am. J. Alzheimers Dis. Other Demen. 2014, 29, 498–502. [Google Scholar] [CrossRef]
- Delwel, S.; Binnekade, T.T.; Perez, R.S.G.M.; Hertogh, C.M.P.M.; Scherder, E.J.A.; Lobbezoo, F. Oral hygiene and oral health in older people with dementia: A comprehensive review with focus on oral soft tissues. Clin. Oral. Investig. 2018, 22, 93–108. [Google Scholar] [CrossRef] [Green Version]
- Van der Maarel-Wierink, C.D.; Vanobbergen, J.N.O.; Bronkhorst, E.M.; Schols, J.M.G.A.; de Baat, C. Oral health care and aspiration pneumonia in frail older people: A systematic literature review. Gerodontology 2013, 30, 3–9. [Google Scholar] [CrossRef]
- Stöhr, J.; Barbaresko, J.; Neuenschwander, M.; Schlesinger, S. Bidirectional association between periodontal disease and diabetes mellitus: A systematic review and meta-analysis of cohort studies. Sci. Rep. 2021, 11, 13686. [Google Scholar] [CrossRef] [PubMed]
- Larvin, H.; Kang, J.; Aggarwal, V.R.; Pavitt, S.; Wu, J. Risk of incident cardiovascular disease in people with periodontal disease: A systematic review and meta-analysis. Clin. Exp. Dent. Res. 2021, 7, 109–122. [Google Scholar] [CrossRef] [PubMed]
- Siegel, E.; Cations, M.; Wright, C.; Naganathan, V.; Deutsch, A.; Aerts, L.; Brodaty, H. Interventions to Improve the Oral Health of People with Dementia or Cognitive Impairment: A Review of the Literature. J. Nutr. Health Aging 2017, 21, 874–886. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021, 88, 105906. [Google Scholar] [CrossRef]
- Haddaway, N.R.; Collins, A.M.; Coughlin, D.; Kirk, S. The Role of Google Scholar in Evidence Reviews and Its Applicability to Grey Literature Searching. PLoS ONE 2015, 10, e0138237. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bramer, W.M.; Rethlefsen, M.L.; Kleijnen, J.; Franco, O.H. Optimal database combinations for literature searches in systematic reviews: A prospective exploratory study. Syst. Rev. 2017, 6, 245. [Google Scholar] [CrossRef]
- NHLBI. Study Quality Assessment Tools. Available online: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (accessed on 7 August 2021).
- Ahmed, S.; Uddin, R.; Ziviani, J.; Khan, A. Global Prevalence of Physical Activity, Sedentary Behaviour, and Sleep of Immigrant Children: A Systematic Review. J. Racial Ethn. Health Disparities 2021, 8, 1364–1376. [Google Scholar] [CrossRef]
- Hinds, N.; Angioi, M.; Birn-Jeffery, A.; Twycross-Lewis, R. A systematic review of shoulder injury prevalence, proportion, rate, type, onset, severity, mechanism and risk factors in female artistic gymnasts. Phys. Ther. Sport 2019, 35, 106–115. [Google Scholar] [CrossRef]
- Rolim, T.D.S.; Fabri, G.M.C.; Nitrini, R.; Anghinah, R.; Teixeira, M.J.; De Siqueira, J.T.T.; Cesari, J.A.F.; De Siqueira, S.R.D.T. Evaluation of patients with Alzheimer’s disease before and after dental treatment. Arq. Neuropsiquiatr. 2014, 72, 919–924. [Google Scholar] [CrossRef] [Green Version]
- Zhang, J.; Wang, Z.; Li, Y.; Yu, P.; Cao, X.; Xu, X.; Xu, S.; Li, S.; Huang, G.; Liu, X. Effects of a Caregiver Training Program on Oral Hygiene of Alzheimer’s Patients in Institutional Care. J. Am. Med. Dir. Assoc. 2021, 22, 1429–1434.e1. [Google Scholar] [CrossRef]
- Thwin, K.M.; Zaitsu, T.; Ueno, M.; Kawaguchi, Y. Effects of oral health education in Myanmar preschool children and guardians. J. Investig. Clin. Dent. 2018, 9, e12346. [Google Scholar] [CrossRef] [PubMed]
- Konstantopoulou, K.; Kossioni, A.; Karkazis, H.; Polyzois, G. Implementation and evaluation of an oral health education programme for caregivers in nursing homes. Spec. Care Dent. 2021, 41, 154–163. [Google Scholar] [CrossRef] [PubMed]
- OECD. Health at a Glance 2019: OECD Indicators; OECD: Paris, France, 2019. [Google Scholar] [CrossRef]
- Sabo, K.; Chin, E. Self-care needs and practices for the older adult caregiver: An integrative review. Geriatr. Nur. 2021, 42, 570–581. [Google Scholar] [CrossRef]
- World Health Organization. Supporting Informal Caregivers of People Living with Dementia. Value Health 2015, 24, 1853–1862. [Google Scholar]
- Jockusch, J.; Hopfenmüller, W.; Nitschke, I. Influence of cognitive impairment and dementia on oral health and the utilization of dental services: Findings of the Oral Health, Bite force and Dementia Study (OrBiD). BMC Oral Health 2021, 21, 399. [Google Scholar] [CrossRef]
- Bressan, V.; Visintini, C.; Palese, A. What do family caregivers of people with dementia need? A mixed-method systematic review. Health Soc. Care Community 2020, 28, 1942–1960. [Google Scholar] [CrossRef]
- Zeng, L.; Zong, Q.; Xu, S.; An, F.; Ungvari, G.S.; Bressington, D.T.; Cheung, T.; Qin, M.; Chen, L.; Xiang, Y. Oral health in patients with dementia: A meta-analysis of comparative and observational studies. Int. J. Geriatr. Psychiatry 2021, 36, 467–478. [Google Scholar] [CrossRef]
| Author (Year) | Design | Intervention | Population Description | Setting | Inclusion Criteria | Age—Mean (SD) | Sex | Prior Oral Hygiene Practices |
|---|---|---|---|---|---|---|---|---|
| Zhang J (2021) | Single-blinded prospective cohort study | Caregiver training | Patients with AD and caregivers in nursing homes in the Greater Zhengzhou Area, China | Nursing homes | Patient: resident for at least 3 months No treatment with antibiotics in the previous 6 weeks. No periodontal treatment in the past three months. Ramfjord teeth or neighboring substitutes were present or 1 or 2 Ramfjord teeth or their substitutes had a probing depth >4 mm. Diagnosis of AD by a neurologist from a class A tertiary care hospital. Patients deemed to be incapable of conducting effective oral hygiene Caregiver: all caregivers must have obtained a senior care certificate on senior care-related knowledge and skills | Patients: Control 76.8 (3.65) limited 75.86 (4.89) comprehensive 76.41 (3.82) Caregivers: Control 33.47 (3.95) limited: 33.86 (3.86) comprehensive 34.02 (4.27) | Patients: control: M/F ratio 15/36 limited: M/F ratio 13/36 comprehensive: M/F ratio 11/35 Caregivers: Not specified | Patients: Regular brushing (%) Control 9.80 Limited 8.16 Comprehensive 10.87 No self brushing (%) Control 56.86 Limited 57.14 Comprehensive 54.35 Regular flossing (%) Control 0 Limited 0 Comprehensive 0 Caregivers: Regular brushing (%) Control 100 Limited 100 Comprehensive 100 No self brushing (%) Control 0 Limited 0 Comprehensive 0 Regular flossing (%) Control 11.76 Limited 8.16 Comprehensive 10.87 |
| Rolim T de S et al. (2014) | Pre-post study design | Dental treatment (all patients received oral hygiene instruction) | Patients with mild AD in Brazil | Not specified | Diagnosis of AD according to the NINCDS-ADRDA9, score between 18 and 26 in the Mini Mental State Exam (MMSE), characterizing mild AD10. The diagnosis was performed by a trained neurologist | Not specified | Not specified | Not specified |
| Author (Year) | Intervention/Duration of Intervention | Oral Hygiene Modality | Oral Health Outcomes | Time Points Measured | Intervention Key Results: mean ± SD (Range) |
|---|---|---|---|---|---|
| Zhang J (2021) | A 15-min instruction video on oral hygiene was given to all participants: It explained how dental plaque contributes to the development of periodontal disease and dental caries as well as the modified Bass method with a demonstration One-on-one training (1 h) reinforcement (5–20 min, variable between caregivers):
| Modified Bass toothbrushing method: This method requires the bristles of the toothbrush to be directed toward the gingival sulcus and at a 45- degree angle to the long axis of the tooth. A horizontal back-and-forth a vibratory stroke is made with the tips of the bristles remaining in their original position, followed by a sweep toward the occlusal surface. The process should be repeated 10 times according to the study’s instructions. | Modified Quigley–Hein Plaque Index (PI) Gingival Index (GI) | Baseline, week 2, week 4, and week 6 | PI
Week 2: 3.12 ± 0.76 z Week 4: 3.25 ± 0.64 z Week 6: 3.20 ± 0.68 z
Week 2: 3.09 ± 0.71 z Week 4: 2.96 ± 0.62 *,z Week 6: 3.03 ± 0.59 z
Week 2: 3.14 ± 0.68 z Week 4: 2.76 ± 0.54 *,z Week 6: 2.46 ± 0.52 *,y, z GI
Week 2: 1.66 ± 0.32 z Week 4: 1.59 ± 0.34 z Week 6: 1.64 ± 0.34 z
Week 2: 1.48 ± 0.38 *,z Week 4: 1.43 ± 0.38 *,z Week 6: 1.51 ± 0.39 z
Week 2: 1.53 ± 0.28 *,z Week 4: 1.32 ± 0.23 *,z Week 6: 1.24 ± 0.24 *,y, z * Statistically different from the mean of the control group at the same point. y Statistically different from the mean of the limited instruction group at the same point. z Statistically different from the mean of the previous session in the same group. |
| Rolim T de S et al. (2014) | Oral hygiene instructions were given to all patients, and dental treatments were given as needed:
| Oral hygiene instructions Dental treatments | Plaque index (PI) DMFT, gingival bleeding index, PPD, cementoenamel junction, CAL and OHIP index | Baseline, one and six months | PI [mean ± standard deviation (range)] Initial evaluation 73.57 ± 5.69 (0.0–100.0) After one month 26.21 ± 11.64 * (8.0–50.4) After six months 60.0 ± 31.62 (20.0–100.0) p-value: <0.001 DMFT [mean± standard deviation (range)] Initial evaluation 27.17 ± 5.69 (11–32) After one month 23.44 ± 8.86 * (8.0–50.4) After six months 27.50 ± 7.54 (11–32) p-value: <0.001 OHIP index [mean± standard deviation (range)] Initial evaluation 3.49 ± 6.27 (0.00–23.21) After one month 1.87 ± 4.92 (0.00–20.09) After six months 0.97 ± 3.49 (0.00–13.20) p-value: 0.009 Medium CAL (mm) [mean± standard deviation (range)] Initial evaluation 2.94 ± 1.26 (1.2–5.9) After one month 2.45 ± 1.00 (1.00–4.0) After six months 2.77 ± 1.27 (1.1–4.0) p-value: 0.449 Medium PPD (mm) [mean ± standard deviation (range)] Initial evaluation 1.57 ± 0.69 (0.5–3.4) After one month 2.52 ± 3.34 * (1.0–12.0) After six months 1.55 ± 0.40 (1.0–2.0) p-value: 0.024 * Analysis of repetitive measures—statistically different from the initial and last evaluations |
| Author (Year) | P1 | P2 | P3 | P4 | P5 | P6 | P7 | P8 | P9 | P10 | P11 | P12 | P13 | P14 | Rating |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Zhang J (2021) | Yes | Yes | ND | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | 78.6% |
| Rolim T de S et al. (2014) | Yes | Yes | ND | Yes | No | Yes | Yes | No | Yes | Yes | No | No | No | No | 50.0% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hernández-Vásquez, A.; Barrenechea-Pulache, A.; Aguirre-Ipenza, R.; Comandé, D.; Azañedo, D. Interventions to Improve the Oral Hygiene of Individuals with Alzheimer’s Disease: A Systematic Review. Dent. J. 2022, 10, 92. https://doi.org/10.3390/dj10050092
Hernández-Vásquez A, Barrenechea-Pulache A, Aguirre-Ipenza R, Comandé D, Azañedo D. Interventions to Improve the Oral Hygiene of Individuals with Alzheimer’s Disease: A Systematic Review. Dentistry Journal. 2022; 10(5):92. https://doi.org/10.3390/dj10050092
Chicago/Turabian StyleHernández-Vásquez, Akram, Antonio Barrenechea-Pulache, Rubén Aguirre-Ipenza, Daniel Comandé, and Diego Azañedo. 2022. "Interventions to Improve the Oral Hygiene of Individuals with Alzheimer’s Disease: A Systematic Review" Dentistry Journal 10, no. 5: 92. https://doi.org/10.3390/dj10050092
APA StyleHernández-Vásquez, A., Barrenechea-Pulache, A., Aguirre-Ipenza, R., Comandé, D., & Azañedo, D. (2022). Interventions to Improve the Oral Hygiene of Individuals with Alzheimer’s Disease: A Systematic Review. Dentistry Journal, 10(5), 92. https://doi.org/10.3390/dj10050092






