Abstract
Leishmaniasis is a complex disease present in a variety of manifestations listed by the World Health Organization (WHO) as one of the neglected diseases with a worse prognosis if not treated. Medicinal inorganic chemistry has provided a variety of drugs based on metal–organic complexes synthesized with different metal centers and organic ligands to fight against a great number of parasite maladies and specifically Leishmaniasis. Taking advantage of the natural properties that many metals present for biotechnological purposes, nanotechnology has offered, in recent years, a new approach consisting on the application of metal nanoparticles to treat a great number of parasitic diseases, as a drug vehicle or as a treatment themselves. The aim of this review is to gather the most widely used metal complexes and metallic nanoparticles and the most recent strategies proposed as antileishmanial agents.
1. Introduction
The concept of neglected diseases (NTDs) englobes all the maladies that cause serious problems to wide populations, but there is not enough investment or research on them. The World Health Organization (WHO) published a list with the main NTDs: Buruli ulcer; Chagas disease; dengue and chikungunya; dracunculiasis; echinococcosis; foodborne trematodiases; human African trypanosomiasis; leishmaniasis; leprosy; lymphatic filariasis; mycetoma, chromoblastomycosis, and other deep mycoses; noma; onchocerciasis; rabies; scabies and other ectoparasitoses; schistosomiasis; soil-transmitted helminthiases; snakebite envenoming; taeniasis/cysticercosis; trachoma; and yaws [1]. The 20 diseases, increased from the initial 17 in the last decade, were chosen because of their adverse impact, relative obscurity, and the availability of tools to combat them [2,3].
According to recent reports from the WHO, leishmaniasis is considered to be one of the seven primary illnesses that affects all continents, and is broadly located in tropical and subtropical poor regions of the New World, but is also present in Europe and Asia by migration [4], affecting more than 90 countries worldwide. An estimated 700,000 to 1 million new cases occur annually, with an annual mortality rate of 95% in visceral leishmaniasis if untreated, being only surpassed by malaria among parasitic diseases [5]. For survival, the Leishmania parasite needs a mammalian reservoir, which leads to anthroponotic cycles in humans or zoonotic cycles in animals like rabbits or dogs. The transmission vectors are mainly dipteral female insects of the genera Phlebotomus in the Old World and Lutzomyia in the New World (Figure 1). The recent migration crisis in the Mediterranean area and Ukraine conflict obligate the relocation of large populations, sometimes in unhealthy conditions, facilitating the proliferation of the infection vectors. These situations, with the blood transfusions from infected patients in host countries, make leishmaniasis a global illness that is spreading out into the Third World.
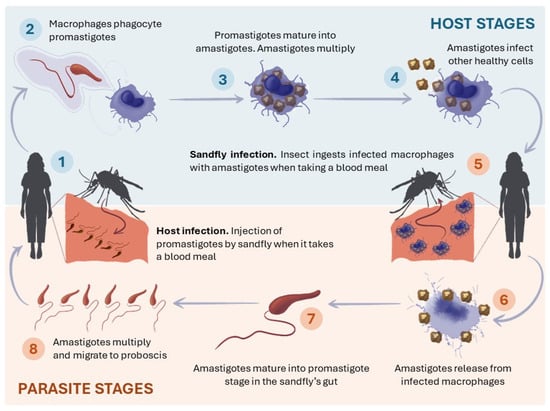
Figure 1.
Leishmania spp. life cycle in humans.
More than 20 Leishmania species cause different forms of leishmaniasis that range in severity from cutaneous lesions to systemic infection [6,7,8], but their manifestation in humans can be classified mainly into three different clinical conditions: visceral, cutaneous, and muco-cutaneous. Visceral leishmaniasis (VL) [9], also known as kala-azar, is the most aggressive and mortal form. It is caused by Leishmania donovani in Asia and in Eastern Africa, where humans are the main pathogen reservoir, and by Leishmania infantum in Latin America and in the Mediterranean area, where VL is a zoonotic disease and dogs and rabbits are the main reservoirs. According to the WHO, almost 13,000 cases of VL occurred in 2020, with an estimated at-risk population of 200 million people [10]. Cutaneous leishmaniasis (CL) [11] is a disfiguring disease, especially for women [12], which produce nodules and ulcers in the skin, and often leaves scars on visible body sites, causing psychological, social, and economic problems, but it does not cause death. It is usually caused by Leishmania mexicana, Leishmania (Viannia) braziliensis, or Leishmania panamensis in the Americas, and Leishmania major or Leishmania tropica in all other countries [13]. Mucocutaneous leishmaniasis (ML) [14], also known as “espundia”, is potentially life threatening and requires treatment. It causes permanent lesions in the mucosa (mouth, nose, or genitals), and occurs years after the onset of cutaneous leishmaniasis. ML is a known risk from Leishmania spp. of the Viannia subgenus, typically found in the Americas (Leishmania (Viannia) braziliensis, Leishmania (Viannia) amazonensis, Leishmania (Viannia) panamensis, and Leishmania (Viannia) guyanensis) [13].
Metals are valuable in multiple research areas due to their wide diversity of properties, promoted by their different electronic configurations, with an extraordinary variety of applications, from industrial to biological disciplines. The unique capabilities of metals can be enhanced by their combination with organic ligands, leading to synergistic effects in the resulting metal complexes, improving their versatility [15,16]. Among their technological uses, their popular use as catalysts can be cited [17,18,19], as can their utility in the material synthesis industry [20] or photochemistry [21]. Medicinal inorganic chemistry can exploit the unique properties of metal ions for the design of new drugs. Recent advances in inorganic chemistry areas make the role of transition metal complexes promising therapeutic compounds [22,23,24]. The advances in inorganic chemistry have made possible the synthesis of a wide series of transition metal complexes with organic ligands of interest, which can be used as therapeutic agents in cancer [25], bacterial [26], or virus [27] infections.
The use of metal complexes in the field of parasitology is developing promising perspectives [28], with transition metal centers like Cu [29,30], Ni [31,32], or Zn [33,34], precious metals like Au [35], Ag [36], Pt, and Pd centers [37], or organometallic cores [38]. The importance of the metal ion and the nature of the organic ligands is critical to understanding the chemistry between the proposed drugs and the parasite environment.
This review includes the use of the most common metal complexes as treatment, alternatives based on biocompatible ligands, and new possibilities based on metallic nanoparticles.
2. Metal Complexes Used as Conventional Therapies against Leishmaniasis
The use of metal complexes as antiparasitic agents is one of the main therapeutic approaches to fight Leishmania spp. infections, with pentavalent antimonials acting as the most effective and low-cost drugs, but they cause strong side effects due to the toxicity of antimony [39,40]. There are also few commercial alternatives without antimony, but their effectivity is not so high as the antimonial established treatments.
2.1. Antimonial Commercial Drugs
The importance of antimony in early medicine is well documented, even being considered to be a general panacea in the 16th century introduced by Paracelsus. The use of the trivalent antimonial, tarter emetic [41], was first reported for the treatment of CL and VL, but later this drug was found to be highly toxic as well as very unstable in tropical climates [40]. Tartar emetic was considered to be an irritating drug, since it exhibited side effects such as cough, chest pain, and severe depression. This led to the discovery of pentavalent antimonials [42], where meglumine antimoniate and sodium stibogluconate stand out among them.
2.1.1. Meglumine Antimoniate
Meglumine antimoniate [43] (Figure 2), commercially known as Glucantime®, is still a first-line drug in the treatment of leishmaniasis in several countries [44,45]. This antimony complex presents high water solubility (>300 mg/mL), and its adsorption can be enhanced for oral administrations with secondary molecules like β-cyclodextrin [46]. It can also be used in combination with liposomes, metallic, and polymeric nanoparticles to improve its biodistribution [47,48]. The mode of action of meglumine antimoniate is still unknown [42], but one of the proposed mechanisms is that Sb(V) would behave as a prodrug, being reduced within the organism into more toxic and active Sb(III), which can enter Leishmania cells primarily [49,50]. Sb(III) can interact with low-molecular thiols, cysteine-containing peptides, and, in particular, thiol-dependent enzymes [51].
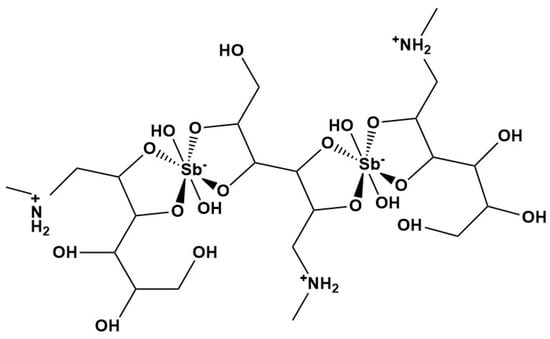
Figure 2.
Meglumine antimoniate or Glucantime® structure.
Despite its commercial use, meglumine antimony causes common adverse effects during treatment, like anorexia, nausea, vomiting, malaise, myalgia, headache, and lethargy. There are many reports of serious side effects in patients treated with Glucantime®, from electrocardiographic changes [52,53] to pancreatic toxicity [54], or the presence of antimony in plasma and skin [55]. Different studies also put in the spotlight the transplacental transference of antimonies from the mother during the gestation process [56], or the problematic nature of pharmacokinetics in children administration [57].
2.1.2. Sodium Stibogluconate
Sodium stibogluconate, or Pentostam®, is also an effective drug in the fight against leishmaniasis. Its ionic nature makes it freely soluble in water (Figure 3), and its mechanism of action is well known since four decades ago [58], focusing on the inhibition of the incorporation of nucleobases into the parasite protein synthesis and blocking its energy metabolism through stibogluconate interactions.
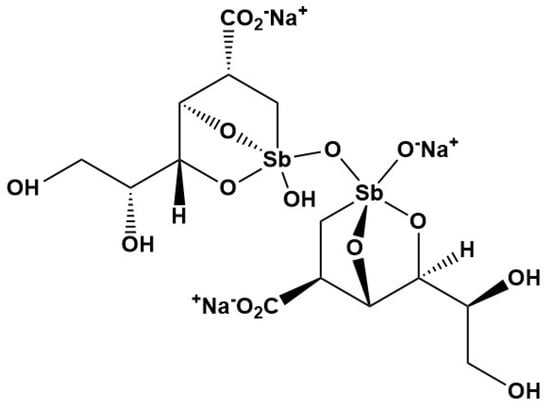
Figure 3.
Sodium stibogluconate or Pentostam® structure.
Despite no serious toxicity being observed even when a ten-fold increase in the daily recommended concentration for sodium stibogluconate was applied, there are few reports where dose-dependent factors promote histological changes in the liver and kidneys [59], and health problems like pancreatitis, nephrotoxicity, and elevation of liver enzymes were also reported [60]. This evidence, joined to the development of drug resistance of Leishmania spp., make it necessary to attempt more efforts to design and test new metal complexes with antileishmanial activity.
Some other antimonial drugs can be mentioned, like trivalent antimonial stibocaptate [61], but their use is less extensive than the first two.
2.2. Other Commercial Drugs against Leishmania spp. and Trypanosoma cruzi
The antiparasitic metal drugs are not limited to the antimonial ones, and other commercial treatments can be mentioned [62], such as organic molecules like amphotericin B [63,64,65], miltefosine [66], or paromomycin [67], as well as combinations of all of them to improve efficacy [68]. Nevertheless, there are not many examples of metal complexes derived from these organic ligands. One approach from Chudzik et al. in 2013 can be mentioned which uses copper complexes of amphotericin-B [69], but its study was focused in the antifungal activity against C. albicans.
On the other hand, benznidazol and nifurtimox are two nitro derivatives commonly used against trypanosoma infections like Chagas disease, a zoonosis malady comparable to leishmaniasis [70,71]. Benznidazole (2-nitro-N-[phenylmethyl]-1H-imidazole-1-acetamide) is a nitroimidazole derivative that showed efficacy against T. cruzi parasites, and different clinical and experimental studies were published using it as a treatment for acute and chronic Chagas disease. Nifurtimox (3-methyl-N-′[(5-nitro-2 furanyl)-methylene]-4-morpholinamine 1,1 dioxide) is a nitrofuran derivative which generates nitroanion radicals by nitroreductases that, in the presence of oxygen, produce free radicals that damage T. cruzi [72]. But once again, their use in combination with metal ions like copper and silver is just at the initial phase, it being worthwhile to mention the work of Cunha da Souza et al. in 2023 [73].
3. Biomimetic Metal Complexes against Leishmaniasis
Due to the high toxicity of antimony [39], there is a need to find novel metal complexes which can substitute the pentavalent antimonials to fight parasite infections, maintaining the advantages of the synergetic effect of the inclusion of metal ions in the structure of the proposed drug, but avoiding the toxicity of heavy metals like antimonies. The variety of metal complexes in the field of parasitology is wide and rich, so this review is focused on recent advances in the derived metal complexes based on biomimetic and well-known commercial drugs against leishmaniasis infections.
3.1. Nucleobase Analogous Active Compounds
Numerous organic ligands with purine or pyridine rings in their structures have been demonstrated to be effective against parasitic infections once they were coordinated with metallic ions.
3.1.1. Azoles
Azoles [74] (Figure 4) represent a broad family of five-membered heterocyclic aromatic compounds whose framework contains from one and up to five nitrogen atom(s), and can also contain at least one S or O atom as a part of the azole conjugated ring (N,S and N,O subclasses of azoles, respectively) [75].
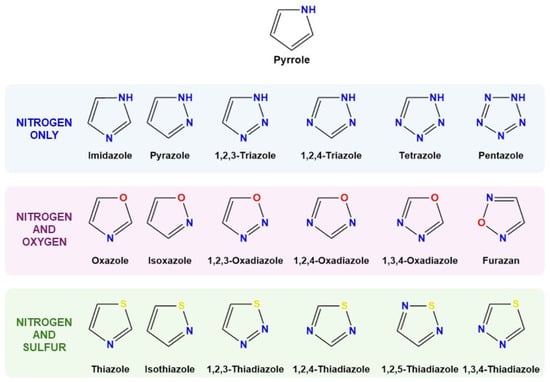
Figure 4.
Chemical structure of pyrrole, the simplest azole, as well as azole rings containing nitrogen only, nitrogen and oxygen, and nitrogen and sulfur. Figure based on reference [74], modified with permission.
Their importance as biological agents has been demonstrated throughout the last decades, with special emphasis on the antibacterial [76] and antifungal [74] effectivity, but their use as antiparasitic agents is also well defined [77,78], even with specificity to fight malaria [79] or amoeba infections [80]. The use of azoles against Leishmania spp. infections has been studied, with a focus on the 14α-demethylase as a distinct target for antileishmanial therapy [81] or for the inhibition of trypanothione reductase [82]. The assays with ketoconazole [83], indazol [84], or chloro-derived azoles such as miconazole, tioconazole, clotrimazole, and their analogs and metal complexes is to be remarked in this context [85].
3.1.2. Triazolopyrimidines
Triazolopyrimidine ligands have been known since early last century [86], but their complexation properties were not studied until 1952 by Birr [87]. Multiple biological applications have been studied for triazolopyrimidine ligands, as well as for their metal complexes, due to their remarkable pharmacology [88,89,90,91]. For the case of 1,2,4-triazolo[1,5-a]pyrimidines ligands [92] (Figure 5A), which have shown the best antiparasitic activity, their structural similarity with purines makes them an optimal model to study the reactivity with different metal ions [93,94,95,96]. Triazolopyrimidines show great versatility as ligands, because of the presence of nitrogen atoms on their skeleton with available electron pairs. The coordination occurs mainly through N3-monodentate or N3,N4-bridging, but there are descriptions of many other bonding routes being possible when the number of exocyclic substituents in the aromatic ring increases. The interaction between metal cations and triazolopyrimidines exhibit a great potential to act as building blocks with enormous versatility, giving rise to multidimensional systems with useful properties, as well as technological and biological properties [97,98,99,100].
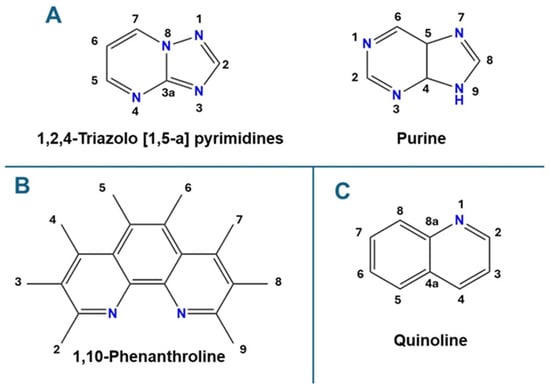
Figure 5.
(A) Basic structure of 1,2,4-triazolo[1,5-a]pyrimidines (left) and purines (right), (B) quinoline structure and substituent numbering, (C) 1,10-phenanthroline structure and substituent numbering.
The 1,2,4-triazolo[1,5-a]pyrimidine family includes a wide variety of derived structures with antileishmanial activity, such as the non-substituted simple structure (tp) [101], the 5,7-dimethyl-1,2,4-triazolo[1,5-a]pyrimidine with two methyl groups (dmtp) [102] and 7-amine-1,2,4-triazolo[1,5-a]pyrimidine (7-atp) with a very reactive amine entity in the structure [103]. To increase the coordination positions, there are also several triazolopyrimidines containing exocyclic oxygen atoms, which spread out the range of metallic centers that can interact with these ligands (i.e., lanthanide ions). Some of the reported oxygenated triazolopyrimidine derivatives are dihydro-5-oxo-[1,2,4]triazolo-[1,5-a]pyrimidine (5HtpO and 7HtpO), whose structures were described by Abul Haj et al. [104], the commercial 4,7-dihydro-5-methyl-7-oxo[1,2,4]-triazolo[1,5-a]pyrimidine (HmtpO) [105], and the most recently reported, 7-oxo-5-phenyl-1,2,4-triazolo[1,5-a]pyrimidine (HftpO) [106]. The efficacy of [1,2,4]-triazolo[1,5-a]pyrimidines against leishmania spp. have been contrasted in different studies [107,108]. Comparing them with reference drug Glucantime ® (meglumine antimoniate), methyl, and amino substituted triazolopyrimidines, the organic molecules slightly increase their efficacy against different leishmania strains like L. infantum or L. braziliensis, but the hydroxy-tryazolopyrimidines are the ones which led to a substantial increase in the leishmanicidal effect, with a selectivity index (SI, proportion between toxicity to the host cells and specificity reducing parasite population) up to 40 times better than the drug reference (it is possible to reach even more than 50 time better effect to trypanosomatid parasites) [106]. These results positioned tryazolopyrimidines as an extraordinary potential alternative to antimonial traditional treatments, with fewer side effects and higher biological activity.
3.1.3. Quinolines
Quinoline is an heterocyclic aromatic nitrogen molecule with a double-ring skeleton containing a benzene ring fused to pyridine at two adjacent carbon atoms (Figure 5B) [109]. The extraordinary variety of potential positions to include substituents (from C2 to C8) make this basic core a very versatile basic unit to build numerous series of biologically active families.
The potential biological applications of quinoline derivatives vary from antibacterial efficacy to antitubercular, antimicrobial, or anticancer applications [110,111,112,113,114], but they also can be used as antiparasitic agents [115] with leishmanicidal efficacy [116,117]. The interest of the scientific community in these compounds increased after 2013 [118], with the work of Bringmann et al. [119], who evaluated 49 different quinolines against promastigote and amastigote forms of L. major, obtaining lower values of IC50 than 10 µM in 20 compounds. The higher SI were obtained with 4′-methylphenyl-pentyl substituted. The halogen ones had great activity against the parasites, but also were very toxic to the J774.1 cells used as a host model in that study. But, in general, modified quinolines show a similar or better efficacy against L. major, positioning them as excellent candidates to further studies and building blocks for metal complexes. From that point, the use of quinolines against Leishmania spp. forms increased during the last decade [120,121].
3.1.4. 1,10-Phenanthrolines
The three-aromatic-ringed 1,10-phenanthroline (Figure 5C) is one of the most versatile and used organic bidentate ligands used to synthesize metal complexes [122]. Its two nitrogen atoms in positions 1 and 10 make it an extraordinary strong chelating agent. Its great solubility in organic solvents makes it a good candidate to interact with metal ions in a solution to coordinate with them as a main ligand or as an auxiliary ligand to complete the coordination sphere. There are recent studies of the influence of this organic ligand and some derivatives, like the 1,10-phenanthroline-5,6-dione of Lane et al. in 2021 [123], where both forms can induce a variety of disorders in a variety of biological systems, like a drastic reduction in cell proliferation, prominent morphological changes, the appearance of electron-dense deposits (mainly consisting of calcium ions) in the parasite’s cytoplasm, as well as triggering perturbations of the mitochondrial membrane and the cisternae of the endoplasmic reticulum of the epimastigote forms of T. cruzi [124].
3.2. Metal Complexes Derived from Nucleobase Analogous Active Compounds
Transition metal complexes represent an attractive platform for the development of anti-parasitic therapeutics, as they present an extraordinary chemical diversity and go by different mechanisms of action, such as the induction of the generation of reactive oxygen species (ROS), enzymatic inhibition, or DNA intercalation [125]. Table 1 summarizes the most significant complexes discussed in this point.

Table 1.
Summary of metal complexes cited in Section 3.2., classified by the organic ligand, metal, and parasite studied, with comparison between the best selectivity index (IC50 for cells/IC50 for parasites, SI) for the extracellular forms of each family.
The family of azole compounds is extraordinarily diverse, and their possible combinations with metals is increasing every day. One of the most useful ligands against leishmania spp. is ketoconazole, an antifungal agent used to treat localized or systemic fungal infections by inhibiting ergosterol synthesis [139]. Its combination with ruthenium, published by Iniguez et al. in 2013, demonstrated that the metal complex improves the leishmanicidal effect of the organic ligand, from 63 SI to 150 SI [126]. The counter-anion salts used in the synthesis play a crucial role in the activity of the ketoconazole ruthenium complexes, with chloride, etilendiamine (en), or bipyridine (bipy) as the most effective ions. Following the ruthenium compounds, clotrimazole ruthenium complexes also exhibit great leishmanicidal power against L. major and T. cruzi [127], and again the use of bipy, en, and acetylacetonate (acac) in the synthesis reaches the best activity.
It is possible to find many examples of metallic complexes with antiparasitic activity with triazolopyrimidines [107,140], especially those with transition metals like copper [141], zinc [128], nickel [129], or ruthenium [130], as well as lanthanide cations [131]. All of these complexes show better IC50 values and higher selectivity indexes than reference drugs against Leishmania spp. and Trypanosoma cruzi. The proposed drugs were assayed in a solution for a cytotoxicity test and for amastigote and promastigote screenings in vitro, but the different solubility of some triazolopyrimidine derivatives make them difficult to manipulate is some cases, especially in that ligands with organic cycles as substituents in positions 5 or 7 [107]. Recently, Martin-Montes et al. [132] reported a novel methodology to deliver the triazolopyrimidine complexes, with the first example of the use of silica nanoparticles as carriers of the ligand and metal complexes in parasitology (Figure 6).
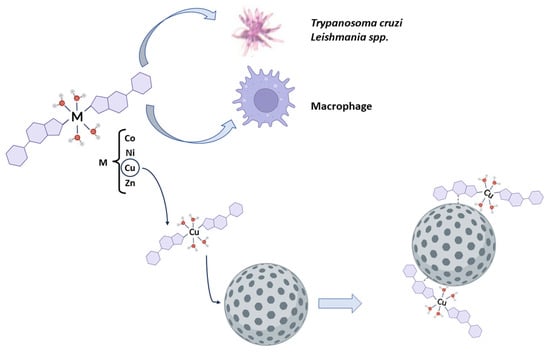
Figure 6.
Schematic representation of the use of triazolopyrimidine metal complexes directly applied to extracellular forms and host cells, as well as those supported on silica nanoparticles to improve their biodistribution. Reproduced with permission from Pharmaceuticals, 2023 [132].
The metallic complexes presented similar acceptable values for IC50 in the promotion of cytotoxicity assays, but they still did not exceed the performance of commercial drugs in some cases, like that of L. braziliensis. Nevertheless, for the triazolopyrimidine ligand, as well as its metal complex [132], the cytotoxicity results were better than those of the reference drugs. Comparing Glucantime and triazolopyrimidine ligands, the concentration needed to consider the organic molecule toxic for the host cells was more than sixty-fold higher than that of the commercial leishmanicidal drug. The results for the antiparasitic activity of the nanomaterials evaluated indicate a great efficacy of the copper complex, with higher values of SI in comparison with free Glucantime, while keeping a similar efficacy range, even though silica nanoparticles were modified with only 20% of the ligand or metal complex, relative to the weight percentage. The release profile shows a complete liberation of the drug in two hours, confirming the complete administration of the complex during the screening experiment.
Despite the increasing studies of quinolines derivatives against Leishmania spp. infections, there are not many examples of quinoline metal complexes against leishmaniasis. The only significant test is the one published by Paloque et al. in 2015 [133], where silver (I) and gold(I) N-heterocyclic carbene–quinoline complexes proved to be promising metallodrugs with selective action against the pathological relevant form of Leishmania spp. From these studies, gold(I) N-heterocyclic carbene-quinoline, and, in particular, a neutral complex, proved to be promising metallodrugs with potent and selective action against the pathologically relevant form of Leishmania infantum, but the standard treatments with amphotericine B or miltefosfine are still more effective. Nevertheless, there is a rich chemistry of antimony (III) hidroxyquinoline complexes with activity against trypanosomatid parasites as an analogous treatment to tri- and pentavalent antimonial standard drugs [142].
The chemistry of 1,10-phenanthroline metal complexes is a well-studied field, mainly with copper ions, where multiple applications are studied, such as the following technological [143] and biological applications: anticancer [144], antibacterial [145], or antifungal [146]. It is also common to observe mixed ligand complexes between one subunit of 1,10-phenanthroline and another biocompatible organic ligand, such as nucleobases [147], quinolines [148], or commercial drugs [149], for example. But, once again, the studies of metal complexes derived from 1,10-phenanthrolines against parasite infections are in low proportion in comparison with other diseases. There are some works about malaria and antiplasmodic activity [150,151] or T. vaginalis [152], but it can be considered to be anecdotic in comparison with anticancer or antibacterial studies. In the last decade, vanadium phenanthroline complexes against Leishmania spp. and Trypanosoma cruzi [153,154], and copper and silver complexes with 1,10-phenanthroline modified ligands published by Oliveira et al. from 2021, are the few examples that can be found in the literature for leishmaniasis [123,134,155]. These compounds have shown significant activity against L. braziliensis, influencing metallopeptidases produced by the parasites and being able to block the interaction process of the parasite with host macrophage cells. Figure 7 shows the morphological changes produced by the use of metal complexes against leishmania extracellular forms [134], playing a critical role in normal parasite population growth and leading to great SI values.
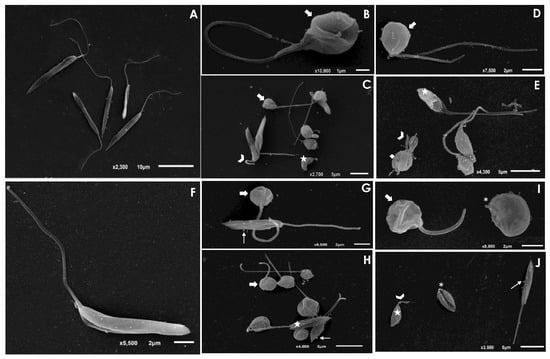
Figure 7.
Scanning electron microscopy (SEM) analysis of L. amazonensis and L. chagasi promastigotes after treatment with the IC50 value of Ag and Cu 1,10-phenentroline complexes. The control cells of L. amazonensis (A) and L. chagasi (F) are presented with an elongated cell body and a long flagellum. The treatment of L. amazonensis with the IC50 value of the Ag complex (B,C) and Cu complex (D,E) showed parasites displaying a rounding of the cell body (arrows), cell shrinkage (stars), and a shortening of the flagellum (arrowheads). In addition, treatment with the Cu complex led to a discontinuity on the cell surface (diamond). L. chagasi treated with the Ag complex (G,H) and Cu compound (I,J) also promoted rounding the in cell body (thick arrows) and cell shrinkage (stars), in addition to the formation of blebs in the membrane (thin arrows). L. chagasi treated with the Cu complex presented shortening (arrowhead) or loss (asterisks) of the flagellum. Reproduced with permission from [134].
3.3. Commercial Drug Metal Complexes
One of the trends in the development of new metal complexes with leishmanicidal activity is to use accepted drugs for other treatments and derivatize them to metallic complexes to test against the parasite infection.
The most extended family of drug employed against leishmaniasis are the analgesic and anti-inflamatory compounds. Ni(II), Mn(II), and Pd(II) ibuprofen complexes were tested against Leishmania amazonensis [135]. Mn(II), Ni(II), and Co(II) diclofenac complexes were tested against the following three different strains of Leishmania spp., Leishmania infantum, Leishmania braziliensis, and Leishmania donovani, to study the three clinical forms of leishmaniasis [136]. In both cases, the efficacy and specificity increased due to the synergetic effect of the metal ion. There are also some studies with paracetamol and aspirin metal complexes, but which only focused on antibacterial activity [156].
Several drugs for hyperuricemia and gout were tested against parasitic infections. Allopurinol [157] and colchicine [158,159,160] are two of the gout-tested recommended drugs used against Leishmania spp. infections, but no metal complex was tested to date. Other examples of active drug complexes tested as antileishmanial agents are anticancer miltefosine in combination with gold or vanadium complexes [137,161]; vomit-inducer bumetanide with a Zn synergetic effect against Leishmania braziliensis [138]; or antidiabetic metformin, lowering the blood sugar level to the minimum physiological limit and destroying parasites [162].
3.4. Mechanisms of Action between Metal Complexes and Parasites
The use of metal complexes derived from leishmanicidal drugs led to a decrease in the infections through a synergetic effect between the organic ligands and metal centers. There are different mechanisms of action proposed for the interaction between metal complexes and parasite forms, like the following: DNA interaction and damage [163], DNA structure disruption, and replication and transcription inhibition, or by the generation of reactive oxygen species (ROS) that cause DNA strands to break; inhibition of metalloenzymes, such as ribonucleotide reductase or topoisomerase, or proteases involved in the parasite’s life cycle, can disrupt protein processing and the metabolism [164]; membrane disruption [165] through ROS generated by metallic complexes that can initiate lipid peroxidation, compromising the integrity of cellular membranes or by directly binding to membrane components, disrupting the membrane’s structure and function, leading to cell lysis; or metabolic disruption [166] by the inhibition of key metabolic pathways targeting essential enzymes for the parasite’s energy production and biosynthesis due to metallic complexes that can impair mitochondrial function, ATP production disruption, and apoptosis induction.
ROS play a critical role in most of the mechanisms proposed by diverse authors to explain the benefits of using metal complexes as alternative leishmanicidal drugs. Many metallic complexes can undergo redox cycling, producing ROS that damage cellular components like lipids, proteins, and DNA. In addition, metal complexes that participate in Fenton-like reactions can catalyze the production of hydroxyl radicals, leading to oxidative stress.
4. Alternative Use of Metals: Metallic Nanoparticles as Antiparasitic Agents
In recent years, nanotechnology approaches have arisen as a promising solution to traditional therapies’ limitations against parasites, namely reduced efficacy and poor penetration (which is especially worrying in the case of intracellular parasites), leading to the administration of higher doses that provoke severe and undesired side-effects. Additional noteworthy improvements that nanoparticle (NP)-based strategies against parasitic infections bring are higher biocompatibility and membrane penetration, the possibility to selectively target parasites (protecting from side toxicity to the host), an improvement in drug delivery and drug stability, or absence of drug resistance (which is a remarkable limitation for many traditional therapies). Although the specific mechanism of action depends on the precise parasite species and on the type of nanoparticle used, general modes of operation are interaction with biological membranes or some parasite’s proteins, impact on the proliferation of the microorganism, or the production of reactive oxygen species (ROS). The generation of ROS, which can be triggered by the excitation of metallic nanoparticles with the appropriate wavelength (visible and infrared), results in the release of free electrons able to hinder cells’ homeostasis and osmotic potential [167,168,169,170].
Moreover, nanoparticle use in the fight against parasitic infections is not only limited to treatment, but also enables the prevention, control, and detection of several infections [171]. Regarding the latter, fluorescent, magnetic, and metal NP (especially gold and silver NP [172]) are promising tools, owing to the possibility of conjugation with different probes or signal enhancers, improving the detection process [173].
One of the main advantages that nanomaterials bring is their versatility in numerous aspects such as application fields, morphologies, compositions, or synthetic procedures. In this context, it is remarkable to highlight the current trend in developing metal nanoparticles for antiparasitic purposes by green methods using natural resources. Examples of natural products used for the green synthesis of nanoparticle-based materials with antiparasitic features are fig, olive [174,175], ginger [176], curcumin [177,178], or onion [179]. Some of the most remarkable advantages that green synthesis pose compared to traditional procedures are cheap precursors, waste conversion into valuable matter, environmental care, and non-toxic products.
Despite the great variety of metallic nanoparticles that can be synthesized, the most numerous research articles found in the literature for antiparasitic purposes are mainly silver and gold, followed by metallic oxides, which could be attributed to their efficacy [180] (Figure 8). Therefore, some of the most outstanding results using these nanoparticles will be reviewed as follows.
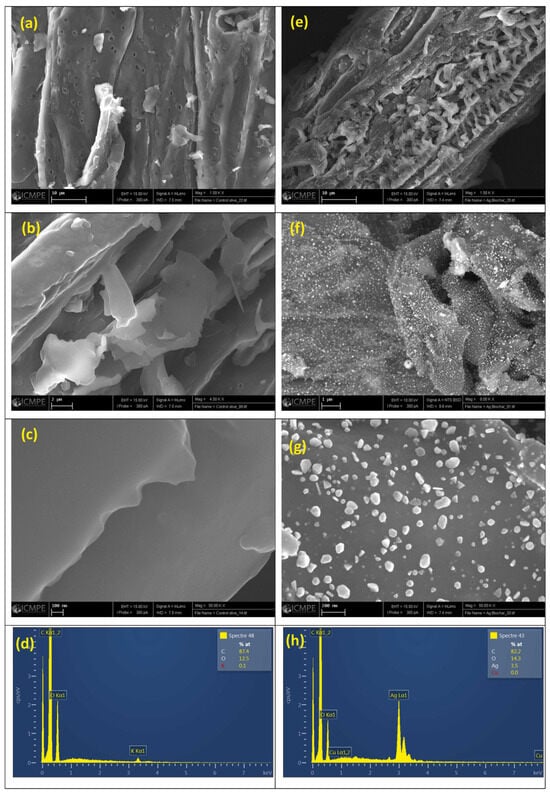
Figure 8.
Example of SEM (a–c,e–g) and EDX (d,h) analyses of Biochar (a–d) and Biochar@Ag (e–h) nanoparticles at various magnification. Reproduced with permission from [180].
4.1. Silver Nanoparticles
Silver nanoparticles (AgNPs) have been found to present several properties which make them excellent candidates for biomedical purposes. AgNPs present low toxicity, an anti-inflammatory effect, antimicrobial activity against numerous microorganisms like bacteria, fungi, protozoa, and some types of viruses, accumulation in tissues, and production of ROS [181]. Despite the fact that AgNPs can be synthesized using a great number of physical (laser ablation, irradiation, evaporation…) or chemical (chemical reduction, sol–gel, pyrolysis…) procedures, bio-based methodologies are currently widespread [182]. The use of biological reactants is crucial due to their capacity to reduce and stabilize Ag ions together with their proven therapeutic effectiveness. Examples of green synthesis methods are proposed by Almayouf and coworkers (using fig and olive extracts as phenolic and flavonoid sources in addition to their chemical reductive capacity) [174], Mohammadi et al. (used ginger rhizome extract) [176], or Javed and colleagues (used an aqueous extract of Mentha Arvensis) [167].
The action of metal nanoparticles is not limited to the activity of the noble metal itself, but can also be used to improve certain properties of other active compounds or to provide synergistic effects to other elements. For example, Badirzadeh et al. designed curcumin-coated silver nanoparticles to enhance curcumin’s water solubility and bioavailability for the treatment of cutaneous leishmaniasis (CL) [178], while Shakeel et al. synthesized thiolated AgNPs to provide muco-adhesion and muco-permeation to the nanosystem and mannosylated chitosan to enhance the uptake of macrophages [183].
Regarding the application of AgNPs, most research articles focus their work on the treatment of different manifestations of leishmaniasis, but are not limited to this parasite. Different strains of Trypanosoma (cruzi [184] or brucei [185,186] respectively) or Toxoplasma gondii [181] are examples of alternative parasites to be approached using AgNPs.
4.2. Gold Nanoparticles
Gold nanoparticles (AuNPs) are widely used for a variety of applications in the healthcare industry such as imaging, targeting, drug delivery, or treatment [187,188]. Additionally, they have shown interesting features for parasite treatment.
Regarding gold nanoparticles synthesis, they can be obtained using both chemical methods and green procedures as well. For example, Want et al. propose gold nanoparticle synthesis by microwave-assisted heating in the presence of a reductant [189], while Raj et al. synthesized chrysin (a non-toxic flavonoid with therapeutic properties) conjugated gold nanoparticles [190]. It is remarkable to highlight the potential of gold nanoparticles as carriers of relevant bioactive molecules able to perform a variety of tasks as enzyme substrates (like glutathione [185]) or inhibitors (as apoferritin [186]).
Gold nanoparticles have already shown significant activity towards both amastigotes and promastigotes, offering a promising alternative against L. donovani, as proven by Muzamil Yaqub et al. [189]. Nevertheless, antileishmanial activity could be improved if gold and silver nanoparticles were combined. Santanu Sasidharan and Prakash Saudagar synthesized 4′,7-dihydroxyflavone modified gold and silver nanoparticles against L. donovani [191]. In a different study, Dayakar Alti et al. obtained gold–silver bimetallic nanoparticles [192]. IC50 values obtained for the bimetallic nanomaterial were an order of magnitude lower than the individual gold nanoparticle designed by Santanu Sasidhara and coworkers (0.03 µg/mL and 0.1226 µg/mL, respectively).
The interest in gold nanoparticles for antiparasitic purposes is not only limited to the development of effective treatments, but can be used in the design of sensitive biosensors for the detection of leishmania. In this regard, gold nanoparticles usually do not have an active role in the recognition event, but are used as support for the biomolecules responsible for the biorecognition process [193] or to improve electron transfer in the case of electrochemical sensors [194].
4.3. Copper Nanoparticles
Copper is a metallic element that also presents interesting features for biomedical purposes like anti-inflammatory, antinociceptive, or antioxidant effects, immune protection, or antimicrobial activity. Therefore, in recent years, taking advantage of the benefits that nanomaterials provide, copper nanoparticles have been explored for health-related applications. Green synthesis procedures have been published based on the use of plant-based raw materials for the synthesis of copper nanoparticles. Caesalpinia Spinosa [47], Lupinus Arcticus [195], or Allium Tuncelianum [179] are examples of vegetable resources described in the literature for such purposes. These eco-friendly procedures have shown to be not only more sustainable, but also to be able to provide high effectivity in their duty; pristine copper nanoparticles, especially when combined with meglumine antimoniate, are able to significantly inhibit the growth rate of L. major [47].
Not only green synthesis procedures have been proposed for the obtention of copper nanoparticles. Welearegay et al. used an advanced gas deposition technique followed by ligand deposition, and the metal nanoparticles synthesized were used for the development of a gas sensor for the detection of cutaneous leishmaniasis. Interestingly, despite gold nanoparticles being the most widely used in sensing films, copper nanoparticles showed better accuracy, sensitivity, and specificity [195].
4.4. Metal Oxide Nanoparticles
4.4.1. Copper Oxide Nanoparticles
A significant advantage that metal oxide nanoparticles have over metallic nanoparticles is that they do not trigger resistance in microorganisms or pathogenic cells. In addition to this, the cost associated with the precursors is much more competitive compared to silver or gold, which are the prevalent metals used for the synthesis of nanoparticles for anti-parasitic purposes. Nevertheless, copper oxide (CuO) nanoparticles must be modified by a ligand coating or sulfidation to be safe for therapeutic use. Few articles have been published describing copper oxide nanoparticles for anti-parasitic purposes, to the best of our knowledge. As an example, Dunia A. Ruda et al. propose the synthesis of copper oxide nanoparticles using the precipitation method as an anti-leishmania agent [196]. Shah Faisal et al. published a green synthesis based on the use of plant-based precursors of multi-purpose copper oxide nanoparticles with high activity against leishmaniasis, observing a high mortality rate of 49.1 and 56.2% inhibition at 400 µg/mL for promastigote and amastigote, respectively [177].
4.4.2. Nickel Oxide Nanoparticles
Nickel oxide (NiO) presents astonishing physico-chemical properties owing to its electronic behavior. It is a p-type semiconductor transition metal oxide with a broad band gap, which provides remarkable ferromagnetic properties and presents thermal and chemical robustness. In addition, nickel oxide also possesses remarkable antibacterial and antifungal properties. To avoid the use of hazardous precursors, green methods are also widely used for the synthesis of nickel oxide nanoparticles. Rhamnus triquetra and olive leaves have been used to obtain nickel oxide nanoparticles for activity against Leishmania spp. (IC50 of 27.32 µg/mL and 37.4 µg/mL for promastigotes and amastigotes, respectively) [197] and the viruses transmitted by Hyalomma dromedarii [175]. Ali Talha Khalil et al. proposed a synthesis using Sageretia thea, which rendered 24.13 µg/mL and 26.74 µg/mL as IC50 values for the promastigote and amastigote cultures of Leishmania tropica [198]. As for other metal-based nanoparticles, nanostructured nickel oxide might also be useful for sensing purposes, in addition to its biomedical application against leishmania. In this regard, Swati Mohan and coworkers developed a sensitive biosensor for visceral leishmaniasis [199].
4.4.3. Zinc Oxide Nanoparticles
Zinc is a biocompatible and biodegradable element recommended for both tissue regeneration and treatment. When combined with oxygen as zinc oxide (ZnO), it is considered to be a safe substance by the US Food and Drug Administration, and has been proven to be an effective antibacterial owing to its capacity to produce ROS and perturb bacterial DNA amplification mechanisms, as well as its capacity to induce lipid membrane oxidation, making these nanoparticles a good alternative to fight against resistant organisms [200,201].
Among zinc oxide nanoparticles, the most outstanding features, in addition to low prize and stability, that make them interesting materials are their wide band gap and photocatalytic behaviors. It is precisely these latter properties which provide one of the main cytotoxic pathways to fight against leishmaniasis; zinc oxide nanoparticles could act as photosensitizers, which are useful in photodynamic therapy against Leishmania, as Akhtar Nadhman et al. established [202].
Different approaches have been found in the literature that use zinc oxide nanoparticles as antiparasitic agents, highlighting nude green-synthesized zinc oxide nanoparticles [203], metal-doped zinc oxide nanoparticles [204], and drug-loaded zinc oxide nanoparticles [200,201,205,206].
In a recent study, Fatemeh Saleh et al. compared the cytotoxic effects of biosynthetic zinc oxide nanoparticles and glucantime towards L. major. Their findings evidence the potential of zinc oxide nanoparticles as antileishmanial agents, since in spite of inducing apoptosis, the toxicity associated with the nanoparticles was lower than glucantime [200]. Nevertheless, in a different study, Samina Nazir et al. evidenced the importance of deeper study about the toxicological behavior of zinc oxide nanoparticles against leishmania, since not only its physiological properties might exert an impact, but also the administration route [207].
Table 2 shows a list of the most significant metal nanoparticle applications for leishmaniasis, from having a direct leishmanicidal effect to sensing and detecting the disease.

Table 2.
Summary of the different kinds of metal nanoparticles’ main applications against leishmaniasis infections.
5. Conclusions
Despite the use of metal complexes in medicine being one of the research areas of bioinorganic discipline of greater interest to the scientific community, there is still a gap to fill in the research for neglected diseases, with a special focus needed on parasitic illnesses such as leishmaniasis. The use of metal complexes derived from biomimetic and biocompatible organic ligands to enhance their applications in cancer, bacterial, or fungal therapies is one of the most prospective for the future, and one with the best perspectives, but contributions to leishmaniasis eradication have experienced a significant slowdown in the last decade.
There are few examples in recent years of the synergetic effects of the combination between leishmanicidal ligands and metal ions, with a significant prevalence of copper complexes due their capacity to generate ROS that can affect multiple vital processes in parasite life cycles. Azole derivatives show the best selectivity indexes in comparison with the rest of the emerging synthetic organic leishmanicidal ligands, while triazolopyrimidine metal complexes are the most versatile due their application to more different types of leishmania strains. The use of novel nanoplatforms as an effective vehicle to transport the metal complexes to the infected organ is a promising new way to explore the possibilities of metal-complex therapy against leishmaniasis. The use of metal elements is not limited to be part of complex structures, due to metallic nanoparticles offering an attractive alternative to metallic compounds with a wide variety of applications, ranging from the direct leishmanicidal effect to the development of biosensors for leishmaniasis or for improving the solubility or biodisponibility of leishmanicidal molecules.
But despite all of the mentioned encouraging results obtained in the last decade, there is still much to be carried out in order to find novel metal complexes with good activity and low toxicity, and an appropriate relationship between their efficacy and their production costs, to develop long term sustainable solutions for the problematic derived from parasitic neglected diseases. Increase funding associated with these types of diseases is an urgent need, in order to reveal the mechanisms of action and the best targets to use the novel metal complexes in the fight against neglected diseases such as leishmaniasis.
Author Contributions
Conceptualization, S.J.-F. and J.M.M.-A.; writing—original draft preparation, S.J.-F. and J.M.M.-A.; writing—review and editing, S.J.-F. and J.M.M.-A. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Neglected Tropical Diseases. Available online: https://www.who.int/news-room/questions-and-answers/item/neglected-tropical-diseases (accessed on 14 April 2024).
- Hopkins, D.R. Neglected Tropical Diseases (NTDs) Slated for Elimination and Eradication. In The Causes and Impacts of Neglected Tropical and Zoonotic Diseases: Opportunities for Integrated Intervention Strategies; National Academies Press: Washington, DC, USA, 2011. [Google Scholar]
- Forgotten People, Forgotten Diseases: The Neglected Tropical Diseases and Their Impact on Global Health and Development, 3rd Edition|Wiley. Available online: https://www.wiley.com/en-es/Forgotten+People%2C+Forgotten+Diseases%3A+The+Neglected+Tropical+Diseases+and+Their+Impact+on+Global+Health+and+Development%2C+3rd+Edition-p-9781683673873 (accessed on 24 March 2024).
- Barrett, M.P.; Croft, S.L. Management of Trypanosomiasis and Leishmaniasis. Br. Med. Bull. 2012, 104, 175–196. [Google Scholar] [CrossRef] [PubMed]
- Mann, S.; Frasca, K.; Scherrer, S.; Henao-Martínez, A.F.; Newman, S.; Ramanan, P.; Suarez, J.A. A Review of Leishmaniasis: Current Knowledge and Future Directions. Curr. Trop. Med. Rep. 2021, 8, 121–132. [Google Scholar] [CrossRef] [PubMed]
- Choi, H.L.; Jain, S.; Postigo, J.A.R.; Borisch, B.; Dagne, D.A. The Global Procurement Landscape of Leishmaniasis Medicines. PLOS Neglected Trop. Dis. 2021, 15, e0009181. [Google Scholar] [CrossRef] [PubMed]
- Benallal, K.E.; Garni, R.; Harrat, Z.; Volf, P.; Dvorak, V. Phlebotomine Sand Flies (Diptera: Psychodidae) of the Maghreb Region: A Systematic Review of Distribution, Morphology, and Role in the Transmission of the Pathogens. PLOS Neglected Trop. Dis. 2022, 16, e0009952. [Google Scholar] [CrossRef] [PubMed]
- Costa-da-Silva, A.C.; Nascimento, D.d.O.; Ferreira, J.R.M.; Guimarães-Pinto, K.; Freire-de-Lima, L.; Morrot, A.; Decote-Ricardo, D.; Filardy, A.A.; Freire-de-Lima, C.G. Immune Responses in Leishmaniasis: An Overview. Trop. Med. Infect. Dis. 2022, 7, 54. [Google Scholar] [CrossRef]
- Scarpini, S.; Dondi, A.; Totaro, C.; Biagi, C.; Melchionda, F.; Zama, D.; Pierantoni, L.; Gennari, M.; Campagna, C.; Prete, A.; et al. Visceral Leishmaniasis: Epidemiology, Diagnosis, and Treatment Regimens in Different Geographical Areas with a Focus on Pediatrics. Microorganisms 2022, 10, 1887. [Google Scholar] [CrossRef] [PubMed]
- Burza, S.; Croft, S.L.; Boelaert, M. Leishmaniasis. Lancet 2018, 392, 951–970. [Google Scholar] [CrossRef] [PubMed]
- de Vries, H.J.C.; Schallig, H.D. Cutaneous Leishmaniasis: A 2022 Updated Narrative Review into Diagnosis and Management Developments. Am. J. Clin. Dermatol. 2022, 23, 823–840. [Google Scholar] [CrossRef] [PubMed]
- Bilgic-Temel, A.; Murrell, D.F.; Uzun, S. Cutaneous Leishmaniasis: A Neglected Disfiguring Disease for Women. Int. J. Women’s Dermatol. 2019, 5, 158–165. [Google Scholar] [CrossRef] [PubMed]
- David, C.V.; Craft, N. Cutaneous and Mucocutaneous Leishmaniasis. Dermatol. Ther. 2009, 22, 491–502. [Google Scholar] [CrossRef]
- Goto, H.; Lindoso, J.A.L. Current Diagnosis and Treatment of Cutaneous and Mucocutaneous Leishmaniasis. Expert Rev. Anti-Infect. Ther. 2010, 8, 419–433. [Google Scholar] [CrossRef] [PubMed]
- Bellotti, D.; Remelli, M. Deferoxamine B: A Natural, Excellent and Versatile Metal Chelator. Molecules 2021, 26, 3255. [Google Scholar] [CrossRef] [PubMed]
- Devi, R.; Singh, K.; Vaidyanathan, S. Synergy in the Energy Transfer between Ligands and EuIII Ions in Molecular Europium Complexes: Single-Component White Light-Emitting Luminogens. J. Mater. Chem. C 2020, 8, 8643–8653. [Google Scholar] [CrossRef]
- Monsur Showkot Hossain, A.; Méndez-Arriaga, J.M.; Gómez-Ruiz, S.; Xie, J.; Gregory, D.H.; Akitsu, T.; Ibragimov, A.B.; Sun, B.; Xia, C. Review on Metal Complexes with 4N-Methyl (Thiosemicarbazone). Polyhedron 2023, 244, 116576. [Google Scholar] [CrossRef]
- Zhang, H.; Qin, X.; Wang, J.; Ma, L.; Chen, T. Metal Complex Catalysts Broaden Bioorthogonal Reactions. Sci. China Chem. 2024, 67, 428–449. [Google Scholar] [CrossRef]
- Kumar, R.; Thakur, A.; Sachin; Chandra, D.; Kumar Dhiman, A.; Kumar Verma, P.; Sharma, U. Quinoline-Based Metal Complexes: Synthesis and Applications. Coord. Chem. Rev. 2024, 499, 215453. [Google Scholar] [CrossRef]
- Banasz, R.; Wałęsa-Chorab, M. Polymeric Complexes of Transition Metal Ions as Electrochromic Materials: Synthesis and Properties. Coord. Chem. Rev. 2019, 389, 1–18. [Google Scholar] [CrossRef]
- Daniel, C. Photochemistry and Photophysics of Transition Metal Complexes: Quantum Chemistry. Coord. Chem. Rev. 2015, 282–283, 19–32. [Google Scholar] [CrossRef]
- Sodhi, R.K.; Paul, S. Metal Complexes in Medicine: An Overview and Update from Drug Design Perspective. Cancer Ther. Oncol. Int. J. 2019, 14, 25–32. [Google Scholar] [CrossRef]
- Hossain, A.M.S.; Méndez-Arriaga, J.M.; Xia, C.; Xie, J.; Gómez-Ruiz, S. Metal Complexes with ONS Donor Schiff Bases. A Review. Polyhedron 2022, 217, 115692. [Google Scholar] [CrossRef]
- Singh, P.; Yadav, P.; Kaur Sodhi, K.; Tomer, A.; Bali Mehta, S. Advancement in the Synthesis of Metal Complexes with Special Emphasis on Schiff Base Ligands and Their Important Biological Aspects. Results Chem. 2024, 7, 101222. [Google Scholar] [CrossRef]
- Trudu, F.; Amato, F.; Vaňhara, P.; Pivetta, T.; Peña-Méndez, E.M.; Havel, J. Coordination Compounds in Cancer: Past, Present and Perspectives. J. Appl. Biomed. 2015, 13, 79–103. [Google Scholar] [CrossRef]
- Evans, A.; Kavanagh, K.A. Evaluation of Metal-Based Antimicrobial Compounds for the Treatment of Bacterial Pathogens. J. Med. Microbiol. 2021, 70, 001363. [Google Scholar] [CrossRef] [PubMed]
- Karges, J.; Cohen, S.M. Metal Complexes as Antiviral Agents for SARS-CoV-2. ChemBioChem 2021, 22, 2600–2607. [Google Scholar] [CrossRef] [PubMed]
- Tahghighi, A. Importance of Metal Complexes for Development of Potential Leishmanicidal Agents. J. Organomet. Chem. 2014, 770, 51–60. [Google Scholar] [CrossRef]
- Machado, J.F.; Marques, F.; Pinheiro, T.; Villa de Brito, M.J.; Scalese, G.; Pérez-Díaz, L.; Otero, L.; António, J.P.M.; Gambino, D.; Morais, T.S. Copper(I)-Thiosemicarbazone Complexes with Dual Anticancer and Antiparasitic Activity. ChemMedChem 2023, 18, e202300074. [Google Scholar] [CrossRef] [PubMed]
- Méndez-Arriaga, J.M.; Rodríguez-Diéguez, A.; Sánchez-Moreno, M. In Vitro Leishmanicidal Activity of Copper (II) 5,7-Dimethyl-1,2,4-Triazolo[1,5-a]Pyrimidine Complex and Analogous Transition Metal Series. Polyhedron 2020, 176, 114272. [Google Scholar] [CrossRef]
- de Oliveira, T.D.; Ribeiro, G.H.; Honorato, J.; Leite, C.M.; Santos, A.C.d.S.; Silva, E.D.; Pereira, V.R.A.; Plutín, A.M.; Cominetti, M.R.; Castellano, E.E.; et al. Cytotoxic and Antiparasitic Activities of Diphosphine-Metal Complexes of Group 10 Containing Acylthiourea as Ligands. J. Inorg. Biochem. 2022, 234, 111906. [Google Scholar] [CrossRef]
- Savir, S.; Wei, Z.J.; Liew, J.W.K.; Vythilingam, I.; Lim, Y.A.L.; Saad, H.M.; Sim, K.S.; Tan, K.W. Synthesis, Cytotoxicity and Antimalarial Activities of Thiosemicarbazones and Their Nickel (II) Complexes. J. Mol. Struct. 2020, 1211, 128090. [Google Scholar] [CrossRef]
- Azevedo-França, J.A.d.; Granado, R.; de Macedo Silva, S.T.; Santos-Silva, G.d.; Scapin, S.; Borba-Santos, L.P.; Rozental, S.; de Souza, W.; Martins-Duarte, É.S.; Barrias, E.; et al. Synthesis and Biological Activity of Novel Zinc-Itraconazole Complexes in Protozoan Parasites and Sporothrix spp. Antimicrob. Agents Chemother. 2020, 64, 10-1128. [Google Scholar] [CrossRef]
- Méndez-Arriaga, J.M.; Rubio-Mirallas, E.; Quirós, M.; Sánchez-Moreno, M. Zinc 1,2,4-Triazolo[1,5-a]Pyrimidine Complexes: Synthesis, Structural Characterization and Their Effect against Chagas Disease. Med. Chem. 2022, 18, 444–451. [Google Scholar] [CrossRef]
- Navarro, M. Gold Complexes as Potential Anti-Parasitic Agents. Coord. Chem. Rev. 2009, 253, 1619–1626. [Google Scholar] [CrossRef]
- Esteban-Parra, G.M.; Méndez-Arriaga, J.M.; Rodríguez-Diéguez, A.; Quirós, M.; Salas, J.M.; Sánchez-Moreno, M. High Antiparasitic Activity of Silver Complexes of 5,7-Dimethyl-1,2,4-Triazolo[1,5 a]Pyrimidine. J. Inorg. Biochem. 2019, 201, 110810. [Google Scholar] [CrossRef] [PubMed]
- Gambino, D.; Otero, L. Facing Diseases Caused by Trypanosomatid Parasites: Rational Design of Pd and Pt Complexes with Bioactive Ligands. Front. Chem. 2022, 9, 816266. [Google Scholar] [CrossRef] [PubMed]
- Gambino, D.; Otero, L. Design of Prospective Antiparasitic Metal-Based Compounds Including Selected Organometallic Cores. Inorganica Chim. Acta 2018, 472, 58–75. [Google Scholar] [CrossRef]
- Sundar, S.; Chakravarty, J. Antimony Toxicity. Int. J. Environ. Res. Public Health 2010, 7, 4267–4277. [Google Scholar] [CrossRef] [PubMed]
- Haldar, A.K.; Sen, P.; Roy, S. Use of Antimony in the Treatment of Leishmaniasis: Current Status and Future Directions. Mol. Biol. Int. 2011, 2011, e571242. [Google Scholar] [CrossRef] [PubMed]
- Gress, M.E.; Jacobson, R.A. X-Ray and White Radiation Neutron Diffraction Studies of Optically Active Potassium Antimony Tartrate, K2Sb2(d-C4H2O6)2·3H2O (Tarter Emetic). Inorganica Chim. Acta 1974, 8, 209–217. [Google Scholar] [CrossRef]
- Frézard, F.; Demicheli, C.; Ribeiro, R.R. Pentavalent Antimonials: New Perspectives for Old Drugs. Molecules 2009, 14, 2317–2336. [Google Scholar] [CrossRef] [PubMed]
- Roberts, W.L.; McMurray, W.J.; Rainey, P.M. Characterization of the Antimonial Antileishmanial Agent Meglumine Antimonate (Glucantime). Antimicrob. Agents Chemother. 1998, 42, 1076–1082. [Google Scholar] [CrossRef]
- Demicheli, C.; Vallejos, V.M.R.; Lanza, J.S.; Ramos, G.S.; Do Prado, B.R.; Pomel, S.; Loiseau, P.M.; Frézard, F. Supramolecular Assemblies from Antimony(V) Complexes for the Treatment of Leishmaniasis. Biophys. Rev. 2023, 15, 751–765. [Google Scholar] [CrossRef] [PubMed]
- Borborema, S.E.T.; Osso, J.A.; de Andrade, H.F.; do Nascimento, N. Biodistribution of Meglumine Antimoniate in Healthy and Leishmania (Leishmania) Infantum Chagasi-Infected BALB/c Mice. Memórias Inst. Oswaldo Cruz 2013, 108, 623–630. [Google Scholar] [CrossRef] [PubMed]
- Martins, P.S.; Ochoa, R.; Pimenta, A.M.C.; Ferreira, L.A.M.; Melo, A.L.; da Silva, J.B.B.; Sinisterra, R.D.; Demicheli, C.; Frézard, F. Mode of Action of β-Cyclodextrin as an Absorption Enhancer of the Water-Soluble Drug Meglumine Antimoniate. Int. J. Pharm. 2006, 325, 39–47. [Google Scholar] [CrossRef] [PubMed]
- Albalawi, A.E.; Abdel-Shafy, S.; Khudair Khalaf, A.; Alanazi, A.D.; Baharvand, P.; Ebrahimi, K.; Mahmoudvand, H. Therapeutic Potential of Green Synthesized Copper Nanoparticles Alone or Combined with Meglumine Antimoniate (Glucantime®) in Cutaneous Leishmaniasis. Nanomaterials 2021, 11, 891. [Google Scholar] [CrossRef] [PubMed]
- Pereira, M.B.; Sydor, B.G.; Memare, K.G.; Verzignassi Silveira, T.G.; Alessi Aristides, S.M.; Dalmarco, E.M.; Vieira Teixeira, J.J.; Campana Lonardoni, M.V.; Demarchi, I.G. In Vivo Efficacy of Meglumine Antimoniate-Loaded Nanoparticles for Cutaneous Leishmaniasis: A Systematic Review. Nanomedicine 2021, 16, 1505–1518. [Google Scholar] [CrossRef] [PubMed]
- Sun, H.; Yan, S.C.; Cheng, W.S. Interaction of Antimony Tartrate with the Tripeptide Glutathione. Eur. J. Biochem. 2000, 267, 5450–5457. [Google Scholar] [CrossRef] [PubMed]
- dos Santos Ferreira, C.; Silveira Martins, P.; Demicheli, C.; Brochu, C.; Ouellette, M.; Frézard, F. Thiol-Induced Reduction of Antimony(V) into Antimony(III): A Comparative Study with Trypanothione, Cysteinyl-Glycine, Cysteine and Glutathione. Biometals 2003, 16, 441–446. [Google Scholar] [CrossRef] [PubMed]
- Colotti, G.; Ilari, A. Antimony-Based Therapy of Leishmaniases, Molecular and Cellular Rationale. In Encyclopedia of Metalloproteins; Kretsinger, R.H., Uversky, V.N., Permyakov, E.A., Eds.; Springer: New York, NY, USA, 2013; pp. 78–86. ISBN 978-1-4614-1533-6. [Google Scholar]
- Serbate Borges Portela, Á.; Margotto Bertollo, C.; da Silva Praxedes, M.F.; Silva Brasileiro, S.A.; Moreira Reis, A.M.; Parreiras Martins, M.A. Adverse Reactions to Meglumine Antimoniate in Brazilian Inpatients with Visceral Leishmaniases: A Case Series. J. Clin. Pharm. Ther. 2020, 45, 573–576. [Google Scholar] [CrossRef] [PubMed]
- Tahir, M.; Bashir, U.; Ahmed, N.; Mumtaz, J. Electrocardiographic changes with standard dose of meglumine antimoniate therapy in cutaneous leishmaniasis. Pak. Armed Forces Med. J. 2021, 71, 1235–1238. [Google Scholar] [CrossRef]
- Lyra, M.R.; Passos, S.R.L.; Pimentel, M.I.F.; Bedoya-Pacheco, S.J.; Valete-Rosalino, C.M.; Vasconcellos, E.C.F.; Antonio, L.F.; Saheki, M.N.; Salgueiro, M.M.; Santos, G.P.L.; et al. Pancreatic toxicity as an adverse effect induced by meglumine antimoniate therapy in a clinical trial for cutaneous leishmaniasis. Rev. Inst. Med. Trop. São Paulo 2016, 58, 68. [Google Scholar] [CrossRef]
- Da Justa Neves, D.B.; Caldas, E.D.; Sampaio, R.N.R. Antimony in Plasma and Skin of Patients with Cutaneous Leishmaniasis—Relationship with Side Effects after Treatment with Meglumine Antimoniate. Trop. Med. Int. Health 2009, 14, 1515–1522. [Google Scholar] [CrossRef]
- Miranda, E.S.; Miekeley, N.; De-Carvalho, R.R.; Paumgartten, F.J.R. Developmental Toxicity of Meglumine Antimoniate and Transplacental Transfer of Antimony in the Rat. Reprod. Toxicol. 2006, 21, 292–300. [Google Scholar] [CrossRef]
- Cruz, A.; Rainey, P.M.; Herwaldt, B.L.; Stagni, G.; Palacios, R.; Trujillo, R.; Saravia, N.G. Pharmacokinetics of Antimony in Children Treated for Leishmaniasis with Meglumine Antimoniate. J. Infect. Dis. 2007, 195, 602–608. [Google Scholar] [CrossRef]
- Berman, J.D.; Waddell, D.; Hanson, B.D. Biochemical Mechanisms of the Antileishmanial Activity of Sodium Stibogluconate. Antimicrob. Agents Chemother. 1985, 27, 916–920. [Google Scholar] [CrossRef]
- Elammari, N.E.; Sariti, S.R. Anti-Leishmanial Drug Pentostam Induced Histological Changes to Liver and Kidney in Male BALB/c Wild Mice. J. Int. Med. Res. Health Sci. 2021, 1, 7–14. [Google Scholar] [CrossRef]
- Herman, J.D.; Gallalee, J.V.; Best, J.M. Sodium Stibogluconate (Pentostam) Inhibition of Glucose Catabolism via the Glycolytic Pathway, and Fatty Acid β-Oxidation in Leishmania Mexicana Amastigotes. Biochem. Pharmacol. 1987, 36, 197–201. [Google Scholar] [CrossRef]
- Elmekki, M.A.; Elhassan, M.M.; Ozbak, H.A.; Qattan, I.T.; Saleh, S.M.; Alharbi, A.H. Epidemiological Trends of Cutaneous Leishmaniasis in Al-Madinah Al-Munawarah Province, Western Region of Saudi Arabia. J. Glob. Infect. Dis. 2017, 9, 146. [Google Scholar] [CrossRef]
- Iqbal, N.; Reeta; Ahluwalia, V.; Agrawal, A.; Dubey, S.; Kumar, J.; Dubey, S. Chapter 8—Medicinally Important Natural Bioactive Compounds for Leishmaniasis Treatment: Efficient Alternate of Toxic Drugs. In Studies in Natural Products Chemistry; Rahman, A., Ed.; Studies in Natural Product Chemistry; Elsevier: Amsterdam, The Netherlands, 2023; Volume 76, pp. 247–297. [Google Scholar]
- Anjum, A.; Shabbir, K.; Din, F.U.; Shafique, S.; Zaidi, S.S.; Almari, A.H.; Alqahtani, T.; Maryiam, A.; Moneeb Khan, M.; Al Fatease, A.; et al. Co-Delivery of Amphotericin B and Pentamidine Loaded Niosomal Gel for the Treatment of Cutaneous Leishmaniasis. Drug Deliv. 2023, 30, 2173335. [Google Scholar] [CrossRef]
- Borges, B.S.; Bueno, G.d.P.; Tomiotto-Pellissier, F.; Figueiredo, F.B.; Soares Medeiros, L.C. In Vitro Anti-Leishmania Activity of Triclabendazole and Its Synergic Effect with Amphotericin B. Front. Cell. Infect. Microbiol. 2023, 12, 1044665. [Google Scholar] [CrossRef]
- Boshrouyeh, R.; Amari, S.; Boshrouyeh Ghandashtani, M.; Alavi, S.E.; Ebrahimi Shahmabadi, H. A Topical Gel Nanoformulation of Amphotericin B (AmB) for the Treatment of Cutaneous Leishmaniasis (CL). J. Sol-Gel Sci. Technol. 2023, 105, 768–780. [Google Scholar] [CrossRef]
- Melcon-Fernandez, E.; Galli, G.; García-Estrada, C.; Balaña-Fouce, R.; Reguera, R.M.; Pérez-Pertejo, Y. Miltefosine and Nifuratel Combination: A Promising Therapy for the Treatment of Leishmania Donovani Visceral Leishmaniasis. Int. J. Mol. Sci. 2023, 24, 1635. [Google Scholar] [CrossRef]
- Matos, A.P.S.; Viçosa, A.L.; Ré, M.I.; Ricci-Júnior, E.; Holandino, C. A Review of Current Treatments Strategies Based on Paromomycin for Leishmaniasis. J. Drug Deliv. Sci. Technol. 2020, 57, 101664. [Google Scholar] [CrossRef]
- Younis, B.M.; Musa, A.M.; Monnerat, S.; Saeed, M.A.; Khalil, E.A.G.; Ahmed, A.E.; Ali, M.A.; Noureldin, A.; Ouattara, G.M.; Nyakaya, G.M.; et al. Safety and Efficacy of Paromomycin/Miltefosine/Liposomal Amphotericin B Combinations for the Treatment of Post-Kala-Azar Dermal Leishmaniasis in Sudan: A Phase II, Open Label, Randomized, Parallel Arm Study. PLOS Neglected Trop. Dis. 2023, 17, e0011780. [Google Scholar] [CrossRef]
- Chudzik, B.; Tracz, I.B.; Czernel, G.; Fiołka, M.J.; Borsuk, G.; Gagoś, M. Amphotericin B–Copper(II) Complex as a Potential Agent with Higher Antifungal Activity against Candida albicans. Eur. J. Pharm. Sci. 2013, 49, 850–857. [Google Scholar] [CrossRef]
- Pérez-Molina, J.A.; Crespillo-Andújar, C.; Bosch-Nicolau, P.; Molina, I. Trypanocidal treatment of Chagas disease. Enferm. Infecc. Microbiol. Clin. 2021, 39, 458–470. [Google Scholar] [CrossRef]
- Lidani, K.C.F.; Andrade, F.A.; Bavia, L.; Damasceno, F.S.; Beltrame, M.H.; Messias-Reason, I.J.; Sandri, T.L. Chagas Disease: From Discovery to a Worldwide Health Problem. Front. Public Health 2019, 7, 166. [Google Scholar] [CrossRef]
- Docampo, R.; Moreno, S.N.J.; Stoppani, A.O.M. Nitrofuran Enhancement of Microsomal Electron Transport, Superoxide Anion Production and Lipid Peroxidation. Arch. Biochem. Biophys. 1981, 207, 316–324. [Google Scholar] [CrossRef]
- de Souza, C.C.; de Azevedo-França, J.A.; Barrias, E.; Cavalcante, S.C.F.; Vieira, E.G.; Ferreira, A.M.D.C.; de Souza, W.; Navarro, M. Silver and Copper-Benznidazole Derivatives as Potential Antiparasitic Metallodrugs: Synthesis, Characterization, and Biological Evaluation. J. Inorg. Biochem. 2023, 239, 112047. [Google Scholar] [CrossRef]
- Teixeira, M.M.; Carvalho, D.T.; Sousa, E.; Pinto, E. New Antifungal Agents with Azole Moieties. Pharmaceuticals 2022, 15, 1427. [Google Scholar] [CrossRef]
- Kuznetsov, A.E. Introductory Chapter: Azoles, Their Importance, and Applications. In Azoles—Synthesis, Properties, Applications and Perspectives; IntechOpen: London, UK, 2021; ISBN 978-1-83968-180-6. [Google Scholar]
- Emami, L.; Faghih, Z.; Ataollahi, E.; Sadeghian, S.; Rezaei, Z.; Khabnadideh, S. Azole Derivatives: Recent Advances as Potent Antibacterial and Antifungal Agents. Curr. Med. Chem. 2023, 30, 220–249. [Google Scholar] [CrossRef]
- Paul, A.; Guria, T.; Roy, P.; Maity, A. Recent Development of Heterocyclic Compounds with Indazole Moiety as Potential Antiparasitic Agents. Curr. Top. Med. Chem. 2022, 22, 1160–1176. [Google Scholar] [CrossRef]
- Azevedo-França, J.A.d.; Ramos, V.F.d.S.; Messori, L.; Santanni, F.; Sorace, L.; Borba-Santos, L.P.; Rozental, S.; Rodrigues, J.C.F.; Navarro, M. Synthesis, Characterization, and Biological Evaluation of Hybrid Copper(II) Complexes Containing Azole Drugs and Planar Ligands against Neglected Diseases. New J. Chem. 2024, 48, 2515–2526. [Google Scholar] [CrossRef]
- Sharma, M.; Prasher, P. An Epigrammatic Status of the ‘Azole’-Based Antimalarial Drugs. RSC Med. Chem. 2020, 11, 184–211. [Google Scholar] [CrossRef]
- Walvekar, S.; Anwar, A.; Anwar, A.; Sridewi, N.; Khalid, M.; Yow, Y.Y.; Khan, N.A. Anti-Amoebic Potential of Azole Scaffolds and Nanoparticles against Pathogenic Acanthamoeba. Acta Trop. 2020, 211, 105618. [Google Scholar] [CrossRef]
- Emami, S.; Tavangar, P.; Keighobadi, M. An Overview of Azoles Targeting Sterol 14α-Demethylase for Antileishmanial Therapy. Eur. J. Med. Chem. 2017, 135, 241–259. [Google Scholar] [CrossRef]
- Baiocco, P.; Poce, G.; Alfonso, S.; Cocozza, M.; Porretta, G.C.; Colotti, G.; Biava, M.; Moraca, F.; Botta, M.; Yardley, V.; et al. Inhibition of Leishmania Infantum Trypanothione Reductase by Azole-Based Compounds: A Comparative Analysis with Its Physiological Substrate by X-Ray Crystallography. ChemMedChem 2013, 8, 1175–1183. [Google Scholar] [CrossRef]
- Braga, S.S. Ruthenium Complexes, an Emerging Class of Leishmanicidal Drug Candidates. Appl. Biosci. 2022, 1, 129–142. [Google Scholar] [CrossRef]
- García-Valdivia, A.A.; García-García, A.; Jannus, F.; Zabala-Lekuona, A.; Méndez-Arriaga, J.M.; Fernández, B.; Medina-O’donnell, M.; Ramírez-Rodríguez, G.B.; Delgado-López, J.M.; Pastrana-Martínez, L.M.; et al. Antiparasitic, Anti-Inflammatory and Cytotoxic Activities of 2D Coordination Polymers Based on 1H-Indazole-5-Carboxylic Acid. J. Inorg. Biochem. 2020, 208, 111098. [Google Scholar] [CrossRef]
- Navarro-Peñaloza, R.; Landeros-Rivera, B.; López-Sandoval, H.; Castro-Ramírez, R.; Barba-Behrens, N. New Insights on Transition Metal Coordination Compounds with Biological Active Azole and Nitroimidazole Derivatives. Coord. Chem. Rev. 2023, 494, 215360. [Google Scholar] [CrossRef]
- Bülow, C.; Haas, K. Synthetische Versuche Zur Darstellung von Derivaten Des Heterokondensierten, Heterocyclischen 1.3-Triazo-7.0′-Pyrimidins. Berichte Dtsch. Chem. Ges. 1909, 42, 4638–4644. [Google Scholar] [CrossRef]
- Birr, E.J. Azo-indolizine als photochemisch interessante Substanzen. Z. Wiss. Phot. 1952, 47, 1755–1764. [Google Scholar]
- Qu, R.; Liu, Y.; Kandegama, W.M.W.W.; Chen, Q.; Yang, G. Recent Applications of Triazolopyrimidine-Based Bioactive Compounds in Medicinal and Agrochemical Chemistry. Mini Rev. Med. Chem. 2018, 18, 781–793. [Google Scholar] [CrossRef]
- Salem, M.A.; Behalo, M.S.; Khidre, R.E. Recent Trend in the Chemistry of Triazolopyrimidines and Their Applications. Mini-Rev. Org. Chem. 2021, 18, 1134–1149. [Google Scholar] [CrossRef]
- Felicetti, T.; Pismataro, M.C.; Cecchetti, V.; Tabarrini, O.; Massari, S. Triazolopyrimidine Nuclei: Privileged Scaffolds for Developing Antiviral Agents with a Proper Pharmacokinetic Profile. Curr. Med. Chem. 2022, 29, 1379–1407. [Google Scholar] [CrossRef]
- Abdelkhalek, A.S.; Attia, M.S.; Kamal, M.A. Triazolopyrimidine Derivatives: An Updated Review on Recent Advances in Synthesis, Biological Activities and Drug Delivery Aspects. Curr. Med. Chem. 2024, 31, 1896–1919. [Google Scholar] [CrossRef]
- Merugu, S.R.; Cherukupalli, S.; Karpoormath, R. An Overview on Synthetic and Medicinal Perspectives of [1,2,4]Triazolo[1,5-a]Pyrimidine Scaffold. Chem. Biodivers. 2022, 19, e202200291. [Google Scholar] [CrossRef]
- Mohamed, A.M.; El-Sayed, W.A.; Ibrahim, A.A.; Abdel-Hafez, N.A.; Ali, K.A.K.; Mohamed, S.F. Recent Trends in the Chemistry of [1,2,4]Triazole[1,5-a]Pyrimidines. Org. Prep. Proced. Int. 2021, 53, 211–239. [Google Scholar] [CrossRef]
- Méndez-Arriaga, J.M.; Oyarzabal, I.; Martín-Montes, Á.; García-Rodríguez, J.; Quirós, M.; Sánchez-Moreno, M. First Example of Antiparasitic Activity Influenced by Thermochromism: Leishmanicidal Evaluation of 5,7-Dimethyl-1,2,4-Triazolo[1,5-a]Pyrimidine Metal Complexes. Med. Chem. 2020, 16, 422–430. [Google Scholar] [CrossRef]
- Esteban-Parra, G.M.; Sebastián, E.S.; Cepeda, J.; Sánchez-González, C.; Rivas-García, L.; Llopis, J.; Aranda, P.; Sánchez-Moreno, M.; Quirós, M.; Rodríguez-Diéguez, A. Anti-Diabetic and Anti-Parasitic Properties of a Family of Luminescent Zinc Coordination Compounds Based on the 7-Amino-5-Methyl-1,2,4-Triazolo[1,5-a]Pyrimidine Ligand. J. Inorg. Biochem. 2020, 212, 111235. [Google Scholar] [CrossRef]
- Kaszuba, A.; Barwiołek, M.; Sitkowski, J.; Wojtczak, A.; Łakomska, I. Structural Characteristics and Biological Properties of New Pseudo-Octahedral Ruthenium(II) Complexes Containing a Biphenyl Moiety. Polyhedron 2024, 249, 116780. [Google Scholar] [CrossRef]
- Caballero, A.B.; Rodríguez-Diéguez, A.; Quirós, M.; Salas, J.M.; Huertas, Ó.; Ramírez-Macías, I.; Olmo, F.; Marín, C.; Chaves-Lemaur, G.; Gutierrez-Sánchez, R.; et al. Triazolopyrimidine Compounds Containing First-Row Transition Metals and Their Activity against the Neglected Infectious Chagas Disease and Leishmaniasis. Eur. J. Med. Chem. 2014, 85, 526–534. [Google Scholar] [CrossRef]
- Karimi-Chayjani, R.; Daneshvar, N.; Nikoo Langarudi, M.S.; Shirini, F.; Tajik, H. Silica-Coated Magnetic Nanoparticles Containing Bis Dicationic Bridge for the Synthesis of 1,2,4-Triazolo Pyrimidine/ Quinazolinone Derivatives. J. Mol. Struct. 2020, 1199, 126891. [Google Scholar] [CrossRef]
- Chkirate, K.; Fettach, S.; El Hafi, M.; Karrouchi, K.; Elotmani, B.; Mague, J.T.; Radi, S.; Faouzi, M.E.A.; Adarsh, N.N.; Essassi, E.M.; et al. Solvent Induced Supramolecular Polymorphism in Cu(II) Coordination Complex Built from 1,2,4-Triazolo[1,5-a]Pyrimidine: Crystal Structures and Anti-Oxidant Activity. J. Inorg. Biochem. 2020, 208, 111092. [Google Scholar] [CrossRef]
- Pinheiro, S.; Pinheiro, E.M.C.; Muri, E.M.F.; Pessôa, J.C.; Cadorini, M.A.; Greco, S.J. Biological Activities of [1,2,4]Triazolo[1,5-a]Pyrimidines and Analogs. Med. Chem. Res. 2020, 29, 1751–1776. [Google Scholar] [CrossRef]
- Maldonado, C.R.; Quirós, M.; Salas, J.M. 1,2,4-Triazolo[1,5-a]Pyrimidin-3-Ium Chloride. Acta Crystallogr. Sect. E 2007, 63, o1509–o1510. [Google Scholar] [CrossRef]
- Esteban-Parra, G.M.; Moscoso, I.; Cepeda, J.; García, J.A.; Sánchez-Moreno, M.; Rodríguez-Diéguez, A.; Quirós, M. Lanthanide(III) Based Complexes Containing 5,7-Dimethyl-1,2,4-Triazolo[1,5-a]Pyrimidine as Long-Lived Photoluminescent Antiparasitic Agents. Eur. J. Inorg. Chem. 2020, 2020, 308–317. [Google Scholar] [CrossRef]
- Méndez-Arriaga, J.M.; Oyarzabal, I.; Escolano, G.; Rodríguez-Diéguez, A.; Sánchez-Moreno, M.; Salas, J.M. In Vitro Leishmanicidal and Trypanocidal Evaluation and Magnetic Properties of 7-Amino-1,2,4-Triazolo[1,5-a]Pyrimidine Cu(II) Complexes. J. Inorg. Biochem. 2018, 180, 26–32. [Google Scholar] [CrossRef]
- Abul Haj, M.; Salas, J.M.; Quirós, M.; Molina, J.; Faure, R. 5-Oxo and 7-Oxo Derivatives of [1,2,4]Triazolo-[1,5-a]Pyrimidine: Characterization and Theoretical Study. J. Mol. Struct. 2000, 519, 165–172. [Google Scholar] [CrossRef]
- Navarro, J.A.R.; Romero, M.A.; Salas, J.M.; Faure, R.; Solans, X. Polymeric Silver(I) Complexes of the Multinucleating Ligand4,7-Dihydro-5-Methyl-7-Oxo[1,2,4]Triazolo[1,5-a]Pyrimidine. Analogous Hydrogen-Bonded Structures in the Crystal and Vapour Phases of the Ligand. J. Chem. Soc. Dalton Trans. 1997, 13, 2321–2326. [Google Scholar] [CrossRef]
- Méndez-Arriaga, J.M.; Esteban-Parra, G.M.; Juárez, M.J.; Rodríguez-Diéguez, A.; Sánchez-Moreno, M.; Isac-García, J.; Salas, J.M. Antiparasitic Activity against Trypanosomatid Diseases and Novel Metal Complexes Derived from the First Time Characterized 5-Phenyl-1,2,4-Triazolo[1,5-a]Pyrimidi-7(4H)-One. J. Inorg. Biochem. 2017, 175, 217–224. [Google Scholar] [CrossRef]
- Salas, J.M.; Caballero, A.B.; Esteban-Parra, G.M.; Méndez-Arriaga, J.M. Leishmanicidal and Trypanocidal Activity of Metal Complexes with 1,2,4-Triazolo[1,5-a]Pyrimidines: Insights on Their Therapeutic Potential against Leishmaniasis and Chagas Disease. Curr. Med. Chem. 2017, 24, 2796–2806. [Google Scholar] [CrossRef] [PubMed]
- Łakomska, I.; Fandzloch, M. Application of 1,2,4-Triazolo[1,5-a]Pyrimidines for the Design of Coordination Compounds with Interesting Structures and New Biological Properties. Coord. Chem. Rev. 2016, 327–328, 221–241. [Google Scholar] [CrossRef]
- Manske, R.H. The Chemistry of Quinolines. Available online: https://pubs.acs.org/doi/pdf/10.1021/cr60095a006 (accessed on 24 March 2024).
- Keri, R.S.; Patil, S.A. Quinoline: A Promising Antitubercular Target. Biomed. Pharmacother. 2014, 68, 1161–1175. [Google Scholar] [CrossRef] [PubMed]
- Ajani, O.; Iyaye, K.T.; Ademosun, O.T. Recent Advances in Chemistry and Therapeutic Potential of Functionalized Quinoline Motifs—A Review. RSC Adv. 2022, 12, 18594–18614. [Google Scholar] [CrossRef] [PubMed]
- Patel, K.B.; Kumari, P. A Review: Structure-Activity Relationship and Antibacterial Activities of Quinoline Based Hybrids. J. Mol. Struct. 2022, 1268, 133634. [Google Scholar] [CrossRef]
- Jeleń, M.; Morak-Młodawska, B.; Korlacki, R. Anticancer Activities of Tetra-, Penta-, and Hexacyclic Phenothiazines Modified with Quinoline Moiety. J. Mol. Struct. 2023, 1287, 135700. [Google Scholar] [CrossRef]
- Kumar, N.; Khanna, A.; Kaur, K.; Kaur, H.; Sharma, A.; Bedi, P.M.S. Quinoline Derivatives Volunteering against Antimicrobial Resistance: Rational Approaches, Design Strategies, Structure Activity Relationship and Mechanistic Insights. Mol. Divers. 2023, 27, 1905–1934. [Google Scholar] [CrossRef]
- Bawa, S.; Kumar, S.; Drabu, S.; Kumar, R. Structural Modifications of Quinoline-Based Antimalarial Agents: Recent Developments. J. Pharm. Bioallied Sci. 2010, 2, 64. [Google Scholar] [CrossRef]
- Silva, C.F.M.; Pinto, D.C.G.A.; Fernandes, P.A.; Silva, A.M.S. Evolution of the Quinoline Scaffold for the Treatment of Leishmaniasis: A Structural Perspective. Pharmaceuticals 2024, 17, 285. [Google Scholar] [CrossRef]
- Senerovic, L.; Opsenica, D.; Moric, I.; Aleksic, I.; Spasić, M.; Vasiljevic, B. Quinolines and Quinolones as Antibacterial, Antifungal, Anti-Virulence, Antiviral and Anti-Parasitic Agents. In Advances in Microbiology, Infectious Diseases and Public Health: Volume 14; Donelli, G., Ed.; Springer International Publishing: Cham, Switzerland, 2020; pp. 37–69. ISBN 978-3-030-53647-3. [Google Scholar]
- Reynolds, K.; Loughlin, W.A.; Young, D.J. Quinolines as Chemotherapeutic Agents for Leishmaniasis. Mini Rev. Med. Chem. 2013, 13, 730–743. [Google Scholar] [CrossRef]
- Bringmann, G.; Thomale, K.; Bischof, S.; Schneider, C.; Schultheis, M.; Schwarz, T.; Moll, H.; Schurigt, U. A Novel Leishmania Major Amastigote Assay in 96-Well Format for Rapid Drug Screening and Its Use for Discovery and Evaluation of a New Class of Leishmanicidal Quinolinium Salts. Antimicrob. Agents Chemother. 2013, 57, 3003–3011. [Google Scholar] [CrossRef] [PubMed]
- Coimbra, E.S.; Antinarelli, L.M.R.; Silva, N.P.; Souza, I.O.; Meinel, R.S.; Rocha, M.N.; Soares, R.P.P.; da Silva, A.D. Quinoline Derivatives: Synthesis, Leishmanicidal Activity and Involvement of Mitochondrial Oxidative Stress as Mechanism of Action. Chem.-Biol. Interact. 2016, 260, 50–57. [Google Scholar] [CrossRef]
- Loiseau, P.M.; Balaraman, K.; Barratt, G.; Pomel, S.; Durand, R.; Frézard, F.; Figadère, B. The Potential of 2-Substituted Quinolines as Antileishmanial Drug Candidates. Molecules 2022, 27, 2313. [Google Scholar] [CrossRef] [PubMed]
- Nishigaki, S.; Yoshioka, H.; Nakatsu, K. The Crystal and Molecular Structure of O-Phenanthroline. Acta Cryst. B 1978, 34, 875–879. [Google Scholar] [CrossRef]
- Lima, A.K.C.; Elias, C.G.R.; Oliveira, S.S.C.; Santos-Mallet, J.R.; McCann, M.; Devereux, M.; Branquinha, M.H.; Dutra, P.M.L.; Santos, A.L.S. Anti-Leishmania Braziliensis Activity of 1,10-Phenanthroline-5,6-Dione and Its Cu(II) and Ag(I) Complexes. Parasitol. Res. 2021, 120, 3273–3285. [Google Scholar] [CrossRef]
- Lane, J.E.; Bogitsh, B.J.; Ribeiro-Rodrigues, R.; Kral, M.V.; Jones, M.M.; Carter, C.E. Ultrastructural Effects of the Chelating Agent 1,10-Phenanthroline on Trypanosoma cruzi Epimastigotes In Vitro. Parasitol. Res. 1998, 84, 399–402. [Google Scholar] [CrossRef]
- Agbale, C.M.; Cardoso, M.H.; Galyuon, I.K.; Franco, O.L. Designing Metallodrugs with Nuclease and Protease Activity. Metallomics 2016, 8, 1159–1169. [Google Scholar] [CrossRef] [PubMed]
- Iniguez, E.; Sánchez, A.; Vasquez, M.A.; Martínez, A.; Olivas, J.; Sattler, A.; Sánchez-Delgado, R.A.; Maldonado, R.A. Metal–Drug Synergy: New Ruthenium(II) Complexes of Ketoconazole Are Highly Active against Leishmania Major and Trypanosoma cruzi and Nontoxic to Human or Murine Normal Cells. J. Biol. Inorg. Chem. 2013, 18, 779–790. [Google Scholar] [CrossRef]
- Martínez, A.; Carreon, T.; Iniguez, E.; Anzellotti, A.; Sánchez, A.; Tyan, M.; Sattler, A.; Herrera, L.; Maldonado, R.A.; Sánchez-Delgado, R.A. Searching for New Chemotherapies for Tropical Diseases: Ruthenium–Clotrimazole Complexes Display High in Vitro Activity against Leishmania Major and Trypanosoma cruzi and Low Toxicity toward Normal Mammalian Cells. J. Med. Chem. 2012, 55, 3867–3877. [Google Scholar] [CrossRef]
- Caballero, A.B.; Marín, C.; Ramírez-Macías, I.; Rodríguez-Diéguez, A.; Quirós, M.; Salas, J.M.; Sánchez-Moreno, M. Structural Consequences of the Introduction of 2,2′-Bipyrimidine as Auxiliary Ligand in Triazolopyrimidine-Based Transition Metal Complexes. In Vitro Antiparasitic Activity. Polyhedron 2012, 33, 137–144. [Google Scholar] [CrossRef]
- Ramírez-Macías, I.; Maldonado, C.R.; Marín, C.; Olmo, F.; Gutiérrez-Sánchez, R.; Rosales, M.J.; Quirós, M.; Salas, J.M.; Sánchez-Moreno, M. In Vitro Anti-Leishmania Evaluation of Nickel Complexes with a Triazolopyrimidine Derivative against Leishmania Infantum and Leishmania Braziliensis. J. Inorg. Biochem. 2012, 112, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Fandzloch, M.; Arriaga, J.M.M.; Sánchez-Moreno, M.; Wojtczak, A.; Jezierska, J.; Sitkowski, J.; Wiśniewska, J.; Salas, J.M.; Łakomska, I. Strategies for Overcoming Tropical Disease by Ruthenium Complexes with Purine Analog: Application against Leishmania spp. and Trypanosoma cruzi. J. Inorg. Biochem. 2017, 176, 144–155. [Google Scholar] [CrossRef]
- Caballero, A.B.; Rodríguez-Diéguez, A.; Salas, J.M.; Sánchez-Moreno, M.; Marín, C.; Ramírez-Macías, I.; Santamaría-Díaz, N.; Gutiérrez-Sánchez, R. Lanthanide Complexes Containing 5-Methyl-1,2,4-Triazolo[1,5-a] Pyrimidin-7(4H)-One and Their Therapeutic Potential to Fight Leishmaniasis and Chagas Disease. J. Inorg. Biochem. 2014, 138, 39–46. [Google Scholar] [CrossRef]
- Martín-Montes, Á.; Jimenez-Falcao, S.; Gómez-Ruiz, S.; Marín, C.; Mendez-Arriaga, J.M. First-Row Transition 7-Oxo-5-Phenyl-1,2,4-Triazolo[1,5-a]Pyrimidine Metal Complexes: Antiparasitic Activity and Release Studies. Pharmaceuticals 2023, 16, 1380. [Google Scholar] [CrossRef] [PubMed]
- Paloque, L.; Hemmert, C.; Valentin, A.; Gornitzka, H. Synthesis, Characterization, and Antileishmanial Activities of Gold(I) Complexes Involving Quinoline Functionalized N-Heterocyclic Carbenes. Eur. J. Med. Chem. 2015, 94, 22–29. [Google Scholar] [CrossRef]
- Oliveira, S.S.C.; Santos, V.S.; Devereux, M.; McCann, M.; Santos, A.L.S.; Branquinha, M.H. The Anti-Leishmania Amazonensis and Anti-Leishmania Chagasi Action of Copper(II) and Silver(I) 1,10-Phenanthroline-5,6-Dione Coordination Compounds. Pathogens 2023, 12, 70. [Google Scholar] [CrossRef] [PubMed]
- Cunha, L.C.; Lage, D.P.; Ferreira, L.S.; Saboia-Vahia, L.; Coelho, E.A.F.; Belo, V.S.; Teixeira-Neto, R.G.; Soares, L.F.; Chagas, R.C.R.; da Silva, E.S. Leishmanicidal Activity of Ibuprofen and Its Complexes with Ni(II), Mn(II) and Pd(II). Inorg. Chem. Commun. 2020, 113, 107756. [Google Scholar] [CrossRef]
- García-García, A.; Méndez-Arriaga, J.M.; Martín-Escolano, R.; Cepeda, J.; Gómez-Ruiz, S.; Salinas-Castillo, A.; Seco, J.M.; Sánchez-Moreno, M.; Choquesillo-Lazarte, D.; Ruiz-Muelle, A.B.; et al. In Vitro Evaluation of Leishmanicidal Properties of a New Family of Monodimensional Coordination Polymers Based on Diclofenac Ligand. Polyhedron 2020, 184, 114570. [Google Scholar] [CrossRef]
- Tunes, L.G.; Morato, R.E.; Garcia, A.; Schmitz, V.; Steindel, M.; Corrêa-Junior, J.D.; Dos Santos, H.F.; Frézard, F.; de Almeida, M.V.; Silva, H.; et al. Preclinical Gold Complexes as Oral Drug Candidates to Treat Leishmaniasis Are Potent Trypanothione Reductase Inhibitors. ACS Infect. Dis. 2020, 6, 1121–1139. [Google Scholar] [CrossRef]
- García-García, A.; Echenique-Errandonea, E.; Cepeda, J.; Choquesillo-Lazarte, D.; Seco, J.M.; Salinas-Castillo, A.; Sánchez-Moreno, M.; Méndez-Arriaga, J.M.; Rodríguez-Diéguez, A. Photoluminescence and in Vitro Cytotoxicity Analysis in a Novel Mononuclear Zn(II) Coordination Compound Based on Bumetanide. Inorganica Chim. Acta 2020, 509, 119708. [Google Scholar] [CrossRef]
- Coksu, I.; Bozkurt, Y.; Akmayan, I.; Demirci, H.; Ozbek, T.; Acar, S. Ketoconazole-Loading Strategy to Improve Antifungal Activity and Overcome Cytotoxicity on Human Renal Proximal Tubular Epithelial Cells. Nanotechnology 2023, 35, 115702. [Google Scholar] [CrossRef] [PubMed]
- Salas, J.M.; Angustias Romero, M.; Purificación Sánchez, M.; Quirós, M. Metal Complexes of [1,2,4]Triazolo-[1,5-a]Pyrimidine Derivatives. Coord. Chem. Rev. 1999, 193–195, 1119–1142. [Google Scholar] [CrossRef]
- Boutaleb-Charki, S.; Marin, C.; Maldonado, C.R.; Rosales, M.J.; Urbano, J.; Guitierrez-Sanchez, R.; Quiros, M.; Salas, J.M.; Sanchez-Moreno, M. Copper (II) Complexes of [1,2,4]Triazolo [1,5-a]Pyrimidine Derivatives as Potential Anti-Parasitic Agents. Drug Metab. Lett. 2009, 3, 35–44. [Google Scholar] [CrossRef] [PubMed]
- Reis, D.C.; Pinto, M.C.X.; Souza-Fagundes, E.M.; Rocha, L.F.; Pereira, V.R.A.; Melo, C.M.L.; Beraldo, H. Investigation on the Pharmacological Profile of Antimony(III) Complexes with Hydroxyquinoline Derivatives: Anti-Trypanosomal Activity and Cytotoxicity against Human Leukemia Cell Lines. Biometals 2011, 24, 595–601. [Google Scholar] [CrossRef] [PubMed]
- Morozkov, G.V.; Abel, A.S.; Lyssenko, K.A.; Roznyatovsky, V.A.; Averin, A.D.; Beletskaya, I.P.; Bessmertnykh-Lemeune, A. Ruthenium(II) Complexes with Phosphonate-Substituted Phenanthroline Ligands as Reusable Photoredox Catalysts. Dalton Trans. 2024, 53, 535–551. [Google Scholar] [CrossRef]
- Osei, P.B.; Northcote-Smith, J.; Fang, J.; Singh, K.; Ortu, F.; Suntharalingam, K. The Bulk Breast Cancer Cell and Breast Cancer Stem Cell Activity of Binuclear Copper(II)-Phenanthroline Complexes. Chem.–A Eur. J. 2023, 29, e202301188. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, J.A.O.; Torres, A.U.; de Sousa, N.A.B.; de Sousa, T.J.D.; Neto, J.G.O.; Reis, A.S.; Lage, M.R.; dos Santos, A.O.; dos Santos, C.C.; de Menezes, A.S.; et al. Synthesis, Characterization, DFT Study, and Antibacterial Activity of a Coordination Complex of Cu(II) with 1,10-Phenanthroline and l-Methionine Ligands. J. Mol. Struct. 2023, 1293, 136197. [Google Scholar] [CrossRef]
- Iqbal, M.; Ali, S.; Tahir, M.N.; Anderson, P.A. Octahedral Copper(II) Carboxylates with 1,10-Phenanthroline: Synthesis, Structural Characterization, DNA-Binding and Anti-Fungal Properties. J. Chem. Crystallogr. 2021, 51, 418–431. [Google Scholar] [CrossRef]
- Abebe, A.; Bayeh, Y.; Belay, M.; Gebretsadik, T.; Thomas, M.; Linert, W. Mono and Binuclear Cobalt(II) Mixed Ligand Complexes Containing 1,10-Phenanthroline and Adenine Using 1,3-Diaminopropane as a Spacer: Synthesis, Characterization, and Antibacterial Activity Investigations. Future J. Pharm. Sci. 2020, 6, 13. [Google Scholar] [CrossRef]
- Deka, B.; Sarkar, T.; Bhattacharyya, A.; Butcher, R.J.; Banerjee, S.; Deka, S.; Saikia, K.K.; Hussain, A. Synthesis, Characterization, and Cancer Cell-Selective Cytotoxicity of Mixed-Ligand Cobalt(III) Complexes of 8-Hydroxyquinolines and Phenanthroline Bases. Dalton Trans. 2024, 53, 4952–4961. [Google Scholar] [CrossRef]
- Ishola, K.T.; Olaoye, O.J.; Oladipo, M.A.; Odedokun, O.A.; Aboyeji, O.O. Synthesis, Characterization and Antimicrobial Properties of Mixed-Ligand Complexes of Some Metal(II) Ions with Barbituric Acid and 1,10-Phenanthroline Ligands. Tanzan. J. Sci. 2023, 49, 491–502. [Google Scholar] [CrossRef]
- Egan, T.J.; Koch, K.R.; Swan, P.L.; Clarkson, C.; Van Schalkwyk, D.A.; Smith, P.J. In Vitro Antimalarial Activity of a Series of Cationic 2,2‘-Bipyridyl- and 1,10-Phenanthrolineplatinum(II) Benzoylthiourea Complexes. J. Med. Chem. 2004, 47, 2926–2934. [Google Scholar] [CrossRef]
- Lai, J.W.; Maah, M.J.; Tan, K.W.; Sarip, R.; Lim, Y.A.L.; Ganguly, R.; Khaw, L.T.; Ng, C.H. Dinuclear and Mononuclear Metal(II) Polypyridyl Complexes against Drug-Sensitive and Drug-Resistant Plasmodium Falciparum and Their Mode of Action. Malar. J. 2022, 21, 386. [Google Scholar] [CrossRef]
- Rigo, G.V.; Petro-Silveira, B.; Devereux, M.; McCann, M.; Santos, A.L.S.d.; Tasca, T. Anti-Trichomonas Vaginalis Activity of 1,10-Phenanthroline-5,6-Dione-Based Metallodrugs and Synergistic Effect with Metronidazole. Parasitology 2019, 146, 1179–1183. [Google Scholar] [CrossRef]
- León, I.E.; Cadavid-Vargas, J.F.; Tiscornia, I.; Porro, V.; Castelli, S.; Katkar, P.; Desideri, A.; Bollati-Fogolin, M.; Etcheverry, S.B. Oxidovanadium(IV) Complexes with Chrysin and Silibinin: Anticancer Activity and Mechanisms of Action in a Human Colon Adenocarcinoma Model. J. Biol. Inorg. Chem. 2015, 20, 1175–1191. [Google Scholar] [CrossRef]
- Benítez, J.; Becco, L.; Correia, I.; Leal, S.M.; Guiset, H.; Pessoa, J.C.; Lorenzo, J.; Tanco, S.; Escobar, P.; Moreno, V.; et al. Vanadium Polypyridyl Compounds as Potential Antiparasitic and Antitumoral Agents: New Achievements. J. Inorg. Biochem. 2011, 105, 303–312. [Google Scholar] [CrossRef] [PubMed]
- Santos, A.L.S.; Lima, A.K.C.; Oliveira, S.S.C.; dos Santos, R.F.; Devereux, M.; McCann, M.; Branquinha, M.H.; Dutra, P.M.L. Decoding the Anti-Leishmania Braziliensis Activity of 1,10-Phenanthroline-5,6-Dione and Its Silver- and Copper-Based Complexes: In Vitro and In Vivo Approaches. Eur. J. Med. Chem. Rep. 2022, 6, 100093. [Google Scholar] [CrossRef]
- Lawal, A.; Obaleye, J.A. Synthesis, Characterization and Antibacterial Activity of Aspirin and Paracetamol-Metal Complexes. Biokemistri 2007, 19, 9–15. [Google Scholar]
- Martinez, S.; Marr, J.J. Allopurinol in the Treatment of American Cutaneous Leishmaniasis. N. Engl. J. Med. 1992, 326, 741–744. [Google Scholar] [CrossRef]
- Potenza, M.; Tellez, M.T. Colchicine Treatment Reversibly Blocks Cytokinesis but Not Mitosis in Trypanosoma cruzi Epimastigotes. Parasitol. Res. 2015, 114, 641–649. [Google Scholar] [CrossRef]
- Fernandes, F.; Ramires, F.J.A.; Ianni, B.M.; Salemi, V.M.C.; Oliveira, A.M.; Pessoa, F.G.; Canzian, M.; Mady, C. Effect of Colchicine on Myocardial Injury Induced by Trypanosoma cruzi in Experimental Chagas Disease. J. Card. Fail. 2012, 18, 654–659. [Google Scholar] [CrossRef] [PubMed]
- Luis, L.; Serrano, M.L.; Hidalgo, M.; Mendoza-León, A. Comparative Analyses of the β-Tubulin Gene and Molecular Modeling Reveal Molecular Insight into the Colchicine Resistance in Kinetoplastids Organisms. BioMed Res. Int. 2013, 2013, e843748. [Google Scholar] [CrossRef] [PubMed]
- Peña-Guerrero, J.; Puig-Rigall, J.; González-Gaitano, G.; Nguewa, P. Chapter 13—Improving the Miltefosine Efficacy against Leishmaniasis by Using Different Nanoassemblies Made from Surfactants or Amphiphilic Antimony (V) Complex. In Applications of Nanobiotechnology for Neglected Tropical Diseases; Formiga, F.R., Inamuddin, Severino, P., Eds.; Academic Press: Cambridge, MA, USA, 2021; pp. 253–290. ISBN 978-0-12-821100-7. [Google Scholar]
- Ismail, A.H.; Al-Garawi, Z.S.; Al-Shamari, K.; Salman, A.T. Metformin Compounds: A Review on the Importance and the Possible Applications. J. Phys. Conf. Ser. 2021, 1853, 012060. [Google Scholar] [CrossRef]
- Navarro, M.; Cisneros-Fajardo, E.J.; Sierralta, A.; Fernández-Mestre, M.; Silva, P.; Arrieche, D.; Marchán, E. Design of Copper DNA Intercalators with Leishmanicidal Activity. J. Biol. Inorg. Chem. 2003, 8, 401–408. [Google Scholar] [CrossRef] [PubMed]
- Rossi, S.; Tudino, V.; Carullo, G.; Butini, S.; Campiani, G.; Gemma, S. Metalloenzyme Inhibitors against Zoonotic Infections: Focus on Leishmania and Schistosoma. ACS Infect. Dis. 2024, 10, 1520–1535. [Google Scholar] [CrossRef]
- Rufino-González, Y.; Ponce-Macotela, M.; García-Ramos, J.C.; Martínez-Gordillo, M.N.; Galindo-Murillo, R.; González-Maciel, A.; Reynoso-Robles, R.; Tovar-Tovar, A.; Flores-Alamo, M.; Toledano-Magaña, Y.; et al. Antigiardiasic Activity of Cu(II) Coordination Compounds: Redox Imbalance and Membrane Damage after a Short Exposure Time. J. Inorg. Biochem. 2019, 195, 83–90. [Google Scholar] [CrossRef] [PubMed]
- Lechuga, G.C.; Pereira, M.C.S.; Bourguignon, S.C. Heme Metabolism as a Therapeutic Target against Protozoan Parasites. J. Drug Target. 2019, 27, 767–779. [Google Scholar] [CrossRef] [PubMed]
- Javed, B.; Raja, N.I.; Nadhman, A.; Mashwani, Z.-R. Understanding the Potential of Bio-Fabricated Non-Oxidative Silver Nanoparticles to Eradicate Leishmania and Plant Bacterial Pathogens. Appl. Nanosci. 2020, 10, 2057–2067. [Google Scholar] [CrossRef]
- Canaparo, R.; Foglietta, F.; Limongi, T.; Serpe, L. Biomedical Applications of Reactive Oxygen Species Generation by Metal Nanoparticles. Materials 2021, 14, 53. [Google Scholar] [CrossRef]
- Kessler, A.; Hedberg, J.; Blomberg, E.; Odnevall, I. Reactive Oxygen Species Formed by Metal and Metal Oxide Nanoparticles in Physiological Media—A Review of Reactions of Importance to Nanotoxicity and Proposal for Categorization. Nanomaterials 2022, 12, 1922. [Google Scholar] [CrossRef]
- Samrot, A.V.; Ram Singh, S.P.; Deenadhayalan, R.; Rajesh, V.V.; Padmanaban, S.; Radhakrishnan, K. Nanoparticles, a Double-Edged Sword with Oxidant as Well as Antioxidant Properties—A Review. Oxygen 2022, 2, 591–604. [Google Scholar] [CrossRef]
- AlGabbani, Q. Nanotechnology: A Promising Strategy for the Control of Parasitic Infections. Exp. Parasitol. 2023, 250, 108548. [Google Scholar] [CrossRef] [PubMed]
- Guerra, R.O.; do Carmo Neto, J.R.; da Silva, P.E.F.; Franco, P.I.R.; Barbosa, R.M.; de Albuquerque Martins, T.; Costa-Madeira, J.; de Assunção, T.S.F.; de Oliveira, C.J.F.; Machado, J.R.; et al. Metallic Nanoparticles and Treatment of Cutaneous Leishmaniasis: A Systematic Review. J. Trace Elem. Med. Biol. 2024, 83, 127404. [Google Scholar] [CrossRef] [PubMed]
- Król, G.; Fortunka, K.; Majchrzak, M.; Piktel, E.; Paprocka, P.; Mańkowska, A.; Lesiak, A.; Karasiński, M.; Strzelecka, A.; Durnaś, B.; et al. Metallic Nanoparticles and Core-Shell Nanosystems in the Treatment, Diagnosis, and Prevention of Parasitic Diseases. Pathogens 2023, 12, 838. [Google Scholar] [CrossRef] [PubMed]
- Almayouf, M.A.; El-khadragy, M.; Awad, M.A.; Alolayan, E.M. The Effects of Silver Nanoparticles Biosynthesized Using Fig and Olive Extracts on Cutaneous Leishmaniasis-Induced Inflammation in Female Balb/c Mice. Biosci. Rep. 2020, 40, BSR20202672. [Google Scholar] [CrossRef] [PubMed]
- Alghamdi, S.Q.; Alotaibi, N.F.; Al-Ghamdi, S.N.; Alqarni, L.S.; Amna, T.; Moustafa, S.M.; Alsohaimi, I.H.; Alruwaili, I.A.; Nassar, A.M. High Antiparasitic and Antimicrobial Performance of Biosynthesized NiO Nanoparticles via Wasted Olive Leaf Extract. Int. J. Nanomed. 2024, 19, 1469–1485. [Google Scholar] [CrossRef] [PubMed]
- Mohammadi, M.; Zaki, L.; KarimiPourSaryazdi, A.; Tavakoli, P.; Tavajjohi, A.; Poursalehi, R.; Delavari, H.; Ghaffarifar, F. Efficacy of Green Synthesized Silver Nanoparticles via Ginger Rhizome Extract against Leishmania Major in Vitro. PLoS ONE 2021, 16, e0255571. [Google Scholar] [CrossRef] [PubMed]
- Faisal, S.; Al-Radadi, N.S.; Jan, H.; Abdullah; Shah, S.A.; Shah, S.; Rizwan, M.; Afsheen, Z.; Hussain, Z.; Uddin, M.N.; et al. Curcuma Longa Mediated Synthesis of Copper Oxide, Nickel Oxide and Cu-Ni Bimetallic Hybrid Nanoparticles: Characterization and Evaluation for Antimicrobial, Anti-Parasitic and Cytotoxic Potentials. Coatings 2021, 11, 849. [Google Scholar] [CrossRef]
- Badirzadeh, A.; Alipour, M.; Najm, M.; Vosoogh, A.; Vosoogh, M.; Samadian, H.; Hashemi, A.S.; Farsangi, Z.J.; Amini, S.M. Potential Therapeutic Effects of Curcumin Coated Silver Nanoparticle in the Treatment of Cutaneous Leishmaniasis Due to Leishmania major in-vitro and in a Murine Model. J. Drug Deliv. Sci. Technol. 2022, 74, 103576. [Google Scholar] [CrossRef]
- Aykur, M.; Göksen Tosun, N.; Kaplan, Ö.; Özgür, A. Efficacy of the Greenly Synthesized Silver, Copper, and Nickel Nanoparticles Using Allium tuncelianum Extract against Acanthamoeba castellanii. J. Drug Deliv. Sci. Technol. 2023, 89, 105013. [Google Scholar] [CrossRef]
- Snoussi, Y.; Sifaoui, I.; Khalil, A.M.; Bhakta, A.K.; Semyonov, O.; Postnikov, P.S.; Michely, L.; Pires, R.; Bastide, S.; Barroso, J.E.-P.; et al. Facile Synthesis of Silver Decorated Biochar as a Novel and Highly Active Biosourced Anti-Kinetoplastid Agent. Mater. Today Commun. 2022, 32, 104126. [Google Scholar] [CrossRef]
- Machado, L.F.; Sanfelice, R.A.; Bosqui, L.R.; Assolini, J.P.; Scandorieiro, S.; Navarro, I.T.; Depieri Cataneo, A.H.; Wowk, P.F.; Nakazato, G.; Bordignon, J.; et al. Biogenic Silver Nanoparticles Reduce Adherence, Infection, and Proliferation of Toxoplasma Gondii RH Strain in HeLa Cells without Inflammatory Mediators Induction. Exp. Parasitol. 2020, 211, 107853. [Google Scholar] [CrossRef]
- Sampath, G.; Chen, Y.-Y.; Rameshkumar, N.; Krishnan, M.; Nagarajan, K.; Shyu, D.J.H. Biologically Synthesized Silver Nanoparticles and Their Diverse Applications. Nanomaterials 2022, 12, 3126. [Google Scholar] [CrossRef]
- Shakeel, M.; Kiani, M.H.; Sarwar, H.S.; Akhtar, S.; Rauf, A.; Ibrahim, I.M.; Ajalli, N.; Shahnaz, G.; Rahdar, A.; Díez-Pascual, A.M. Emulgel-Loaded Mannosylated Thiolated Chitosan-Coated Silver Nanoparticles for the Treatment of Cutaneous Leishmaniasis. Int. J. Biol. Macromol. 2023, 227, 1293–1304. [Google Scholar] [CrossRef]
- Brito, T.K.; Viana, R.L.S.; Moreno, C.J.G.; Barbosa, J.d.S.; Júnior, F.L.d.S.; Medeiros, M.J.C.d.; Melo-Silveira, R.F.; Almeida-Lima, J.; Pontes, D.d.L.; Silva, M.S.; et al. Synthesis of Silver Nanoparticle Employing Corn Cob Xylan as a Reducing Agent with Anti-Trypanosoma cruzi Activity. Int. J. Nanomed. 2020, 15, 965–979. [Google Scholar] [CrossRef]
- Wang, X.; Zhang, D.; Jiang, N.; Wang, X.; Zhang, N.; Zhang, K.; Sang, X.; Feng, Y.; Chen, R.; Yang, N.; et al. Induction of Apoptosis in Trypanosoma brucei Following Endocytosis of Ultra-Small Noble Metal Nanoclusters. Nano Today 2021, 38, 101122. [Google Scholar] [CrossRef]
- Adeyemi, O.S.; Arowolo, A.T.; Hetta, H.F.; Al-Rejaie, S.; Rotimi, D.; Batiha, G.E.-S. Apoferritin and Apoferritin-Capped Metal Nanoparticles Inhibit Arginine Kinase of Trypanosoma Brucei. Molecules 2020, 25, 3432. [Google Scholar] [CrossRef]
- Hu, X.; Zhang, Y.; Ding, T.; Liu, J.; Zhao, H. Multifunctional Gold Nanoparticles: A Novel Nanomaterial for Various Medical Applications and Biological Activities. Front. Bioeng. Biotechnol. 2020, 8, 990. [Google Scholar] [CrossRef]
- Jimenez-Falcao, S.; Méndez-Arriaga, J.M.; García-Almodóvar, V.; García-Valdivia, A.A.; Gómez-Ruiz, S. Gold Nanozymes: Smart Hybrids with Outstanding Applications. Catalysts 2023, 13, 13. [Google Scholar] [CrossRef]
- Want, M.Y.; Yadav, P.; Khan, R.; Chouhan, G.; Islamuddin, M.; Aloyouni, S.Y.; Chattopadhyay, A.P.; AlOmar, S.Y.; Afrin, F. Critical Antileishmanial In Vitro Effects of Highly Examined Gold Nanoparticles. Int. J. Nanomed. 2021, 16, 7285–7295. [Google Scholar] [CrossRef]
- Raj, S.; Sasidharan, S.; Tripathi, T.; Saudagar, P. Biofunctionalized Chrysin-Conjugated Gold Nanoparticles Neutralize Leishmania Parasites with High Efficacy. Int. J. Biol. Macromol. 2022, 205, 211–219. [Google Scholar] [CrossRef]
- Sasidharan, S.; Saudagar, P. Gold and Silver Nanoparticles Functionalized with 4′,7-Dihydroxyflavone Exhibit Activity against Leishmania donovani. Acta Trop. 2022, 231, 106448. [Google Scholar] [CrossRef]
- Alti, D.; Veeramohan Rao, M.; Rao, D.N.; Maurya, R.; Kalangi, S.K. Gold–Silver Bimetallic Nanoparticles Reduced with Herbal Leaf Extracts Induce ROS-Mediated Death in Both Promastigote and Amastigote Stages of Leishmania donovani. ACS Omega 2020, 5, 16238–16245. [Google Scholar] [CrossRef]
- Ruang-areerate, T.; Sukphattanaudomchoke, C.; Thita, T.; Leelayoova, S.; Piyaraj, P.; Mungthin, M.; Suwannin, P.; Polpanich, D.; Tangchaikeeree, T.; Jangpatarapongsa, K.; et al. Development of Loop-Mediated Isothermal Amplification (LAMP) Assay Using SYBR Safe and Gold-Nanoparticle Probe for Detection of Leishmania in HIV Patients. Sci. Rep. 2021, 11, 12152. [Google Scholar] [CrossRef]
- Martins, B.R.; Barbosa, Y.O.; Andrade, C.M.R.; Pereira, L.Q.; Simão, G.F.; de Oliveira, C.J.; Correia, D.; Oliveira, R.T.S.; da Silva, M.V.; Silva, A.C.A.; et al. Development of an Electrochemical Immunosensor for Specific Detection of Visceral Leishmaniasis Using Gold-Modified Screen-Printed Carbon Electrodes. Biosensors 2020, 10, 81. [Google Scholar] [CrossRef]
- Alanazi, A.D.; Alnomasy, S.F. Immunomodulatory, Antioxidant, and Anti-Inflammatory Activities of Green Synthesized Copper Nanoparticles for Treatment of Chronic Toxoplasma gondii Infection. Pharmaceuticals 2023, 16, 1574. [Google Scholar] [CrossRef]
- Ruda, D.A.; Al-Karam, L.Q.; Ghadhban, E. The Effect of Calcination Temperature and Solvent on the Synthesis of CuO Nanoparticles and Assessment as an Anti-Leishmania Agent. AIP Conf. Proc. 2019, 2190, 020067. [Google Scholar] [CrossRef]
- Iqbal, J.; Abbasi, B.A.; Ahmad, R.; Mahmoodi, M.; Munir, A.; Zahra, S.A.; Shahbaz, A.; Shaukat, M.; Kanwal, S.; Uddin, S.; et al. Phytogenic Synthesis of Nickel Oxide Nanoparticles (NiO) Using Fresh Leaves Extract of Rhamnus Triquetra (Wall.) and Investigation of Its Multiple In Vitro Biological Potentials. Biomedicines 2020, 8, 117. [Google Scholar] [CrossRef]
- Khalil, A.T.; Ovais, M.; Ullah, I.; Ali, M.; Shinwari, Z.K.; Hassan, D.; Maaza, M. Sageretia Thea (Osbeck.) Modulated Biosynthesis of NiO Nanoparticles and Their in Vitro Pharmacognostic, Antioxidant and Cytotoxic Potential. Artif. Cells Nanomed. Biotechnol. 2018, 46, 838–852. [Google Scholar] [CrossRef]
- Mohan, S.; Srivastava, P.; Maheshwari, S.N.; Sundar, S.; Prakash, R. Nano-Structured Nickel Oxide Based DNA Biosensor for Detection of Visceral Leishmaniasis (Kala-Azar). Analyst 2011, 136, 2845–2851. [Google Scholar] [CrossRef]
- Saleh, F.; Kheirandish, F.; Abbasi, M.; Ahmadpour, F.; Veiskarami, S.; Mirderikvand, A. Comparison of Biosynthetic Zinc Oxide Nanoparticle and Glucantime Cytotoxic Effects on Leishmania major (MRHO/IR/75/ER). J. Basic Microbiol. 2024, 64, 2300490. [Google Scholar] [CrossRef]
- Mahmoudi, M.; Shabani, M.; Dehdast, S.A.; Saberi, S.; Elmi, T.; Chiari Fard, G.; Tabatabaie, F.; Akbari, S. The Characterization and Antileishmanial Evaluation on Leishmania Major with Chitosan/Zno Bio-Nanocomposite as Drug Delivery Systems. Nanomed. Res. J. 2022, 7, 140–149. [Google Scholar] [CrossRef]
- Nadhman, A.; Nazir, S.; Ihsanullah Khan, M.; Arooj, S.; Bakhtiar, M.; Shahnaz, G.; Yasinzai, M. PEGylated Silver Doped Zinc Oxide Nanoparticles as Novel Photosensitizers for Photodynamic Therapy against Leishmania. Free Radic. Biol. Med. 2014, 77, 230–238. [Google Scholar] [CrossRef]
- Jan, H.; Shah, M.; Usman, H.; Khan, M.A.; Zia, M.; Hano, C.; Abbasi, B.H. Biogenic Synthesis and Characterization of Antimicrobial and Antiparasitic Zinc Oxide (ZnO) Nanoparticles Using Aqueous Extracts of the Himalayan Columbine (Aquilegia pubiflora). Front. Mater. 2020, 7, 249. [Google Scholar] [CrossRef]
- Khashan, K.S.; Sulaiman, G.M.; Hussain, S.A.; Marzoog, T.R.; Jabir, M.S. Synthesis, Characterization and Evaluation of Anti-Bacterial, Anti-Parasitic and Anti-Cancer Activities of Aluminum-Doped Zinc Oxide Nanoparticles. J. Inorg. Organomet. Polym. 2020, 30, 3677–3693. [Google Scholar] [CrossRef]
- Hamdy, D.A.; Ismail, M.A.M.; El-Askary, H.M.; Abdel-Tawab, H.; Ahmed, M.M.; Fouad, F.M.; Mohamed, F. Newly Fabricated Zinc Oxide Nanoparticles Loaded Materials for Therapeutic Nano Delivery in Experimental Cryptosporidiosis. Sci. Rep. 2023, 13, 19650. [Google Scholar] [CrossRef]
- Albalawi, A.E.; Shater, A.F.; Alanazi, A.D.; Almohammed, H.I. Unveiling of the Antileishmanial Activities of Linalool Loaded Zinc Oxide Nanocomposite through Its Potent Antioxidant and Immunomodulatory Effects. Acta Trop. 2024, 252, 107155. [Google Scholar] [CrossRef]
- Nazir, S.; Rabbani, A.; Mehmood, K.; Maqbool, F.; Shah, G.M.; Khan, M.F.; Sajid, M. Antileishmanial Activity and Cytotoxicity of ZnO-Based Nano-Formulations. Int. J. Nanomed. 2019, 14, 7809–7822. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).