Stress Concentration of Hybrid Occlusal Splint-Mouthguard during a Simulated Maxillofacial Traumatic Impact: 3D-FEA
Abstract
1. Introduction
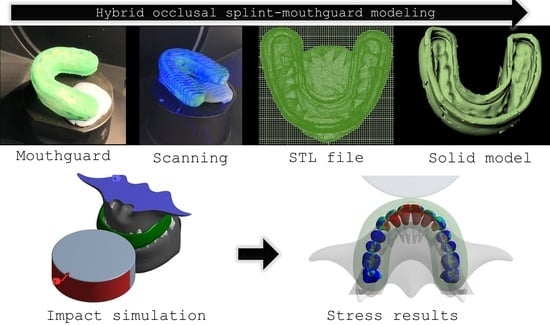
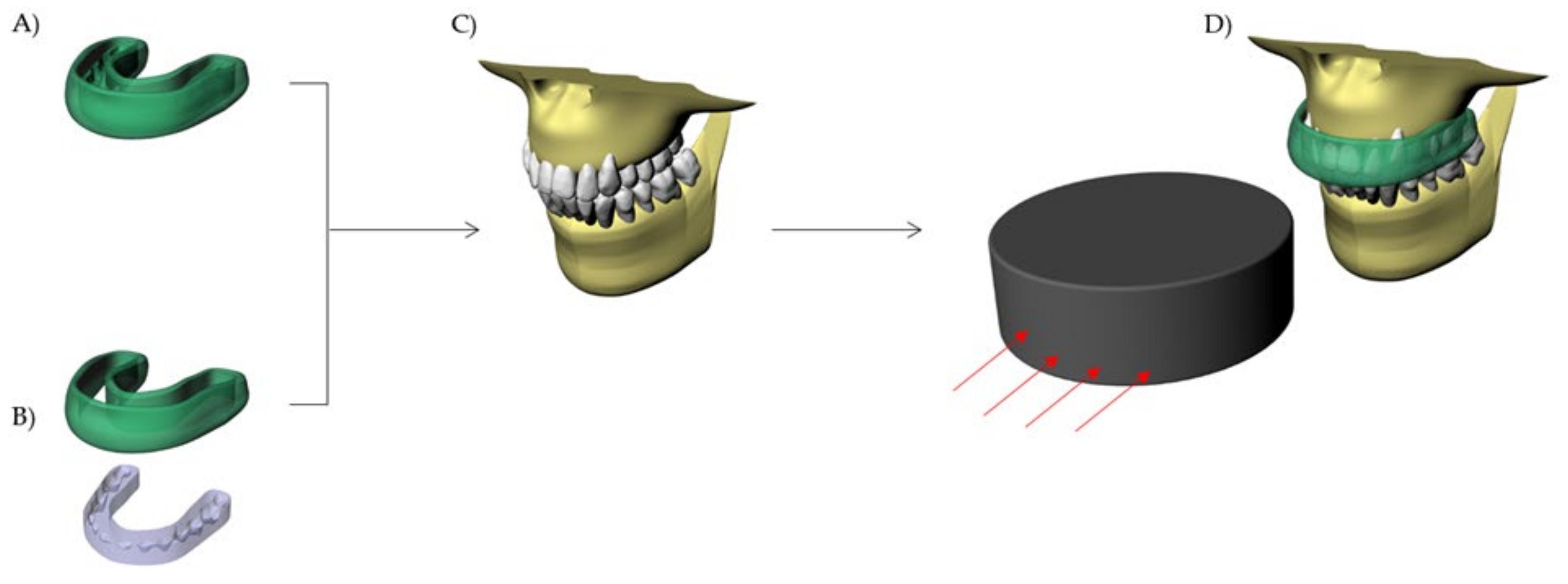
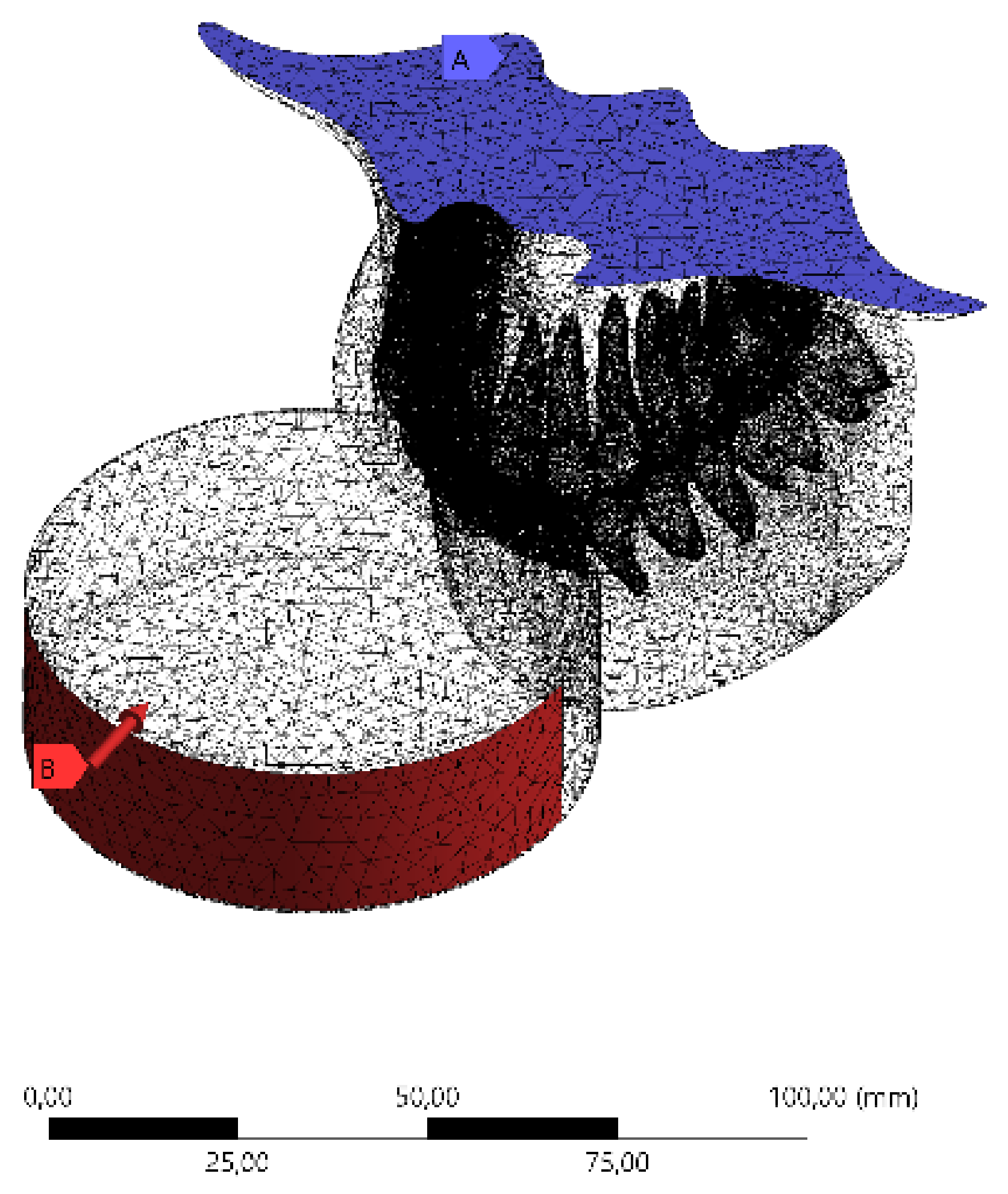
2. Materials and Methods
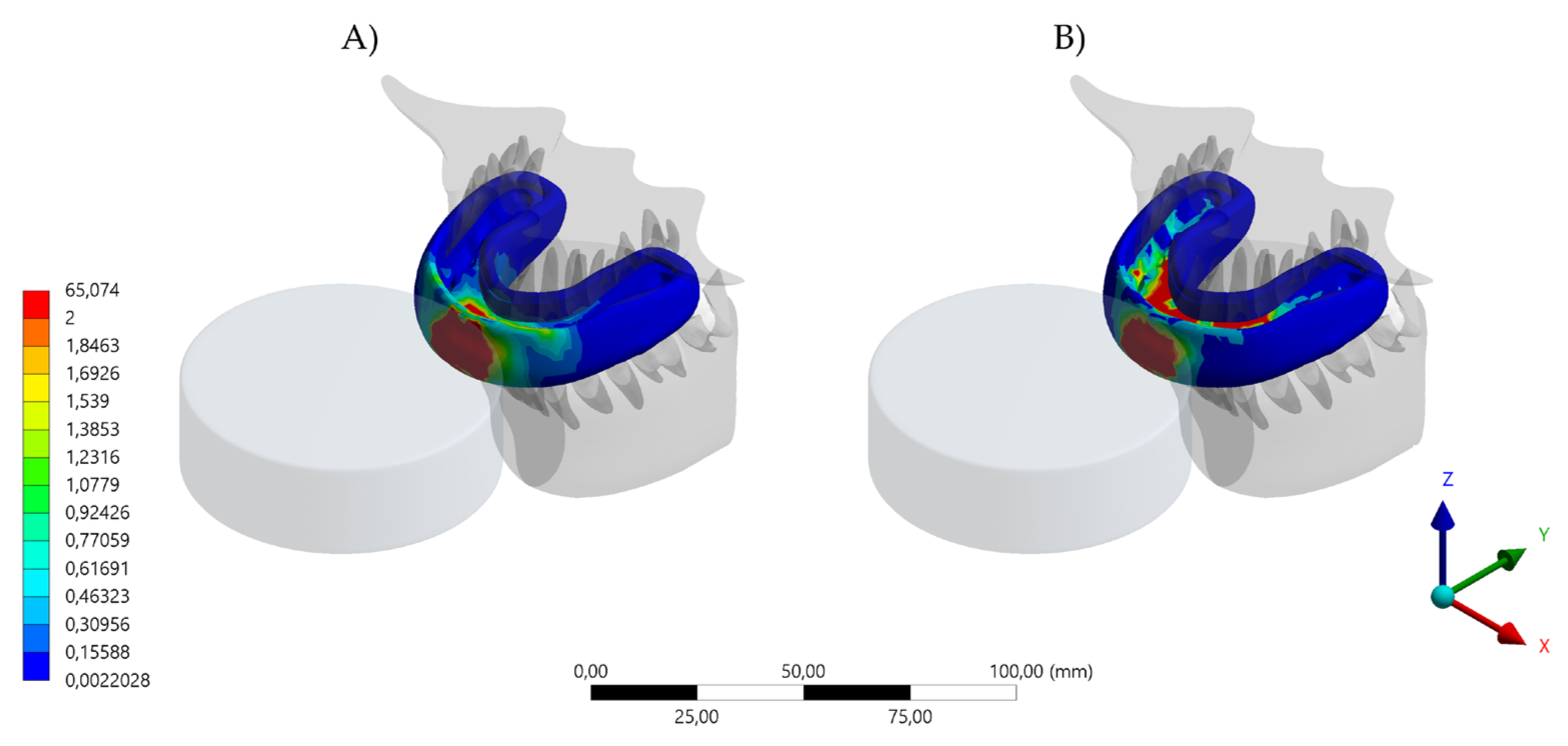
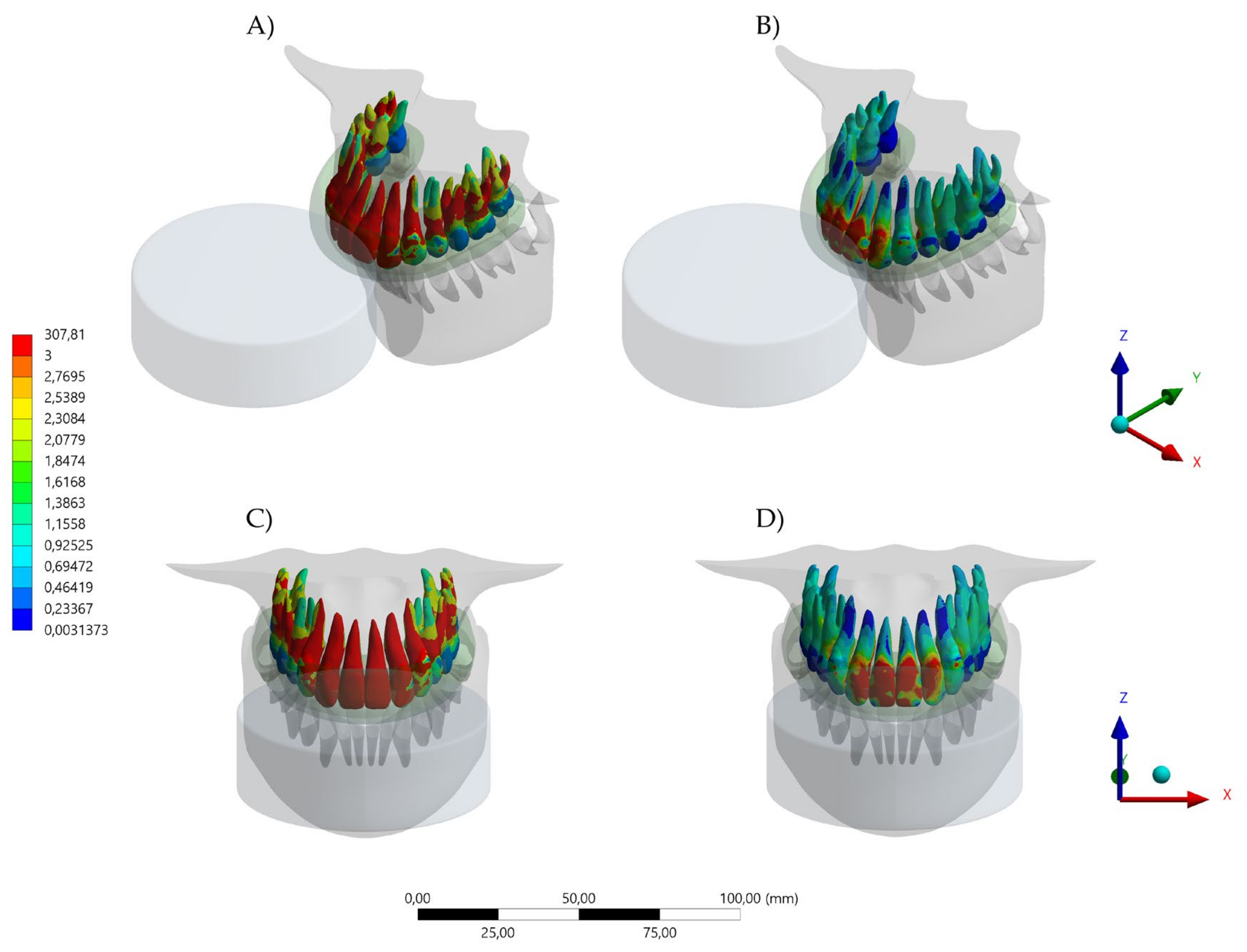
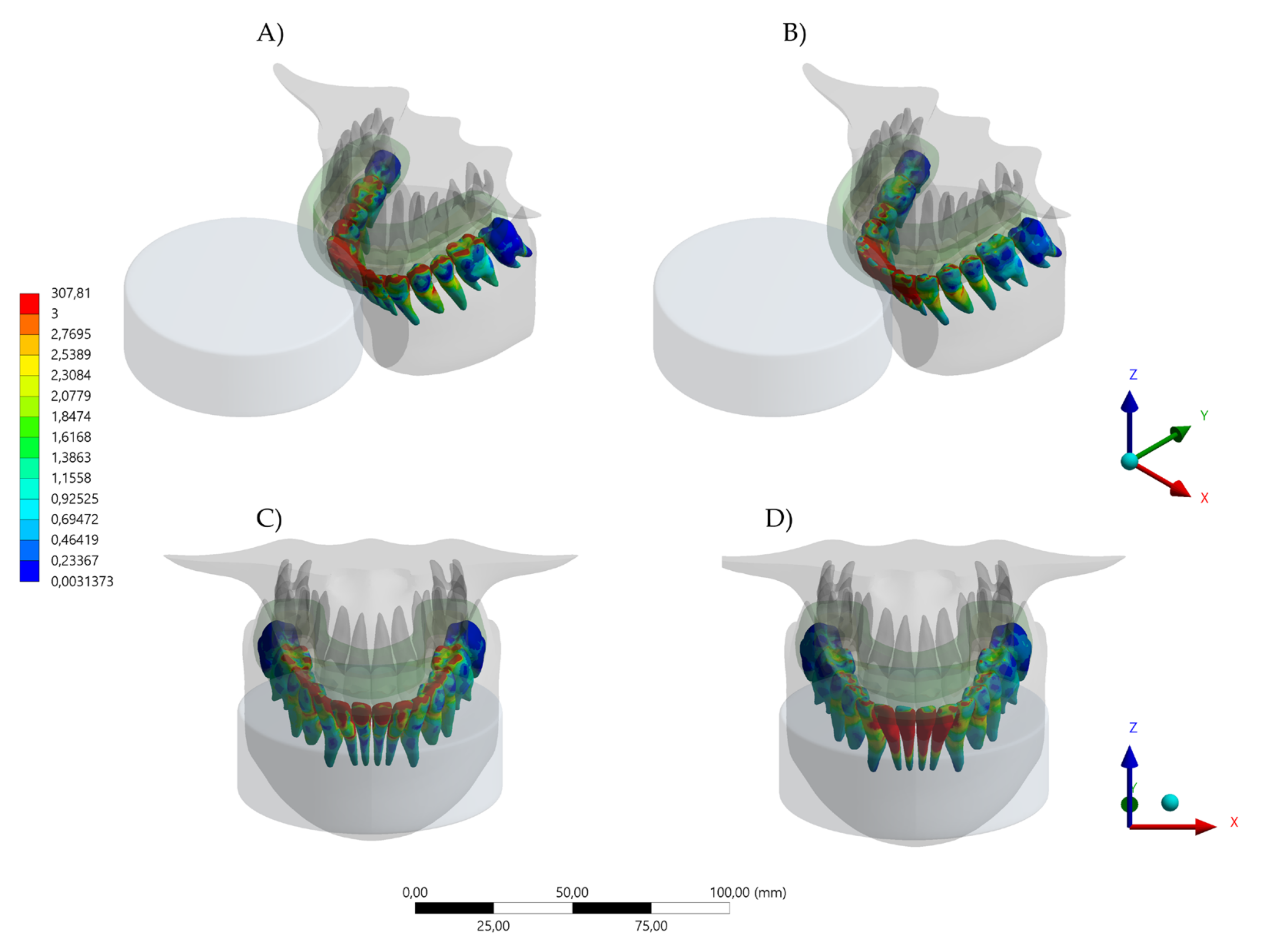
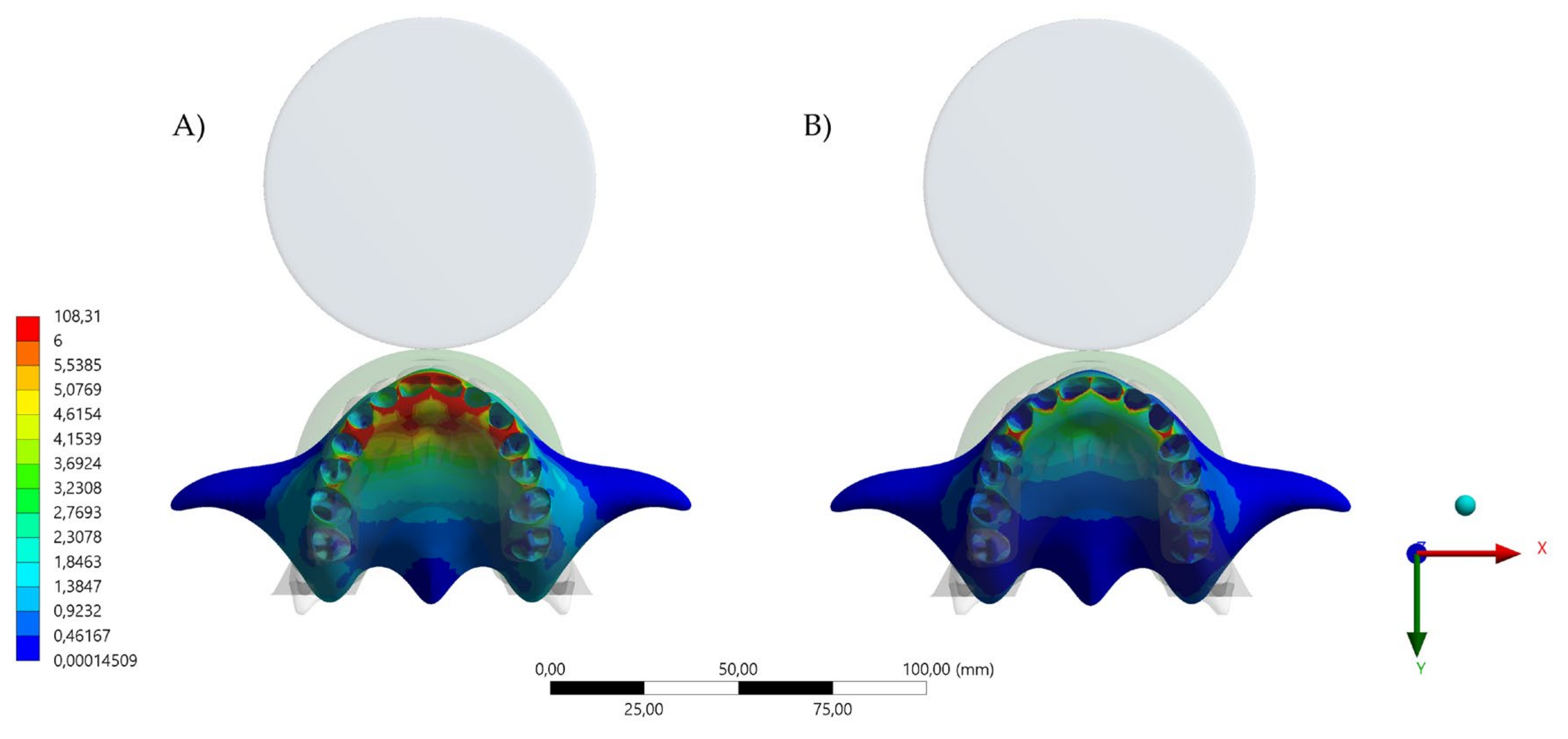
3. Results and Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Miró, A.; Buscà, B.; Aguilera-Castells, J.; Arboix-Alió, J. Acute effects of wearing bite-aligning mouthguards on muscular strength, power, agility and quickness in a trained population: A systematic review. Int. J. Environ. Res. Public Health 2021, 18, 6933. [Google Scholar] [CrossRef]
- Tripodi, D.; Cosi, A.; Fulco, D.; D’Ercole, S. The impact of sport training on oral health in athletes. Dent. J. 2021, 9, 51. [Google Scholar] [CrossRef]
- Tribst, J.P.M.; Dal Piva, A.M.d.O.; Bottino, M.A.; Kleverlaan, C.J.; Koolstra, J.H. Mouthguard use and TMJ injury prevention with different occlusions: A three-dimensional finite element analysis. Dent. Traumatol. 2020, 36, 662–669. [Google Scholar] [CrossRef]
- Tribst, J.P.M.; Dal Piva, A.M.d.O.; Borges, A.L.S.; Bottino, M.A. Simulation of mouthguard use in preventing dental injuries caused by different impacts in sports activities. Sport Sci. Health 2019, 15, 85–90. [Google Scholar] [CrossRef]
- Kalman, L.; Dal Piva, A.M.d.O.; de Queiroz, T.S.; Tribst, J.P.M. Biomechanical Behavior Evaluation of a Novel Hybrid Occlusal Splint-Mouthguard for Contact Sports: 3D-FEA. Dent. J. 2022, 10, 3. [Google Scholar] [CrossRef] [PubMed]
- Afrashtehfar, K.I.; Chung, J. Mouthguard Use May Reduce Dentofacial Injuries in Field Hockey Players: Question: In Field Hockey Players, What Are the Prevalence and Characteristics of Dentofacial Trauma and Mouthguard Use? Evid. Based. Dent. 2017, 18, 48–49. [Google Scholar] [CrossRef] [PubMed]
- Tribst, J.P.M.; de Oliveira Dal Piva, A.M.; Borges, A.L.S.; Bottino, M.A. Influence of custom-made and stock mouthguard thickness on biomechanical response to a simulated impact. Dent. Traumatol. 2018, 34, 429–437. [Google Scholar] [CrossRef] [PubMed]
- Sousa, A.M.; Pinho, A.C.; Messias, A.; Piedade, A.P. Present status in polymeric mouthguards. A future area for additive manufacturing? Polymers 2020, 12, 1490. [Google Scholar] [CrossRef]
- Baena Lopes, M.; Romero Felizardo, K.; Danil Guiraldo, R.; Fancio Sella, K.; Ramos Junior, S.; Gonini Junior, A.; Bittencourt Berger, S. Photoelastic stress analysis of different types of anterior teeth splints. Dent. Traumatol. 2021, 37, 256–263. [Google Scholar] [CrossRef] [PubMed]
- Tribst, J.P.M.; Dal Piva, A.M.d.O.; Ausiello, P.; De Benedictis, A.; Bottino, M.A.; Borges, A.L.S. Biomechanical analysis of a custom-made mouthguard reinforced with different Elastic Modulus laminates during a simulated maxillofacial trauma. Craniomaxillofac. Trauma Reconstr. 2021, 14, 254–260. [Google Scholar] [CrossRef] [PubMed]
- Cicek, T.; Dhamo, B.; Wolvius, E.B.; Wesselink, P.R.; Kragt, L. Effectiveness of the new mandatory mouthguard use and orodental injuries in Dutch field hockey. Phys. Sportsmed. 2021, 49, 455–462. [Google Scholar] [CrossRef] [PubMed]
- Vucic, S.; Drost, R.W.; van Wijk, A.J.; Wesselink, P.R.; Wolvius, E.B. Patterns of orodental injury and mouthguard use in Dutch field hockey. Br. J. Sports Med. 2016, 50, 661–668. [Google Scholar] [CrossRef]
- Wetselaar, P.; Vermaire, E.J.H.; Lobbezoo, F.; Schuller, A.A. The prevalence of awake bruxism and sleep bruxism in the Dutch adult population. J. Oral Rehabil. 2019, 46, 617–623. [Google Scholar] [CrossRef]
- Okeson, J.P. The effects of hard and soft occlusal splints on nocturnal bruxism. J. Am. Dent. Assoc. 1987, 114, 788–791. [Google Scholar] [CrossRef] [PubMed]
- Dalewski, B.; Kamińska, A.; Kiczmer, P.; Węgrzyn, K.; Pałka, Ł.; Janda, K.; Sobolewska, E. Pressure algometry evaluation of two occlusal splint designs in bruxism management-randomized, controlled clinical trial. J. Clin. Med. 2021, 10, 2342. [Google Scholar] [CrossRef] [PubMed]
- Kalman, L. Preliminary investigation of a novel mouthguard. Int. J. Prev. Med. 2018, 9, 60. [Google Scholar] [CrossRef] [PubMed]
- Unkovskiy, A.; Huettig, F.; Kraemer-Fernandez, P.; Spintzyk, S. Multi-Material 3D Printing of a Customized Sports Mouth Guard: Proof-of-Concept Clinical Case. Int. J. Environ. Res. Public Health 2021, 18, 12762. [Google Scholar] [CrossRef] [PubMed]
- Borges, A.L.S.; Dal Piva, A.M.d.O.; Concílio, L.R.d.S.; Paes-Junior, T.J.d.A.; Tribst, J.P.M. Mouthguard use effect on the biomechanical response of an ankylosed maxillary central incisor during a traumatic impact: A 3-dimensional finite element analysis. Life 2020, 10, 294. [Google Scholar] [CrossRef] [PubMed]
- Tiernan, S.; Meagher, A.; O’Sullivan, D.; O’Kelly, E. Finite element simulation of head impacts in mixed martial arts. Comput. Methods Biomech. Biomed. Eng. 2021, 24, 278–288. [Google Scholar] [CrossRef]
- Gialain, I.O.; Coto, N.P.; Driemeier, L.; Noritomi, P.Y.; Dias, R.B.e. A three-dimensional finite element analysis of the sports mouthguard. Dent. Traumatol. 2016, 32, 409–415. [Google Scholar] [CrossRef]
- Toma, M.; Chan-Akeley, R.; Lipari, C.; Kuo, S.-H. Mechanism of coup and contrecoup injuries induced by a knock-out punch. Math. Comput. Appl. 2020, 25, 22. [Google Scholar] [CrossRef]
- Campaner, L.M.; Silveira, M.P.M.; Andrade, G.S.; Borges, A.L.S.; Bottino, M.A.; Dal Piva, A.M.D.O.; Lo Giudice, R.; Ausiello, P.; Tribst, J.P.M. Influence of polymeric restorative materials on the stress distribution in posterior fixed partial dentures: 3D finite element analysis. Polymers 2021, 13, 758. [Google Scholar] [CrossRef] [PubMed]
- Iwasaki, H.; Inaba, R.; Iwata, H. Biting force and physical fitness in athletes. Nihon Eiseigaku Zasshi 1994, 49, 654–659. [Google Scholar] [CrossRef][Green Version]
- Paterson, N.T.; Gorham, D.A.; Matela, R.; Moffatt, J.E.; Greasley, A. A finite element study of the mechanics of sports. Sports Eng. 2004, 7, 182–195. [Google Scholar]
- Kim, H.-N.; Kwon, Y.-B.; Jun, E.-J.; Kim, J.-B. Health-risk behavior-, mental health-, and physical exercise-related risk factors for tooth fractures in Korean adolescents. Int. J. Environ. Res. Public Health 2020, 17, 7815. [Google Scholar] [CrossRef] [PubMed]
- Hayashi, K.; Churei, H.; Tanabe, G.; Togawa, K.; Chowdhury, R.U.; Ueno, T. Improving the wearing rate of mouthguards in the youth rugby category affects the total future mouthguard wearing rate. Dent. J. 2020, 8, 77. [Google Scholar] [CrossRef]
- Takahashi, M.; Bando, Y. Effects on the thickness of single-layer mouthguards with different model positions on the forming table and different sheet frame shapes for the forming device. Dent. Traumatol. 2022, 38, 88–94. [Google Scholar] [CrossRef]
- Veríssimo, C.; Bicalho, A.A.; Soares, P.B.F.; Tantbirojn, D.; Versluis, A.; Soares, C.J. The effect of antagonist tooth contact on the biomechanical response of custom-fitted mouthguards. Dent. Traumatol. 2017, 33, 57–63. [Google Scholar] [CrossRef] [PubMed]
- Mizuhashi, F.; Koide, K.; Watarai, Y. Difference in laminated mouthguard thickness according to the laminate order. Dent. Traumatol. 2021, 37, 497–501. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, M.; Bando, Y. Effect on thickness of a single-layer mouthguard of positional relationship between suction port of the vacuum forming device and the model. Dent. Traumatol. 2021, 37, 502–509. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Avila, M.B.; Gutmann, J.L.; Navas-Barrantes, E.; Leal-Fernández, M.C.; Mejía-Morales, S. Management of external replacement root resorption in a tooth with a history of avulsion. Endod. Pract. Today 2020, 14, 145–150. [Google Scholar]
- Sarao, S.K.; Rattai, J.; Levin, L. Dental trauma among hockey players: Preventive measures, compliance and injury types. J. Can. Dent. Assoc. 2021, 87, l8. [Google Scholar]
- Hayashi, K.; Chowdhury, R.U.; Chowdhury, N.U.; Shrestha, A.; Pradhan, I.; Shahrin, S.; Toyoshima, Y.; Tanabe, G.; Yoshida, Y.; Togawa, K.; et al. Thickness change and deformation of custom-made mouthguards after two years of use by Bangladeshi field hockey players. Dent. Traumatol. 2021, 37, 617–622. [Google Scholar] [CrossRef] [PubMed]
- Gholampour, S.; Gholampour, H.; Khanmohammadi, H. Finite element analysis of occlusal splint therapy in patients with bruxism. BMC Oral Health 2019, 19, 205. [Google Scholar] [CrossRef]
- Gribov, D.; Antonik, M.; Butkov, D.; Stepanov, A.; Antonik, P.; Kharakh, Y.; Pivovarov, A.; Arutyunov, S. Personalized biomechanical analysis of the mandible teeth behavior in the treatment of masticatory muscles parafunction. J. Funct. Biomater. 2021, 12, 23. [Google Scholar] [CrossRef] [PubMed]
- Sliwkanich, L.; Ouanounou, A. Mouthguards in dentistry: Current recommendations for dentists. Dent. Traumatol. 2021, 37, 661–671. [Google Scholar] [CrossRef]
- Stamos, A.; Mills, S.; Malliaropoulos, N.; Cantamessa, S.; Dartevelle, J.-L.; Gündüz, E.; Laubmeier, J.; Hoy, J.; Kakavas, G.; Le Garrec, S.; et al. The European Association for Sports Dentistry, Academy for Sports Dentistry, European College of Sports and Exercise Physicians consensus statement on sports dentistry integration in sports medicine. Dent. Traumatol. 2020, 36, 680–684. [Google Scholar] [CrossRef]
- Messias, A.; Gomes, I.J.; Reis, P.N.B.; Amaro, A.M.; Neto, M.A. The effectiveness of dental protection and the material arrangement in custom-made mouthguards. Appl. Sci. 2021, 11, 9363. [Google Scholar] [CrossRef]
- Kamenskikh, A.; Kuchumov, A.G.; Baradina, I. Modeling the contact interaction of a pair of antagonist teeth through individual protective mouthguards of different geometric configuration. Materials 2021, 14, 7331. [Google Scholar] [CrossRef]


| Material/Structure | Elastic Modulus (MPa) | Poisson Ratio | Density (g/cm3) |
|---|---|---|---|
| Enamel | 84,100 | 0.30 | 2.14 |
| Dentin | 18,600 | 0.30 | 2.97 |
| Bone tissue | 13,700 | 0.30 | 2.00 |
| Polycarbonate | 2200 | 0.30 | 1.20 |
| Ethylene vinyl acetate | 18 | 0.30 | 0.95 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tribst, J.P.M.; Dal Piva, A.M.d.O.; Kalman, L. Stress Concentration of Hybrid Occlusal Splint-Mouthguard during a Simulated Maxillofacial Traumatic Impact: 3D-FEA. Dent. J. 2022, 10, 65. https://doi.org/10.3390/dj10040065
Tribst JPM, Dal Piva AMdO, Kalman L. Stress Concentration of Hybrid Occlusal Splint-Mouthguard during a Simulated Maxillofacial Traumatic Impact: 3D-FEA. Dentistry Journal. 2022; 10(4):65. https://doi.org/10.3390/dj10040065
Chicago/Turabian StyleTribst, João Paulo Mendes, Amanda Maria de Oliveira Dal Piva, and Les Kalman. 2022. "Stress Concentration of Hybrid Occlusal Splint-Mouthguard during a Simulated Maxillofacial Traumatic Impact: 3D-FEA" Dentistry Journal 10, no. 4: 65. https://doi.org/10.3390/dj10040065
APA StyleTribst, J. P. M., Dal Piva, A. M. d. O., & Kalman, L. (2022). Stress Concentration of Hybrid Occlusal Splint-Mouthguard during a Simulated Maxillofacial Traumatic Impact: 3D-FEA. Dentistry Journal, 10(4), 65. https://doi.org/10.3390/dj10040065