The Efficacy of Erbium-Ion, Diode, and CO2 Lasers in Debonding Attachments Used During Overlay Orthodontic Treatment and the Risk of Hard Tooth Tissue Damage Compared to Traditional Methods—An In Vitro Study
Abstract
1. Introduction
2. Materials and Methods
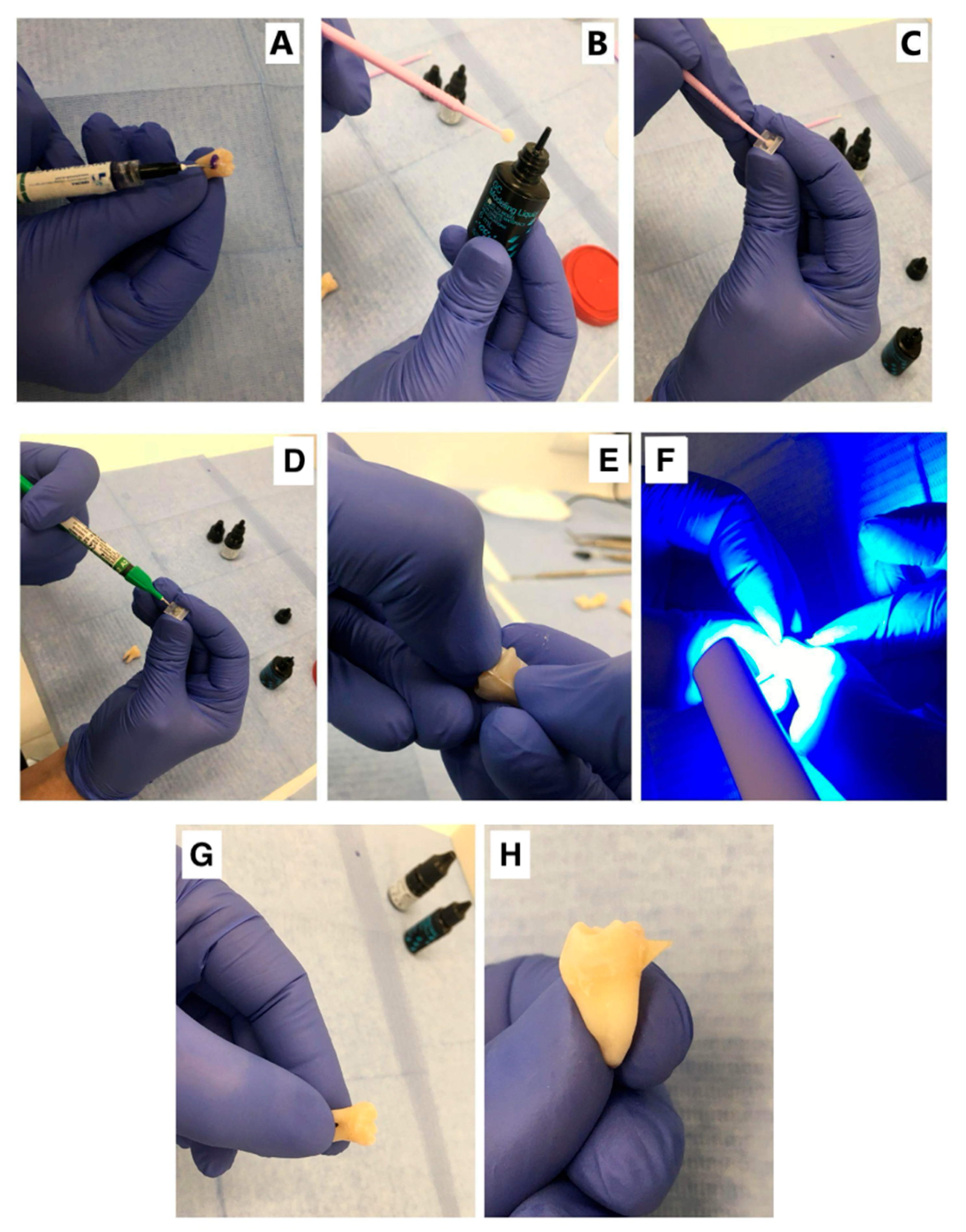
2.1. Sample Preparation
2.2. Study Groups
- Control (Reference) Group (n = 10)
- Group RT (n = 10): Attachment removal was performed using rotary tools (RT). Specimens in the RT group were prepared using Drill New Technology instruments (Edenta Etbl, Au SG, Switzerland). A tungsten carbide drill for contra-angle handpieces, with a short, rounded cone, was used in combination with a W&H Synea Fusion dental handpiece (Austria) operating at 40,000 rpm with water spray.
- Group D (n = 10): Attachment debonding was carried out using a semiconductor diode laser (SMARTm PRO, Lasotronix, Piaseczno, Poland). The laser operated in pulsed mode with an average power of 3.4 W, an impulse time of 500 µs, and a recess time of 80 µs. It emitted a wavelength of 980 nm, with the pilot beam set to 10% power. The exposure duration was 11 s, and energy was delivered through a 300 µm spot diameter, totaling 37 J. Based on these parameters, the estimated fluence was 52,336 J/cm2, and the irradiance was 4811 W/cm2.
- Group C (n = 10): Attachment debonding was performed using a CO2 laser (ADSS model FG 900S, ADSS Group Development Co. Ltd., Beijing, China). Each abutment was irradiated perpendicularly at the margin, targeting the composite near the attachment site. The laser operated in pulsed mode at 3 W, with a 10 ms pulse time, 10 ms pause time, and a frequency of 50 Hz. A 635 nm red diode pilot beam (<2 mW) was used for aiming. Irradiation was performed in spot mode with 1 mm spacing to ensure uniform coverage. Assuming a typical spot diameter of 500 µm, the irradiance was estimated at 1531 W/cm2. Fluence was not calculated due to the absence of total exposure time.
- Group E (n = 10): Attachment debonding was performed using an Er:YAG laser (LiteTouch, Light Instruments Ltd., Yokne’am, Israel). This ablative fractional laser emits a focused beam at a wavelength of 2940 nm, which is highly absorbed in water, allowing for efficient ablation with minimal scatter and shallow penetration (within tens of micrometres). The laser’s core consists of an erbium-doped yttrium aluminum garnet crystal, activated by a xenon lamp. A 3.0 W beam was applied in two 10-s sequences, delivering 200 mJ per pulse at a frequency of 15 Hz. Irradiation was precisely directed along the attachment edge at 1 mm intervals. For a 900 µm spot diameter, the estimated fluence was 31.45 J/cm2, and irradiance was 471.7 W/cm2.
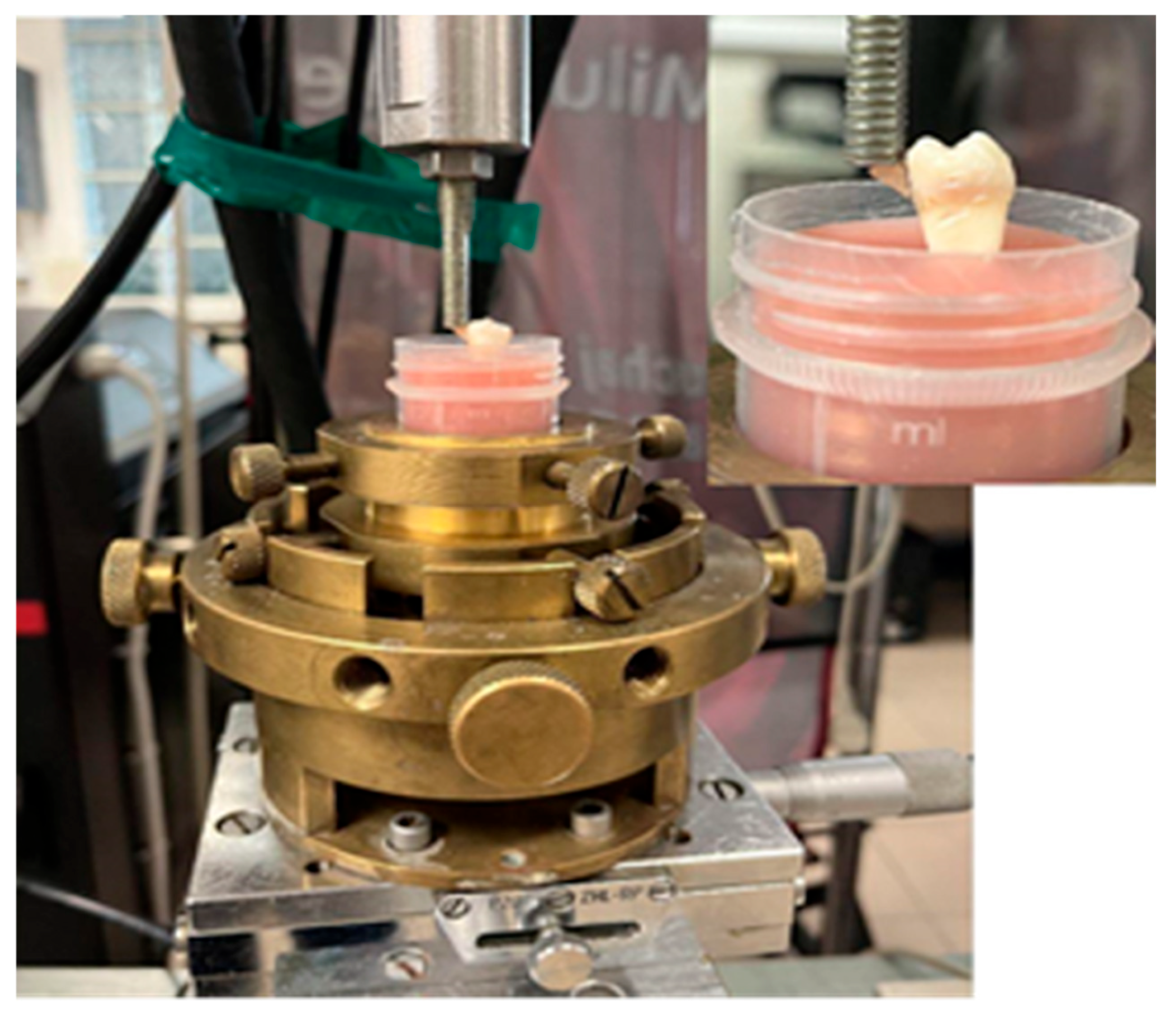
2.3. The Shear Test
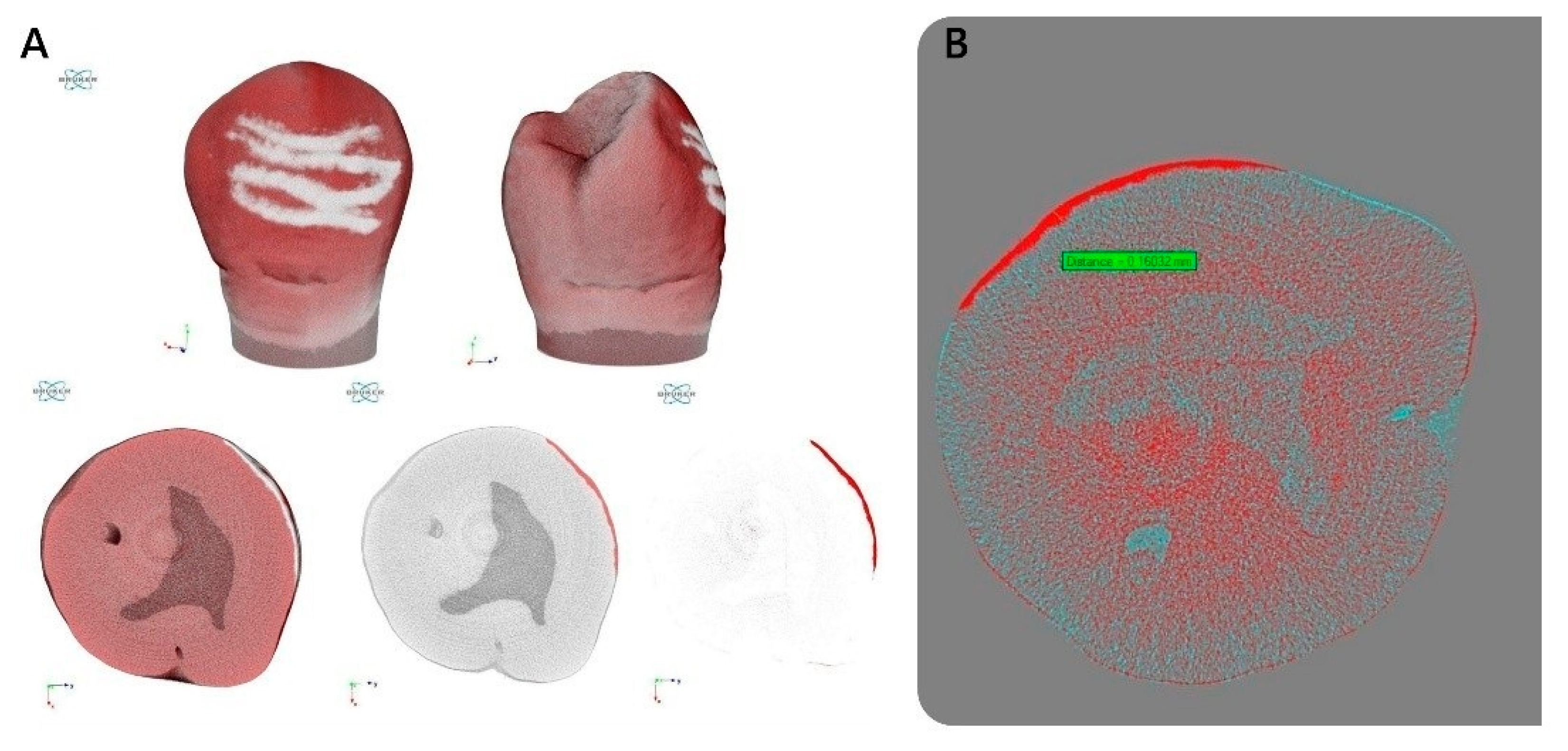
2.4. High-Resolution X-Ray Micro-Computed Tomography
2.5. Optical Profilometry
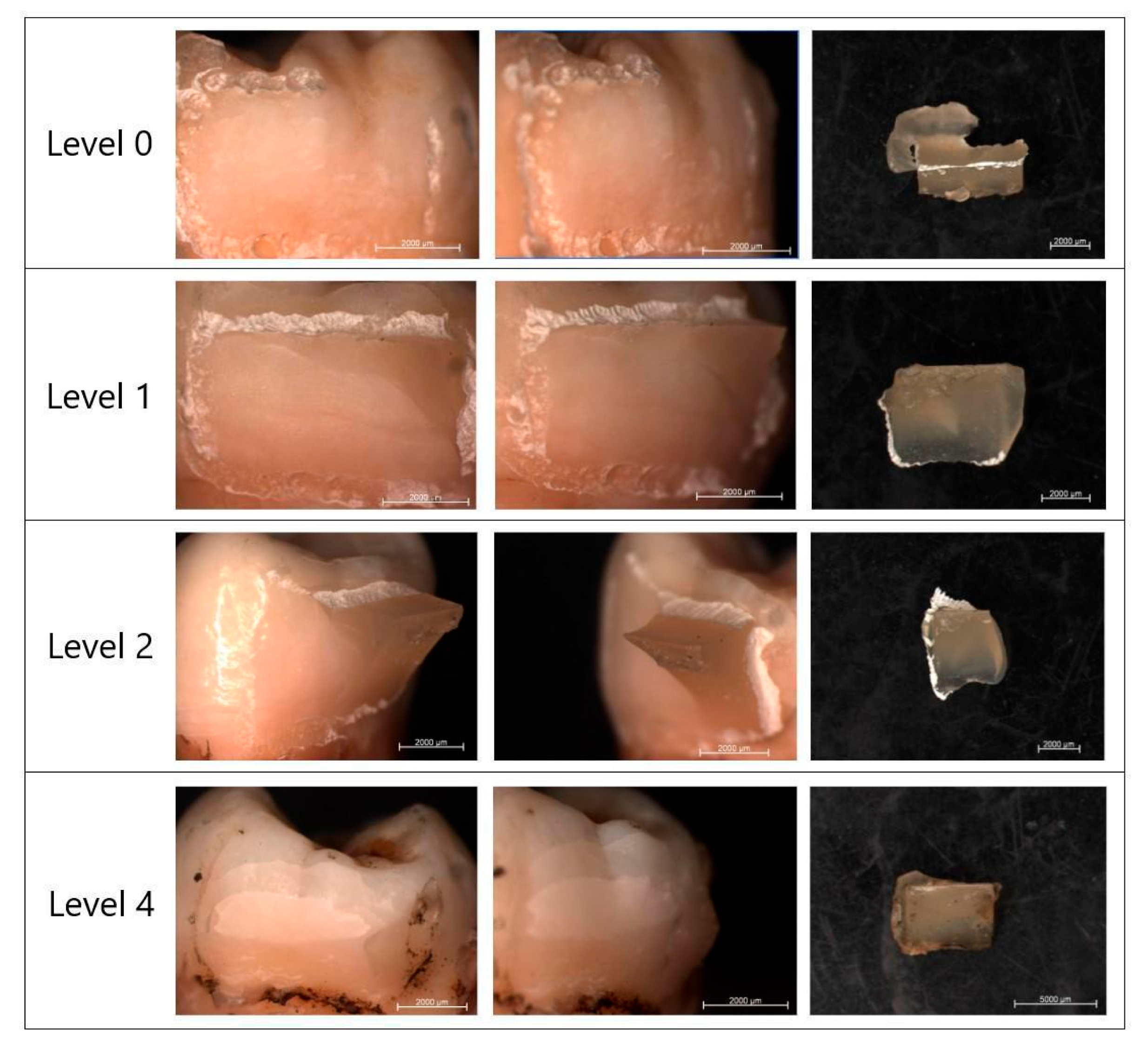
2.6. Evaluation of Adhesive Remnant (ARI) Score
2.7. Statistical Analysis
3. Results
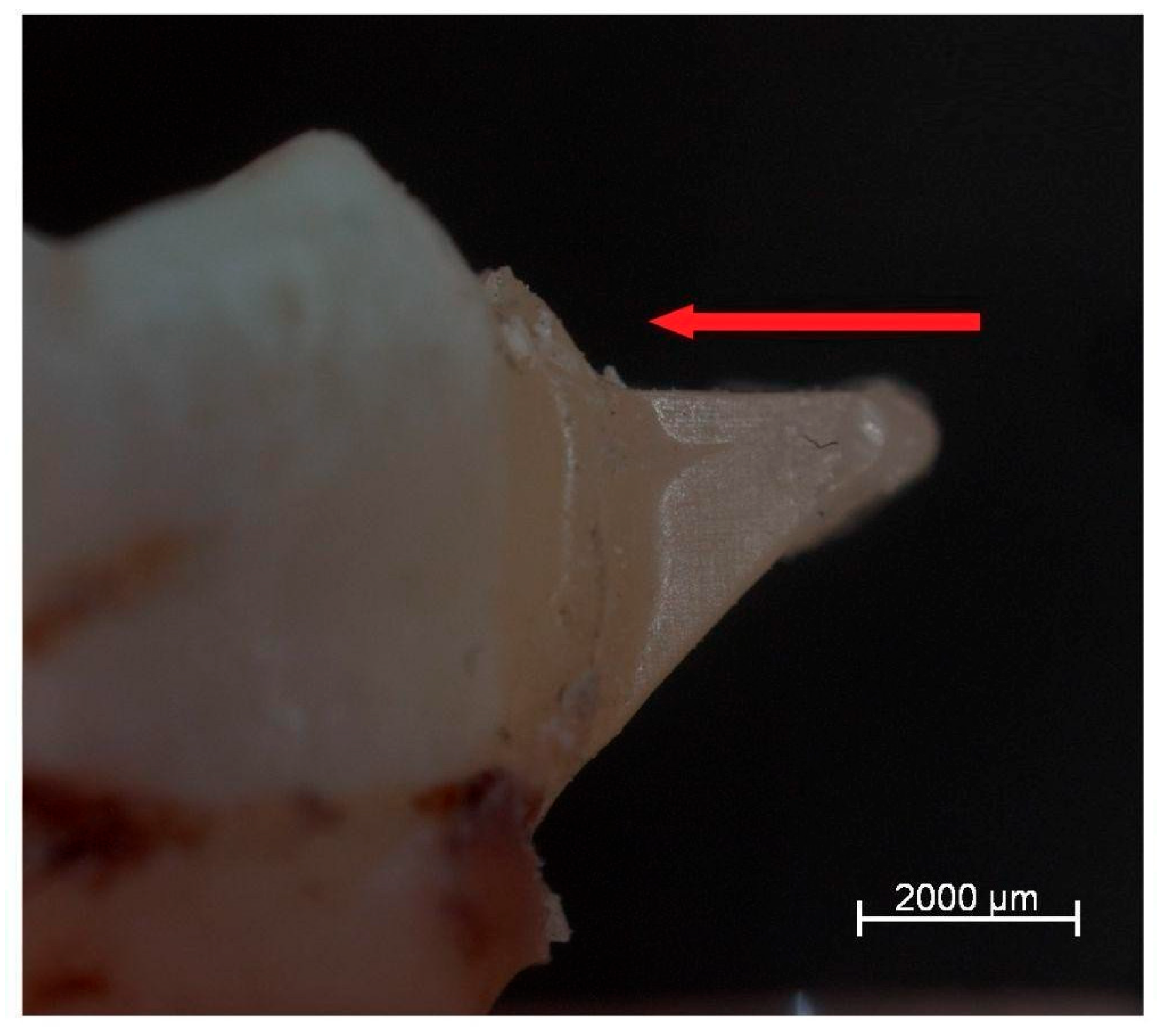
3.1. Effect of Laser Application on Enamel Microstructure (Micro-CT Analysis)
3.2. Surface Roughness Analysis (Optical Profilometry)
3.3. Shear Bond Strength of Attachments to Enamel
3.4. Morphological Evaluation of Enamel Surfaces After Attachment Removal
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Grassia, V.; Fiori, A.; Diodati, F.; Sayahpour, B.; Jamilian, A.; Armogida, N.G.; d’Apuzzo, F.; Nucci, L. Clear aligners: A network and bibliometric analysis of 50 pivotal articles. Dent. Med. Probl. 2025, 62, 161–171. [Google Scholar] [CrossRef]
- Hong, K.; Kim, W.-H.; Eghan-Acquah, E.; Lee, J.-H.; Lee, B.-K.; Kim, B. Efficient Design of a Clear Aligner Attachment to Induce Bodily Tooth Movement in Orthodontic Treatment Using Finite Element Analysis. Materials 2021, 14, 4926. [Google Scholar] [CrossRef]
- Ju, G.-Y.; Oh, S.; Lim, B.-S.; Lee, H.-S.; Chung, S.H. Effect of Simplified Bonding on Shear Bond Strength between Ceramic Brackets and Dental Zirconia. Materials 2019, 12, 1640. [Google Scholar] [CrossRef]
- Bae, G.-S. Clinical limitations and its solutions of the clear overlay appliance treatment. J. Korean Dent. Assoc. 2016, 54, 563–574. [Google Scholar] [CrossRef]
- Behnaz, M.; Farahnaki, A.; Rahimipour, K.; Mousavi, R.; Davoodi, N.S. Lingual Orthodontic Treatment: Efficacy and Complications. J. Adv. Oral Res. 2019, 10, 65–74. [Google Scholar] [CrossRef]
- Boyd, R.L. Esthetic Orthodontic Treatment Using the Invisalign Appliance for Moderate to Complex Malocclusions. J. Dent. Educ. 2008, 72, 948–967. [Google Scholar] [CrossRef]
- Breece, G.L.; Nieberg, L.G. Motivations for Adult Orthodontic Treatment. J. Clin. Orthod. 1986, 20, 166–171. [Google Scholar]
- Kim, H.; Choi, B.; Lim, S.; Gang, S. A Comparative Study about Bonding Strength of Customized Metalbase for Lingual Orthodontic Appliance Made by Non-Precious Metal. Oral Biol. Res. 2016, 40, 187–192. [Google Scholar]
- Kravitz, N.D.; Kusnoto, B.; BeGole, E.; Obrez, A.; Agran, B. How Well Does Invisalign Work? A Prospective Clinical Study Evaluating the Efficacy of Tooth Movement with Invisalign. Am. J. Orthod. Dentofac. Orthop. 2009, 135, 27–35. [Google Scholar] [CrossRef]
- Elkharashi, A.; Grzech-Leśniak, K.; Deeb, J.G.; Abdulmajeed, A.A.; Bencharit, S. Exploring the use of pulsed erbium lasers to retrieve a zirconia crown from a zirconia implant abutment. PLoS ONE 2020, 15, e0233536. [Google Scholar] [CrossRef]
- Lizarelli, R.D.F.; Moriyama, L.T.; Bagnato, V.S. Ablation of Composite Resins Using Er:YAG Laser—Comparison with Enamel and Dentin. Lasers Surg. Med. 2003, 33, 132–139. [Google Scholar] [CrossRef] [PubMed]
- McNamara, J.A.; Kramer, K.L.; Juenker, J.P. Invisible Retainers. J. Clin. Orthod. 1985, 19, 570–578. [Google Scholar] [PubMed]
- Meier, B.; Wiemer, K.B.; Miethke, R.-R. Invisalign--Patient Profiling. Analysis of a Prospective Survey. J. Orofac. Orthop. Der Kieferorthopadie 2003, 64, 352–358. [Google Scholar] [CrossRef] [PubMed]
- Melsen, B. Northcroft Lecture: How Has the Spectrum of Orthodontics Changed over the Past Decades? J. Orthod. 2011, 38, 134–143. [Google Scholar] [CrossRef]
- Locadia, M.; Sprangers, M. Kwaliteit van Leven. In Medische Psychologie; Bohn Stafleu van Loghum: Houten, The Netherlands, 2006; pp. 155–160. ISBN 978-90-313-4462-8. [Google Scholar]
- Lascala, N.; Moussalli, N. Laser Therapy in Periodontics. In Periodontal Therapeutic Compendium, 3rd ed.; Artes Médicas: São Paulo, Brazil, 1999; pp. 293–307. [Google Scholar]
- Rahimipour, K.; Mousavi, R.; Behnaz, M.; Dalaie, K.; Farahnaki, A.; Davoodi, N.S. Invisalign Orthodontic System: Treatment Efficacy, Complications, Patients’ Attitude. Orthod. Forum 2020, 15, 108–123. [Google Scholar] [CrossRef]
- Reinisch, L. Laser Physics and Tissue Interactions. Otolaryngol. Clin. N. Am. 1996, 29, 893–914. [Google Scholar] [CrossRef]
- Deeb, J.G.; Grzech-Leśniak, K.; Weaver, C.; Matys, J.; Bencharit, S. Retrieval of Glass Fiber Post Using Er:YAG Laser and Conventional Endodontic Ultrasonic Method: An In Vitro Study. J. Prosthodont. 2019, 28, 1024–1028. [Google Scholar] [CrossRef]
- Ryf, S.; Flury, S.; Palaniappan, S.; Lussi, A.; van Meerbeek, B.; Zimmerli, B. Enamel loss and adhesive remnants following bracket removal and various clean-up procedures in vitro. Eur. J. Orthod. 2012, 34, 25–32. [Google Scholar] [CrossRef]
- Deeb, J.G.; Skrjanc, L.; Kanduti, D.; Carrico, C.; Saturno, A.M.; Grzech-Leśniak, K. Evaluation of Er:YAG and Er,Cr:YSGG laser irradiation for the debonding of prefabricated zirconia crowns. Adv. Clin. Exp. Med. 2021, 30, 7–15. [Google Scholar] [CrossRef]
- Ireland, A.J.; Hosein, I.; Sherriff, M. Enamel loss at bond-up, debond and clean-up following the use of a conventional light-cured composite and a resin-modified glass polyalkenoate cement. Eur. J. Orthod. 2005, 27, 413–419. [Google Scholar] [CrossRef]
- Deeb, J.G.; Grzech-Leśniak, K.; Brody, E.R.; Matys, J.; Bencharit, S. Erbium Laser-assisted Ceramic Debonding: A Scoping Review. J. Prosthodont. 2022, 31, E100–E124. [Google Scholar] [CrossRef] [PubMed]
- Nelson, J.S.; Yow, L.; Liaw, L.H.; Macleay, L.; Zavar, R.B.; Orenstein, A.; Wright, W.H.; Andrews, J.J.; Berns, M.W. Ablation of Bone and Methacrylate by a Prototype Mid-Infrared Erbium:YAG Laser. Lasers Surg. Med. 1988, 8, 494–500. [Google Scholar] [CrossRef] [PubMed]
- Niemz, M.H. Laser-Tissue Interactions: Fundamentals and Applications, 4th ed.; Springer International Publishing AG: Cham, Switzerland, 2019; ISBN 978-3-030-11917-1. [Google Scholar]
- Oztoprak, M.O.; Nalbantgil, D.; Erdem, A.S.; Tozlu, M.; Arun, T. Debonding of Ceramic Brackets by a New Scanning Laser Method. Am. J. Orthod. Dentofac. Orthop. 2010, 138, 195–200. [Google Scholar] [CrossRef] [PubMed]
- Oztoprak, M.O.; Tozlu, M.; Iseri, U.; Ulkur, F.; Arun, T. Effects of Different Application Durations of Scanning Laser Method on Debonding Strength of Laminate Veneers. Lasers Med. Sci. 2012, 27, 713–716. [Google Scholar] [CrossRef]
- Glinkowski, W.; Pokora, L. Lasery w Terapii; Laser Instruments-Centrum Techniki Laserowej: Warszawa, Poland, 1993. [Google Scholar]
- Niemz, M.H. Laser–Tissure Interactions—Fundamentals and Applications, 3rd ed.; Springer Press: Heidelberg, Germany, 2003. [Google Scholar]
- Kuhn, K.; Schmid, C.U.; Luthardt, R.G.; Rudolph, H.; Diebolder, R. Er:YAG laser-induced damage to a dental composite in simulated clinical scenarios for inadvertent irradiation: An in vitro study. Lasers Med. Sci. 2022, 37, 1017–1030. [Google Scholar] [CrossRef]
- Yang, X.; Ye, S.; Wei, B.; Zeng, L. Removal of resin cement using a picosecond laser: An in vitro study. J. Prosthet. Dent. 2025, 133, 1058.e1–1058.e9. [Google Scholar] [CrossRef]
- Yassaei, S.; Aghili, H.; Joshan, N. Effects of Removing Adhesive from Tooth Surfaces by Er:YAG Laser and a Composite Bur on Enamel Surface Roughnessand Pulp Chamber Temperature. Dent. Res. J. 2015, 12, 254–259. [Google Scholar]
- Ajwa, N.; Alfayez, H.; Al-Oqab, H.; Melibary, R.; Alzamil, Y. The Effect of Erbium-Doped Yttrium Aluminum Garnet Laser in Debonding of Orthodontic Brackets: A Systematic Review of the Literature. Photobiomodulation Photomed. Laser Surg. 2021, 39, 725–733. [Google Scholar] [CrossRef]
- Khalil, A.S.; Tamish, N.M.; Elkalza, A.R. Assessment of Chemical, Ultrasonic, Diode Laser, and Er:YAG Laser Application on Debonding of Ceramic Brackets. BMC Oral Health 2022, 22, 79. [Google Scholar] [CrossRef]
- Rechmann, P.; Buu, N.C.H.; Rechmann, B.M.T.; Le, C.Q.; Finzen, F.C.; Featherstone, J.D.B. Laser All-Ceramic Crown Removal-a Laboratory Proof-of-Principle Study-Phase 1 Material Characteristics. Lasers Surg. Med. 2014, 46, 628–635. [Google Scholar] [CrossRef]
- Michalak, M.; Kiryk, S.; Kotela, A.; Wiśniewska, K.; Kiryk, J.; Zborowski, J.Z.; Matys, J.; Dobrzyński, M. Orthodontic Ceramic Bracket Removal Using Lasers: A Systematic Review. J. Funct. Biomater. 2025, 16, 123. [Google Scholar] [CrossRef] [PubMed]
- Paolone, G.; Mandurino, M.; Baldani, S.; Paolone, M.G.; Goracci, C.; Scolavino, S.; Gherlone, E.; Cantatore, G.; Gastaldi, G. Quantitative Volumetric Enamel Loss after Orthodontic Debracketing/Debonding and Clean-Up Procedures: A Systematic Review. Appl. Sci. 2023, 13, 5369. [Google Scholar] [CrossRef]
- Zheng, X.; Huang, X. Evaluation of the Re-Bond Strength of Debonded Metal and Ceramic Brackets Following Er: YAG Laser Treatment. BMC Oral Health 2024, 24, 710. [Google Scholar] [CrossRef] [PubMed]
- De Souza Henkin, F.; Macêdo, E.; da Silva Santos, K.; Schwarzbach, M.; Samuel, S.M.W.; Mundstock, K.S. In Vitro Analysis of Shear Bond Strength and Adhesive Remnant Index of Different Metal Brackets. Dent. Press J. Orthod. 2016, 21, 67–73. [Google Scholar] [CrossRef]
- Grzech-Leśniak, K.; Matys, J.; Żmuda-Stawowiak, D.; Mroczka, K.; Dominiak, M.; Brugnera Junior, A.; Gruber, R.; Romanos, G.E.; Sculean, A. Er:YAG Laser for Metal and Ceramic Bracket Debonding: An In Vitro Study on Intrapulpal Temperature, SEM, and EDS Analysis. Photomed. Laser Surg. 2018, 36, 595–600. [Google Scholar] [CrossRef]
- Indumathi, G.; Premkumar, S.; Amit, K. Assessment of Enamel Loss After Debonding of Ceramic, Composite Plastic And Metal Brackets-An In Vitro Study. J. Contemp. Orthod. 2019, 3, 1–10. [Google Scholar] [CrossRef]
- Vidor, M.M.; Felix, R.P.; Marchioro, E.M.; Hahn, L. Enamel Surface Evaluation after Bracket Debonding and Different Resin Removal Methods. Dent. Press J. Orthod. 2015, 20, 61–67. [Google Scholar] [CrossRef]
- Tocchio, R.M.; Williams, P.T.; Mayer, F.J.; Standing, K.G. Laser Debonding of Ceramic Orthodontic Brackets. Am. J. Orthod. Dentofac. Orthop. 1993, 103, 155–162. [Google Scholar] [CrossRef]
- Kiryk, J.; Matys, J.; Nikodem, A.; Burzyńska, K.; Grzech-Leśniak, K.; Dominiak, M.; Dobrzyński, M. The Effect of Er:YAG Laser on Shear Bond Strength of Orthodontic Brackets to Enamel—A Preliminary Study. Materials 2021, 14, 2093. [Google Scholar] [CrossRef]
- Chan, K.H.; Hirasuna, K.; Fried, D. Analysis of Enamel Surface Damage after Selective Laser Ablation of Composite from Tooth Surfaces. Photonics Lasers Med. 2014, 3, 37–45. [Google Scholar] [CrossRef]
- Obata, A.; Tsumura, T.; Niwa, K.; Ashizawa, Y.; Deguchi, T.; Ito, M. Super Pulse CO2 Laser for Bracket Bonding and Debonding. Eur. J. Orthod. 1999, 21, 193–198. [Google Scholar] [CrossRef] [PubMed]
- Dostalova, T.; Jelinkova, H.; Remes, M.; Šulc, J.; Němec, M. The Use of the Er:YAG Laser for Bracket Debonding and Its Effect on Enamel Damage. Photomed. Laser Surg. 2016, 34, 394–399. [Google Scholar] [CrossRef] [PubMed]
- Fried, W.A.; Chan, K.H.; Darling, C.L.; Fried, D. Use of a DPSS Er:YAG Laser for the Selective Removal of Composite from Tooth Surfaces. Biomed. Opt. Express 2018, 9, 5026–5036. [Google Scholar] [CrossRef] [PubMed]
- Almeida, H.C.; Vedovello Filho, M.; Vedovello, S.A.; Young, A.A.A.; Ramirez-Yanez, G.O. ER: YAG Laser for Composite Removal after Bracket Debonding: A Qualitative SEM Analysis. Int. J. Orthod. 2009, 20, 9–13. [Google Scholar]
- Mousa, M.M.; Al-Jannan, H.M.G.; Sultan, K.; Ajaj, M.A.; Hajeer, M.Y.; Al-Manadili, A.; Ammar, A.M.; Awawdeh, M. Effectiveness of Two Intensity Levels of Diode Laser in Debonding Metallic Brackets Regarding Enamel Surface Integrity and Pulpal Temperature: An Ex-Vivo Study. Cureus 2023, 15, e41372. [Google Scholar] [CrossRef]
- Matys, J.; Grzech-Leśniak, K.; Flieger, R.; Dominiak, M. Assessment of an Impact of a Diode Laser Mode with Wavelength of 980 Nm on a Temperature Rise Measured by Means of K-02 Thermocouple: Preliminary Results. Dent. Med. Probl. 2016, 53, 345–351. [Google Scholar] [CrossRef]
- Morford, C.K.; Buu, N.C.H.; Rechmann, B.M.T.; Finzen, F.C.; Sharma, A.B.; Rechmann, P. Er:YAG Laser Debonding of Porcelain Veneers. Lasers Surg. Med. 2011, 43, 965–974. [Google Scholar] [CrossRef]
- Chan, K.H.; Hirasuna, K.; Fried, D. Rapid and Selective Removal of Composite from Tooth Surfaces with a 9.3 µm CO2 Laser Using Spectral Feedback. Lasers Surg. Med. 2011, 43, 824–832. [Google Scholar] [CrossRef]
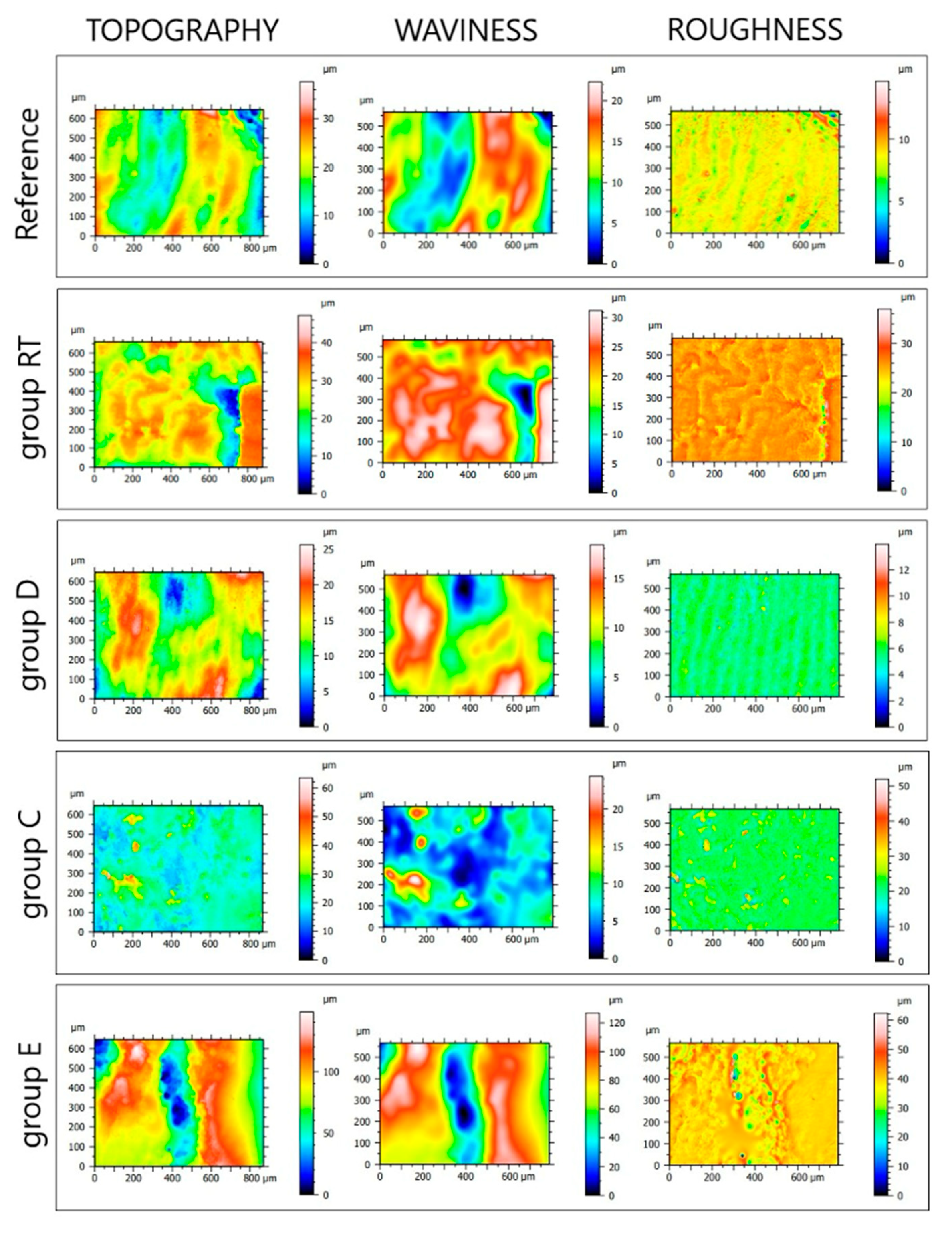
| Roughness Parameters | Reference | RT | Group D | Group C | Group E | p-Value |
|---|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | ||
| Sa [µm] | 0.28 ± 0.04 | 0.31 ± 0.08 | 0.30 ± 0.03 | 0.79 ± 0.06 | 2.04 ± 0.08 | <0.05 for CvsE; C, EvsReference, RT, D |
| Sq [µm] | 0.39 ± 0.05 | 0.46 ± 0.14 | 0.42 ± 0.04 | 1.24 ± 0.10 | 4.19 ± 0.12 | <0.05 for CvsE; C, EvsReference, RT, D |
| Sz [µm] | 11.49 ± 3.84 | 27.44 ± 17.33 | 11.53 ± 3.61 | 43.30 ± 3.23 * | 251.21 ± 3.23 * | <0.05 for CvsE; C, EvsReference, RT, D; RTvsReference, D |
| Sp [µm] | 6.71 ± 3.40 | 9.02 ± 6.99 | 6.79 ± 2.34 | 20.49 ± 0.37 * | 125.79 ± 1.17 * | <0.05 for CvsE; C, EvsReference, RT, D |
| Sv [µm] | 4.78 ± 1.23 | 18.44 ± 20.88 | 4.74 ± 1.26 | 22.80 ± 3.13 * | 125.42 ± 2.06 * | <0.05 for CvsE; C, EvsReference, RT, D; RTvsReference, D |
| Mechanical Parameters | τ [MPa] | F [N] | l [mm] | p-Value |
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | ||
| Reference | 196.189 ± 75.29 | 15.189 ± 4.57 | 0.637 ± 0.21 | <0.05 |
| Group D | 126.008 ± 80.58 | 9.764 ± 6.06 | 0.413 ± 0.28 | <0.05 |
| Group C | 116.360 ± 43.26 * | 9.292 ± 3.36 | 0.400 ± 0.13 * | <0.05 |
| Group E | 81.679 ± 45.52 * | 6.080 ± 2.97 * | 0.294 ± 0.13 * | <0.05 |
| p-value | <0.05 for C; EvsReference, EvsC, D | <0.05 for C; EvsReference, EvsC, D | <0.05 for C; EvsReference, EvsC, D | - |
| ARI Score | 0 | 1 | 2 | 3 | 4 |
|---|---|---|---|---|---|
| Reference | 25% | 38% | 19% | 0% | 19% |
| Group D | 20% | 67% | 7% | 0% | 7% |
| Group C | 33% | 33% | 33% | 0% | 0% |
| Group E | 67% | 11% | 22% | 0% | 0% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Florczak-Matyjek, A.; Nikodem, A.; Kensy, J.; Matys, J.; Grzech-Leśniak, K. The Efficacy of Erbium-Ion, Diode, and CO2 Lasers in Debonding Attachments Used During Overlay Orthodontic Treatment and the Risk of Hard Tooth Tissue Damage Compared to Traditional Methods—An In Vitro Study. Photonics 2025, 12, 621. https://doi.org/10.3390/photonics12060621
Florczak-Matyjek A, Nikodem A, Kensy J, Matys J, Grzech-Leśniak K. The Efficacy of Erbium-Ion, Diode, and CO2 Lasers in Debonding Attachments Used During Overlay Orthodontic Treatment and the Risk of Hard Tooth Tissue Damage Compared to Traditional Methods—An In Vitro Study. Photonics. 2025; 12(6):621. https://doi.org/10.3390/photonics12060621
Chicago/Turabian StyleFlorczak-Matyjek, Alina, Anna Nikodem, Julia Kensy, Jacek Matys, and Kinga Grzech-Leśniak. 2025. "The Efficacy of Erbium-Ion, Diode, and CO2 Lasers in Debonding Attachments Used During Overlay Orthodontic Treatment and the Risk of Hard Tooth Tissue Damage Compared to Traditional Methods—An In Vitro Study" Photonics 12, no. 6: 621. https://doi.org/10.3390/photonics12060621
APA StyleFlorczak-Matyjek, A., Nikodem, A., Kensy, J., Matys, J., & Grzech-Leśniak, K. (2025). The Efficacy of Erbium-Ion, Diode, and CO2 Lasers in Debonding Attachments Used During Overlay Orthodontic Treatment and the Risk of Hard Tooth Tissue Damage Compared to Traditional Methods—An In Vitro Study. Photonics, 12(6), 621. https://doi.org/10.3390/photonics12060621







