Peripheral Wavefront Sensor with Fixation Target Made by Optical Simulation for Measuring Human Eye Regardless of Spectacle
Abstract
1. Introduction
2. Methods
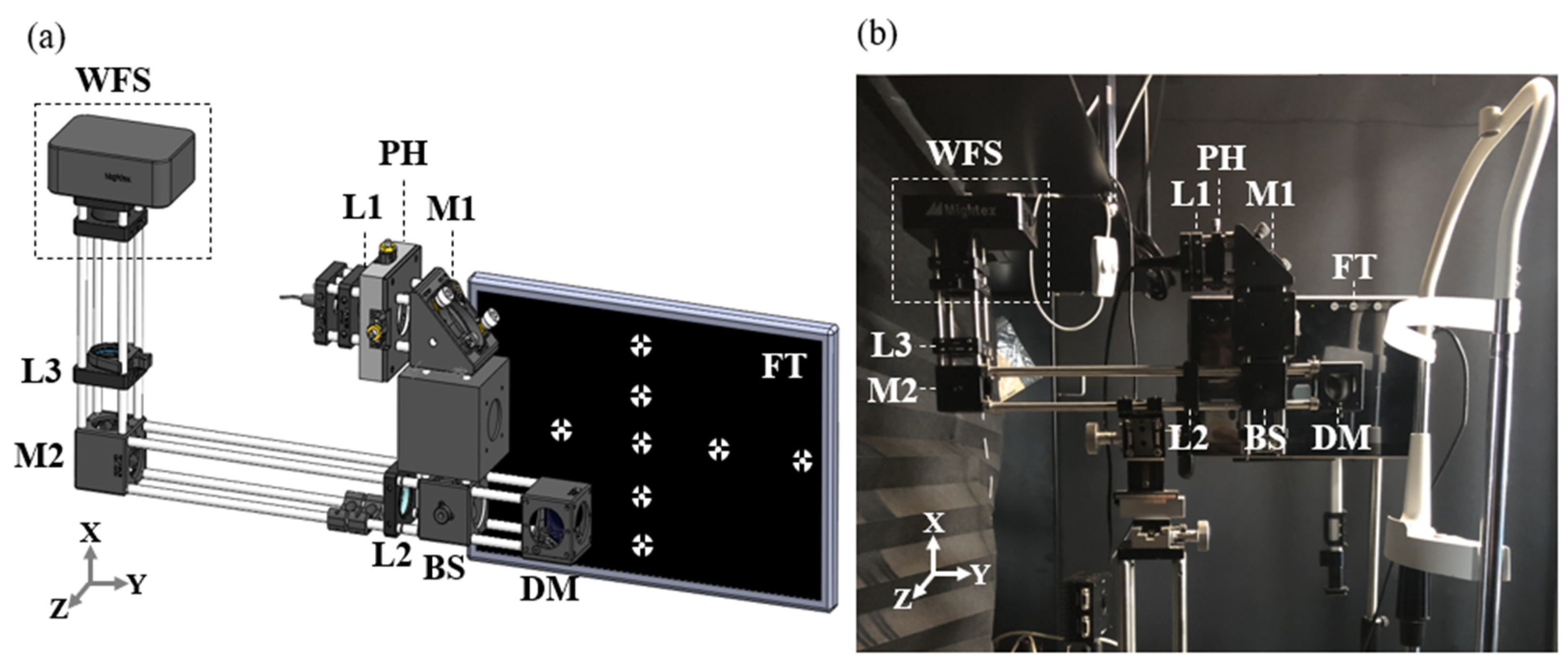
2.1. Hardware and Setting
2.2. Experiment Process
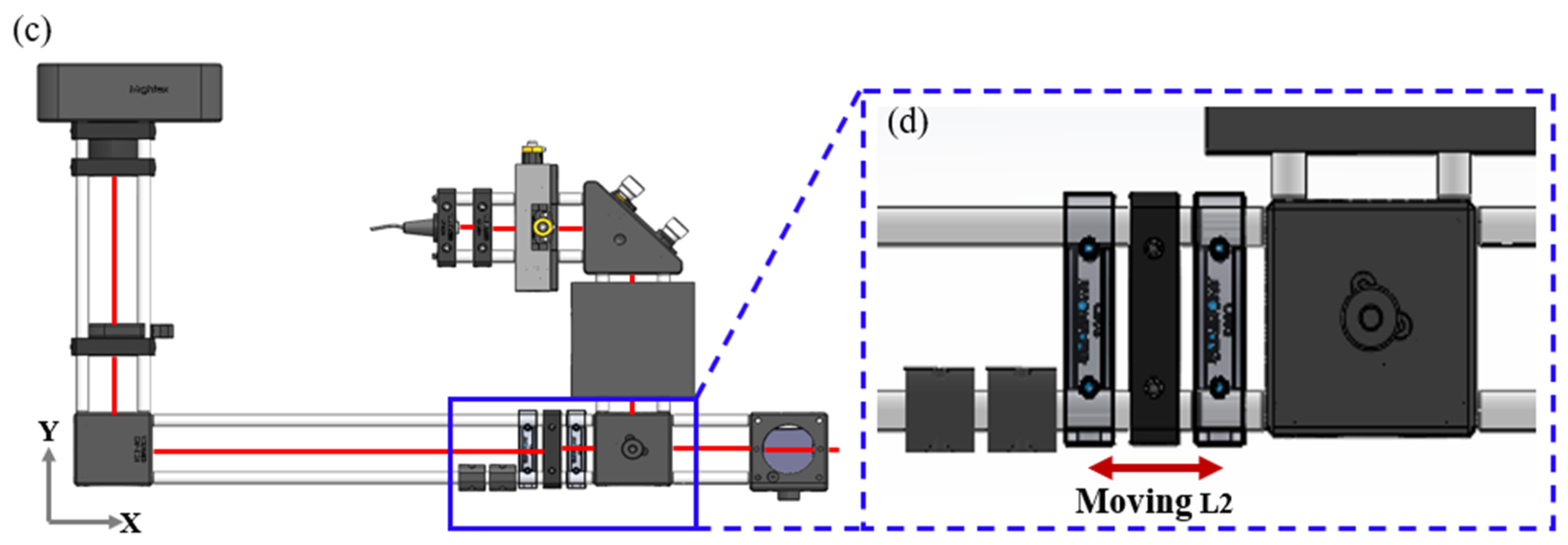
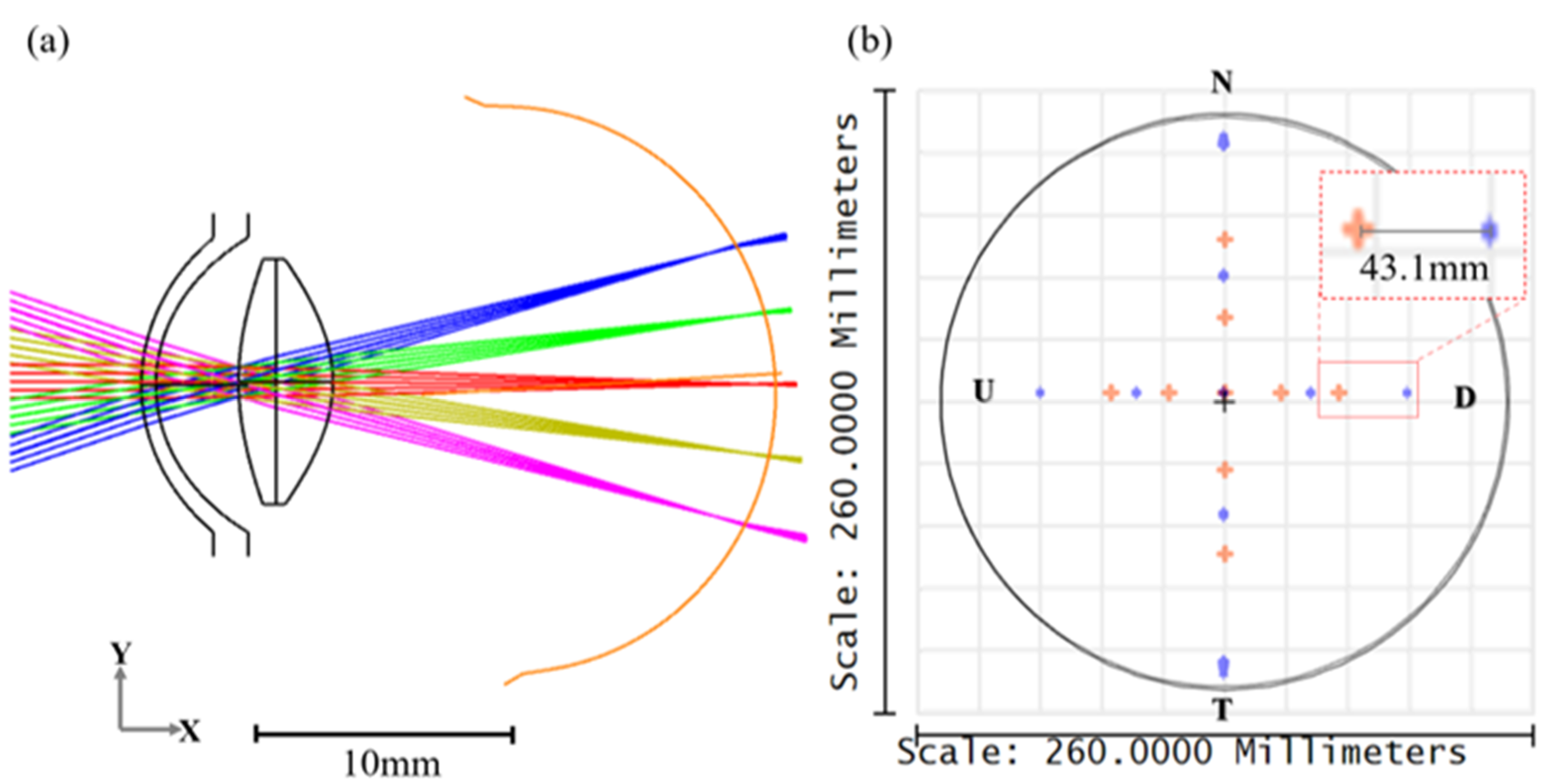
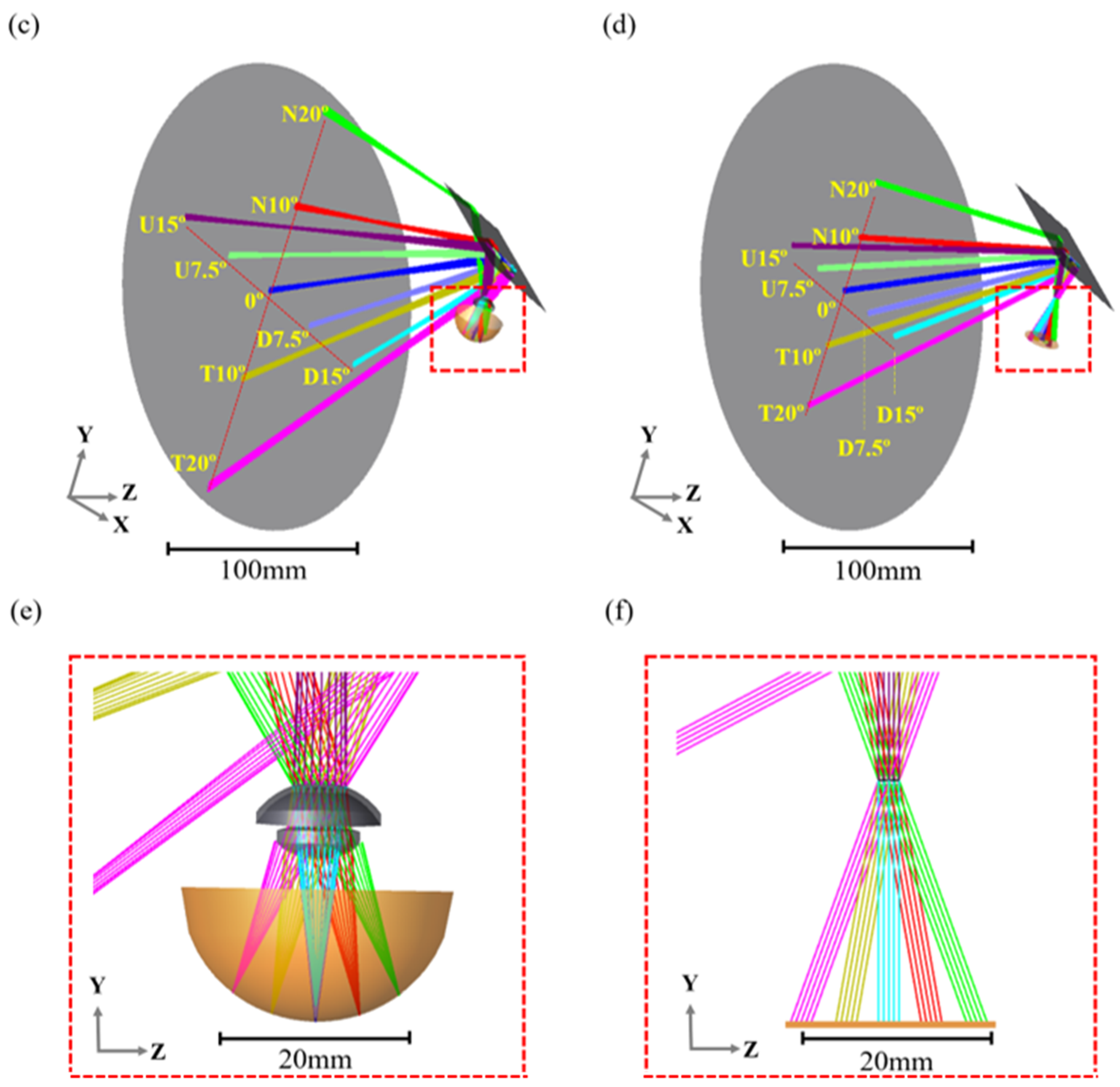
2.3. OpticStudio® Simulation
2.4. Data Acquisition
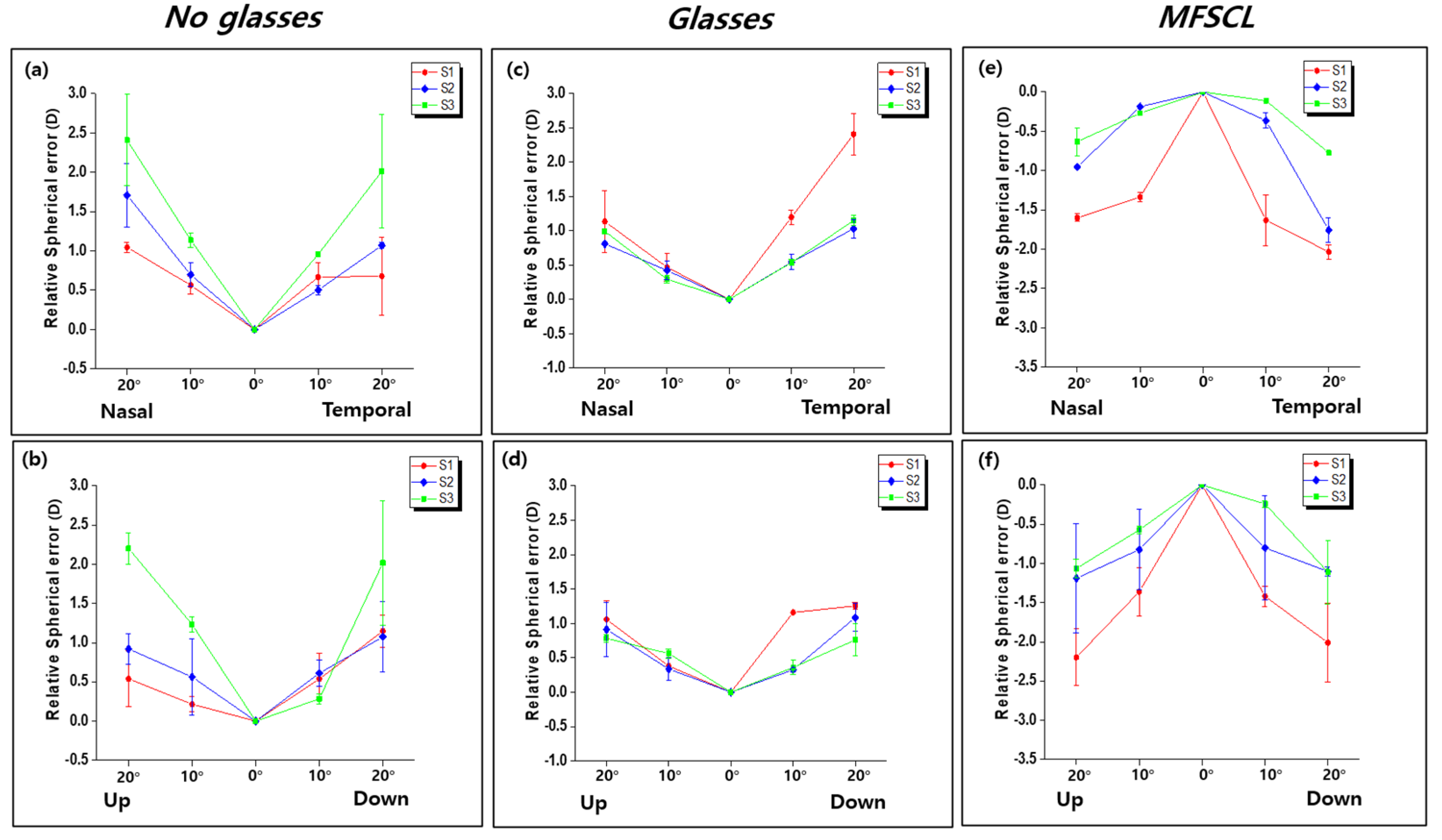
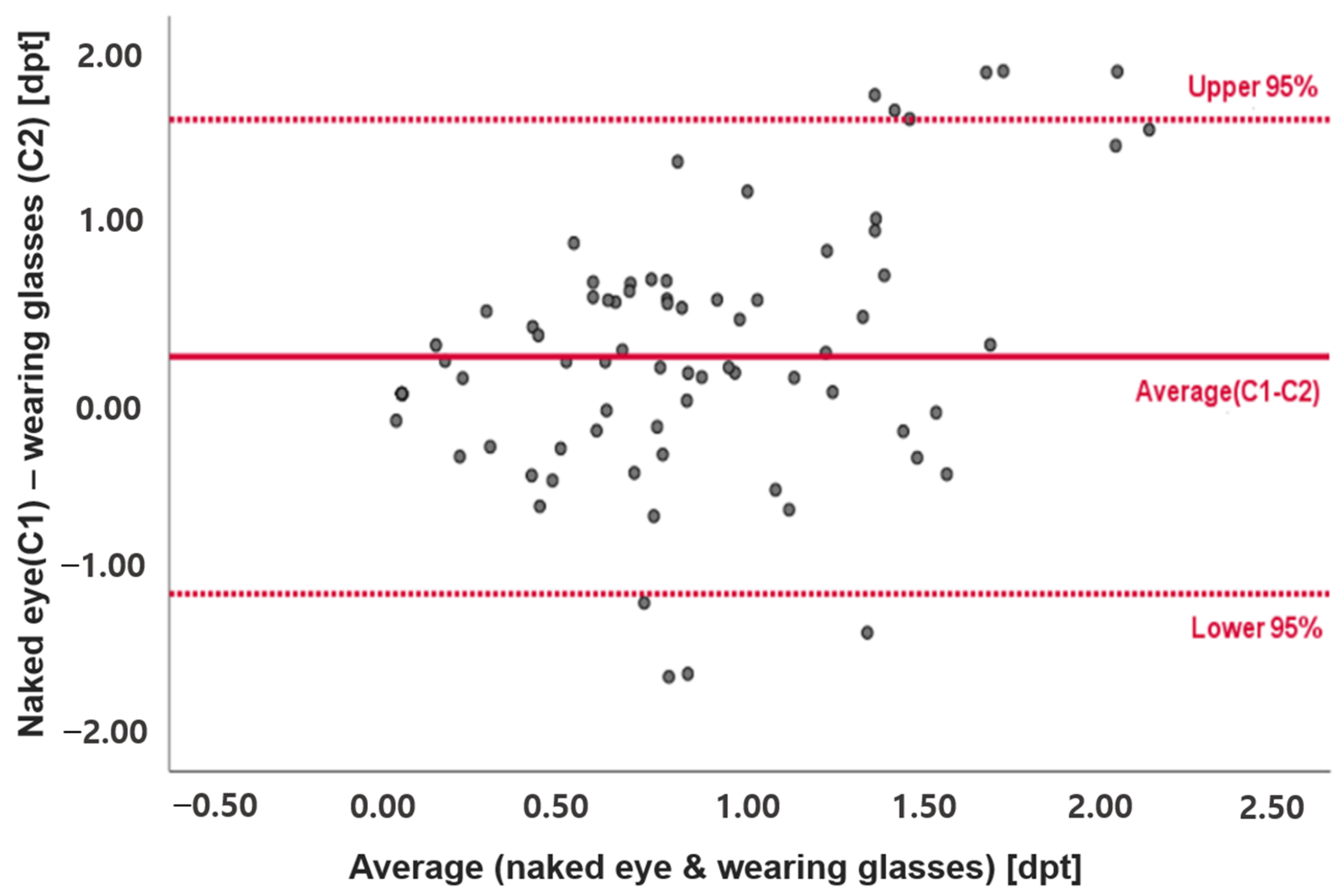
3. Results
3.1. Quantitative Analysis of the Fixation Target
3.2. Data Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rose, K.; Orth, B.; Bmed, W.S.; Morgan, I.; Mitchell, P. Clinical and Epidemiology The increasing prevalence of myopia: Implications for Australia. Clin Exp Ophthalmol. 2001, 29, 116–120. [Google Scholar] [CrossRef] [PubMed]
- Lin, L.; Shih, Y.; Hsiao, C.; Chen, C. Prevalence of Myopia in Taiwanese Schoolchildren: 1983 to 2000. Ann. Acad. Med. Singap. 2004, 33, 27–33. [Google Scholar]
- Vitale, S.; Ellwein, L.; Cotch, M.F.; Ferris, F.L.; Sperduto, R. Prevalence of refractive error in the United States, 1999–2004. Arch. Ophthalmol. 2008, 126, 1111–1119. [Google Scholar] [CrossRef] [PubMed]
- Smith, E.L.; Hung, L.-F.; Huang, J. Relative peripheral hyperopic defocus alters central refractive development in infant monkeys. Vis. Res. 2009, 49, 2386–2392. [Google Scholar] [CrossRef] [PubMed]
- Holden, B.A.; Fricke, T.R.; Wilson, D.A.; Jong, M.; Naidoo, K.S.; Sankaridurg, P.; Wong, T.Y.; Naduvilath, T.; Resnikoff, S. Global Prevalence of Myopia and High Myopia and Temporal Trends from 2000 through 2050. Ophthalmology 2016, 123, 1036–1042. [Google Scholar] [CrossRef] [PubMed]
- Baird, P.N.; Saw, S.-M.; Lanca, C.; Guggenheim, J.A.; Smith, E.L., III; Zhou, X.; Matsui, K.-O.; Wu, P.-C.; Sankaridurg, P.; Chia, A.; et al. Myopia. Nat. Rev. Dis. Primers 2020, 6, 99. [Google Scholar] [CrossRef] [PubMed]
- Sankaridurg, P.; Tahhan, N.; Kandel, H.; Naduvilath, T.; Zou, H.; Frick, K.D.; Resnikoff, S. IMI impact of myo-pia. Investig. Ophthalmol. Vis. Sci. 2021, 62, 2. [Google Scholar] [CrossRef]
- Hung, L.-F.; Crawford, M.; Smith, E.L. Spectacle lenses alter eye growth and the refractive status of young monkeys. Nat. Med. 1995, 1, 761–765. [Google Scholar] [CrossRef] [PubMed]
- Sng, C.C.A.; Lin, X.-Y.; Gazzard, G.; Chang, B.; Dirani, M.; Lim, L.; Selvaraj, P.; Ian, K.; Drobe, B.; Wong, T.-Y.; et al. Change in peripheral refraction over time in Singapore Chinese children. Investig. Opthalmology Vis. Sci. 2011, 52, 7880–7887. [Google Scholar] [CrossRef]
- Smith, E.L. Spectacle lenses and emmetropization: The role of optical defocus in regulating ocular development. Optom. Vis. Sci. 1998, 75, 388–398. [Google Scholar] [CrossRef]
- Saw, S.; Zhang, M.; Hong, R.; Fu, Z.; Pang, M.; Tan, D.T.H. Near-Work Activity, Night-lights, and Myopia in the Singa-pore-China Study. Arch. Ophthalmol. 2020, 120, 620–627. [Google Scholar] [CrossRef] [PubMed]
- Pärssinen, O.; Lyyra, A.L. Myopia and myopic progression among schoolchildren: A three-year follow-up study. Investig. Ophthalmol. Vis. Sci. 1993, 34, 2794–2802. [Google Scholar]
- Mutti, D.O.; Mitchell, G.L.; Hayes, J.R.; Jones, L.A.; Moeschberger, M.L.; Cotter, S.A.; Kleinstein, R.N.; Manny, R.E.; Twelker, J.D.; Zadnik, K.; et al. Accommodative lag before and after the onset of myopia. Investig. Ophthalmol. Vis. Sci. 2006, 47, 837–846. [Google Scholar] [CrossRef] [PubMed]
- Saw, S.-M.; Chua, W.-H.; Hong, C.-Y.; Wu, H.-M.; Chan, W.-Y.; Chia, K.-S.; Stone, R.A.; Tan, D. Nearwork in early-onset myopia. Investig. Ophthalmol. Vis. Sci. 2002, 43, 332–339. [Google Scholar]
- Gwiazda, J.; Thorn, F.; Held, R.; Cruz, A.; Machado, A.; Carvalho, R. Accommodation, accommodative convergence, and response AC/A ratios before and at the onset of myopia in children. Optom. Vis. Sci. 2005, 82, 273–278. [Google Scholar] [CrossRef] [PubMed]
- Sierra, H.; Cordova, M.; Chen, C.S.J.; Rajadhyaksha, M. Peripheral Defocus with Spherical and Multifocal Soft Contact Lenses. J. Investig. Dermatol. 2015, 135, 612–615. [Google Scholar] [CrossRef] [PubMed]
- Yoo, Y.-S.; Kim, D.Y.; Byun, Y.-S.; Ji, Q.; Chung, I.-K.; Whang, W.-J.; Park, M.R.; Kim, H.-S.; Na, K.-S.; Joo, C.-K.; et al. Impact of peripheral optical properties induced by orthokeratology lens use on myopia progression. Heliyon 2020, 6, e03642. [Google Scholar] [CrossRef] [PubMed]
- Lundstrom, L.; Mira-Agudelo, A.; Artal, P. Peripheral optical errors and their change with accommodation differ between emmetropic and myopic eyes. J. Vis. 2009, 9, 17. [Google Scholar] [CrossRef]
- Thibos, L.N.; Wheeler, W.; Horner, D. Power vectors: An application of fourier analysis to the description and statistical analysis of refractive error. Optom. Vis. Sci. 1997, 74, 367–375. [Google Scholar] [CrossRef]
- Lundström, L.; Manzanera, S.; Prieto, P.M.; Ayala, D.B.; Gorceix, N.; Gustafsson, J.; Unsbo, P.; Artal, P. Effect of optical correction and remaining aberrations on peripheral resolution acuity in the human eye. Opt. Express 2007, 15, 12654–12661. [Google Scholar] [CrossRef]
- Wei, X.; Thibos, L. Design and validation of a scanning Shack Hartmann aberrometer for measurements of the eye over a wide field of view. Opt. Express 2010, 18, 1134–1143. [Google Scholar] [CrossRef] [PubMed]
- Jaeken, B.; Lundström, L.; Artal, P. Fast scanning peripheral wave-front sensor for the human eye. Opt. Express 2011, 19, 7903–7913. [Google Scholar] [CrossRef] [PubMed]
- Thaler, L.; Schütz, A.; Goodale, M.; Gegenfurtner, K. What is the best fixation target? The effect of target shape on stability of fixational eye movements. Vis. Res. 2013, 76, 31–42. [Google Scholar] [CrossRef] [PubMed]
- Hirasawa, K.; Okano, K.; Koshiji, R.; Funaki, W.; Shoji, N. Smaller fixation target size is associated with more stable fixation and less variance in threshold sensitivity. PLoS ONE 2016, 11, e0165046. [Google Scholar] [CrossRef] [PubMed]
- Polans, J.; Jaeken, B.; McNabb, R.P.; Artal, P.; Izatt, J.A. Asymmetric wide-field optical model of the human eye with tilted and decentered crystalline lens that reproduces experimentally measured aberrations: Errata. Optica 2018, 5, 1461. [Google Scholar] [CrossRef]
- Yoon, G.; Pantanelli, S.; Nagy, L.J. Large-dynamic-range Shack-Hartmann wavefront sensor for highly aberrated eyes. J. Biomed. Opt. 2006, 11, 30502. [Google Scholar] [CrossRef]
- Williams, D.R.; Vaughn, W.J.; Singer, B.D.; Hofer, H.; Yoon, G.Y.; Artal, P.; Aragón, J.L.; Prieto, P.; Vargas, F. Rapid, Automatic Measurement of The Eyes Wave Aberration. US 6,827,444 B2, 7 December 2004. [Google Scholar]
- Liang, J.; Grimm, B.; Goelz, S.; Bille, J.F. Objective measurement of wave aberrations of the human eye with the use of a Hartmann–Shack wave-front sensor. J. Opt. Soc. Am. A 1994, 11, 1949–1957. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Warnecke, J.M.; Haghi, M.; Deserno, T.M. Unobtrusive health monitoring in private spaces: The smart vehicle. Sensors 2020, 20, 2442. [Google Scholar] [CrossRef]
- Abecassis, V.; Monteiro, D.W.D.L.; Salles, L.P.; Cruz, C.A.D.M.; Belmonte, P.N.A. Impact of CMOS pixel and electronic circuitry in the performance of a Hartmann-Shack wavefront sensor. Sensors 2018, 18, 3282. [Google Scholar] [CrossRef]
- Kim, M.J.; Zheleznyak, L.; MacRae, S.; Tchah, H.; Yoon, G. Objective evaluation of through-focus optical performance of presbyopia-correcting intraocular lenses using an optical bench system. J. Cataract. Refract. Surg. 2011, 37, 1305–1312. [Google Scholar] [CrossRef]
- Chen, L.; Artal, P.; Gutierrez, D.; Williams, D.R. Neural compensation for the best aberration correction. J. Vis. 2007, 7, 9. [Google Scholar] [CrossRef]
- Suliman, A.; Rubin, A. A review of higher order aberrations of the human eye. Afr. Vis. Eye Health 2019, 78, 8. [Google Scholar]
- Lin, Z.; Martinez, A.; Chen, X.; Li, L.; Sankaridurg, P.; Holden, B.A.; Ge, J. Peripheral defocus with single-vision spectacle lenses in myopic children. Optom. Vis. Sci. 2010, 87, 4–9. [Google Scholar] [CrossRef]
- Ruiz-Pomeda, A.; César, V.-C. Slowing the progression of myopia in children with the MiSight contact lens: A narrative review of the evidence. Ophthalmol. Ther. 2020, 9, 783–795. [Google Scholar] [CrossRef]
- Huang, X.; Wang, F.; Lin, Z.; He, Y.; Wen, S.; Zhou, L.; Lu, F.; Jiang, J. Visual quality of juvenile myopes wearing multifocal soft contact lenses. Eye Vis. 2020, 7, 1–8. [Google Scholar] [CrossRef]
- Gifford, K.L.; Richdale, K.; Kang, P.; Aller, T.A.; Lam, C.S.; Liu, Y.M.; Langis, M.; Jeroen, M.; Janis, B.O.; Kathryn, A.R.; et al. IMI–clinical management guidelines report. Investig. Ophthalmol. Vis. Sci. 2019, 60, M184–M203. [Google Scholar] [CrossRef]
- Cheng, D.; Schmid, K.L.; Woo, G.C.; Drobe, B. Randomized trial of effect of bifocal and prismatic bifocal spectacles on myopic progression two-year results. Arch. Ophthalmol. 2010, 128, 12–19. [Google Scholar] [CrossRef]
- Geng, Y.; Schery, L.A.; Sharma, R.; Dubra, A.; Ahmad, K.; Libby, R.T.; Williams, D.R. Optical properties of the mouse eye. Biomed. Opt. Express 2011, 2, 717–738. [Google Scholar] [CrossRef]
- Radhakrishnan, H.; Charman, W.N. Peripheral refraction measurement: Does it matter if one turns the eye or the head? Ophthalmic Physiol. Opt. 2007, 28, 73–82. [Google Scholar] [CrossRef]
- Mathur, A.; Atchison, D.A.; Scott, D.H. Ocular aberrations in the peripheral visual field. Opt. Lett. 2008, 33, 863–865. [Google Scholar] [CrossRef][Green Version]
- Anstice, N.S.; Phillips, J.R. Effect of Dual-Focus Soft Contact Lens Wear on Axial Myopia Progression in Children. Ophthalmology 2011, 118, 1152–1161. [Google Scholar] [CrossRef]
- Sankaridurg, P.; Holden, B.; Smith, E.; Naduvilath, T.; Chen, X.; de la Jara, P.L.; Martinez, A.; Kwan, J.; Ho, A.; Frick, K.; et al. Decrease in rate of myopia progression with a contact lens designed to reduce relative peripheral hyperopia: One-year results. Investig. Ophthalmol. Vis. Sci. 2011, 52, 9362–9367. [Google Scholar] [CrossRef]
- Smith, E.L. Optical treatment strategies to slow myopia progression: Effects of the visual extent of the optical treatment zone. Exp. Eye Res. 2013, 114, 77–88. [Google Scholar] [CrossRef]
- Zhu, Q.; Liu, Y.; Tighe, S.; Zhu, Y.; Su, X.; Lu, F.; Hu, M. Retardation of myopia progression by multifocal soft contact lenses. Int. J. Med. Sci. 2019, 16, 198–202. [Google Scholar] [CrossRef]
- González-Méijome, J.M.; Peixoto-De-Matos, S.C.; Faria-Ribeiro, M.; Lopes-Ferreira, D.P.; Jorge, J.; Legerton, J.; Queiros, A. Strategies to regulate myopia progression with contact lenses: A review. Eye Contact Lens 2016, 42, 24–34. [Google Scholar] [CrossRef]
- Sun, Y.; Xu, F.; Zhang, T.; Liu, M.; Wang, D.; Chen, Y.; Liu, Q. Orthokeratology to control myopia progression: A meta-analysis. PLoS ONE 2015, 10, e0124535. [Google Scholar]
- Cho, P.; Cheung, S.W.; Edwards, M. The longitudinal orthokeratology research in children (LORIC) in Hong Kong: A pilot study on refractive changes and myopic control. Curr. Eye Res. 2005, 30, 71–80. [Google Scholar] [CrossRef]
- Walline, J.J.; Jones, L.A.; Sinnott, L.T. Corneal reshaping and myopia progression. Br. J. Ophthalmol. 2009, 93, 1181–1185. [Google Scholar] [CrossRef]
- Kakita, T.; Hiraoka, T.; Oshika, T. Influence of overnight orthokeratology on axial elongation in childhood myopia. Investig. Opthalmology Vis. Sci. 2011, 52, 2170–2174. [Google Scholar] [CrossRef]
- Santodomingo-Rubido, J.; Villa-Collar, C.; Gilmartin, B.; Gutiérrez-Ortega, R. Myopia control with orthokeratology contact lenses in Spain: Refractive and biometric changes. Investig. Opthalmology Vis. Sci. 2012, 53, 5060–5065. [Google Scholar] [CrossRef]
- Hiraoka, T.; Kakita, T.; Okamoto, F.; Takahashi, H.; Oshika, T. Long-term effect of overnight orthokeratology on axial length elongation in childhood myopia: A 5-year follow-up study. Investig. Opthalmology Vis. Sci. 2012, 53, 3913–3919. [Google Scholar] [CrossRef]

| Subjects | S1 | S2 | S3 |
|---|---|---|---|
| Sex | M | M | M |
| Age | 25 | 26 | 26 |
| Spherical refraction (D) | −2 | −4.75 | −5.0 |
| Astigmatism (D) | 0 | −1.0 | −0.75 |
| Retinal Angle | Conventional Method Distance | Newly Designed® Distance | Conventional Method Angle | Newly Designed® Angle |
|---|---|---|---|---|
| Horizontal 20° | 72.8 mm | 115.9 mm | 20° | 30.09° |
| Horizontal 10° | 35.3 mm | 49.3 mm | 10° | 13.84° |
| Vertical 15° | 53.6 mm | 77.9 mm | 15° | 21.28° |
| Vertical 7.5° | 26.3 mm | 37.3 mm | 7.5° | 10.56° |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oh, S.-K.; Kim, J.-M.; Yoon, G.-Y.; Yoo, Y.-S.; Kim, D.Y. Peripheral Wavefront Sensor with Fixation Target Made by Optical Simulation for Measuring Human Eye Regardless of Spectacle. Photonics 2024, 11, 332. https://doi.org/10.3390/photonics11040332
Oh S-K, Kim J-M, Yoon G-Y, Yoo Y-S, Kim DY. Peripheral Wavefront Sensor with Fixation Target Made by Optical Simulation for Measuring Human Eye Regardless of Spectacle. Photonics. 2024; 11(4):332. https://doi.org/10.3390/photonics11040332
Chicago/Turabian StyleOh, Su-Keun, Jung-Min Kim, Geun-Young Yoon, Young-Sik Yoo, and Dae Yu Kim. 2024. "Peripheral Wavefront Sensor with Fixation Target Made by Optical Simulation for Measuring Human Eye Regardless of Spectacle" Photonics 11, no. 4: 332. https://doi.org/10.3390/photonics11040332
APA StyleOh, S.-K., Kim, J.-M., Yoon, G.-Y., Yoo, Y.-S., & Kim, D. Y. (2024). Peripheral Wavefront Sensor with Fixation Target Made by Optical Simulation for Measuring Human Eye Regardless of Spectacle. Photonics, 11(4), 332. https://doi.org/10.3390/photonics11040332





